Abstract
Background: Mobile health (m-health) utilizes widespread access to mobile phone technologies to expand health services. Community health workers (CHWs) provide first-level contact with health facilities; combining CHW efforts with m-health may be an avenue for improving primary care services. As part of a primary care improvement project, a pilot CHW program was developed using a mobile phone-based application for outreach, referral, and follow-up between the clinic and community in rural Zambia. Materials and Methods: The program was implemented at six primary care sites. Computers were installed at clinics for data entry, and data were transmitted to central servers. In the field, using a mobile phone to send data and receive follow-up requests, CHWs conducted household health surveillance visits, referred individuals to clinic, and followed up clinic patients. Results: From January to April 2011, 24 CHWs surveyed 6,197 households with 33,304 inhabitants. Of 15,539 clinic visits, 1,173 (8%) had a follow-up visit indicated and transmitted via a mobile phone to designated CHWs. CHWs performed one or more follow-ups on 74% (n=871) of active requests and obtained outcomes on 63% (n=741). From all community visits combined, CHWs referred 840 individuals to a clinic. Conclusions: CHWs completed all planned aspects of surveillance and outreach, demonstrating feasibility. Components of this pilot project may aid clinical care in rural settings and have potential for epidemiologic and health system applications. Thus, m-health has the potential to improve service outreach, guide activities, and facilitate data collection in Zambia.
Key words: : e-health, information management, technology, telehealth
Introduction
Mobile health (m-health) is a growing field using the ubiquity of low-cost mobile phone technologies to connect health services and patients. Mobile phone subscriptions were held by 96% of the world's population in 2013, including 89% penetration in the developing world.1 Zambia is no exception, with 78% of urban and 40% of rural populations owning a mobile phone in 2010.2 Mobile phones have been widely used in health-related settings3 to improve clinical guidance via electronic care algorithms,4 affect patient behaviors,5–8 and collect data.9,10 However, proportionally few trials have crossed from pilot phase to scale11 or covered multiple diseases or components of care.12,13
Community health workers (CHWs) have been successfully used in varied primary healthcare interventions in developing countries.14–16 Coupling mobile phone technology with CHWs is a particularly underdocumented area. Intuitive advantages include standardizing data collection, on-the-go clinical guidance, and linking the field to central sites. Presented here is the overview of a CHW program using mobile phone technology to improve clinical guidance, data collection, and patient services between community and clinic. Preliminary results also demonstrate feasibility of the CHW pilot program, which was one part of a large-scale primary healthcare cluster randomized stepped-wedge trial in Lusaka Province, Zambia.
Materials and Methods
Program Context: Better Health Outcomes Through Mentoring and Assessment
In August 2010, a new system of CHW activities was initiated at six pilot sites in three rural Zambian health districts (Chongwe, Kafue, and Luangwa), with an estimated population of 456,017.17 A description of the overall project, Better Health Outcomes through Mentoring and Assessment (BHOMA), has been reported elsewhere.18 In brief, BHOMA is a stepped-wedge cluster randomized trial to improve clinical care quality, with interventions at both rural primary care facilities and the community. The primary outcome is overall mortality, with secondary outcomes of mortality by population, prevalence of malaria in children under five years old, and proportion of human immunodeficiency virus (HIV)-positive patients with controlled disease. The intervention phase began in April 2011 and will continue through 2014. This description covers the pre-implementation pilot project, from August 2010 to April 2011.
Pilot CHW Program
The CHW program was one of multiple community pilot interventions involved in the BHOMA trial. The goal was to strengthen connections between the clinic and community through patient follow-up and referral, and to emphasize early treatment and referral of ill individuals via routine household visitation. The program was organized around rural and periurban health clinic sites and their surrounding catchment areas, typically a less than four kilometer radius around a facility.
Prior to this program, the Ministry of Health (MoH) supported volunteer CHWs at all public clinics. Their activities included surveillance, referral, and follow-ups in a catchment area, but often with nonstandardized, paper systems. With endorsement from the MoH, these CHWs were incorporated where possible, and new CHWs (two on average) were recruited as needed to bring the total employed to four per site. Each CHW was responsible for surveying approximately 500 households using bicycles provided by the program.
Data Sources and System
At each facility, standardized patient care forms were introduced for pediatric, adult, general antenatal, ill antenatal, and labor and delivery visits. These forms were modeled on the Integrated Management of Childhood, Adolescent and Adult Illnesses (IMCI/IMAI) and highlighted IMCI/IMAI-defined “danger signs” such as fever.19,20 Simple touch screen computers (model 615; J2 Retail Systems Inc., Irvine, CA) were placed at each facility for data entry. Following a patient visit, support staff entered the completed paper forms on these computers, connected with a local network to another small computer (model fitPC2 Revision 1.4; CompuLab Ltd., Yokneam Elite, Israel) acting as a local server for data storage. Transmission from local to central server occurred over cellular modems (model E220; Huawei Technologies Co. Ltd., Shenzhen, Guangdong, China) to send encrypted data packets over general packet radio service (GPRS) using the existing cellular network to access the Internet. From the central server, data were transmitted back to district servers for storage and to allow viewing of aggregate reports. Server data storage was done with CouchDB database software (Apache Software Foundation, Forest Hill, MD).
