Abstract
Turning disciplinary knowledge about preadolescents’ and adolescents’ exposure to risk factors for cancer as adults into solutions for preventing such an outcome requires that investigators from a variety of backgrounds and disciplines come together to share knowledge. Optimally, these collaborations would occur across two dimensions: (1) transdisciplinary, from the molecular or cellular level (e.g., animal studies of endocrine disruption) to the societal level (e.g., economic studies related to state tobacco policies), and (2) translational, using basic research findings in clinical and other sciences to implement prevention programs and public policy. Only when collaboration is commonplace can the disparate groups of investigators working on cancer prevention during pre-adolescence and adolescence gain a holistic picture of the risk factors, inform one another’s work, and learn what we need to know to devise successful interventions for preventing cancer. Working transdisciplinarily also helps to ensure that messages to health professionals, policymakers, the news media, and the public are consistent and coordinated. At present, those investigating preadolescent and adolescent risk for adult cancer disseminate their knowledge individually, thus missing the opportunity to synthesize knowledge, coordinate dissemination, and implement prevention programs. In this paper, we distinguish multidisciplinary, interdisciplinary, and transdisciplinary approaches, argue for the benefits of a transdisciplinary approach to devising successful solutions and how to achieve transdisciplinary functioning.
Keywords: translational research, transdisciplinary, team science, collaboration, cancer
We are not students of some subject matter, but students of problems. And problems may cut across the borders of any subject matter or discipline.
— Karl Popper, 1963
Introduction
Research on cancer prevention and risk reduction among preadolescents and adolescents is diverse because each research investigation focuses on a particular point on a continuum from the cellular to societal influences on health (Figure 1), producing a range of knowledge from the effect of certain exposures on the mammary gland (1) to the effect of public policies aimed at reducing risky health-related behaviors (2). Investigations of individual behaviors (e.g., changing diet (3), increasing physical activity (3), getting the HPV vaccine (4), and improving social relationships such as early family relationships (5) fit between cellular and societal research. Investigations differ too in the phase of human development on which they focus and in the population groups they target. Some studies produce basic biologic, behavioral, or social knowledge; others investigate services and develop and test interventions to reduce risk and prevent cancer (6). Yet despite advances in knowledge in many spheres, progress toward preventing or controlling cancer at the population level is woefully inadequate.
Figure 1.
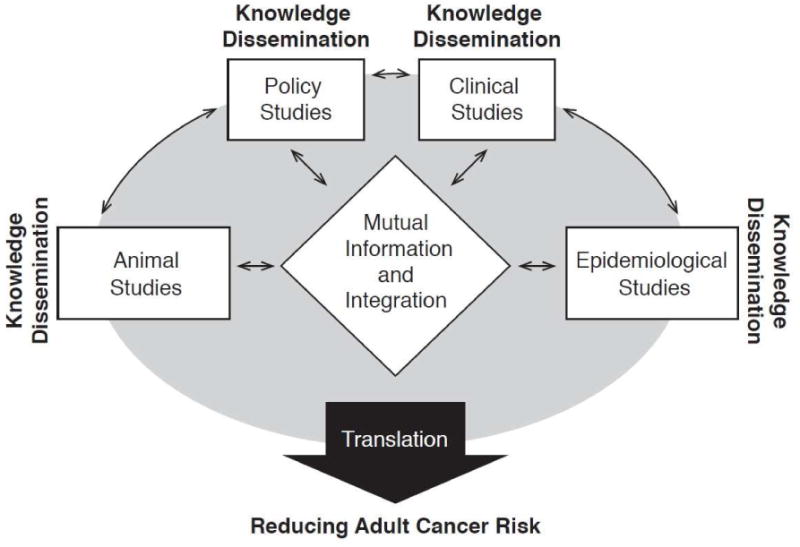
Dynamic model of cancer research that extends from discovery to translation into solutions for preventing cancer.
Footnote: Adapted from the Canadian Cancer Control Strategy.
