Abstract
Objective
To assess the independent impact of waist circumference on mortality across the entire range of body mass index (BMI), and to estimate the loss in life expectancy related to a higher waist circumference.
Methods
We pooled data from 11 prospective cohort studies with 650,386 white adults aged 20–83 years and enrolled from January 1, 1986 through December 31, 2000. We used proportional hazards regression to estimate hazard ratios (HR) and 95% confidence intervals (95%CI) for the association of waist circumference with mortality.
Results
During a median follow-up of 9 years (maximum=21 years), 78,268 participants died. After accounting for age, study, BMI, smoking status, alcohol consumption, and physical activity, there was a strong positive linear association of waist circumference with all-cause mortality was observed for men (HR=1.52 for 110+ versus <90cm, 95%CI, 1.45–1.59; HR=1.07 per 5cm increment, 95%CI, 1.06–1.08) and women (HR=1.80 for 95+ versus <70cm, 95%CI, 1.70–1.89; HR=1.09 per 5cm increment, 95%CI, 1.08–1.09). The estimated decrease in life expectancy for highest versus lowest waist circumference was ~3 years for men and ~5 years for women. The HR per 5cm increment in waist circumference was similar for both sexes at all BMI levels from 20–50 kg/m2, but it was higher at younger ages, higher for longer follow-up, and lower among male current smokers. The associations were stronger for heart and respiratory disease mortality than for cancer.
Conclusions
In white adults, higher waist circumference was positively associated with higher mortality at all levels of BMI from 20–50 kg/m2. Waist circumference should be assessed in combination with BMI, even for those in the normal BMI range, as part of risk assessment for obesity-related premature mortality.
Increasing obesity, including central obesity, poses a major clinical and public health challenge due to elevated disease risks and premature mortality. Obesity is most commonly measured using body mass index (BMI), defined as weight in kilograms divided by the square of height in meters. Obese individuals (≥30.0 kg/m2) have higher all-cause mortality than persons with normal BMI (18.5–24.9 kg/m2).1–6 However, in studies observing this association, lower BMI is also associated with higher mortality, resulting in a J or U-shaped risk curve. The shape of the BMI and mortality curve is explained in part by confounding due to tobacco use, pre-existing illness, recent weight loss or short duration of follow-up.5 In addition, there are important limitations in using BMI as a measure of obesity because BMI does not discriminate fat from lean mass or abdominal from gluteofemoral fat, both of which have different health implications.7 This partly explains the imperfect diagnostic accuracy of BMI in identifying individuals with excess body fat, particularly in the BMI range of 25–29.9 kg/m2 and among men and the elderly.8
Waist circumference strongly correlates with abdominal obesity and is the most commonly used clinical measure of body fat distribution.7,9 Waist circumference has been positively associated with all-cause mortality in most studies3,10–17 with only a few exceptions.18,19 Abdominal obesity appears to be more strongly associated with multiple chronic diseases than is gluteofemoral obesity, likely through adverse metabolic effects (e.g., decreased glucose tolerance, reduced insulin sensitivity, and adverse lipid profiles) of visceral relative to subcutaneous fat.7,9,20
The US Preventive Services Task Force21 recommends screening for obesity based on a BMI of ≥30 kg/m2, while the US National Institutes of Health22 recommends only measuring waist circumference in people whose BMI is in the overweight (25.0–29.9 kg/m2) or class I obesity range (30.0–34.9 kg/m2), using clinically-defined cut-points of 102cm for men and 88cm for women to define elevated risk. However, measurement of waist circumference is not recommended for underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), or for grades II-III obesity (≥35.0 kg/m2), although it has been noted that increased waist circumference may be a risk marker in persons of normal weight.22 Because of the high correlation between BMI and waist circumference, it has been difficult for even the largest studies3,16,17 to model the impact of waist circumference on mortality across all categories of BMI, and even those that have done this, the groupings of BMI were quite large. Given the established clinical utility of BMI, it is particularly important to fully understand the magnitude of risk of waist circumference within clinically meaningful categories of BMI.
To overcome these limitations, we examined the association of waist circumference with all-cause mortality in a pooled analysis of 650,000 participants from 11 prospective cohort studies. These pooled analyses included 78,000 deaths, which is five times larger than any individual study published to date.3,16,17 This large sample size allowed us to (1) systematically model the association of waist circumference with mortality using clinically intuitive 5cm (~2 inch) increments for men and women, and (2) evaluate risk within relatively narrow bands of BMI to assess the validity of guidelines that use a single clinical cut-point for waist circumference and do not recommend monitoring waist circumference in underweight, normal, or extremely obese men and women.22 We also estimated for the first time the potential years of life lost due to a large waist circumference.
METHODS
Study Cohorts
Prospective cohort studies from the BMI and mortality pooling project 5 were eligible for this analysis. All individual studies were approved by an institutional review board and participants provided informed consent. We excluded studies that did not collect waist circumference within 3 years of ascertaining baseline weight; all10,11,14,17,23–26 but three16,27,28 studies collected waist circumference at the same time as weight. Waist circumference was measured by a technician in one study,14 while in the remaining studies it was reported by participants using measurement instructions and a paper tape provided by the study. The self-reported waist circumference data were found to be valid and reliable in several studies that formally assessed it.28–30 All variables were harmonized across cohort studies as previously described.5
Participants were followed from study baseline (the year in which waist circumference was reported) to date of death, end of follow-up, or loss to follow-up. Cause of death was coded according to the International Classification of Diseases (9th or 10th revisions).
