Abstract
Background:
Chronic pain affects millions of racially diverse Americans. Evidence suggests that group medical visits are effective for treating chronic pain; similarly, a number of studies demonstrate the effectiveness of certain evidence-based complementary therapies in managing pain.
Objectives:
The primary goal of this study is to evaluate the feasibility of the integrative medical group visit (IMGV) care model in an inner-city racially diverse outpatient clinic. IMGV combines patient-centered, non-pharmacologic strategies and principles of mindfulness-based stress-reduction with a group medical visit to reduce pain and associated symptoms.
Methods:
We surveyed patients pre and post an 8-session IMGV program to evaluate changes in pain in the last week (0-10 point scale) and comorbid symptoms including depression (Patient Health Questionaire-8 [PHQ-8]), perceived stress, and sleep quality. We also recorded referrals to the program, patients screened for eligibility, total enrollment, loss to follow-up, and attendance.
Results:
Seventy patients joined IMGV, and of these, 65 (93%) enrolled in the study. Over the course of 12 months, 7 groups met (median 9 patients/group; range 8-13 participants). Mean difference in pain level for all patients between baseline and 8 weeks was 0.7 (SD=2.0, P=.005). Mean difference in PHQ-8 depression score for patients with baseline score ≥5 was 2.6 (SD=4.6, P<.001). Statistically significant improvements were also seen in sleep quality and perceived stress.
Conclusion:
A group visits program combining conventional and integrative medicine for predominantly racially diverse patients is feasible.
Key Words: Group medical visit, patient-centered non-pharmacologic strategies, chronic pain, mindfulness-based stress reduction, integrative medical group visits
INTRODUCTION
Chronic pain affects 100 million Americans, and healthcare for these individuals costs up to $635 billion.1 Research shows that pain is consistently undertreated in patients of low socioeconomic and minority status.2 Current medical treatments for chronic pain consist mostly of pain medications (narcotics and non-steroidal anti-inflammatory drugs [NSAIDS]) and physical therapy. In treating chronic pain, primary care providers (PCPs) cite concerns about drug seeking, poor self-management, patient psychological factors, and compliance as barriers to optimal pain treatment.3 Additionally, in resource-poor primary care settings that are taking care of people with many social and economic concerns, time restraints and lack of access to providers can lead to disparities in pain treatment.2 This article reports on the feasibility of conducting an integrative medical group visit (IMGV) to address chronic pain and associated symptoms in racially diverse outpatients.
A growing body of evidence suggests that group medical visits may be effective for some patients in treating chronic pain.4 The group model of medical care addresses some of the current issues faced by minority patients with chronic pain by improving access to physicians, health outcomes, and quality of care.5 Many group medical visits include individual medical attention for each group participant, teaching time (didactic and interactive), time for patient self-management, and time for the group to connect and socialize. Groups usually range from 8 to 12 patients with one to two clinician facilitators. In the diabetes literature, group medical visits improve health status indicators such as health-related quality of life, disability days, patient satisfaction, diabetic control, patients' trust in their physician, coordination of care, and more culturally competent care.6-8
Mindfulness-based stress reduction (MBSR) is a promising intervention that has been applied to patients suffering from a number of chronic illnesses, including pain.9,10 Founded by Jon Kabat-Zinn at the University of Massachusetts, it consists of an 8-week group curriculum delivered by a trained mindfulness instructor in weekly 2.5-hour classes. Mindfulness is the practice of purposeful awareness of the present moment with a nonjudgmental attitude.11 The curricululm includes didatic discussion of stress, mindfulness, and experiential practice (sitting meditation, body scan, walking meditation, and yoga). A recent systematic review identified 17 randomized controlled trials of MBSR. Eleven studies showed improvement in mental health measures compared to wait-list or standard care controls. For patients with chronic pain, there was an overall improvement in pain scores and mental health status.12 Patients with two or more comorbid pain conditions had the greatest improvement in pain.9
Systematic reviews report data on the safety and effectiveness of evidenced-based complementary medicine (EBCM) therapies as an adjunct to the standard of care for certain chronic conditions such as pain.13 Complementary or non-pharmacologic therapies listed in the American Pain Society/American College of Physician Clinical Practice Guidelines as having some benefit for chronic low back pain include massage therapy, acupuncture, yoga, and cognitive behavioral therapy.14-18
In low–socioeconomic-status minority populations, disparities also exist in the utilization of complementary and alternative medicine (CAM). For example, compared to non-Hispanic whites (43%), only 26% of blacks and 24% of Hispanics report CAM use.19 Factors such as limited disposable income, lack of access to local CAM practitioners, and no insurance coverage for these therapies prevent low–socioeconomic-status minority populations from using CAM.