In August 2011, the Division of Cancer Prevention and Control at the Centers for Disease Control and Prevention (CDC) brought together an expert panel of investigators from a range of disciplines and approaches to acquiring knowledge. The purpose was to discuss the problem of preadolescent and adolescent exposures to risk for cancer during adulthood, with a shared aim of preventing cancer. The expert panel’s charge was to accelerate progress toward cancer prevention and control by collaborating on research and interventions, by looking for opportunities to change public perceptions and policy in order to reduce environmental causes of disease, and by creating action plans to reduce cancer rates. Although most investigators on the panel were aware of one another’s work before the meeting and a few had even worked together, it became clear that despite their shared aim, each member had a slightly different take on cancer prevention. This is not surprising, since the group was assembled to facilitate an encompassing and holistic view of pre-adolescent and adolescent risk factors and exposes for adult cancer.
Expert panel members’ investigations differ along a number of dimensions (7,8,9,10,11). First, they differ in level of analysis, ranging from molecular and genetic investigations into the causes of cancer to societal investigations to reduce cancer rates. Members also varied in the types of research they do: basic, clinical, behavioral, or social science. And they differ in where their work is situated along the continuum from discovery in the laboratory to translation of findings into community programs to prevent cancer. Yet another difference was members’ approaches to cancer prevention and control. Some work with animal models, some with clinical samples, and others with publicly-available data. A few work in communities that range from Hispanics in rural Texas to adolescents living in public housing in Boston. Lastly, the focus of panel members’ work is on different stages of human development, from in utero to late adolescence.
The major challenges to collaboration for the group were two-fold. First, the group had to achieve a sufficient quality and degree of communication to be able to synthesize members’ individual knowledge, form a holistic and inclusive picture of preadolescent and adolescent risk factors and exposures, and develop shared action plans and interventions for cancer prevention. In short, members had to broaden their individual perspectives and approaches to encompass this new and broader charge. Operating collectively to develop effective evidence-based solutions requires that each member acknowledge the other members’ contributions and respect the cultures of other members’ disciplines is the bedrock of cross-disciplinary communication. When this level of communication is achieved, individual knowledge and empirical findings can be synthesized and new intellectual space created that allows coordinated action plans and interventions to be developed.
The second challenge to collaboration involves turning integrated plans into consistent and coordinated cancer prevention and control messages for stakeholders, including healthcare professionals, policymakers, the news media, and the public. This is particularly challenging in light of the long latency period that can occur between preadolescent and adolescent exposure to carcinogens and the onset of cancer. At present, those investigating preadolescent and adolescent risk factors disseminate their knowledge individually, thus missing an opportunity to synthesize knowledge, coordinate dissemination of findings, and collaborate on implementation. The payoff to moving from investigating individually to investigating with a diverse yet coordinated team that is able to devise integrated solutions is great, however, and is an incentive to investigators to work outside the comfort zones of individual disciplines. In this paper, we argue for the value of new approaches to collaborate to solve a complex problem such as preventing adult cancers and make an argument for knowledge synthesis as an effective means of problem solving. We distinguish between multidisciplinary, interdisciplinary, and transdisciplinary approaches to collaboration, argue for the benefits of a transdisciplinary approach to devising successful solutions, provide guidance on how to achieve transdisciplinary functioning, and offer suggestions for developing and sustaining such an approach.
Modes of Disciplinary Collaboration
Awareness is growing that the determinants of cancer interact in complex ways. To deal with these determinants, we need new ways of collaborating, ways that use input from all researchers in pertinent fields and enhance their ability to work together. In arguing for disciplinary collaboration, the Committee on Facilitating Interdisciplinary Research of the National Academies noted in 2005 that “how human societies evolve, make decisions, interact, and solve problems are all matters that call for diverse insights. Very fundamental questions are inherently complex (12).”
A related argument was made for cancer control research, namely that inputs are needed at multiple levels, from the molecular or cellular level of research to the societal level. Factors at each level are known to interact in complex ways to cause cancer and disparities in cancer rates (13). Hiatt and Breen (14) make the case that collaboration has the potential to “yield a detailed and vivid snapshot of the impact of the web of causation and to rationalize interventions at various critical points in the resulting picture.” Conversely, an inadequate understanding of the causes of cancer leads to inadequate solutions.
