Supplemental Digital Content is Available in the Text.
Magnetic resonance imaging (MRI) without clear indications led to a cascade of subsequent diagnostic and invasive services, which occurred within 6 months after imaging. Early MRI was significantly associated with a large and sustained escalation in medical costs, even after grouping by severity and controlling for pain and demographic covariates.
Keywords: low back pain, radiculopathy, nonspecific back pain, evidence-based guidelines, MRI, workers' compensation, costs
Abstract
Study Design.
Retrospective cohort study.
Objective.
To compare type, timing, and longitudinal medical costs incurred after adherent versus nonadherent magnetic resonance imaging (MRI) for work-related low back pain.
Summary of Background Data.
Guidelines advise against MRI for acute uncomplicated low back pain, but is an option for persistent radicular pain after a trial of conservative care. Yet, MRI has become frequent and often nonadherent. Few studies have documented the nature and impact of medical services (including type and timing) initiated by nonadherent MRI.
Methods.
A longitudinal, workers' compensation administrative data source was accessed to select low back pain claims filed between January 1, 2006 and December 31, 2006. Cases were grouped by MRI timing (early, timely, no MRI) and subgrouped by severity (“less severe,” “more severe”) (final cohort = 3022). Health care utilization for each subgroup was evaluated at 3, 6, 9, and 12 months post-MRI. Multivariate logistic regression models examined risk of receiving subsequent diagnostic studies and/or treatments, adjusting for pain indicators and demographic covariates.
Results.
The adjusted relative risks for MRI group cases to receive electromyography, nerve conduction testing, advanced imaging, injections, and surgery within 6 months post-MRI risks in the range from 6.5 (95% CI: 2.20–19.09) to 54.9 (95% CI: 22.12–136.21) times the rate for the referent group (no MRI less severe). The timely and early MRI less severe subgroups had similar adjusted relative risks to receive most services. The early MRI more severe subgroup cases had generally higher adjusted relative risks than timely MRI more severe subgroup cases. Medical costs for both early MRI subgroups were highest and increased the most over time.
Conclusion.
The impact of nonadherent MRI includes a wide variety of expensive and potentially unnecessary services, and occurs relatively soon post-MRI. Study results provide evidence to promote provider and patient conversations to help patients choose care that is based on evidence, free from harm, less costly, and truly necessary.
Level of Evidence: N/A
A cascade effect in medical care refers to “a chain of events initiated by an unnecessary test...which results in ill-advised tests or treatments that may cause avoidable adverse effects and/or morbidity”1 and is well documented across several specialties of medical care. Electronic fetal monitoring has been associated with a 40% higher Cesarean section rate, without fetal outcome improvement.2 Unnecessary cardiac stress tests generating false-positive results lead to significant morbidity and mortality due to unnecessary invasive testing and surgery.3
Radiological lumbar imaging is also problematic as it frequently reveals “abnormalities” of uncertain clinical significance similar to those seen in asymptomatic individuals.4 Magnetic resonance imaging (MRI) has become more frequent as it has no radiation exposure risk,5,6 and is problematic because it is highly sensitive but often not specific in identifying the cause of back pain.7–9
Evidence-based acute low back pain (LBP) guidelines recommend against routine MRI, except for “red flag” conditions (severe trauma, infection, cancer, cauda equina syndrome). MRI is an option to guide epidural steroid injections or surgery for persistent radicular pain after a trial of conservative care.10,11
Guideline recommendations are intended to avoid subsequent unnecessary and iatrogenic care, yet there is little information to document the extent and timing of unnecessary or nonindicated medical services after nonadherent MRI. Services received post-MRI have been documented in a few studies, but none have assessed their type and timing.12–18
The study purpose was to compare the nature, timing, and associated longitudinal costs of post-MRI medical services in persons receiving early MRI with those who never had MRI or had MRI after a trial of conservative care, using a health services data set. It was hypothesized that rates and costs of post-MRI diagnostic and/or invasive services would be higher in patients who had early MRI than for those who never had MRI or who had MRI after a trial of conservative care, after grouping by severity and controlling for pain indicators and demographic factors.