Statistical Analysis
We restricted the analysis to non-Hispanic white participants (based on self-report of race/ ethnicity) and ages 20 to 84 years at baseline. We further excluded participants with a BMI of <15.0 kg/m2 or ≥50.0 kg/m2 and a waist circumference of ≤51cm or ≥190cm.
Waist circumference was categorized into six levels for men and seven levels for women, using sex-specific 5cm increments, with the lowest level of waist circumference as the reference group. Hazard ratios (HRs) and 95% confidence intervals (CIs) for all-cause and cause-specific mortality, stratified on study, were estimated by fitting Cox proportional hazards models with age as the underlying time metric. We adjusted for education, marital status, smoking status, alcohol consumption, physical activity and BMI (categories in eTable 1). We did not adjust for diabetes, prevalent heart disease, or hypertension to avoid bias introduced when adjusting for variables known to be on the causal pathway between abdominal obesity and mortality.31 All analyses used sex-specific cutpoints and most results were presented separately for men and women, although we combined them for some analyses, with the highest two levels of waist circumference collapsed for women. We also modeled waist circumference as a continuous variable, reporting risk based on 5cm increments. We assessed heterogeneity between cohorts using the I2 statistic.32
Years of life expectancy lost were derived using direct adjusted survival curves,33 which is a simple extension of the proportional hazards framework (like that of a Kaplan-Meier curve) except that the survival curve uses age as the underlying time metric and adjusts for covariate differences. This method uses proportional hazards models to calculate survival curves for each individual and then averages them to obtain the survival curve for all men and for all women. Curves for each level of waist circumference were estimated by counterfactual; i.e., by applying the hazard coefficient for the waist circumference category to the sex-specific study population. This estimates survival as if assigning all participants within each sex alternately to one level of waist circumference or another. Life expectancy was estimated as the age at which 50% of the population would have been expected to have died according to the adjusted survival curve. The years of life gained/lost were calculated as the difference between the life expectancy for the group with a given waist circumference and that of the sex-specific reference group. Life expectancy analyses were restricted to participants whose ages were 40 or more years. All analyses were performed using SAS version 9.0 (SAS Institute).
RESULTS
Characteristics of Cohorts
We included 650,386 participants from 11 cohorts, with baseline years ranging from January 1, 1986 through December 31, 2000 (Table 1). The median age at baseline was 62 years; 58% of participants were female, and 52% were ever smokers. The mean BMI was 26.5±3.8 kg/m2 for men and 25.3±4.7 kg/m2 for women; the mean waist circumference was 97.4±10.5cm for men 81.5±13.1cm for women. For men, waist circumference was positively associated with BMI and former smoking status and negatively with physical activity, while it was only weakly associated with education and was not appreciably associated with prevalent disease, marital status or alcohol consumption (eTable 1). For women, waist circumference was associated with higher BMI and prevalent disease, while it was only weakly associated with smoking status, marital status, alcohol consumption and physical activity and was not appreciably associated with education. Waist circumference was correlated (Pearson r) with BMI for both men (r=0.77) and women (r=0.72).
TABLE 1.
Cohort Characteristics for the Pooled Analysis of Waist Circumference and Mortality
| Study | Sex | N | Year study entry |
Follow-up (years) Median (max) |
Age at entry (yrs) Median (range) |
BMI, kg/m2 Mean (SD) |
Waist, cm Mean (SD) |
Ever Smoker |
Baseline CA or CVDa |
Deaths |
|---|---|---|---|---|---|---|---|---|---|---|
| NIH-AARP Diet and Health Study (AARP) 16 | Combined | 217428 | 1996–1997 | 9 (10) | 63 (51–72) | 21413 | ||||
| Women | 83066 | 25.8 (5.0) | 85 (13) | 53% | 13% | 6085 | ||||
| Men | 134362 | 26.9 (3.9) | 98 (11) | 66% | 21% | 15328 | ||||
| BCDDPb Follow-up Study (BCDDP) 23 | Women | 25950 | 1993–1995 | 3 (5) | 66 (46–83) | 25.4 (4.6) | 82 (12) | 45% | 26% | 3849 |
| California Teachers Study (CTS) 28 | Women | 71374 | 1997–2000 | 7 (8) | 55 (25–83) | 24.4 (4.6) | 82 (13) | 34% | 26% | 2524 |
| Cohort of Swedish Men (COSM) 25 | Men | 34098 | 1998 | 9 (9) | 60 (46–80) | 25.7 (3.3) | 96 (10) | 62% | 38% | 4298 |
| Cancer Prevention Study-II (CPS-II) 17 | Combined | 120407 | 1997–1999 | 10 (11) | 68 (45–83) | 20561 | ||||
| Women | 64941 | 25.7 (4.8) | 86 (13) | 44% | 23% | 8125 | ||||
| Men | 55466 | 26.5 (3.7) | 99 (10) | 66% | 36% | 12436 | ||||
| Health Professionals Follow-up Study (HPFS) 11 | Men | 29688 | 1987 | 16 (21) | 56 (40–78) | 25.3 (3.0) | 95 (9) | 53% | 34% | 6460 |
| Iowa Women's Health Study (IWHS) 10 | Women | 37937 | 1986 | 18 (19) | 62 (53–71) | 26.1 (4.8) | 69 (11) | 34% | 17% | 10545 |
| Melbourne Collaborative Cohort Study (MCCS) 14 | Combined | 41323 | 1990–1994 | 15 (19) | 56 (28–81) | 4763 | ||||
| Women | 24374 | 26.7 (4.9) | 80 (12) | 31% | 8% | 2087 | ||||
| Men | 16949 | 27.2 (3.6) | 94 (10) | 59% | 8% | 2676 | ||||
| NYU Women's Health Study (NYUWHS) 27 | Women | 7279 | 1986–1991 | 17 (19) | 54 (34–73) | 24.5 (4.3) | 74 (12) | 55% | 8% | 715 |
| Swedish Mammography Cohort (SMC) 24 | Women | 29955 | 1998 | 9 (9) | 61 (49–83) | 25.0 (3.9) | 84 (11) | 45% | 34% | 2342 |
| Women's Lifestyle and Health Study (WLHS) 26 | Women | 34947 | 1991–1992 | 16 (16) | 40 (30–50) | 23.4 (3.5) | 77 (9) | 57% | 10% | 798 |
| Summary | Combined | 650386 | 1986–2000 | 9 (21) | 62 (25–83) | 78268 | ||||
| Women | 379823 | 1986–2000 | 9 (19) | 61 (25–83) | 25.3 (4.7) | 81.5 (13.1) | 44% | 19% | 37070 | |
| Men | 270563 | 1987–1999 | 9 (21) | 64 (28–83) | 26.5 (3.8) | 97.4 (10.5) | 64% | 27% | 41198 |
Prevalent cancer (CA) or cardiovascular disease (CVD) at study baseline.
