Significance
Mast cells (MC) are long-lived cells that accumulate in inflamed tissues. IL-33 has been characterized extensively as a MC activator, but a contribution of IL-33 and its receptor IL-1 receptor-related protein ST2 to MC survival remains unappreciated. Here, we show that IL-33 attenuates apoptosis of human and murine MC, principally via the antiapoptotic molecule B-cell lymphoma-X large (BCLXL). In vivo, IL-33 and ST2 can confer a cell-intrinsic survival advantage to murine MC, particularly in the context of inflammation. These results identify the IL-33/ST2 axis as an important pathway supporting MC persistence in tissues, raising the possibility that therapeutic targeting of IL-33 could limit the contribution of MC to chronic inflammatory diseases.
Keywords: arthritis, helminth infection
Abstract
Mast cells (MC) are potent innate immune cells that accumulate in chronically inflamed tissues. MC express the IL-33 receptor IL-1 receptor-related protein ST2 at high level, and this IL-1 family cytokine both activates MC directly and primes them to respond to other proinflammatory signals. Whether IL-33 and ST2 play a role in MC survival remains to be defined. In skin-derived human MC, we found that IL-33 attenuated MC apoptosis without altering proliferation, an effect mediated principally through the antiapoptotic molecule B-cell lymphoma-X large (BCLXL). Murine MC demonstrated a similar mechanism, dependent entirely on ST2. In line with these observations, St2−/− mice exhibited reduced numbers of tissue MC in inflamed arthritic joints, in helminth-infected intestine, and in normal peritoneum. To confirm an MC-intrinsic role for ST2 in vivo, we performed peritoneal transfer of WT and St2−/− MC. In St2−/− hosts treated with IL-33 and in WT hosts subjected to thioglycollate peritonitis, WT MC displayed a clear survival advantage over coengrafted St2−/− MC. IL-33 blockade specifically attenuated this survival advantage, confirming IL-33 as the relevant ST2 ligand mediating MC survival in vivo. Together, these data reveal a cell-intrinsic role for the IL-33/ST2 axis in the regulation of apoptosis in MC, identifying thereby a previously unappreciated pathway supporting expansion of the MC population with inflammation.
Mast cells (MC) are tissue-resident effector cells that contribute both to innate and adaptive immunity (1). MC help defend against bacterial and helminthic infection (2, 3) and play a role in tissue remodeling (4, 5). MC can also contribute to a variety of allergic and nonallergic inflammatory diseases, such as anaphylaxis, atopic dermatitis, asthma, inflammatory arthritis, psoriasis, and multiple sclerosis (6, 7). Under many of these conditions, the number of MC in affected tissues increases by tenfold or more, amplifying the contribution of MC-derived mediators to ongoing inflammation (6–8). Regulation of the MC population is poorly understood, and therapeutic intervention to limit MC accumulation potentially could attenuate injury associated with inflammatory diseases (9, 10).
The survival of mature MC in tissues depends on signals from neighboring cells (11, 12). The single most important mediator in this process is stem cell factor (SCF), a master regulator of MC proliferation, differentiation, survival, and activation. Mice with genetic mutations affecting SCF or its receptor Kit have few or no MC in healthy or inflamed tissues, whereas activating mutations of Kit give rise to pathologic mastocytosis (13–15). IL-3 is another well-recognized MC growth factor (16). SCF/Kit and IL-3 interface with several antiapoptotic pathways, up-regulating the antiapoptotic protein B-cell lymphoma-2 (BCL-2) and downregulating the proapoptotic protein Bim (14, 17–19). Aside from SCF/Kit and IL-3, other cytokines have been reported to support MC survival, but their effects appear to be restricted to specific MC subtypes. IL-4 promotes survival of intestinal MC via both BCL-2 and B-cell lymphoma-X large (BCLXL) but may suppress survival in human cord blood MC as well as murine bone marrow-derived MC (BMMC) (20–23). IL-10 can either promote or impair survival depending on the type of MC studied (21, 22).
Recently, substantial attention has focused on the role of IL-33 in MC biology. A member of the IL-1 family, IL-33 is expressed primarily by stromal cells, such as epithelial cells, endothelial cells, and fibroblasts, as well as by certain hematopoietic cells, including MC themselves (24–26). IL-33 is an “alarmin” released upon cell necrosis and also can be secreted by live cells after mechanical stretching and via other incompletely defined mechanisms (27, 28). Its receptor ST2 (also called IL-1 receptor-related protein 1) is highly expressed by MC. Acting via ST2, IL-33 participates in MC activation in murine models of anaphylaxis and arthritis, serving both as a direct MC activator and as a factor that primes MC for enhanced cytokine release upon subsequent stimulation by IgE and IgG (29–32). IL-33 also prominently modulates the MC phenotype, promoting accumulation of MC protease 6 (the murine ortholog of human tryptase β) in vitro and in vivo (33).
In cardiomyocytes and hepatocytes, IL-33 protects against apoptosis (34, 35), raising the possibility of an analogous effect in MC. Improved in vitro survival has been observed in human umbilical cord blood-derived MC exposed to IL-33 and in cultured murine MC under certain conditions, but this effect is incompletely characterized, and its relevance in vivo remains unknown (36, 37). In the present study, we show that IL-33 promotes the survival of both human and murine MC, mediated principally by up-regulation of the antiapoptotic factor BCLXL. In vivo, IL-33 and ST2 play a nonredundant role in promoting MC survival in peritoneum and potentially other sites. These data reveal a role for the IL-33/ST2 axis in the survival of tissue MC, particularly in the context of inflammation, raising the possibility that this axis could be targeted to limit the contribution of MC to chronic inflammatory diseases.
Results
IL-33 Sustains Human MC Survival via BCLXL.