The IMGV is an innovative, patient-centered model of care bringing together medical group visits, EBCM, and the principles of MBSR (Figure). IMGV aims to address patient needs in a comprehensive manner by incorporating patient-centered strategies, improving adherence to chronic care management, and improving health and coping.
Figure.
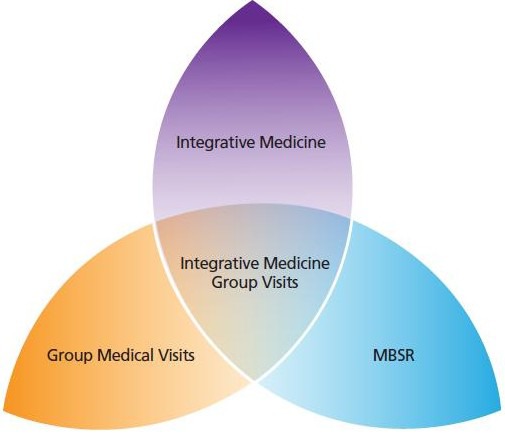
Boston Medical Center Integrative Medical Group Visits: the merger of three paradigms.
Relatively little rigorous research has been conducted on the feasibility of an IMGV model.20 The primary aim of this study was to assess the feasibility of offering an IMGV care model to a predominantly underserved, minority population in a busy outpatient clinic. Our secondary outcomes were change in pain level and other common comorbidities such as depressive symptoms, sleep quality, stress, and anxiety.
MATERIALS AND METHODS
Study design
This prospective observational cohort study enrolled 65 participants from the IMGV clinical program between April 2012 and April 2013. Patients could participate in the IMGV program without participating in the research. All participants in the study had registered for but not yet begun the IMGV program at time of study enrollment. Baseline data were collected prior to the start of the first group. The Boston University Medical Center Institutional Review Board approved this study.
Setting
Boston Medical Center (BMC), Massachusetts, is a private, not-for-profit, 496-bed, academic medical center and the largest safety net hospital in New England. Approximately 70% of the patients come from under-served populations, including low-income families, elders, people with disabilities, and immigrants. All IMGV sessions took place in a conference room within the Family Medicine Ambulatory Care Clinic, a primary care outpatient clinic located in the hospital (cooking classes took place in the hospital's teaching kitchen).
Intervention
IMGV engages patients in an intensive 8-week series of clinician-facilitated groups that combine patient education on self-care management, the principles of MBSR, and EBCM group experiences (self-massage, acupuncture, and cooking classes; Table 1). No more than one group was conducted at any time due to resources and physical space limitations. The IMGV model uses principles of adult learning and engagement, allowing for experience and knowledge sharing to empower and motivate patients to create an individualized treatment plan for their chronic conditions (Table 2). Each week, 8 to 12 patients met for 2.5-hour sessions co-led by a family medicine physician and meditation instructor with MBSR experience. Individual CAM providers were guest facilitators for individual sessions when their specialty (eg, self-massage, acupuncture) was featured. Using motivational interviewing and shared decision-making techniques, the clinical provider/facilitator and patients discussed individual strategies.
Table 1.
