Abstract
Hypertension is a significant and costly public health problem. It is a major, but modifiable contributor for the development of cardiovascular disease. Randomized controlled trials have shown that controlling hypertension reduces the risk of stroke, coronary artery disease, congestive heart failure, end-stage renal disease, peripheral vascular disease, as well as overall mortality. The risk of developing these hypertension-related complications is continuous, starting at a blood pressure level as low as 115/75 mm Hg. Despite the inherent health risks associated with uncontrolled hypertension, elevated blood pressure remains inadequately treated in the majority of patients. This article reviews guidelines for optimal evaluation of hypertension and current therapeutic options available to combat this common yet pervasive disease.
Hypertension affects approximately 1 of 3 adults in the United States, and about 2 million new cases are diagnosed each year.1,2 An additional 28% of the US population is afflicted with prehypertension, and approximately 7% of Americans are not aware that they even have hypertension.3 Globally, hypertension affects more than 1 billion people and is projected to reach 1.56 billion by 2025.4 It is the leading cause of death and the second leading cause of lost disability-adjusted life-years worldwide.4 Randomized controlled clinical trials have shown that control of hypertension reduces the risk of stroke, coronary artery disease, congestive heart failure, end-stage renal disease, peripheral vascular disease, and mortality.1,5 The risk of developing these complications is continuous, starting at a blood pressure (BP) level as low as 115/75 mm Hg.6
The total direct and indirect cost for hypertension in the United States in 2009 is estimated at $73.4 billion.3 Approximately 10% ($15 billion) of the US total annual drug expenditure is on antihypertensive medications.7 Despite these staggering costs, only 34% of Americans with hypertension are at their BP goal (<140/90 mm Hg).1 The reason for this failure is multi-factorial and only speculative, and not because of the lack of awareness or lack of effective pharmacologic agents or lack of understanding of the role of lifestyle modification. Since hypertension will develop in most Americans in their lifetime,8 early preventive measures and prompt management, including lifestyle and pharmacologic options, are essential to minimize complications associated with this condition.
Patient Evaluation
The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) redefined hypertension and published an updated report in 2003.1 Recognizing that the risk for cardiovascular disease (CVD) and adverse outcomes exists linearly and continuously as BP rises, the JNC-7 panel established a new hypertension category called prehypertension (120–139 mm Hg/80–89 mm Hg). Patients in this category are at risk for developing CVD and overt hypertension; therefore, intensive lifestyle modifications are strongly recommended to prevent further complications. JNC-7 also combined the previous stage 2 and 3 hypertension into just 1 stage—stage 2 hypertension. Pharmacologic intervention is strongly recommended for patients in stage 2 (Table 1).
Table 1.
Classification and Management of BP for Adults
| Initial drug therapy | ||||||
|---|---|---|---|---|---|---|
| BP classification | Systolic BP, mm Hga | Diastolic BP, mm Hga | Lifestyle modifications | Follow-up recommendationb | Without compelling indication | With compelling indication |
| Normal | <120 | and <80 | Encourage | Recheck in 2 y | No antihypertensive indicated | Drug(s) for compelling indications |
| Prehypertension | 120–139 | or 80–89 | Yes | Recheck in 1 y | ||
| Stage 1 hypertension | 140–159 | or 90–99 | Yes | Confirm within 2 mo | Thiazide-type diuretics for most | Drug(s) for compelling indications |
| May consider ACE inhibitors, ARBs, beta-blockers, CCBs, or combination | Other antihypertensives (diuretics, ACE inhibitors, ARBs, beta-blockers, CCBs) as needed | |||||
| Stage 2 hypertension | ≥160 | or ≥100 | Yes | Evaluate in 1–4 wk depending on clinical situation (evaluate and treat immediately if BP >180/110 mm Hg) | 2-drug combination for most (usually thiazide-type diuretics and ACE inhibitors, ARBs, beta-blockers, or CCBs) | |
If there is discrepancy between systolic and diastolic BP, the higher value determines staging. Treatment is determined by highest BP category.
Based on the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
ACE indicates angiotensin-converting enzyme; ARBs, angiotensin receptor blockers; BP, blood pressure; CCBs, calcium channel blockers.
Source: Chobanian AV, et al. Hypertension. 2003;42:1206–1252.
Despite the prevalence of hypertension, approximately 90% to 95% of American adults with elevated BP are found to have no identifiable cause for their condition. Of the 5% with known causes, renal parenchymal and renovascular diseases are the most common culprits.1 Other notable etiologies for hypertension include1:
Chronic kidney disease
Coarctation of the aorta
Cushing syndrome
Obstructive sleep apnea
Medications
Pheochromocytoma
Primary hyperaldosteronism
Renovascular disease
Thyroid/parathyroid disease.