Collaborations among disciplines are generally divided into three types that differ in the extent to which investigators operate outside the boundaries of their individual disciplines. Differences occur in the extent to which researchers share the language of their disciplines, pool bodies of knowledge and theory, and jointly develop new methods of analysis. In multidisciplinary research, investigators come together to solve a research problem, but each discipline approaches the problem through a separate lens. These researchers leave the collaboration with no discernible change in their approach to science. For example, they might come together at the beginning of a research project with separate but related research questions, collect and analyze data independently, form independent conclusions based on their separate research questions, and then come together at the end of the project to try to make sense of it all. This practice is like trying to fit square pegs into round holes. Those who work interdisciplinarily transfer disciplinary knowledge to one another for the purposes of research and may, to some extent, share research questions. Yet the boundaries between disciplines return when an answer is found that serves the needs of the root disciplines. Some interdisciplinary collaborations have, however, forged new disciplines such as neuropsychology or bioethics that endure through time.
Transdisciplinarity (which Rosenfield defines as “research in which exchanging information, altering discipline-specific approaches, sharing resources, and integrating disciplines achieves a common scientific goal” (15)) achieves the highest degree of collaboration among disciplines. Transdisciplinarity relies on early agreement on research questions, methods, goals, and timelines, and it may entail the development of multifaceted, broadly analytical models for researching problems. Transdisciplinary scholars transcend and operate outside their own boundaries and cultures to achieve synergy, inform one another’s work, and create new intellectual spaces in which no one discipline dominates and no way of knowing is privileged over other ways. Emmons et al. acknowledge, for example, the tremendous inefficiency that occurs when boundaries between the social, behavioral, and biologic disciplines are rigidly maintained in research on obesity and energy balance, saying “If the primary focus of work in obesity and energy balance is on sociocultural factors, eventually the limits of not considering both environmental and physiologic factors will be realized (16).” Franco and Tota note that if epidemiologists and microbiologists worked closely together in the 1980s, erroneous conclusions might have been drawn about the sexually transmissible agent causing cervical cancer and HPV infection might have been assigned an ancillary role among a constellation of factors (17).
Reducing preadolescent risk factors and exposures for adult cancer is the shared problem for which the CDC expert panel was convened. If transdisciplinarity were to be achieved by the group, the outcome might well be a new multifaceted, broadly analytical understanding of preadolescent and adolescent risk factors and exposures for adult cancer that could inform solutions and undergird a well-integrated plan for their dissemination to stakeholders. In the words of the 2005 National Academies report, expert panel members would “catalyze the skillful design of research plans and the integration of knowledge and skills in multiple disciplines, rather than ‘stapling together’ similar or overlapping proposals (12).”
Transdisciplinary Research in Cancer Control
Despite a growing emphasis on transdisciplinarity in cancer research, it remains an ideal that few transdisciplinary groups achieve. This, in part, is because transdisciplinarity is neither intuitive nor necessarily congruent with current academic systems but, instead, must be learned and supported. Yet training in transdisciplinary collaboration has been slow to appear, despite a decade of exhortation for such collaborations (13,14,18). For the most part, scholars continue to be trained in the language and methods of their own disciplines, with minimal exposure to those of other disciplines. Although scattered transdisciplinary training programs exist (19), they have yet to be systematically integrated into formal curricula at any level of education. This lack of systematic training in transdisciplinary science reinforces the siloed nature of research, hinders the transfer of knowledge across disciplines, and makes it impossible to develop broad analytical perspectives on inherently complex human problems. Workshops and other short trainings on transdisciplinary and team science are insufficient to produce sustained change, resulting in investigators continuing to regress toward the mean of siloed research.
In addition to institutions providing training in transdisciplinarity, they must also support the practice if it is to be sustained and grow. During the last decade collaborations among disciplines were encouraged through initiatives such as CDC’s expert panel, the National Cancer Institute (NCI)-funded Centers for Population Health and Health Disparities, Transdisciplinary Research in Energetics and Cancer, and Transdisciplinary Tobacco Use Research Centers, and the NCI and National Institute for Environmental Health Science-funded Breast Cancer and the Environment Research Program. Despite this encouragement, universities and other cancer research institutions continue to recognize and reward work by individuals when it comes to tenure and promotion. Teams of investigators working across departments, divisions, and schools of universities remain the exception rather than the rule, primarily because of the nature of institutional incentives. Appointment and promotion guidelines that emphasize the contributions of transdisciplinary research and the time required for establishing teams would help to ensure that transdisciplinary research and practice is valued and rewarded appropriately. In general, within academe the science of transdisciplinary research is inadequately recognized for its contribution to cancer control and other beneficial outcomes, even in the case of the multimillion-dollar initiatives funded by NCI.
