Abstract
Veterans of all war eras have a high rate of chronic disease, mental health disorders, and chronic multi-symptom illnesses (CMI).1-3 Many veterans report symptoms that affect multiple biological systems as opposed to isolated disease states. Standard medical treatments often target isolated disease states such as headaches, insomnia, or back pain and at times may miss the more complex, multisystem dysfunction that has been documented in the veteran population. Research has shown that veterans have complex symptomatology involving physical, cognitive, psychological, and behavioral disturbances, such as difficult to diagnose pain patterns, irritable bowel syndrome, chronic fatigue, anxiety, depression, sleep disturbance, or neurocognitive dysfunction.2-4 Meditation and acupuncture are each broad-spectrum treatments designed to target multiple biological systems simultaneously, and thus, may be well suited for these complex chronic illnesses. The emerging literature indicates that complementary and integrative medicine (CIM) approaches augment standard medical treatments to enhance positive outcomes for those with chronic disease, mental health disorders, and CMI.5-12
Key Words: iRest Yoga Nidra, acupuncture, veterans, military, complementary and integrative medicine (CIM), chronic multisymptom illness (CMI)
INTRODUCTION
Veterans of all war eras have a high rate of chronic disease, mental health disorders, and chronic multi-symptom illnesses (CMI).1-3 Many veterans report symptoms that affect multiple biological systems as opposed to isolated disease states. Standard medical treatments often target isolated disease states such as headaches, insomnia, or back pain and at times may miss the more complex, multisystem dysfunction that has been documented in the veteran population. Research has shown that veterans have complex symptomatology involving physical, cognitive, psychological, and behavioral disturbances, such as difficult to diagnose pain patterns, irritable bowel syndrome, chronic fatigue, anxiety, depression, sleep disturbance, or neurocognitive dysfunction.2-4 Meditation and acupuncture are each broad-spectrum treatments designed to target multiple biological systems simultaneously, and thus, may be well suited for these complex chronic illnesses. The emerging literature indicates that complementary and integrative medicine (CIM) approaches augment standard medical treatments to enhance positive outcomes for those with chronic disease, mental health disorders, and CMI.5-12
The War Related Illness and Injury Study Center at the Washington, DC, Veterans Affairs (VA) Medical Center (WRIISC-DC) has maintained an ongoing CIM program for veterans since 2007. This program offers outpatient acupuncture and iRest Yoga Nidra (Integrative Restoration Institute, San Rafael, California) as a complement to standard care for veterans of any combat era. Through “word of mouth” recruitment alone, the WRIISC-DC has successfully attracted veterans to these services as evidenced by 2857 total iRest Yoga Nidra and acupuncture patient visits in 2010. Clinicians have grown accustomed to referring to CIM interventions, particularly for veterans with chronic, difficult to treat conditions, and veterans demonstrate a high level of acceptability for both acupuncture and iRest interventions. The CIM program is well integrated into the Washington DC VA Medical Center and receives ongoing referrals without solicitation from multiple services (ie, Pain Clinic, Neurology Service, Mental Health Service, Trauma Services, Social Work, Primary Care, Hematology, Rehabilitation Medicine, Geriatrics, and Women's Clinic).
iRest Yoga Nidra is a form of guided meditation that induces deep relaxation through a multifaceted approach that includes breathing, body sensing, imagery, and progressive relaxation techniques. In the WRIISC-DC clinic, iRest yoga nidra is provided in a group setting by experienced instructors who have completed training under the developer of this meditation technique, Dr Richard Miller. As reported in various meta-analyses and systematic reviews, meditation-based approaches can lead to improvements in multiple physical and mental health problems simultaneously.5-8 Additionally, once learned, these approaches can be maintained as self-care practices by using mobile applications and CD or MP3 recordings. Thus, they can be cost-effective and sustainable adjuncts to care in the management of chronic disease.