Screening and Diagnosis
Hypertension screening is strongly recommended for all American adults older than age 18, according to the latest recommendations from the US Preventive Services Task Force and the American Academy of Family Physicians.9,10 Screening should be repeated every 2 years for patients with BP <120/80 mm Hg and annually for those with BP between 120 mm Hg to 39 mm Hg systolic BP and 80 mm Hg to 89 mm Hg diastolic BP.1
The key to the diagnosis of hypertension is accurate measurements of BP. Improper hand positioning, incorrect BP cuff size, and insufficient time to relax (<5 minutes) before BP measurements are common errors that can lead to falsely elevated readings. At least 2 BP readings of ≥140/90 mm Hg obtained at 3 different office visits and separated by 2 to 4 weeks are needed to make the diagnosis of hypertension.11 When classifying a patient's BP to determine treatment, choose the highest category between the systolic and diastolic BP. Ambulatory BP monitoring or serial home BP measurements are recommended for patients suspected of having “white coat” hypertension (acute BP elevation in the clinic setting but normal BP when taken outside of the physician's office) or for those with labile or inconsistent readings during the medical encounter.
A medical history and physical examination are necessary for all patients with hypertension. The main goals are to look for reversible precipitating factors, the presence and/or extent of end-organ damage, and the presence of additional cardiovascular (CV) risk factors, such as diabetes or smoking. Laboratory testing should also be obtained in all patients with hypertension. These tests should include urinalysis, hemoglobin or hematocrit, basic metabolic panel, fasting lipids, and electrocardiogram.1 Urine microalbumin-to-creatinine ratio is an independent marker for overall CV risk and should also be obtained.12
Treatment Strategies
The goal of hypertension treatment is to reduce BP to <140/90 mm Hg; however, in patients with hypertension and diabetes or renal disease, the BP goal is even lower, targeted at ≤130/80 mm Hg.1 Nonpharmacologic interventions should be instituted in all patients with hypertension. When used early, lifestyle modifications can decrease other disease risks and may avoid the need for drug therapy. Maintaining a healthy lifestyle, however, is not sufficient or is difficult to comply with, and most patients will require pharmacologic interventions to control their BP.
KEY POINTS
-
▸
Hypertension is a global epidemic, affecting about 1 of 3 American adults, and about 2 million new cases are diagnosed annually.
-
▸
Evidence shows that controlling hypertension reduces the risk of stroke, heart disease, end-stage renal disease, peripheral vascular disease, and the associated costs.
-
▸
Approximately 10% ($15 billion) of the US annual total drug expenditure is on antihypertensives. The total direct and indirect costs of hypertension in 2009 are estimated at $73.4 billion.
-
▸
Despite the many therapeutic options, most patients are still not at blood pressure goals. Instituting early preventive measures is essential to minimize complications associated with this costly condition.
Lifestyle Modifications
JNC-7 endorses lifestyle modifications for all patients with prehypertension or hypertension. These modifications include weight loss, reduced sodium intake, physical activity, limiting alcohol consumption, and incorporating the Dietary Approaches to Stop Hypertension (DASH) eating plan.1 In the PREMIER clinical trial, researchers compared the impact of comprehensive lifestyle modifications, which incorporate the JNC-7 recommendations (“established plus DASH” group) with behavioral modification without DASH (“established” group) and with an “advice-only” group. Results showed greater reductions in systolic BP and diastolic BP in the established group compared with the advice-only group (mean reductions were 11.1 mm Hg, 10.5 mm Hg, and 6.6 mm Hg, systolic BP, and 6.4 mm Hg, 5.5 mm Hg, and 3.8 mm Hg, diastolic BP, respectively), with the greatest reductions seen when DASH was also incorporated.13
Pharmacotherapy
Drug therapy is needed if lifestyle modifications cannot adequately bring BP to goal. First-line medications used in the treatment of hypertension include diuretics, angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), beta-blockers, and calcium channel blockers (CCBs). Some patients will require 2 or more antihypertensive medications to achieve their BP target. In newly diagnosed patients with BP >20/10 mm Hg above goal,2 antihypertensives or a combination hypertensive may be added immediately.1 To minimize side effects, a second drug with a complementary mechanism of action should be added before the initial drug is used in the maximum recommended dosing.
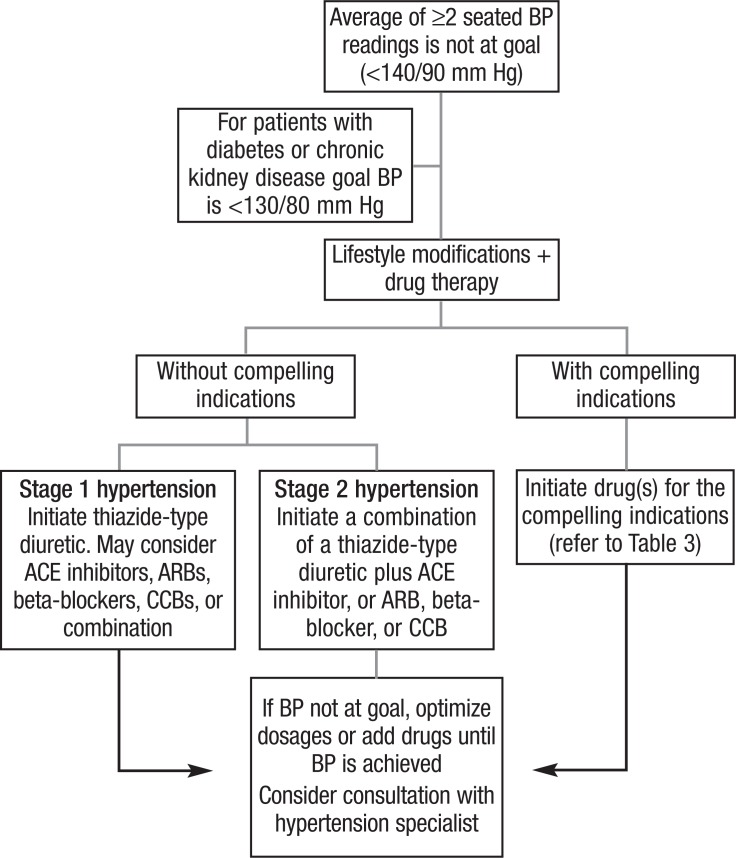
Table 2 outlines the many antihypertensives used today. The Figure provides an algorithm for the treatment of hypertension. Table 3 lists the recommended drug classes according to compelling indications.
