Abstract
New financial penalties for institutions with high readmission rates have intensified efforts to reduce rehospitalization. Several interventions that involve multiple components (e.g., patient needs assessment, medication reconciliation, patient education, arranging timely outpatient appointments, and providing telephone follow-up), have successfully reduced readmission rates for patients discharged to home. The effect of interventions on readmission rates is related to the number of components implemented, whereas single-component interventions are unlikely to reduce readmissions significantly. For patients discharged to post-acute care facilities, multicomponent interventions have reduced readmissions through enhanced communication, medication safety, advanced care planning, and enhanced training to manage common medical conditions that commonly precipitate readmission. To help hospitals direct resources and services to patients with greater likelihood of readmission, a number of risk stratification methods are available. Future work should better define the role of home-based services, information technology, mental health care, caregiver support, community partnerships, and new transitional care personnel.
Keywords: Transitions of care, Hospital discharge, Readmission risk, Post-acute care
In recent years, widespread and intense efforts to reduce excess hospital readmissions have been spurred by heightened awareness of both the prevalence of readmission as well as new financial penalties linked to readmission rates. In this review, we will summarize the prevalence of hospital readmission, approaches to reduce readmission for patients discharged to home or to post-acute care (PAC) facilities, and methods to identify patients at high-risk of readmission. We will also note several areas where additional work is needed.
Prevalence of Hospital Readmission
Though readmission rates in the United States have been high for many years, Jencks and colleagues brought this issue to the forefront with their landmark 2009 article.(1) Analyzing 2003–2004 claims data, they demonstrated that 19.6% of Medicare beneficiaries were readmitted to the hospital within 30 days of discharge, and 34.0% were readmitted within 90 days. Medical and surgical patients were both affected, though medical patients had a higher readmission rate (21.1% vs. 15.6% among surgical patients at 30 days) and accounted for 77.1% of the rehospitalizations. The highest 30-day readmission rates were observed for patients with heart failure (26.9%), psychoses (24.6%), recent vascular surgery (23.9%), chronic obstructive pulmonary disease (22.6%), and pneumonia (20.1%). During the last decade, risk-adjusted 30-day readmission rates among Medicare beneficiaries have remained relatively constant.(2)
Readmission rates have been documented in other populations as well. For example, in Veterans Affairs hospitals, the 30-day all-cause readmission rate was 15.2% in 2009–2010.(3) In 2007, the 30-day readmission rate among non-elderly adults (age 21–64, excluding obstetric admissions) was approximately 10.7% for patients with Medicaid and 6.3% for patients with private insurance.(4)
Public Reporting and Penalties
In an effort to drive down rates of hospital readmissions, the Centers for Medicare and Medicaid Services (CMS) has publicly reported risk-standardized readmission rates for acute heart failure, pneumonia, and myocardial infarction since 2009.(5) Beginning in 2013, readmission rates following total hip and/or total knee replacement as well as hospital-wide unplanned readmission rates will be added. Each measure has a rigorous risk-adjustment methodology that controls for differences in hospitals’ patient population.(6–8) These models, however, rely primarily on the presence of comorbid conditions, as determined from claims data, and do not account for other factors associated with a successful transition to home, such as patient race, health literacy, socioeconomic status, social support, community resources, or practice patterns.(9–11) Thus, their ability to level the playing field for comparing hospital performance is somewhat limited.(9; 10)
The cost of readmissions to the health care system is substantial, accounting for an estimated $17.4 billion in spending annually by Medicare alone.(1) The Hospital Readmissions Reduction Program (HRRP), established in the Affordable Care Act,(12) authorizes Medicare to reduce payment to hospitals with excess readmission rates. The penalties are based on a calculation of the risk-standardized 30-day readmission rate for the previous three years for Medicare beneficiaries hospitalized with heart failure, pneumonia, or acute myocardial infarction, though it is expected that other conditions will soon be added. Hospitals with higher than expected readmission rates are penalized a percentage of their total CMS reimbursement, beginning at 1% in year 1 of the program, up to 3% in year 3. These financial penalties have produced the intended outcome of intensifying hospital efforts to reduce excess readmissions.
These initiatives are based on the notion that readmissions reflect the quality of care. Many disagree, however, with the adoption of 30-day all-cause readmissions as a quality metric for diverse reasons.(10; 13; 14) First, although it may be reasonable to hold hospitals accountable for problems that patients experience during the first week after discharge, readmissions occurring after that may increasingly reflect patient self-management, outpatient care, community resources, or the development of new problems that go beyond the control of the discharging hospital.(10) Second, it is unclear what proportion of readmissions are truly preventable, as estimates range from 5% to 79%, with a median of 27%.(15) Third, hospital readmission rates are not meaningfully related to other performance measures that are accepted to be valid reflections of hospital quality.(16) Fourth, academic institutions and hospitals in socioeconomically disadvantaged areas are disproportionately affected by the new readmission penalties.(17) This has raised concern that institution of these penalties may exacerbate existing health disparities. Finally, because CMS penalties are based on 3-year performance, if hospitals do successfully reduce their readmission rates, the financial benefit will not be seen immediately, and will be realized only if improvements are sustained.
Interventions for Patients Discharged from Hospital to Home
These concerns notwithstanding, given current policies, hospitals are seeking a path forward to reduce readmissions. A review of common issues that arise during transitions of care is available,(18) as are recent reviews that summarize interventions to reduce hospital readmission,(19) improve patient safety at hospital discharge,(20) enhance medication reconciliation,(21) and improve handovers from the hospital to the outpatient setting.(22) Publications have also highlighted the role of ambulatory care practices in fostering more effective transitions in care.(23; 24) Here we will focus on interventions to reduce readmission, most of which are hospital-initiated.