Likewise, tenure and promotion committees traditionally focus on discovery and new advances in understanding and research that change the field, ascribing a lower status to applying scientific advances to improving the delivery of healthcare services and the health of communities. Imbalance in how different ways of knowing are rewarded by institutional administrators makes it difficult to establish a level playing field that would allow ideas to flow from all quarters (19). When one way of knowing is privileged over others, the input from some investigators receives less weight, impeding the free flow of information between investigators that allows the creation of new ideas and novel solutions.
Increasing the level of collaboration among researchers needed to inform solutions requires structural changes within institutions, agencies, and universities. Needed are structures that foster interactions and training across disciplines and that prevent one discipline or group of disciplines from being favored over others. Favoring one way of knowing over others breeds mistrust, conflict, misunderstanding, and lack of appreciation for the expertise of others, all of which impedes the free flow of ideas between disciplines. Mechanisms for avoiding these pitfalls include creating shared instructional and work space across disciplines, cross-training opportunities for pre- and post-doctoral fellows, and setting up one central administrator to oversee research awards so that the work of one department, division, or school is not privileged over others (20).
Translation
Transdisciplinary research in cancer prevention and control in its fullest form should cover the entire continuum from basic research on cells to applied research on preventing cancer in society at large. Scientists who can influence cancer prevention and cancer disparities include clinicians, biologists, behavioral scientists, and social scientists. Devising solutions also relies on knowledge-sharing from basic science to clinical science to program implementation and policy change. Arguably, knowledge-sharing is an even greater challenge to collaboration than knowledge generation, because investigators operate in many different settings and geographic areas. Clinical scientists might operate from freestanding cancer centers or academic medical centers, while those whose primary focus is policy are located on academic campuses or in departments of health, and basic scientists work primarily in laboratories. This lack of shared space and face-to-face contact impedes communication, exposure to new ideas, and opportunities for information-sharing, and collaboration.
Communication facilitates both research and translation of findings into practical solutions. Facilitating communication among those who are working in different aspects of cancer prevention increases the chance of success. For example, work from a variety of disciplines on the phenotypes of nicotine addiction has important implications for preventing lung cancer: Stevens et al. (21) identified two loci in the CHRNA5-CHRNA3-CHRNB4 gene cluster associated with smoking behavior, and Bierut et al. (22) identified variants in the cluster that contribute to nicotine addiction. More recent contributions in imaging genetics (23) contributed to the development of endophenotypes, or stable, heritable traits related to a disorder or its symptoms that are detectable in at-risk individuals and closer to gene variants than are clinical phenotypes. Translating these discoveries on variation in nicotine addiction into practical prevention programs has great potential to reduce cancer rates.
All this work on nicotine addiction is impressive. Yet for any of it to lead to decreased rates of smoking in the population, information must be exchanged at a number of junctures. Clinical tests must be developed to measure propensity for addiction, which then must be rigorously tested and introduced into clinical practice. Next, treatment programs tailored to specific at-risk subgroups must be developed, rigorously tested, and introduced into provider systems in a way that heightens their chance of acceptance and sustainability. Lastly, broad impact depends on developing a plan for introducing these programs to consumers and healthcare providers in a variety of settings. Clinicians who are aware of the discovery of genetic variation in nicotine addiction will be better at explaining the relative merits of smoking cessation programs to their patients. Likewise, health educators who can explain variations in nicotine addiction and the dynamics of various treatment options will be more effective in their efforts at helping preadolescents, adolescents, and adults who want to quit smoking.