Table 2.
Selected Oral Antihypertensive Drugs
| Drug | Dose range, mg/d | Common side effects | Comments | Cost for 30-day supplya |
|---|---|---|---|---|
| Aldosterone antagonists | ||||
| Eplerenone (Inspra) | 50–100 | Dizziness, fatigue, GI disturbances, hyperkalemia, hypertriglyceridemia | More specific in aldosterone blockade Contraindicated in patients at high risk for hyperkalemia | $127.88-$255.76 |
| Spironolactone (Aldactone) | 25–50 | CNS effects (drowsiness, lethargy, headache, fatigue), GI disturbances, hyperkalemia, menstrual irregularities, gynecomastia, mastodynia | $15.99-$21.99 | |
| Alpha1-blockers | ||||
| Doxazosin (Cardura) | 1–16 | Dizziness, headache, lack of energy, nausea, palpitations, orthostatic hypotension | $17.99-$47.98 | |
| Prazosin (Minipress) | 2–20 | $17.99-$67.98 | ||
| Terazosin (Hytrin) | 1–20 | $14.45-$27.98 | ||
| Alpha2-agonists | ||||
| Clonidine tablets (Catapres) | 0.1–0.8 | Dry mouth, dizziness, drowsiness, constipation | Rebound hypertension with abrupt discontinuation | $7-$26.65 |
| Methyldopa (Aldomet) | 250–1000 | Drowsiness, decrease in mental acuity, orthostatic hypotension, nasal congestion, sexual difficulty, bradycardia | First-line agent when hypertension is first diagnosed in pregnancy Positive Coombs' test | $6.50-$25.99 |
| ACE inhibitors | ||||
| Benazepril (Lotensin) | 10–40 | Hypotension, cough, hyperkalemia, dizziness, headache, diarrhea, nausea, rash (primarily captopril), alteration or loss of taste perception (primarily captopril) | Contraindicated in patients with bilateral renal artery stenosis | $23.99 |
| Captopril (Capoten) | 25–100 | $7.19-$9.40 | ||
| Enalapril (Vasotec) | 2.5–40 | $12.99-$23.98 | ||
| Fosinopril (Monopril) | 10–40 | $30-$30.99 | ||
| Lisinopril (Prinivil, Zestril) | 5–40 | $14.89-$17.99 | ||
| Moexipril (Univasc) | 7.5–30 | $36.99-$69.98 | ||
| Perindopril (Aceon) | 4–16 | $65.15-$157.91 | ||
| Quinapril (Accupril) | 10–80 | $19.99-$43.98 | ||
| Ramipril (Altace) | 1.25–20 | $42-$123.98 | ||
| Trandolapril (Mavik) | 1–4 | $16.65-$33.60 | ||
| Angiotensin II receptor antagonists | ||||
| Candesartan (Atacand) | 8–32 | Hypotension, hyperkalemia, dizziness, fatigue, diarrhea | Recommended after intolerance or failure with ACE inhibitors | $67.70-$88.44 |
| Eprosartan (Teveten) | 400–800 | $92.44 | ||
| Irbesartan (Avapro) | 75–300 | $74.85-$91.15 | ||
| Losartan (Cozaar) | 25–100 | $58.99-$92.22 | ||
| Olmesartan (Benicar) | 20–40 | $67.06-$75.34 | ||
| Telmisartan (Micardis) | 20–80 | $75.20-$85.01 | ||
| Valsartan (Diovan) | 80–320 | $79.31-$122.27 | ||
| Beta-blockers | ||||
| Atenolol (Tenormin) | 25–100 | Bradycardia, hypotension, GI disturbances, dizziness, fatigue, insomnia, heart failure, reduced peripheral circulation, impotence, depression, nightmares, bronchospasm in patients with asthma, masks symptoms of or potentiates hypoglycemia in patients with diabetes, hypertriglyceridemia | $5-$5.30 | |
| Bisoprolol (Zebeta) | 2.5–10 | $16.50-$35.13 | ||
| Carvedilol (Coreg) | 12.5–50 | Approved for CHF Has alpha-adrenergic–blocking activity |
$29.98-$32 | |
| Labetalol (Normodyne, Trandate) | 200–800 | Has alpha-adrenergic–blocking activity | $20.99-$57.98 | |
| Metoprolol tartrate (Lopressor) | Metoprolol succinate approved for CHF | $12.99-$25.98 | ||
| Metoprolol succinate (Toprol XL) | 50–100 | Metoprolol succinate approved for CHF | $12.99-$25.98 $25.99-$33.88 |
|
| Nadolol (Corgard) | 40–120 | $15.99-$47.97 | ||
| Propranolol (Inderal) | 40–160 | $8.40-$10.66 | ||