Integrative Medical Group Visit 8-Session Curriculum
| Weekly: Vitals and pain level recorded by participant; healthy buffet of food served at the end of each session |
| Session 1. Mind-body Exercise: introduction to concepts of IMGV (ground rules for safety and confidentiality), beginner's mind, foundations of mindfulness, mindful raisin-eating exercise; Doc Talk: Introduction to concepts of IMGV (ground rules for safety and confidentiality) EBCM: body scan |
| Session 2. Mind-body Exercise: body scan, working with perceptions, Upstream Downstream fable; thinking outside the box (9 dots exercise); Doc Talk: Stress response and reactions in body; EBCM: self-massage |
| Session 3. Mind-body Exercise: mindful yoga, responding vs reacting to stress, the mind-body connection, pleasant events; Doc Talk: The body's response to chronic stress (blood pressure); EBCM: yoga |
| Session 4. Mind-body Exercise: sitting meditation, unpleasant events; Doc Talk: The body's response to chronic stress (cholesterol); mid-term group evaluation |
| Session 5. Mind-body Exercise: meditation triangle of awareness (thoughts, emotions, bodily experience), reacting and responding to stress; Doc Talk: Food is medicine (glycemic index and healthy eating) |
| Session 6. Mind-body Exercise: walking meditation, difficult communications, deep listening activity; Doc Talk: The body's experience of pain (anti-inflammatory foods and omega-3 fatty acids) EBCM: acupuncture |
| Session 7. Mind-body Exercise: loving kindness meditation, communication skills; Doc Talk: Healthy eating on a budget; EBCM: cooking class in demonstration kitchen |
| Session 8. Mind-body Exercise: meditation, body scan, yoga; Doc talk: Practice for the rest of your life; graduation celebration and diplomas |
Abbreviations: EBCM, evidenced-based complementary medicine; IMGV: integrative medical group visit.
Doc Talk: clinician didactic.
Table 2.
Standard Integrative Medical Group Visit Session Format
| Curriculum Elements | Time (min) |
|---|---|
| Participant check-in and vitals | 10 |
| Centering meditation | 10 |
| “Doc talk” | 20 |
| Mindfulness exercise or discussion | 30 |
| Discussion of home practice | 10 |
| Wrap-up | 10 |
| Experiential session or mindfulness exercise | 60 |
| Total Time: | 150 |
To enhance self-management skills, patients were trained to record their own vital signs prior to the start of each group. Additionally, at each group the physician provided one-on-one contact with each group member either before the group or after the group finished. One-on-one visits took place in an adjacent clinic room. This provided opportunity when needed for specific medication adjustments, diagnostic test ordering, or referrals.
Before starting the groups, participants signed a confidentiality agreement. By signing this agreement, patients authorized the discussion of personal health information in the group setting and also agreed to respect the confidentiality of others in the group by not disclosing any information. The agreement specified that they cannot hold the organization liable for any breach of confidentiality committed by other group members.
At each class, group facilitators assigned participants “home practice,” which included informal and formal mindfulness practices including meditation, yoga, and body scan. Compact discs were given to all participants to facilitate home practice (each track was 40 to 45 minutes). Following the principles of MBSR, participants were instructed to reflect on and record events in their daily lives.
In order to increase attendance and teach the principles of healthy eating, after each weekly meeting, the coordinator served a healthy buffet of food. Meals included a whole grain such as quinoa, brown rice, or barley; a fruit and vegetable offering, often a salad; and a lean, non-animal protein such as tofu or legumes. Meals were meant to introduce participants to foods they may not have previously eaten, with the goal of giving them ideas for creating their own nutritious, low-cost meals at home. Nutrition topics were also integrated into the weekly “doc talks,” which included information on omega-3–rich, high-fiber, low-glycemic, and low-cholesterol foods.21 Eating meals together created an opportunity to develop a sense of community, practice mindful eating, and model healthy nutrition.
After being exposed to various EBCM through IMGV, participants were invited to take advantage of free or low-cost CAM services available at BMC, including yoga, tai chi, cooking classes, acupuncture, and massage therapy. After the 8-week period, patients continued to meet for an integrative medical group visit approximately every 3 months. Although all groups were led by the same facilitators and followed the same curriculum, we did not formally access the internal validity of the groups.
Participant Recruitment
The clinicians within the Family Medicine clinic as well as providers at BMC and its affiliated community health centers referred patients to the IMGV. We advertised the IMGV using multiple methods, including flyers in visible areas in the clinics, presentations to providers and staff members, patient orientation sessions, and electronic messages to providers via the electronic medical record. The Integrative Medicine Clinical Services Coordinator called the referred patients to explain the program, assess interest and commitment, and answer any questions.
The IMGV program is designed for racially diverse low health literacy patients with chronic health conditions including pain. To test the feasibility of the IMGV program, participants were included in the groups if they had a diagnosis of any chronic pain (eg, musculoskeletal pain, headaches, fibromyalgia) and one or more chronic conditions (eg, diabetes, depression, or metabolic syndrome). Since this was a feasibility study, we did not define the duration of chronic pain or pain level required for inclusion into the groups. Participants had to be at least 18 years of age and able to speak English.