Hansen and colleagues performed a systematic review of 43 interventions to reduce 30-day hospital readmission.(19) Overall, the quality of studies was low, with only 16 being randomized controlled trials (RCTs). Most studies (56%) tested the effect of single-component interventions, while the remainder tested bundles. The authors described a taxonomy of intervention components including broad categories of predischarge interventions (e.g., patient education, discharge planning, medication reconciliation, appointment scheduled before discharge); postdischarge interventions (e.g., timely follow-up, timely PCP communication, follow-up telephone call, patient hotline, home visit); and bridging interventions (e.g., transition coach, patient-centered discharge instructions, provider continuity). The most common categories of interventions were patient education, discharge planning, follow-up telephone call, patient-centered discharge instructions, and discharge coaches or nurses who interacted with the patient before and after discharge. Of interest (and concern), the authors found no consistent evidence from RCTs that any one intervention by itself significantly reduced hospital readmission. Of the 16 RCTs, only 5 yielded significant reductions in hospital readmission. One of these provided early discharge planning (a single-component intervention) to high-risk patients.(25) One small pilot study(26) and three larger investigations(27–29) implemented multicomponent intervention bundles, which resulted in absolute reductions in 30-day readmission of 3.6 to 28 percentage points. The latter three interventions merit additional description, as they are often given as examples of how health care systems can successfully reduce readmission (Table).
Table.
Selected multi-component transitional care interventions tested in randomized controlled trials.
| Author, year | Intervention | Setting; study sample | Key elements | Outcomes |
|---|---|---|---|---|
| Naylor, 1994(27) | Comprehensive discharge planning | Academic hospital in Philadelphia; Community-dwelling elders with selected medical and surgical conditions,a and their caregivers |
Advanced practice nurse:
|
Reduced readmission rate for medical patients at 6 weeks (10% vs. 23%, p<0.05) |
| Coleman, 2004(28) | Care Transitions Intervention | Not-for-profit health system in Colorado; Community-dwelling elders with selected medical and surgical conditionsb |
Nurse transition coach:
|
Reduced readmission rate at 30 days (8.3% vs. 11.9%, p<0.05) and 90 days (16.7% vs. 22.5%, p<0.05) in adjusted analysis |
| Jack, 2009(29) | Project Reengineering Discharge (RED) | Safety-net hospital in Boston; Adults admitted to medical teaching services |
Nurse discharge advocate:
|
Reduced hospital utilization (combined endpoint of emergency department visits and rehospitalization) at 30 days, incidence rate ratio = 0.695 (95% CI, 0.515 to 0.937) |
Congestive heart failure, angina/myocardial infarction, coronary artery bypass grafting, cardiac valve replacement.
Stroke, congestive heart failure, coronary artery disease, cardiac arrhythmias, chronic obstructive pulmonary disease, diabetes, spinal stenosis, hip fracture, peripheral vascular disease, deep venous thrombosis, pulmonary embolism.
Naylor’s model utilizes an advanced practice nurse who meets with the patient and caregiver in the hospital, performs a structured needs assessment, and provides comprehensive discharge planning including education and coordination of post-discharge services.(27) Post-discharge telephone follow-up includes reinforcement of education, monitoring of symptoms and progress, and adjustment of the care plan as needed. The intervention reduced readmissions during the first 6 weeks after discharge among medical patients.(27) A more intensive form of the intervention that included home visits was also effective in reducing rehospitalization among high-risk elderly patients.(30)
The Care Transitions Intervention (CTI), developed by Coleman,(31) utilizes a nurse transition coach who educates and empowers patients to better navigate their own care. The CTI emphasizes four “pillars” – medication self-management, a patient-owned health record, follow-up with a primary care provider or specialist, and awareness of red flags. The intervention lowered 30- and 90-day readmission rates in an RCT,(28) and also reduced readmissions in a real-world effectiveness study.(32)
Project Reengineering Discharge (RED), developed by Jack and colleagues,(33) addresses both the system and patients’ navigation of the discharge process through 11 mutually reinforcing components (Table). When implemented in an urban university hospital by nurse discharge advocates, participants randomized to the intervention group had a lower rate of 30-day hospital utilization (emergency department visits and rehospitalizations).(29)
Overall, this literature demonstrates that singular interventions (e.g., providing patient education or scheduling follow-up) are unlikely to significantly reduce hospital readmission.(19) Multifaceted intervention bundles are likely necessary for substantial improvement in readmission rates. Although the above multicomponent initiatives differ substantially in their approach, they all bridge the hospital and post-discharge periods with dedicated transitional care personnel, patient-centered discharge instructions, and telephone follow-up. To our knowledge, no studies have been published regarding the comparative effectiveness of these different approaches. Thus, it has been challenging for health systems to know what combination of interventions to deploy.
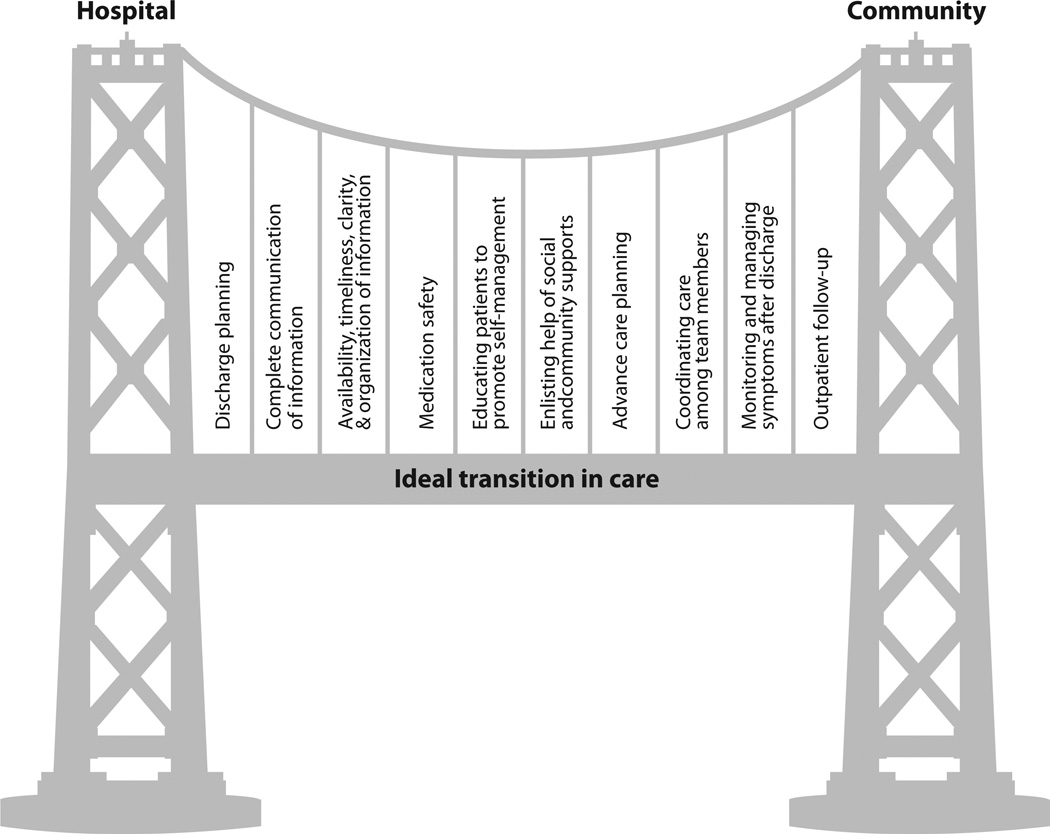
We recently described a framework – the Ideal Transition in Care – that assimilates the key components of transitional care interventions into a single model.(14) The Ideal Transition framework posits that multiple interventions across the continuum of care from hospital to home are needed to support the hospital discharge transition, and that the strength of the transition depends on the number of intervention components that span this continuum. There are 10 key components to an Ideal Transition including discharge planning, medication safety, advance care planning, coordination among team members, and follow-up (Figure).
