Abstract
Background
Risk factors that are associated with depression in the mother also negatively affect the child. This research sought to extend current knowledge by examining the duration and timing of maternal depression as a moderator of: (1) the impact of dependent interpersonal stress (DIS), such as partner conflict or low social support, and contextual risk (e.g. poverty) on child dysregulation; and (2) continuity in early child dysregulation.
Method
Mother–child pairs (n=12 152) who participated in the Avon Longitudinal Study of Parents and Children (ALSPAC) were examined between pregnancy and age 4 years. Data on maternal depression were collected five times between pregnancy and 33 months postpartum; on DIS and contextual risk three times between pregnancy and 33 months; and on child dysregulation at age 2 and 4 years.
Results
Longitudinal latent class analysis identified a class of mothers (10%) who evinced a chronic level of depression between pregnancy and 33 months. For chronic-depressed versus non-depressed mothers, the results indicate that: (1) DIS predicted higher child dysregulation if experienced between pregnancy and age 2; (2) contextual risk had a differential effect on child dysregulation if experienced during pregnancy; and (3) children had higher continuity in dysregulation between age 2 and age 4.
Conclusions
Assessing the impact of the timing and duration of maternal depression, and different types of co-occurring risk factors, on child well-being is important. Maternal depression and associated DIS, in comparison to contextual risk, may be more responsive to intervention.
Keywords: Avon Longitudinal Study of Parents and Children, child dysregulation, contextual risk, dependent interpersonal stress, maternal depression
Introduction
In their seminal paper, Goodman & Gotlib (1999) posed the question, ‘What is it about having a depressed mother that places a child at increased risk for abnormal development?’ (p. 461), and then proposed a developmental model, with four main mechanisms, to explain the increased risk transmission. The first two mechanisms are biological: the heritability of depression (Kendler et al. 2006) and dysfunctional neuroregulatory mechanism in children (Oberlander et al. 2008). The third is disturbed interpersonal processes, including child exposure to negative maternal cognitions and maladaptive parenting (Cummings et al. 2005; Pawlby et al. 2011). The focus of the present research is Goodman & Gotlib’s (1999) fourth mechanism: the stressful contexts of the children.
Studies have long shown that children are negatively affected not only by their mother’s depression but also by risk factors associated with their mother’s depression (Billings & Moos, 1983; Cox et al. 1987a; Hammen et al. 1987). Risk factors associated with maternal depression are reported to influence difficult childhood temperament (Cicchetti et al. 1998), neurological function (Ashman et al. 2008) and externalizing and internalizing disorders (Barker et al. 2012). The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trials (Weissman et al. 2006) showed that, although the children of mothers whose depression remitted also showed signs of improvement, the children who did not improve had mothers whose depression did not remit and who had experienced the most severe risk factors.
These results suggest that interventions aimed at the well-being of children of depressed parents also need to target associated risk factors. Goodman & Gotlib (1999) suggested that at least two types of information may further inform interventions: (1) differentiating dependent interpersonal stress (DIS) from contextual risk; and (2) the timing and duration of depression. With regard to stress, Hammen (1991, 2006) distinguished DIS, such as relationship disputes or low social support (Kendler & Gardner, 2010), from more independent contextual risks (e.g. poverty, crime), in that depressed persons can generate and increase DIS whereas rates of contextual risks are less influenced by depression. Stressors such as DIS, however, seem to occur at elevated rates in high-risk contexts (Brown et al. 2008; Kessler et al. 2010), as does maternal depression (Barker et al. 2012), and each can impact child well-being. For example, one study reported that difficult-to-manage preschool children had depressed mothers with low social support and high poverty (Parry, 1986). The distinction between contextual risk and DIS is important; if high DIS is at last partially dependent on depression, these stressors may be more responsive to interventions than contextual risks.
Goodman & Gotlib (1999) also suggested that the duration and timing of child exposure to depression could act as a moderator in the link between maternal depression and long-term courses of child psychopathology. The authors stated that: (1) as many as 25% of persons who experience a first major depression may go on to experience chronic depression; and (2) long-term effects of chronic maternal depression on child psychopathology may be more pronounced early in development. Biological systems relevant to regulation of arousal are functionally immature during pregnancy and at birth, but mature gradually during the first years of life (Glover, 2011). A healthy maternal lifestyle (prenatal and early postnatal) and the sensitive regulation of the infant’s emotions and behaviors are most needed during the first few years of life, to ensure mastery of early social and behavorial skills (Goodman & Gotlib, 1999; Feldman et al. 2009). However, the presence of chronic depression and associated risk factors may render a mother incapable of providing such care to herself and to her child during pregnancy and the first years of a child’s life. Research has indeed shown that DIS related to maternal depression can negatively affect adolescent psychopathology (Hammen et al. 2004; Garber & Cole, 2010). The degree to which similar effects are present early in development, within an integrated developmental model that incorporates (a) DIS and contextual risk and (b) the duration and timing of maternal depression, is yet to be evaluated.
The focus of the present research was threefold. The first aim was to evaluate the duration and timing of maternal depression (from pregnancy to 33 months). It was expected that up to 25% of the sample could show a chronic class of clinical depression (Goodman & Gotlib, 1999). The second aim was to examine the degree to which a class of chronic depression might moderate the impact of DIS and contextual risk on child emotional-behavioral psychopathology in the following manner: (1) DIS would have significantly greater impact on child psychopathology for chronic depressed versus non-depressed mothers; and (2) compared with the DIS, the impact of contextual risk on child psychopathology would not show consistent contrasts. The rationale for the differing hypotheses of contextual risks versus DIS is from previous research showing that, during infancy, contextual risk can affect caregiver mental health more than that of the child (Kohen et al. 2008). The third aim was to determine whether, as expected, child emotional-behavioral dysregulation would show higher continuity for chronic-depressed versus non-depressed mothers.