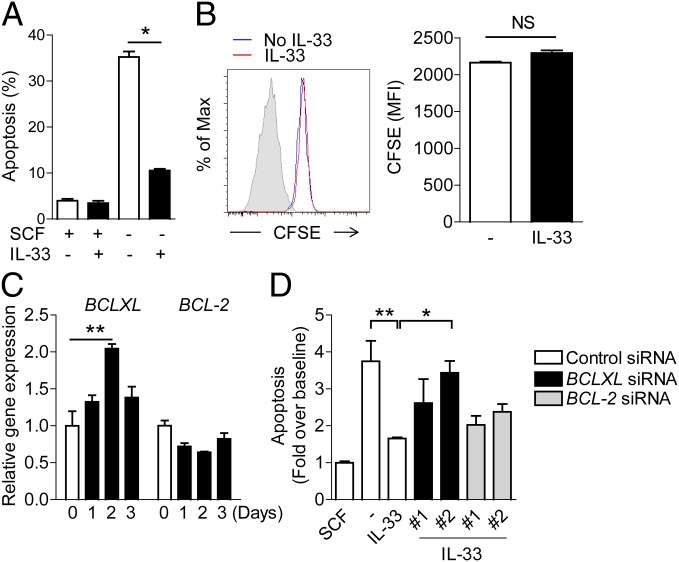
Human MC were cultured from human skin in serum-free medium containing SCF (38). Growth factor withdrawal is a standard model of apoptosis induction (39). Accordingly, MC (1 × 105/mL) were treated with or without IL-33 (10 ng/mL) in the presence or absence of SCF for 3 d. The percentage of apoptotic MC [Annexin V+ propidium iodide (PI)−] was measured using flow cytometry. IL-33 significantly inhibited MC apoptosis, reducing the fraction of cells undergoing apoptosis by a factor of three (Fig. 1A). To clarify whether this effect could reflect enhanced proliferation of surviving cells, we performed a carboxyfluorescein succinimidyl ester (CFSE) dilution assay. No difference in proliferation was observed after IL-33 stimulation, confirming that reduction of apoptosis was the sole basis for enhanced survival in IL-33–stimulated human MC (Fig. 1B).
Fig. 1.
IL-33 promotes the survival of human skin-derived MC by up-regulating BCLXL gene expression. (A) Human skin-derived MC at 1 × 105/mL were treated with or without IL-33 (10 ng/mL) in the presence or absence of SCF for 3 d. MC apoptosis was assessed by flow cytometry. (B) Cell division was measured by CFSE dilution assay in live MC (Annexin V−PI−) with or without IL-33 in the absence of SCF for 3 d. Gray shading is unlabeled control. (C) MC at 1 × 105/mL were stimulated with IL-33 (10 ng/mL) for 1, 2, or 3 d in replicates. The relative gene expression of BCLXL and BCL-2 was measured using real-time PCR. Data are representative of at least two donors and three independent experiments. (D) Twenty-four hours after siRNA transfection, MC were treated with or without IL-33 (10 ng/mL) in the presence or absence of SCF for 3 d. The fold increase in apoptosis was calculated by normalizing each group to its baseline in the presence of SCF. The data presented are combined from three independent experiments. *P < 0.05; **P < 0.01; NS, not significant.
BCLXL and BCL-2 play central roles in the regulation of cell survival in human MC (11, 40, 41). To test the effect of IL-33 on BCLXL and BCL-2, we analyzed expression of BCLXL and BCL-2 using quantitative PCR after 1, 2, and 3 d of stimulation with IL-33. Interestingly, IL-33 increased the expression of BCLXL but not BCL-2 (Fig. 1C). To confirm the involvement of BCLXL, we used gene silencing. BCLXL or BCL-2 were each targeted with two different siRNA sequences. For both genes, the knockdown efficacy of siRNA #2 (∼90%) was more potent than that of siRNA #1 (∼60%) (Fig. S1A). Under SCF culture conditions, potent knockdown of either gene increased apoptosis by 1.4- to 1.7-fold (Fig. S1B) (16). The protective effect of IL-33 was almost abolished by silencing BCLXL, whereas BCL-2 knockdown had a minor impact (Fig. 1D). Taken together, these results indicate that IL-33 protects human MC from apoptosis primarily through expression of BCLXL.
The IL-33 Receptor ST2 Is Required for the Prosurvival Effect of IL-33.
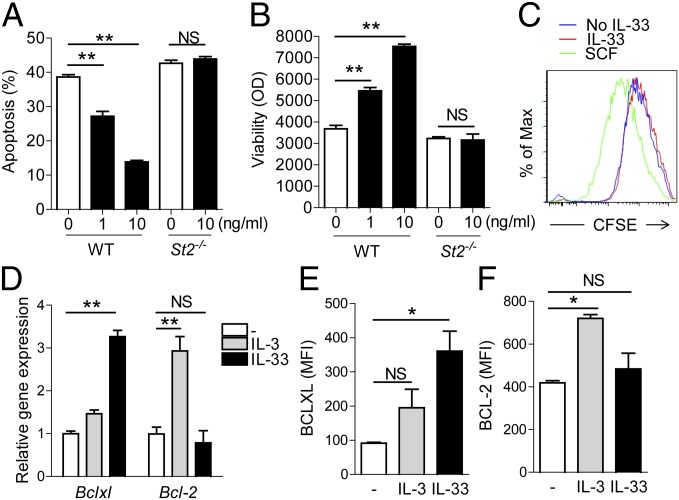
ST2 is the only known receptor for IL-33. Recently, inconsistent experimental results in Il33−/− and St2−/− mice have raised the possibility that other receptor(s) might play a role in IL-33 responses (42). To clarify whether the prosurvival effect of IL-33 on MC is mediated through ST2 and to assess whether murine models could be used to assess the in vivo importance of the IL-33/ST2 axis in MC survival, we generated murine BMMC from WT and St2−/− mice (43). Consistent with our human findings, IL-33 dose-dependently inhibited apoptosis and promoted the viability of BMMC subjected to cytokine deprivation (Fig. 2 A and B). This effect was completely abolished in St2−/− BMMC, confirming that ST2 is the only IL-33 receptor mediating the prosurvival function of IL-33 in these cells. As in human MC, the survival benefit of IL-33 was mediated exclusively by reduced apoptosis, because, unlike SCF, IL-33 failed to promote cell division as assessed by CFSE dilution (Fig. 2C). Consistent with our human data, we found that IL-33 specifically enhanced expression of BCLXL but not BCL-2 (Fig. 2 D–F). In contrast, exposure to the alternate murine BMMC survival factor IL-3 was associated with up-regulation of BCL-2 instead of BCLXL, demonstrating that the IL-33/ST2 axis represents a distinct pathway of protection from apoptosis (Fig. 2 D–F). These results confirm the importance of BCLXL in attenuating MC apoptosis by IL-33 and establish an essential role for ST2 in this effect.
