Abstract
Many healthcare stakeholders, including insurers and employers, agree that growth in healthcare costs is inevitable. But the current trend toward further cost-shifting to employees and other health plan members is unsustainable. In 2008, the Zitter Group conducted a large national study on the relationship between insurers and employers, to understand how these 2 healthcare stakeholders interact in the creation of health benefit design. The survey results were previously summarized and discussed in the February/March 2009 issue of this journal. The present article aims to assess the implications of those results in the context of the growing tendency to increase patient cost-sharing, a weak US economy, and poor health habits. Increasing cost-sharing is a blunt instrument: although it may reduce utilization of frivolous services, it may also result in individuals forgoing medically necessary care. Increases in deductibles will lead to an overall decrease in optimal care-seeking behavior as families juggle healthcare costs with a weak economy and stagnating wages.
In the spring of 2008, the Zitter Group conducted a large national study of the insurer—employer relationship to understand how these 2 stakeholders interact in the creation of healthcare benefit design. The 2-arm study consisted of concurrent web-based quantitative surveys with commercial managed care executives, large employers, and major employer benefits consultants.1 It was designed to provide a richly detailed snapshot of trends in employer-sponsored healthcare coverage. Despite having varying ideas on specific healthcare benefit design strategies, employers and insurers assign similar weights to the importance of cost, quality, and access when making benefit design decisions.1,2 For both groups, the importance assigned to cost is 1.5 times higher in value than healthcare access or healthcare quality.1 Throughout the survey, both groups cited access and quality concerns, but in the current environment of steadily rising cost growth, the importance assigned to cost takes on an even greater significance. The survey results were summarized in the February/March issue of this journal.1 The present article is a follow-up to that article, and its goal is to place those survey results in the context of increased patient cost-sharing, a weak US economy, and the poor health habits that are characteristic of many segments of the American population.
According to the data from the Benefit Design Index, in the absence of clear alternatives to traditional benefit designs, cost-shifting to patients through increases in copayments, deductibles, and premiums remains the primary cost-containment strategy used by employers and insurers. More than half of employers and three quarters of insurers have increased their premiums and deductibles between June 2007 and June 2008.1 Furthermore, two thirds of insurers and half of employers do not believe that the recent slowing growth rate of premiums is sustainable and, as a result, expect to increase all forms of patient cost-sharing.1 However, employers remain aware of the dangers of passing too many costs to employees; high out-of-pocket costs can translate into reduced adherence to medical treatments and, ultimately, deteriorating employee health and productivity.1,2
In 2003, 30% of employees reported having a chronic health condition.3 That rate was likely to be even higher in 2008.4 The American Hospital Association reported that approximately 69 million workers took 1 or more sick days in 2003, totaling 407 million lost work days.3 In addition, 50% of employees reported being distracted at work by health concerns, reducing their productivity.3 Although absenteeism and lost productivity cost estimates vary widely, it is likely that they cost US businesses several million dollars a year.5,6 Combine the burdens of high employer healthcare costs, deteriorating employee health, and a weak US economy, and you have the ingredients for a “perfect storm”—one that is likely to lead to an insurance “death spiral,” from which we may not be able to recover.
Weakness of Cost-Shifting as a Cost-Control Strategy
The cost-shifting strategy has several important weaknesses, some of which remain only partially understood. The seminal cost-sharing research was that of the RAND's Health Insurance Experiment (HIE),7 which began in 1971 and continued for 15 years. This multimillion-dollar research was funded by the Department of Health and Human Services and was designed to answer 2 key questions7:
How much more medical care will people use if it is provided free of charge?
What are the consequences for their health?
Economics teaches us that when the prices of services rise, demand falls. It is therefore not surprising that the RAND's HIE results indicated that increased patient cost-sharing decreased utilization of health services.8,9 The reasons for this are not fully understood, but it is clear that cost-shifting is a blunt instrument, with the reduction in utilization occurring for necessary as well as unnecessary services.
