Abstract
Managing chronic pain effectively is often challenging for health care providers and patients. Telehealth technologies can bridge geographic distance and improve patients' quality of care in communities where access to pain specialists has previously been unavailable. This paper describes the development and evaluation of a telehealth intervention (TelePain) designed to address the need for pain specialist consultation regarding pain and symptom management issues in non-academic medical centers. We describe the theoretical foundation and development of a multifaceted intervention using a cluster randomized clinical trial design. Health care providers and their patients with chronic pain are enrolled in the study. Patient participants receive the intervention (report of symptoms and receipt of a pain graph) weekly for 8 weeks and are contacted at 12 weeks for completion of post-intervention follow-up measures. Their providers attend Telepain sessions which involve a didactic presentation on an evidence-based topic related to pain management followed by patient case presentations and discussion by community clinicians. Symptom management recommendations for each patient case are made by a panel of pain specialists representing internal medicine, addiction medicine, rehabilitation medicine, anesthesiology, psychiatry, and nursing. The outcomes assessed in this randomized trial focus on pain intensity, pain's interference on function and sleep, and anxiety, depression, and cost-effectiveness. Some of the challenges and lessons that we have learned early in implementing the TelePain intervention are also reported.
Keywords: pain, symptom management, randomized trial, telehealth
Background
Approximately 100 million adults in the United States are affected by chronic pain.1 The prevalence of chronic pain in adults in the United States has been estimated to range from 14.6% to 64%.2–5 The prevalence has been found to be higher among females (34.3%) than males (26.7%), to increase with age, and is most often due to non-specific lower back pain followed by osteoarthritis pain.2
Pain lowers patients’ work productivity, requires patients to seek medical treatment, and complicates treatment for other health problems; thus, its economic costs are high in the United States.6 Using the 2008 Medical Expenditure Panel Survey, Gaskin and Richard6 found the total costs—U.S. health care costs attributable to pain and the annual costs of pain associated with lower worker productivity—ranged from $560 to $635 billion in 2010 dollars. This cost is greater than each of the annual costs for heart disease, cancer, and diabetes.6
Chronic pain may often be managed with opioid therapy. Escalating prescription opioid use and abuse have emerged as major public health problems. This escalation may be related to more deaths due to opioid misuse than to traffic fatalities, and in a ten-fold increase in drug abuse treatment admissions for opioids.7 Washington State’s 2012 opioid prescribing rules now require pain specialty consultations for high-dose patients, i.e., patients receiving more than 120 mg/day of morphine or equivalent.8
Managing chronic pain effectively is challenging and requires health care providers who are knowledgeable in both pharmacologic and nonpharmacologic treatment for pain. Because pain management interventions are individualized to each patient, health care providers must have an understanding of the realm of interventions to best manage pain. Provider pain management education is needed as indicated by findings from a recent survey of 856 primary care physicians and advanced registered nurse practitioners in Washington State. 9 The survey, which focused on changes in practice patterns and use of support tools in the prescription of opioids for the treatment of chronic noncancer pain, found the majority of providers needed access to “more efficient, innovative means of support and education related to treating patients with chronic noncancer pain, such as telemedicine consultation.”9
Rural Pain Management
Many rural communities in the United States are disadvantaged by limited access to pain medicine specialists, and inadequate pain medicine training and support for community health care providers.10 These communities are also experiencing economic decline and an aging population base.11 Meanwhile, their health care organizations are in a vulnerable position: they face financial challenges due to low population densities, few economies of scale, and high rates of fixed costs per service, yet they need to provide sufficient financial and quality-of-life incentives to retain providers to adequately meet the needs of their communities. Additional issues that can adversely impact retention of providers in rural areas include professional isolation and lack of access to continuing medical education.12
Rural residents are more likely than their urban counterparts to be in poorer overall health, suffer from more multiple chronic or serious illnesses and disabilities, be uninsured or under-insured, be living in poverty, be older, have less formal education, and lack social support and a regular source of health care.12 Access to health care is often hampered by long travel distances, which is exacerbated by poor secondary roads and winters with inclement weather conditions. Rural residents often experience delays in obtaining care that is not available locally.14 Furthermore, in many cases, rural residents are required to leave the supportive environment of family and community to obtain care available in urban settings. These residents may benefit by programs that provide local health care providers with access to pain management education and consultation; thus, improving the quality of care within the community.