Breast Cancer Detection Demonstration Project.
Association with All-Cause Mortality
During 6.2 million person-years of follow-up (median=9, maximum=21 years), 78,268 deaths occurred (including 28,917 cancer, 24,411 CVD, and 6,202 respiratory disease deaths). Waist circumference was strongly and positively associated with all-cause mortality for both men and women in unadjusted models, and these associations were only slightly attenuated after adjustment for marital status, education, smoking status, alcohol consumption, and physical activity (Table 2). Further adjustment for height did not alter these associations (data not shown), while further adjustment for BMI led to a stronger and more linear association of the HR for waist circumference with mortality for both men and women (Table 2). Men with a waist circumference of 110+ cm had 52% greater mortality risk compared with those <90cm (HR=1.52; 95% CI, 1.45–1.59); women with a waist circumference ≥95cm had 80% greater mortality risk compared with those <70cm (HR, 1.80; 95% CI, 1.70–1.89). Each 5cm increment in waist circumference was associated with a 7% increased mortality risk for men (HR, 1.07; 95% CI, 1.06–1.08) and a 9% increased mortality risk for women (HR, 1.09; 95% CI, 1.08–1.09). The association of waist circumference with mortality was broadly similar with or without BMI adjustment for men at BMI <25 and 25–49.9 kg/m2, while for women, BMI appeared to be a confounder for both BMI <25.0 kg/m2 and 25–49.9 kg/m2 (eFigure 1).
TABLE 2.
Association of Waist Circumference with All-Cause Mortality, Pooled Analysis of 11 Cohort Studies
| Category of Waist Circumference |
||||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | P-trend | |
| Men | ||||||||
| Cutpoint (cm) | <90.0 | 90.0–94.9 | 95.0–99.9 | 100.0–104.9 | 105.0–109.9 | 110.0+ | ||
| Median of group (cm) | 86.4 | 92.0 | 96.5 | 101.6 | 106.7 | 115.0 | ||
| N | 61,442 | 57,867 | 53,780 | 39,134 | 27,308 | 31,032 | ||
| Deaths | 7939 | 7977 | 7806 | 6291 | 4834 | 6351 | ||
| Person-years | 618,574 | 567,777 | 519,551 | 369,595 | 252,139 | 279,799 | ||
| Ratea | 474 | 450 | 468 | 543 | 615 | 767 | ||
| Hazard Ratio (95% CI) | ||||||||
| Basic modelb | 1 (reference) | 0.98 (0.95, 1.01) | 0.99 (0.96, 1.02) | 1.10 (1.06, 1.13) | 1.22 (1.18, 1.27) | 1.56 (1.51, 1.61) | <0.0001 | |
| Multivariate-adjustedc | 1 (reference) | 0.97 (0.94, 1.01) | 0.98 (0.95, 1.01) | 1.05 (1.01, 1.08) | 1.13 (1.09, 1.17) | 1.37 (1.32, 1.42) | <0.0001 | |
| Further adjusted for BMId | 1 (reference) | 1.04 (1.01, 1.08) | 1.08 (1.05, 1.12) | 1.19 (1.15, 1.24) | 1.30 (1.24, 1.35) | 1.52 (1.45, 1.59) | <0.0001 | |
| Life expectancy | 85.5 | 85.2 | 85.0 | 84.0 | 83.5 | 82.4 | ||
| Years of life lost | 0 | 0.3 | 0.5 | 1.5 | 2.0 | 3.1 | ||
| Women | ||||||||
| Cutpoint (cm) | <70.0 | 70.0–74.9 | 75.0–79.9 | 80.0–84.9 | 85.0–89.9 | 90.0–94.9 | 95.0+ | |
| Median of group (cm) | 66.0 | 72.4 | 77.0 | 81.9 | 86.4 | 91.4 | 101.6 | |
| N | 67,862 | 62,287 | 57,755 | 56,353 | 44,452 | 32,878 | 58,236 | |
| Deaths | 7918 | 4940 | 4821 | 4984 | 4140 | 3322 | 6945 | |
| Person-years | 795,238 | 637,511 | 573,935 | 530,947 | 403,653 | 291,844 | 502,015 | |
| Ratea | 362 | 345 | 348 | 345 | 348 | 388 | 455 | |
| Hazard Ratio (95% CI) | ||||||||
| Basic modelb | 1 (reference) | 1.07 (1.03, 1.11) | 1.12 (1.08, 1.17) | 1.15 (1.11, 1.20) | 1.19 (1.14, 1.24) | 1.27 (1.21, 1.33) | 1.62 (1.56, 1.69) | <0.0001 |
| Multivariate-adjustedc | 1 (reference) | 1.07 (1.03, 1.11) | 1.12 (1.08, 1.16) | 1.13 (1.09, 1.18) | 1.15 (1.10, 1.20) | 1.21 (1.16, 1.27) | 1.49 (1.43, 1.55) | <0.0001 |
| Further adjusted for BMId | 1 (reference) | 1.17 (1.13, 1.22) | 1.28 (1.23, 1.33) | 1.34 (1.29, 1.40) | 1.40 (1.34, 1.47) | 1.50 (1.42, 1.58) | 1.79 (1.70, 1.89) | <0.0001 |
| Life expectancy | 90.5 | 89.5 | 88.5 | 88.2 | 87.8 | 87.5 | 85.5 | |
| Years of life lost | 0 | 1.0 | 2.0 | 2.3 | 2.7 | 3.0 | 5.0 | |
Rate per 100,000 person-years, standardized to age distribution of men or women in the dataset.