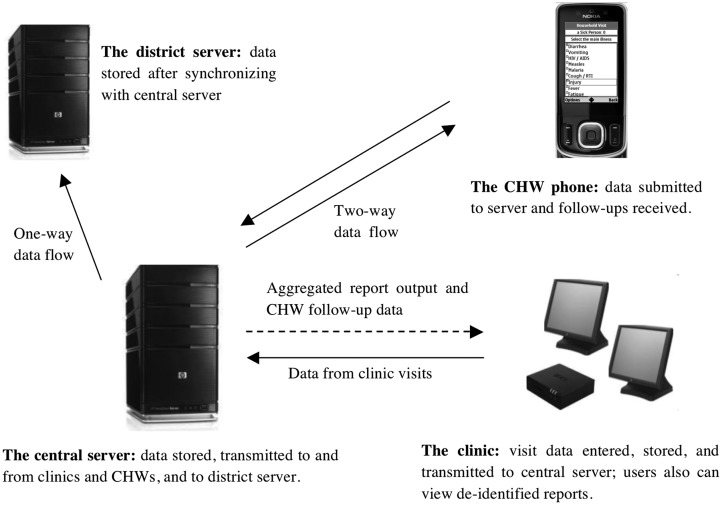
In the community around participating health clinics, CHWs captured data using survey instruments programmed onto a mobile phone provided by the project. The surveys were created with existing free, open-source software called CommCare™ (Dimagi, Inc., Charlestown, MA) that runs on Java-enabled phones.21 Four surveys were developed: a household visit, patient follow-up, referral, and monthly activity summary. The surveys collected data on demographics, disease symptoms and severity, and care-seeking behaviors and correlated with the patient clinic visit forms. Survey responses also cued preset clinical guidance incorporated from the IMCI/IMAI, following the World Health Organization's validated approach.22,23 In the field, CHWs entered surveys on mobile phones in “real time” to document the client interview. Completed surveys were submitted if cellular network coverage was available. If not, or if the phone was powered off, the data were temporarily stored on the phone until network coverage became available and then removed after submission. Data were transmitted to the central server via GPRS and then back to the district servers. Pilot CHWs' data fees were prepaid monthly by the project. There were two main outputs for both clinic and CHW data after reaching the central and district servers. First, authorized users could view data at the clinic and program offices for performance reporting. Second, a list of follow-up requests was sent from the central server to a mobile phone via GPRS each time the CHW synchronized his or her phone with the server, as presented in Figure 1. Follow-up requests were based on specific criteria (Table 1) applied to patient visits at the clinic.
Fig. 1.
Overview of the data system involved in a community health worker (CHW) program using a mobile phone application to guide follow-up, referral of patients, and household visitation. Data were transmitted from the CHW and clinic to a central server via general packet radio service, which could then send back data to the CHW for follow-ups, to the clinic for monitoring reports, and to the district server for storage.
Table 1.
Criteria for Follow-Up Cases Applied to Patient Visits at a Participating Health Facility
| FOLLOW-UP CASE CRITERIA | WHEN FOLLOW-UP CASE SENT TO PHONE | WINDOW BEFORE CASE LOST TO FOLLOW-UP |
|---|---|---|
| Provider asked patient to return to the clinic in <5 days and appointment missed | 3 days after missed return appointment date | 6 weeks after sent to phone |
| Serious symptoms at presentation, provider set return visit in ≥5 days, and appointment missed | 3 days after missed return appointment date | 6 weeks after sent to phone |
| Serious symptoms at presentation and patient referred to another facility | 9 days after initial visit to primary care facility | 6 weeks after sent to phone |
| Pregnancy case with no birth outcome reached by 40 weeks of gestational age | 40 weeks after recorded last menstrual period | 4 weeks after sent to phone |
If a visit met the criteria, follow-ups were sent automatically to a community health worker's mobile phone after routing through a central server. Symptom severity was based on the Integrated Management of Childhood, Adolescent and Adult Illnesses for predefined patient “danger signs,” applied to clinic visit forms.
The initial version (version 1.0) of the software for the mobile phones and clinics was implemented in August 2010. A revised version (version 2.0) was implemented in January 2011. Clinic software upgrades could be done manually or remotely via a secure shell protocol to connect to the central server. The phone application required manual updates after initial set-up. Trained program staff provided technical support. Solar power was supplied, including for charging mobile phones, at any facility where no national power grid was accessible.
