Abstract
Background
We describe a successful interdisciplinary liaison program that effectively reduced health care-acquired (HCA), methicillin-resistant Staphylococcus aureus (MRSA) in a university hospital setting.
Methods
Baseline was from January 2006 to March 2008, and intervention period was April 2008 to September 2009. Staff nurses were trained to be liaisons (link nurses) to infection prevention (IP) personnel with clearly defined goals assigned and with ongoing monthly education. HCA-MRSA incidence per 1,000 patient-days (PD) was compared between baseline and intervention period along with total and non-HCA-MRSA, HCA and non-HCA-MRSA bacteremia, and hand soap/sanitizer usage. Hand hygiene compliance was assessed.
Results
A reduction in MRSA rates was as follows in intervention period compared with baseline: HCA-MRSA decreased by 28% from 0.92 to 0.67 cases per 1,000 PD (incidence rate ratio, 0.72; 95% confidence interval: 0.62–0.83, P < .001), and HCA-MRSA bacteremia rate was reduced by 41% from 0.18 to 0.10 per 1,000 PD (incidence rate ratio, 0.59; 95% confidence interval: 0.42–0.84, P = .003). Total MRSA rate and MRSA bacteremia rate also showed significant reduction with nonsignificant reductions in overall non-HCA-MRSA and non-HCA-MRSA bacteremia. Hand soap/sanitizer usage and compliance with hand hygiene also increased significantly during IP.
Conclusion
Link nurse program effectively reduced HCA-MRSA. Goal-defined metrics with ongoing reeducation for the nurses by IP personnel helped drive these results.
Keywords: MRSA, Multi-disciplinary, Infection prevention, Liaison, Patient safety, Nosocomial, Hand hygiene, Handwashing
Increasing antibiotic resistance among the most common bacterial pathogens, in the hospital and community, presents a growing threat to human health worldwide.1 Health care-acquired (HCA) infections cause significant morbidity and mortality in addition to posing huge financial burden to health care systems.2–7 This is especially true for methicillin-resistant Staphylococcus aureus (MRSA), which can cause a variety of infections with variable but significant cost impact.8,9 The avoided cost was estimated to be $2,051,286 for 58 MRSA infections avoided over the 2-year period during the Effective Processes in Infection Control project by the Spartanburg Regional Healthcare System.10 Hospital reimbursement is now affected for certain hospital-acquired infections including MRSA infections.11
It is possible to significantly reduce the rates of HCA-MRSA and other multidrug-resistant organisms with attention to IP practices.9,12–16 Improving hand hygiene compliance among health care workers (HCW) has shown to have a positive impact on HCA-MRSA.17,18 This may be achieved by engaging front-line HCW in the process of infection prevention (IP). Such an engagement may require a multidisciplinary effort with well-defined goals and an effective feedback process. An IP program entitled “Partners in your Care” initially developed at the University of Pennsylvania19–23 was previously implemented at our medical center in March 2006. Unfortunately, the program struggled to survive, until it was subsequently disbanded. This experience led to a root cause evaluation for its failure within the Department of Clinical Epidemiology (Infection Prevention). Ownership of such quality improvement programs needs to be with the individual patient care unit (PCU) staff themselves, and IP needs sustained presence on PCUs to facilitate this ownership. Some studies describing the perceptions of HCW on IP practices including hand hygiene stress the need to spread knowledge of IP and effective hand hygiene beyond IP professionals to other HCW for ongoing success.24–27 Collaboration between IP professionals and staff nurses (link nurses) from the individual PCUs to reduce HCA infections, especially MRSA, has been described in the past. However the strategies for carrying out the collaboration and the success of such programs were variable.15,28–31
Previous descriptions of link nurse programs acknowledge operational difficulties such as high turnover of staff, insufficient time for training, and monitoring their effectiveness.30,31 Overcoming these early challenges may result in a successful and sustainable program that will be a valuable asset for IP. We hypothesized that a well-designed link nurse program will result in a decrease in HCA-MRSA by causing an increase in hand hygiene participation. We demonstrate how a multidisciplinary effort led by a clinical epidemiology team has successfully developed and sustained this program.
METHODS
Study design
This quality improvement study implemented an IP program (Link Nurse Program) to reduce HCA-MRSA incidence. It was implemented as a performance improvement initiative at all of the hospitals affiliated with The Ohio State University Wexner Medical Center (OSUWMC) including University Hospital, Ross Heart Hospital, University Hospital East, the James Cancer Hospital and Richard Solove Research Institute, and the Dodd Rehabilitation Hospital. Data analysis was performed to evaluate the effect of Link Nurse Program on HCA-MRSA. The OSUWMC is a 1,191-bed hospital with 5 infection preventionists (at the time of this study) and 3 physicians in the Department of Clinical Epidemiology. Waiver from the OSUWMC’s Institutional Review Board was obtained and the study deemed a quality improvement effort.
