Abstract
Purposes
The objective of this study was to evaluate the effectiveness of a streamlined interfacility referral protocol in reducing door-to-balloon (D2B) times for patients experiencing acute ST-segment elevation myocardial infarction (STEMI).
Basic Procedures
In a retrospective database review, we compared D2B times for patients requiring interfacility transfer after the implementation of a streamlined referral protocol. All patients undergoing interfacility transport with a referring diagnosis of STEMI were eligible for inclusion. Quality management databases were reviewed by trained abstractors using standardized data entry forms for D2B times from July 2009 through June 2010. Median D2B times with interquartile ranges are reported.
Main Findings
A total of 133 patients exhibited complete data and were included in the analysis, 54 of which were transferred via the streamlined referral protocol. Streamlined referral patients exhibited a median D2B time of 101 minutes (interquartile range, 88–128) vs a median D2B time of 122 minutes (interquartile range, 99–157) for the traditional referral group (P = .001). Door-to-balloon times of 90 minutes or less were achieved in 13% of the traditional referral patients and in 30% of the streamlined protocol group (odds ratio, 2.9; 95% confidence interval, 1.2–7).
Principal Conclusion
The implementation of a streamlined referral protocol has significantly reduced D2B times for patients diagnosed with STEMI that required interfacility transport for intervention.
1. Introduction
Increased attention has been focused on reducing door-to-balloon (D2B) times for patients experiencing ST-segment myocardial infarction (STEMI). Percutaneous coronary intervention (PCI) has been shown to be more effective than thrombolytic therapy for the treatment of STEMI [1,2], and delays in D2B time can result in a significantly increased mortality risk. Rathore et al [3] evaluated the National Cardiovascular Registry for in-hospital mortality and found that adjusted in-hospital mortality for patients with D2B times of 90, 120, and 180 minutes was 4.3%, 5.6%, and 8.4%, respectively. Given this link between mortality risk and delay in definitive therapy, national guidelines recommend a target D2B time of 90 minutes [4] for patients that present to hospitals with PCI capabilities. Unfortunately, this target time is often not met.
One factor that results in significant delays in D2B time is the time required to transport a patient that presents to a hospital without PCI capability to one capable of performing PCI. Although most of the adult population in the United States lives within 60 minutes of a PCI-capable hospital, approximately 21% of adults do not [5]. For this significant minority, transport to a closer facility capable of providing PCI is often the norm. In this group requiring an additional care transition, the 90-minute D2B time is rarely achieved. Given the significant morbidity and mortality associated with delays in definitive therapy, more efficient hospital transport protocols are needed to bring D2B times closer to the 90-minute standard.
Several hospitals or health systems have reported strategies to decrease D2B times, which have focused on referral or transport processes. These strategies have reduced D2B times with only 1 hospital reporting a reduction meeting the 90-minute D2B time [6]. Other reported times ranged from 95 to 120 minutes [7–11]. In spite of these advances, D2B times in general for patients undergoing interfacility transport by air are still suboptimal [12]. A recent multicenter review revealed a median D2B time for patients requiring interfacility transport by air of 131 minutes [12]. This study called for continued exploration of strategies to reduce transport and referral times. The objective of this study is to determine the effect of a streamlined referral protocol on D2B time for patients experiencing STEMI that present to non-PCI performing hospitals.
2. Methods
2.1. Design
This was a retrospective cohort study involving a quality monitoring database review as part of an initiative to improve D2B times for patients with acute STEMI. Two cohorts were analyzed after implementation of the streamlined referral protocol: patients transferred using the streamlined protocol and patients referred through the traditional referral process.
The setting for this investigation was a 1300-bed Midwest tertiary care center that serves as a regional referral center in Northeast Ohio. The cardiac catheterization laboratory is fully staffed weekdays, with on-call staffing for nights and weekends. The hospital operates a hospital-based critical care transport (CCT) team consisting of 2 helicopters and 1 ground ambulance that operate 24 hours a day 7 days a week. One helicopter and the ambulance are stationed at the main hospital, whereas the other helicopter is located 35 miles away at a community hospital. All CCT crews are staffed with an acute care nurse practitioner and critical care registered nurse and/or critical care paramedic.