Acupuncture originated in China more than 2500 years ago and is one of the oldest, most frequently used medical procedures in the world.9 It is defined as a Chinese medical procedure that treats illnesses and provides symptom relief by inserting needles at specified sites on the body.9 The WRIISC-DC acupuncture clinic includes individual and group auricular acupuncture. Individual acupuncture involves an individual session with a licensed acupuncturist trained in the Worsley 5-element model. In group auricular acupuncture, five acupuncture points on each ear are needled by a licensed acupuncturist in a group setting. These five points are explicitly designed to bring balance to the autonomic nervous system and are intended to restore balance and regulation to the sense of inner disorganization created by chronic or acute mental and/or physical stress. A growing body of research has shown that acupuncture may improve many physical and mental symptoms including nausea, headaches, musculoskeletal pain, fibromylagia, insomnia, depression, posttraumatic stress disorder, and addiction.9-12
METHODS
As part of program evaluation, anonymous self-report satisfaction questionnaires were administered periodically throughout a 1-year period (2010) to a random subset of veterans in the acupuncture and iRest Yoga Nidra WRIISC-DC clinics. Satisfaction questionnaires included questions regarding symptom reduction, patient satisfaction, and recommending these services to other veterans. These questionnaires were distributed to veterans attending acupuncture and iRest Yoga Nidra services and were completed at the end of treatment sessions.
Acupuncture (n = 118) and iRest Yoga Nidra (n = 186) satisfaction questionnaires were administered and collected for data analysis. Frequency analyses were used to evaluate the data collected from these satisfaction questionnaires. The iRest Yoga Nidra sample consisted of 29 females and 157 males, and the acupuncture sample consisted of 45 female and 73 males.
RESULTS
Completed satisfaction questionnaires of the acupuncture clinic (n = 118) suggest that 96% of surveyed veterans reported complete (45%) or somewhat (51%) improvement in physical and mental health symptoms. Furthermore, survey respondents reported good to excellent quality of care (97%), and 99% would recommend acupuncture to another veteran. Completed satisfaction questionnaires of the iRest Yoga Nidra clinic (n = 186) suggest that 95% of surveyed veterans reported complete (10%) or somewhat (85%) improvement in a wide range of both physical and mental health symptoms. Notably, survey respondents also reported very good to excellent quality of care (97%), and 100% reported that they would recommend iRest Yoga Nidra to other veterans. The overall acupuncture and iRest Yoga Nidra satisfaction questionnaire results are shown in Figure 1.
Figure 1.
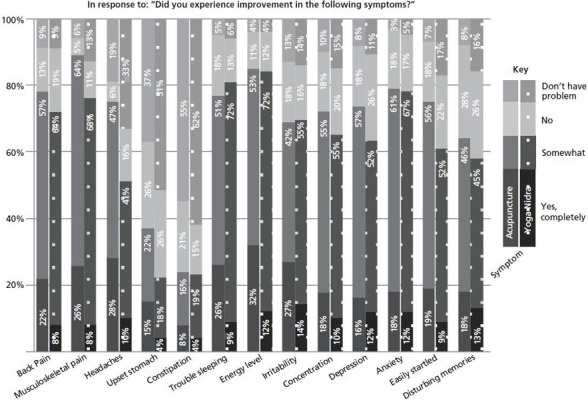
Total: acupuncture (n=118) and iRest Yoga Nidra (n=186) satisfaction data.
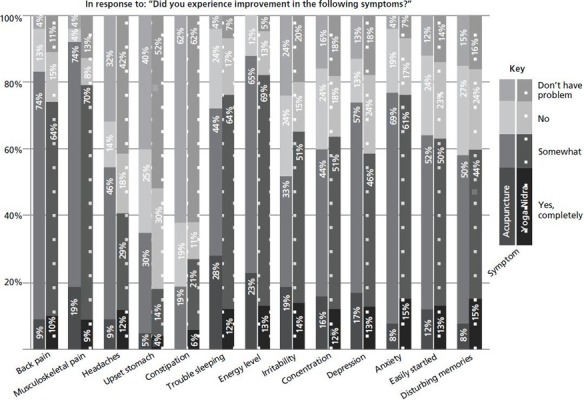
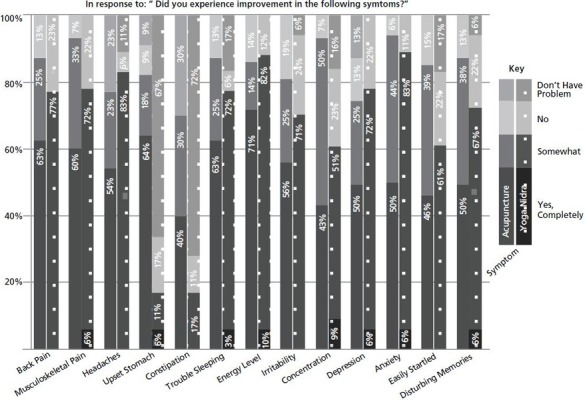
When examining the responses by war era, the majority of Operation Iraqi Freedom/Operation Enduring Freedom (OIF/OEF), Gulf War and Vietnam War veterans reported symptom improvement and satisfaction with both acupuncture and iRest Yoga Nidra services. The acupuncture and iRest Yoga Nidra satisfaction questionnaire results analyzed by war era are shown in Figures 2 through 4.