Translation of basic research findings from the biological, behavioral, and social sciences into cancer prevention and control interventions that are disseminated and implemented in communities has an end goal of improving the health of the population. For sustainable reductions in cancer incidence rates, research findings must be used in a way that takes into account the context, value system, and needs of each affected communities, whether the population is defined by race or ethnicity, age, or geographic area, such as Hispanic adolescents living along the Texas-Mexico border. It also is true, however, for virtual communities, such as adolescents with rare cancers caused by chemical exposures, who might be widely dispersed around the country and only are able to communicate electronically. A third type of community is what we might call an artificial community, or one that that is created by investigators for purposes of research, but whose members do not self-identify as being part of that community. An example might be obese adolescents who do not think of themselves either as obese or as part the group that researchers have labeled obese for the purposes of their study.
Research findings translate best into community cancer prevention programs when investigators work in concert with community stakeholders. Community-based participatory research involves engaging community stakeholders, thus enhancing the relevance and effectiveness of interventions by producing research findings that are meaningful to community members (24). An example is the USDA-ARS Delta Nutrition Research Initiative, in which residents in and around Marvel, Arkansas, partnered with investigators from the National Center for Toxicological Research a) to investigate the interaction of nutrition, genetics, and environment and b) to devise interventions to reduce any adverse effects (25). Working with community stakeholders at various levels helps to ensure that interventions are tailored to community needs. The CDC’s Cancer Prevention and Control Research Network is a broad group of academic, public health, and community partners that conduct community-based participatory research aimed at reducing the burden of cancer (26).
Institutional incentives for increasing the implementation of evidence-based practices aimed at cancer prevention and control are also crucial for the successful translation of discovery into improvements in health. Incentives are needed because, like other areas of modern public health research, integrating transdisciplinary research into practice requires substantial team work and time, in part through building and sustaining community relationships. Team research may make quantifying individual contributions to a project difficult. Establishing reportable metrics for tenure and promotion is a necessary step for fostering translation. Strong partnerships between investigators and administrators are needed to design and push forward such metrics.
Developing Integrated Health Messages
Investigators conducting animal studies, clinical studies, epidemiological studies, and policy studies usually disseminate the knowledge that they produce within their own disciplines and arenas (e.g., smoking behavior, HPV vaccine uptake, state tobacco policies) rather than to researchers outside their disciplines who could use their findings to create prevention programs (Figure 2).
Figure 2.
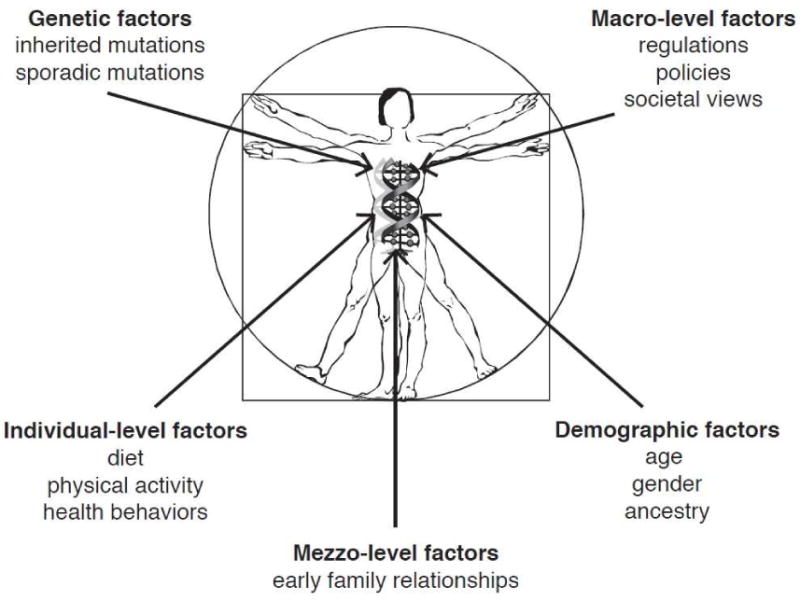
Preadolescent and adolescent risk factors for adult cancer.
The result of non-communication between disciplines is that research-based recommendations are seldom coordinated and, in fact, one set of recommendations may differ from another set even when both sets are based on similar evidence. Investigators are rewarded for discovering and for working alone, and the consequence of this reward system is a failure to adequately inform healthcare providers, the public, and policy makers about our work in a way that can be understood and used to reduce risk for cancer.