Telehealth and Pain Management
Telehealth technologies can bridge geographic distance and increase patients’ quality of care in communities where specialized health care has previously been unavailable. The growth of technological innovations such as high-capacity digital networks, powerful computer hardware and software, high-resolution digital image compression, and the Internet has had a great impact on the process of health care delivery and has introduced ways to increase rural populations’ access to specialized care services. Studies show that telehealth offers positive outcomes and high satisfaction for patients, primary care providers, and specialist consultants.15–20
The economic consequences of telehealth have been examined in several settings including home settings for patients with chronic conditions such as congestive heart failure.21 Findings indicate the potential for cost savings exists through reductions in rehospitalization rates and unexpected use of health care services such as emergency department services.22 Additionally, providers are able to bill for management of higher levels of care provision as their confidence for managing complex cases increases. Telehealth’s effect on health care utilization and pain management outcomes and its associated cost-effectiveness, however, has not been explored.
The use of telehealth technology to discuss treatment options with a specialist is well-developed for chronic pain management.23 Project ECHO (Extension for Community Health Outcomes) is an example of a successful telehealth program that provides chronic pain management education and consultation to health care providers in rural and underserved communities.24, 25 This program has shown significant improvements in providers’ self-reported knowledge, skills and practice;24 however, it is not known what effect this type of program has on patient outcomes.
Using telehealth to improve pain care was first piloted at the University of Washington (UW) in 2006 as part of a project with American Indian communities, funded by Health Resources and Services Administration’s (HRSA) Office for the Advancement of Telehealth.26,27 The project included 9 tribal clinics in Washington state and 26 clinics in Alaska. The telehealth system was found to be a successful method for delivering services to tribal clinics. In 2009, the project was expanded through an NIH grant to include rural hospitals and clinics.28 In 2011, it merged with Project ECHO.
The purpose of this study is to develop and test a telehealth-enhanced symptom management intervention (TelePain) designed to advance and improve access to quality pain and symptom management care for community populations. This study examines both patient and provider outcomes of a telehealth provider education and consultation program. We describe the theoretical foundation and development of this multifaceted intervention as well as the design of a randomized clinical trial to evaluate TelePain. We also report some of the lessons learned in implementing this study.
Theoretical Foundation of the Intervention
The symptom-management approach is based on the Symptom Management Conceptual Model. The model comprises three domains (person, health/illness, and environment) which influence the model’s three dimensions (symptom experience, management strategies, and outcomes).29 The person domain includes individual characteristics. The health/illness domain includes health status, risk factors, and disease and injury. The environment domain includes physical, social, and cultural characteristics. The symptom experience dimension is the individual’s perception of a symptom. The management strategies dimension includes specifications of the interventions, such as taking oral pain medication every six hours. The outcomes dimension focuses on functional status, self-care, costs, quality of life, morbidity and comorbidity, mortality, and emotional status. The model is based on the premise that all three dimensions must be considered for effective symptom management.
In this study, the person domain is an adult; the health/illness domain is pain; and the environment domain is the home setting in the community. The proposed pain and symptom management intervention addresses all three domains of the conceptual model, thus providing a holistic and effective approach to symptom management.
Overview of the Study
This study, approved by the UW institutional review board (IRB), uses a cluster randomized trial of a telehealth-enhanced symptom management intervention for chronic pain management (figure 1). This is the first study to our knowledge to use an experimental design to explore the cost-effectiveness of a telehealth-enhanced intervention in chronic pain management. The telehealth platform of our study intervention provides an innovative approach to an unaddressed problem: the need for efficient and cost-effective chronic pain and symptom management in communities.
Figure 1.
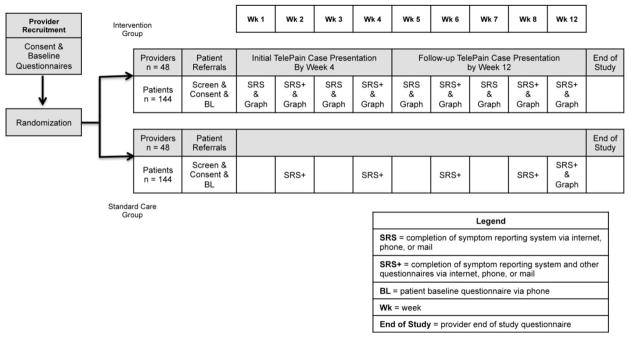
Schematic Diagram of Study Procedures
The study is designed to answer the main question: For community patients, does a telehealth-enhanced pain and symptom management intervention provide better pain management than the current usual care? The economic research question is: From a societal perspective, should community health care organizations that care for adult patients invest in telehealth-enhanced symptom management as a cost-effective alternative to the current usual care?
The study aims include: (a) to evaluate the effectiveness of the telehealth-enhanced chronic pain management intervention on pain severity among patients at 2 months compared to the standard care group, (b) to evaluate the effectiveness of the intervention on fatigue, dyspnea, constipation, anxiety, depression, and quality of life among patients at 2 months compared to the standard care group; (c) to evaluate the effectiveness of the intervention on provider knowledge and attitudes regarding pain and on providers’ perceived competence in treating symptoms at 3 months compared to the standard care group; and (d) to establish the cost-effectiveness of the intervention from a societal perspective (the incremental cost per quality-adjusted life year [QALY] gained), by incorporating the cost of the intervention and the impact on health care utilization, patient travel and time costs, and caregiver time costs.