Study time period
The baseline period for this study was January 1, 2006, to March 31, 2008. Intervention period was April 1, 2008, to September 30, 2009.
Routine surveillance and IP practices
When multidrug-resistant pathogens (defined as resistance to ≥ 2 drugs within 2 or more drug classes) are identified by the Clinical Microbiology Laboratory, contact isolation (CI) precautions (ie, gloving and gowning for those who enter the room) are instituted. These precautions are also instituted when patients with a history of MRSA or vancomycin-resistant enterococcus are readmitted to the hospital.
Selection and training of link nurses
Department of Clinical Epidemiology physicians (co-authors) approached the 3 chief nursing officers individually with a proposal detailing each of the 3 hospitals’ individual rates of HCA-MRSA, compliance to hand hygiene, and CI in the winter of 2007. We presented a plan to monitor outcome measures that are described below and obtained approval from hospital administration to implement the program. We selected 1 to 2 link nurses per PCU, who either volunteered or were nominated by nursing administrators and/or nurse managers of each PCU. The time commitment for participation in the program was considered as part of their work time. We offered an opportunity to use their work for a clinical ladder project for advancement. The original commitment was for attendance at a 2-day training course and monthly 1-hour meetings, both led by Clinical Epidemiology, with at least 4 hours per month per nurse dedicated to this ongoing work on each PCU.
Clinical Epidemiology conducted 3 consecutive 16-hour training sessions (in April 2008, June 2008, and March 2009); the curriculum included the basics and principles of IP. Clinical Microbiology Laboratory provided a 2-hour laboratory tour with on-site education on microbiology supporting the IP principles within the 16 hours. All link nurses were required to attend the training within the first year that they joined the program. Clinical Epidemiology led monthly follow-up meetings for link nurses to evaluate progress and provide ongoing education on IP issues.
Duties of link nurses
Link nurses monitored hand hygiene on a daily basis during their regularly scheduled shifts along with CI compliance (at least 10 audits per month) among HCW and physicians on their respective units and provided on-the-spot feedback. They were also asked to bring specific IP issues that they identified on their unit to the attention of Clinical Epidemiology, which would subsequently address those issues as part of topic-focused monthly meetings. The subjects ranged from HCW noncompliance with IP policies to system issues that potentially hindered compliance. The link nurses reviewed IP information provided during the link nurse monthly meetings and shared it at the individual PCU staff meetings. The assigned 4 hours/month were spent attending monthly link nurse meeting, disseminating information at staff meetings and preparing informational bulletins for quality boards on PCUs, one-on-one education to the staff, in-service education, observing hand hygiene and CI precaution practice on their units and identifying existing barriers that hinder performance and identifying barriers to compliance, and on-the-spot feedback to the staff in the event of a breach in compliance.
Feedback to the units
Monthly data on hand hygiene and CI were collected by the link nurses and submitted to Clinical Epidemiology. Compliance was defined as using alcohol hand sanitizer or soap and water to clean hands prior to entry or upon exiting the patient’s room. Each observation (entry or exit) was counted as 1 audit. Compliance with CI was defined as wearing CI gown and gloves prior to entering a CI room. Quarterly data on unit-specific HCA-MRSA infection rates were provided back to the link nurses, who shared their respective unit-specific data along with monthly hand hygiene and CI compliance. In addition, unit-specific HCA-MRSA was communicated directly to the link nurse and nurse manager each week as identified by Clinical Epidemiology. Link nurses would then reeducate staff on the importance of hand hygiene, CI, and aseptic precautions through poster boards and staff meetings.
Incentive system
Lunch was provided to the link nurses during the monthly meetings. A graduate student was hired and trained by Clinical Epidemiology to perform additional hand hygiene audits on each PCU to objectively assess hand hygiene and identify a best performing unit each month. A winning (best performing) unit was selected monthly using a 3-strike method with only 3 audits performed on each unit by the graduate student. A unit was declared as the winner if that unit has passed all 3 audits. If multiple units passed the 3 audits, the process was repeated until only 1 unit could be identified as the winner in each hospital. An incentive in the form of a lunch or dinner was provided for the entire PCU during 1 shift. A commemorative plaque stating the unit’s success was awarded to the winning units at the Supervisory Council (attended by hospital managers and administrative leadership) and is displayed in their nursing station. Recognition plaques rotate through the winning units each month.