MATERIALS AND METHODS
Subjects
As previously described,12 all accepted LBP claims filed between January 1, 2006 and December 31, 2006 were extracted from a nationally representative United States workers' compensation (WC) administrative data source (representing approximately 10% of the private WC market). Data extracted for a 2-year period from the date of LBP onset, included age, sex, job tenure, paid medical bills, and associated Clinical Procedural Terminology codes,19 and International Classification of Diseases, Ninth Revision diagnostic codes assigned to services provided within 15 days postonset.20 Inclusion criteria included at least 1 day compensated lost time and at least 1 year of job tenure. Complex cases (those with red-flag conditions, non-LBP diagnoses, or multiple injuries) and cases with a LBP claim within the prior year were excluded, yielding a cohort of 3253. The study was approved by the Institutional Review Board of the Liberty Mutual Research Institute for Safety.
Exposure
To compare services received after the initial lumbar MRI (based on Clinical Procedural Terminology codes 72148, 72149, and 72158) with those without MRI, 3 groups were specified according to the timing of the MRI.19 “No MRI” cases received no MRI during the 2-year study period. “Early MRI” cases received MRI within the first 30 days.12 Because various guidelines recommend different timeframes (from 4 wk21 to 6 wk22) before obtaining MRI to evaluate patients with persistent radicular back pain or spinal stenosis, “timely MRI” group was defined as those who received MRI starting at 42 days postonset through 180 days (to exclude the few cases whose imaging was delayed for either complicating medical or nonmedical reasons). On the basis of these definitions, 231 cases were excluded for MRI that fell outside of the specified periods (170 from 31 to 41 d postonset, 61 after 180 d postonset), resulting in a final cohort of 3022 from 48 states.
Within each group, cases were classified into “more severe” and “less severe” subgroups based on International Classification of Diseases, Ninth Revision codes, to evaluate whether severity affected utilization. The more severe subgroup included those who received any services with diagnoses including herniated disc, lumbar radiculopathy or neuropathy, spinal stenosis, sciatica, or possible instability. Remaining cases assigned to the less severe subgroup had diagnostic codes associated with degenerative changes, nonspecific back pain, or miscellaneous diagnoses (Supplemental Digital Content, Table 1 available at http://links.lww.com/BRS/A872).
Outcomes and Follow-up
For each subgroup, the occurrence of services received post-MRI was identified using Clinical Procedural Terminology codes and based on the first receipt of diagnostic studies (electromyography, nerve conduction velocity, and advanced imaging) and/or invasive treatments (injections and surgery) (Supplemental Digital Content, Table 2 available at http://links.lww.com/BRS/A872). Advanced imaging included myelography, discography, computed tomography, bone scan, and repeat MRI. Injections included epidural, facet and sacroiliac joint, and trigger point injections. Surgery included lumbar discectomy, laminectomy, and fusions.
Health care utilization for each MRI subgroup was evaluated at 3, 6, 9, and 12 months post-MRI. A comparable post-MRI follow-up period for the no MRI group was defined as starting at 15 days (median days to MRI for early MRI group) postonset.
Total medical costs, based on paid medical bills, were computed for each subgroup. Costs for the pre-MRI periods were aggregated from date of onset to the first 14 days for the no MRI groups, up to 30 days postonset for the early MRI groups, and between 42 and 180 days for the timely MRI groups. Post-MRI costs were aggregated from the day after MRI (or the 16th day for the no MRI groups) to the 3-, 6-, 9-, and 12-month follow-up dates. All totals exclude MRI costs.
Covariates
Because higher opioid usage has been shown to be associated with higher medical costs and an increased risk to undergo subsequent surgery,23 we adjusted for individual differences in pain indicators. Early opioid use (receipt of opioid analgesics within 15 days postonset) and the associated total morphine-equivalent amount (MEA) were used as surrogates for pain. Morphine-equivalent amount was calculated on the basis of the number of pills, strength, and equianalgesic dose.23 Demographic covariates included age, sex, and job tenure.
Statistical Analysis
To examine services received post-MRI and compare outcomes of the early and timely MRI groups to the no MRI groups for comparable periods, the percentage of cases within each MRI subgroup who received each category of services at 3-month intervals up to a year post-MRI was first examined. Next, multivariate log binomial regression was used to model the relative risk (risk ratio) of receiving a category of service for each MRI subgroup. Repeated measures analysis of variance was used to compare medical expenditures across time for each MRI group (Figure 1). Analysis of variances and pairwise comparisons were used to compare the MRI groups on their demographic and pain characteristics. All models adjusted for these potential covariates. SAS software, version 9.2 (SAS Institute Inc., Cary, NC) was used for all analyses.
Figure 1.