Fig. 2.
The prosurvival effect of IL-33 depends on the expression of its receptor ST2. (A) WT and St2−/− BMMC (1 × 106/mL) were treated with or without IL-33 at 1 or 10 ng/mL in the absence of SCF/IL-3. MC apoptosis was assessed by flow cytometry after 3 d. (B) Cell viability in parallel wells was measured using alamarBlue dye. (C) Cell proliferation was analyzed by CFSE dilution assay on day 5. (D) BMMC at 1 × 106/mL were stimulated with 10 ng/mL of IL-33 or IL-3 in the absence of SCF for 24 h. Relative gene expression of Bclxl and Bcl-2 was analyzed by using real-time PCR. (E and F) The protein expression of BCLXL (E) and BCL-2 (F) was assessed using intracellular staining followed by flow cytometric analysis. Data are representative of at least two donors and two or three separate experiments. *P < 0.05; **P < 0.01; NS, not significant.
IL-33 Promotes BMMC Survival in both a Direct and an Indirect Manner.
IL-33 stimulation of MC induces the elaboration of numerous mediators (32, 37, 44, 45), raising the possibility that IL-33 might promote MC survival indirectly through the production of other factors. Therefore we used St2−/− BMMC to test the role of factors released by MC upon IL-33 exposure. WT and St2−/− MC were cultured together in a Transwell system wherein these cell populations were separated by a 0.4-μm filter to permit free diffusion of soluble mediators but allow separate analysis of each cell type. In this shared environment, IL-33 attenuated apoptosis of WT MC to a significantly greater extent than St2−/− MC, confirming a direct ST2-mediated effect of IL-33 on MC survival (Fig. 3A). However, IL-33–stimulated WT BMMC partially rescued cocultured St2−/− MC, indicating the release of non–IL-33 factors that also can contribute to survival (Fig. 3A). Consistent with this result, supernatants from WT BMMC cultured with or without IL-33 partially attenuated apoptosis of St2−/− BMMC subjected to growth factor deprivation (Fig. 3B). This effect was unaccompanied by induction of Bclxl in St2−/− BMMC (Fig. 3C), demonstrating that promotion of survival via BCLXL in this context is a direct and specific result of ST2 engagement.
Fig. 3.
IL-33 promotes MC survival in a direct and an indirect manner. (A) WT and St2−/− BMMC were introduced into the top or bottom chamber of a Transwell system (pore size 0.4 μm; Costar Corp.), or vice versa. Cocultured cells were treated with IL-33 (10 ng/mL) for 3 d after deprivation of SCF/IL-3. MC apoptosis was assessed by flow cytometry. (B) IL-33–conditioned medium was collected from WT BMMC culture either with or without IL-33 treatment in the absence of SCF/IL-3 after 1, 2, and 3 d and was transferred into the parallel St2−/− BMMC culture without SCF/IL-3. The cell apoptosis in St2−/− BMMC was evaluated after 3 d. (C) IL-33–conditioned medium collected on day 2 was transferred to St2−/− BMMC culture. After 24 h, the gene expression of Bclxl was evaluated by using real-time PCR. Data are representative of at least two independent experiments. *P < 0.05; **P < 0.01; NS, not significant.
ST2 Deficiency Is Associated with Impaired MC Accumulation in Vivo.
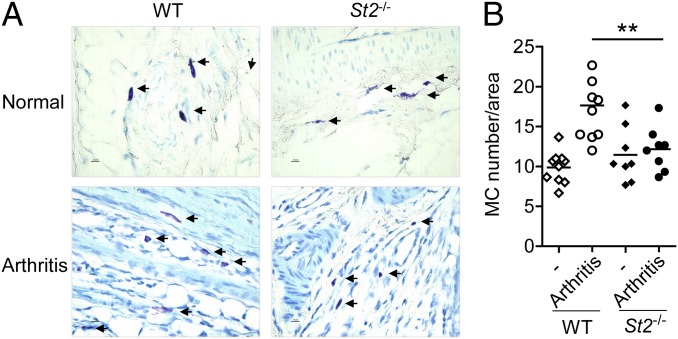
Compared with cultured MC, tissue-resident MC exhibit a diverse range of phenotypes and a much more complex set of local environments. To examine a role for IL-33/ST2 in vivo, we enumerated MC in tissues from WT and St2−/− mice in the waning phase of inflammation, when reduced SCF expression might relatively deprive an expanded MC population of growth factor support (46). We tested two models. K/BxN arthritis is an IgG-mediated immune complex arthritis that induces marked joint tissue inflammation within a few days of i.p. administration of arthritogenic serum. In this model, the number of MC in inflamed joint tissues more than doubles over the course of disease (47). Despite a somewhat milder course of arthritis in St2−/− mice, MC accumulation in actively inflamed joints at day 4 after the administration of K/BxN serum has been shown to be similar in WT and St2−/− animals (48), suggesting no significant difference in MC expansion during the initiation phase. We therefore examined synovial MC density at a point when the intensity of inflammation has begun to decline, day 10 after the administration of K/BxN serum. Consistent with our hypothesis, we found MC density to be reduced in both paw (Fig. S2) and ankle tissue (Fig. 4 A and B) in St2−/− animals. Next, we investigated intestinal helminth infection. After introduction of Trichinella spiralis by gavage, a robust intestinal accumulation of MC peaks at ∼14 d, declining progressively thereafter (49). Deficiency of ST2 does not affect intestinal worm burden, although these animals exhibit reduced intestinal Th2 responses and an enhanced larval burden in muscle (32, 48, 50). At analysis on day 21 after infection, the number of tissue MC was substantially lower in St2−/− mice than in control mice, suggesting that IL-33 has a role in the maintenance rather than the expansion of tissue MC populations (Fig. S3).
Fig. 4.
MC accumulation in inflamed joints is attenuated in St2−/− mice. K/BxN arthritis was induced by i.p. injection of arthritic serum. (A) On day 10, joints were removed and evaluated by toluidine blue. (B) The MC numbers in normal and arthritic ankles were quantified in three different areas per section under a light microscope. (Magnification: 200×.) Data are representative of three independent experiments. **P < 0.01.
WT MC Display a Cell-Intrinsic Survival Advantage over St2−/− MC in Murine Peritoneum.