Funding
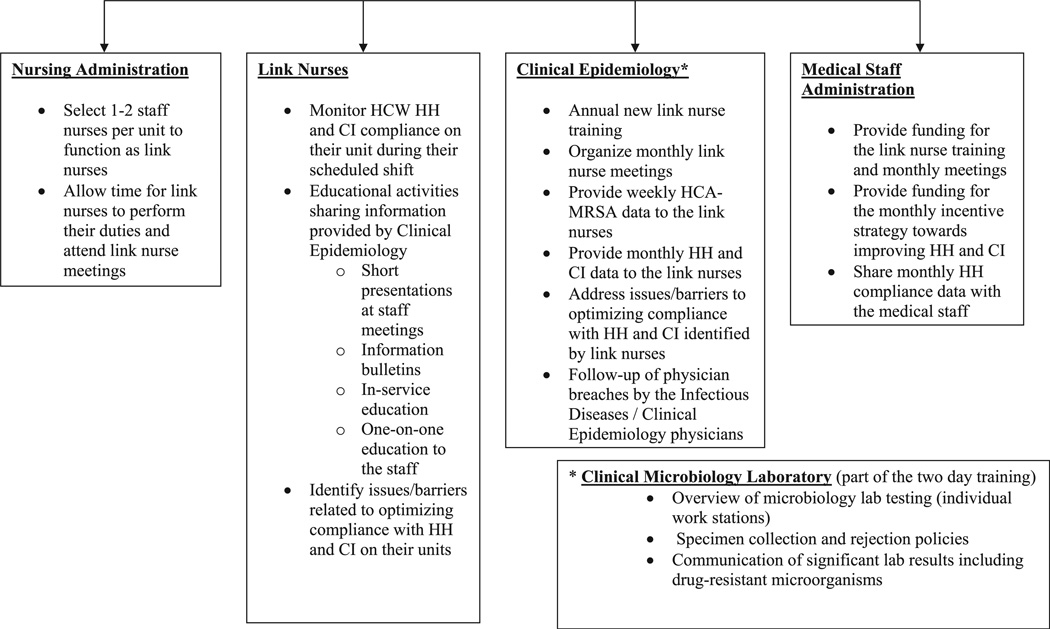
In addition to the 4-hour commitment for each link nurse per month to carry out the activities, our hospital leadership provided $10,000 in funding. This facilitated additional link nurse training sessions (as needed) and supported the graduate student for conducting and collating objective audits for the incentive program and the incentives to the link nurses. Funding has subsequently been renewed as a budget line item in the Clinical Epidemiology annual budget. The role of the multidisciplinary team members in the Link Nurse Program is described in Figure 1.
Fig. 1.
Multidisciplinary team: responsibilities of team members related to Link Nurse Program. HCW, Health care worker; HH, hand hygiene; CI, contact isolation.
Outcome measures and study hypotheses
The primary study hypothesis was that the HCA-MRSA incidence can be reduced by initiating a liaison program focusing on IP increasing hand hygiene participation as measured by direct observation of hand hygiene behavior and the volume of hand soap and alcohol-based hand rub used on the units. The primary outcome measure was HCA-MRSA incidence per 1,000 patient-days (PD). HCA-MRSA was defined as MRSA cultured for the first time on or after hospital day (HD) 4, with HD1 being the day of admission, in a patient who did not have a past history of MRSA infection nor colonization. MRSA cultured before HD 4 and those cultured after HD 4 in a patient with a history of MRSA infection or colonization was categorized as non-HCA-MRSA. MRSA rates were based only on clinical cultures. MRSA screening cultures (assessing for colonization) were not included in the rates. The secondary outcome measures are the total MRSA incidence rate, non-HCA-MRSA incidence rate, total MRSA bacteremia incidence rate, HCA-MRSA bacteremia incidence rate, non-HCA-MRSA bacteremia incidence rate, and, last, hand soap/sanitizer use per month and hand hygiene compliance.
Statistical analysis
As used in previous studies,13 a Poisson regression analysis was used to generate an incidence rate ratio (IRR) compared with baseline MRSA rates. The association between the HCA-MRSA rate and soap/sanitizer use was summarized using the Pearson correlation coefficient. This was performed to assess whether the improvement in MRSA rates could be related to improvement in hand hygiene. Any obvious outliers were to be excluded based on the quarterly data (StataCorp, 2007, version 10; College Station, TX).