This problem is most pronounced in low-income families (ie, the “working poor”). Household resources are finite, and the financial resources available for health expenditures will be increased or reduced as other outlays—such as energy or food—rise or fall. Therefore, it is expected that increases in the cost of necessary items, such as food or energy, will limit the share of resources available for healthcare expenditures. This was confirmed by the RAND's HIE, which showed that poorer participants in the study had worse health outcomes.10
Results of another study, by Goldman and colleagues, have shown that increased cost-sharing in one area can lead to reductions in use for other products and services, with potentially negative consequences for health outcomes.11 The more ill patients are, the more therapies or healthcare services they consume. Therefore, the patients most affected by increased cost-sharing are those whom society can least afford to reduce their consumption of medically necessary care. The problem of poor health outcomes becomes only larger as more time passes; as patients forgo needed care, the risk of serious clinical consequences increases.
KEY POINTS
-
▸
Employes and insurers assign a 1.5 greater value to healthcare costs than to access or quality of care.
-
▸
Cost-shifting to patients through rising copayments, deductibles, and premiums remains the main cost-containment strategy used by employers and insurers.
-
▸
More than 50% of employers and 75% of insurers increased their premiums and deductibles from June 2007 to June 2008.
-
▸
The RAND's Health Insurance Experiment and other studies indicate that increased patient cost-sharing decreases utilization of health services. Not surprisingly, poor participants in the RAND study also had worse health outcomes.
-
▸
Despite 2 new benefit design trends—consumer-directed health plans and value-based benefit designs—the marketplace is not moving toward this type of innovation and remains focused on cost.
-
▸
Willingness to pay is used as a measure of the value of a particular healthcare service, but this is misleading, because willingness to pay depends on one's income or ability to pay, not necessarily on the value of the service.
-
▸
Restructuring the healthcare system must focus on paying for disease prevention rather than for each sickness episode. Prevention is key to moving past the failed policies of shifting costs to patients and perpetuating poor health.
Underinsured and uninsured adults report access and medical bill problems at remarkably similar rates. In 2007, an estimated 25 million American adults (aged 19–64 years) were underinsured, a 60% increase from 2003.12 According to an analysis by the Commonwealth Fund, cost-shifting to the member (or employee) has exacerbated the underinsurance phenomenon. Premiums consume 5% or more of family income for 41% of underinsured Americans; they consume 10% or more of family income for 19%.12
As reported by the Center for Studying Health System Change, underinsured as well as uninsured status undermines optimal care-seeking behavior.4 For the 59 million Americans reporting healthcare access problems, cost was the most frequently cited obstacle to care. In 2007, 69% of people who went without or delayed needed care cited worries about cost, a 3.8% increase from 2003.4 But results from the Benefit Design Index indicate that the rate of underinsured Americans is likely to continue to climb, reflecting likely increases in premiums, deductibles, and coinsurance.1,2
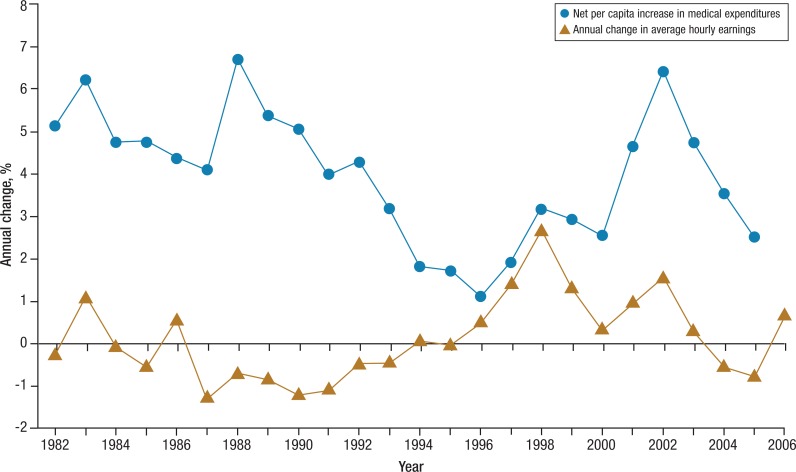
It must be understood that rising healthcare cost-sharing comes at the expense of wages. Under our current healthcare system, employers pay premiums to health insurance companies, who in turn pay for care. This has the effect of insulating employers as well as employees from the direct cost of healthcare. As a result, employers adjust to rising healthcare premiums by either reducing employee wages or by shifting higher premium costs to employees. In the current economic climate, employee wages have remained relatively flat, further moving healthcare out of reach for many Americans (Figure 1).13
Figure 1. Changes in Per Capita Health Expenditures and Average Hourly Earnings (Adjusted for Inflation), 1982–2005.