Hazard ratios were calculated with age as the underlying time scale and stratified by study.
Further adjusted for education, marital status, smoking status, alcohol consumption, and physical activity
Further adjusted for BMI (categorical)
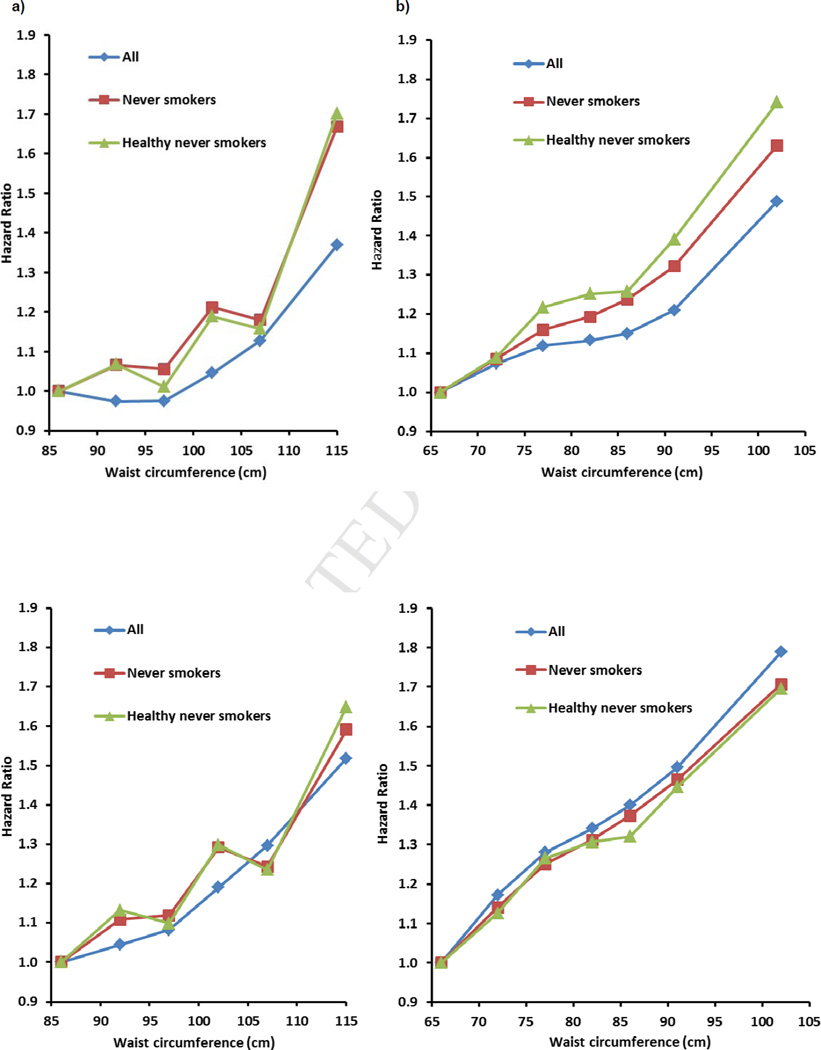
Our earlier pooled analysis of BMI and mortality5 was restricted to never smokers and participants with no history of cancer or heart disease at each study’s baseline to eliminate confounding by these factors. In this analysis, restriction on these factors had a relatively minor impact on the observed associations of waist circumference with mortality, particularly after adjustment for BMI (Figure 1). Based on these results, we elected to use all participants and to adjust for BMI in subsequent analyses.
Figure 1.
Hazard Ratios for Waist Circumference and All-Cause Mortality: a) Men and b) Women, Adjusted for Education, Marital Status, Smoking Status, Alcohol Consumption and Physical Activity; c) Men and d) Women, Further Adjusted for BMI.
Premature Mortality
eFigure 2 shows the expected loss in life expectancy, assuming a causal relation, for each level of waist circumference for men and women separately. For the highest level of waist circumference relative to the lowest level, the estimated decrease in life expectancy was ~3 years for men and ~5 years for women (Table 2).