Upon agreeing to attend the IMGV program, participants were invited by the coordinator meet one-on-one to review what happens in the groups, hear about the opportunity to participate in research, and if interested, sign a consent form and fill out a baseline questionnaire. The coordinator provided assistance in filling out the surveys to any participant with low literacy. To inform themselves of a patient's history and health conditions, the IMGV physicians reviewed patient charts prior to the start of the group.
Measures
Patients who elected to participate in the research study completed questionnaires at baseline and after the 8-week intensive clinical program. Qualitative data on patient experience including satisfaction of IMGV were collected through open-ended questionnaire items, as well as individual, semi-structured interviews at the end of the groups.
We used self-reported data for sociodemographic variables, which included age, race, education, work status, annual household income, and primary language at home. We reviewed patient problem lists in the electronic medical record to collect data on comorbidities and chronic pain diagnosis. Average pain in the previous week was assessed using an 11-point (0-10) numerical rating scale.22,23 Depression (Patient Health Questionaire-8 [PHQ-8]),24 sleep quality (Pittsburgh Sleep Quality Index [PSQI]),25 stress (Perceived Stress Scale [PSS]),26,27 and anxiety (Generalized Anxiety Disorder 7-item scale [GAD-7])28 were also assessed. We collected participants' pain levels and vitals on a weekly basis. Before each group, participants recorded their weight, pulse, blood pressure, and pain score with the assistance of the medical assistant. Body mass index (BMI) was calculated by the research assistant. Using an automatic blood pressure machine, patients took their own blood pressure (in a seated position using the arm of their choice). Feasibility measures included number of patients referred to the group, number of patients screened, total enrollment, loss to follow-up, and number of visits attended by participants.
Statistical Analysis
Recruitment, retention, and baseline data were summarized with descriptive statistics including means, medians, and standard deviations for continuous variables and frequencies for categorical variables. The primary analytic method was intention-to-treat. All participants with baseline and 8-week data were included in the analysis, regardless of attendance or adherence to protocol. For pain and blood pressure, a last value carried forward approach was used to replace missing data.
In order to assess for changes in the other comorbid conditions such as depression, anxiety, and sleep problems, subgroup analyses were also conducted for secondary outcome measures. Participants were included in the subgroup if they reported a minimum baseline score for the respective outcome measure. Minimum values were chosen a priori and based upon clinical significance: PHQ-8 ≥5 (mild depression)24; GAD-7 ≥528; PSQI ≥525; PSS ≥1427; systolic blood pressure ≥140 or diastolic blood pressure ≥90, and BMI ≥30. Secondary outcomes are presented only for those individuals who met the baseline inclusion score for each measure. We calculated change scores for each outcome by subtracting baseline data from 8-week measurements. The Student's t-test was used to determine if the mean change score was statistically different from zero. A two-sided P value of .05 was used for all statistical tests. All analyses were performed using SAS v9.2 (SAS Institute Inc, Cary, North Carolina).
RESULTS
A total of 309 patients were referred to IMGV between April 2012 and April 2013. A large number of these patients could not be reached for further follow-up (n=103), did not show up to an in-person screening visit or the first group visit (n=74), or were unable to participate due to time of group or disinterest (n=62). Seventy patients joined IMGV, and of these, 65 (93%) enrolled in the study. Over the course of 12 months, 7 groups of patients participated in the IMGV program (median 9 patients/group; range 8-13 participants). The attendance rate across IMGV groups was 64%, with 68% of participants attending ≥5 weekly sessions. Among participants who completed the baseline survey, 8 (11%) were unable to be reached at 8 weeks to complete the follow-up survey.
Table 3 summarizes the sociodemographic and health characteristics of participants at baseline. Approximately two-thirds were women, and the mean age was approximately 50 years. Participants were predominantly black, and half of the participants had not attended any college. The vast majority were either disabled or unemployed. About three-fourths had annual household incomes of $30 000 or less. The majority spoke English at home. Psychological and physical morbidity were high in the groups, with more than half of patients diagnosed with hypertension, depression, and two or more chronic pain conditions. Back pain, headache, and knee pain were the most common conditions noted in the medical chart. On average, patients had moderate to severe self-reported pain, and reported high stress (PSS), and poor sleep quality (PSQI).
Table 3.