Reprinted with permission from JAMA. 2008;299:1057–1059. Copyright © 2008 American Medical Association. All rights reserved.
A key concept in the debate is “willingness to pay” (WTP), which indicates how much a consumer is able or willing to pay for a product. Although it is used as a measure of value of a particular healthcare service, WTP is a misleading measure of value, because it depends on the consumer's income. For products and services with high intrinsic value, a lack of sufficient income leads to a misleadingly small WTP.14 Nevertheless, the literature on WTP does not seem widely believed by either insurers or employers.14,15 According to the Benefit Design Index, both groups estimate that cost-sharing burdens for prescription drugs must be significant—in excess of $35—before utilization patterns change, or demand for necessary care begins to fall.2 This $35 estimate significantly overstates a patient's WTP, as reported in the health economic literature,15 with negative implications for plan design and downstream behavior. Insurers and employers seem to be ignoring the research on WTP as a way to justify continuing to shift costs to patients. As more costs are shifted, patients become less able to afford needed medical care.
This becomes especially troubling when considering sick patients. It is well established in the literature that for certain chronic conditions, forgoing early treatment will lead to progressively poorer outcomes. Diabetes, elevated cholesterol levels, and hypertension are generally conditions treated with a combination of pharmacologic and lifestyle modifications, such as diet and exercise—relatively low-cost treatment methods. In many cases, these lower-cost treatments have been shown to reduce or delay later medical costs.16–18
However, in the face of increased cost-sharing, patients forgo necessary treatment.19–21 Furthermore, some early experiments in innovative plan designs reduce cost-sharing for treatments deemed valuable, such as medications for diabetes.22 These experiments seem to indicate that these more sophisticated benefit designs can actually improve compliance and down-the-line healthcare outcomes.22
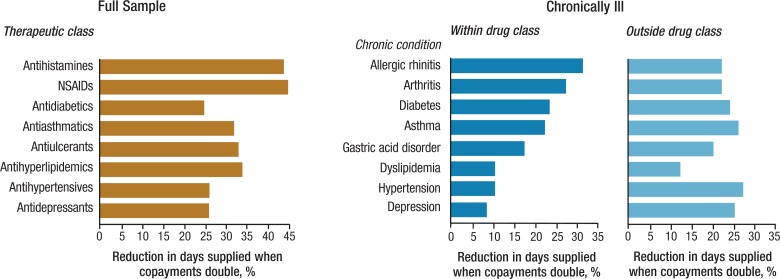
Goldman and colleagues found that doubling the copayment of tier-2 drugs from $6.31 for generics and $12.62 for preferred brands to $12.62 and $25.70, respectively, reduced utilization of drugs for chronic diseases that stall disease progression—such as antihyperlipidemics, antihypertensives, antidiabetics—as well as drugs that treat symptoms or intermittent conditions, such as nonsteroidal antiinflammatory drugs (NSAIDs) and antihistamines. The largest decreases occurred in NSAIDs (45%) and antihistamines (44%), but all drug classes were affected (Figure 2).11 The cost-sharing levels studied for generics and preferred brands were well below the $35 limit widely believed necessary by insurers and employers,1 as mentioned earlier.