CHW Activities
Quarterly household surveillance visits
Each CHW was responsible for surveying all households within his or her catchment area on a quarterly basis, with a goal of identifying and referring individuals in need of care from either second-hand interview or direct evaluation. Household surveys were conducted with any adult household member. Separate interviews or surveys could be conducted as needed for referrals or clinic follow-up visits. Referral eligibility was based on MoH guidelines24 and included patients with certain symptoms (e.g., cough with fast respiratory rate), pregnant women not under care, and HIV-infected individuals not enrolled in care.
Follow-up requests
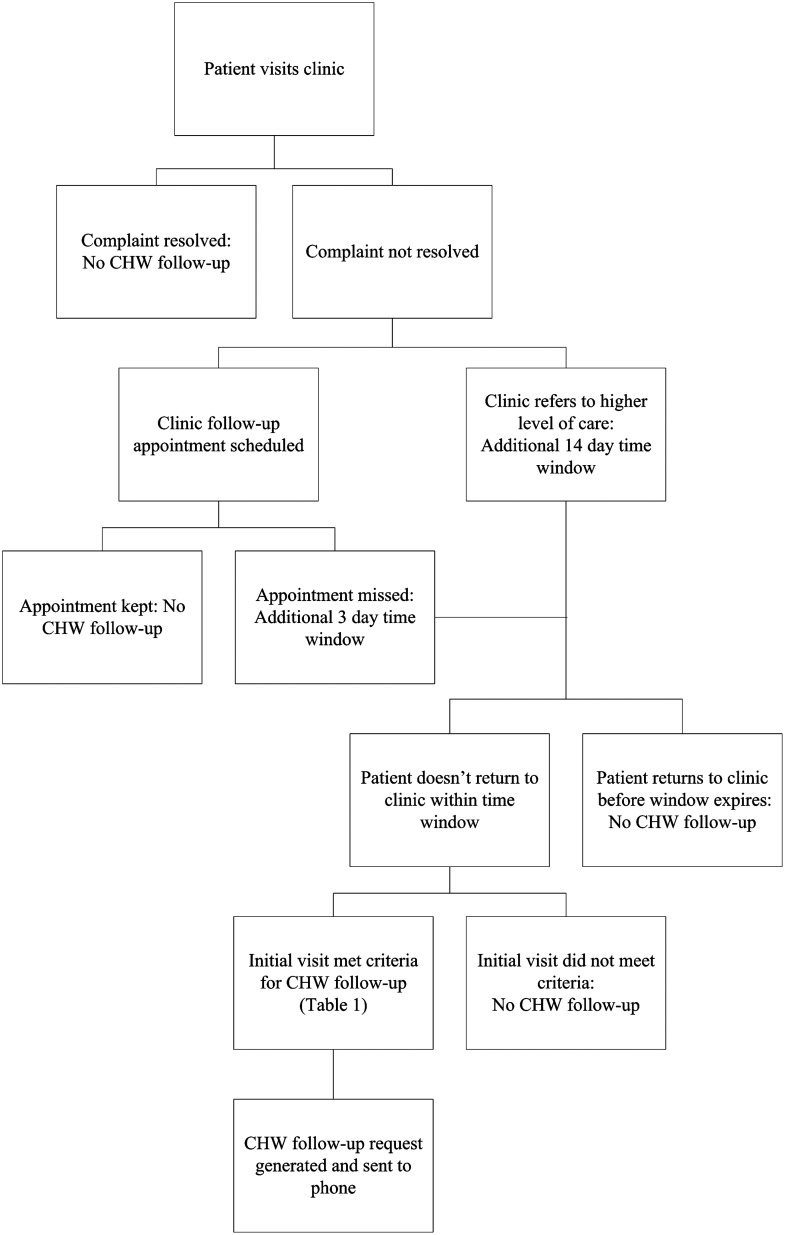
At the clinic, patient data were entered at the conclusion of a visit. If preset criteria were met, such as “danger signs” at the clinic visit, the software could automatically generate a follow-up request intended for the CHW's mobile phone. This request was sent to the phone only after a set period of time had elapsed wherein the patient could return to the clinic (Fig. 2); a patient's timely return to the clinic (and subsequent entry of patient data) was recognized by the software, which then “closed” the case. If the patient failed to return within the allotted time window, the follow-up request was transmitted to the phone with a target date for the CHW to interview the patient (usually three to five days after the missed clinic appointment). An interval of four to six weeks given to complete the request before the case was classified as lost to follow-up. The case was closed by the CHW when the CHW reported one of the following patient outcomes: the illness resolved (via CHW direct evaluation), death, movement from the area, or refusal of interview. If a CHW was unable to locate a patient in person or referred the patient back to clinic or if an illness was unresolved at follow-up, the case remained active on the phone and in the central database until an outcome was recorded (either at the clinic or by the CHW) or the follow-up window expired.