Patient participants receive the intervention (report of symptoms and receipt of a pain graph) weekly for 8 weeks and are contacted at 12 weeks for completion of post-intervention follow-up measures. Their health care providers present their clinical case at the TelePain video conference to a panel of academic pain specialists within the first 4 weeks of the patient’s study enrollment. At the end of the patient’s study participation, their case is presented again as follow-up. The one month follow-up interval, i.e., 3 months after enrollment in the study, was selected because patients would be seen again by their health care provider at this time point. The standard care group patients provide a report of their pain and other symptoms every 2 weeks for 8 weeks and at week 12 for completion of follow-up measures.
The interdisciplinary research team includes the nurse scientist principle investigator and co-investigators: a palliative care expert physician, a pain management expert physician, a psychologist, a health care economist, and a biostatistician. The team is completed by two research nurses, two research assistants, a doctorally-prepared nurse pain management expert, and the director of the UW Telehealth Services.
Description of the Intervention
The telehealth-enhanced symptom management intervention (TelePain) uses low-cost, commercially available technology as its mode of delivery. The intervention has three components: (a) video case conferences between community health care providers and pain and symptom management experts to manage cases and engage community providers in evidence-based practice resources and peer support, (b) weekly report of pain and other symptoms using a Web-based patient reported outcome instrument, and (c) weekly graphs of patients’ reported pain experience.
Video Case Conferences
Videoconferencing is used for case-based learning to improve community health care providers’ ability to manage more complex cases, reinforce evidence-based practice, and model an interdisciplinary approach to care. Expert symptom management consultants from UW provide weekly 90-minute case conferences via videoconference for community health care providers in the intervention group. The teleconsultant team participating in each telepain session includes specialists whose expertise spans pain medicine, internal medicine, anesthesiology, rehabilitation medicine, psychiatry, addiction medicine, nursing, and complementary and integrative pain management. In addition to receiving the teleconsultant team’s recommendations, community health care providers have the opportunity to learn from each other through provider interaction during the videoconference. The video case conferences also offer brief didactic presentations on core topics essential to chronic pain care (see Table 1) and continuing medical education (CME) credits. The topics were identified from the International Association for the Study of Pain Curriculum Outline on Pain for Medicine.30 One topic is covered each week and its selection is based on speaker availability. Provider study participants have attended a range of 1–20 telepain sessions; thus receiving a range of 1.5–30 CMEs per provider.
Table 1.
Core and Supplemental Didactic Topics
| Core Topics: | Supplemental Topics: |
|---|---|
|
|
The community health care provider submits information about each patient who is participating in the study within the first four weeks of the patient’s study enrollment. This information is submitted by fax to the teleconsultant team no less than a day in advance of the video case conference. The community health care provider submits the patient history, including diagnosis, current medical issues, current symptom management issues, and specific questions for the consulting team. All identifying information is omitted and the patient is referred to only by an assigned patient number.
The teleconsultant team makes recommendations for difficult pain and symptom management issues which include behavioral, lifestyle, rehabilitative, cognitive, and pharmacological strategies. The latter focuses on minimizing side effects and maximizing symptom control. Tailored interventions are identified to manage pain effectively. The consultants also provide guidelines on how to assess and manage symptoms over time, as well as when to respond to symptoms and when to practice “watchful waiting.” Recommendations are based on guidelines from the Agency Medical Director’s Group31, the American Academy of Pain Medicine32, the American Pain Society33, and the Federation of State Medical Boards.34 A summary of the recommendations is faxed and e-mailed to the community health care provider. The provider shares the recommendations with the patient at his or her next visit. The patient’s preferences and the provider’s clinical judgment are considered in determining which recommendations to implement. The community health care provider gives a follow-up presentation of the patient at the end of the patient’s study period, approximately at week 12. An example of a telepain case and consultants’ recommendations is provided in Table 2.
Table 2.
Telepain Case Consultation Example
| Initial Case Presentation: 59 year old female diagnosed with lumbar and thoracic degeneration, stenosis, multiple cervical foraminal narrowing, chronic pain in the cervical and lower lumbar regions, bipolar disorder, and history of alcoholism. Opioid Risk Tool score is 12. Medications include: Vicodin, Ibuprofen, Neurontin, Trazadone, Lamictal, Xanax, and Carisoprodol. |
Recommendations from Consultants:
|
Follow-up Presentation: Patient accepted all of the recommendations provided above.
|
Follow-up Recommendations from Consultants:
|
Patient Report of Symptoms
The study intervention includes a weekly report of patient symptoms from home via a reporting system through the Internet, a novel multimodal UW Pain tool. If patients are not comfortable using the Internet, they may choose to report their symptoms by phone or on a paper version. If the patient chooses to report by phone, they are called by the research team weekly for 8 weeks and the Web-based patient reported outcome instrument is completed over the phone. If the patient chooses the paper version, a hard copy of the survey is mailed to the patient and they are instructed to return the survey by mail in a postage-paid envelope provided to the patient. Patients who have chosen the paper version have been highly motivated and the response rate has been 100%.