Conclusions
Efforts by agencies such as the CDC to bring together investigators from a range of disciplines involved in solving the problem of preadolescent and adolescent exposure to risk for adult cancer and efforts by the National Cancer Institute and National Institute of Environmental Health Sciences to foster transdisciplinary science hold promise for turning knowledge on preadolescent and adolescent risk factors into solutions for preventing cancer.
What is also needed is for universities and other research institutions to set up a curriculum to teach transdisciplinary research as early in the educational process as possible. Only when investigators can integrate their work, with input from communities, can we begin create multifaceted solutions to reduce cancer incidence rates. Likewise we must disseminate the solutions in a consistent and integrated way so that they are less confusing for stakeholders and have a greater chance of improving the nation’s health.
Implications and Contribution.
Turning disciplinary knowledge on preadolescent and adolescent risk factors for adult cancer into solutions for preventing such cancers requires bringing together investigators from a variety of backgrounds and approaches. When these disparate groups of investigators work together to devise solutions, their chances of success increase.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fenton SE. The mammary gland: a tissue sensitive to environmental exposures. Rev Environ Health. 2009;24(4):319–25. doi: 10.1515/reveh.2009.24.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tworek C, Yamaguchi R, Kloska DD, et al. State-level tobacco control policies and youth smoking cessation measures. Health Policy. 2010;97:136–44. doi: 10.1016/j.healthpol.2010.04.009. http://dx.doi.org/10.1016/j.healthpol.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fuemmler BF, Pendzich MK, Tercyak KP. Weight, dietary behavior, and physical activity in childhood and adolescence: implications for adult cancer risk. Obes Facts. 2009;2(3):179–86. doi: 10.1159/000220605. http://dx.doi.org/10.1159/000220605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenthal SL, Rupp R, Zimet DG, et al. Uptake of HPV vaccine: demographics, sexual history and values, parenting style and vaccine attitudes. J Adolesc Health. 2008;43(3):239–45. doi: 10.1016/j.jadohealth.2008.06.009. http://dx.doi.org/10.1016/j.jadohealth.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 5.Ellis BJ, Shirtcliff EA, Boyce WT, et al. Quality of early family relationships and the timing and tempo of puberty: effects depend on biological sensitivity to context. Dev Psychopathol. 2011;23:85–99. doi: 10.1017/S0954579410000660. http://dx.doi.org/10.1017/S0954579410000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Douyon M, Chavez M, Bunte D. The GirlStars Program: challenges to recruitment and retention in a physical activity and health education program for adolescent girls living in public housing. Prev Chronic Dis. 2010;7(2) http://www.cdc.gov/pcd/issues/2010/mar/08_0248.htm. [PMC free article] [PubMed] [Google Scholar]
- 7.Cost NG, Applegate KE. Image Gently: a campaign to reduce children’s and adolescents’ risk for cancer during adulthood. J Adolesc Health. 2013;52(X) doi: 10.1016/j.jadohealth.2013.03.006. Sxx=Sxx. DOI: [DOI] [PubMed] [Google Scholar]
- 8.Dube SR, Arrazola RA, Lee J, Engstrom M, Malarcher A. Pro-tobacco influences and susceptibility to smoking cigarettes among middle and high school students—United States, 2011. J Adolesc Health. 2013;52(X) doi: 10.1016/j.jadohealth.2012.07.007. Sxx=Sxx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazovich D, Choi K, Rolnick C, Jackson JM, Forster J, Southwell B. An intervention to decrease adolescent indoor tanning: a multi-method pilot study. J Adolesc Health. 2013;52(X) doi: 10.1016/j.jadohealth.2012.08.009. Sxx=Sxx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strunin L, Wulach L, Yang GJ, Evans TC, Hamdan SU, Davis GL, Bowen DJ. Preventing cancer: a community-based program for youths in public housing. J Adolesc Health. 2013;52(X) doi: 10.1016/j.jadohealth.2013.01.010. Sxx=Sxx. DOI: [DOI] [PubMed] [Google Scholar]