Although consistent with our expectations, conclusions based on comparing WT with St2−/− mice are inherently limited. ST2 is broadly expressed, and differences in MC density inevitably will reflect the role of ST2 in the development, tissue localization, and effector activity of multiple lineages. Therefore we sought a more tractable model to test whether ST2 confers a cell-intrinsic survival benefit on MC.
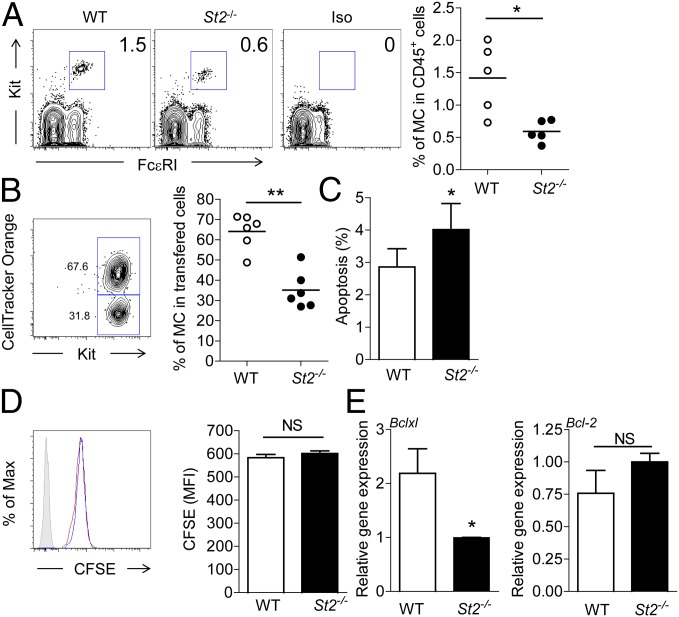
Peritoneal MC are mature connective tissue MC easily identified by flow cytometry through the high expression of surface FcεRI and Kit (51, 52) (Fig. 5A). Interestingly, and in contrast to our findings in healthy gut and joint tissue, we observed that St2−/− mice exhibited relatively fewer peritoneal MC than WT animals (∼0.5% vs. ∼1.4% of CD45+ peritoneal leukocytes) (Fig. 5A). Recognizing that peritoneal lining cells express IL-33 (53), we elected to use the peritoneal environment to study the role of the IL-33/ST2 axis on MC survival in vivo. We adapted an established MC i.p. engraftment system (54), choosing to analyze transferred cells within 1 wk of engraftment to minimize potential effects of ST2 on engraftment efficiency and tissue localization. WT and St2−/− BMMC (1.5 × 106 cells each) were labeled with CFSE plus CellTracker Orange or with CFSE alone, respectively, and were transferred i.p. together into St2−/− recipients, thereby allowing us to compare survival and proliferation of these cells within the same environment. In preliminary studies, the number of recovered donor cells ranged from ∼0.9–1.6 × 105 after 3 d; the proportion of dye-labeled cells in total CD45+ cells ranged from 14 to 20%, whereas the proportion of endogenous recipient MC ranged from 1.7 to 2.1%. The recovered dye-labeled cells were confirmed to be Kit+, excluding the possibility that peritoneal scavengers phagocytizing fluorescent debris could have been misidentified as engrafted MC. Recombinant IL-33 (100 ng per mouse) then was administered i.p. once daily, followed by collection of peritoneal cells on day 6 to determine cell survival, apoptosis, and proliferation. On average, ∼65% of labeled cells remaining on day 6 were WT, and ∼35% were St2−/− (Fig. 5B; flow cytometry gating strategy is shown in Fig. S4). This effect did not represent an intrinsic growth or survival advantage of WT BMMC, as demonstrated by equivalent survival of WT and St2−/− BMMC in culture (Fig. S5; see also Fig. 2A). Consistent with our in vitro data, transferred St2−/− BMMC exhibited a slightly higher percentage of early apoptotic cells than WT MC (Fig. 5C) in the absence of any difference in proliferation as determined by CFSE dilution (Fig. 5D). Further, WT but not St2−/− BMMC exhibited enhanced expression of Bclxl but not Bcl-2 (Fig. 5E). Thus, a direct and ST2-specific survival benefit associated with enhanced expression of BCLXL emerged clearly in this complex in vivo milieu. Notably, only 3–4% of transferred cells harvested on day 6 exhibited apoptosis, presumably because apoptotic cells are removed rapidly by host peritoneal cells through phagocytosis.
Fig. 5.
WT MC display a survival advantage over St2−/− MC in response to IL-33 in murine peritoneum. (A) Peritoneal cells were harvested by peritoneal lavage from WT and St2−/− mice (n = 5). The proportions of resident MC (CD45+Kit+FcεRI+) in total leukocytes (CD45+) were analyzed using flow cytometry. (B) A 1:1 mixture (1.5 × 106 each) of WT and St2−/− BMMC labeled with CFSE plus CellTracker Orange and CFSE alone, respectively, or vice versa, was transferred into peritoneum in St2−/− mice on day 0. IL-33 (100 ng per mouse) was administered i.p. every day for 6 d, and the survival of MC in peritoneum on day 6 was analyzed by flow cytometry. Representative plots show WT and St2−/− MC populations; quantitative data reflect the proportion of remaining donor WT and St2−/− MC in each mouse. (C) The percentage of apoptotic cells (Annexin V+Live/Dead−) in each population. (D) Assessment of proliferation by CFSE fluorescence. (E) Bclxl and Bcl-2 mRNA levels in WT and St2−/− MC populations harvested from murine peritoneum on day 6 (samples analyzed individually from n = 5–6 mice). Data are representative of two independent experiments. *P < 0.05, **P < 0.01; NS, not significant.
The IL-33/ST2 Axis Contributes to MC Survival in Peritonitis.