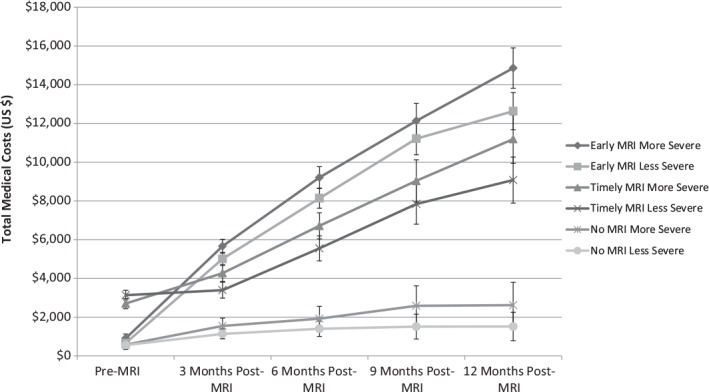
Total medical costs over time by MRI diagnostic group. MRI indicates magnetic resonance imaging.
RESULTS
Table 1 presents descriptive statistics on the demographic and pain covariates for each MRI subgroup. More than 80% of the more severe subgroups had an early diagnosis of radiculopathy (data not shown). All MRI groups had higher percentages of those who received early opioids. Both early MRI groups had the highest MEA levels in the first 15 days. The timely MRI less severe subgroup received MRI significantly sooner than the timely MRI more severe subgroup (by an average of 11 d).
TABLE 1. Descriptive Statistics for Demographics and Covariates.
| MRI Groups by Severity | Demographics | Covariates | ||||
|---|---|---|---|---|---|---|
| Age, yr | Sex, Female % | Tenure, yr | Early Opioid, % | MEA in First 15 d,* mg | Time to First Lumbar MRI, d | |
| No MRI less severe (n = 1546) | 40.7 (40.1–41.3) | 31.0 | 6.8 (6.5–7.2) | 22.5 | 316.6 (274.8–358.3) | ... |
| No MRI more severe (n = 271) | 41.9 (40.6–43.1) | 33.9 | 7.8 (6.8–8.8) | 21.8 | 416.8 (253.1–580.6) | ... |
| Timely MRI less severe (n = 214) | 39.9 (38.5–41.3) | 34.1 | 6.7 (5.7–7.6) | 38.8 | 352 (289.7–414.3) | 69.7 (66.0–73.5) |
| Timely MRI more severe (n = 209) | 42.8 (41.4–44.2) | 38.3 | 7.7 (6.5–8.8) | 28.2 | 377.5 (276.5–478.4) | 81.0 (76.0–86.1) |
| Early MRI less severe (n = 458) | 42.1 (41.2–43.0) | 24.7 | 7.9 (7.2–8.6) | 34.1 | 523.5 (407.9–639.2) | 14.8 (14.0–15.6) |
| Early MRI more severe (n = 324) | 42.4 (41.4–43.5) | 22.2 | 7.9 (7.1–8.8) | 42.0 | 529.2 (436.0–622.4) | 16.3 (15.5–17.2) |
Data represent means with 95% confidence intervals in parentheses.
*Means for MEA (morphine-equivalent amount) in first 15 days are calculated only for those with opioid prescriptions.
MRI indicates magnetic resonance imaging.
The majority of services were received relatively soon post-MRI. Most of those who received injections, nerve testing, or surgery, and about half who received advanced imaging by the 6-month period received these services within the first 3 months post-MRI (Table 2). Therefore, we focused on modeling the risk ratios for services at 6 months post-MRI. Model results for outcomes at 3, 9, and 12 months post-MRI were similar (data not shown).
TABLE 2. Descriptive Outcomes Post-MRI.
| MRI Groups by Severity | Injection | EMG/NCV | Advanced Imaging | Surgery | ||||
|---|---|---|---|---|---|---|---|---|
| 3 mo, % | 6 mo, % | 3 mo, % | 6 mo, % | 3 mo, % | 6 mo, % | 3 mo, % | 6 mo, % | |
| No MRI less severe (n = 1546) | 1.0 | 1.4 | 0.1 | 0.3 | 0.6 | 0.8 | 0.2 | 0.5 |
| No MRI more severe (n = 271) | 2.6 | 3.7 | 1.5 | 1.5 | 0.4 | 0.4 | 0.7 | 0.7 |
| Timely MRI less severe (n = 214) | 25.2 | 35.5 | 6.1 | 11.2 | 7.0 | 13.1 | 0.9 | 2.8 |
| Timely MRI more severe (n = 209) | 27.8 | 36.8 | 9.6 | 13.9 | 5.3 | 10.0 | 5.3 | 8.6 |
| Early MRI less severe (n = 458) | 33.0 | 38.9 | 8.1 | 12.2 | 7.6 | 14.4 | 8.1 | 13.3 |
| Early MRI more severe (n = 324) | 36.7 | 46.6 | 13.9 | 17.6 | 8.6 | 17.0 | 10.2 | 16.0 |
Percentages represent the frequency of the first receipt of these outcomes post-MRI within each MRI diagnostic group. Injections include injections of the epidural space, facet and sacroiliac joints, and trigger points. Advanced imaging includes myelography, discography, CT scans, bone scans, and repeat MRIs. Surgery includes lumbar discectomy, laminectomy, and fusions.