RESULTS
Reduction in MRSA incidence
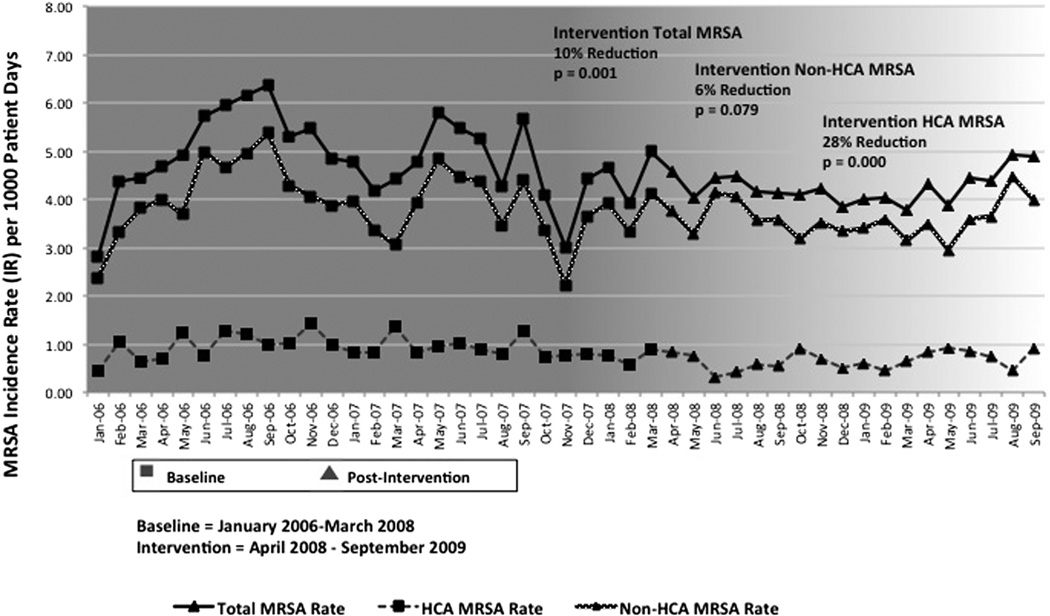
There were 0.92 HCA-MRSA cases per 1,000 PD (639 cases of HCA-MRSA in 692,738 PD) in the baseline (Table 1). The overall HCA-MRSA rate decreased by 28% to 0.67 cases per 1,000 PD (318 cases in 477,567 PD) with IRR of 0.72 (95% confidence interval: 0.62–0.83, P < .001). The total MRSA rate decreased from 4.83 to 4.25 per 1,000 PD (2,031 cases in 477,567 PD); the IRR was 0.90 (95% confidence interval: 0.85–0.95, P = .001) (Table 1, Fig 2). The HCA-MRSA bacteremia rate decreased from 0.18 to 0.10 per 1,000 PD (50 cases in 477,567 PD); the IRR was 0.59 (95% confidence interval: 0.42–0.84, P = .003) with 41% reduction compared with the baseline. The total MRSA bacteremia rate dropped from 0.49 to 0.34 per 1,000 PD (161 cases in 477,567 PD); the IRR was 0.68 (95% confidence interval: 0.56–0.84, P <.001) (Table 1). The overall non-HCA-MRSA rate decreased by 6% from 3.91 to 3.59 cases per 1,000 PD with IRR of 0.94 (95% confidence interval: 0.88–1.01, P = .079) (Table 2). Non-HCA-MRSA bacteremia decreased from 0.37 to 0.23 cases per 1,000 PD with IRR of 0.74 (95% confidence interval: 0.58–0.94, P = .015) (Table 1).
Table 1.
MRSA rate per 1,000 patient-days and incidence rate ratio in the intervention period compared with baseline period
| Surveillance period | No. of MRSA cases | Patient-days | MRSA rate/1,000 patient-days | IRR (95% CI) | Percentage reduction (95% CI) | P value | |
|---|---|---|---|---|---|---|---|
| Total MRSA | Baseline | 3,347 | 692,738 | 4.83 | - | - | - |
| Intervention | 2,031 | 477,567 | 4.25 | 0.90 (0.85–0.95) | 10 (5–15) | .001 | |
| HCA-MRSA | Baseline | 639 | 692,738 | 0.92 | - | - | - |
| Intervention | 318 | 477,567 | 0.67 | 0.72 (0.62–0.83) | 28 (17–28) | < .001 | |
| Non-HCA-MRSA | Baseline | 2,708 | 692,738 | 3.91 | - | - | - |
| Intervention | 1,713 | 477,567 | 3.59 | 0.94 (0.88–1.01) | 6 | .079 | |
| Total blood MRSA | Baseline | 342 | 692,738 | 0.49 | - | - | - |
| Intervention | 161 | 477,567 | 0.34 | 0.68 (0.56–0.84) | 32 (16–44) | < .001 | |
| Blood HCA-MRSA | Baseline | 125 | 692,738 | 0.18 | - | - | - |
| Intervention | 50 | 477,567 | 0.10 | 0.59 (0.42–0.84) | 41 (16–58) | .003 | |
| Blood non-HCA-MRSA | Baseline | 217 | 692,738 | 0.37 | - | - | - |
| Intervention | 111 | 477,567 | 0.23 | 0.74 (0.58–0.94) | 26 (6–42) | .015 |
CI, confidence interval; HCA, health care acquired; IRR, incidence rate ratio; MRSA, methicillin-resistant Staphylococcus aureus.
Fig. 2.
MRSA incidence rate (IR) per 1,000 patient-days.