Figure 2.
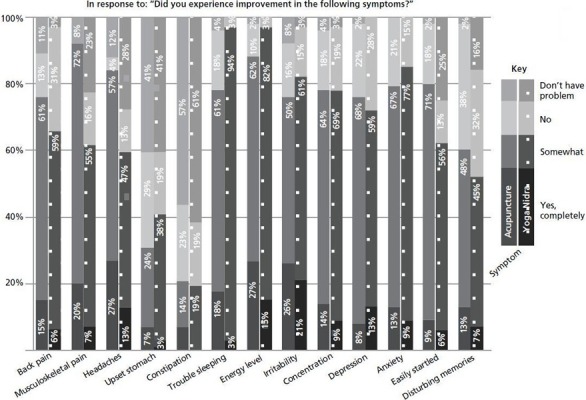
Operation Enduring Freedom/Operation Iraqi Freedom veterans: acupuncture (n=55) and iRest Yoga Nidra (n=36) satisfaction data.
Figure 4.
Vietnam veterans: acupuncture (n=31) and iRest Yoga Nidra (n=14) satisfaction data.
Figure 3.
Gulf War veterans: acupuncture (n=17) and iRest Yoga Nidra (n=20) satisfaction data.
DISCUSSION
Satisfaction data suggest that the vast majority of sampled veterans who received acupuncture and iRest Yoga Nidra were satisfied with care quality, noticed symptom improvement, and would recommend these services to other veterans. Notably, veterans reported improvement in multiple biological systems, including headaches, musculoskeletal pain, back pain, digestive difficulties, and a range of mental health symptoms. This preliminary research elucidates the potential for using CIM modalities in the treatment of veterans with chronic physical and mental health conditions. To date, there is limited published research investigating CIM treatment modalities specifically in the veteran population; thus, these satisfaction data add to the extant literature and suggests that CIM is widely accepted within a veteran population, and veterans report symptom improvement and satisfaction with these services.
The Veterans Health Administration (VHA) has 152 medical centers, and a recent 2011 survey by the Healthcare Analysis and Information Group (HAIG) indicated that 125 VHA facilities (82%) provide CIM service and/or refer patients to CIM service providers, with acupuncture and meditation being the two most common forms of treatment.13 Of the 125 sites that offered CIM modalities, the top five reasons for providing these services included (1) promote wellness (83%), (2) patient preferences (80%), (3) as an adjunct to chronic care (78%), (4) proven clinical effect (73%), and (5) provider request (65%).13 It is likely that many VA medical centers are considering developing formal CIM clinics and programs, and the present findings provide initial evidence for the high utilization and satisfaction of CIM within the VHA. These preliminary data can be used to assist with CIM program development in both the VHA and Department of Defense settings, especially as veteran interest and potential benefit for clinical care are considered. It is also likely, given the high rates of satisfaction in this sample, that a system of care with CIM components would see positive influence on satisfaction rates of overall care (ie, VHA healthcare) for those veterans electing to participate.
Although the preliminary satisfaction findings are promising, there are significant limitations of these data. The satisfaction questionnaires were not distributed in a controlled manner for data collection; they were given at the end of treatment sessions in the context of program development and quality improvement. Thus, it was not a systematic evaluation of the CIM treatments, and the data are subject to patient bias and perhaps even repeat responders. Veterans were not systematically tracked so attrition, demographics, and changes over time in treatment response and satisfaction were not available for examination. Also, the sample likely has a bias toward positive responding given that the sample includes those who were enrolled in the clinic(s) and we did not have a way to measure dropouts or those who were enrolled but decided not to complete a questionnaire because they were less satisfied and did not want to report non-positive findings. Nevertheless, the data collection was a first step in CIM program evaluation and influenced the development of a pilot study to systematically evaluate patient outcomes and satisfaction for those enrolled in the WRIISC-DC CIM services. Had we not found such a positive signal, we may not have pursued further clinical expansion and refinement from a research perspective. This pilot study will ameliorate many of the threats to validity described above and build on these preliminary satisfaction findings. The WRIISC-DC plans to use this pilot study to design more well-controlled research studies to further examine the effectiveness of these modalities and how they may best integrate within existing post-deployment healthcare.