MRI indicates magnetic resonance imaging; CT, computed tomography; EMG/NCV, electromyography/nerve conduction velocity.
Risk ratios to receive diagnostic services and invasive treatments at 6 months post-MRI were highest for the early MRI groups, ranging between 17.8 and 54.9 times as likely as the referent group (no MRI less severe), after adjusting for demographic and pain covariates (Table 3). Adjusted relative risks for the timely MRI subgroups were similarly high, ranging between 6.5 and 42.8 times as likely as the referent group. Comparisons of the MRI subgroups (within severity levels) showed that the risk ratios for receiving these services for the early and timely MRI groups were significantly higher than for the no MRI group. Relative risks for receipt of surgery and injections at 6 months post-MRI for the early MRI subgroups were higher than the timely MRI subgroups (Table 4). There was moderate variation in the risk ratios to receive services due to severity within MRI groups (Supplemental Digital Content, Table 3 available at http://links.lww.com/BRS/A872).
TABLE 3. Adjusted Multivariate Log Binomial Model Results at 6 Months Post-MRI.
| MRI Groups by Severity | Injections | EMG/NCV | Advanced Imaging | Surgery | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | Wald 95% CI | P | RR | Wald 95% CI | P | RR | Wald 95% CI | P | RR | Wald 95% CI | P | |
| No MRI more severe (n = 271) | 2.70 | 1.29–5.67 | 0.009 | 4.59 | 1.24–16.98 | 0.023 | 0.48 | 0.06–3.66 | 0.48 | 1.64 | 0.34–7.83 | 0.54 |
| Timely MRI less severe (n = 214) | 25.17 | 15.86–39.95 | 0.001 | 35.13 | 13.53–91.22 | 0.001 | 16.60 | 8.56–32.18 | 0.001 | 6.48 | 2.20–19.09 | 0.001 |
| Timely MRI more severe (n = 209) | 26.24 | 16.56–41.58 | 0.001 | 42.77 | 16.73–109.36 | 0.001 | 13.04 | 6.51–26.11 | 0.001 | 20.07 | 8.49–47.46 | 0.001 |
| Early MRI less severe (n = 458) | 27.40 | 17.64–42.57 | 0.001 | 38.08 | 15.33–94.59 | 0.001 | 17.81 | 9.70–32.71 | 0.001 | 28.35 | 13.05–61.58 | 0.001 |
| Early MRI more severe (n = 324) | 32.70 | 21.03–50.84 | 0.001 | 54.89 | 22.12–136.21 | 0.001 | 20.53 | 11.08–38.01 | 0.001 | 33.80 | 15.46–73.87 | 0.001 |
| No MRI less severe (n = 1546) | Ref. | Ref. | Ref. | Ref. | ||||||||
Ref = no MRI less severe. Estimates of risk ratios (relative risk) adjusted for age, sex, job tenure, and use of early opioids.
MRI indicates magnetic resonance imaging; EMG/NCV, electromyography/nerve conduction velocity; RR, relative risk; 95% CI, 95% confidence interval; Ref, Reference group.
TABLE 4. Comparisons Across MRI Groups (Within Severity) at 6 Months Post-MRI.