Table 2.
Hand soap and sanitizer usage in the intervention period compared with baseline period
| Surveillance period |
Soap and hand sanitizer usage |
Standard deviation (range) |
P value |
|
|---|---|---|---|---|
| Monthly mean of soap and hand sanitizer usage | Baseline | 19,301 | 5,559 (2,232–27,000) | - |
| Intervention | 31,794 | 6,962 (20,354–47,245) | < .001 |
Mean monthly soap use was 19,301 ounces (standard deviation, 5,559 [range, 2,232–27,000]) before intervention and was 31,794 (standard deviation, 6,962 [range, 20,354–47,245]) after intervention (P < .001) (Table 2). There was a highly negative correlation between the quarterly average infection rate and the quarterly soap use (r = −0.76, P = .003).
Compliance with hand hygiene and CI precautions
We found that compliance with hand hygiene gradually increased from30% in 6months prior to the intervention to 93% in the 6 months after starting the intervention per audits performed by the units’ administrative personnel and/or link nurses. It stayed above 90% throughout the study period. We measured compliance with CI precautions (wearing gown and gloves upon entry into patient’s room) during our intervention period; the compliance was 80% per audits performed by the link nurses during the first 6 months of measurement, which then increased to over 90% and remained stable throughout the study period.
Cost avoidance
Using the mean attributable cost for MRSA infections ($35,367 per case) published9 in 2003 and methods previously used,10 we calculated the cost avoidance achieved by the Link Nurse Program during the study period. The number of HCA-MRSA cases for intervention period was projected using the rate from baseline period and period’s actual PDs. This projection was used to determine the prevented HCA-MRSA cases and therefore cost avoided. Using these calculations, we projected that the number of HCA-MRSA cases for the intervention period was 441, and we calculated that the number of infections avoided over the 2-year period was 198 with an avoided cost of $7,002,666.
DISCUSSION
Effective IP programs require the commitment of adequate resources and clear lines of communication among different layers within the health care structure. Strong support from hospital administration is crucial for the success of such programs as is buy-in and involvement of grass roots staff. We describe the development of an IP program that utilized a multidisciplinary team that worked toward engaging all HCW in IP. Our goal was to increase hand hygiene compliance and thereby decrease HCA-MRSA by developing a multidisciplinary team that engages all HCW in IP on each PCU.
Our medical center had an infection preventionist to patient bed ratio of 1:250. The Link Nurse Program, with intense training and ongoing monthly meetings, provided a workable solution to spread human resources and expertise across a variety of PCUs to support and reinforce our IP efforts. Clinical Epidemiology and Clinical Microbiology collaborated to create an ongoing link nurse curriculum and program. Support and input was obtained from nursing and medical leadership. We specifically targeted hand hygiene, CI, and HCA-MRSA in our monthly meetings by providing unit-specific data pertaining to these measures. Link nurses shared these data at their monthly staff meetings.
We demonstrated that the HCA-MRSA rates have significantly decreased since the initiation of our link nurse program (Fig 2).We have also assessed the non-HCA-MRSA rates and total MRSA rates during these time periods to align outcomes. Such a decrease in non-HCA-MRSA might imply that the decrease in HCA-MRSA may have been the result of decreasing burden of MRSA independent of this intervention. Instead, we demonstrated that there was no significant reduction in non-HCA-MRSA, whereas there were significant reductions in HCA-MRSA and total MRSA rates in the intervention period compared with the baseline (Fig 2). This strongly supports our conclusion that our link nurse program led to a significant reduction in HCA-MRSA rates in our medical center. Similarly, we demonstrated a statistically significant reduction in HCA and total MRSA bloodstream infection rates.
We demonstrated a correlation between our increasing hand sanitizer and soap use and the decreasing HCA-MRSA rates during our intervention period when the Link Nurse Program was implemented. One of the expected benefits of this program was in engaging HCW in IP and getting them excited about patient outcomes while drawing their attention to HCA infections. We have not measured the intensity of the HCW engagement, but we have observed an increase in HCW participation in IP-related activities. There were increased questions from staff about hand hygiene compliance, MRSA, infections in general, CI procedures, and unit-specific challenges toward reaching the goals. It should be understood that well-trained liaisons of IP belonging to individual PCUs can provide consistent presence and guidance to the hospital staff in real time on their own units.
Even though unit-level champions were described in some other studies, the size of our health care system, the diversity among the 5 hospitals with regard to patient populations, and the success and sustenance of the program despite all these differences make our program unique. Our Link Nurse Program has become an integral part of our institution with ongoing monthly meetings with multidisciplinary aspects of a topic being addressed at each meeting. It is regarded as one of the most successful programs in our hospitals and is a remarkable achievement in IP efforts. We continue to monitor hand hygiene and HCA-MRSA, which has been stable beyond the study period.