Subgroup Analyses
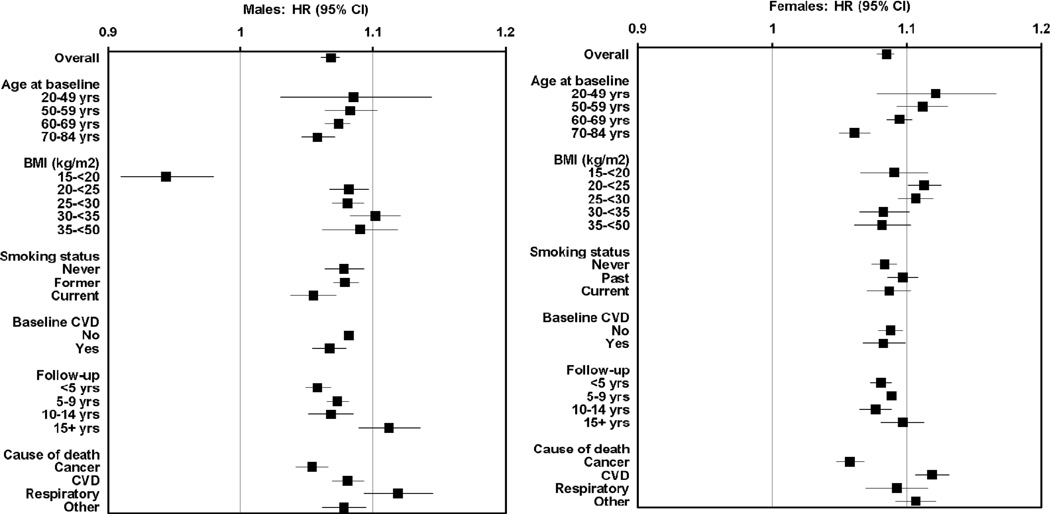
To increase statistical power, we modeled waist circumference on a continuous scale using 5cm increments. While statistically significant heterogeneity in HRs was observed for individual studies, all estimates were qualitatively consistent in terms of effect size (eFigure 3). Statistically significant heterogeneity in several key subgroups defined on baseline age, smoking status, baseline CVD, and length of follow-up was also observed (Figure 2 and eTable 2), although overall estimates were qualitatively similar. While the association of waist circumference with all-cause mortality for both sexes was strongest for ages 20–49 and 50–59 years at baseline, even among men and women ages 70–84 years the HRs were elevated. HRs were similar by baseline CVD status for both sexes and by smoking status for women, but for men they were slightly weaker for current smokers. HRs were similar at <5, 5–9 and 10–14 years of follow-up, while the HRs were greater at 15+ years, particularly for men. For analyses stratified on baseline BMI, the HRs were of similar magnitude, with the exception of BMI <20 kg/m2 for men, where the HR was below 1. The waist circumference association was strongest for deaths due to respiratory diseases in men and CVD for women, while deaths due to cancer showed the weakest (but still evident) associations for both sexes.
Figure 2.
Hazard Ratios (HR) and 95% Confidence Intervals (CI) for Waist Circumference (per 5cm) and All-Cause Mortality, by Sex for Selected Subgroups.
Hazard ratios were calculated with age as the underlying time scale and stratified by study, and were adjusted for education, marital status, smoking, alcohol, physical activity and BMI
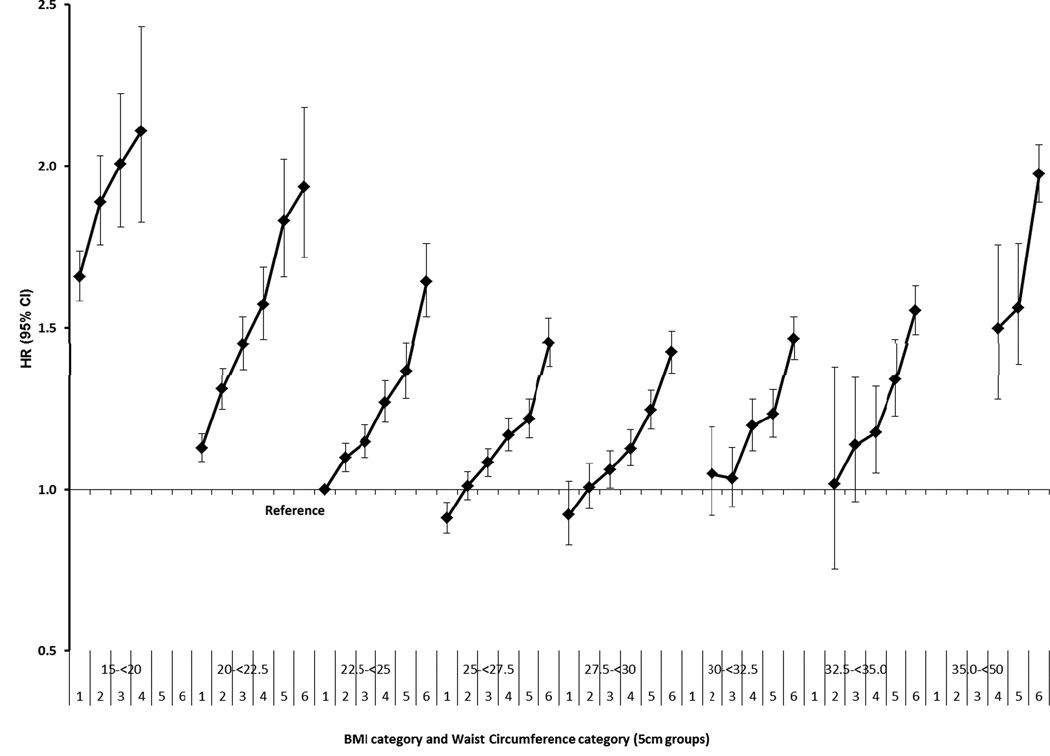
Joint Analysis
We next assessed the joint association of waist circumference and BMI with mortality for both sexes combined (Figure 3). Using the lowest category of waist circumference (<90cm for men and <70cm for women) and a BMI of 22.5–24.9 kg/m2 as the reference group, we observed a strong, generally linear association of waist circumference with mortality within each category of BMI (note that Figure 3 excludes point estimates based on <100 deaths; complete data available in eTable 3). The highest HRs for waist circumference were observed at the extremes of BMI (<20 and 35.0+ kg/m2), but clear increases in mortality risk were also observed for the normal BMI range (20.0–24.9 kg/m2) and for overweight groups (25.0–27.4 and 27.5–29.9 kg/m2). Results based on the NIH guideline cutpoints22 (eTable 4) does not capture the graded risk that we identified in Figure 3.