Method
Sample
The Avon Longitudinal Study of Children and Parents (ALSPAC) was established to understand how genetic and environmental characteristics influence health and development in parents and children. All pregnant women resident in a defined area in the South West of England, with an expected date of delivery between 1 April 1991 and 31 December 1992, were eligible and 13761 women (contributing 13867 pregnancies) were recruited. These women have been followed over the past 19–22 years (Fraser et al. 2012). When compared to 1991 National Census Data, the ALSPAC sample was found to be similar to the UK population as a whole (Boyd et al. 2012). Ethical approval for the study was obtained from the ALSPAC Law and Ethics Committee and the Local Research Ethics Committees.
Measures
Mothers completed questionnaires during their pregnancy and their child’s infancy and childhood. The early risk factors examined here were drawn from the family adversity measure (Bowen et al. 2005) completed between birth and approximately 4 years of child age.
Maternal depression
Maternal depression was assessed repeatedly (at 32 weeks prenatal, and 8 weeks, 8 months, 21 months and 33 months postnatal) with the Edinburgh Postnatal Depression Scale, a widely used 10-item self-report questionnaire that has been shown to be valid during and outside the postnatal period (Cox et al. 1987b; Murray & Carothers, 1990). A score of 13 predicts a clinical diagnosis of depression (Murray & Carothers, 1990).
Contextual risk factors
Contextual risk factors consisted of mother reports, during pregnancy, between child age 0 and 2 years, and between child age 2 and 4 years. At each age, any indication of the risk resulted in a score of 1 (0=none). There were seven total risks, resulting in a potential range of 0–7 risk exposures. The seven risks included: (1) inadequate basic living conditions such as not having a working bath/shower, no hot water, no indoor toilet and/or no working kitchen (pregnancy: assessed at 8 weeks; age 0–2: assessed at 2, 8 and 21 months; age 2–4: assessed at 33 and 47 months); (2) inadequate housing as any indication of crowding (pregnancy: at 8 weeks; age 0–2: 21 months; age 2–4: 33 months) and/or homelessness (pregnancy: at 18 weeks; age 0–2: 2, 8 and 21 months; age 2–4: 33 months); (3) housing defects as any indication of mold, roof leaks, and rats, mice or cockroaches (pregnancy: at 18 weeks; age 0–2: 8 and 21 months; age 2–4: 33 months); (4) poverty, coded using the Registrar General’s social class scale (OPCS, 1991) (pregnancy: at 32 weeks; age 0–2: 8 and 21 months; age 2–4: 33 months); (5) being a single caregiver [e.g. not cohabiting, not in a relationship (pregnancy: at 32 weeks; age 0–2: 6 and 21 months; age 2–4: 33 and 47 months)]; (6) early parenthood [≤19 years (at 18 weeks in pregnancy)]; and (7) low educational attainment [e.g. did not finish mandatory schooling (pregnancy: at 32 weeks; age 0–2: 21 months; age 2–3: 33 months)].
DIS
Data on DIS were collected at the same times as that on the contextual risks. The five DIS factors resulted in a possible range of 0–5 exposures, and included: (1) mother experiencing partner cruelty [e.g. any indication of emotional and/or physical abuse from partner (pregnancy: assessed 18 weeks; age 0–2: 2, 6 and 21 months; age 2–4: 33 and 47 months)]; (2) low partner affection to mother [e.g. partner does not show affection, does not hug/kiss, low intimate bond (pregnancy: at 12 weeks; age 0–2: 8 months; age 2–4: 33 months)]; (3) low partner social support [does not discuss feelings with, feel supported by (pregnancy: at 18 weeks; age 0–2: 2 and 8 months)]; (4) low practical support [i.e. whether there is anyone who could lend the mother £100 and/or anyone the mother could turn to in times of trouble (pregnancy: at 12 weeks; age 0–2: 2 and 8 months)]; and (5) major family problems as examined through social services data [e.g. child in the household taken into extra-familial care, child in household registered with at-risk register, child no longer living in household (pregnancy: at 18 weeks; age 0–2: 21 months; age 2–4: 33 and 47 months)].
Child emotional and behavioral dysregulation
Child emotional and behavioral dysregulation at ages 2 and 4 was measured by mother reports on the Carey Infant Temperament Scale (Carey & McDevitt, 1978) and the Strengths and Difficulties Questionnaire (SDQ; Goodman, 2001) respectively. Four subscales from the Carey Infant Scale were included: activity, adaptability, intensity and mood. For the SDQ, three subscales where included: hyperactivity, conduct problems and emotional difficulties. These subscales were used as indicators of the latent construct of child dysregulation. In a two-factor confirmatory solution, model fit was marginal [Comparative Fit Index (CFI)=0.91, root mean square error of approximation (RMSEA)=0.087, 95% confidence interval (CI) 0.081–0.089]; the standardized loadings for the latent dysregulation construct for the Carey Scales (range 0.57–0.83) and the SDQ (range 0.43–0.73) were acceptable (Tabachnick & Fidell, 2001); there were no sex differences in the loadings (, p=0.377); and the latent coefficient of prediction was high (b=0.597, s.e.=0.013, p<0.0001) and suggestive of homotypic continuity of a construct.