Figure 2. Predicted Change in Annual Days Supplied when Copayments Doubled by Drug Class, Population.
Reprinted with permission from JAMA. 2004;291:2344–2350. Copyright © 2004 American Medical Association. All rights reserved.
Although the relationship between increased patient cost-sharing and underutilization of necessary medical care has been well documented, there is a lack of longitudinal data that measure the long-term cost implications that may be related to forgoing needed care because of increased cost-sharing. It is reasonable to postulate that if patients are forgoing needed medical care, and if treating chronic conditions early on is cheaper than treating them later—then over the long-term healthcare costs for these individuals will increase as their disease worsens, and forgoing care can no longer be an option. To our knowledge, no studies have followed patients over the long-term and documented the long-term impact on healthcare costs.
In addition, little work has been done to study the link between increasing medical spending and the impact on health outcomes. If increased cost-sharing negatively affects health outcomes, we would expect the opposite to be true: decreased patient cost-sharing should improve health outcomes. Martin and collegues developed a theoretical model to study this question. The model was based on data from the British healthcare system. By adjusting for the relative healthcare needs of the studied population, Martin and colleagues showed (in a theoretical model) that increased expenditure by the government (and therefore decreased levels of patient cost-sharing) would be associated with fewer deaths.23 How does this fit with the traditional view of health insurance economics?
Moral Hazard and Health Insurance
Traditional health insurance economics rests on specific assumptions about the impact of insured status on individual behavior. Since the late 1960s, economists have suggested that because health insurance lowers the price of healthcare to consumers but leaves its costs unchanged, the additional care consumed by insured persons is inefficient.11 The term moral hazard is used to describe situations in which an individual does not bear the full consequences of his or her actions and, therefore, has a tendency to act less carefully than he or she otherwise would.14 Economists assume that reduced prices will generate excess or inefficient utilization by increasing demand for products and services with limited benefits, citing cosmetic procedures and prescription sunglasses as examples. In other words, insured people will automatically consume more healthcare services, even if those services are not necessary. Cost-sharing represents an attempt to offset the theorized effects of moral hazard.14
However, accumulating clinical evidence24–28 presents an increasingly stark contrast to economic theory. Nyman suggests that health insurance actually represents an income transfer from the healthy to the sick, facilitating the consumption of products and services that would otherwise be unaffordable.14 As a consequence, the moral hazard associated with insurance—the changes in behavior that result from being insured—consists primarily of patients seeking standard treatments for common diseases. This reinforces the fact that although higher cost-sharing burdens may reduce healthcare expenditures, there is no way to ensure that only inappropriate utilization will be so affected. In fact, Martin and colleagues demonstrated that the opposite is true.23 Increased health spending by the British government that limits the individual's financial burden would reduce systemic healthcare costs because of the better health of the average citizen.23
Innovations in Benefit Design
Current efforts at healthcare reform have resulted in 2 new benefit design trends—consumer-directed health plans (CDHPs) and value-based benefit designs (VBBDs). CDHPs are benefit designs that consist of tax-advantaged health savings accounts, coupled with high-deductible health plans.29 Theoretically, CDHPs should make patients become savvy buyers of healthcare services by shopping for the best “deal” of any needed healthcare expenses. However, there is considerable debate regarding whether CDHPs may result in increased costs related to increasingly poor health outcomes as patients forgo needed medical care.29
Experts express concern that many patients do not have the understanding necessary to make discretionary decisions regarding healthcare decisions. Furthermore, for a CDHP design to be successful, patients must have access to cost and quality data, which are generally not available for most healthcare providers.30
According to the Benefit Design Index, there is a significant difference in the rate of adopting CDHPs between insurers and employers. Whereas the majority of insurers (61.2%) have adopted such plans, only a minority of employers (24.1%) have done so.2 Employers continue to express concern regarding down-the-line healthcare costs and CDHPs.2 However, the current economic climate may force more employers into a situation in which they must choose between adopting a CDHP or offering no health benefits. CDHPs are also a more sophisticated form of increasing patient cost-sharing. Without the tools, education, and information that will turn the average healthcare consumer into a sophisticated buyer of health services, it is likely that many patients will default to making these decisions based on cost rather than true valuation of care.