| Injections | EMG/NCV | Advanced Imaging | Surgery | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | Wald 95% CI | P | RR | Wald 95% CI | P | RR | Wald 95% CI | P | RR | Wald 95% CI | P | |
| Less severe | ||||||||||||
| Early MRI vs. no MRI (ref.) | 27.40 | 17.64–42.57 | 0.001 | 38.08 | 15.33–94.58 | 0.001 | 17.81 | 9.70–32.71 | 0.001 | 28.35 | 13.05, 61.58 | 0.001 |
| Timely MRI vs. no MRI (ref.) | 25.17 | 15.86–39.95 | 0.001 | 35.13 | 13.53–91.22 | 0.001 | 16.60 | 8.56–32.18 | 0.001 | 6.48 | 2.20–19.09 | 0.001 |
| Early MRI vs. timely MRI (ref.) | 1.09 | 0.88–1.35 | 0.43 | 1.08 | 0.69–1.70 | 0.73 | 1.07 | 0.71–1.62 | 0.74 | 4.38 | 1.92–9.96 | 0.001 |
| More severe | ||||||||||||
| Early MRI vs. no MRI (ref.) | 12.10 | 6.51–22.49 | 0.001 | 11.97 | 4.93–32.63 | 0.001 | 42.99 | 5.98–308.95 | 0.001 | 20.67 | 5.08, 84.14 | 0.001 |
| Timely MRI vs. no MRI (ref.) | 9.71 | 5.16–18.30 | 0.001 | 9.32 | 3.33–26.11 | 0.001 | 27.31 | 3.70–201.33 | 0.001 | 12.28 | 2.88–52.26 | 0.001 |
| Early MRI vs. timely MRI (ref.) | 1.25 | 1.01–1.54 | 0.04 | 1.28 | 0.85–1.95 | 0.24 | 1.57 | 0.98–2.53 | 0.06 | 1.68 | 1.01–2.80 | 0.04 |
Multivariate log binomial model results comparing across MRI groups within severity. Estimates of risk ratios (relative risk) adjusted for age, sex, job tenure, and use of early opioids.
MRI indicates magnetic resonance imaging; EMG/NCV, electromyography/nerve conduction velocity; ref., reference group; RR, relative risk; 95% CI, 95% confidence interval.
Medical costs (excluding MRI costs) for the early MRI groups were highest and increased the most over time. Costs for the timely MRI groups were second highest, whereas the no MRI groups had a much lower rate of cost increase over time (Figure 1).
DISCUSSION
In this longitudinal study, lumbar MRI without indication led to a subsequent cascade of diagnostic and therapeutic services (including surgery), which generally occurred soon after MRI. This cascade was more related to MRI than to severity or pain indicators, suggesting an effect of guideline nonadherence. Even after grouping by severity and controlling for pain and demographic covariates, early MRI was significantly associated with a large and sustained medical cost escalation, reflecting an overall medical utilization increase, which was greater than seen for the no MRI and timely groups.
This study is the first to assess post-MRI services after a trial of conservative care (timely MRI) and to assess the financial impact of services after guideline-adherent conservative care, including the timing, type of services, and costs over time, after grouping by severity and controlling for covariates. This study also provides more detail than other studies regarding services received post-MRI.12,14–18 A recent study of WC claimants in Washington State found a similar increased likelihood to receive injections and surgery and incur higher medical costs after nonadherent early MRI, but did not assess services or costs incurred after timely MRI.18 The associated increased surgery risk for both the early and timely less severe subgroups supports similar findings in primary care and Medicare populations.14,15 Early MRI has also been associated with prolonged disability, even after controlling for potential confounders.12,17 Another study found little change in services associated with early MRI, but patients' sense of well-being decreased after receiving imaging results.24
The findings are troublesome because cases were selected on the basis of the absence of red-flag indications that might warrant early MRI. Although MRI may be considered for persistent radicular pain after a course of conservative care to guide epidural steroid injection or surgery for radiculopathy,11 the timely MRI less severe subgroup was unlikely to have radiculopathy and was unlikely to have indications for many of the subsequent services. However, their receipt of services was similar to the timely more severe subgroup, suggesting unnecessary and costly care.
It is striking that the cascade of services received by the early MRI less severe subgroup was similar to the other 3 MRI subgroups. In addition, this subgroup underwent surgery significantly sooner than the timely more severe subgroup. The finding that the early and timely less severe subgroups received MRI sooner than the 2 more severe subgroups suggests that the MRI and surgery were done for inappropriate reasons.
The data do not indicate how MRI testing led to the cascade, however, several pathways can be postulated. Patients concerned about nonspecific symptoms may pressure providers to order MRI to find a physical cause of their pain, and then demand interventions to address the purported cause. Providers may think that they are obligated to address abnormalities found prior to returning patients to work, or employers may mistakenly think MRI demonstrates whether the employee is “safe” to return to work.