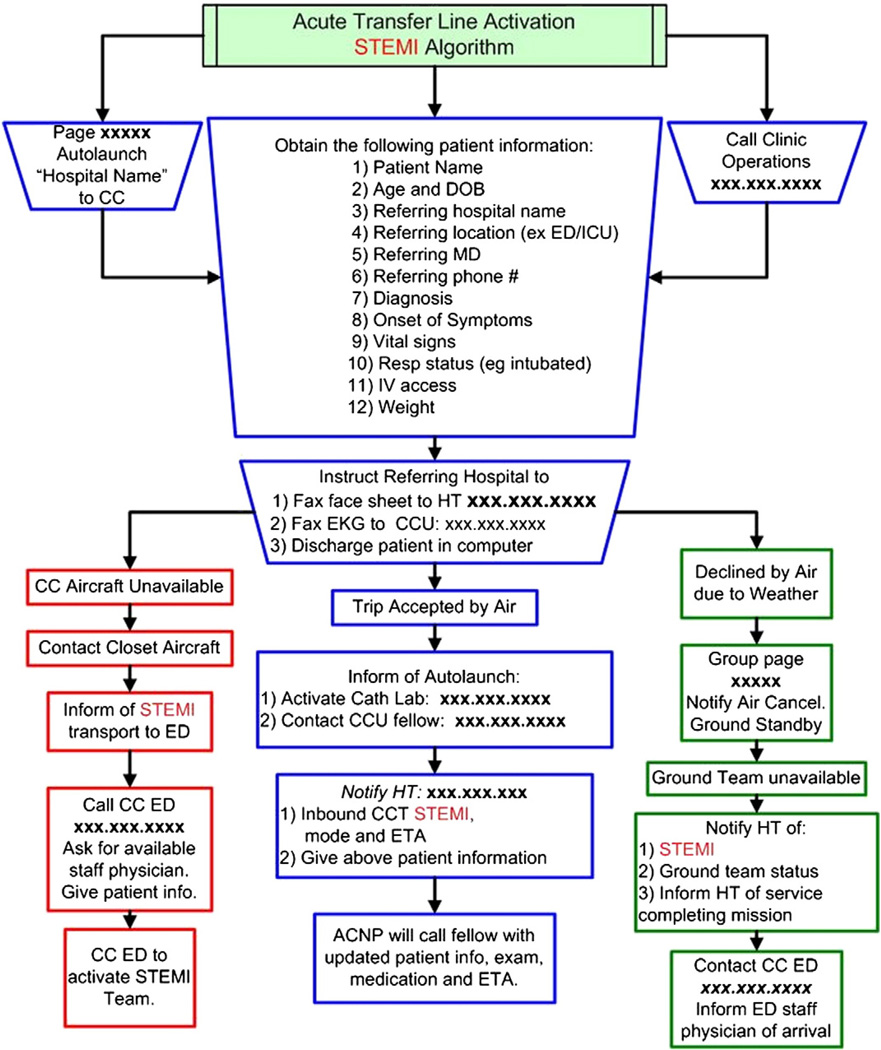
The traditional referral protocol was reviewed to identify areas for improvement by the transport team and cardiology management team. This protocol processed time-sensitive patient transfer requests the same as all other transfer requests. It consisted of 21 steps with an average time to complete of 42 minutes, ranging from 23 to 64 minutes. An abbreviated streamlined protocol was then developed (Fig. 1) bypassing the usual hospital transfer process and incorporated 2 of 6 recommendations from Bradley et al [13]. These recommendations provided the ability for the referring emergency department (ED) physician to activate the streamlined protocol as well as for entire system activation based on one phone call.
Fig. 1.
STEMI Streamlined Referral Protocol.
In brief, referring facilities were provided with a contact telephone number linked directly to a CCT coordinator via a hotline dedicated to streamlined referrals. Upon receiving a hotline request, the coordinator obtains patient information, location, and simultaneously dispatches the aircraft. The coordinator also instructs the referring hospital to fax the patient's electrocardiogram to the coronary care unit and a demographic sheet to the hospital transfer center. The aircraft is dispatched without regard for bed availability and without accepting physician communication before dispatch. While the transport is taking place, the coordinator activates the catheterization laboratory to reserve a table or to activate the on-call team and then contacts the on-call cardiologist to inform them of the referral and information regarding the referring facility.
2.2. Study sample
All patients undergoing transport by helicopter or ground for acute STEMI to the Cleveland Clinic for emergent PCI by the hospitalbased CCT team from July 2009 through June of 2010 were eligible for this study. As this was a quality improvement project, the study was granted exemption from further review by the institutional review board.