| Calcium channel blockers | ||||
| Dihydropyridines | ||||
| Amlodipine (Norvasc) | 2.5–10 | Peripheral edema, palpitations, headache, dizziness, fatigue, nausea | $5.33-$8 | |
| Felodipine (Plendil) | 2.5–20 | $37.99-$115.45 | ||
| Nicardipine (Cardene SR) | 60–120 | $101.19-$125.99 | ||
| Nifedipine (Adalat CC, Procardia XL) | 30–60 | $54.19-$72.79 | ||
| Nondihydropyridines | ||||
| Diltiazem (Cardizem CD, Dilacor XR, Tiazac) | 120–420 | Dizziness, headache, bradycardia, hypotension, constipation, nausea, weakness, gingival hyperplasia, edema, AV block | Decrease AV nodal conduction Has negative inotropic effects | $25.99-$45.66 |
| Verapamil sustained-release capsule (Verelan) | 120–480 | $25.99-$75.98 | ||
| Verapamil sustained-release tablet (Calan SR, Isoptin SR) | $21.99-$37.98 | |||
| Diuretics | ||||
| Loop | ||||
| Bumetanide (Bumex) | 0.5–2 | Hyperuricemia, hypokalemia, hyperglycemia, hypocalcemia, increased urination at onset of therapy, dizziness, weakness, muscle cramps, photosensitivity, hypotension | Preferred diuretics for patients with severe chronic kidney disease/failure | $5.67-$19.31 |
| Furosemide (Lasix) | 20–80 | $4.20-$8.39 | ||
| Torsemide (Demadex) | 2.5–10 | $9.50-$19.99 | ||
| Thiazide | ||||
| Chlorthalidone | 12.5–25 | Similar electrolyte abnormalities as loop diuretics except for hypercalcemia, increased urination at onset of therapy, dizziness, weakness, muscle cramps, photosensitivity, hypotension | $5-$10 | |
| Hydrochlorothiazide (Microzide, HydroDiuril) | 12.5–50 | $4.80-$14.99 | ||
| Indapamide (Lozol) | 1.25–2.5 | $5-$13.99 | ||
| Metolazone (Zaroxolyn) | 1.25–5 | $21.50-$37.37 | ||
| Potassium-sparing | ||||
| Amiloride (Midamor) | 5–10 | Hyperkalemia, GI disturbances, muscle cramps, weakness, headache, dizziness | $50.45-$100.90 | |
| Triamterene (Dyrenium) | 50–100 | $41.99-$64.04 | ||
| Renin inhibitor | ||||
| Aliskiren (Tekturna) | 150–300 | Diarrhea, headache, dizziness, fatigue, cough | $82.38-$101.80 | |
| Vasodilators | ||||
| Hydralazine (Apresoline) | 25–100 | Tachycardia, palpitations, GI disturbances, headache | $7.80-$27.98 | |
| Minoxidil (Loniten) | 2.5–80 | Tachycardia, hypertrichosis, sodium and water retention | $10-$143.97 | |
Cost calculated from generic, if available, and lowest bottle size available. Cost source: www.drugstore.com.
ACE indicates angiotensin-converting enzyme; AV, atrioventricular; CHF, congestive heart failure; CNS, central nervous system; GI, gastrointestinal.
Sources: Lacy CF, Armstrong LL, Goldman MP, eds. Drug Information Handbook. 17th ed. Hudon, OH: Lexi-Comp; 2008; AHFS Drug Information. Bethesda, MD: American Society of Health-System Pharmacists; 2008.
Figure. Treatment Algorithm for Hypertension.
ACE indicates angiotensin-converting enzyme; ARBs, angiotensin receptor blockers; CCBs, calcium channel blockers.
Source: Chobanian AV, et al. Hypertension. 2003;42:1206–1252.
Table 3.
Compelling Indications
| Recommended drugs | |||||
|---|---|---|---|---|---|
| Compelling indication | Diuretic | Beta-blocker | ACEI | ARB CCB | Aldosterone antagonist |
| Heart failure | x | x | x | x | x |
| Postmyocardial infarction | x | x | x | ||
| High coronary disease risk | x | x | x | x | |
| Diabetes | x | x | x | x x | |
| Chronic kidney disease | x | x | |||
| Recurrent stroke prevention | x | x | |||
ACEI indicates angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker.
Source: Chobanian AV, et al. Hypertension. 2003;42:1206–1252.