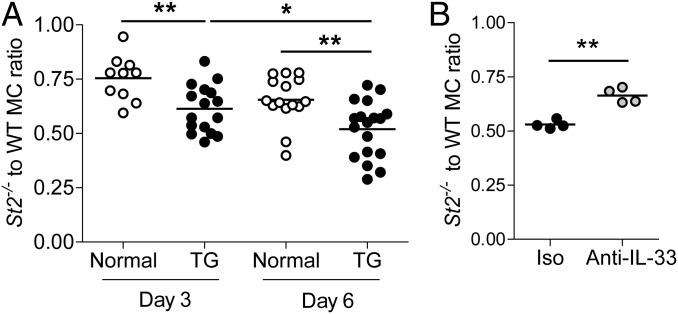
To test whether ST2 expression conferred a survival advantage under conditions of inflammation, equal numbers of labeled WT and St2−/− BMMC were engrafted i.p. into WT animals with or without peritonitis induced by thioglycollate. The cells engrafted well in both normal and inflammatory conditions (0.76 ± 0.13 × 105, n = 2 and 1.70 ± 0.10 × 105, n = 5, recovered after 6 d from normal and inflamed peritoneum, respectively, in preliminary studies). Consistent with our earlier results, expression of ST2 favored survival as indicated by a decrease in the ratio of St2−/− to WT MC recovered, and this advantage was enhanced in the inflamed environment (Fig. 6A). Importantly, cytokine neutralization via a blocking anti–IL-33 antibody (32, 55) (Fig. S6) attenuated the survival advantage of WT over St2−/− BMMC (Fig. 6B), confirming involvement of IL-33 in the survival of MC in the inflamed peritoneum. In the absence of peritonitis, we identified no effect of anti–IL-33 blocking antibody on the St2−/−/WT cell ratio (Fig. S7).
Fig. 6.
The IL-33/ST2 axis contributes to MC survival in thioglycollate (TG)-induced peritonitis. (A) Peritonitis was initiated by i.p. injection of thioglycollate 1 d before cell transfer. A 1:1 mixture of WT and St2−/− BMMC labeled with CFSE plus CellTracker Orange and CFSE or of CD45.1 WT and CD45.2 St2−/− BMMC (2 × 106 each) labeled with CFSE was transferred to normal or inflamed peritoneum in WT mice. Surviving cells were harvested and analyzed using flow cytometry after 3 or 6 d. (B) IL-33 antibody (Nessy-1) or an isotype antibody was given to mice with peritonitis (40 μg per mouse, i.p., for 3 d). After 3 d, the ratio of surviving St2−/− to WT MC was assessed by flow cytometry. Data are representative of two to six independent experiments. *P < 0.05, **P < 0.01.
Discussion
Mast cells are found in most healthy vascularized tissues, and their numbers expand markedly under inflammatory conditions (56). Multiple lines of evidence show that mediators from surrounding cells are critical to the regulation of MC phenotype and survival, although many mechanistic details are lacking (57). The present findings demonstrate that IL-33, acting via its receptor ST2, represents an antiapoptotic signal for both murine and human MC and that the IL-33/ST2 axis plays a previously unrecognized role to support MC survival in vivo.
Mechanistically, we find that IL-33 drives expression of the antiapoptotic protein BCLXL and that BCLXL is the principal mediator of IL-33–mediated protection. This pathway only partially overlaps the pathway by which IL-33 supports the survival of other cell types. In rat cardiomyocytes, IL-33 abrogates hypoxia-induced apoptosis in association with elevation of a series of antiapoptotic molecules, including BCLXL, BCL-2, c-IAP, c-IAP2, XIAP, and survivin; this effect is specific to hypoxia and is not observed under conditions of normal oxygen tension (34). In murine hepatocytes, IL-33 suppresses apoptosis in Concanavalin A-induced hepatitis through up-regulation of BCL-2 and down-regulation of Bax (35). Thus, the pathways by which IL-33 prevents cell death vary with cell type and the conditions inducing apoptosis.
In MC, BCL-2 and BCLXL can each promote survival, and inhibition of both essentially eliminates MC in vivo, confirming that they represent the antiapoptotic molecules of dominant physiological relevance for MC (58, 59). Both BCL-2 and BCLXL strongly bind and inhibit active Bax, thereby preventing this apoptotic effector from damaging the mitochondrial outer membrane and precipitating cellular demise (41). Bax is known to play a preeminent role mediating apoptosis induced by growth factor deprivation (60). Our data reveal that either SCF or IL-3 (acting via BCL-2) or IL-33 (acting via BCLXL) can sustain MC populations exposed to this proapoptotic stress (18, 19, 58). Whether other causes of apoptosis, such as hypoxia, engage the same pathways remains to be determined.
The survival signals that protect MC from apoptosis and thereby allow accumulation in tissues likely will vary with context and probably are complex. We find that WT MC survive better than St2−/− MC cotransferred into the peritoneum in the presence of exogenous IL-33 or under conditions of thioglycollate peritonitis. In some of these experiments, the recipients themselves were St2−/− mice, excluding graft rejection as the cause of this effect. In thioglycollate peritonitis, differential survival was attenuated by IL-33 blockade. No similar effect of IL-33 blockade emerged in the absence of induced inflammation, although we did observe a relative paucity of peritoneal MC in St2−/− mice compared with their WT counterparts, likely reflecting the inadequacy of our short-term engraftment system to model all facets of ST2-mediated MC persistence in the peritoneum. These findings confirm that, in the peritoneum, the IL-33/ST2 axis can play an important role in MC preservation, potentially because these free-floating cells have reduced access to surface-bound SCF. In contrast, in synovium and intestine, the MC population is numerically normal under healthy conditions and in early, but not later, inflammation. ST2 plays multiple roles in these complex models, prohibiting firm conclusions about the role of ST2-mediated protection from apoptosis. Even if MC were the only cells lacking ST2, we still would be unable to disentangle differential apoptosis from effects of ST2 on MC development, distribution, or ST2-based interaction with neighboring cells. Despite this limitation, the results from arthritis and helminth infection remain strikingly concordant with our in vitro findings and in vivo peritoneal data, lending plausibility to the suggestion that the role of ST2 confirmed in our peritoneal transfer experiments may be operative more broadly, including in tissue MC.
Beyond the direct antiapoptotic effect of ST2 ligation on MC, we show that IL-33 also can promote MC survival indirectly by triggering MC to produce soluble factors that contribute to their own survival. MC exposed to IL-33 produce numerous mediators (6, 8, 32, 37, 44, 45), and the cytokine or combination of cytokines that promote survival of bystander St2−/− MC in our system remains to be determined. Interestingly, we find these indirect signals operate independently of Bclxl up-regulation, highlighting the relative specificity of this pathway for IL-33/ST2.