- 11.Thomas TL, Strickland O, Diclemente R, Higgins M. An opportunity for cancer prevention during preadolescence and adolescence: stopping human papillomavirus (HPV)-related cancer through HPV vaccination. J Adolesc Health. 2013;52(X) doi: 10.1016/j.jadohealth.2012.08.011. Sxx=Sxx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Committee on Facilitating Interdisciplinary Research; Committee on Science, Engineering and Public Policy; National Academy of Sciences; National Academy of Engineering; The Institute of Medicine. Facilitating Interdisciplinary Research. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 13.Gehlert S, Colditz G. Cancer disparities: unmet challenges in the elimination of disparities. Cancer Epidemiol Biomarkers Prev. 2011;20(9):1809–14. doi: 10.1158/1055-9965.EPI-11-0628. http://dx.doi.org/10.1158/1055-9965.EPI-11-0628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hiatt RA, Breen N. The social determinants of cancer: a challenge for transdisciplinary science. Am J Prev Med. 2008;35(2S):S141–50. doi: 10.1016/j.amepre.2008.05.006. http://dx.doi.org/10.1016/j.amepre.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenfield PL. The potential of transdisciplinary research for sustaining and extending linkages between the health and social sciences. Soc Sci Med. 1992;35:1343–57. doi: 10.1016/0277-9536(92)90038-r. http://dx.doi.org/10.1016/0277-9536(92)90038-R. [DOI] [PubMed] [Google Scholar]
- 16.Emmons KM, Viswanath K, Colditz G. The role of transdisciplinary collaboration in translating and disseminating health research: lessons learned and exemplars of success. Am J Prev Med. 2008;35(2S):S204–10. doi: 10.1016/j.amepre.2008.05.009. http://dx.doi.org/10.1016/j.amepre.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Franco EL, Tota J. Human papillomavirus infection and risk of cervical precancer: using the right methods to answer the right questions. Am J Epidemiol. 2009;171:164–68. doi: 10.1093/aje/kwp392. http://dx.doi.org/10.1093/aje/kwp392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stokols D, Misra S, Moser RP, et al. The ecology of team science: Understanding contextual influences on transdisciplinary collaboration. Am J Prev Med. 2008;35(2S):96–115. doi: 10.1016/j.amepre.2008.05.003. http://dx.doi.org/10.1016/j.amepre.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Gehlert S, Browne T. From cells to society: transdisciplinary training. In: Haire-Joshu D, McBride T, editors. Transdisciplinary Public Health: Research Methods and Practice. San Francisco: Jossey-Bass; In press. [Google Scholar]
- 20.Gehlert S, Murray A, Sohmer D, et al. The importance of transdisciplinary collaborations for understanding and resolving health disparities. Soc Work Public Health. 2008;25(3):408–22. doi: 10.1080/19371910903241124. http://dx.doi.org/10.1080/19371910903241124. [DOI] [PubMed] [Google Scholar]
- 21.Stevens VL, Bierut LJ, Talbot JT, et al. Nicotinic receptor gene variants influence susceptibility to heaving smoking. Cancer Epidemiol Biormarkers Prev. 2008;17(12):3517–25. doi: 10.1158/1055-9965.EPI-08-0585. http://dx.doi.org/10.1158/1055-9965.EPI-08-0585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bierut LJ, Stitzel JA, Wang JC, et al. Variants in nicotinic receptors and risk for nicotine dependence. Am J Psychiatry. 2008;165(9):1163–71. doi: 10.1176/appi.ajp.2008.07111711. http://dx.doi.org/10.1176/appi.ajp.2008.07111711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ersche KD, Turton AJ, Pradhan S, et al. Drug addiction endophenotypes: impulsive versus sensation-seeking personality traits. Biol Psychiat. 2010;68(8):770–73. doi: 10.1016/j.biopsych.2010.06.015. http://dx.doi.org/10.1016/j.biopsych.2010.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Israel BA, Eng E, Schulz AJ, et al. Methods in Community-Based participatory Research for Health. San Francisco: Jossey-Bass; 2005. [Google Scholar]
- 25.McCabe-Sellers BJ, Lovera D, Nuss HJ, et al. Personalizing nutrigenomics research through community-based participatory research and omics technologies. J Integrative Biol. 2008;12(4):263–72. doi: 10.1089/omi.2008.0041. http://dx.doi.org/10.1089/omi.2008.0041. [DOI] [PubMed] [Google Scholar]
- 26.Center for Disease Control and Prevention. Cancer Prevention and Control Research Network. http://www.cpcrn.org/