We have identified key elements of the program that we believe have contributed to the success and sustainability of the program. First, developing such a program required meticulous planning with prior approval from nursing and medical administration from all hospitals. This gave us an opportunity to engage hospital management in our attempt to engage HCW in IP activities. They not only provided moral support and agreed to implement this program but also provided financial support. Support came in the form of annual funding as described in the Methods section in addition to the nursing time allotted for the link nurse activities. We believe this support was crucial to our success. Second, we rigorously trained our link nurses with 16-hour training sessions and continued to reinforce their training with monthly meetings. We believe that this rigorous and committed approach to the training of link nurses ensured that they were comfortable in tackling IP activities and secured their commitment to the program. We religiously provided feedback on hand hygiene, CI, and HCA-MRSA at monthly meetings to encourage their commitment to the program. Third, we ensured that the link nurses shared the data at their monthly staff meetings. This guaranteed that the IP data actually reached the staff. Fourth, we addressed every process gap identified by the HCWs and brought forth by the link nurses and shared the end results in monthly meetings. We believe this has garnered credibility for the program and led to our success. Last, continued dialogue with nursing and medical leadership about the progress of the program with updates and status reports helped us to keep the hospital administration engaged. Even though this effort was initiated by Clinical Epidemiology, the multidisciplinary involvement of other departments such as Clinical Microbiology and Nursing in the planning and implementation worked well for this program.
We also encountered certain challenges. The large size of our health care system and the diversity of our hospitals posed a challenge. Clinical Epidemiology obtained support from the individual nursing leaders at each of these hospitals, who were engaged from the beginning. This approach helped us overcome local obstacles within the hospitals. Another challenge was maintaining the interest of link nurses over long periods of time. We addressed this by making the sessions interactive, by dividing link nurses into small groups for a part of every monthly meeting, by pairing small groups of link nurses with infection preventionists for one-on-one sessions, by organizing lectures based on the interests of link nurses, and by providing regular, monthly feedback on their unit-specific performance. Our infection preventionists also developed an ongoing working relationship with their link nurses and approached them with questions and any issues originating from their PCUs. Maintaining credibility for the program is a challenging task. We achieved this by addressing every question or issue brought up by the link nurses. We shared the experience with the group to facilitate group learning from individual experiences. Clinical Epidemiology maintains ownership of the data feedback, conduct of the training sessions and monthly meetings, and addressing the issues suggested by the link nurses.
Previous descriptions of link nurse programs acknowledge operational difficulties such as high turnover of staff, insufficient time for training, and monitoring their effectiveness.30,31 We have aggressively trained our link nurses, monitored their units’ performance, and provided feedback. We believe this can be achieved in any health care system. High turnover of staff is a challenge for our program. We addressed that by actively seeking new link nurses as soon as the position became vacant. Support from nursing administration was extremely important to achieve rapid recruitment into the vacant positions. We ensured that the newly recruited link nurses were trained at the next available 16-hour training session. We have tied the Link Nurse Program to the Clinical Ladder Program, which provides an opportunity for the staff nurses to advance their careers. Another challenge worth discussing is the cost associated with the program. The cost avoidance of over 7 million dollars was achieved through the Link Nurse Program, which is well worth the effort, and the cost associated with training, alcohol-based hand sanitizer, or soap.
Our study is not without its limitations. We chose our current study design akin to studies such as ours.13,15 With our study design, simultaneous IP interventions could not be assessed as in a randomized controlled trial. Randomization was not feasible because the intervention was a hospital-wide study among a small group of hospitals that shared physicians and other hospital staff. Behavioral changes associated with IP practices cannot be contained in the participating units when staff is shared between PCUs and hospitals. The ethical acceptability of control groups in situations perceived as threatening to patients (HCA-MRSA transmission rates) was another obstacle as described in another study.13 We did not measure the increase in HCW knowledge related to hospital-acquired infection prevention. However, our goal was to successfully implement this multidisciplinary program and show an increase in hand hygiene participation and a reduction in our HCA-MRSA rates. Clear increases in hand soap/sanitizer consumption and hand hygiene compliance with direct correlation to reduction in HCA-MRSA transpired with no changes in additional beds in the health system. No other changes in IP such as addition of hand hygiene dispensers were ongoing during this study period. The only other initiative ongoing was a central line-associated bloodstream infection reduction initiative in a 19-bed, medical-surgical intensive care unit at our 200-bed University East Hospital. We also did not measure the impact of this program on HCA infections because of other multidrug-resistant organisms. Our audits were conducted by internal administrative personnel on the respective PCUs, which may raise questions about the objectivity of the audits, but we have shown an increase in hand hygiene compliance using the same method and an increase in hand sanitizer/soap use with a decrease in HCA-MRSA rates.