Other possibilities include a desire by physicians to identify a treatable physical cause, or economic and social factors. Focusing treatment on potentially unrelated diagnostic findings reflects the biomedical back pain model that predominates for many patients25 and providers,26 and seems to drive treatment.27 An invasive pain treatment model has been advocated, directing therapeutic interventions at multiple “pain generators,” based on an overinterpretation of the meaning of “abnormalities”28 that are commonly observed in asymptomatic people.7–9 As a result, patients may become engaged in an unhelpful treatment model that starts with MRI, followed by injections and additional diagnostic testing. However, a systematic review found little value in subsequent interventions based solely on such abnormalities10 and a recent report indicated that there is insufficient evidence to support injections for chronic back pain management.29 Although a large percentage of the early MRI more severe subgroup had a radiculopathy-related diagnosis for which guidelines clearly recommend a “wait and see” approach, many providers are influenced by this diagnosis and obtain imaging prematurely.30 Such an approach can lead to heightened urgency for both providers and patients to focus on “fixing” a physical abnormality that, in many cases, resolves spontaneously within a month.31 Such a focus diverts patients from more appropriate noninvasive interventions that can lead to better long-term functional results.
Economic and social factors may also be important drivers of nonadherent imaging, including physician self-referral, other overutilization financial incentives, oversupply of MRI scanners, and entitlement viewpoints that have all been documented to influence the rate of LBP health care utilization.13,32,33 Studies have reported excessive MRI utilization related to self-referral by physician-owners or shareholders of imaging centers.34–36 Swedlow et al34 concluded that self-referral increased WC medical costs by increasing the frequency of requests for clinically inappropriate MRIs. Baras and Baker13 reported that increases in surgery for nonspecific LBP and in early MRI were associated with an increase in the supply of scanners.
Although this study did not access MRI results, 2 studies reported that findings from nonadherent MRIs were more likely to be negative.37,38 Similarly, whether the timely MRI more severe group patients had appropriate indications for MRI cannot be determined with certainty; it is much more likely that they met some of the indications, compared with those who received early MRI. They were more likely to represent cases with radiculopathy that failed to resolve over time and it is suggested that their medical cost trajectory in the first-year post-MRI reflects what would be expected for guideline-adherent care.
Study strengths include robust longitudinal data, with almost complete capture of detailed information on each paid LBP-related medical service regardless of provider because WC is legally the first payer for all injury-related services for the treatment duration. The data represent a working age population that is not represented in the majority of national LBP health services research studies in the United States, which often rely on Medicare data. The cohort's national scope presents a snapshot of typical community-based practice in 48 states.
There are several potential limitations. The first is that WC insurance is a unique system and medical utilization tends to be higher than in general medical care.39,40 Yet, these results seem to parallel utilization trends in Medicare data and in a smaller community-based study.27 Administrative data has known limitations including absence of clinical information to classify cases into more or less severe categories or history of recurrent or chronic LBP.41,42 However, results from a prior study based entirely on administrative data12 were similar to a subsequent study based on clinical information extracted from claims medical reports,17 suggesting that administrative data can be used to both select acute LBP cases and International Classification of Diseases, Ninth Revision codes can be used to classify cases into severity categories. Although other potential covariates including socioeconomic level or race are not available, they are not indicators for MRI utilization. Finally, administrative data lack information on the decision-making process that leads to obtaining MRI and subsequent medical services.
CONCLUSION
The impact of nonadherent MRI utilization is significant in terms of the cost of potentially unnecessary and unhelpful medical services, which occurs relatively soon after MRI. The additional burden of a lost sense of well-being and of having a mistaken conceptual causal model and solution for one's LBP is difficult to estimate. The study results provide evidence to promote conversations between providers and patients to help patients choose care that is supported by evidence, free from harm, and truly necessary.
Further research is needed to identify specific pathways and decisions that lead to obtaining nonadherent MRI and a subsequent cascade of services. Longitudinal interviews could provide information on the important cascade-enhancing factors suggested by Deyo,1 including patient demands, overinterpretation, intolerance of ambiguity, economic incentives, and referral patterns that lead to overutilization, and unreasonable promises of a “cure.”
Key Points
MRI without clear indications led to a cascade of subsequent diagnostic and therapeutic services (including surgery), which generally occurred within 6 months after imaging.
This cascade was more related to the MRI than to severity, pain indicators, or demographic characteristics.
Even after grouping by severity and controlling for pain indicators and demographic factors, early MRI (receipt <30 d postonset) was significantly associated with a large and sustained escalation in medical costs, reflecting increases in overall medical utilization, which was greater than the costs for the no MRI and timely (receipt >42 d postonset) groups.
Study results provide evidence to promote provider and patient conversations to help patients choose care that is based on evidence, free from harm, less costly, and truly necessary.