Attrition and missing data
A total of 12151 of the original 13 867 mothers were included in the analysis. Mothers who were excluded had complete missing data on the five self-reports of depression. Of the 12151 who were included, 1.1% had one report of depression, 8.4% had two reports of depression, 13.7% had three reports of depression, 25.7% had four reports of depression and 51% had five reports of depression. The included mothers had complete data available for at least one of both the scale scores of DIS and contextual risk. Child dysregulation was available for 85% of the 12151 mothers. As listwise deletion of families with partial complete data can increase sample bias (e.g. exclude the most high risk families; Enders, 2010), missing for child dysregulation was handled via Full Information Maximum Likelihood Estimation (Enders, 2010).
Analysis
The analysis proceeded in three main steps. In the first step we estimated a longitudinal latent class (LLC) model of maternal depression, a type of analysis that accounts for time ordering of variables and can function as a piecewise growth mixture model (see Croudace et al. 2003). More generally, an LLC model can easily describe classes of mothers who may follow different non-linear patterns of depression (e.g. prenatal only, postnatal only, chronic depression) over time. A series of models was fitted, starting with a one-class model and moving to a five-class model. Previously, recommendations (e.g. Mutheén, 2004) on selecting the best model for the data included reference to fit indices such as the Bayesian Information Criterion (BIC; lower values indicate a more parsimonious model), the Lo–Mendell–Rubin likelihood ratio test (LMR-LRT: a k – 1 LR-based method for determining the ideal number of trajectories) and entropy (a measure of classification accuracy with values closer to 1 indexing greater precision). Clark & Mutheén (unpublished observations) have recently suggested that entropy is crucial, with a recommended value of 0.80.
In the second step, correlations between the variables by the different latent classes of maternal depression were examined. For example, here it was assessed the degree to which DIS and contextual risks correlated higher with child psychopathology for depressed versus non-depressed mothers.
In the third step, the patterns in the correlations were tested in a multiple group, autoregressive cross-lagged (ARCL) model. The ARCL technique is widely used to assess associations in data derived from non-experimental, longitudinal research designs (Curran & Bollen, 2001). In this modeling approach, each variable in the model is regressed on all of the variables that precede it in time, which includes autoregressions (child dysregulation predicting child dysregulation) and cross-lags (DIS predicting child dysregulation). For moderation, the ARCL coefficients can be stratified by group (e.g. depressed versus non-depressed mothers) and nested differences can be tested. Withintime correlations (DIS and contextual risk during pregnancy) can also be estimated and controlled for in the cross-lagged effects.
All analyses were conducted in Mplus version 6.21 (Mutheén & Mutheén, 1998–2010). To provide robust estimates and to account for missing values, full information maximum likelihood estimation with robust standard errors (MLR) was used. Model fit was determined through the CFI (acceptable fit ≥0.90) (Bentler & Bonett, 1980) and RMSEA (acceptable fit ≤0.08) (Browne & Cudeck, 1993). Satorra–Bentler scaled χ2 difference tests (Satorra, 2000) were used to test nested model comparisons, which adjust for non-normality in the distribution of the data.
Results
Step 1: LLC models of maternal depression
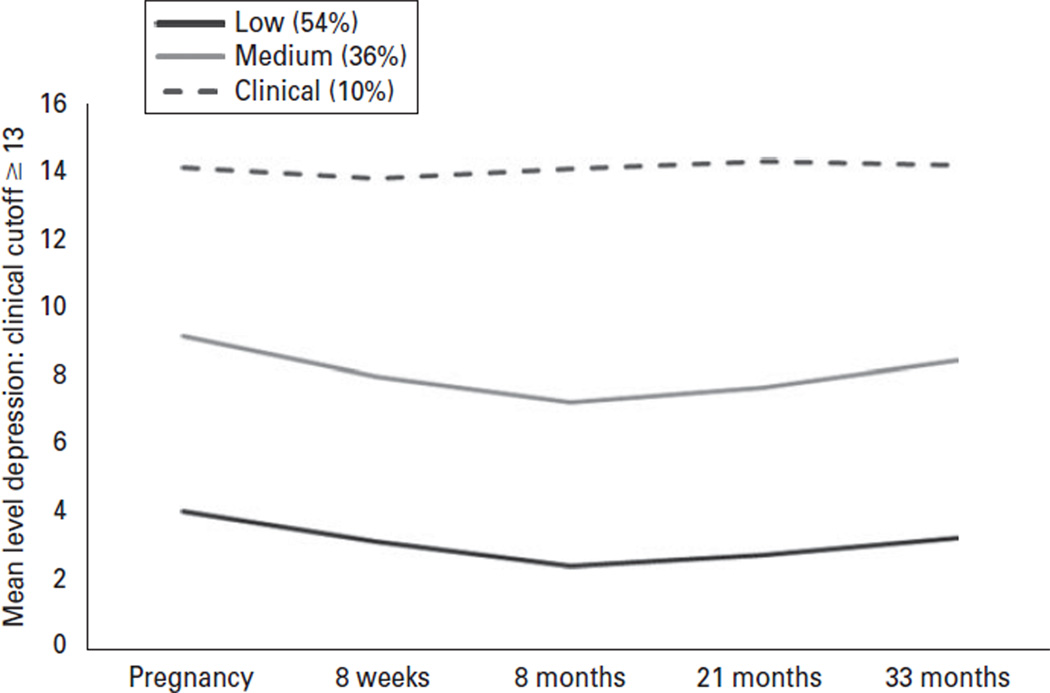
Figure 1 shows the three-class model of maternal depression, and the fit statistics for the one-class to five-class models. As can be seen, although the BIC decreased with additional classes, at the four-class model the entropy was less than 0.80 at the five-class model, and the LMR-LRT was non-significant, which, when combined, suggested that the three-class or two-class model was a better fit to the data. The three-class model was chosen. The principal difference between the three-class and two-class models was that in the former, a chronic-depressed group of mothers (i.e. the scores on the EPDS, at each assessment, were >13) was identified whereas the latter had two non-depressed classes mothers, who varied in symptom levels.