Fig. 2.
Flowchart for creating a community health worker (CHW) mobile phone follow-up request. If a patient complaint (illness or pregnancy-related) was not resolved at the clinic, a referral to a higher level of care or a follow-up clinic appointment could be scheduled. For those patients who had initial clinic visits that met the criteria for severity, a potential CHW follow-up was generated by the software. If a patient then missed the return clinic appointment or had been referred to a higher-level facility, a short-term additional window was then given for the patient to return to the clinic. If the patient did not return to the clinic in this window, the follow-up request was then released to the CHW mobile phone.
Referrals and monthly activity survey
During either a routine household or a follow-up visit in the community, CHWs could refer clients with a concerning history and/or exam finding to the clinic using a separate referral survey on the mobile phone. This generated an ID number at survey completion, which the CHW wrote onto a paper form for the client to take to the facility, to allow tracking of those who returned to the clinic. The CHW had the ability to designate a referral as “life-threatening,” a distinction tracked to evaluate if it would impact referral outcomes. CHWs also submitted a monthly survey of self-reported activities, including travel time and patient visits, with an opportunity for feedback or reporting problems. This monthly survey was for troubleshooting and monitoring only.
Program Monitoring and Data Analysis
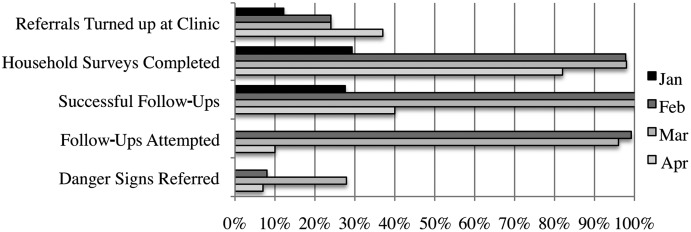
Program monitoring occurred both at the sites and centrally. A team leader elected by the CHWs at each site was responsible for conducting bimonthly progress meetings with other CHWs. A trained clinic nurse held an additional monthly meeting at the clinic with all the CHWs. Individual performance reports were created for these meetings based on data submitted at both the facility and community, describing aspects such as patient attendance at clinic after CHW referral or number of follow-up requests completed. The reports were visible centrally at the program offices, at the MoH district offices, and at the individual clinics. A sample aggregated performance report is shown in Figure 3.
Fig. 3.
Aggregated average performance report for 22 of 24 community health workers at pilot clinics from January to April 2011. Data submitted by the community health workers and from patient visits at the clinic were aggregated into graphical de-identified reports used for performance evaluation and monitoring in scheduled meetings with each community health worker.
This analysis was limited to information collected in version 2.0 of the database, which ran from its initial deployment on January 27, 2011 to the freeze date of May 1, 2011. Patient-level information was excluded from version 1.0 because of concerns around data reliability during the introductory training period. The analysis was conducted using SAS version 9.1 software (SAS Institute, Cary, NC). Ethical approval for the project was granted through the University of Zambia Biomedical Research Ethics Committee (Lusaka, Zambia), the University of North Carolina at Chapel Hill Institutional Review Board (Chapel Hill, NC), and the University of Alabama Birmingham Institutional Review Board (Birmingham, AL).
Results
Quarterly Surveillance Household Visits
Between January and April 2011, 24 CHWs conducted and submitted data for 6,197 routine household visits (mean, 100 visits per month per CHW), representing 33,304 total household members, including 6,294 children (under 5 years). In total, two deaths were reported through routine household visits during these months, both of children less than one year old.