Graphs
The patient’s pain experience is visually depicted in a graph format which is generated weekly for the patient to view. The graph provides three aspects of the patient’s pain experience: (a) pain intensity and distress, (b) pain interference and difficulty performing one activity important to the patient, and (c) pain interference with falling asleep and staying asleep. Depending on which version of the symptom reporting system is used, either the patient or the research team generates the graph. Patients are then instructed to share and discuss the graph with their community health care provider at their next clinic visit. At week 8, patients are asked (a) if they found the graph helpful and if yes, what was helpful, (b) if they shared the graph with their provider -- if no, why not and if yes, what was discussed and what changes were made to their pain management plan. Standard care group patient participants are mailed a graph when they complete the study at week 12.
Implementation
The community health care provider is the unit of randomization in this cluster-randomized design. After completing the baseline questionnaires, providers from community clinics are randomized to the treatment or standard care group by the study biostatistician. Patients are assigned to the same group as their provider.
Participant Eligibility, Recruitment, and Incentives
Providers
The community health care providers are from Washington State, Wyoming, Alaska, Montana, and Idaho. Eligible providers include physicians, physician assistants, nurse practitioners, and registered nurses who provide direct care to patients with chronic pain. After the provider’s clinic submits a letter of support to the UW IRB, providers are consented by their reading of the study information statement on the study website. The research team’s phone numbers are listed so providers can contact a research team member to ask questions about the study. Consent is indicated through completion of the baseline measures collected via the Internet. This consent process allows us to successfully reach distant geographical areas.
Following randomization, the providers identify eligible patients in their caseload using the following criteria: (a) ≥ 18 years of age, (b) diagnosed with pain, (c) completion of an outpatient visit in the past 2 months, (d) functional fluency in English, (e) no or only mild cognitive impairment, and (f) no problems with regular phone lines because of hearing assistive devices. Eligible patients are asked by their provider if they are interested in being contacted about this study. If patients agree to be contacted by the research team, the provider gives their name and phone number to the research team via fax, phone, or e-mail. Providers receive $100 for participating in the study. If two of the provider’s patients agree to participate in the study, the provider will receive an additional $100 check for their time. For each additional patient who agrees to participate, the provider will receive a $100 check. Providers in the intervention group also receive free CME credits for each UW TelePain video case conference attended. An additional incentive for Washington providers is that the teleconsultation meets the state’s 2012 opioid prescribing rules requirement for pain specialty consultations for high-dose and high-risk patients.
Providers receive weekly e-mails from the research team to request patient referrals and to notify them of which patients are currently participating in the study. Providers may have up to 15 patients enrolled in the study.
Patients
Interested patients are contacted by phone by a research nurse who reads the consent form to them and answers questions regarding the study. If the patient agrees to participate in the study, they are screened for eligibility and baseline measures are collected by the research nurse. Patients are asked to choose which symptom reporting system they would like to use: Internet, phone, or paper version. Patients who choose the Internet delivery method receive verbal and written instructions for using this Web-based system. They create a password for accessing the Web-based system and receive email reminders for completing the weekly assessments. The participants who select the phone delivery method identify a convenient day and time to be called by the research team. Patients are compensated $100 for participating and receive a $25 check for completing the baseline survey, $25 for completing the 8-week survey, and $50 for completing the 12-week survey.
Study Measures
Provider Outcomes
The community health care provider completes the KnowPain-12 questionnaire35, the Knowledge and Attitude Survey Regarding Pain36, and the Perceived Competency Scale37. Providers complete the outcome measures at baseline and after their patients have completed the study, at approximately 3 months (Table 3). Surveys are completed on the Internet via the study Website.
Table 3.