Fig. 1.
Longitudinal latent classes of maternal depression. One-class model: entropy=not applicable (n.a.), Bayesian Information Criterion (BIC)=320814.32, Lo–Mendell–Rubin likelihood ratio test (LMR-LRT)=n.a.; two-class model: entropy=0.84, BIC=303650.96, LMR-LRT=0.0000; three-class model: entropy=0.81, BIC=298662.28, LMR-LRT=0.0000; four-class model: entropy=0.78, BIC=297433.04, LMR-LRT=0.0000; five-class model: entropy=0.78, BIC=296784.33, LMR-LRT=0.4625.
The three classes identified were those mothers who were chronic-depressed (10%), those who reported medium symptoms (36%) and those who reported low symptoms (54%). The latter two classes of mothers (i.e. the medium and low) were combined to allow comparisons of chronic-depressed mothers with the non-depressed mothers.
Step 2: Correlations of study variables for chronic-depressed versus non-depressed mothers
Table 1 contains the correlations, means, standard deviations and skew of the study variables. These statistics are separated by the LLC analyses of maternal depression. With regard to correlations, child dysregulation was associated with both contextual risk and DIS, and these were somewhat larger for chronic-depressed than non-depressed mothers. With regard to mean levels of risk exposures, prevalence was low but, on average, at least two times greater in contextual risks and three times greater for DIS, for chronic-depressed versus non-depressed mothers. Skew was high for the DIS of non-depressed mothers and was therefore transformed.
Table 1.
Correlations and descriptive statistics of the variables included in the study by non-depressed mothers (above the diagonal) and chronic-depressed mothers (below the diagonal)
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
|---|---|---|---|---|---|---|---|---|
| (1) Child dysregulation: age 2 | – | 0.577 | 0.064 | 0.069 | 0.057 | 0.083 | 0.125 | 0.046 |
| (2) Child dysregulation: age 4 | 0.683 | – | 0.119 | 0.164 | 0.153 | 0.099 | 0.159 | 0.141 |
| (3) Contextual risk: pregnancy | 0.201 | 0.230 | – | 0.632 | 0.423 | 0.255 | 0.216 | 0.123 |
| (4) Contextual risk: age 0–2 | 0.155 | 0.251 | 0.625 | – | 0.666 | 0.216 | 0.207 | 0.139 |
| (5) Contextual risk: age 2–4 | 0.077 | 0.209 | 0.390 | 0.624 | – | 0.156 | 0.168 | 0.172 |
| (6) DIS: pregnancy | 0.243 | 0.251 | 0.278 | 0.274 | 0.278 | – | 0.429 | 0.188 |
| (7) DIS: age 0–2 | 0.143 | 0.264 | 0.208 | 0.267 | 0.257 | 0.445 | – | 0.159 |
| (8) DIS: age 2–4 | 0.031 | 0.114 | 0.093 | 0.133 | 0.390 | 0.170 | 0.391 | – |
| Non-depressed | ||||||||
| Mean (s.d.) | 75.53 (13.94) | 7.16 (3.76) | 0.34 (0.69) | 0.67 (0.91) | 0.53 (0.81) | 0.34 (0.69) | 0.61 (0.90) | 0.25 (0.55) |
| Raw skew | −0.03 | 0.65 | 1.87 | 1.53 | 1.75 | 2.30 | 1.56 | 2.29 |
| log skew | – | – | – | – | – | 1.62 | 0.88 | 1.75 |
| Depressed | ||||||||
| Mean (s.d.) | 82.28 (14.79) | 9.41 (4.37) | 0.87 (1.00) | 1.21 (1.21) | 1.01 (1.06) | 1.51 (1.23) | 1.84 (1.47) | 1.06 (0.79) |
| Raw skew | −0.02 | 0.42 | 1.12 | 0.98 | 1.18 | 1.07 | 0.35 | 1.02 |
| Log skew | – | – | – | – | – | 0.48 | −0.29 | 0.66 |
DIS, Dependent interpersonal stress; s.d., standard deviation; –, not transformed.
All correlations are significant at p<0.05.
Step 3: Multiple group ARCL model
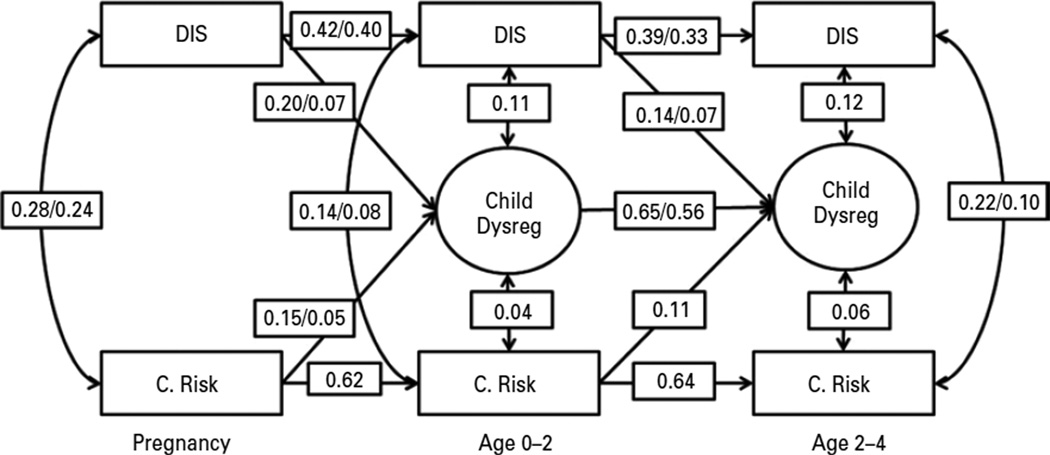
To examine differences in the chronic-depressed versus non-depressed mothers we tested a series of nested model comparisons, including: (1) the cross-lagged predictions of the DIS, contextual risks and child dysregulation; (2) the auto-regressions of the DIS, contextual risks and child dysregulation; and (3) the within-time associations between DIS and contextual risks. The model where all parameters were free to vary between depressed and non-depressed mothers showed an acceptable fit (, p<0.001, CFI=0.92, RMSEA=0.063, 90% CI 0.061–0.065). This model was the comparison model for all nested tests presented below.