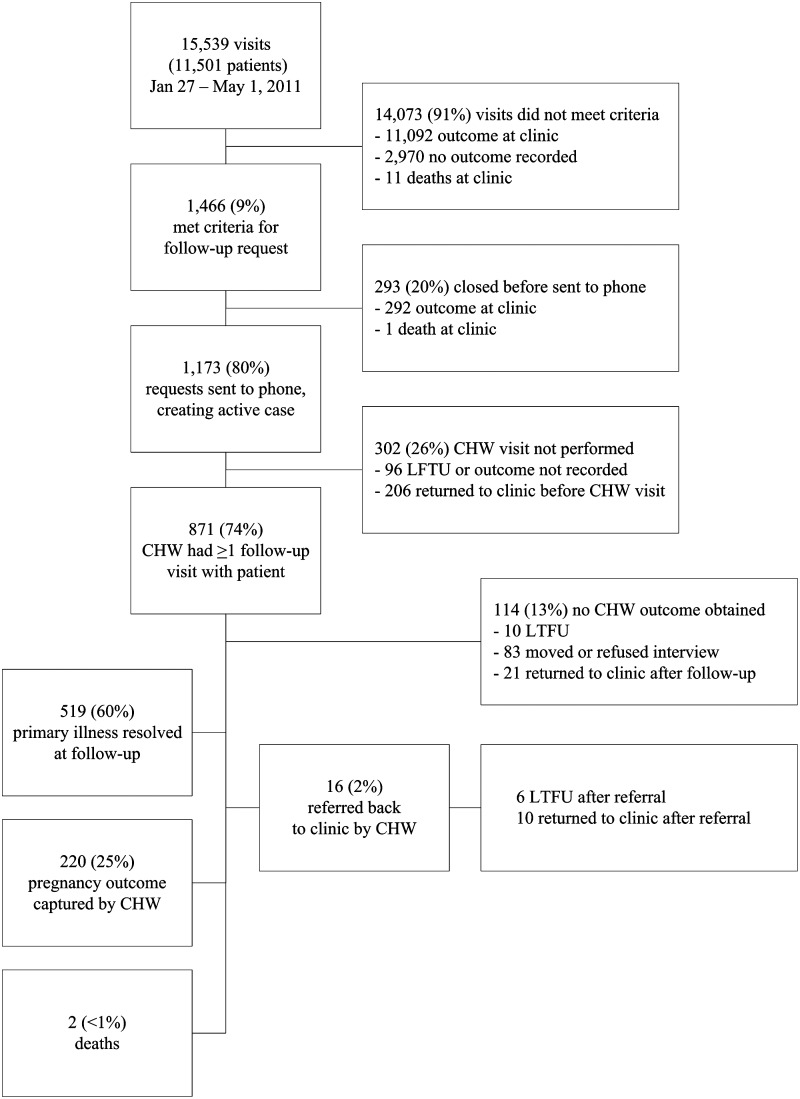
Community Follow-Up After a Clinic Visit
There were a total of 15,539 clinical visits at the six pilot facilities over the course of the study period (Fig. 4), representing 11,501 individuals with at least one clinic visit. Of these visits, 1,466 (9%) met criteria (Table 1) for a CHW follow-up visit. Prior to a request being transmitted to the phone, 293 potential cases were closed by a patient returning to the clinic on his or her own. Overall, 1,173 clinic visits resulted in an active follow-up request being generated and sent to a phone, and CHWs were able to have at least one visit with 873 cases. In total, CHWs interviewed and obtained outcomes on 741 of 1,173 (63.2%) of the requests. Another 237 (20.2%) outcomes were subsequently obtained at the clinic, either after an initial CHW interview and subsequent patient return to clinic (n=31) or by a patient returning to clinic before the CHW completed the follow-up (n=206). The remaining 195 (16.6%) cases were without an outcome (including those who left the area, who refused interview, or were lost to follow-up). Either at CHW follow-up or at the clinic, 14 deaths were recorded (Table 2).
Fig. 4.
Flowchart of clinic visits that generated requests for community health worker (CHW) follow-up. After cases met the criteria for follow-up, their data were sent to a CHW mobile phone, and resolution was reached through a CHW completing the request, the patient returning to the clinic, or expiration of the request after four to six weeks. LTFU, lost to follow-up.
Table 2.
Deaths Recorded at the Clinic or at Follow-Up with a Community Health Worker, with an Initial Clinic Visit January 27 to May 1, 2011
| AGE (YEARS) | SEX | DIAGNOSIS AT CLINIC | DETAILS |
|---|---|---|---|
| 0 | M | Other ear/nose/throat problem | Died at the clinic during first clinic visit |
| 0 | F | Acute diarrhea | Died at the clinic during first clinic visit |
| 1 | F | Not recorded | Died at the clinic during first clinic visit |
| 6 | M | Other | Danger signs noted at presentation. Died at the clinic during visit; had previously been seen at the clinic for same illness |
| 9 | M | Other | Died at the clinic during first clinic visit |
| 17 | F | Other | Died at the clinic during first clinic visit |
| 20 | F | Not recorded | Died at the clinic during first clinic visit |
| 33 | M | Not recorded | Referred to an outside facility. Death recorded at CHW follow-up 10 days after clinic visit |
| 35 | M | Wasting syndrome | Died at the clinic during first clinic visit |
| 40 | M | Other | Died at the clinic during first clinic visit |
| 40 | F | Not recorded | Danger signs noted at the first clinic visit, referred to an outside facility. Death recorded at CHW follow-up 23 days after clinic visit |
| 57 | F | Other | Died at the clinic during first clinic visit |
| 62 | M | Not recorded | Died at the clinic during first clinic visit |
| 68 | F | Hypertension | Died at the clinic during first clinic visit |
CHW, community health worker; F, female; M, male.