Primary Study Measures
| Aim | Study Measures | Baseline | 1, 3, 5, 7 weeks (Intervention patients only) | 2, 4, 6 weeks | 8 weeks | 12 weeks |
|---|---|---|---|---|---|---|
| Patient Outcomes | ||||||
| a | Pain Intensity, Enjoyment of Life, and Interference with General Activity (PEG) Numeric scales40 | X | X | X | X | X |
| b | PHQ-438,39 (anxiety & depression) | X | X | X | X | X |
| b | Fatigue, shortness of breath, constipation numerical scales | X | X | X | X | |
| b ,d | HUI-342–45 (quality of life) | X | X | X | X | |
| d | Health Resource Utilization Survey46 | X | X | X | X | |
| d | Caregiving Time48 | X | X | X | X | |
| d | Work Productivity and Activity Impairment Questionnaire47 | X | X | X | X | |
| Provider Outcomes | ||||||
| c | Knowledge and Attitudes Scale36 | X | X | |||
| c | Perceived Competency Scale37 | X | X | |||
| c | KnowPain 1235 | X | X |
Patient Outcomes
The patient completes the symptom reporting system, which is a patient reported outcome (PRO) Web-based tool that queries the patient about symptoms over the past week. The symptom reporting system includes the PHQ-438,39; the Pain Intensity, Enjoyment of Life, and Interference with General Activity (PEG) Numeric scales40, and items addressing analgesic side effects, number of “bad days” when more medication than is prescribed was needed, and treatment satisfaction. The symptom reporting system also includes the Opioid Risk Tool (ORT)41 which is completed at baseline and available during video case conferences to help providers assess risk of aberrant drug-related behavior where additional monitoring is indicated. Additionally, the patient completes the HUI-342–45; Health Resource Utilization Survey46; Work Productivity and Activity Impairment Questionnaire47 Caregiving Time48; and numeric scales for fatigue, shortness of breath, and constipation. All of these outcome measures have established reliability and validity. The patient is also asked about non-medicine pain relief methods used and what medications they are taking for pain, anxiety, depression, sleep, and constipation. All patients are contacted by the research team via phone to complete the baseline measures. Standard care patients complete the study measures at weeks 2, 4, 6, 8, and 12. Surveys for both groups take approximately 5 to 15 minutes.
Intervention Measures
Data collected from the video case conference presentations include the patient history and clinical problems, expert recommendations, and follow-up information on recommendations implemented and patient results. At 8 weeks, intervention patients complete the Telemedicine Perception Questionnaire.49
Economic Data
In addition to the medication, health utilization, productivity and caregiver information collected by the symptom reporting system, economic evaluation data are collected from the clinic’s billing services and, if needed, from review of the patients’ medical records six months after they complete the study. Obtaining cost data is challenging since it may require collecting data from both paper records and the electronic medical record. Working closely with the clinic’s billing services is key to obtaining economic evaluation data. We have created a data collection tool which is used by the clinic’s billing services and by the research team when completing medical record abstractions.
Analysis Plan
Overview of Analytic Approach
The conduct of the study and all analyses will be based on the intent-to-treat principle. Analyses for patient outcomes will be by mixed-effect models using hierarchical linear modeling (HLM).50,51 The primary outcome variable will be average pain in past week, as reported on the symptom reporting system, measured at week 8. The model will include a random provider effect and a fixed group effect. Baseline (pre-intervention) pain will be included as a covariate.
With 48 providers per treatment arm, 3 patients per provider, and an ICC of 0.2, the Design Effect (Deff) = 1.4 and the effective sample size is 103 per treatment arm, reduced from 144 actual patients per arm. Based on a t-test comparing the two treatment arms (N = 103 per arm), there is 82% power to detect a standardized effect size (i.e. the difference in means between intervention and control arms, divided by the within-group standard deviation) of 0.4, and 95% power to detect a standardized effect size of 0.5. This study should have over 80% power for detecting a treatment effects on all of the outcome measures. These power calculations are probably conservative, since they are based on a simple t-test while the actual analysis will be by mixed model which accounts for the multiple weeks of outcome data and controls for baseline pain and other possible baseline covariates.
Analyses for provider outcomes will be by analysis of covariance, comparing the two treatment arms on provider knowledge and attitudes regarding pain, providers’ perceived competence in treating symptoms, and the KnowPain-12 questionnaire responses as measured at 3 months, and controlling for the baseline value of that measure as a covariate.
A description of the economic evaluation analysis plan has been previously published.48 Analyses for the economic evaluation will be supplemented with a secondary analysis based on received treatment (i.e., patients in the intervention group who did not receive the intervention as planned will be placed in the standard care group).
Study Progress, Challenges, and Lessons Learned
The study began enrolling patients in May 2012 and as of February 2014, we have enrolled 22 clinics, 26 providers, and 154 patients. The number of patients per provider ranges from 1 to 15 (mean = 6). Interim analyses are not being conducted in order to preserve a p value of 0.05 for hypothesis testing of the primary outcome.
Lessons Learned
It has been challenging to recruit healthcare organizations, providers, and patients. Participating clinics have primarily been those that have a preexisting relationship with UW Telehealth Services. Site visits have been very important to build relationships with clinics and their providers. The most active provider participants have been those who have administrative support for attending the TelePain sessions. An added incentive for participating clinics is for providers to learn evidence-based pain management interventions from specialists and the ability to bill for additional services by participation in TelePain. For example, a provider could bill for a more complex service for subsequent visits provided that the patient’s condition supports the enhanced level of service and the physician mentions the case consultation in their documentation.