Figure.
The Ideal Transition in Care framework. (Reprinted with permission)
Burke and colleagues recently performed an updated systematic review, mapping transitional care interventions to the 10-component Ideal Transition in Care framework.(34) They included 61 interventions, 42 of which have been studied in RCTs. The number of components included in prior interventions ranged from 1 to 8, with an average of 3.5. The most common components included were patient education (with an emphasis on promoting self-management), medication safety, and coordination of care. Just under half (47.5%) of interventions demonstrated a statistically significant reduction in readmissions. Consistent with prior reviews, no singular intervention component significantly reduced readmissions, though a trend was present for patient education and engaging social and community supports (p=0.06 for each). The only significant predictor of success in reducing readmissions was the number of domains included in the intervention (p=0.002). Others have also recently shown that the number of strategies employed by hospitals is significantly associated with 30-day risk-standardized readmission rates in heart failure.(35)
Interventions for Patients Discharged to Post-Acute Care Facilities
A substantial proportion of patients cared for in the hospital require subsequent treatment in a post-acute care (PAC) facility, which may include either a skilled nursing or rehabilitation facility. Among patients > 65 years of age, discharges to PAC facilities account for roughly 28% of all hospital discharges.(36) Although this represents the minority of all hospital discharges, this population accounts for a substantial proportion of overall and disease specific hospital readmissions. Among Medicare beneficiaries discharged to a PAC facility in 2006, nearly 25% of patients were readmitted within 30 days at a cost of $4.34 billion.(37) The rate of readmissions from PAC has increased by as much as 30% since 2000,(37) and is especially high in some conditions, such as congestive heart failure.(38; 39)
Many factors affect the readmission rate among patients in PAC facilities. The decision to rehospitalize a post-acute care patient is influenced by a) patients’ condition and preferences, b) PAC preferences and characteristics, and c) the influence of local, state, and national policies.(40) Patients discharged to PAC facilities tend to be older, have increased number of comorbidities, increased medication burden, higher severity of illness, and more deficits in cognition and/or function when compared to patients discharged to home. It is not surprising that these factors are associated with increased risk of admission or readmission from PAC.(41–46) In addition to severity of illness and comorbidities, patient and caregiver goals of care (including do-not-resuscitate orders) are highly predictive of hospital readmission from a PAC setting.(44; 47) For example, O’Malley found that the presence of advanced directives increased the time between hospitalization among nursing home patients.(44) Factors specific to PAC settings also influence the risk of hospitalization. These include communication barriers between the hospital and PAC facility,(48; 49) communication barriers within individual PAC facilities,(49) limited resources and training,(50) quality of care,(44; 47) and staffing patterns (e.g., nurse retention and level of physician engagement).(51) Finally, financial incentives and broader health policies further increase readmission risk. The historical lack of accountability for hospital readmissions has previously allowed hospitals to benefit financially from rehospitalization and impeded motivation to better coordinate care between the acute and post-acute care settings.
Reducing readmissions from PAC facilities will require approaches that address patient, PAC facility, and policy factors that influence rehospitalization. Fewer controlled studies in this context are available to guide practice, but the published literature does allow recommendations to be made. As with discharges to home, multicomponent interventions are more likely to have sustainable success.(19; 52) Importantly, preventive steps should be initiated early in the acute hospital stay for patients at high risk for discharge to PAC. This group includes patients admitted from PAC facilities as well as patients identified on the basis of symptom burden or a validated prediction tool.(53; 54) Once identified, special attention must be paid to preparing the patient for the next phase of their care in the PAC setting. This includes attention to medication reconciliation, polypharmacy, and discontinuation of high-risk geriatric medications when not indicated.(43; 55) For example, antipsychotic medications initiated in the acute care setting for agitated delirium are often continued without indication and potentially increase the risk for rehospitalization.(43; 46; 56) In addition, care should be made to minimize the use of urinary catheters, peripherally inserted central catheters (PICC lines), and other indwelling devices at the time of discharge, as these present potential safety hazards and increased risk of rehospitalization.(55; 57; 58) Finally, patients transitioning to PAC facilities should be included in routine advanced care planning discussions. These should provide adequate information about short- and long-term prognosis, expectations about the PAC setting, and discussion of goals of care to ensure that future healthcare decisions align with patient preferences. Each of these steps (i.e., medication safety, elimination of safety hazards, advanced care planning) should be continued and reinforced in the post-acute setting.(59; 60)
Multicomponent interventions such as Interventions to Reduce Acute Care Transfers (INTERACT) and Project RED include each of these components.(52; 61–63) In addition, these programs employ additional tools to enhance inter- and intra-facility communication, care pathways and training to manage common medical conditions that may precipitate rehospitalization, and enhanced follow-up procedures (e.g., early follow-up appointments, patient phone calls) to ensure continuity of care following PAC discharge. INTERACT is the most rigorously studied of the multicomponent PAC interventions, all of which are laid out in a comprehensive fashion on their web site available at http://interact2.net/. INTERACT has been studied in as many as 25 community skilled nursing facilities.(52) Following six months of biweekly training by an experienced nurse practitioner, participating facilities experienced a 17% reduction in self-reported hospital admissions compared to the same 6 month period from the year prior. Among the most engaged facilities reductions were as high as 24%.(52)
Identification of High-Risk Patients
Applying high-intensity, multifaceted efforts to all inpatients may not be possible for many institutions, so there has been much interest in predicting patients at highest risk of rehospitalization to allow for targeted intervention. Three studies have specifically applied transitional interventions only to high-risk patients, reporting absolute risk reduction of 30-day readmissions by 11 to 28 percentage points.(25; 26; 30) These studies used simple checklists of various risk criteria to enroll patients, most frequently including increased age, presence of multiple medical comorbidities, functional impairment, poor social support, and prior healthcare utilization.