Diuretics. Diuretics can be divided into 3 groups—thiazides, loop, and potassium-sparing diuretics.
Thiazides. Thiazides act by inhibiting the absorption of sodium and chloride in the distal convoluted tubule. The benefits of thiazides for stroke, heart failure, and coronary artery disease (CAD) outcomes have been well-established in trials, such as the VA Cooperative Studies in the 1960s,14 Systolic Hypertension in the Elderly Program (SHEP) in the 1980s,15 and the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) in the 1990s.16 Based on the ALLHAT results showing thiazides' superiority to other classes of antihypertensives in terms of secondary end points and costs, the JNC-7 issued its recommendations for thiazides as first-line therapy for hypertension.
Recently these recommendations were challenged by the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trial, which showed that the combination of benazepril and amlodipine was superior to the benazepril and hydrochlorothiazide combination in reducing CV events in high-risk patients with hypertension.17 The difference in these studies was the use of chlorthalidone in earlier trials and hydrochlorothiazide in ACCOMPLISH. In light of this evidence, it has been suggested that the benefits seen in previous trials were attributed to a class effect, when in fact hydrochlorothiazide does not provide the same benefit profile as chlorthalidone. With these data, some clinicians have now considered chlorthalidone as the preferred thiazide agent.18,19 Because of their proved efficacy and low cost, thiazides will continue to be favored as first-line drugs for hypertension.
Loop diuretics. Loop diuretics act on the thick ascending loop of Henle, where they selectively inhibit the luminal Na+/K+/2Cl– symporter thereby reducing NaCl reabsorption. Loop diuretics are highly efficacious in that they target a segment of the nephron with great reabsorptive capacity.20 These agents can be used alone or in combination for the management of hypertension. Although thiazides are the preferred class of diuretics, loop diuretics may be preferred in patients with congestive heart failure, acute pulmonary edema, or renal disease.21 Loop diuretics are relatively inexpensive and are available in generic forms.
Potassium-sparing diuretics. Potassium-sparing diuretics act on the distal and cortical collecting tubules to decrease sodium reabsorption by either blocking aldosterone receptors (spironolactone, eplerenone) or by inhibiting Na+ influx through epithelium sodium ion channels in the apical membrane of the collecting tubule (amiloride and triamterene).20 These are mild diuretics and are effective in the treatment of hypertension, but are seldom used alone.21 These agents are recommended as adjunct therapy in the treatment of hypertension, especially when their hyperkalemic effect is desired. Through their actions on aldosterone receptors, spironolactone and eplerenone have been shown to reduce morbidity and mortality in patients with heart failure.22,23 Caution must be taken when these agents are used in conjunction with an ACE inhibitor or ARB because clinically significant hyperkalemia can occur.
ACE inhibitors. ACE inhibitors exert their BP-lowering effects by inhibiting the conversion of the inactive angiotensin I to the active angiotensin II. In addition, bradykinins and subsequently prostaglandins are increased, which contributes to ACE inhibitor BP-lowering effects.24 JNC-7 endorses the use of ACE inhibitors when any of the following compelling indications exist: heart failure, postmyocardial infarction (MI), high risk of CAD, diabetes, chronic kidney disease, and/or stroke.21 A Cochrane search revealed no difference in BP-lowering effects among the different ACE inhibitors, with BP-lowering trough levels of −8/–5 mm Hg.25 These effects were seen at half or more of the maximum manufacturer recommended doses.25 A study conducted in the Durham Veterans Affairs Medical Center (VAMC) revealed greater cost-savings when ACE inhibitors are initially used for the management of hypertension compared with ARBs.26 Because of cost-savings, an ACE inhibitor should be tried before the initiation of an ARB.
Angiotensin receptor blockers. ARBs block angiotensin II from binding to its receptor, thereby preventing it from causing vasoconstriction and fluid retention. The Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET) established that the ARB, telmisartan, is not inferior to the ACE inhibitor in reducing CV and renal events in high-risk patients without heart failure.27 A similar effect is seen with other ARBs and was confirmed in a recent Cochrane search, showing comparable BP-lowering effects between ARBs and ACE inhibitors.25 A recent cost-effectiveness analysis of ACE inhibitors and ARBs for hypertension conducted in the Durham VAMC revealed ARB-initiated patients incurred an expected cost of $6271 over 10 years compared with an ACE inhibitor–initiated patient cost of $2434. This study revealed a greater cost in the initiation of ARBs whether the patient continued this class of medication, switched to an ACE inhibitor, or stopped either medication.26 Because the ACE inhibitors are less costly, ARBs should be tried only as an alternative when there is intolerance (ie, cough or angioedema) or failure with ACE inhibitors.
Renin inhibitors. Aliskiren is the first agent in a new class of antihypertensive drugs that inhibits the conversion of angiotensinogen to angiotensin I via renin inhibition. It is approved for monotherapy as well as in combination with other antihypertensives. One study has shown that aliskiren is not inferior to other antihypertensive agents and is significantly superior to ramipril in reducing mean systolic BP.28 Studies have also demonstrated greater reductions in BP in combined therapy with other antihypertensive agents compared with either agent alone.28,29 Another study even showed that aliskiren may have renoprotective effects, reducing mean urinary albumin to creatinine ratio by 20% in patients with type 2 diabetes.30 However, because of cost concerns and robust clinical outcomes of ACE inhibitors and ARBs, aliskiren is currently recommended as a second-line agent.