Baseline Sociodemographic and Health Characteristics for 65 Participants in Integrative Medical Group Visits
| Characteristics | n (%) |
|---|---|
| Mean age, y (Sd) | 50.7 (10.5) |
| Female | 44 (68) |
| Race/Ethnicity | |
| White | 15 (23) |
| Black | 39 (60) |
| Hispanic | 6 (9) |
| Multiple | 5 (8) |
| Education | |
| Some high school or less | 13 (20) |
| High school graduate | 12 (19) |
| Vocational/trade school | 8 (12) |
| Some college | 23 (35) |
| College degree or greater | 9 (14) |
| Work Status | |
| Employed | 12 (19) |
| Unemployed or laid off | 19 (29) |
| Disabled | 26 (40) |
| Retired/Other | 8 (12) |
| Annual Household Income | |
| Less than $10,000 | 30 (46) |
| $10,000-$29,999 | 17 (26) |
| $30,000-$49,999 | 4 (6) |
| $50,000-$74,999 | 1 (2) |
| Don't know/Refused | 13 (20) |
| Primary Language at Home | |
| English | 54 (83) |
| Spanish | 6 (9) |
| Other | 5 (8) |
| Comorbidities | |
| Diabetes mellitus | 21 (32) |
| Obesity | 26 (40) |
| Depression | 40 (62) |
| Anxiety | 17 (26) |
| Hypertension | 36 (55) |
| Pain | |
| Abdominal | 13 |
| Back | 37 |
| Neck | 11 |
| Joint | |
| Knee | 16 |
| Hip | 7 |
| Shoulder | 8 |
| Foot/ankle | 13 |
| Pelvic | 7 |
| Headache | 19 |
| Fibromyalgia | 10 |
| Pain disorder (not otherwise specified) | 17 |
| Baseline Outcome Scores | |
| Pain Intensity in previous week, mean (SD) | 7.2 (2.4) |
| Patient Health Questionaire-8, mean (SD) | 12.2 (7.5) |
| Generalized Anxiety Disorder 7-item scale, mean (SD) | 10.5 (6.4) |
| Pittsburgh Sleep Quality Index, mean (SD) | 11.6 (4.3) |
| Perceived Stress Scale, mean (SD) | 22.2 (7.8) |
| Systolic blood pressure, mmHg, mean(SD) | 129 (16.7) |
| Diastolic blood pressure, mmHg, mean (SD) | 83 (10.8) |
| Body mass index, mean (SD) | 32.8 (6.3) |
Table 4 presents mean change scores for pain and all secondary outcomes. Mean pain scores decreased almost one point (0.7; (SD)=2.0, P=.005]). Although this change was statistically significant, it was modest and less than the 1.0 to 1.5–point difference that is often considered a clinically significant change.22 Improvement in depression, as measured by the PHQ-8, was clinically and statistically significant. Statistically significant reductions were also seen for sleep quality and perceived stress, but no significant change was observed for anxiety level. Of the 18 participants with hypertension, there was 11 millimeters of mercury (mmHg) decrease in mean systolic pressure from baseline to 8 weeks.
Table 4.
Mean Change Scores for Pain and Secondary Outcomes
| Measure | No.a | Mean Change Score (Sd) | P value |
|---|---|---|---|
| Pain intensity | 59 | –0.7 (2.0) | .005 |
| Patient Health Questionaire-8 | 41 | –2.6 (4.6) | <.001 |
| Generalized Anxiety Disorder 7-item scale | 39 | –0.7 (5.5) | .4 |
| Pittsburgh Sleep Quality Index | 23 | –1.3 (2.9) | .04 |
| Perceived Stress Scale | 49 | –2.0 (6.6) | .04 |
| Systolic blood pressure | 18 | –10.6 (19.9) | .04 |
| Diastolic blood pressure | 18 | –0.6 (11.5) | .84 |
| Body mass index | 34 | –0.1 (0.7) | .36 |
All participants were included in the primary outcome measure pain analysis. Participants were included in secondary outcome analyses if their baseline outcome measurement was equal to or greater than an a priori minimum score (PHQ-8 ≥524; GAD-7 ≥528; PSQI ≥525; PSS ≥1427; SBP ≥140 or DBP ≥90, BMI ≥30).
Abbreviations: GAD-7, Generalized Anxiety Disorder 7-item scale; PHQ-8, Patient Health Questionaire-8; PSQI, Pittsburgh Sleep Quality Index; PSS, Perceived Stress Scale; SD, standard deviation.