High-risk patients may also be identified through readmission risk prediction models, a number of which have been developed and validated during the last 30 years.(9) When considering the value of these models, several aspects must be taken into consideration, including model complexity, data availability, and model performance. The simplest approaches are ideal for busy clinicians and frequently only contain four or five variables.(64) In contrast, other models include more than 90 separate variables and take advantage of the breadth of administrative data available.(65) In general, there is some trade-off between ease of use and discriminative ability of the model. It is important for individuals and institutions to carefully consider the goal of their risk prediction when selecting a model for use.
Another important consideration in model selection is the timing of data availability. In order for a readmission risk score to be most clinically useful, it must be calculable early enough during the index hospitalization to allow time for intervention.(9) Many of the prediction models developed using large administrative databases include variables that are not readily available early in a hospitalization, such as total length of stay and whether the patient is discharged to a skilled nursing facility.(65; 66) While these models may have utility for purposes of risk adjustment and hospital comparison, they are less practical for real-time clinical prediction.
Model performance or discriminative ability has been a topic of much debate. Predictive ability is most commonly measured by comparing the C-statistic. A C-statistic of 0.8 or greater indicates excellent discriminative capability, while a value of 0.7 to 0.8 is considered adequate, and less than 0.7 is suboptimal.(67) A recent systematic review found that the majority of existing readmission models had only a modest ability for accurate prediction, with only six studies to date reporting a C-statistic of greater than 0.7.(9) This may be due in part to the fact that most existing models rely heavily on comorbidities, prior hospitalizations, and basic demographic information. Few have evaluated other factors linked to readmission such as health literacy, functional impairment, language barriers, and level of social support.(9; 14) A small number of studies have begun to evaluate the effect of including these factors, and have generally found that the combination of administrative data, comorbidities, and self-reported variables performs better than any one category alone.(68–70)
Prediction models also may perform better when they are tailored to the specific patient population. Factors affecting readmission rates vary based on discharge destination (home vs. PAC facility) as well as by socioeconomic condition and primary diagnosis. CMS has sponsored the development of several methodologically sound models specific to discharge diagnosis,(6–8) though they only utilize administrative data and perform modestly, with C-statistics ranging from 0.60 to 0.66.(9) Disease-specific risk prediction models have been reported elsewhere in the literature for acute myocardial infarction and heart failure,(71; 72) as well as stroke and chronic obstructive pulmonary disease.(73; 74)
Although most models have limited ability to accurately predict the probability of readmission for any one patient, most are at least able to stratify patients into low and high risk groups.(68; 70) Some programs have correspondingly adopted more a qualitative approach to both risk assessment and intervention. Project BOOST (Better Outcomes for Older adults through Safe Transitions), led by the Society of Hospital Medicine, employs a simple risk tool assessing eight patient factors that contribute to readmission risk.(75) Each identified risk factor is then paired with suggestions for specific interventions to mitigate risk and reduce readmissions. A related strategy that we are using in our own work is to perform a structured assessment of patients’ transitional care needs and provide tailored support delivered by a dedicated transition care coordinator. This needs assessment focuses on intervenable risk factors, such as understanding of medications, functional status limitations, and the need for timely follow-up. This strategy also directs the greatest assistance to patients who have the greatest needs.
New Frontiers and Areas Where Additional Work Is Needed
As the number of transitional care interventions grows, we will see an increase in reports of both positive and negative studies. Authors should carefully describe their patient selection and intervention components, as well as details of how the intervention was implemented (e.g., for telephone calls – who called, when, how often, and what was discussed), so that the most effective approaches can be determined and replicated.(76) In addition, a number of specific areas warrant further investigation and consideration in the next generation of care transition interventions. These include home-based services, telemonitoring and other information technology, mental health care, caregiver engagement and support, partnerships with the community and other healthcare facilities, and role definition for new transitional care personnel.
In the home setting, further work is needed to understand what type and intensity of services should be offered after discharge to reduce unplanned readmissions. Some successful readmission reduction programs have included home visits.(28; 30) However, there is no consistent evidence that home visits reduce readmission rates in the absence of larger coordinated efforts.(77) If linkages between the hospital and outpatient setting improve, home health may provide a natural bridge, warranting further study as the standard of care changes.
Information technology (IT) provides an appealing prospect both for monitoring and as a means of intervention. Telehealth monitoring provides both of these opportunities, but has not been widely incorporated into current care transition interventions. Early studies showed potential benefit of telemonitoring for disease management, though a large trial showed no reduction in readmission rates.(78) Nevertheless, this and other technologies must be considered anew within the context of larger multifaceted interventions. As the number of care transition-related IT products increases, further work will be necessary to clarify which of these products are most clinically effective, cost-effective, and for which populations.