Acknowledgments
The authors thank Helen Marucci-Wellman, ScD, and Raymond McGorry, MS, PT, who provided technical reviews of earlier drafts of the manuscript and Margaret Rothwell who provided administrative, technical, and material support. The Liberty Mutual Research Institute for Safety sponsored the study. The parent company, Liberty Mutual Insurance, had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Preliminary findings were presented on February 18, 2011 at the Melbourne International Forum XI: Primary Care Research on Low Back Pain in Melbourne, Australia.
Supplemental digital content is available for this article. Direct URL citations appearing in the printed text are provided in the HTML and PDF version of this article on the journal's web site (www.spinejournal.com).
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
One of the authors (A.Z.B.) received student internship funding from the University of Massachusetts-Lowell for participation in review activities such as data monitoring boards, statistical analysis, end point committees, and the like and writing or reviewing the manuscript.
Relevant financial activities outside the submitted work: employment.
References
- 1.Deyo RA. Cascade effects of medical technology. Ann Rev Public Health 2002;23:23–44 [DOI] [PubMed] [Google Scholar]
- 2.Shy KK, Luthy DA, Bennett F, et al. Effects of electronic fetal-heart-rate monitoring, as compared with periodic auscultation, on the neurologic development of premature infants. N Engl J Med 1990;322:588–93 [DOI] [PubMed] [Google Scholar]
- 3.Banerjee A, Newman DR, Van den Bruel A, et al. Diagnostic accuracy of exercise stress testing for coronary artery disease: a systematic review and meta-analysis of prospective studies. Int J Clin Pract 2012;66:477–92 [DOI] [PubMed] [Google Scholar]
- 4.Jarvik JG. Imaging of adults with low back pain in the primary care setting. Neuroimaging Clin N Am 2003;13:293–305 [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Mirza SK, Turner JA, et al. Overtreating chronic back pain: time to back off? J Am Board Fam Med 2009;22:62–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mafi JN, McCarthy EP, Davis RB, et al. Worsening trends in the management and treatment of back pain. JAMA Intern Med 2013;173:1573–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg 1990;72:403–8 [PubMed] [Google Scholar]
- 8.Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med 2002;137:586–97 [DOI] [PubMed] [Google Scholar]
- 9.Jensen MC, Brant-Zawadzki MN, Obuchowski NA, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 1994;331:69–73 [DOI] [PubMed] [Google Scholar]
- 10.Chou R, Fu R, Carrino JA, et al. Imaging strategies for low back pain: systematic review and meta-analysis. Lancet 2009;373:463–72 [DOI] [PubMed] [Google Scholar]
- 11.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007;147:478–91 [DOI] [PubMed] [Google Scholar]
- 12.Webster BS, Cifuentes M. Relationship of early magnetic resonance imaging for work-related acute low back pain with disability and medical utilization outcomes. J Occup Environ Med 2010;52:900–7 [DOI] [PubMed] [Google Scholar]
- 13.Baras JD, Baker LC. Magnetic resonance imaging and low back pain care for Medicare patients. Health Affairs (Millwood) 2009;28:w1133–40 [DOI] [PubMed] [Google Scholar]
- 14.Jarvik JG, Hollingworth W, Martin B, et al. Rapid magnetic resonance imaging vs. radiographs for patients with low back pain: a randomized controlled trial. J Am Med Assoc 2003;289:2810–8 [DOI] [PubMed] [Google Scholar]
- 15.Lurie JD, Birkmeyer NJ, Weinstein JN. Rates of advanced spinal imaging and spine surgery. Spine 2003;28:616–20 [DOI] [PubMed] [Google Scholar]
- 16.You JJ, Bederman SS, Symons S, et al. Patterns of care after magnetic resonance imaging of the spine in primary care. Spine 2013;38:51–9 [DOI] [PubMed] [Google Scholar]
- 17.Webster BS, Bauer A, Choi Y, et al. Iatrogenic consequences of early MRI in acute work-related disabling low back pain. Spine 2013;38:1939–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Graves JM, Fulton-Kehoe D, Jarvik JG, et al. Health care utilization and costs associated with adherence to clinical practice guidelines for early magnetic resonance imaging among workers with acute occupational low back pain. Health Serv Res 2014;49:645–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Medical Association. Current Procedural Terminology (CPT). Chicago, IL: American Medical Association; 2009 [Google Scholar]
- 20.Commission on Professional and Hospital Activities. International Classification of Diseases, 9th Revision, Clinical Modification, ICD-9-CM. Ann Arbor, MI: Edwards Brothers, Inc.; 1980 [Google Scholar]
- 21.Bigos S, Bowyer O, Braen G, et al. Acute Low Back Problems in Adults: Clinical Practice Guideline no. 14. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services; 1994 [Google Scholar]
- 22.Goertz M, Thorson D, Bonsell J, et al. Health care guideline. Adult acute and subacute low back pain. 15th edition Updated November 2012. Available at: https://www.icsi.org/_asset/bjvqrj/LBP.pdf Accessed July 19, 2013.