Calcium channel blockers. CCBs lower BP by preventing the entry of calcium into vascular smooth muscles, resulting in vasodilation and reduced vascular contractility. The 2 types of CCBs are (1) dihydropyridines, which act on peripheral blood vessels, and (2) nondihydropyridines, which act on cardiac muscles and peripheral blood vessels. Randomized controlled trials have demonstrated that dihydropyridines are effective at reducing CV events, mortality, and strokes particularly in the elderly.1,31 Nondihydropyridines are useful in the treatment of cardiac arrhythmias. Both types of drugs are effective as monotherapy in reducing BP and are generally well tolerated. Recent results from the ACCOMPLISH trial have shown that CCBs are comparable first-line agents and are well tolerated when combined with another drug, especially an ACE inhibitor.17 JNC-7 recognizes CCBs as a possible first-line drug class for patients at high risk for CVD or for those with diabetes (Table 3).1
Beta-blockers. Beta-blockers lower BP primarily by blocking beta-1 adrenergic receptors resulting in slower heart rate, decreased cardiac contractility, and reduced cardiac output.24 As a result, beta-blockers are considered first-line medications in patients with acute MI. Beta-blockers also inhibit renin release and subsequently angiotensin II production and are therefore useful in the treatment of hypertensive patients with congestive heart failure and/or with asymptomatic left ventricular hypertrophy (LVH).1
Clinical differences to consider when selecting an individual beta-blocker are beta-receptor selectivity and intrinsic sympathomimetic activity (ISA). Beta-blockers (ie, atenolol, bisoprolol, and metoprolol) with a greater affinity to beta-1 receptors (heart) than beta-2 receptors (lungs, kidneys, and vasculature) are considered cardio-selective. Nonselective beta-blockers have affinity to beta-1 and beta-2 receptors and may not be the preferred agents when treating a CV indication. Some beta-blockers (ie, labetalol, carvedilol) also have an alpha receptor-blocking component, thus increasing its BP-lowering capabilities. Beta-blockers with ISA (ie, pindolol) have some stimulatory effects on the receptors they block, but less than a pure agonist. These agents are preferred when bradycardia is a concern.
In the absence of acute MI, congestive heart failure, and asymptomatic LVH, most experts agree that beta-blockers should not be used as first-line treatment in patients with essential hypertension. Recent meta-analyses have shown that beta-blockers, in comparison with other antihypertensives, are less effective in lowering BP5 and may be associated with increased risk of all-cause mortality and stroke, especially in patients older than age 60.32,33 A recent Cochrane review has evaluated 13 randomized controlled trials to quantify the efficacy and safety of beta-blockers as first-line therapy for essential hypertension, concluding that beta-blockers are not effective first-line hypertensive drugs.34 More important, there was “a trend towards worst outcomes in comparison with calcium channel blockers, renin-angiotensin system inhibitors, and thiazide diuretics.”34
Alpha-blockers. Alpha-blockers lower BP by blocking vasoconstricting alpha-1 adrenoreceptors on vascular smooth muscles. They are beneficial in hypertensive men with benign prostate hypertrophy; otherwise, they are not recommended for initial monotherapy. In ALLHAT, doxazosin was associated with increased risk for CV events compared with chlorthalidone.16
Direct vasodilators. Hydralazine and minoxidil are 2 common agents in this class. Both directly relax vascular smooth muscle, primarily arterioles, through different mechanisms of action. Although both are effective antihypertensive medications, their side-effect profiles preclude their use as initial monotherapy agents or as first-line therapies and make them useful only as add-on therapy, especially in patients with severe hypertension or renal insufficiency. They are often prescribed in combination with a beta-blocker and a diuretic to negate side effects, such as reflex tachycardia and fluid retention. Minoxidil is given once a day, but diffuse hair/facial hair growth (hirsutism) minimizes its use in women. Hydralazine is effective in the treatment of hypertensive emergencies. A severe but less frequent adverse event that may potentially occur with chronic hydralazine use is drug-induced systemic lupus erythematosus, which is reversible with discontinuation of the medication.
Combination Therapy
Combination therapy is beneficial and should be initiated when BP is more than 20/10 mm Hg above goal.1 Most combination therapies utilize antihypertensive agents that act by different but complementary mechanisms to maximize BP-lowering effects. Advantages of fixed combination therapy include better compliance, fewer side effects, faster response, and possibly lower cost, depending on the choice of agents and the insurance programs.