Because CDHPs are a relatively new benefit phenomenon, there is a dearth of published data on the long-term health outcomes of patients enrolled in CDHPs. Mark Snyder, Director of Health, Wellness and Benefits, Owens Corning Corporation, presented longitudinal healthcare outcomes from his company's CDHP program, at the February 2009 Employer Health and Human Capital Congress.31 Mr Snyder reported that Owens Corning has had 71% of its employees enrolled in a CDHP benefit-design program since 2004. The company has found that the CDHP population performs similarly to its preferred provider organization (PPO) population in metrics such as office visits, emergency department visits, cervical and colon cancer screenings, mammograms, and cholesterol levels. However, Mr Snyder acknowledged that neither the PPO nor the CDHP groups performed well on any health measure. The company did report a significant dip in preventive care in 2004–2005. To compensate for that, Owens Corning added a rider to cover all preventive care at 100%. Mr Snyder also reported that although the company realized significant savings in 2004, 2005, and 2006, it is now tracking with industry averages for costs.31
As often happens with health interventions, Owens Corning may now be seeing a regression to the mean32 in its benefit costs and, therefore, has not realized any true success with its CDHP program. Furthermore, Mr Snyder acknowledged that the results presented were not statistically robust, because Owens Corning does not have access to all data streams or the resources for a full analysis. This presentation highlights a warning signal for CDHPs—without access to all data and the resources to analyze that data, employers cannot be certain whether employees' health may be declining under CDHP benefit designs. By the time Owens Corning and other employers with this type of benefit design have the answer to that question, it may be too late, because employees' health may have deteriorated too far to implement lower-cost preventive measures.
VBBD is a second recent innovation in benefit design. VBBDs are benefit designs that lower patient cost-sharing for healthcare services that are deemed valuable in preventing long-term health complications such as annual physicals or medications for diabetic patients.33 VBBDs are an attempt to correct the problems of moral hazard. Using cost-sharing becomes a tool to promote informed healthcare decisions by patients. Patients are encouraged to use services that may prevent high-cost conditions, such as cancer or diabetes, as well as remain adherent to treatments for chronic conditions.34
Early data on VBBDs have shown that if implemented properly, they can be successful35; however, they require an upfront investment that many employers may not be able to afford in the current economy. Often, it takes 2 to 3 years to see a return on that investment,36 too long for employers struggling to stay afloat in a poor economy. Insurers remain reluctant to invest in VBBDs when their customers are not buying them. As a result, the marketplace is not moving in the direction of innovation but rather is staying focused on cost.
Impact on the Insurance Risk Pool
Another consideration in this debate is the impact cost-sharing may have on the insurance risk pool. Health insurance relies on the assumption that the majority of those insured would have limited utilization of medical services. The premiums paid by healthy members offset the medical costs of the sick members, making health insurance affordable for all insured.37
As healthcare costs continue to skyrocket, we must consider the viability of the third-party payer system in the United States. Increasing premiums have a direct link to the number of uninsured and underinsured, with the largest impact on low-income families.37–39 As more and more Americans are forced to choose between health insurance and other necessities (eg, food and housing), the insured risk pool will decrease. This may lead to a situation in which we do not have enough healthy insured people in the risk pool to offset the costs of the sick members, which will result in further increases in premiums and will force more individuals to forgo health insurance.40
Cost-Shifting: A Double-Edged Instrument
Payers and employers agree that growth in healthcare costs is inevitable. At the same time, further cost-shifting to individuals is unsustainable. Increasing cost-sharing is a blunt instrument: although it may reduce utilization of care that is not medically necessary, it may also result in individuals forgoing necessary care that may prevent healthcare complications down the line. Increases in deductibles will lead to an overall decrease in optimal care-seeking behavior, as families juggle healthcare costs with rising prices and stagnating wages.