Disclosures The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and had no relevant conflicts to disclose.
Contributor Information
Amanda Hull, War Related Illness and Injury Study Center, Veteran Affairs Medical Center, Washington, DC, United States..
Matthew Reinhard, War Related Illness and Injury Study Center, Veteran Affairs Medical Center, Washington, DC, United States..
Kelly McCarron, War Related Illness and Injury Study Center, Veteran Affairs Medical Center, Washington, DC, United States..
Nathaniel Allen, War Related Illness and Injury Study Center, Veteran Affairs Medical Center, Washington, DC, United States..
M. Cory Jecmen, War Related Illness and Injury Study Center, Veteran Affairs Medical Center, Washington, DC, United States..
Jeanette Akhter, War Related Illness and Injury Study Center, Veteran Affairs Medical Center, Washington, DC, United States..
Alaine Duncan, War Related Illness and Injury Study Center, Veteran Affairs Medical Center, Washington, DC, United States..
Karen Soltes, War Related Illness and Injury Study Center, Veteran Affairs Medical Center, Washington, DC, United States..
REFERENCES
- 1.Schult T, Awosika E, Hodgson M, Dyrenforth S.Disparities in health behaviors and chronic conditions in health care providers in the Veterans Health Administration. J Occup Environ Med. 2011; 53(10): 1134–45 [DOI] [PubMed] [Google Scholar]
- 2.Li B, Mahan CM, Kang HK, Eisen SA, Engel CC.Longitudinal health study of US 1991 Gulf War veterans: changes in health status at 10-year follow-up. Am J Epidemiol. 2011October1; 174(7): 761–8 [DOI] [PubMed] [Google Scholar]
- 3.Wilk J, Hoge C.Military and veteran populations. Benedek D, Wynn G.Clinical manual for management of PTSD (349–369). Arlington, VA: American Psychiatric Publishing, Inc; 2011 [Google Scholar]
- 4.Blanchard MS, Eisen SA, Alpern Ret al. Chronic multisymptom illness complex in Gulf War I veterans 10 years later. Am J Epidemiol. 2006; 163(1): 66–75 [DOI] [PubMed] [Google Scholar]
- 5.Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD.A pilot randomized control trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. 2010; 151(2): 530–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeidan F, Johnson SK, Diamond BJ, David Z, Goolkasian P.Mindfulness meditation improves cognition: Evidence of brief mental training. Conscious Cogn. 2010; 19(2): 597–605 [DOI] [PubMed] [Google Scholar]
- 7.Toneatto T, Nguyen L.Does mindfulness meditation improve anxiety and mood symptoms? A review of the controlled research. Can J Psychiatry. 2007April; 52(4): 260–6 [DOI] [PubMed] [Google Scholar]
- 8.Grossman P, Niemann L, Schmidt S, Walach H.Mindfulness-based stress reduction and health benefits: A meta-analysis. J Psychosom Res. 2004; 57(1): 35–43 [DOI] [PubMed] [Google Scholar]
- 9.Lee C, Wallerstedt D, Duncan Aet al. (2011). Design and rationale of a comparative effectiveness study to evaluate two acupuncture methods for the treatment of headaches associated with traumatic brain injury. Med Acupunct. 2011; 23(4): 237–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.NIH Consensus Statement. Acupuncture. 1997; 15(5): 1–34 [PubMed] [Google Scholar]
- 11.Hollifield M, Sinclair-Lian N, Warner TD, Hammerschlag R.Acupuncture for post-traumatic stress disorder. J Nerv Ment Dis. 2007June; 195(6): 504–13 [DOI] [PubMed] [Google Scholar]
- 12.Hull SK, Page CP, Skinner BD, Linville JC, Coeytaux RR.Exploring outcomes associated with acupuncture. J Altern Complement Med. 2006April; 12(3): 247–54 [DOI] [PubMed] [Google Scholar]
- 13.Hammond M, Vandenberg P.Complementary and alternative medicine. Milwaukee, WI: Healthcare Analysis and Information Group; 2011 [Google Scholar]