At initial CHW follow-up, reported resolution of the primary illness from a clinic visit (n=519) was more likely in pediatric (<15 versus ≥15 years: odds ratio [OR]=1.50; 95% confidence interval [CI], 1.26, 1.79) and male (OR=1.34; 95% CI, 1.13, 1.60) patients. Patients who had IMCI/IMAI-defined “danger signs” at the initial clinic visit were significantly more likely to report resolution versus those who did not, for both pediatric (OR=7.22; 95% CI, 4.09, 12.77) and adult (OR=8.81; 95% CI, 4.37, 17.79) patients.
Referrals to the Clinic from the Community
From both the quarterly surveillance visits and community follow-up visits, CHWs created separate referrals for 840 individuals from the home to a pilot clinic. Of these, 187 (22.3%) clients visited the clinic after referral, including 83% within one day of the date of referral. Of the total referrals, 166 (19.8%) were categorized as “life-threatening” by the CHW, yet the referral success rate was no better among those with versus those without this distinction (23% versus 19%; OR=1.24; 95% CI, 0.83, 1.83). There were no statistical differences in the sex of returners compared with nonreturners (females, 58% versus 55% [OR=1.13; 95% CI, 0.72, 1.77]), in age (<15 years, 50% versus 48% [OR=1.09; 95% CI, 0.78, 1.54]), or in frequency of top diagnoses (cough, 24% versus 24% [OR=0.95; 95% CI, 0.67, 1.33]; other, 25% versus 20% [OR=1.38; 95% CI, 0.98, 1.95]; or fever, 20% versus 19% [OR 1.00; 95% CI, 0.70, 1.43]). Characteristics of referred patients are shown in Table 3.
Table 3.
Characteristics of Patients Referred to a Clinic (n=840) During a Routine Home Visit or as a Clinic Follow-Up by a Community Health Worker, Stratified by Patients Who Subsequently Returned to the Clinic Versus Those Who Did Not
| REFERRAL | CLINIC VISIT (N=187) | NO CLINIC VISIT (N=653) | TOTAL (N=840) |
|---|---|---|---|
| Average age (years) | 22.5 (n=187) | 21.3 (n=452) | 21.5 (n=639) |
| Age <15 | 4.1 (n=94) | 5.1 (n=217) | 4.8 (n=312) |
| Age ≥15 | 41.0 (n=93) | 36.2 (n=235) | 37.5 (n=327) |
| Female sex | 58.0% (n=54/93) | 55.2% (n=256/464) | 55.7% (n=310/557) |
| Referrals categorized as life-threatening | 22.5% (n=42/187) | 19.0% (n=124/653) | 19.8% (n=166/840) |
| CHW diagnosis | |||
| Cough | 24% (n=68) | 24% (n=244) | 24% (n=312) |
| Other | 25% (n=73) | 20% (n=206) | 21% (n=279) |
| Fever | 20% (n=57) | 19% (n=197) | 19% (n=254) |
| Headache | 15% (n=43) | 18% (n=188) | 17% (n=231) |
| Diarrhea | 5% (n=13) | 6% (n=59) | 5% (n=72) |
| Malaria | 2% (n=6) | 4% (n=44) | 4% (n=50) |
| Infection | 4% (n=12) | 3% (n=27) | 3% (n=39) |
| Vomiting | 2% (n=6) | 3% (n=27) | 3% (n=33) |
| Injury | 2% (n=7) | 2% (n=22) | 2% (n=29) |
| Fatigue | 1% (n=3) | 1% (n=5) | 1% (n=8) |
| HIV/AIDS | — (n=0) | 1% (n=8) | 1% (n=8) |
| Measles | — (n=0) | 1% (n=8) | 1% (n=8) |
| Stroke | — (n=0) | <1% (n=3) | <1% (n=3) |
Diagnoses by community health workers (CHWs) were based on a CHW's assessment of patient signs and symptoms. Patients may have more than one diagnosis.
HIV/AIDS, human immunodeficiency virus/acquired immunodeficiency syndrome.
Discussion
This program demonstrates the real-world application of m-health in the context of rural primary care. Promising surveillance systems were reflected in the volume of households reached in routine visits and individuals referred to clinic from the field, although it was not possible to predict clinic attendance. With standardized patient visit forms at the facility, the software system generated automated follow-ups for CHW mobile phones that allowed case tracking between clinic and field. CHWs were able to successfully visit most of the follow-up requests and collected outcomes on the majority of these cases from the field.
A specific strength of the program was the scale of community outreach through CHW routine household visits. Reliable health surveillance networks for early illness identification and referral are critical to strengthening health systems.25 Through 6,197 surveillance home visits, almost 8% of the estimated population of the three rural districts17 were reached by only 24 CHWs, and over 800 individuals were referred to the clinic from field visits. However, although the hope was to promote early identification and referral of ill individuals, it was not possible to predict clinic attendance using symptoms, CHW-assessed severity of illness, or demographics.