The cross-lagged predictions varied significantly between the chronic-depressed and non-depressed mothers. (, p<0.0001). (Note that there were 10 degrees of freedom for the overall difference test as there were 10 total cross-lagged parameters; see Fig. 2.) Nested difference tests showed that the following predictions were greater for chronic-depressed versus non-depressed mothers: (1) contextual risks (pregnancy) predicted child dysregulation (age 2) (, p=0.023) (2) DIS (pregnancy) predicted child dysregulation (age 2) (, p=0.003), and (3) DIS (age 0–2) predicted child dysregulation (age 4) (, p=0.013). Chronic-depressed and non-depressed mothers did not significantly differ in (1) the significant prediction of contextual risks (age 0–2) to age 4 child dysregulation or in (2) the cross-lagged effects between DIS and contextual risks.
Fig. 2.
Multiple group path analysis. Path coefficients: depressed/non-depressed or averaged across all mothers; single arrow paths=predictions; double arrow paths=correlations; circles=latent variables (items not shown for the sake of a simple presentation); rectangular=manifest variable. All parameters shown are significant at p<0.05. The pathways from child emotional and behavioral dysregulation (Child Dysreg) to dependent interpersonal stress (DIS) and contextual risks (C. Risk) failed to reach significance; predictions between DIS and C. Risk are not shown for the simplicity of the presentation (and because these relationships are not central to the current research questions), but are available on request from the author.
The auto-regressions also varied significantly between the depressed and non-depressed mothers (, p<0.001). Nested difference tests showed that, compared to non-depressed mothers, chronic-depressed mothers reported higher continuity in: (1) age 2 to age 4 child dysregulation (, p=0.023); (2) DIS from pregnancy to age 0–2 (, p=0.021); and (3) DIS from age 0–2 to age 2–4 (, p<0.001). Beyond these differences, in general, the magnitude of the continuity for contextual risk was approximately 1.5 times higher than the magnitude of continuity of the DIS.
Within-time associations varied significantly between the chronic-depressed and non-depressed mothers (, p<0.001). Nested difference tests showed that the associations between DIS and contextual risks were significantly higher for chronic-depressed versus non-depressed mothers at pregnancy (, p<0.001), at age 0–2 (, p<0.001) and at age 2–4 (, p<0.001). The within-time covariance of DIS and contextual risks with child dysregulation were significant, but did not significantly vary between chronic-depressed and non-depressed mothers. Of interest, DIS was significantly higher in correlations with child dysregulation than contextual risks with child dysregulation, at age 0–2 (, p=0.035) and age 2–4 (, p=0.011).
Discussion
This study is the first to examine the timing and duration of maternal depression as a moderator of the impact of co-occurring DIS and contextual risk on early child dysregulation, and continuity in early child dysregulation. Of the 12152 ALSPAC mothers, 10% were identified as being chronically depressed between pregnancy and 33 months postpartum, so the duration was long and the child’s exposure was early. Compared to children of non-depressed mothers, children of chronic-depressed mothers were exposed to higher levels of DIS and contextual risks. At both pregnancy and age 2, the DIS impact on later child dysregulation was significantly higher for children of chronic-depressed mothers. At pregnancy, the impact of contextual risk on child dysregulation was also significantly higher for children of chronic-depressed mothers. Furthermore, children of chronic-depressed mothers showed higher continuity in dysregulation.
To examine the timing and duration of maternal depression, the current study used an LLC approach and identified 10% of the mothers to be at a clinical level of depression between pregnancy and 33 months postpartum. Previous studies using a similar analytic approach have similarly identified a group of chronic and clinically depressed mothers. Of note, when centered around the first years of a child’s life, the percentage of mothers in the chronic-depressed class (11%) was very close to that of the current study (Campbell et al. 2007). However, when the studies also included later developmental periods (pre-adolescence and adolescence), the percentage of chronic-depressed mothers (2.5–4.0%) was lower (Ashman et al. 2008; Campbell et al. 2009). These findings corroborate the previous reports that rates of depression in females peak during pregnancy and in the early postnatal years (Kessler, 2003), and that latent class approaches can capture this peak but only if focused within early development (e.g. Nagin, 2005).
However, whatever the duration of the developmental period, Campbell et al. (2007, 2009) reported that youth whose mothers were in a latent class of chronic-depression had the highest internalizing and externalizing difficulties (e.g. at both at school entry and at age 15), in addition to the highest exposure to associated risk factors. The use of latent classes as predictors of outcomes, however, can somewhat limit the assessment of dynamic co-occurring developmental processes, such as risk exposures, that might also contribute to child dysregulation (see, for example, Barker et al. 2010). There is good reason to assess dynamic processes related to maternal depression, as previous research has indicated that associated risk factor exposure can explain half (or more) of the risk transmission of maternal depression (Cicchetti et al. 1998; Barker et al. 2012). Moreover, risk exposure (e.g. poverty, poor inter-relationships with others, poor housing conditions) is greatest while the mother is clinically depressed (Cox et al. 1987a; Hammen et al. 1987), and when maternal depression remits, children also tend to improve (Garber et al. 2011).