In conclusion, Link Nurse Program resulted in reduced HCA-MRSA incidence by increasing hand hygiene participation. Effective IP programs require the commitment of adequate resources and clear lines of communication among different layers within the health care structure. A multidisciplinary link nurse program engaging both hospital administration and grass roots staff in preventing infections may prove of value in preventing HCA infections in other facilities. This program “extends” the number of personnel to assist in engaging all HCW in IP activities every day. Strong support from hospital administration was crucial for our success, as was accountability, buy in, and involvement of the unit-based staff.
Acknowledgment
The authors thank all link nurses for their commitment and contribution to the program.
Supported by Clinical and Translational Science Awards (CTSA) Program for Biostatistical support and, in part, by the United States National Center for Advancing Translational Sciences (8UL1TR000090-05; to X.P.).
J.E. Mangino has served on an advisory board for Cepheid and has received research grants from Merck and Co and Medline Industries.
Footnotes
The Ohio State University Wexner Medical Center’s Link Nurse Program was awarded one of four honorable mentions for partnership in infection prevention at the Fifth Decennial International Conference on Healthcare-Associated Infections, 2010.
Preliminary findings were previously reported by M.M. Sopirala, L. Fawley, D. Taylor, L. Wellington, P. Kulich, J. Dickman, and J. E. Mangino. OSUMC Infection Control Link Nurse Program. Society for Healthcare Epidemiology of America (SHEA) 19th Annual Scientific Meeting; March 19–22, 2009; San Diego, CA.
Conflicts of interest: The remaining authors report no conflicts.
References
- 1.National Healthcare Safety Network (NHSN) report, data summary for 2006 through 2007, issued November 2008. Am J Infect Control. 2008;36:609–626. doi: 10.1016/j.ajic.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003;36:53–59. doi: 10.1086/345476. [DOI] [PubMed] [Google Scholar]
- 3.Blot SI, Vandewoude KH, Hoste EA, Colardyn FA. Outcome and attributable mortality in critically ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus. Arch Intern Med. 2002;162:2229–2235. doi: 10.1001/archinte.162.19.2229. [DOI] [PubMed] [Google Scholar]
- 4.Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y. The impact of methicillin resistance in Staphylococcus aureus bacteremia on patient outcomes: mortality, length of stay, and hospital charges. Infect Control Hosp Epidemiol. 2005;26:166–174. doi: 10.1086/502522. [DOI] [PubMed] [Google Scholar]
- 5.Gould IM. Costs of hospital-acquired methicillin-resistant Staphylococcus aureus (MRSA) and its control. Int J Antimicrob Agents. 2006;28:379–384. doi: 10.1016/j.ijantimicag.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Barnett TE. The not-so-hidden costs of surgical site infections. AORN J. 2007;86:249–258. doi: 10.1016/j.aorn.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173:2039–2046. doi: 10.1001/jamainternmed.2013.9763. [DOI] [PubMed] [Google Scholar]
- 8.Engemann JJ, Carmeli Y, Cosgrove SE, Fowler VG, Bronstein MZ, Trivette SL, et al. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003;36:592–598. doi: 10.1086/367653. [DOI] [PubMed] [Google Scholar]
- 9.Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and Enterococcus. Infect Control Hosp Epidemiol. 2003;24:362–386. doi: 10.1086/502213. [DOI] [PubMed] [Google Scholar]
- 10.Cromer AL, Hutsell SO, Latham SC, Bryant KG, Wacker BB, Smith SA, et al. Impact of implementing a method of feedback and accountability related to contact precautions compliance. Am J Infect Control. 2004;32:451–455. doi: 10.1016/j.ajic.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Medicare and Medicaid Services. Roadmap for implementing value driven healthcare in the traditional Medicare fee-for-service program. [Accessed December 14, 2013]; Available from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/downloads/vbproadmap_oea_1-16_508.pdf.