Our studies used skin-derived human MC, murine BMMC, and murine peritoneal, synovial, and intestinal MC. The consistency of our findings suggests that the prosurvival effect of IL-33/ST2 in MC may be broadly conserved. Further investigation is required to confirm the effect of IL-33/ST2 on specific types of MC and in other tissues and disease states. Given the diversity of MC phenotypes and inflammatory tissue settings, it is likely that IL-33 will play a more important role for MC survival in some contexts than in others.
Our findings raise the interesting possibility that antagonism of IL-33 or ST2 could selectively attenuate MC accumulation in chronically inflamed tissues. Whether such disruption of MC expansion will help the host may vary with disease context. MC can produce a range of lipids, cytokines, and proteases, depending on the stimulus and the MC’s developmental phenotype. At the start of an inflammatory process, tissue MC populations usually are relatively sparse, serving primarily as sentinels rather than as major effectors of innate immunity. As their numbers expand with inflammation, the role MC play likely evolves (7). In chronic inflammation, MC could continue to “feed the fire” via ongoing mediator release, antigen presentation, or other mechanisms. Alternately, MC could help suppress disease, for instance by protease-mediated elimination of proinflammatory mediators, by facilitating tissue remodeling, or by promoting tolerance (61–64). The effect of attenuating MC survival by blocking the IL-33/ST2 axis will be important to consider when evaluating IL-33 and ST2 as potential therapeutic targets.
Materials and Methods
Human skin MC were cultured as described previously (38). Mouse BMMC were developed from mouse bone marrow as described previously (32). Real-time PCR, siRNA knockdown, and flow cytometry were performed as indicated in SI Materials and Methods. Arthritis was induced by the i.p. injection of K/BxN serum as previously described (32). MC quantification was performed blindly on paraffin-embedded 4-µm sections stained with toluidine blue using established methods. Peritonitis was initiated by instillation of 1 mL of sterile aged 3% (wt/vol) thioglycollate broth i.p. 1 d before cell transfer. WT and St2−/− BMMC were transferred at a 1:1 ratio into peritoneum. Some groups were injected with isotype antibody or anti–IL-33 (Nessy-1; Enzo Life Sciences) (40 µg per mouse, i.p. once daily). Animal experiments were approved by the Institutional Animal Care and Use Committee of the Dana-Farber Cancer Institute (Animal Welfare Assurance Number: A3023-01). All efforts were made to minimize the suffering of animals used in this research. Statistical analysis was performed using Student t test, and data were analyzed using GraphPad Prism software version 4. Results are presented as the mean ± SEM. P values less than 0.05 were considered significant.
Supplementary Material
Acknowledgments
We thank Dr. Michael B. Brenner for providing K/BxN mouse serum for our arthritis experiments, Dr. Andrew N. J. McKenzie for the gift of St2−/− mice, and Dr. Richard T. Lee for helpful discussions. J.-X.W. was supported by the Arthritis National Research Foundation. P.A.N. was supported by National Institutes of Health Grants AR051321 and AR062328 and by the Cogan Family Foundation.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission. C.G. is a guest editor invited by the Editorial Board.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1404182111/-/DCSupplemental.
References
- 1.Wedemeyer J, Tsai M, Galli SJ. Roles of mast cells and basophils in innate and acquired immunity. Curr Opin Immunol. 2000;12(6):624–631. doi: 10.1016/s0952-7915(00)00154-0. [DOI] [PubMed] [Google Scholar]
- 2.Hepworth MR, Maurer M, Hartmann S. Regulation of type 2 immunity to helminths by mast cells. Gut Microbes. 2012;3(5):476–481. doi: 10.4161/gmic.21507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hepworth MR, et al. Mast cells orchestrate type 2 immunity to helminths through regulation of tissue-derived cytokines. Proc Natl Acad Sci USA. 2012;109(17):6644–6649. doi: 10.1073/pnas.1112268109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Younan GJ, et al. Mast cells are required in the proliferation and remodeling phases of microdeformational wound therapy. Plast Reconstr Surg. 2011;128(6):649e–658e. doi: 10.1097/PRS.0b013e318230c55d. [DOI] [PubMed] [Google Scholar]
- 5.Jung M, et al. Mast cells produce novel shorter forms of perlecan that contain functional endorepellin: A role in angiogenesis and wound healing. J Biol Chem. 2013;288(5):3289–3304. doi: 10.1074/jbc.M112.387811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Theoharides TC, et al. Mast cells and inflammation. Biochim Biophys Acta. 2012;1822(1):21–33. doi: 10.1016/j.bbadis.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nigrovic PA, Lee DM. Synovial mast cells: Role in acute and chronic arthritis. Immunol Rev. 2007;217:19–37. doi: 10.1111/j.1600-065X.2007.00506.x. [DOI] [PubMed] [Google Scholar]
- 8.Nigrovic PA, et al. Mast cells contribute to initiation of autoantibody-mediated arthritis via IL-1. Proc Natl Acad Sci USA. 2007;104(7):2325–2330. doi: 10.1073/pnas.0610852103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benoist C, Mathis D. Mast cells in autoimmune disease. Nature. 2002;420(6917):875–878. doi: 10.1038/nature01324. [DOI] [PubMed] [Google Scholar]
- 10.Woolley DE. The mast cell in inflammatory arthritis. N Engl J Med. 2003;348(17):1709–1711. doi: 10.1056/NEJMcibr023206. [DOI] [PubMed] [Google Scholar]
- 11.Ekoff M, Nilsson G. Mast cell apoptosis and survival. Adv Exp Med Biol. 2011;716:47–60. doi: 10.1007/978-1-4419-9533-9_4. [DOI] [PubMed] [Google Scholar]
- 12.Gurish MF, Austen KF. Developmental origin and functional specialization of mast cell subsets. Immunity. 2012;37(1):25–33. doi: 10.1016/j.immuni.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Kitamura Y, Hirota S, Nishida T. A loss-of-function mutation of c-kit results in depletion of mast cells and interstitial cells of Cajal, while its gain-of-function mutation results in their oncogenesis. Mutat Res. 2001;477(1-2):165–171. doi: 10.1016/s0027-5107(01)00117-8. [DOI] [PubMed] [Google Scholar]