Figure 3.
Hazard Ratios (HR) and 95% Confidence Intervals (CI) for Waist Circumference in 5cm Increments* and All-Cause Mortality by Body Mass Index (BMI) Category (Men and Women Combined), Adjusted for Education, Marital Status, Smoking Status, Alcohol Consumption, Physical Activity and BMI.
*Waist circumference cutpoints (cm) for men <90.0, 90.0–94.9, 95.0–99.9, 100.0–104.9, 105.0–109.9, 110.0+ and women <70.0, 70.0–74.9, 75.0–79.9, 80.0–84.9, 85.0–89.9, 90.0+.
Results were similar in sex-specific analyses (eFigure 4). With respect to cause of death, a similar pattern of increased risk of death with increasing waist circumference was observed within each category of BMI, with greater risks for CVD and respiratory disease mortality relative to cancer mortality (eFigure 5).
Discussion
In this pooled analysis of 11 cohort studies with over 650,000 participants we found a strong positive association of waist circumference in 5cm increments with total mortality after accounting for BMI, and this association was observed across a very wide range of BMI. This association remained after adjustment for a variety of demographic and lifestyle factors, physical activity and BMI, and held also for healthy never smokers. While broadly similar across almost all subgroups, the magnitude of risk was higher for younger ages and for longer lengths of follow-up, and was lower for current male smokers. Waist circumference was more strongly associated with CVD and respiratory disease mortality than cancer mortality.
Adjustment for BMI increased the linearity and strengthened the association of waist circumference with mortality, which has been reported previously.3,12,13,15,17 Adjustment for BMI may decrease confounding by pre-existing diseases, pathologic conditions, or general frailty, all of which are associated with low lean body mass.7 The analysis of the joint effect of waist circumference and BMI on mortality further supports the linear association for waist circumference after accounting for BMI. Indeed, the positive association of waist circumference with mortality was similar in magnitude across all categories of BMI from 20–50 kg/m2 for men and 15–50 kg/m2 for women. Finally, losses in life expectancy at age 40 were ~3 years for men and ~5 years for women when comparing those in the highest versus lowest waist circumference groups.
This study has several key strengths, including the largest sample size reported to date for assessing the association of waist circumference with mortality. This allowed us to estimate with high precision the association of waist circumference with mortality within narrow categories of BMI covering the entire range of BMI from 15–50 kg/m2. We used standardized cutpoints and adjustment factors, and assessed the consistency across a wide range of study populations. We also assessed the impact of confounding by smoking and prevalent illness through stratification. Limitations include use of only a single measurement of waist circumference and BMI, and, except for one study,14 waist circumference and BMI were self-reported. Self-reported waist circumference has been shown to be reasonably strongly correlated with measured waist circumference (r=0.80).30,34 Typically it is under-reported by about 2–3cm but the degree of underreporting tends to increase with increasing circumference. These reporting errors likely resulted in under-estimation of the magnitude of the mortality risks in our study. While we were able to adjust for physical activity, we did not have an objective measure cardiorespiratory fitness, and therefore have incomplete adjustment for this potentially important confounder35; future studies should include such measures. Our results were restricted to white populations with a median age of 62 years at study baseline, and may not apply to the oldest old36 or other racial/ethnic groups. While many studies have found superior survival for CVD patients with a higher BMI,37 we observed similar associations for waist circumference and overall morality irrespective of baseline CVD, cautioning that our assessment was limited to self-report of any history of CVD.
Our pooled analysis of 11 studies had five times more deaths than any individual study published to date, which provided much greater precision and more importantly the ability to investigate the impact of waist circumference within narrow levels of BMI to assess independent effects. Our overall results are broadly consistent with those of other studies with more than 1000 deaths and not in this analysis.3,12,13,15 The EPIC cohort3 is the largest study not in this pooled analysis, with 359,387 participants and 14,723 deaths (versus 78,268 here); in EPIC, each 5cm increase in waist circumference was associated with a 17% increased risk of death for men (95% CI, 1.15–1.20) and a 13% increased risk of death for women (95% CI, 1.11–1.15). Our summary estimates were slightly lower, consistent with the older population of this study and the weaker association with increasing age.38 Within EPIC the cross-classification of waist circumference by BMI was limited to 3 broad levels of BMI compared to 8 in our pooled analysis. This fine stratification enabled us to reduce the impact of residual variation in BMI on the waist circumference results and to examine the relationship of waist circumference in the severely obese (BMI >35 kg/m2 (Figure 3)), for which EPIC had limited data. In a pooled analysis of 203,338 persons from 58 studies (1 from this analysis11), higher waist circumference was associated with higher coronary heart disease risk (7,750 cases) for each category of BMI divided into thirds.39 In a meta-analysis of 58,609 people from 29 studies (3 from this analysis14,24,25), increased mortality risk (4,798 deaths) with higher waist circumference was observed in both healthy weight and overweight persons aged 65–74 years. These results are also broadly consistent with our findings. None of these previous studies estimated the reduction in life-expectancy associated with central adiposity.