- 12.Garner JS. Guideline for isolation precautions in hospitals: part I. Evolution of isolation practices. Am J Infect Control. 1996;24:24–31. doi: 10.1016/s0196-6553(96)90050-4. [DOI] [PubMed] [Google Scholar]
- 13.Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet. 2000;356:1307–1312. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 14.Jernigan JA, Titus MG, Gröschel DH, Getchell-White S, Farr BM. Effectiveness of contact isolation during a hospital outbreak of methicillin-resistant Staphylococcus aureus. Am J Epidemiol. 1996;143:496–504. doi: 10.1093/oxfordjournals.aje.a008770. [DOI] [PubMed] [Google Scholar]
- 15.Miyachi H, Furuya H, Umezawa K, Itoh Y, Ohshima T, Miyamoto M, et al. Controlling methicillin-resistant Staphylococcus aureus by stepwise implementation of preventive strategies in a university hospital: impact of a link-nurse system on the basis of multidisciplinary approaches. Am J Infect Control. 2007;35:115–121. doi: 10.1016/j.ajic.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 16.Pittet D, Allegranzi B, Boyce J. World health Organization World Alliance for patient safety first Global patient safety challenge Core group of Experts. The World health Organization guidelines on hand hygiene in health care and their consensus recommendations. Infect Control Hosp Epidemiol. 2009;30:611–622. doi: 10.1086/600379. [DOI] [PubMed] [Google Scholar]
- 17.Kim YC, Kim MH, Song JE, Ahn JY, Oh DH, Kweon OM, et al. Trend of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia in an institution with a high rate of MRSA after the reinforcement of antibiotic stewardship and hand hygiene. Am J Infect Control. 2013;41:e39–e43. doi: 10.1016/j.ajic.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 18.Lederer JW, Jr, Best D, Hendrix V. A comprehensive hand hygiene approach to reducing MRSA health care-associated infections. Jt Comm J Qual Patient Saf. 2009;35:180–185. doi: 10.1016/s1553-7250(09)35024-2. [DOI] [PubMed] [Google Scholar]
- 19.McGuckin M, Waterman R, Portena L, Belloa S, Caruso M, Juzaitis B, et al. Patient education model for increasing handwashing compliance. Am J Infect Control. 1999;27:309–314. doi: 10.1016/s0196-6553(99)70049-0. [DOI] [PubMed] [Google Scholar]
- 20.McGuckin M, Taylor A, Martin V, Porten L, Salcido R. Evaluation of a patient education model for increasing hand hygiene compliance in an inpatient rehabilitation unit. Am J Infect Control. 2004;32:235–238. doi: 10.1016/j.ajic.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 21.McGuckin M, Waterman R, Storr IJ, Bowler IC, Ashby M, Topley K, et al. Evaluation of a patient-empowering hand hygiene programme in the UK. J Hosp Infect. 2001;48:222–227. doi: 10.1053/jhin.2001.0983. [DOI] [PubMed] [Google Scholar]
- 22.Gawande A. On washing hands. N Engl J Med. 2004;350:1283–1286. doi: 10.1056/NEJMp048025. [DOI] [PubMed] [Google Scholar]
- 23.Borg MA, Ben Bachir M, Cookson BD, Redjeb SB, Elnasser Z, Rasslan O, et al. Self-protection as driver for hand hygiene among healthcare workers. Infect Control Hosp Epidemiol. 2009;30:578–580. doi: 10.1086/597511. [DOI] [PubMed] [Google Scholar]
- 24.Borg MA, Ben Bachir M, Cookson BD, Ben Redjeb S, Elnasser Z, Rasslan O, et al. Health care worker perceptions of hand hygiene practices and obstacles in a developing region. Am J Infect Control. 2009;37:855–857. doi: 10.1016/j.ajic.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Souweine B, Lautrette A, Aumeran C, Bénédit M, Constantin JM, Bonnard M, et al. Comparison of acceptability, skin tolerance, and compliance between handwashing and alcohol-based handrub in ICUs: results of a multicentric study. Intensive Care Med. 2009;35:1216–1224. doi: 10.1007/s00134-009-1485-5. [DOI] [PubMed] [Google Scholar]
- 26.Smith SM. A review of hand-washing techniques in primary care and community settings. J Clin Nurs. 2009;18:786–790. doi: 10.1111/j.1365-2702.2008.02546.x. [DOI] [PubMed] [Google Scholar]
- 27.Dierssen-Sotos T, Brugos-Llamazares V, Robles-García M, Rebollo-Rodrigo H, Fariñas-Alvarez C, Antolín-Juarez FM, et al. Evaluating the impact of a hand hygiene campaign on improving adherence. Am J Infect Control. 2010;38:1–4. doi: 10.1016/j.ajic.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 28.Teare EL, Peacock A. The development of an infection control link-nurse programme in a district general hospital. J Hosp Infect. 1996;34:267–278. doi: 10.1016/s0195-6701(96)90107-3. [DOI] [PubMed] [Google Scholar]
- 29.McGuckin M, Shubin A, Hujcs M. Interventional patient hygiene model: Infection control and nursing share responsibility for patient safety. Am J Infect Control. 2008;36:59–62. doi: 10.1016/j.ajic.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 30.Dawson SJ. The role of the infection control link nurse. J Hosp Infect. 2003;54:251–257. doi: 10.1016/s0195-6701(03)00131-2. [DOI] [PubMed] [Google Scholar]
- 31.Seto WH, Yuen SW, Cheung CW, Ching PT, Cowling BJ, Pittet D. Hand hygiene promotion and the participation of infection control link nurses: an effective innovation to overcome campaign fatigue. Am J Infect Control. 2013;41:1281–1283. doi: 10.1016/j.ajic.2013.04.011. [DOI] [PubMed] [Google Scholar]