Comorbid psychiatric disease and substance abuse increase the risk of readmission.(9; 79) Among adults admitted with mental health conditions, small studies have tested approaches to reduce psychiatric rehospitalization.(80) However, among medical inpatients, addressing psychiatric disease and substance abuse has not been a focus of most transitional care interventions. Efficient and effective strategies are needed to treat patients with depression, anxiety, schizophrenia, and substance abuse in this setting. Incorporating behavioral therapy in the hospital, during home health visits, and in the ambulatory care setting may be beneficial and warrants further study.
Enhancing the discharge process may be best achieved with robust engagement of caregiver and family support when available. Successful interventions have included caregivers longitudinally throughout the discharge process,(28–30) particularly as it relates to education, medication counseling, and planning outpatient follow-up. Yet an area that needs additional exploration is support to caregivers themselves. Caregivers are at higher risk of depression and heart disease,(81; 82) and even experience higher mortality rates.(83) Teaching patients and their families strategies for self-care, empowerment and advocacy are proving to be useful tactics, but new models to adequately support caregivers and provide necessary respite are needed.
Community partnerships are emerging as one meaningful way for hospitals to successfully reduce readmissions. The CMS Community-based Care Transitions Program (CCTP) represents a large, formal network of organized partnerships between acute-care hospitals and community-based organizations.(84) The community organizations provide timely care transition services for patients after hospital discharge, monitor performance, and provide feedback to CMS. Initiatives involving congregations are another way to engage the community and leverage local support structures to better meet patients’ needs. For example, the Memphis Congregational Health Network is a hospital-community partnership involving more than 500 area churches. It has reported significant reductions in readmission and mortality, as well as higher patient satisfaction scores.(85) Other partnerships involve hospitals establishing post-discharge follow-up clinics or collaborating with post-acute care facilities.(86; 87) Such partnerships will require commitment from multiple area institutions, but may be necessary in order to achieve substantial and sustainable reductions in readmissions. The formation of accountable care organizations and the advent of bundled payments may help foster the necessary collaboration across these settings.(12)
The period of time of transitioning from the hospital to home or the post-acute care setting is now fully recognized as a critical period of a patient’s illness, and one that requires unique and specific skills to achieve optimal outcomes. New members and roles on the health care team are emerging with this new recognition. New transition care personnel may include transition coaches, discharge advocates, and transition care coordinators, as well as expanded roles for home health providers, advanced practice nurses, case managers, mental health providers, and social workers. These valuable personnel can help arrange services, coordinate care, and help ensure that patient and family preferences are respected. One important area related to hospital utilization is performing advanced care planning to establish goals of care and circumstances under which patients prefer additional hospital care, particularly for patients with poor functional status or limited life expectancy. These new team members will need to be integrated into health care teams so that their skills can be optimally used, and new compensation structures developed to appropriately reimburse their involvement in patient care.
Conclusions
Reducing readmissions has become a mandate for hospitals across the United States, hastened by implementation of public reporting and financial penalties for excess readmissions. However, despite an immediate need to improve the quality of discharge planning and transitional care, there is limited high-quality evidence outlining how to best accomplish this. The scientific literature shows that individual interventions are unlikely to significantly reduce readmission rates.(19) In contrast, some multifaceted interventions have been successful in this regard.(27–30) Effective interventions share certain features: having multiple components that span both inpatient and outpatient settings and delivery by dedicated transitional care personnel. New evidence suggests that the number of components in a care transitions intervention is significantly related to its effectiveness,(34; 35) which strengthens the argument for more robust interventions.
Multifaceted interventions require substantial resources for planning, implementation, and monitoring. Though transitional care interventions may be cost-effective in certain settings,(28–30) hospitals will each need to determine their current level of performance, the amount of financial penalty that can potentially be recouped, what resources they already have in place, and what new resources they can allocate to readmission reduction efforts in light of other quality and safety initiatives. In making this assessment, it is useful to also consider other improvements that may result from a greater focus on transitions, such as more efficient processes of care, better teamwork, improved patient satisfaction, and improved performance in other areas of quality and safety.(20)
Given the resources required, it is reasonable for hospitals to focus efforts on patients at higher risk of readmission. These patients may be identified either on the presence of certain characteristics (advanced age, polypharmacy, decreased functional status, etc.)25,26,30 or by using predictive models that quantify the risk of readmission.(9) At present, it is uncertain which of these approaches is superior, but either can provide some stratification for the allocation of resources and attention. Using a structured needs assessment to identify areas of concern and provide focused resources to patients may prove to be an effective way to tailor assistance to patients’ needs.
As efforts unfold to reduce readmissions, it will be critical to rigorously assess their effectiveness and sustainability. To the extent that some readmissions are preventable, and that being readmitted is undesirable for most patients, reducing avoidable readmissions presents a potentially large opportunity to reduce cost, improve quality, and improve the patient experience simultaneously.
Acknowledgments
Funding Acknowledgements
Dr. Theobald is supported by the Office of Academic Affiliations, Department of Veterans Affairs, VA National Quality Scholars Program, and this work was made possible by the use of the facilities at VA Tennessee Valley Healthcare System, Nashville, Tennessee.
Dr. Vasilevskis was supported by the National Institute on Aging of the National Institutes of Health under Award Number K23AG040157 and the Veterans Affairs Clinical Research Center of Excellence, and the Geriatric Research, Education and Clinical Center (GRECC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans’ Affairs.
Footnotes
Disclosures
Dr. Kripalani is a consultant to and holds equity in PictureRx, LLC, which makes patient education materials; and has a consulting agreement with Amedisys, Inc. Neither company played a role in the preparation of this review article. Drs. Theobald and Vasilevskis and Mrs. Anctil do not have relevant conflicts of interest to disclose.
Contributor Information
Sunil Kripalani, Email: sunil.kripalani@vanderbilt.edu.
Cecelia N Theobald, Email: cecelia.theobald@vanderbilt.edu.
Beth Anctil, Email: beth.anctil@vanderbilt.edu.
Eduard E Vasilevskis, Email: ed.vasilevskis@vanderbilt.edu.