- 14.Waskow C, Bartels S, Schlenner SM, Costa C, Rodewald HR. Kit is essential for PMA-inflammation-induced mast-cell accumulation in the skin. Blood. 2007;109(12):5363–5370. doi: 10.1182/blood-2006-08-039131. [DOI] [PubMed] [Google Scholar]
- 15.Brockow K, Metcalfe DD. Mastocytosis. Chem Immunol Allergy. 2010;95:110–124. doi: 10.1159/000315946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mekori YA, Oh CK, Metcalfe DD. The role of c-Kit and its ligand, stem cell factor, in mast cell apoptosis. Int Arch Allergy Immunol. 1995;107(1-3):136–138. doi: 10.1159/000236955. [DOI] [PubMed] [Google Scholar]
- 17.Möller C, et al. Stem cell factor promotes mast cell survival via inactivation of FOXO3a-mediated transcriptional induction and MEK-regulated phosphorylation of the proapoptotic protein Bim. Blood. 2005;106(4):1330–1336. doi: 10.1182/blood-2004-12-4792. [DOI] [PubMed] [Google Scholar]
- 18.Baghestanian M, et al. Activation of human mast cells through stem cell factor receptor (KIT) is associated with expression of bcl-2. Int Arch Allergy Immunol. 2002;129(3):228–236. doi: 10.1159/000066773. [DOI] [PubMed] [Google Scholar]
- 19.Rinaudo MS, Su K, Falk LA, Halder S, Mufson RA. Human interleukin-3 receptor modulates bcl-2 mRNA and protein levels through protein kinase C in TF-1 cells. Blood. 1995;86(1):80–88. [PubMed] [Google Scholar]
- 20.Lorentz A, et al. IL-4-induced priming of human intestinal mast cells for enhanced survival and Th2 cytokine generation is reversible and associated with increased activity of ERK1/2 and c-Fos. J Immunol. 2005;174(11):6751–6756. doi: 10.4049/jimmunol.174.11.6751. [DOI] [PubMed] [Google Scholar]
- 21.Oskeritzian CA, et al. Recombinant human (rh)IL-4-mediated apoptosis and recombinant human IL-6-mediated protection of recombinant human stem cell factor-dependent human mast cells derived from cord blood mononuclear cell progenitors. J Immunol. 1999;163(9):5105–5115. [PubMed] [Google Scholar]
- 22.Speiran K, et al. Endogenous suppression of mast cell development and survival by IL-4 and IL-10. J Leukoc Biol. 2009;85(5):826–836. doi: 10.1189/jlb.0708448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burton OT, et al. Direct effects of IL-4 on mast cells drive their intestinal expansion and increase susceptibility to anaphylaxis in a murine model of food allergy. Mucosal Immunol. 2013;6(4):740–750. doi: 10.1038/mi.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moussion C, Ortega N, Girard JP. The IL-1-like cytokine IL-33 is constitutively expressed in the nucleus of endothelial cells and epithelial cells in vivo: A novel ‘alarmin’? PLoS ONE. 2008;3(10):e3331. doi: 10.1371/journal.pone.0003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saenz SA, Taylor BC, Artis D. Welcome to the neighborhood: Epithelial cell-derived cytokines license innate and adaptive immune responses at mucosal sites. Immunol Rev. 2008;226:172–190. doi: 10.1111/j.1600-065X.2008.00713.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liew FY, Pitman NI, McInnes IB. Disease-associated functions of IL-33: The new kid in the IL-1 family. Nat Rev Immunol. 2010;10(2):103–110. doi: 10.1038/nri2692. [DOI] [PubMed] [Google Scholar]
- 27.Kakkar R, Hei H, Dobner S, Lee RT. Interleukin 33 as a mechanically responsive cytokine secreted by living cells. J Biol Chem. 2012;287(9):6941–6948. doi: 10.1074/jbc.M111.298703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martin MU. Special aspects of interleukin-33 and the IL-33 receptor complex. Semin Immunol. 2013;25(6):449–457. doi: 10.1016/j.smim.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 29.Lunderius-Andersson C, Enoksson M, Nilsson G. Mast Cells Respond to Cell Injury through the Recognition of IL-33. Front Immunol. 2012;3:82. doi: 10.3389/fimmu.2012.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tjota MY, et al. IL-33-dependent induction of allergic lung inflammation by FcγRIII signaling. J Clin Invest. 2013;123(5):2287–2297. doi: 10.1172/JCI63802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen X, et al. Fc gamma receptor signaling in mast cells links microbial stimulation to mucosal immune inflammation in the intestine. Am J Pathol. 2008;173(6):1647–1656. doi: 10.2353/ajpath.2008.080487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaieda S, et al. Interleukin-33 primes mast cells for activation by IgG immune complexes. PLoS ONE. 2012;7(10):e47252. doi: 10.1371/journal.pone.0047252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaieda S, et al. Synovial fibroblasts promote the expression and granule accumulation of tryptase via interleukin-33 and its receptor ST-2 (IL1RL1) J Biol Chem. 2010;285(28):21478–21486. doi: 10.1074/jbc.M110.114991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seki K, et al. Interleukin-33 prevents apoptosis and improves survival after experimental myocardial infarction through ST2 signaling. Circ Heart Fail. 2009;2(6):684–691. doi: 10.1161/CIRCHEARTFAILURE.109.873240. [DOI] [PubMed] [Google Scholar]
- 35.Volarevic V, et al. Protective role of IL-33/ST2 axis in Con A-induced hepatitis. J Hepatol. 2012;56(1):26–33. doi: 10.1016/j.jhep.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 36.Iikura M, et al. IL-33 can promote survival, adhesion and cytokine production in human mast cells. Lab Invest. 2007;87(10):971–978. doi: 10.1038/labinvest.3700663. [DOI] [PubMed] [Google Scholar]
- 37.Ho LH, et al. IL-33 induces IL-13 production by mouse mast cells independently of IgE-FcepsilonRI signals. J Leukoc Biol. 2007;82(6):1481–1490. doi: 10.1189/jlb.0407200. [DOI] [PubMed] [Google Scholar]