The combination of an ACE inhibitor or ARB with a diuretic is an effective and well-tolerated initial regimen. The ACCOMPLISH trial recently demonstrated that the combination of a CCB plus an ACE inhibitor is also very effective.17 Concurrent use of an ACE inhibitor and an ARB is not a preferred combination, although rarely used in heart failure or in diabetes patients with significant proteinuria; one should be cautious about increased risk of side effects, as confirmed by the ONTARGET study.27 In ONTARGET, patients receiving a combination of an ACE inhibitor and an ARB had significantly greater risk of hypotension, syncope, renal dysfunction, and hyperkalemia. Other less-effective combinations include beta-blockers/ACE inhibitors, beta-blockers/alpha-blockers or agonists, and beta-blockers/nondihydropyridines.
Resistant Hypertension
Resistant hypertension is the failure to achieve goal BP despite adherence to 3 antihypertensive agents, including a diuretic at maximal tolerated doses.1,21 An approach to managing resistant hypertension includes reevaluating factors that may contribute to lack of BP control and aggressive use of antihypertensive agents at maximal tolerated doses. Factors that may contribute to uncontrolled hypertension include suboptimal BP measurement technique, white-coat effect, poor adherence, and inappropriate dosing. Patients who are identified as having these factors are considered as having pseudoresistance. Factors that contribute to hypertension, as well as resistant hypertension, include medications (inclusive of over-the-counter or nonprescribed drugs, such as decongestants, or nonsteroidals), excess alcohol consumption, excess dietary sodium intake, obesity, diabetes mellitus, and older age. Causes of secondary hypertension must also be sought. If a correctable cause is not identified, the next step is to initiate aggressive pharmacologic therapy, with a goal of blocking all possible mechanisms of BP elevation.
The cornerstone of therapy is the use of diuretics, because plasma expansion is a common pathophysiologic mechanism to resistance.35,36 Consideration of kidney function is required when selecting an optimal diuretic as ineffectiveness is seen when thiazides are used in patients with an estimated glomerular filtration rate (eGFR) <30 mL/min. At lower eGFR values, loop diuretics may be used.36 Choice of other agents should be based on patient characteristics, which includes concomitant disease states (Table 3).
A fourth agent may be added if goal BP is still not achieved. There is evidence that the addition of spironolactone may have significant BP reductions, as seen in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA) with a reduction of BP as much as 21.9/9.5 mm Hg that was unaffected by sex, age, smoking, or diabetes status.37 Other studies show similar reductions in persons with and without hyperaldosteronism.36 The addition of spironolactone should be considered in patients who are obese or have sleep apnea, because these conditions have been associated with aldosterone excess.38
Eplerenone is an alternative aldosterone antagonist if adverse events are experienced with spironolactone. Failure of a 4-drug regimen may require referral to a hypertension specialist. Less favorable options before referral include centrally acting alpha-agonists (clonidine and methyldopa) or vasodilators (hydralazine and minoxidil).
Conclusion
Hypertension is a global epidemic, yet many guidelines and pharmacologic options are available to prevent the morbidity and mortality associated with this disease. Although lifestyle modifications are frequently neglected, they should be started early and continued indefinitely. Some patients will require more than 1 antihypertensive agent to control their BP. Combination therapies are effective and are recommended in patients with stage 2 hypertension. Regardless of which drug is used, the most important aspect of treating hypertension is reducing BP to goal. Effective communication between physicians, other healthcare professionals, and patients is paramount in the successful treatment of hypertension.
Biography

Quang Nguyen
Contributor Information
Quang Nguyen, Assistant Professor, Department of Endocrinology, Diabetes, and Metabolism, University of Nevada School of Medicine, Reno.
Joann Dominguez, Internal Medicine Resident, California Pacific Medical Center, San Francisco.
Loida Nguyen, Clinical Pharmacy Specialist, VA Sierra Nevada Health Care System, Reno.
Nageshwara Gullapalli, Assistant Professor of Medicine and Associate Program Director, Internal Medicine Residency Program, University of Nevada School of Medicine, Reno.
References
- 1.Chobanian AV, Bakris GL, Black HR, et al. for the National Heart, Lung, and Blood Institute. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42: 1206–1252. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. High blood pressure. www.cdc.gov/bloodpressure/. Accessed March 21, 2009.
- 3.Lloyd-Jones D, Adams R, Carnethon M, et al. for the Writing Group Members. Heart Disease and Stroke Statistics 2009 Update: a Report from the American Heart Association Staistics Committee and Stroke Statistics Subcommittee. Circulation. 2009; 119: e21–e181. [DOI] [PubMed] [Google Scholar]
- 4.Alcocer L, Cueto L. Hypertension, a health economics perspective. Ther Adv Cardiovasc Dis. 2008; 2: 147–155. [DOI] [PubMed] [Google Scholar]
- 5.Psaty BM, Lumley T, Furberg CD, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003; 289: 2534–2544. [DOI] [PubMed] [Google Scholar]
- 6.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002; 360: 1903–1913. [DOI] [PubMed] [Google Scholar]
- 7.Spurgeon D. NIH promotes use of lower cost drugs for hypertension. BMJ. 2004; 328: 539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: the Framingham Heart Study. JAMA. 2002; 287: 1003–1010. [DOI] [PubMed] [Google Scholar]
- 9.US Preventive Services Task Force. Screening for high blood pressure: US Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2007; 147: 783–786. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Family Physicians. Recommendations for clinical preventive services: high blood pressure. www.aafp.org/online/en/home/clinical/exam/f-j.html. Accessed April 11, 2009.