A core second strength was the comprehensiveness of the data system, with complementary and standardized collection tools allowing tracking of cases between community and clinic. Of all clinic cases sent for a follow-up request, CHWs contributed outcomes on 60% of cases and had a community follow-up visit with 74% within four to six weeks, demonstrating the ability to follow individual cases through phases of care. Monitoring was also a key capacity of the program, with monthly reports and performance meetings for both CHW and clinics used for tracking progress and troubleshooting.
An important weakness was the low ascertainment of deaths and potential for biased outcomes sampling. During routine household visits, the lack of unique household identifiers, reporting methods (e.g., depending on verbal report of deaths), and possible failure to complete separate referral surveys potentially contributed to sampling bias, low referral rates, and under-reporting of mortality. Additionally, the high rates of resolution at the time of CHW follow-up for those with IMCI/IMAI-defined “danger signs” at the initial clinic visit raised the concern that existing algorithms for follow-up might be missing those who were actually ill; accordingly, the software was revised to trigger follow-up of 1:50 clinic patients not meeting criteria for follow-up otherwise.
This program had specific technical challenges. The software required multiple updates as feedback and data became available. Despite education requirements, literacy and technologic proficiency levels were barriers to some CHWs. It was also necessary to monitor phone use for tampering or inaccurate data entry. Powering phones was another problem in several sites and required purchasing small solar phone chargers in addition to the solar panels installed at the facilities for power.
Implementation in similar settings has other limitations to consider, including stress placed on existing systems, costs implications, and effects of project conclusion. To this end, CHW workload monitoring and feedback mechanisms were incorporated into the system. Formal cost evaluations will be included in the BHOMA outcomes. Lastly, building on existing MoH infrastructure, avoiding incentives tied to outcomes, and prioritizing use of low-cost local supplies will ideally minimize impact of project withdrawal.
M-health is an increasingly active area of research. However, many existing interventions have a narrow scope,11,26 whereas this system is comparably widely focused in both technologic scale and program goals. Furthermore, although the majority of past m-health publications are of pilot results,11 the ongoing BHOMA intervention and its expanded outcomes provide an important context for the pilot project. Consistent with m-health trends in the developing world, this pilot project used open-source rather than proprietary software. This adaptation of CommCare™ differs from other applications where customization may include multimedia (video, voice), enhanced two-way communication (e.g., CHW to CHW), or increased epidemiologic data collection.12
This program could be adapted for other low-resource settings—and other health services—if basic infrastructure such as a cellular network was available. For example, similar systems could be used to promote HIV services such as adherence counseling through household visitation, follow-up of ill or inactive patients, and referral of appropriate clients. Diverse CommCare™ projects are underway in over 25 countries, including maternal health projects in Afghanistan and child health in Tanzania.27
Although rigorous outcomes are unavailable until BHOMA's conclusion, these data suggest that CHWs and mobile phone technology have potential for increasing service outreach, facilitating clinic–community interaction, and enhancing data collection in Zambia.
Acknowledgments
The Zambian Ministry of Health is thanked for their support and participation in the primary care improvement program, and the BHOMA team members are also thanked. Funding for the primary care program was provided through the African Health Initiative of the Doris Duke Charitable Foundation. Trainee and salary support for L.S. was provided by the U.S. National Institutes of Health through the International Clinical Research Scholars and Fellows Program (grant R24 TW007988).
Disclosure Statement
M.T. and C.Z. are, or have been, employed by Dimagi, Inc., a classified benefit corporation that makes CommCare™ as free, open-source software. These authors contributed to the technical descriptions contained in this publication. L.S., N.S., J.J., R.C., B.H.C., J.S.A.S., and N.C. declare no competing financial interests exist.