Scheduling time to attend TelePain sessions has also been challenging for both specialist providers at the university setting and for the community health care providers. One of the methods we have used to make the sessions more accessible is scheduling sessions either early in the morning or over the lunch hour, so it is a “lunch and learn” session. As noted, one incentive for providers is that they receive 1.5 hours of CME at no cost for participating in TelePain, so providers are able to earn required CME hours without leaving their office.
Providers are referring patients, but we have faced challenges with enrollment. Of the 227 eligible patients referred to the study, the research team was unable to reach 23 (10%) patients by phone, and 50 (22%) patients declined to enroll due to reasons such as being too busy, not interested, did not want medical records reviewed, currently participating in other research studies, and study was too much of a time commitment. This is a complex study population that may have limited self-management skills and chaotic social support and lives. We have recently increased the patient incentive from $50 to $100, expecting that this will improve patient enrollment.
Significance
Access to specialty care for pain patients living in the community is often difficult. The majority of pain specialists are concentrated in urban areas, causing geographical barriers that must be overcome as well as additional time and money constraints. Since a consultation with a pain specialist is not available to most pain patients, participation by their primary care provider in TelePain has been demonstrated as a feasible solution to improving patients' quality of care. It is also an efficient solution for providers to learn about evidence-based practices from university-based experts. TelePain bridges physical distances through the use of video, Web, and telephone conferencing technologies to increase access to chronic pain management. This study will provide important empirical data on the use of TelePain in providing chronic pain and symptom management in communities.
Acknowledgments
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under award number #R01NR012450 and the National Cancer Institute of the National Institutes of Health under award number #R42 CA141875. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- CME
continuing medical education
- HLM
hierarchical linear modeling
- HRSA
Health Resources and Services Administration
- HUI-3
Health Utilities Index-3
- IRB
institutional review board
- MSW
Master of Social Work
- ORT
Opioid Risk Tool
- PEG
Pain Intensity, Enjoyment of Life, and Interference with General Activity
- PHQ-4
Patient Health Questionnaire-4
- PRO
patient reported outcome
- QALY
quality-adjusted life year, UW, University of Washington
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Linda H. Eaton, Email: lineaton@uw.edu.
Debra B. Gordon, Email: debrag3@uw.edu.
Sheryl Wyant, Email: swyant@uw.edu.
Brian R. Theodore, Email: brianrt@uw.edu.
Alexa R. Meins, Email: ameins@uw.edu.
Cara Towle, Email: ctowle@uw.edu.
David Tauben, Email: tauben@uw.edu.
Ardith Z. Doorenbos, Email: doorenbo@uw.edu.
References
- 1.Johannes CB, Le TK, Zhou X. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: National Academy of Sciences; 2011. [Google Scholar]
- 2.Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010 Nov;11(11):1230–1239. doi: 10.1016/j.jpain.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Hardt J, Jacobsen C, Goldberg J, Nickel R, Buchwald D. Prevalence of chronic pain in a representative sample in the United States. Pain Med. 2008 Oct;9(7):803–812. doi: 10.1111/j.1526-4637.2008.00425.x. [DOI] [PubMed] [Google Scholar]
- 4.Watkins EA, Wollan PC, Melton LJ, 3rd, Yawn BP. A population in pain: report from the Olmsted County health study. Pain Med. 2008 Mar;9(2):166–174. doi: 10.1111/j.1526-4637.2007.00280.x. [DOI] [PubMed] [Google Scholar]
- 5.Portenoy RK, Ugarte C, Fuller I, Haas G. Population-based survey of pain in the United States: differences among white, African American, and Hispanic subjects. J Pain. 2004 Aug;5(6):317–328. doi: 10.1016/j.jpain.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012 Aug;13(8):715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Warner M, Chen LH, Makuc DM, Anderson RN, Minino AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011 Dec;(81):1–8. [PubMed] [Google Scholar]
- 8.Group AMD. [Accessed July 29, 2013];Interagency Guideline on Opioid Dosing for Chronic Non-cancer Pain: An educational aid to improve care and safety with opioid therapy 2010 Update. http://www.agencymeddirectors.wa.gov/Files/OpioidGdline.pdf.
- 9.Franklin GM, Fulton-Kehoe D, Turner JA, Sullivan MD, Wickizer TM. Changes in opioid prescribing for chronic pain in Washington State. Journal of the American Board of Family Medicine. 2013;26(4):394–400. doi: 10.3122/jabfm.2013.04.120274. [DOI] [PubMed] [Google Scholar]
- 10.Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: National Academy of Sciences; 2011. [PubMed] [Google Scholar]
- 11.Aging Ao. [Accessed July 29, 2013];A profile of older Americans. 2012 http://www.aoa.gov/Aging_Statistics/Profile/2012/docs/2012profile.pdf.