- 23.Webster BS, Verma S, Gatchel R. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery, and late opioid use. Spine 2007;32:2127–32 [DOI] [PubMed] [Google Scholar]
- 24.Modic MT, Obuchowski NA, Ross JS, et al. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology 2005;237:597–604 [DOI] [PubMed] [Google Scholar]
- 25.Campbell C, Guy A. Why can't they do anything for a simple back problem? A qualitative examination of expectations for low back pain treatment and outcome. J Health Psychol 2007;12:641–52 [DOI] [PubMed] [Google Scholar]
- 26.Tait RC, Chibnall JT, Kalauokalani D. Provider judgments of patients in pain: seeking symptom certainty. Pain Medicine 2009;10:11–34 [DOI] [PubMed] [Google Scholar]
- 27.Carey TS, Freburger JK, Holmes GM, et al. A long way to go: practice patterns and evidence in chronic low back pain care. Spine 2009;34:718–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boswell MV, Shah RV, Everett CR, et al. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Phys 2005;8:1–47 [PubMed] [Google Scholar]
- 29.Staal JB, Nelemans PJ, de Bie RA. Spinal injection therapy for low back pain. J Am Med Assoc 2013;309:2439–40 [DOI] [PubMed] [Google Scholar]
- 30.Webster BS, Courtney TK, Huang Y-H, et al. Physician's initial management of acute low back pain versus evidence-based guidelines: influence of sciatica. J Gen Intern Med 2005;20:1132–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract 2002;52:119–23 [PMC free article] [PubMed] [Google Scholar]
- 32.Shreibati JB, Baker LC. The relationship between low back magnetic resonance imaging, surgery, and spending: impact of physician self-referral status. Health Serv Res 2011;46:1362–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Webster BS, Verma S, Pransky GS. Outcomes of workers' compensation claimants with low back pain undergoing intradiscal electrothermal therapy. Spine 2004;29:435–41 [DOI] [PubMed] [Google Scholar]
- 34.Swedlow A, Johnson G, Smithline N, et al. Increased costs and rates of use in the California workers' compensation system as a result of self-referral by physicians. N Engl J Med 1992;327:1502–6 [DOI] [PubMed] [Google Scholar]
- 35.Mitchell JM. The prevalence of physician self-referral arrangements after Stark II: evidence from advanced diagnostic imaging. Health Affairs (Millwood) 2007;26:w415–24 [DOI] [PubMed] [Google Scholar]
- 36.Kilani RK, Paxton BE, Stinnett SS, et al. Self-referral in medical imaging: a meta-analysis of the literature. J Am Coll Radiol 2011;8:469–76 [DOI] [PubMed] [Google Scholar]
- 37.Paxton BE, Lungren MP, Srinivasan RC, et al. Physician self-referral of lumbar spine MRI with comparative analysis of negative study rates as a marker of utilization appropriateness. AJR Am J Roentgenol 2012;198:1375–9 [DOI] [PubMed] [Google Scholar]
- 38.Lehnert BE, Robert L, Bree RL. Analysis of appropriateness of outpatient CT and MRI referred from primary care clinics at an academic medical center: How critical is the need for improved decision support? J Am Coll Radiol 2010;7:192–7 [DOI] [PubMed] [Google Scholar]
- 39.Johnson WG, Burton JF, Jr, Thornquist L, et al. Why does workers' compensation pay more for health care? Benefits Q 1993;9:22–31 [PubMed] [Google Scholar]
- 40.Taylor VM, Deyo RA, Ciol M, et al. Surgical treatment of patients with back problems covered by workers' compensation versus those with other sources of payment. Spine 1996;21:2255–9 [DOI] [PubMed] [Google Scholar]
- 41.Deyo RA, Taylor VM, Diehr P, et al. Analysis of automated administrative and survey databases to study patterns and outcomes of care. Spine 1994;19:2083S–91S [DOI] [PubMed] [Google Scholar]
- 42.Faciszewski T. Administrative databases in spine research. Spine 1997;22:1270–5 [DOI] [PubMed] [Google Scholar]