Continued increases in premiums will have detrimental effects on the health insurance risk pool: younger, healthier individuals will be priced out of the market, leaving sicker, older individuals in the pool, thereby leading to an insurance “death spiral” that may be hard to recover from.
Most notably, costs continue to grow dramatically, and American health outcomes do not compare favorably with those in other developed countries,41 suggesting the broad failure of the strategy. Further analysis of the RAND's HIE data showed that, “If, as is widely believed, cost increases are driven by treatment expense and new technologies, cost-sharing can contribute to reducing costs at each point in time but may have little effect on the overall rate of cost growth.”7
Despite accumulating evidence that cost-shifting leads to undesirable health and cost consequences and, more important, has largely failed to slow healthcare cost growth, employers and insurers continue to rely on this method as their primary cost-containment strategy. Our current healthcare system has not met its fundamental goal of good health for most Americans. Rates of diabetes, hypertension, stroke, heart disease, pulmonary conditions, and mental illness are all on the rise42—pointing to a broken system.
Conclusion
As we move forward, a new solution must be implemented, one in which we move away from antiquated thinking on how health insurance should be implemented. A restructuring of our system, in which healthcare providers are paid for preventing poor health rather than being paid for each episode of care, is fundamental to moving past the failing cycle of cost-shifting to patients, increasing healthcare costs, and continuing the poor health of Americans. The system needs to be realigned so that all stakeholders are invested in improving health rather than in treating the sick. VBBDs are a step in the right direction, but without support from health insurers and the government, this innovation is likely to remain out of reach of most employers.
Biography

Melinda C. Haren
Contributor Information
Melinda C. Haren, Director of Business Content, The Zitter Group, Millburn, NJ.
Kirk McConnell, Senior Analyst, The Zitter Group, Millburn, NJ.
Arthur F. Shinn, Founder and President, Managed Pharmacy Consultants, Lake Worth, FL.
References
- 1.Haren M, McConnell K. Patient cost-sharing on the rise: results from the Benefit Design Index. Am Health Drug Benefits. 2009; 2: 70–77. [PMC free article] [PubMed] [Google Scholar]
- 2.The Zitter Group. Benefit Design Index. Spring 2008. Data on file at the Zitter Group.
- 3.American Hospital Association. Healthy people are the foundation for a productive America. TrendWatch. Spring 2007. www.aha.org/aha/trendwatch/2007/twoct2007health.pdf. Accessed January 31, 2009.
- 4.Cunningham PJ, Felland LE. Falling behind: Americans’ access to medical care deteriorates, 2003–2007. Center for Studying Health System Change. Tracking Report. No. 19. www.hschange.com/CONTENT/993. Accessed January 21, 2009. [PubMed]
- 5.Lang SS. Economists coin new word, ‘presenteeism,’ to describe worker slowdowns that account for up to 60 percent of employer health costs. Cornell News. April 20, 2004. www.news.cornell.edu/releases/April04/cost.illness.jobs.ssl.html. Accessed January 21, 2009.
- 6.Cost of lost productivity. Apples for Health. March 7, 2003. www.applesforhealth.com/HealthyBusiness/coslosprod4.html. Accessed January 21, 2009.
- 7.RAND Health. RAND's Health Insurance Experiment (HIE). www.rand.org/health/projects/hie/. Accessed September 4, 2008.