2.3. Data sources
A hospital-based CCT log was used to track all streamlined cases for acute STEMI. This log was created as part of a quality improvement initiative for the hospital-based CCT program and includes data on all transports conducted by the program. The transport log is completed at the end of each patient transport mission by the medical crew. These data are directly entered into a standardized computer-based data collection form using information directly from the chart generated during the transport. Each mission is logged with the nature (streamlined vs traditional) and time of the receiving call from the referring hospital, the referring diagnosis and facility, and the time and final clinical disposition of the patient. This is a secure database, and data are locked from further editing once submitted into the log. A single CCT team member with prior experience in data management was responsible for management, security, and quality maintenance of the database.
A data subset of all streamlined cases was abstracted from this larger database and maintained by 1 team member responsible for monthly tracking and reporting of all streamlined missions and times. Retrospective analysis of the main CCT log was conducted to identify all STEMI transfers for 12 months following implementation of the streamlined protocol. Medical record numbers in this database were then used to match patients in this data subset with the hospital's acute myocardial infarction (AMI) database to identify D2B times. The hospital-based AMI database is a cardiology driven and managed quality database to track D2B times for all STEMI referrals from all sources. This database is constructed using medical records from both the referring and receiving facilities by a data collection nurse with expertise in data abstraction and management for these purposes. Only patients with a referring diagnosis of STEMI and a positive cardiac catheterization defined as coronary artery occlusion deemed to be associated with an acute coronary syndrome by the interventional cardiologist are included in this database.
Door-to-balloon times were analyzed between 2 groups, those transferred via the streamlined referral protocol and those transferred via the traditional referral process. Any case appearing in the CCT STEMI log but not in the AMI database is reviewed using the hospitals electronic medical record for cardiac catheterization findings to determine the rate of false-positive activation of the streamlined STEMI protocol. Only cases that had complete data entered into the CCT STEMI log and AMI database were included for analysis.
2.4. Outcome measures
The primary outcome variable, D2B time, was defined as the time from arrival at the referring facility to the time of percutaneous coronary intervention. Additional outcomes included analysis of door-in door-out times, transport times, and catheterization laboratory times. Door-in door-out time is defined as the total admission time of the patient at the referring hospital, beginning when the patient is first documented as arriving to the referring hospital and ending when the patient is discharged to the care of the transport team. Transport time is the time from discharge from the referring hospital to arrival in the catheterization laboratory. Catheterization laboratory time is the time of arrival in the laboratory to percutaneous coronary intervention. All time interval data were abstracted from the AMI database.
2.5. Statistical analysis
We calculated median time and interquartile ranges for each time interval in minutes. Categorical data are presented as absolute and relative frequencies. The Shapiro-Wilk test was used to assess normality. The data were nonnormally distributed. Log transformations of the time data were then performed and normality reassessed, with 2 time intervals still remaining nonnormally distributed. Therefore, differences between groups were assessed using the nonparametric Mann-Whitney U test and Fisher exact test for categorical data. We set α at .05 to determine significance. All analyses were performed using IBM SPSS Statistics (IBM SPSS Statistics 20, 2011, Armonk, NY).
3. Results
From July 2009 through June 2010, a total of 225 cases were entered into the AMI database. Of those cases, 33 originated in the main hospital ED, and another 59 cases exhibited incomplete data, resulting in a total study sample of 133 patients. There were no statistically significant differences in demographics between groups (Table 1). Fifty-four patients were transferred through the streamlined referral process as opposed to 79 through the traditional referral process. Time intervals and between-group differences are presented in Table 2. Overall, D2B times were significantly reduced for patients who were transferred via the streamlined referral process. Door-to-balloon times of 90 minutes or less were achieved in 13% of the traditional referral patients and in 30% of the streamlined protocol group (odds ratio, 2.9; 95% confidence interval, 1.2–7).
Table 1.
Patient demographics
| Traditional transfer (n = 79) |
Streamlined transfer (n = 54) |
P* | Incomplete data streamlined transfers (n = 24) |
|
|---|---|---|---|---|
| Sex (female) | 57 (72%) | 35 (65%) | .37 | 88 (33%) |
| Age, median (IQR) | 61 (50–72) | 55 (49–64) | .09 | 61 (53–74) |
| Race (white) | 61 (77%) | 35 (65%) | .3 | 13 (54%) |
| Mortality (died) | 5 (6%) | 2 (4%) | .51 | 2 (8%) |
Categorical data presented as frequency and (%) of group. IQR means interquartile range.