Our results strongly suggest that BMI and waist circumference jointly serve as important predictors of mortality in the general population, so that clinically it may not be useful to try to select one measure over the other.9,40 This also accords with recent work demonstrating that both measures have a complex association with metabolic syndrome risk factors.41 There is also emerging evidence that modest exercise and a healthy diet are associated with reductions in metabolic risk profile, morbidity and mortality irrespective of weight status or weight change.42 A majority of randomized trials have found that increased physical activity is associated with significant reductions in waist circumference or visceral fat despite either no change in weight or a change of <3%.42 Thus, management of excess waist circumference would be predicted to lower mortality across most BMI categories. Our results also suggest that current recommendations22 regarding waist circumference, which are predicated on using a single sex-specific cutpoint and evaluation only in the BMI range of 25–34.9 kg/m2, should be broadened as part of risk assessment for premature mortality. Our large sample size enabled us to detect a graded, linear increase in mortality risk across the full range of BMI including those within the normal and underweight category. The continuous association we observed makes it more difficult to define clinical cut-points for waist circumference, and suggests the importance of measuring waist circumference in more patients and implementing interventions to reduce larger circumferences (even among those with normal BMIs) and monitor trends to prevent increases over time.
Conclusion
In white adults, higher waist circumference was positively associated with higher mortality at all levels of BMI from 20–50 kg/m2. Waist circumference should be assessed in combination with BMI, even for those in the normal BMI range, as part of risk assessment for obesity-related premature mortality.
Supplementary Material
Acknowledgment
Grant Support: The NIH-AARP Diet and Health study was supported by the Intramural Research Program of the National Cancer Institute, National Institutes of Health. The BCDDP Follow-up Study has been supported by the Intramural Research Program of the National Cancer Institute, National Institutes of Health. The CTS was supported by National Cancer Institute grant CA77398 and contract 97-10500 from the California Breast Cancer Research Fund. The Cancer Prevention Study II was supported by the American Cancer Society. The Cohort of Swedish Men was supported by the Swedish Research Council, the Swedish Council for Working Life and Social Research and the Swedish Cancer Society. The Health Professionals Follow-up Study is supported by National Cancer Institute grant P01 CA055075. The Iowa Women's Health Study is supported by the National Cancer Institute grant R01 CA39742. The Melbourne Collaborative Cohort Study receives core funding from The Cancer Council Victoria and is additionally supported by grants from the Australian NHMRC (209057, 251533, and 396414). The NYU Women’s Health Study is supported by National Cancer Institute grants R01 CA098661 and P30 CA016087 and by Center grant ES000260 from the National Institute of Environmental Health Sciences. The Swedish Mammography Cohort was supported by the Swedish Research Council, Swedish Council for Working Life and Social Research and the Swedish Cancer Society. The Women’s Lifestyle and Health project was supported by the Swedish Cancer Society and the Swedish Research Council.
We thank Sondra Buehler for editorial assistance.
Abbreviations and Acronyms
- BMI
body mass index
- HR
hazard ratio
- CI
confidence interval
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures: None reported.
REFERENCES
- 1.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298(17):2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 3.Pischon T, Boeing H, Hoffmann K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359(20):2105–2120. doi: 10.1056/NEJMoa0801891. [DOI] [PubMed] [Google Scholar]
- 4.Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orpana HM, Berthelot JM, Kaplan MS, Feeny DH, McFarland B, Ross NA. BMI and mortality: results from a national longitudinal study of Canadian adults. Obesity (Silver Spring) 2010;18(1):214–218. doi: 10.1038/oby.2009.191. [DOI] [PubMed] [Google Scholar]
- 7.Snijder MB, van Dam RM, Visser M, Seidell JC. What aspects of body fat are particularly hazardous and how do we measure them? Int J Epidemiol. 2006;35(1):83–92. doi: 10.1093/ije/dyi253. [DOI] [PubMed] [Google Scholar]
- 8.Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes. 2008;32(6):959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr. 2002;75(4):683–688. doi: 10.1093/ajcn/75.4.683. [DOI] [PubMed] [Google Scholar]
- 10.Folsom AR, Kushi LH, Anderson KE, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women's Health Study. Arch Intern Med. 2000;160(14):2117–2128. doi: 10.1001/archinte.160.14.2117. [DOI] [PubMed] [Google Scholar]
- 11.Baik I, Ascherio A, Rimm EB, et al. Adiposity and mortality in men. Am J Epidemiol. 2000;152(3):264–271. doi: 10.1093/aje/152.3.264. [DOI] [PubMed] [Google Scholar]
- 12.Bigaard J, Tjonneland A, Thomsen BL, Overvad K, Heitmann BL, Sorensen TI. Waist circumference, BMI, smoking, and mortality in middle-aged men and women. Obes Res. 2003;11(7):895–903. doi: 10.1038/oby.2003.123. [DOI] [PubMed] [Google Scholar]
- 13.Janssen I, Katzmarzyk PT, Ross R. Body mass index is inversely related to mortality in older people after adjustment for waist circumference. J Am Geriatr Soc. 2005;53(12):2112–2118. doi: 10.1111/j.1532-5415.2005.00505.x. [DOI] [PubMed] [Google Scholar]