- 12.Jukkala AM, Henly SJ, Lindeke LL. Rural perceptions of continuing professional education. J Contin Educ Nurs. 2008 Dec;39(12):555–563. doi: 10.3928/00220124-20081201-08. [DOI] [PubMed] [Google Scholar]
- 13.Agriculture USDA. [Accessed July 29, 2013];State Fact Sheets: Washington. 2013 http://www.ers.usda.gov/data-products/state-fact-sheets.aspx.
- 14.Rosenthal TC, Fox C. Access to health care for the rural elderly. JAMA. 2000 Oct 25;284(16):2034–2036. doi: 10.1001/jama.284.16.2034. [DOI] [PubMed] [Google Scholar]
- 15.Edirippulige S, Martin-Khan M, Beattie E, Smith AC, Gray LC. A systematic review of telemedicine services for residents in long term care facilities. J Telemed Telecare. 2013 Apr 23; doi: 10.1177/1357633X13483256. [DOI] [PubMed] [Google Scholar]
- 16.Nazareth S, Kontorinis N, Muwanwella N, Hamilton A, Leembruggen N, Cheng WS. Successful treatment of patients with hepatitis C in rural and remote Western Australia via telehealth. J Telemed Telecare. 2013 Feb;19(2):101–106. doi: 10.1258/jtt.2012.120612. [DOI] [PubMed] [Google Scholar]
- 17.Watanabe SM, Fairchild A, Pituskin E, Borgersen P, Hanson J, Fassbender K. Improving access to specialist multidisciplinary palliative care consultation for rural cancer patients by videoconferencing: report of a pilot project. Support Care Cancer. 2013 Apr;21(4):1201–1207. doi: 10.1007/s00520-012-1649-7. [DOI] [PubMed] [Google Scholar]
- 18.Hilgart JS, Hayward JA, Coles B, Iredale R. Telegenetics: a systematic review of telemedicine in genetics services. Genet Med. 2012 Sep;14(9):765–776. doi: 10.1038/gim.2012.40. [DOI] [PubMed] [Google Scholar]
- 19.Jodar-Sanchez F, Ortega F, Parra C, et al. Implementation of a telehealth programme for patients with severe chronic obstructive pulmonary disease treated with long-term oxygen therapy. J Telemed Telecare. 2013 Jan;19(1):11–17. doi: 10.1177/1357633X12473909. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Theobald D, Wu J, et al. Effect of telecare managemnet on pain and depression in patients with cancer: a randomized trial. The Journal of the American Medical Association. 2010 Jul;304(2):163–171. doi: 10.1001/jama.2010.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnston B, Wheeler L, Deuser J, Sousa KH. Outcomes of the Kaiser Permanente Tele-Home Health Research Project. Arch Fam Med. 2000 Jan;9(1):40–45. doi: 10.1001/archfami.9.1.40. [DOI] [PubMed] [Google Scholar]
- 22.Rojas SV, Gagnon MP. A systematic review of the key indicators for assessing telehomecare cost-effectiveness. Telemed J E Health. 2008 Nov;14(9):896–904. doi: 10.1089/tmj.2008.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGeary DD, McGeary CA, Gatchel RJ. A comprehensive review of telehealth for pain management: where we are and the way ahead. Pain Pract. 2012 Sep;12(7):570–577. doi: 10.1111/j.1533-2500.2012.00534.x. [DOI] [PubMed] [Google Scholar]
- 24.Katzman JG, Comerci G, Boyle JF, Duhigg D, Shelley B, Olivas C, Daitz B, Carroll C, Som D, Monette R, Kalishman S, Arora S. Innovative telementoring for pain management: project ECHO pain. Journal of Continuing Education in the Health Professions. 2014;34(1):68–75. doi: 10.1002/chp.21210. [DOI] [PubMed] [Google Scholar]
- 25.Scott JD, Unruh KT, Catlin MC, Merrill JO, Tauben DJ, Rosenblatt R, buchwald D, Doorenbos A, towle C, Ramers CB, Spacha DH. Project ECHO: a model for complex, chronic care in the Pacific Northwest region of the United States. J Telemed Telecare. 2012 Dec;18(8):481–484. doi: 10.1258/jtt.2012.GTH113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haozous E, Doorenbos AZ, Demiris G, et al. Role of telehealth/videoconferencing in managing cancer pain in rural American Indian communities. Psychooncology. 2012 Feb;21(2):219–223. doi: 10.1002/pon.1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doorenbos AZ, Demiris G, Towle C, et al. Developing the Native People for Cancer Control Telehealth Network. Telemed J E Health. 2011 Jan-Feb;17(1):30–34. doi: 10.1089/tmj.2010.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Medicine U. [Accessed August 8, 2013];Anesthesiology and Medicine: About Telepain. http://depts.washington.edu/anesth/care/pain/telepain/index.shtml.