Significance testing is only between the traditional transfer and streamlined transfer groups.
Table 2.
Time intervals
| Traditional transfer (n = 79) |
Streamlined transfer (n = 54) |
P | |
|---|---|---|---|
| ED | 60 (45–84) | 55 (44–67) | .07 |
| Transport | 28 (20–42) | 25 (20–35) | .08 |
| Catheterization laboratory | 25 (19–31) | 24.5 (18–29) | .39 |
| D2B time | 122 (99–157) | 101 (88–128) | .001 |
Data reported in minutes as median (25%–75% interquartile range). Emergency department time is total time patient spent in referring department, including time waiting for arrival of transport team. Transport time is the 1-way time from referring hospital to accepting catheterization laboratory. Catheterization laboratory time is the time of arrival in laboratory to PCI. Door-to-balloon time is total time from presentation at outside ED to PCI.
Of the 59 cases with incomplete data, 24 were identified in the streamlined transfer log but had no corresponding AMI database log entry. Of the 24 streamlined referrals with no corresponding AMI database entry, 3 underwent PCI. The other 35 cases had incomplete times entered in the AMI database that prevented analysis of the time intervals. Of those remaining 35 patients with incomplete data, 18 patients underwent catheterization with 5 patients progressing to surgical intervention while the other 13 received medical management and/or were discharged home, never receiving cardiac catheterization. In addition, 1 patient underwent catheterization and was transferred to another hospital for surgical intervention, and 3 patients were transferred to non–health system hospitals prohibiting follow-up. The 13 patients who did not undergo cardiac catheterization were considered false-positive referrals for STEMI, resulting in a 9.7% (13/133) over triage rate.
4. Discussion
This study adds to a small but growing body of literature demonstrating the potential of streamlined referral transport systems to reduce D2B times much closer to the 90-minute standard for patients experiencing STEMI [7–9]. The streamlined group exhibited a significantly lower median D2B time when compared with the traditional transport group during the same period. When compared with other studies including both ground and air transport modalities, the median D2B time of 101 minutes is lower than the reported medians, which ranged from 115 to 128 minutes [7–9]. Given the current American Heart Association guidelines for D2B times, however, further process improvement efforts are needed. Additional reductions in D2B time may be achieved by focusing on each step of the transport process and adapting practices that will contribute to reducing the total transport time.
Herrin at al [14] reported that only 9.7% of patients from a national sample achieved less than 30-minute ED door-in to door-out times. This study population further supported that achieving less than 30 minute referring ED times is difficult, with only 3 of the 133 patients achieving this time goal. McGrath et al [15] analyzed factors that prolonged bedside times and total mission time. Factors considered not amenable to change included from the time of request to transport, time to arrival of the transport team, and then leaving with the patient from the referring agency to arrival to the catheterization laboratory. Stated differently, the travel time for the transport team, usually in a helicopter, entails a minimum fixed travel time that cannot be improved upon.
The streamlined referral group did experience a 3-minute reduction in median transport; however, overall D2B times were reduced by 21 minutes. Although not measured in this study, time savings may have been achieved during the transport team activation and transport crew response period. The transport team activation to time-of-arrival at patient bedside is subsumed within the ED period: the largest reduction in time between the clinical cohorts is the 17- minute reduction in the 75% quartile in the streamlined cohort, with an overall 5-minute time savings for the streamlined cohort.
One factor identified as having the potential for improvement is the transport team bedside time or time spent in the referring ED. Several suggestions provided to decrease bedside time include facilitating communication between the referring care providers and transport crew and having predefined lists of task and required documentation ready for the transport team upon their arrival. Implementing one or all of these suggestions may further improve overall D2B times [15].
Current American Heart Association guidelines call for thrombolytic therapy as the primary reperfusion modality when D2B times exceed 90 minutes in STEMI patients received in transfer from another hospital [16]. Unfortunately, current interfacility transport protocols still frequently result in patients receiving PCI as primary reperfusion therapy beyond the 90-minute recommended guideline [12]. In spite of improved D2B times after implementation of the streamlined referral protocol, a significant number of patients received PCI beyond the 90-minute guidelines. To best serve these patients in the future, plans for further refinement of the streamlined program will include the development of a fibrinolytic therapy protocol. Pinto et al [17] reported that odds of death for patients receiving PCI were equal to those receiving fibrinolysis at around 114 minutes. It is important to prospectively identify those patients who cannot be transported to a catheterization laboratory within 90 minutes as recommended [16] or possibly out to 114 minutes, which would capture 61% (33/54) of the current study population. Delays in transport can be attributed to factors such as distance, inclement weather, availability of a transport team, or delay in arrival of catheterization laboratory personnel. Prospectively identifying those patients that will not arrive in 90 to 114 minutes can facilitate the recommendation of administering fibrinolytics at the time of initial call for transport.