For the qualitative interviews, responses to open-ended questions about patient satisfaction were overall positive. General themes included the impact IMGV had on their confidence and skill to self-manage pain. Qualitative data suggest that increased self-efficacy and improvement in symptoms (eg, mood, sleep disorders) may help mediate improvement in pain level. Illustrative comments included
The program is very helpful with my stress and my daily living with pain. I love it.
Before I started these meetings I pretty much gave up my life because it felt worthless. The pain had taken over my life. After the group meetings I have been meditating, breathing; when I feel that my anxiety levels are rising I use my tools.
Meditation is very good, it helps me sleep better. I am learning that I can get control all by myself.
DISCUSSION
To address chronic pain and other co-morbid conditions, we developed an 8-week standardized IMGV care model and tested its feasibility in an underserved, racially diverse patient population. We determined that it is feasible to conduct an IMGV in a busy inner city outpatient clinic. Attendance to group sessions was overall very good. Participants experienced improvements in pain, depression, sleep quality, perceived stress, and systolic blood pressure. Based on qualitative data, patient satisfaction with the IMGV model was high overall.
Our results demonstrate that it is feasible to implement a complex group visit intervention (medical group visit, EBCM, and MBSR) in a diverse patient population. This study adds to the growing group medical visit research literature.29-32 Several studies have demonstrated the feasibility and effectiveness of a group visit model for managing the needs of underserved, chronically ill patients, demonstrating participants' increased satisfaction with their primary care physicians, better quality of life, and greater self-efficacy.33,34 A recent review of group medical visits for the management of chronic pain found moderate evidence for use as part of a multidisciplinary treatment program. Investigators discovered added benefits beyond improved clinical outcomes, including greater clinic efficiency and a stronger patient-provider relationship.4
Few studies, however, exist on the intersection of MBSR, EBCM, and the group medical visit model—the IMGV. For example, Geller et al reported on a study of mostly Hispanic low-income patients using a group visit model offering exercise, meditation, and acupuncture. This model improved all eight subscales of the Short Form-36 with statistically significant changes in bodily pain, mental health, and vitality.35 Like the IMGV model at BMC, this intervention offers patients EBCM; however, patients are able to choose what they do at each visit rather than participate in a standardized curriculum. In contrast to the IMGV model, these group visits use a drop-in model of participation where there is no set start or end date, so participants may attend when they want. There is also evidence supporting the use of MBSR9,10 and other EBCM36-38 techniques for chronic pain, demonstrating their effectiveness at reducing pain and improving function.
Our feasibility study has several important limitations. Given the pilot nature of the IMGV, our sample size was small and there was no comparison group. Results reported in this paper are for short-term outcomes only. Regarding generalizability, many patients who were referred to the IMGV ultimately did not enroll for a variety of logistical and psychosocial reasons. Although there were many referrals for Spanish-speaking patients, groups were held only in English. Groups were run during the day only, preventing many employed patients from participating. Lastly, only two physicians and two meditation instructors were involved in teaching the groups.
Chronic pain affects millions of racially diverse Americans and creates significant financial and psychological burden.1 There is a need to develop and disseminate models of care that are effective complements to conventional pharmacotherapy for chronic pain. Future research on IMGV should include larger, adequately powered randomized controlled trials with long-term follow-up. This will be critical to evaluate whether the IMGV model improves outcomes, quality of care, and/or patient and provider satisfaction. With billions of dollars being spent on chronic pain treatment each year,1 evaluating the cost effectiveness of IMGV is also important. Given the differential prevalence and impact of pain in minority, underserved populations,2 research should be conducted on patient-centered care models such as IMGV to evaluate whether they can help reduce existing disparities.
Acknowledgments
The authors wish to thank all the study participants, the staff of the Family Medicine Clinic at Boston Medical Center, the meditation instructors (Erin Sharaf, Bonita Jones), CAM providers (Anna Dunwell, Monica Delgado Chaffee, Lisa Spellman, Ellen Highfield, Paula Nesoff, Tracey Burg), curriculum contributors (David Rakel and colleagues at University of Wisconsin; Ryan Bradley and Sonja Max, authors of the Food User's Manual), Susan Chung, Kirsten Resnick, Larry Hanawalt, and Alix Carey. This study was generously supported by a gift from an anonymous family foundation. The funder had no role in the design, conduct, analysis, or reporting of the study.