The present study is the first the use latent classes of maternal depression to assess the dynamic cooccurrence of different types of risk factors and also continuity in child dysregulation. Children of chronic-depressed mothers were more exposed to and affected by DIS at pregnancy and age 2. Contextual risk, however, had more effect on children of chronic-depressed mothers at pregnancy only. The distinction between DIS and contextual risk may be important. The stress generation hypothesis (Hammen, 1991) that underlies DIS has emphasized that depressed persons can create interpersonal stress (e.g. conflict with partner, low social support, low partner affection). Therefore, the generation of DIS by a depressed caregiver can serve to maintain a risk environment that is proximal to the social milieu during pregnancy and the first years of life, when the child is particularly dependent on the quality of the environment provided by the caregiver (Goodman & Gotlib, 1999).
Of note, after pregnancy, the contextual risks transitioned to function as a general risk for dysregulation in children of chronic-depressed and non-depressed mothers alike, which underscores the ubiquitous nature of poverty on the well-being of children and adults (e.g. Miller et al. 2009; Shonkoff et al. 2009). However, the fact that contextual risk during pregnancy impacted later child dysregulation for chronic-depressed mothers might support the critical period hypothesis, where, for example, high stress and depression during pregnancy can lead to an intrauterine environment that is not conducive to healthy fetal development (Weinstock, 2008), and can then increase risk for behavioral and emotional maladjustment in the child (Glover, 2011). However, the exact mechanisms of this pre- and post-natal difference could not be tested because of the non-biological nature of the data in this study (Barker et al. 2011).
Continuity in child deregulation (age 2–4) was found to be higher for children of chronic-depressed mothers. It is important to note that in Goodman & Gotlib’s (1999) theoretical model, this age range was defined as a period of increased vulnerability for long-term maladjustment (in adolescence and adulthood). Hence, the current research should be considered a test of early vulnerability in children. That said, the current results do show a transition from age 2 dysregulated temperament (Carey & McDevitt, 1978) to a measure (at age 4) that has been validated in children and adolescents, and that has good predictability of adolescent conduct disorder and depression (Goodman, 2001).
Of note, however, the high continuity in dysregulation for children of chronic-depressed mothers was above and beyond the impact of DIS and contextual risks. Hence, in accordance with Goodman & Gotlib (1999), additional factors, such as the heritability of depression, neuroregulatory mechanisms and maladaptive parenting, need to be examined to explain the increased continuity in deregulation. A related point is that the DIS measure used here is broad and includes only one item that assesses the most researched, and perhaps influential (Rutter & Quinton, 1984), interpersonal stressor: the effect of marital discord on children (Cummings et al. 2004). Therefore, the current results may have underestimated the effect of marital discord. Moreover, the marital discord item used here came from mothers self-reporting partner cruelty. Although this was conceptualized as partially dependent on mother’s depression, this may not be the case for all women. Certain of these women may have been victimized by their partners, which could also result in higher depression and DIS, along with increased potential of co-occurring child maltreatment (Holden, 2003).
The present results should be interpreted in the context of six main limitations. First, much of the research on dependent stressors follows contextual threat methods established by Brown & Harris (1978) and Hammen et al. (1989) that include interviews that objectify the circumstances and impact of the stress, which are meant to minimize potential biases associated with self-reports. Second, the current study was limited by the use of symptom scales to assess depression in mothers and dysregulation in children rather than more thorough diagnostic interviews and/or observations. Third, most measures were based on maternal reports, raising the possibility of shared method variance. Future studies should incorporate multiple informants. Fourth, although the mothers and children of ALSPAC represent a broad spectrum of socio-economic status (SES) backgrounds, the sample includes relatively low rates of ethnic minorities. The present results will need replication with more ethnically diverse samples. Fifth, the present paper focused on maternal depression and associated risk factors. As highlighted in the introduction and discussion sections of this paper, however, the quality of parenting a child receives is an important potential mediator of the association measures of maternal psychopathology and child maladjustment. Sixth, the analytic routine chosen for this study was specific to the overall research question: comparing the relative impacts of DIS and contextual risks on child dysregulation of chronic-depressed versus non-depressed mothers. Testing the specifics of the stress generation hypothesis would require a different analytic model.
The current study is useful if the results can be translated into practical knowledge on how risk factors associated with depression in the mother may affect children’s adjustment. Our results underscore that early timing and extensive duration of maternal depression co-occur with early timing and long duration of child exposure to DIS and contextual risks. Because the children of the chronic-depressed mothers were impacted by the depression, DIS and contextual risk, beginning in pregnancy and in the first years of life, preventive interventions that target at-risk families as early as possible are warranted. For example, identifying at-risk women during pregnancy with the intention to provide intensive postpartum support may reduce postnatal depression for these women (Dennis, 2005). Hence, the children of at-risk mothers who receive such support may be less exposed to DIS than at-risk mother who do not. As suggested by Garber et al. (2011), practical and cost-efficient support, at the community level, should also be considered a valuable resource. For example, obstetric clinics and community agencies (e.g. schools, churches, health-care settings) may be used to provide at-risk parents with information about how parental depression can work to generate stressful interpersonal life events that can also affect their children.