- 8.Chernew ME, Newhouse JP. What does the RAND Health Insurance Experiment tell us about the impact of patient cost-sharing on health outcomes? Am J Manag Care. 2008; 14: 412–414. [PubMed] [Google Scholar]
- 9.Fairman KA. The future of prescription drug cost-sharing: real progress or dropped opportunity? J Manag Care Pharm. 2008; 14: 70–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.RAND Health. The Health Insurance Experiment: a classic RAND study speaks to the current healthcare reform debate. 2006. www.rand.org/pubs/research_briefs/RB9174/index1.html. Accessed September 4, 2008.
- 11.Goldman DP, Joyce GF, Escarce JJ, et al. Pharmacy benefits and the use of drugs by the chronically ill. JAMA. 2004;291: 2344–2350. [DOI] [PubMed] [Google Scholar]
- 12.Schoen C, Collins SR, Kriss JL, Doty MM. How many are underinsured? Trends among U.S. adults, 2003 and 2007. Health Aff (Millwood). 2008; 27: w298–w309. [DOI] [PubMed] [Google Scholar]
- 13.Emanuel EJ, Fuchs VR. Who really pays for health care? The myth of “shared responsibility.” JAMA. 2008; 299: 1057–1059. [DOI] [PubMed] [Google Scholar]
- 14.Nyman J. The Theory of Demand for Health Insurance. Palo Alto, CA: Stanford Economics and Finance; 2002. [Google Scholar]
- 15.Palmer AJ, Annemans L, Roze S, et al. Cost-effectiveness of early irbesartan treatment versus control (standard antihypertensive medications excluding ACE inhibitors, other angiotensin-2 receptor antagonists, and dihydropyridine calcium channel blockers) or late irbesartan treatment in patients with type 2 diabetes, hypertension, and renal disease. Diabetes Care. 2004; 27: 1897–1903. [DOI] [PubMed] [Google Scholar]
- 16.Eddy DM, Schlessinger L, Kahn R. Clinical outcomes and cost-effectiveness of strategies for managing people at high risk for diabetes. Ann Intern Med. 2005; 143: 251–264. [DOI] [PubMed] [Google Scholar]
- 17.Mattola MF. The role of exercise in the prevention and treatment of gestational diabetes mellitus. Curr Diab Rep. 2008; 8: 299–304. [DOI] [PubMed] [Google Scholar]
- 18.Yang LY, Gutin B, Barbeau P, et al. Cost-effectiveness of a school-based obesity prevention program. J Sch Health. 2008; 78: 619–624. [DOI] [PubMed] [Google Scholar]
- 19.Stagnitti MN. Medical Expenditure Panel Survey Statistical Brief #5: Medical care and treatment for chronic conditions, 2000. www.meps.ahrq.gov/mepsweb/data_files/publications/st5/stat05.pdf. Accessed September 22, 2008.
- 20.Cohen SB, Yu W. Medical Expenditure Panel Survey Statistical Brief #191: The persistence in the level of health expenditures over time: estimates for the U.S. population, 2004–2005. November 30, 2007. www.meps.ahrq.gov/mepsweb/data_files/publications/st191/stat191.pdf. Accessed September 22, 2008.
- 21.CDC data show that millions of uninsured adults forgo needed treatment for chronic health conditions. www.prnewswire.com/cgi-bin/stories.pl?ACCT=109&STORY=/www/story/05-02-2005/0003536443&EDATE=. Accessed September 22, 2008.