Literature Cited
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N. Engl. J. Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Joynt KE, Jha AK. Thirty-day readmissions--truth and consequences. N. Engl. J. Med. 2012;366:1366–9. doi: 10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 3.Kaboli PJ, Go JT, Hockenberry J, Glasgow JM, Johnson SR, et al. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann. Intern. Med. 2012;157:837–45. doi: 10.7326/0003-4819-157-12-201212180-00003. [DOI] [PubMed] [Google Scholar]
- 4.Jiang HJ, Wier LM. HCUP Statistical Brief #89. Agency for Healthcare Research and Quality, Rockville, MD; Apr, 2010. All-Cause Hospital Readmissions among Non-Elderly Medicaid Patients. Available at http://www.hcup-us.ahrq.gov/reports/statbriefs/sb89.pdf. [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services. [Accessed July 15];Hospital Compare. 2013 Available at www.hospitalcompare.hhs.gov.
- 6.Krumholz HM, Normand ST, Keenan PS, Desai MM, Lin Z, et al. [Accessed July 17];Hospital 30-day acute myocardial infarction readmission measure methodology. 2013 Available at: http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2Fpage%2FQnetTier3&cid=1219069855841.
- 7.Krumholz HM, Normand ST, Keenan PS, Desai MM, Lin Z, et al. [Accessed July 17];Hospital 30-day pneumonia readmission measure methodology. 2013 Available at: http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2Fpage%2FQnetTier3&cid=1219069855841.
- 8.Krumholz HM, Normand ST, Keenan PS, Desai MM, Lin Z, et al. [Accessed July 17, 2013];Hospital 30-day heart failure readmission measure methodology. 2008 Available at: http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2Fpage%2FQnetTier3&cid=1219069855841.
- 9.Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–98. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joynt KE, Jha AK. A path forward on Medicare readmissions. N. Engl. J. Med. 2013;368:1175–7. doi: 10.1056/NEJMp1300122. [DOI] [PubMed] [Google Scholar]
- 11.Calvillo-King L, Arnold D, Eubank KJ, Lo M, Yunyongying P, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J. Gen. Intern. Med. 2013;28:269–82. doi: 10.1007/s11606-012-2235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patient Protection and Affordable Care Act. Hospital Readmissions Reduction Program. Pub L No. 111–148, 124 Stat 408, S3025. [Google Scholar]
- 13.Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305:504–505. doi: 10.1001/jama.2011.72. [DOI] [PubMed] [Google Scholar]
- 14.Burke RE, Kripalani S, Vasilevskis EE, Schnipper JL. Moving beyond readmission penalties: creating an ideal process to improve transitional care. J. Hosp. Med. 2013;8:102–109. doi: 10.1002/jhm.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183:E391–E402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stefan MS, Pekow PS, Nsa W, Priya A, Miller LE, et al. Hospital performance measures and 30-day readmission rates. J. Gen. Intern. Med. 2013;28:377–385. doi: 10.1007/s11606-012-2229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309:342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 18.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J. Hosp. Med. 2007;2:314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 19.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann. Intern. Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 20.Rennke S, Nguyen OK, Shoeb MH, Magan Y, Wachter RM, Ranji SR. Hospital-initiated transitional care interventions as a patient safety strategy: a systematic review. Ann. Intern. Med. 2013;158:433–440. doi: 10.7326/0003-4819-158-5-201303051-00011. [DOI] [PubMed] [Google Scholar]
- 21.Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices: a systematic review. Arch. Intern. Med. 2012;172:1057–1069. doi: 10.1001/archinternmed.2012.2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann. Intern. Med. 2012;157:417–428. doi: 10.7326/0003-4819-157-6-201209180-00006. [DOI] [PubMed] [Google Scholar]
- 23.Kim CS, Flanders SA. In the Clinic. Transitions of care. Ann. Intern. Med. 2013;158 doi: 10.7326/0003-4819-158-5-201303050-01003. ITC3-1. [DOI] [PubMed] [Google Scholar]
- 24.Sokol PE, Wynia MK. There and Home Again. American Medical Association, Chicago, IL: Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions; 2012. AMA Expert Panel on Care Transitions. Available at: www.ama-assn.org/go/patientsafety. [Google Scholar]
- 25.Evans RL, Hendricks RD. Evaluating hospital discharge planning: a randomized clinical trial. Med. Care. 1993;31:358–370. doi: 10.1097/00005650-199304000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J. Hosp. Med. 2009;4:211–218. doi: 10.1002/jhm.427. [DOI] [PubMed] [Google Scholar]
- 27.Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann. Intern. Med. 1994;120:999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- 28.Coleman EA, Parry C, Chalmers S, Min S. The Care Transitions Intervention: results of a randomized controlled trial. Arch. Intern. Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 29.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann. Intern. Med. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 31.Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J. Am. Geriatr. Soc. 2004;52:1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 32.Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: translating from efficacy to effectiveness. Arch. Intern. Med. 2011;171:1232–1237. doi: 10.1001/archinternmed.2011.278. [DOI] [PubMed] [Google Scholar]
- 33.Greenwald JL, Denham CR, Jack BW. The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process. J. Patient Saf. 2007;3:97–106. [Google Scholar]
- 34.Burke R, Guo R, Misky GJ. Identifying keys to success for reducing readmissions: using the Ideal Transition in Care framework. J. Gen. Intern. Med. 2013;28:S94. doi: 10.1186/1472-6963-14-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bradley EH, Curry L, Horwitz LI, Sipsma H, Wang Y, et al. Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ. Cardiovasc. Qual. Outcomes. 2013;6:444–450. doi: 10.1161/CIRCOUTCOMES.111.000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agency for Healthcare Research and Quality. [Accessed July 2];HCUPnet. 2013 Available at: http://hcupnet.ahrq.gov.