- 29.Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. Journal of Advanced Nursing. 2001;33(5):668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- 30.International Association for the Study of Pain. [Accessed April 25, 2014];Curriculum Outline on Pain for Medicine. https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=729.
- 31.Agency Medical Director’s Group. [Accessed April 25, 2014];Opioid Dosing Guidelines. http://www.agencymeddirectors.wa.gov/opioiddosing.asp.
- 32.American Academy of Pain Medicine. [Accessed April 25, 2014];Clinical Guidelines. http://www.painmed.org/library/Clinical_Guidelines.aspx.
- 33.American Pain Society. [Accessed April 25, 2014];Clinical Practice Guidelines. http://www.americanpainsociety.org/resources/content/apsclinicalpracticeguidelines.html.
- 34.Federation of State Medical Boards. [Accessed April 25, 2014];Model Policy in the Use of Opioid Analgesics in the Treatment of Chronic Pain. http://www.fsmb.org/pdf/pain_policy_july2013.pdf.
- 35.Gordon DB, Loeser JD, Tauben D, Rue T, Stogicza A, Doorenbos A. Development of the KnowPain-12 Pain Management Knowledge Survey. Clin J Pain. 2013 Oct 16; doi: 10.1097/AJP.0000000000000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McCaffery M, Ferrell BR. Nurses' knowledge of pain assessment and management: how much progress have we made? J Pain Symptom Manage. 1997 Sep;14(3):175–188. doi: 10.1016/s0885-3924(97)00170-x. [DOI] [PubMed] [Google Scholar]
- 37.Williams GC, Deci EL. Internalization of biopsychosocial values by medical students: a test of self-determination theory. J Pers Soc Psychol. 1996 Apr;70(4):767–779. doi: 10.1037//0022-3514.70.4.767. [DOI] [PubMed] [Google Scholar]
- 38.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999 Nov 10;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 39.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006 May 22;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 40.Krebs EE, Bair MJ, Damush TM, Tu W, Wu J, Kroenke K. Comparative responsiveness of pain outcome measures among primary care patients with musculoskeletal pain. Med Care. 2010 Nov;48(11):1007–1014. doi: 10.1097/MLR.0b013e3181eaf835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005 Nov-Dec;6(6):432–442. doi: 10.1111/j.1526-4637.2005.00072.x. [DOI] [PubMed] [Google Scholar]
- 42.Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Franks P, Hanmer J, Fryback DG. Relative disutilities of 47 risk factors and conditions assessed with seven preference-based health status measures in a national U.S. sample: toward consistency in cost-effectiveness analyses. Medical Care. 2006;44(5):478–485. doi: 10.1097/01.mlr.0000207464.61661.05. [DOI] [PubMed] [Google Scholar]
- 44.Lubetkin EI, Gold MR. Comprehensibility of measures of health-related quality of life in minority and low-income patients. J Natl Med Assoc. 2002 May;94(5):327–335. [PMC free article] [PubMed] [Google Scholar]
- 45.Rasanen P, Roine E, Sintonen H, Semberg-Konttinen V, Ryynanen OP, Roine R. Use of quality-adjusted life years for the estimation of effectiveness of health care: A systematic literature review. Int J Technol Assess Health Care. 2006 Spring;22(2):235–241. doi: 10.1017/S0266462306051051. [DOI] [PubMed] [Google Scholar]
- 46.Furlong WJ, Feeny DH, Torrance GW, Barr RD. The Health Utilities Index (HUI) system for assessing health-related quality of life in clinical studies. Ann Med. 2001 Jul;33(5):375–384. doi: 10.3109/07853890109002092. [DOI] [PubMed] [Google Scholar]
- 47.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993 Nov;4(5):353–365. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 48.Bensink ME, Eaton LH, Morrison ML, et al. Cost Effectiveness Analysis for Nursing Research. Nursing Research. 2013;62(4):279–285. doi: 10.1097/NNR.0b013e318298b0be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Demiris G, Speedie SM, Finkelstein S. Change of patient’s perceptions of TeleHomeCare. Telemed J E Health. 2001;7(3):241–248. doi: 10.1089/153056201316970948. [DOI] [PubMed] [Google Scholar]
- 50.Little R, DBR . Statistical Analysis with Missing Data. New York City, NY: Wiley; 1987. [Google Scholar]
- 51.Raudenbush S, Bryk A, Cheong Y, Congdon R., Jr . HLM 6: Hierarchical Linear and Nonlinear Modeling. Lincolnwood, IL: Scientific Software International; 2004. [Google Scholar]