Disclosures The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and declared none; this project was funded by an anonymous family foundation. Dr Paula Gardiner is the recipient of Grant Number K07 AT005463-01A1 from the National Center for Complementary & Alternative Medicine. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Complementary & Alternative Medicine or the National Institutes of Health.
Contributor Information
Paula Gardiner, Program for Integrative Medicine and Health Disparities, Department of Family Medicine, Boston Medical Center, Massachusetts, United States..
Danielle Dresner, Program for Integrative Medicine and Health Disparities, Department of Family Medicine, Boston Medical Center, Massachusetts, United States..
Katherine Gergen Barnett, Program for Integrative Medicine and Health Disparities, Department of Family Medicine, Boston Medical Center, Massachusetts, United States..
Ekaterina Sadikova, Program for Integrative Medicine and Health Disparities, Department of Family Medicine, Boston Medical Center, Massachusetts, United States..
Robert Saper, Program for Integrative Medicine and Health Disparities, Department of Family Medicine, Boston Medical Center, Massachusetts, United States..
REFERENCES
- 1.Relieving pain in America: a blueprint for transforming prevention, care, education and research. Institute of Medicine. 2011. http://www.nap.edu/catalog.php?record_id=13172 AccessedJune18, 2013
- 2.Green CR, Anderson KO, Baker TAet al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003; 4(3): 277–94 [DOI] [PubMed] [Google Scholar]
- 3.Upshur CC, Luckmann RS, Savageau JA.Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med. 2006; 21(6): 652–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaynor CH, Vincent C, Safranek Set al. FPIN's clinical inquiries. Group medical visits for the management of chronic pain. Am Fam Physician. 2007; 76(11): 1704–5 [PubMed] [Google Scholar]
- 5.Jaber R, Braksmajer A, Trilling JS.Group visits: a qualitative review of current research. J Am Board Fam Med. 2006; 19(3): 276–290 [DOI] [PubMed] [Google Scholar]
- 6.Wagner EH, Grothaus LC, Sandhu Net al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001; 24(4): 695–700 [DOI] [PubMed] [Google Scholar]
- 7.Clancy DE, Brown SB, Magruder KMet al. Group visits in medically and economically disadvantaged patients with type 2 diabetes and their relationships to clinical outcomes. Top Health Inf Manage. 2003; 24(1): 8–14 [PubMed] [Google Scholar]
- 8.Sadur CN, Moline N, Costa Met al. Diabetes management in a health maintenance organization: Efficacy of care management using cluster visits. Diabetes Care. 1999; 22(12): 2011–7 [DOI] [PubMed] [Google Scholar]
- 9.Rosenzweig S, Greeson JM, Reibel DKet al. Mindfulness-based stress reduction for chronic pain conditions: variation in treatment outcomes and role of home meditation practice. J Psychosom Res. 2010; 68(1): 29–36 [DOI] [PubMed] [Google Scholar]
- 10.Kabat-Zinn J, Lipworth L, Burney R.The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985; 8(2): 163–90 [DOI] [PubMed] [Google Scholar]
- 11.Kabat-Zinn J.Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pr. 2003; 10(2): 144–56 [Google Scholar]
- 12.Fjorback LO, Arendt M, Ornbøl Eet al. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: a systematic review of randomized controlled trials. Acta Psychiatr Scand. 2011; 124(2): 102–19 [DOI] [PubMed] [Google Scholar]
- 13.Calonge N.Primary care interventions to prevent low back pain in adults. Agency for Healthcare Research and Quality; 2004. http://www.uspreventiveservicestaskforce.org/3rduspstf/lowback/lowbackrs.pdf AccessedJune3, 2014
- 14.Chou R, Huffman LH.American Pain Society, American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007; 147(7): 492–504 [DOI] [PubMed] [Google Scholar]
- 15.Cherkin DC, Eisenberg D, Sherman KJet al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. 2001; 161(8): 1081–8 [DOI] [PubMed] [Google Scholar]
- 16.Manheimer E, White A, Berman Bet al. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005; 142(8): 651–63 [DOI] [PubMed] [Google Scholar]