- 37.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. (Millwood) 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Allen LA, Hernandez AF, Peterson ED, Curtis LH, Dai D, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ. Heart Fail. 2011;4:293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen J, Ross JS, Carlson MDA, Lin Z, Normand S-LT, et al. Skilled nursing facility referral and hospital readmission rates after heart failure or myocardial infarction. Am. J. Med. 2012;125:100. doi: 10.1016/j.amjmed.2011.06.011. e1-.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med. Care Res. Rev. 2008;65:3–39. doi: 10.1177/1077558707308754. [DOI] [PubMed] [Google Scholar]
- 41.Dombrowski W, Yoos JL, Neufeld R, Tarshish CY. Factors predicting rehospitalization of elderly patients in a postacute skilled nursing facility rehabilitation program. Arch. Phys. Med. Rehabil. 2012;93:1808–1813. doi: 10.1016/j.apmr.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 42.Lima JC, Intrator O, Karuza J, Wetle T, Mor V, Katz P. Nursing home medical staff organization and 30-day rehospitalizations. J. Am. Med. Dir. Assoc. 2012;13:552–557. doi: 10.1016/j.jamda.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morandi A, Bellelli G, Vasilevskis EE, Turco R, Guerini F, et al. Predictors of rehospitalization among elderly patients admitted to a rehabilitation hospital: The role of polypharmacy, functional status, and length of stay. J. Am. Med. Dir. Assoc. 2013 doi: 10.1016/j.jamda.2013.03.013. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O’Malley AJ, Caudry DJ, Grabowski DC. Predictors of nursing home residents’ time to hospitalization. Health Serv. Res. 2011;46:82–104. doi: 10.1111/j.1475-6773.2010.01170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ouslander JG, Diaz S, Hain D, Tappen R. Frequency and diagnoses associated with 7- and 30-day readmission of skilled nursing facility patients to a nonteaching community hospital. J. Am. Med. Dir. Assoc. 2011;12:195–203. doi: 10.1016/j.jamda.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 46.Rolland Y, Andrieu S, Crochard A, Goni S, Hein C, Vellas B. Psychotropic drug consumption at admission and discharge of nursing home residents. J. Am. Med. Dir. Assoc. 2012;13:407. doi: 10.1016/j.jamda.2011.12.056. e7-.e12. [DOI] [PubMed] [Google Scholar]
- 47.Gozalo P, Teno JM, Mitchell SL, Skinner J, Bynum J, et al. End-of-life transitions among nursing home residents with cognitive issues. N. Engl. J. Med. 2011;365:1212–1221. doi: 10.1056/NEJMsa1100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.King BJ, Gilmore-Bykovskyi AL, Roiland RA, Polnaszek BE, Bowers BJ, Kind AJH. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J. Am. Geriatr. Soc. 2013 doi: 10.1111/jgs.12328. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kirsebom M, Wadensten B, Hedström M. Communication and coordination during transition of older persons between nursing homes and hospital still in need of improvement. J. Adv. Nurs. 2013;69:886–895. doi: 10.1111/j.1365-2648.2012.06077.x. [DOI] [PubMed] [Google Scholar]
- 50.Young Y, Inamdar S, Dichter BS, Kilburn H, Jr, Hannan EL. Clinical and nonclinical factors associated with potentially preventable hospitalizations among nursing home residents in New York state. J. Am. Med. Dir. Assoc. 2011;12:364–371. doi: 10.1016/j.jamda.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 51.Thomas KS, Mor V, Tyler DA, Hyer K. The relationships among licensed nurse turnover, retention, and rehospitalization of nursing home residents. Gerontologist. 2013;53:211–221. doi: 10.1093/geront/gns082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ouslander JG, Lamb G, Tappen R, Herndon L, Diaz S, et al. Interventions to reduce hospitalizations from nursing homes: Evaluation of the INTERACT II collaborative quality improvement project. J. Am. Geriatr. Soc. 2011;59:745–753. doi: 10.1111/j.1532-5415.2011.03333.x. [DOI] [PubMed] [Google Scholar]
- 53.Louis-Simonet M, Kossovsky M, Chopard P, Sigaud P, Perneger T, Gaspoz J-M. A predictive score to identify hospitalized patients’ risk of discharge to a post-acute care facility. BMC Health Serv. 2008:Res. 8. doi: 10.1186/1472-6963-8-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sheppard KD, Brown CJ, Hearld KR, Roth DL, Sawyer P, et al. Symptom burden predicts nursing home admissions among older adults. J.Pain Symptom Manage. 2012 doi: 10.1016/j.jpainsymman.2012.10.228. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Borenstein J, Aronow H, Bolton L, Choi J, Bresee C, Braunstein GD. Early recognition of risk factors for adverse outcomes during hospitalization among Medicare patients: a prospective cohort study. BMC Geriatr. 2013:13. doi: 10.1186/1471-2318-13-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Morandi A, Vasilevskis EE, Pandharipande PP, Girard TD, Solberg LM, et al. Inappropriate medications in elderly ICU survivors: where to intervene? Arch. Intern. Med. 2011;171:1032–1034. doi: 10.1001/archinternmed.2011.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bellelli G, Bernardini B, Pievani M, Frisoni GB, Guaita A, Trabucchi M. A score to predict the development of adverse clinical events after transition from acute hospital wards to post-acute care settings. Rejuvenation Res. 2012;15:553–563. doi: 10.1089/rej.2012.1332. [DOI] [PubMed] [Google Scholar]
- 58.Chopra V, Anand S, Krein SL, Chenoweth C, Saint S. Bloodstream infection, venous thrombosis, and peripherally inserted central catheters: Reappraising the evidence. Am. J. Med. 2012;125:733–741. doi: 10.1016/j.amjmed.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 59.Berkowitz RE, Jones RN, Rieder R, Bryan M, Schreiber R, et al. Improving disposition outcomes for patients in a geriatric skilled nursing facility. J. Am. Geriatr. Soc. 2011;59:1130–1136. doi: 10.1111/j.1532-5415.2011.03417.x. [DOI] [PubMed] [Google Scholar]