4.1. Limitations
This was a retrospective chart review and, as such, limited only to patient records that were able to be linked across all documentation sources. Patients without complete data may have experienced different D2B times. In addition, this was a quality improvement project with results that are specific to our program. Finally, reasons for referring STEMI patients via the streamlined vs traditional referral protocol were not explored and could include other variables influencing D2B time differences between groups.
5. Conclusions
Several approaches have been implemented through transport programs and PCI-capable hospitals to reduce D2B times for patients experiencing AMI. Analysis of the previous referral process identified areas for improvement and resulted in the development of a streamlined referral protocol. Implementation of this streamlined referral protocol significantly reduced D2B times for patients presenting to non-PCI performing facilities experiencing STEMI.
Footnotes
Prior presentations: Critical Care Transport Medicine Conference, Nashville, TN, April 2 to 4, 2012.
References
- 1.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 2.Grines CL, et al. A randomized trial of transfer for primary angioplasty versus onsite thrombolysis in patients with high-risk myocardial infarction: the Air Primary Angioplasty in Myocardial Infarction study. J AmColl Cardiol. 2002;39(11):1713–1719. doi: 10.1016/s0735-1097(02)01870-3. [DOI] [PubMed] [Google Scholar]
- 3.Rathore SS, et al. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:b1807. doi: 10.1136/bmj.b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kushner FG, et al. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120(22):2271–2306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 5.Nallamothu BK, et al. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation. 2006;113(9):1189–1195. doi: 10.1161/CIRCULATIONAHA.105.596346. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed B, et al. Consistent door-to-balloon times of less than 90 minutes for STEMI patients transferred for primary PCI. J Invasive Cardiol. 2009;21(9):429–433. [PubMed] [Google Scholar]
- 7.Aguirre FV, et al. Rural interhospital transfer of ST-elevation myocardial infarction patients for percutaneous coronary revascularization: the Stat Heart Program. Circulation. 2008;117(9):1145–1152. doi: 10.1161/CIRCULATIONAHA.107.728519. [DOI] [PubMed] [Google Scholar]
- 8.Ting HH, et al. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the Mayo Clinic STEMI Protocol. Circulation. 2007;116(7):729–736. doi: 10.1161/CIRCULATIONAHA.107.699934. [DOI] [PubMed] [Google Scholar]
- 9.Jollis JG, et al. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA. 2007;298(20):2371–2380. doi: 10.1001/jama.298.20.joc70124. [DOI] [PubMed] [Google Scholar]
- 10.Henry TD, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116(7):721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 11.Blankenship JC, et al. Rapid triage and transport of patients with ST-elevation myocardial infarction for percutaneous coronary intervention in a rural health system. Am J Cardiol. 2007;100(6):944–948. doi: 10.1016/j.amjcard.2007.04.031. [DOI] [PubMed] [Google Scholar]
- 12.McMullan J, et al. Reperfusion is delayed beyond guideline recommendations in patients requiring interhospital helicopter transfer for treatment of ST-segment elevation myocardial infarction. Ann Emerg Med. 2010;57(3):213–220. doi: 10.1016/j.annemergmed.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 13.Bradley EH, et al. Achieving door-to-balloon times that meet quality guidelines: how do successful hospitals do it? J Am Coll Cardiol. 2005;46(7):1236–1241. doi: 10.1016/j.jacc.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Herrin J, et al. National performance on door-in to door-out time among patients transferred for primary percutaneous coronary intervention. Arch Intern Med. 2011;171(21):1879–1886. doi: 10.1001/archinternmed.2011.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGrath CP, Rosen GS, Bechtel GA. Improving bedside to departure care in air transport of ST segment elevation myocardial infarction patients: a 2-year retrospective study of performance. Air Med J. 2010;29(2):84–87. doi: 10.1016/j.amj.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Antman EM, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction) Circulation. 2004;110(5):588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 17.Pinto DS, et al. Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy. Circulation. 2006;114(19):2019–2025. doi: 10.1161/CIRCULATIONAHA.106.638353. [DOI] [PubMed] [Google Scholar]