- 11.The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997; 157: 2413–2446. [DOI] [PubMed] [Google Scholar]
- 12.Forman JP, Brenner BM. Hypertension and microalbuminuria: the bell tolls for thee. Kidney Int. 2006; 69: 22. [DOI] [PubMed] [Google Scholar]
- 13.Appel LJ, Champagne CM, Harsha DW, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003; 289: 2083–2093. [DOI] [PubMed] [Google Scholar]
- 14.Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967; 202: 1028–1034. [PubMed] [Google Scholar]
- 15.SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991; 265: 3255–3264. [PubMed] [Google Scholar]
- 16.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002; 288: 2981–2997. [DOI] [PubMed] [Google Scholar]
- 17.Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008; 359: 2414–2428. [DOI] [PubMed] [Google Scholar]
- 18.Saklayen MG. Which diuretic should be used for the treatment of hypertension? Am Fam Physician. 2008; 78: 444–446. [PubMed] [Google Scholar]
- 19.Ernst ME, Carter BL, Basile JN. All thiazide-like diuretics are not chlorthalidone: putting the ACCOMPLISH study into perspective. J Clin Hypertens (Greenwich). 2009; 11: 5–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jackson EK. Diuretics. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 11th ed.Columbus, OH: McGraw-Hill Professional; 2005:737–770. [Google Scholar]
- 21.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA. 2003; 289: 2560–2572 Erratum: JAMA. 2003; 290: 197. [DOI] [PubMed] [Google Scholar]
- 22.Pitt B, Zannad F, Remme WJ, et al. for the Randomized Aldactone Evaluation Study Investigators. The effect of spironolactone on the morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999; 341: 709–717. [Google Scholar]
- 23.Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003; 348: 1309–1321. [DOI] [PubMed] [Google Scholar]
- 24.Hoffman BB. Therapy of Hypertension. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 11th ed.Columbus, OH: McGraw-Hill Professional; 2005:845–868. [Google Scholar]
- 25.Heran BS, Wong MM, Heran IK, Wright JM. Blood pressure-lowering efficacy of angiotensin receptor blockers for primary hypertension. Cochrane Database Syst Rev. 2008;(4):CD003822. [DOI] [PMC free article] [PubMed]
- 26.Powers B, Datta S, Oddone E. A cost-effectiveness analysis of ACE-inhibitors vs. angiotensin receptor blockers for the treatment of hypertension. Presented at the Health Service Research and Development Service 2009 national meeting, February 11–13, 2009; Baltimore, MD. Abstract 1049.
- 27.Yusuf S, Teo KK, Pogue J, et al. for the ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008; 358: 1547–1559. [DOI] [PubMed] [Google Scholar]
- 28.Uresin Y, Taylor AA, Kilo C, et al. Efficacy and safety of the direct renin inhibitor aliskiren and ramipril alone or in combination in patients with diabetes and hypertension. J Renin Angiotensin Aldosterone Syst. 2007; 8: 190–198. [DOI] [PubMed] [Google Scholar]
- 29.Villamil A, Chrysant SG, Calhoun D, et al. Renin inhibition with aliskiren provides additive antihypertensive efficacy when used in combination with hydrochlorothiazide. J Hypertens. 2007; 25: 217–226. [DOI] [PubMed] [Google Scholar]
- 30.Parving HH, Persson F, Lewis JB, et al. Aliskiren combined with losartan in type 2 diabetes and nephropathy. N Engl J Med. 2008; 358: 2433–2446. [DOI] [PubMed] [Google Scholar]
- 31.Neal B, MacMahon S, Chapman N; for the Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood pressure-lowering drugs results of prospectively designed overviews of randomised trials. Lancet. 2000; 355: 1955–1964. [DOI] [PubMed] [Google Scholar]
- 32.Carlberg B, Samuelsson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet. 2004; 364: 1684–1689. [DOI] [PubMed] [Google Scholar]
- 33.Medical Research Council trial of treatment of hypertension in older adults: principal results. MRC Working Party. BMJ. 1992; 304: 405–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wiysonge CS, Bradley H, Mayosi BM, et al. Beta-blockers for hypertension. Cochrane Database Syst Rev. 2007;(1):CD002003. [DOI] [PubMed]
- 35.Moser M, Setaro J. Resistant or difficult-to-control hypertension. N Engl J Med. 2006; 355: 385–392. [DOI] [PubMed] [Google Scholar]
- 36.Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008; 52: 1749–1757. [DOI] [PubMed] [Google Scholar]
- 37.Chapman N, Dobson J, Wilson S, et al. Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension. 2007; 49: 839–845. [DOI] [PubMed] [Google Scholar]
- 38.Goodfriend TL, Calhoun DA. Resistant hypertension, obesity, sleep apnea, and aldosterone: theory and therapy. Hypertension. 2004; 43: 518–524. [DOI] [PubMed] [Google Scholar]