- 38.Norton SK, et al. A new class of human mast cell and peripheral blood basophil stabilizers that differentially control allergic mediator release. Clin Transl Sci. 2010;3(4):158–169. doi: 10.1111/j.1752-8062.2010.00212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Collins MK, Perkins GR, Rodriguez-Tarduchy G, Nieto MA, Lopez-Rivas A. Growth factors as survival factors: Regulation of apoptosis. BioEssays. 1994;16(2):133–138. doi: 10.1002/bies.950160210. [DOI] [PubMed] [Google Scholar]
- 40.Mekori YA, Gilfillan AM, Akin C, Hartmann K, Metcalfe DD. Human mast cell apoptosis is regulated through Bcl-2 and Bcl-XL. J Clin Immunol. 2001;21(3):171–174. doi: 10.1023/a:1011083031272. [DOI] [PubMed] [Google Scholar]
- 41.Billen LP, Kokoski CL, Lovell JF, Leber B, Andrews DW. Bcl-XL inhibits membrane permeabilization by competing with Bax. PLoS Biol. 2008;6(6):e147. doi: 10.1371/journal.pbio.0060147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kamradt T, Drube S. A complicated liaison: IL-33 and IL-33R in arthritis pathogenesis. Arthritis Res Ther. 2013;15(3):115. doi: 10.1186/ar4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Townsend MJ, Fallon PG, Matthews DJ, Jolin HE, McKenzie AN. T1/ST2-deficient mice demonstrate the importance of T1/ST2 in developing primary T helper cell type 2 responses. J Exp Med. 2000;191(6):1069–1076. doi: 10.1084/jem.191.6.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moulin D, et al. Interleukin (IL)-33 induces the release of pro-inflammatory mediators by mast cells. Cytokine. 2007;40(3):216–225. doi: 10.1016/j.cyto.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 45.Allakhverdi Z, Smith DE, Comeau MR, Delespesse G. Cutting edge: The ST2 ligand IL-33 potently activates and drives maturation of human mast cells. J Immunol. 2007;179(4):2051–2054. doi: 10.4049/jimmunol.179.4.2051. [DOI] [PubMed] [Google Scholar]
- 46.Kiener HP, et al. Tumor necrosis factor alpha promotes the expression of stem cell factor in synovial fibroblasts and their capacity to induce mast cell chemotaxis. Arthritis Rheum. 2000;43(1):164–174. doi: 10.1002/1529-0131(200001)43:1<164::AID-ANR21>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 47.Shin K, et al. Lymphocyte-independent connective tissue mast cells populate murine synovium. Arthritis Rheum. 2006;54(9):2863–2871. doi: 10.1002/art.22058. [DOI] [PubMed] [Google Scholar]
- 48.Xu D, et al. IL-33 exacerbates autoantibody-induced arthritis. J Immunol. 2010;184(5):2620–2626. doi: 10.4049/jimmunol.0902685. [DOI] [PubMed] [Google Scholar]
- 49.Friend DS, et al. Mast cells that reside at different locations in the jejunum of mice infected with Trichinella spiralis exhibit sequential changes in their granule ultrastructure and chymase phenotype. J Cell Biol. 1996;135(1):279–290. doi: 10.1083/jcb.135.1.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scalfone LK, et al. Participation of MyD88 and interleukin-33 as innate drivers of Th2 immunity to Trichinella spiralis. Infect Immun. 2013;81(4):1354–1363. doi: 10.1128/IAI.01307-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Galli SJ, Borregaard N, Wynn TA. Phenotypic and functional plasticity of cells of innate immunity: Macrophages, mast cells and neutrophils. Nat Immunol. 2011;12(11):1035–1044. doi: 10.1038/ni.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Malbec O, et al. Peritoneal cell-derived mast cells: An in vitro model of mature serosal-type mouse mast cells. J Immunol. 2007;178(10):6465–6475. doi: 10.4049/jimmunol.178.10.6465. [DOI] [PubMed] [Google Scholar]
- 53.Enoksson M, et al. Intraperitoneal influx of neutrophils in response to IL-33 is mast cell-dependent. Blood. 2013;121(3):530–536. doi: 10.1182/blood-2012-05-434209. [DOI] [PubMed] [Google Scholar]
- 54.Nakano T, et al. Pillars article: Fate of bone marrow-derived cultured mast cells after intracutaneous, intraperitoneal, and intravenous transfer into genetically mast cell-deficient w/wv mice. Evidence that cultured mast cells can give rise to both connective tissue type and mucosal mast cells. J Immunol. 2009;183(11):6863–6881. [PubMed] [Google Scholar]
- 55.Ohno T, et al. Paracrine IL-33 stimulation enhances lipopolysaccharide-mediated macrophage activation. PLoS ONE. 2011;6(4):e18404. doi: 10.1371/journal.pone.0018404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Metcalfe DD. Mast cells and mastocytosis. Blood. 2008;112(4):946–956. doi: 10.1182/blood-2007-11-078097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gurish MF, Austen KF. The diverse roles of mast cells. J Exp Med. 2001;194(1):F1–F5. doi: 10.1084/jem.194.1.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hartmann K, et al. Expression of Bcl-2 and Bcl-xL in cutaneous and bone marrow lesions of mastocytosis. Am J Pathol. 2003;163(3):819–826. doi: 10.1016/S0002-9440(10)63442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Karlberg M, et al. The BH3-mimetic ABT-737 induces mast cell apoptosis in vitro and in vivo: Potential for therapeutics. J Immunol. 2010;185(4):2555–2562. doi: 10.4049/jimmunol.0903656. [DOI] [PubMed] [Google Scholar]
- 60.Karlberg M, et al. Pro-apoptotic Bax is the major and Bak an auxiliary effector in cytokine deprivation-induced mast cell apoptosis. Cell Death Dis. 2010;1:e43. doi: 10.1038/cddis.2010.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Caughey GH. Mast cell proteases as protective and inflammatory mediators. Adv Exp Med Biol. 2011;716:212–234. doi: 10.1007/978-1-4419-9533-9_12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Galli SJ, Tsai M. Mast cells: Versatile regulators of inflammation, tissue remodeling, host defense and homeostasis. J Dermatol Sci. 2008;49(1):7–19. doi: 10.1016/j.jdermsci.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nowak EC, et al. Tryptophan hydroxylase-1 regulates immune tolerance and inflammation. J Exp Med. 2012;209(11):2127–2135. doi: 10.1084/jem.20120408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roy A, et al. Mast cell chymase degrades the alarmins heat shock protein 70, biglycan, HMGB1, and interleukin-33 (IL-33) and limits danger-induced inflammation. J Biol Chem. 2014;289(1):237–250. doi: 10.1074/jbc.M112.435156. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.