- 22.Mahoney JJ. Value-based benefit design: using a predictive modeling approach to improve compliance. J Managed Care Pharm. 2008; 14 (6 suppl B): 3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin S, Rice N, Smith PC. Does health care spending improve health outcomes? Evidence from English programme budgeting data. J Health Econ. 2008; 27: 826–842. [DOI] [PubMed] [Google Scholar]
- 24.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001; 285: 421–449. [DOI] [PubMed] [Google Scholar]
- 25.Kennedy J, Erb C. Prescription noncompliance due to cost among adults with disabilities in the United States. Am J Public Health. 2002; 92: 1120–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heisler M, Langa KM, Eby EL, et al. The health effects of restricting prescription medication use because of cost. Med Care. 2004; 42: 626–634. [DOI] [PubMed] [Google Scholar]
- 27.Huskamp HA, Deverka PA, Epstein AM, et al. The effect of incentive-based formularies on prescription-drug utilization and spending. N Engl J Med. 2003; 349: 2224–2232. [DOI] [PubMed] [Google Scholar]
- 28.Wong MD, Andersen R, Sherbourne CD, et al. Effects of cost-sharing on care seeking and health status: results from the Medical Outcomes Study. Am J Public Health. 2001; 91: 1889–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berenson RA, Cassel CK. Consumer-driven healthcare may not be what patients need—caveat emptor. JAMA. 2009;301: 321–323. [DOI] [PubMed] [Google Scholar]
- 30.Jost TS. Health Care at Risk: A Critique of the Consumer-Driven Movement. Durham, NC: Duke University Press; 2007.
- 31.Snyder M. Consumer directed healthcare [online presentation]. Employer Health and Human Capital Congress. February 2009. www.worldcongress.com/presentations/v2/index.cfm?p=presentations.cfm&confCode=HH09035&letter=s. Accessed February 10, 2009.
- 32.Research Methods Knowledge Base. Regression to the mean. October 2006. www.socialresearchmethods.net/kb/regrmean.php. Accessed February 10, 2009.
- 33.Atlantic Information Services. Plans experiment with ‘value-based’ benefit designs, but cite operational challenges. www.aishealth.com/ManagedCare/DM/MCW_Value-Based_Benefit_Designs.html. Accessed February 10, 2009.
- 34.Midwest Business Group on Health. MBGH Annual Employer Benefit Survey reveals growing shift to value-based benefit design [press release]. May 2, 2008. http://benefitslink.com/pr/detail.php?id=41884. Accessed February 10, 2009.
- 35.Malley JJ. An ounce of prevention: the potential for value-based pharmacy benefits in cost containment. Benefits Q. 2008; 24: 25–28. [PubMed] [Google Scholar]
- 36.Goff VV. Pharmacy benefits: new concepts in plan design. NHPF Issue Brief. 2002;(772):1–16. [PubMed]
- 37.Pauly M, Herring B. Risk pooling and regulation in today's individual health insurance market. December 15, 2006. http://aspe.hhs.gov/daltcp/reports/2006/riskpool.htm. Accessed September 26, 2008. [DOI] [PubMed]
- 38.National Bureau of Economic Research. Health insurance subsidies, coverage, and costs. www.nber.org/aginghealth/spring03/w9567.html. Accessed September 26, 2008. [PubMed]
- 39.Kasier Commission on Medicaid and the Uninsured. The Uninsured: A Primer: Key Facts About Americans Without Health Insurance. January 2006. www.kff.org/uninsured/upload/7451.pdf. Accessed September 26, 2008.
- 40.Starr Sered S, Fernandopulle R. Uninsured in America: Life and Death in the Land of Opportunity. April 2005. Berkeley, CA: University of California Press; 2005.
- 41.Davis K, Schoen C, Schoenbaum SC, et al. Mirror, Mirror on the Wall: An International Update on the Comparative Performance of American Healthcare. May 2007. The Commonwealth Fund; www.commonwealthfund.org/Content/Publications/Fund-Reports/2007/May/Mirror–Mirror-on-the-Wall–An-International-Update-on-the-Comparative-Performance-of-American-Healt.aspx. Accessed March 11, 2009. [Google Scholar]
- 42.Arvantes J. Chronic diseases spark dramatic increase in treatment cost while lowering productivity, study says. AAFP News. June 4, 2008. www.aafp.org/online/en/home/publications/news/news-now/health-of-the-public/20080604milken-report.html. Accessed February 10, 2009.