References
- 1.International Telecommunication Union World telecommunication/ICT indicators database 2013, 17th edition. Geneva: International Telecommunication Union, 2013. Available at www.itu.int/en/ITU-D/Statistics/ (last accessed September16, 2013) [Google Scholar]
- 2.Montez D. Mobile communications in Zambia, a demand-side analysis based on the AudienceScapes survey, including insights on mobile money use. Washington, DC: InterMedia Survey Institute, 2010. Available at www.audiencescapes.org/ (last accessed September16, 2013) [Google Scholar]
- 3.Krishna S, Austin Boren S, Balas EA. Healthcare via cell phones: A systematic review. Telemed J E Health 2009;15:231–240 [DOI] [PubMed] [Google Scholar]
- 4.DeRenzi B, Lesh N, Parikh T, Sims C, Maokla W, Chemba M, et al. . E-imci: Improving pediatric health care in low-income countries. Proceeding of the 26th Annual SIGCHI Conference on Human Factors in Computing Systems Florence, Italy: ACM, 2008:753–762 [Google Scholar]
- 5.Kaewkungwal J, Singhasivanon P, Khamsiriwatchara A, Sawang S, Meankaew P, Wechsart A. Application of smart phone in “Better Border Healthcare Program:” A module for mother and child care. BMC Med Inform Decis Mak 2010;10:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hardy H, Kumar V, Doros G, Farmer E, Drainoni ML, Rybin D, et al. . Randomized controlled trial of a personalized cellular phone reminder system to enhance adherence to antiretroviral therapy. AIDS Patient Care STDS 2011;25:153–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brendryen H, Kraft P. Happy Ending: A randomized controlled trial of a digital multi-media smoking cessation intervention. Addiction 2008;103:478–484 [DOI] [PubMed] [Google Scholar]
- 8.Franklin VL, Waller A, Pagliarit C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med 2006;23:1332–1338 [DOI] [PubMed] [Google Scholar]
- 9.Tomlinson M, Solomon W, Singh Y, Doherty T, Chopra M, Ijumba P, et al. . The use of mobile phones as a data collection tool: A report from a household survey in South Africa. BMC Med Inform Decis Mak 2009;9:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curioso WH, Karras BT, Campos PE, Buendia C, Holmes KK, Kimball AM. Design and implementation of Cell-PREVEN: A real-time surveillance system for adverse events using cell phones in Peru. AMIA Annu Symp Proc 2005:176–180 [PMC free article] [PubMed] [Google Scholar]
- 11.Tomlinson M, Rotheram-Borus MJ, Swartz L, Tsai AC. Scaling up m-health: Where is the evidence? PLoS Med 2013;10:e1001382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kallander K, Tibenderana JK, Akpogheneta OJ, Strachan DL, Hill Z, ten Asbroek AH, et al. . Mobile health (m-health) approaches and lessons for increased performance and retention of community health workers in low- and middle-income countries: A review. J Med Internet Res 2013;15:e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bastawrous A, Armstrong MJ. Mobile health use in low- and high-income countries: An overview of the peer-reviewed literature. J R Soc Med 2013;106:130–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, van Wyk B, et al. . Lay health workers in primary and community health care. Cochrane Database Syst Rev 2005;(1):CD004015. [DOI] [PubMed] [Google Scholar]
- 15.Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, van Wyk BE, et al. . Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev 2010;(3):CD004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sazawal S, Black RE. Effect of pneumonia case management on mortality in neonates, infants, and preschool children: A meta-analysis of community-based trials. Lancet Infect Dis 2003;3:547–556 [DOI] [PubMed] [Google Scholar]
- 17.Kalumbi J, ed. 2010 census of population and housing, preliminary population figures. Lusaka, Zambia: Central Statistical Office Zambia, 2011 [Google Scholar]
- 18.Stringer JSA, Chisembele-Taylor A, Chibwesha C, Chi HF, Ayles H, Manda H, et al. . Protocol-driven primary care and community linkages to improve population health in rural Zambia: The Better Health Outcomes through Mentoring and Assessment (BHOMA) project. BMC Health Serv Res 2013;13(Suppl 2):S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization UNICEF. Integrated management of childhood illness. Geneva: World Health Organization, 2008 [Google Scholar]
- 20.World Health Organization. Integrated management of adolescent and adult illness. Geneva: World Health Organization, 2004 [Google Scholar]
- 21.Mhila G, DeRenzi B, Mushi C, Wakabi T, Steele M, Dhadialla P, et al. . Using mobile applications for community-based social support for chronic patients. 6th Health Informatics in Africa Conference (HELINA) Pan Africa Health Informatics Association, Abidjan, Cote d'Ivoire, 2009 [Google Scholar]
- 22.Nguyen DT, Leung KK, McIntyre L, Ghali WA, Sauve R. Does integrated management of childhood illness (IMCI) training improve the skills of health workers? A systematic review and meta-analysis. PLoS One 2013;8:e66030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campbell H, Gove S. Integrated management of childhood infections and malnutrition: A global initiative. Arch Dis Child 1996;75:468–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Central Board of Health Zambia Integrated technical guidelines for frontline healthworkers, 2nd ed. Lusaka, Zambia: Central Board of Health Zambia, 2002 [Google Scholar]
- 25.World Health Organization. Everybody's business: Strengthening health systems to improve health outcomes: WHO's framework for action. Geneva: World Health Organization, 2007 [Google Scholar]
- 26.Free C, Phillips G, Felix L, Galli L, Patel V, Edwards P. The effectiveness of m-health technologies for improving health and health services: A systematic review protocol. BMC Res Notes 2010;3:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dimagi Inc. CommCare—Community Health Mobile Platform. 2011. Available at www.dimagi.com/commcare/ (last accessed July30, 2011)