Acknowledgments
I am very grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses; and to colleagues (R. T. Salekin, E. Viding, B. Maughan, T. Kretschmer) for providing the feedback on a previous version of the manuscript. The UK Medical Research Council (grant ref. 74883), the Wellcome Trust (grant ref. 0754567) and the University of Bristol provide core support for ALSPAC. E. D. Barker had full access to all of the data in this study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The analysis and writing of the paper was supported by a grant from the National Institute of Child and Human Development to E. D. Barker (NIH-1R01 HD068437-01A1).
Footnotes
Declaration of Interest
None.
References
- Ashman SB, Dawson G, Panagiotides H. Trajectories of maternal depression over 7 years: relations with child psychophysiology and behavior and role of contextual risks. Development and Psychopathology. 2008;20:55–77. doi: 10.1017/S0954579408000035. [DOI] [PubMed] [Google Scholar]
- Barker ED, Copeland W, Maughan B, Jaffee SR, Uher R. Relative impact of maternal depression and associated risk factors on offspring psychopathology. British Journal of Psychiatry. 2012;200:124–129. doi: 10.1192/bjp.bp.111.092346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker ED, Jaffee SR, Uher R, Maughan B. The contribution of prenatal and postnatal maternal anxiety and depression to child maladjustment. Depression and Anxiety. 2011;28:696–702. doi: 10.1002/da.20856. [DOI] [PubMed] [Google Scholar]
- Barker ED, Oliver BR, Maughan B. Co-occurring problems of early onset persistent, childhood limited, and adolescent onset conduct problem youth. Journal of Child Psychology and Psychiatry. 2010;51:1217–1226. doi: 10.1111/j.1469-7610.2010.02240.x. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Billings AG, Moos RH. Comparisons of children of depressed and nondepressed parents: a social-environmental perspective. Journal of Abnomal Child Psychology. 1983;11:463–485. doi: 10.1007/BF00917076. [DOI] [PubMed] [Google Scholar]
- Bowen E, Heron J, Waylen A, Wolke D. Risk for domestic violence during and after pregnancy: findings from a British longitudinal study. British Journal of Obstetrics and Gynaecology. 2005;112:1083–1089. doi: 10.1111/j.1471-0528.2005.00653.x. [DOI] [PubMed] [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, Molloy L, Ness A, Ring S, Davey Smith G. Cohort Profile: The ‘Children of the 90s’ – the index offspring of the Avon Longitudinal Study of Parents and Children. International Journal of Epidemiology. 2012 doi: 10.1093/ije/dys064. Published online: 16 April 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GW, Craig TKJ, Harris TO. Parental maltreatment and proximal risk factors using the Childhood Experience of Care & Abuse (CECA) instrument: a life-course study of adult chronic depression – 5. Journal of Affective Disorders. 2008;110:222–233. doi: 10.1016/j.jad.2008.01.016. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris T. Social Origins of Depression: A Study of Psychiatric Disorder in Women. London: Tavistock; 1978. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993. pp. 230–258. [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology. 2007;43:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Morgan-Lopez AA, Cox MJ, McLoyd VC. A latent class analysis of maternal depressive symptoms over 12 years and offspring adjustment in adolescence. Journal of Abnormal Psychology. 2009;118:479–493. doi: 10.1037/a0015923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey WB, McDevitt SC. Revision of the Infant Temperament Questionnaire. Pediatrics. 1978;61:735–739. [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Maternal depressive disorder and contextual risk: contributions to the development of attachment insecurity and behavior problems in toddlerhood. Development and Psychopathology. 1998;10:283–300. doi: 10.1017/s0954579498001618. [DOI] [PubMed] [Google Scholar]
- Cox AD, Puckering C, Pound A, Mills M. The impact of maternal depression in young children. Journal of Child Psychology and Psychiatry. 1987a;28:917–928. doi: 10.1111/j.1469-7610.1987.tb00679.x. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: the development of the Edinburgh 10-item Postnatal Depression Scale. British Journal of Psychiatry. 1987b;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Croudace TJ, Jarvelin MR, Wadsworth MEJ, Jones PB. Developmental typology of trajectories to nighttime bladder control: epidemiologic application of longitudinal latent class analysis. American Journal of Epidemiology. 2003;157:834–842. doi: 10.1093/aje/kwg049. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Goeke-Morey MC, Papp LM. Everyday marital conflict and child aggression. Journal of Abnormal Child Psychology. 2004;32:191–202. doi: 10.1023/b:jacp.0000019770.13216.be. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Keller MB, Davies DR. Towards a family process model of maternal and paternal depressive symptoms: exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Bollen KA. The best of both worlds: combining autoregressive and latent curve models. In: Collins LM, Sayer AG, editors. New Methods for the Analysis of Change. Washington, DC: American Psychological Association; 2001. pp. 105–135. [Google Scholar]
- Dennis C-L. Psychosocial and psychological interventions for prevention of postnatal depression : systematic review. British Medical Journal. 2005;331:15. doi: 10.1136/bmj.331.7507.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK. Applied Missing Data Analysis. New York: Guilford Press; 2010. [Google Scholar]
- Feldman R, Granat A, Pariente C, Kanety H, Kuint J, Gilboa-Schechtman E. Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:919–927. doi: 10.1097/CHI.0b013e3181b21651. [DOI] [PubMed] [Google Scholar]
- Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, Henderson J, Macleod J, Molloy L, Ness A, Ring S, Nelson SM, Lawlor DA. Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. International Journal of Epidemiology. 2012 doi: 10.1093/ije/dys066. Published online: 16 April 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Ciesla JA, McCauley E, Diamond G, Schloredt KA. Remission of depression in parents: links to healthy functioning in their children. Child Development. 2011;82:226–243. doi: 10.1111/j.1467-8624.2010.01552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Cole DA. Intergenerational transmission of depression: a launch and grow model of change across adolescence. Development and Psychopathology. 2010;22:819–830. doi: 10.1017/S0954579410000489. [DOI] [PubMed] [Google Scholar]
- Glover V. Annual Research Review: Prenatal stress and the origins of psychopathology: an evolutionary perspective. Journal of Child Psychology and Psychiatry. 2011;52:356–367. doi: 10.1111/j.1469-7610.2011.02371.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the Strengths and Difficulties Questionnaire (SDQ) Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed parents: a developmental approach to the understanding of mechanisms. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnomal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress generation in depression : reflections on origins, research, and future directions. Journal of Clinical Psychology. 2006;62:1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- Hammen C, Ellicott A, Gitlin M, Jamison KR. Sociotropy/autonomy and vulnerability to specific life events in patients with unipolar depression and bipolar disorders. Journal of Abnormal Psychology. 1989;98:154–160. doi: 10.1037//0021-843x.98.2.154. [DOI] [PubMed] [Google Scholar]
- Hammen C, Gordon D, Burge D, Adrian C, Jaenicke C, Hiroto D. Maternal affective disorders, illness, and stress: risk for children’s psychopathology. American Journal of Psychiatry. 1987;144:736–741. doi: 10.1176/ajp.144.6.736. [DOI] [PubMed] [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72:511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Holden GW. Children exposed to domestic violence and child abuse: terminology and taxonomy. Clinical Child and Family Psychology Review. 2003;6:151–160. doi: 10.1023/a:1024906315255. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO. Dependent stressful life events and prior depressive episodes in the prediction of major depression: the problem of causal inference in psychiatric epidemiology. Archives of General Psychiatry. 2010;67:1120–1127. doi: 10.1001/archgenpsychiatry.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gatz M, Gardner CO, Pedersen NL. A Swedish national twin study of lifetime major depression. American Journal of Psychiatry. 2006;163:109–114. doi: 10.1176/appi.ajp.163.1.109. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Epidemiology of women and depression. Journal of Affective Disorders. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Aguilar-Gaxiola S, Alhamzawi AO, Alonso J, Angermeyer M, Benjet C, Bromet E, Chatterji S, de Girolamo G, Demyttenaere K, Fayyad J, Florescu S, Gal G, Gureje O, Haro JM, Hu C-Y, Karam EG, Kawakami N, Lee S, Lépine J-P, Ormel J, Posada-Villa J, Sagar R, Tsang A, Üstün TB, Vassilev S, Viana MC, Williams DR. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. British Journal of Psychiatry. 2010;197:378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohen DE, Leventhal T, Dahinten SV, McIntosh CN. Neighborhood disadvantage: pathways of effects for young children. Child Development. 2008;79:156–169. doi: 10.1111/j.1467-8624.2007.01117.x. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Fok AK, Walker H, Lim A, Nicholls EF, Cole S, Kobor MS. Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proceedings of the National Academy of Sciences USA. 2009;106:14716–14721. doi: 10.1073/pnas.0902971106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, Carothers A. The validation of the Edinburgh Post-natal Depression Scale on a community sample. British Journal of Psychiatry. 1990;157:288–290. doi: 10.1192/bjp.157.2.288. [DOI] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of Quantitative Methodology for the Social Sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Muthén LK, Muthén BO. Mplus. Statistical Analyses with Latent Variables. User’s Guide. Los Angeles, CA: Mutheén & Mutheén; 1998–2010. [Google Scholar]
- Nagin DS. Group-Based Modeling of Development Over the Life Course. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Oberlander TF, Weinberg J, Papsdorf M, Grunau R, Misri S, Devlin AM. Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics. 2008;3:97–106. doi: 10.4161/epi.3.2.6034. [DOI] [PubMed] [Google Scholar]
- OPCS. Standard Occupational Classification. Volume 3. London: Office of Population Census and Surveys. HMSO; 1991. [Google Scholar]
- Parry G. Paid employment, life events, social support, and mental health in working-class mothers. Journal of Health and Social behavior. 1986;27:193–208. [PubMed] [Google Scholar]
- Pawlby S, Hay D, Sharp D, Waters CS, Pariante CM. Antenatal depression and offspring psychopathology: the influence of childhood maltreatment. British Journal of Psychiatry. 2011;199:106–112. doi: 10.1192/bjp.bp.110.087734. [DOI] [PubMed] [Google Scholar]
- Rutter M, Quinton D. Parental psychiatric disorder : effects on children. Psychological Medicine. 1984;14:853–880. doi: 10.1017/s0033291700019838. [DOI] [PubMed] [Google Scholar]
- Satorra A. Scaled and adjusted restricted tests in multi-sample analysis of moment structures. In: Heijmans RDH, Pollock DSG, Satorra A, editors. Innovations in Multivariate Statistical Analysis. London: Kluwer Academic Publishers; 2000. pp. 233–247. [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. Journal of the American Medical Association. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. Boston, MA: Allyn & Bacon; 2001. [Google Scholar]
- Weinstock M. The long-term behavioural consequences of prenatal stress. Neuroscience and Biobehavioral Reviews. 2008;32:1073–1086. doi: 10.1016/j.neubiorev.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Hughes CW, Garber J, Malloy E, King CA, Cerda G, Sood AB, Alpert JE, Trivedi MH, Rush AJ STAR*D-Child Team. Remissions in maternal depression and child. Journal of the American Medical Association. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]