- 60.Carlson MDA, Lim B, Meier DE. Strategies and innovative models for delivering palliative care in nursing homes. J. Am. Med. Dir. Assoc. 2011;12:91–98. doi: 10.1016/j.jamda.2010.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Berkowitz RE, Fang Z, Helfand BKI, Jones RN, Schreiber R, Paasche-Orlow MK. Project ReEngineered Discharge (RED) lowers hospital readmissions of patients discharged from a skilled nursing facility. J. Am. Med. Dir. Assoc. 2013 doi: 10.1016/j.jamda.2013.03.004. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 62.Ouslander JG, Perloe M, Givens JH, Kluge L, Rutland T, Lamb G. Reducing potentially avoidable hospitalizations of nursing home residents: results of a pilot quality improvement project. J. Am. Med. Dir. Assoc. 2009;10:644–652. doi: 10.1016/j.jamda.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 63.Tena-Nelson R, Santos K, Weingast E, Amrhein S, Ouslander J, Boockvar K. Reducing potentially preventable hospital transfers: results from a thirty nursing home collaborative. J. Am. Med. Dir. Assoc. 2012;13:651–656. doi: 10.1016/j.jamda.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 64.van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–557. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shulan M, Gao K, Moore CD. Predicting 30-day all-cause hospital readmissions. Health Care Manag. Sci. 2013;16:167–175. doi: 10.1007/s10729-013-9220-8. [DOI] [PubMed] [Google Scholar]
- 66.Philbin EF, DiSalvo TG. Prediction of hospital readmission for heart failure: development of a simple risk score based on administrative data. J. Am. Coll. Cardiol. 1999;33:1560–1566. doi: 10.1016/s0735-1097(99)00059-5. [DOI] [PubMed] [Google Scholar]
- 67.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd. New York, NY: John Wiley & Sons; 2000. [Google Scholar]
- 68.Amarasingham R, Moore BJ, Tabak YP, Drazner MH, Clark CA, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med. Care. 2010;48:981–988. doi: 10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- 69.Coleman EA, Min SJ, Chomiak A, Kramer AM. Posthospital care transitions: patterns, complications, and risk identification. Health Serv. Res. 2004;39:1449–1465. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Halfon P, Eggli Y, Pretre-Rohrbach I, Meylan D, Marazzi A, Burnand B. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med. Care. 2006;44:972–981. doi: 10.1097/01.mlr.0000228002.43688.c2. [DOI] [PubMed] [Google Scholar]
- 71.Desai MM, Stauffer BD, Feringa HH, Schreiner GC. Statistical models and patient predictors of readmission for acute myocardial infarction: a systematic review. Circ. Cardiovasc. Qual. Outcomes. 2009;2:500–507. doi: 10.1161/CIRCOUTCOMES.108.832949. [DOI] [PubMed] [Google Scholar]
- 72.Ross JS, Mulvey GK, Stauffer B, Patlolla V, Bernheim SM, et al. Statistical models and patient predictors of readmission for heart failure: a systematic review. Arch. Intern. Med. 2008;168:1371–1386. doi: 10.1001/archinte.168.13.1371. [DOI] [PubMed] [Google Scholar]
- 73.Bahadori K, FitzGerald JM. Risk factors of hospitalization and readmission of patients with COPD exacerbation--systematic review. Int. J. Chron. Obstruct. Pulmon. Dis. 2007;2:241–251. [PMC free article] [PubMed] [Google Scholar]
- 74.Lichtman JH, Leifheit-Limson EC, Jones SB, Watanabe E, Bernheim SM, et al. Predictors of hospital readmission after stroke: a systematic review. Stroke. 2010;41:2525–2533. doi: 10.1161/STROKEAHA.110.599159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Society of Hospital Medicine. [Accessed July 17];Better Outcomes for Older adults through Safe Transitions (BOOST) 2013 Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/html_CC/project_boost_background.cfm.
- 76.Shekelle PG, Pronovost PJ, Wachter RM, Taylor SL, Dy SM, et al. Advancing the science of patient safety. Ann. Intern. Med. 2011;154:693–6. doi: 10.7326/0003-4819-154-10-201105170-00011. [DOI] [PubMed] [Google Scholar]
- 77.Linertova R, Garcia-Perez L, Vazquez-Diaz JR, Lorenzo-Riera A, Sarria-Santamera A. Interventions to reduce hospital readmissions in the elderly: in-hospital or home care. A systematic review. J. Eval. Clin. Pract. 2011;17:1167–75. doi: 10.1111/j.1365-2753.2010.01493.x. [DOI] [PubMed] [Google Scholar]
- 78.Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, et al. Telemonitoring in patients with heart failure. N. Engl. J. Med. 2010;363:2301–9. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Burke RE, Donze J, Schnipper JL. Contribution of psychiatric illness and substance abuse to 30-day readmission risk. J.Hosp. Med. 2013 doi: 10.1002/jhm.2044. (epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 80.Vigod SN, Kurdyak PA, Dennis CL, Leszcz T, Taylor VH, et al. Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. Br. J. Psychiatry. 2013;202:187–194. doi: 10.1192/bjp.bp.112.115030. [DOI] [PubMed] [Google Scholar]
- 81.Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol. Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 82.Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. Am. J. Prev. Med. 2003;24:113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 83.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 84.Centers for Medicare and Medicaid Services. [Accessed July 18];Community-based Care Transitions Program. 2013 Available at: http://innovation.cms.gov/initiatives/CCTP/.
- 85.Cutts T, Baker B. Church-health system partnership facilitates transitions from hospital to home for urban, low-income African Americans, reducing mortality, utilization, and costs. [Accessed July 18];AHRQ Innovations Exchange. 2013 Available at: http://www.innovations.ahrq.gov/content.aspx?id=3354.
- 86.Doctoroff L. Interval examination: establishment of a hospitalist-staffed discharge clinic. J. Gen. Intern. Med. 2012;27:1377–1382. doi: 10.1007/s11606-012-2150-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gandara E, Ungar J, Lee J, Chan-Macrae M, O’Malley T, Schnipper JL. Discharge documentation of patients discharged to subacute facilities: a three-year quality improvement process across an integrated health care system. Jt. Comm. J. Qual. Patient Saf. 2010;36:243–251. doi: 10.1016/s1553-7250(10)36039-9. [DOI] [PubMed] [Google Scholar]