- 17.Sherman KJ, Cherkin DC, Wellman RDet al. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Arch Intern Med. 2011; 171(22): 2019–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cherkin DC, Sherman KJ, Kahn Jet al. A comparison of the effects of 2 types of massage and usual care on chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2011; 155(1): 1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Center for Complementary and Alternative Medicine. The use of complementary and alternative medicine in the United States. http://nccam.nih.gov/news/camstats/2007/camsurvey_fs1.htm AccessedJune3, 2014
- 20.Khorsan R, Coulter ID, Crawford Cet al. Systematic review of integrative health care research: Randomized control trials, clinical controlled trials, and meta-analysis. Evid-Based Complement Altern Med. 2011; doi:10.1155/2011/636134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bradley R, Max S.Food user manual volume 1: an introduction. Seattle, WA: Ryan Bradley and Sonja Max; 2012 [Google Scholar]
- 22.Von Korff M, Jensen MP, Karoly P.Assessing global pain severity by self-report in clinical and health services research. Spine. 2000; 25(24): 3140–51 [DOI] [PubMed] [Google Scholar]
- 23.Ritter PL, González VM, Laurent DDet al. Measurement of pain using the visual numeric scale. J Rheumatol. 2006; 33(3): 574–80 [PubMed] [Google Scholar]
- 24.Kroenke K, Strine TW, Spitzer RLet al. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009; 114(1-3): 163–73.doi:10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- 25.Buysse DJ, Reynolds CF, Monk THet al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2): 193–213 [DOI] [PubMed] [Google Scholar]
- 26.Hewitt PL, Flett GL, Mosher SW.The Perceived Stress Scale: Factor structure and relation to depression symptoms in a psychiatric sample. J Psychopathol Behav Assess. 1992; 14(3): 247–57.doi:10.1007/BF00962631 [Google Scholar]
- 27.Cohen S, Kamarck T, Mermelstein R.A global measure of perceived stress. J Health Soc Behav. 1983; 24(4): 385–96 [PubMed] [Google Scholar]
- 28.Spitzer RL, Kroenke K, Williams JBWet al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006; 166(10): 1092–1097.doi:10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 29.Kirsh S, Watts S, Pascuzzi Ket al. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007; 16(5): 349–53.doi:10.1136/qshc.2006.019158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trento M, Passera P, Bajardi Met al. Lifestyle intervention by group care prevents deterioration of Type II diabetes: a 4-year randomized controlled clinical trial. Diabetologia. 2002; 45(9): 1231–9.doi:10.1007/s00125-002-0904-8 [DOI] [PubMed] [Google Scholar]
- 31.Riley SB, Marshall ES.Group visits in diabetes care: a systematic review. Diabetes Educ. 2010; 36(6): 936–44.doi:10.1177/0145721710385013 [DOI] [PubMed] [Google Scholar]
- 32.Clancy DE, Huang P, Okonofua Eet al. Group visits: Promoting adherence to diabetes guidelines. J Gen Intern Med. 2007; 22(5): 620–4.doi:10.1007/s11606-007-0150-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Scott JC, Conner DA, Venohr Iet al. Effectiveness of a group outpatient visit model for chronically ill older health maintenance organization members: A 2-Year randomized trial of the cooperative health care clinic. J Am Geriatr Soc. 2004; 52(9): 1463–70.doi:10.1111/j.1532-5415.2004.52408.x [DOI] [PubMed] [Google Scholar]
- 34.Beck A, Scott J, Williams Pet al. A randomized trial of group outpatient visits for chronically ill older HMO members: the cooperative health care clinic. J Am Geriatr Soc. 1997; 45(5): 543–9 [DOI] [PubMed] [Google Scholar]
- 35.Geller JS, Orkaby A, Cleghorn GD.Impact of a group medical visit program on Latino health-related quality of life. Explore J Sci Heal. 2011; 7(2): 94–9.doi:10.1016/j.explore.2010.12.005 [DOI] [PubMed] [Google Scholar]
- 36.Cramer H, Lauche R, Haller Het al. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013; 29(5): 450–60.doi:10.1097/AJP.0b013e31825e1492 [DOI] [PubMed] [Google Scholar]
- 37.Berman BM, Lao L, Langenberg Pet al. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004; 141(12): 901–10 [DOI] [PubMed] [Google Scholar]
- 38.Cherkin DC, Sherman KJ, Kahn Jet al. Effectiveness of focused structural massage and relaxation massage for chronic low back pain: protocol for a randomized controlled trial. Trials. 2009; 10: 96 doi:10.1186/1745-6215-10-96 [DOI] [PMC free article] [PubMed] [Google Scholar]