- 14.Simpson JA, MacInnis RJ, Peeters A, Hopper JL, Giles GG, English DR. A comparison of adiposity measures as predictors of all-cause mortality: the Melbourne Collaborative Cohort Study. Obesity (Silver Spring) 2007;15(4):994–1003. doi: 10.1038/oby.2007.622. [DOI] [PubMed] [Google Scholar]
- 15.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117(13):1658–1667. doi: 10.1161/CIRCULATIONAHA.107.739714. [DOI] [PubMed] [Google Scholar]
- 16.Koster A, Leitzmann MF, Schatzkin A, et al. Waist circumference and mortality. Am J Epidemiol. 2008;167(12):1465–1475. doi: 10.1093/aje/kwn079. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs EJ, Newton CC, Wang Y, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170(15):1293–1301. doi: 10.1001/archinternmed.2010.201. [DOI] [PubMed] [Google Scholar]
- 18.Price GM, Uauy R, Breeze E, Bulpitt CJ, Fletcher AE. Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death. Am J Clin Nutr. 2006;84(2):449–460. doi: 10.1093/ajcn/84.1.449. [DOI] [PubMed] [Google Scholar]
- 19.Walter S, Kunst A, Mackenbach J, Hofman A, Tiemeier H. Mortality and disability: the effect of overweight and obesity. Int J Obes. 2009;33(12):1410–1418. doi: 10.1038/ijo.2009.176. [DOI] [PubMed] [Google Scholar]
- 20.Despres JP, Lemieux I, Bergeron J, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vac Biol. 2008;28(6):1039–1049. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]
- 21.Moyer VA. Screening for and Management of Obesity in Adults: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2012;157(5):1–6. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- 22.National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 23.Moore SC, Mayne ST, Graubard BI, et al. Past body mass index and risk of mortality among women. Int J Obes. 2008;32(5):730–739. doi: 10.1038/sj.ijo.0803801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolk A, Larsson SC, Johansson JE, Ekman P. Long-term fatty fish consumption and renal cell carcinoma incidence in women. JAMA. 2006;296(11):1371–1376. doi: 10.1001/jama.296.11.1371. [DOI] [PubMed] [Google Scholar]
- 25.Orsini N, Bellocco R, Bottai M, Pagano M, Michaelsson K, Wolk A. Combined effects of obesity and physical activity in predicting mortality among men. J Intern Med. 2008;264(5):442–451. doi: 10.1111/j.1365-2796.2008.01985.x. [DOI] [PubMed] [Google Scholar]
- 26.Lu M, Ye W, Adami HO, Weiderpass E. Prospective study of body size and risk for stroke amongst women below age 60. J Intern Med. 2006;260(5):442–450. doi: 10.1111/j.1365-2796.2006.01706.x. [DOI] [PubMed] [Google Scholar]
- 27.Toniolo PG, Levitz M, Zeleniuch-Jacquotte A, et al. A prospective study of endogenous estrogens and breast cancer in postmenopausal women. J Natl Cancer Inst. 1995;87(3):190–197. doi: 10.1093/jnci/87.3.190. [DOI] [PubMed] [Google Scholar]
- 28.Canchola AJ, Anton-Culver H, Bernstein L, et al. Body size and the risk of postmenopausal breast cancer subtypes in the California Teachers Study cohort. Cancer Causes Control. 2012;23(3):473–485. doi: 10.1007/s10552-012-9897-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kushi LH, Kaye SA, Folsom AR, Soler JT, Prineas RJ. Accuracy and reliability of self-measurement of body girths. Am J Epidemiol. 1988;128:740–748. doi: 10.1093/oxfordjournals.aje.a115027. [DOI] [PubMed] [Google Scholar]
- 30.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1(6):466–473. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Hu FB. Obesity and mortality. In: Hu FB, editor. Obesity Epidemiology. New York, NY: Oxford University Press; 2008. pp. 216–233. [Google Scholar]
- 32.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 33.Makuch RW. Adjusted survival curve estimation using covariates. J Chronic Dis. 1982;35(6):437–443. doi: 10.1016/0021-9681(82)90058-3. [DOI] [PubMed] [Google Scholar]
- 34.Spencer EA, Roddam AW, Key TJ. Accuracy of self-reported waist and hip measurements in 4492 EPIC-Oxford participants. Public Health Nutr. 2004;7(6):723–727. doi: 10.1079/phn2004600. [DOI] [PubMed] [Google Scholar]
- 35.McAuley PA, Blair SN. Obesity paradoxes. J Sports Sci. 2011;29(8):773–782. doi: 10.1080/02640414.2011.553965. [DOI] [PubMed] [Google Scholar]
- 36.Heim N, Snijder MB, Heymans MW, Deeg DJ, Seidell JC, Visser M. Optimal cutoff values for high-risk waist circumference in older adults based on related health outcomes. Am J Epidemiol. 2011;174(4):479–489. doi: 10.1093/aje/kwr093. [DOI] [PubMed] [Google Scholar]
- 37.De Schutter A, Lavie CJ, Patel DA, Milani RV. Obesity paradox and the heart: which indicator of obesity best describes this complex relationship? Curr Opin Clin Nutr Metab Care. 2013;16(5):517–524. doi: 10.1097/MCO.0b013e328363bcca. [DOI] [PubMed] [Google Scholar]
- 38.Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obes Rev. 2007;8(1):41–59. doi: 10.1111/j.1467-789X.2006.00248.x. [DOI] [PubMed] [Google Scholar]
- 39.Wormser D, Kaptoge S, Di Angelantonio E, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377(9771):1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flegal KM, Graubard BI. Estimates of excess deaths associated with body mass index and other anthropometric variables. Am J Clin Nutr. 2009;89(4):1213–1219. doi: 10.3945/ajcn.2008.26698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grundy SM, Adams-Huet B, Vega GL. Variable contributions of fat content and distribution to metabolic syndrome risk factors. Metab Syndr Relat Disord. 2008;6(4):281–288. doi: 10.1089/met.2008.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ross R, Bradshaw AJ. The future of obesity reduction: beyond weight loss. Nat Rev Endocrinol. 2009;5(6):319–325. doi: 10.1038/nrendo.2009.78. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.