Abstract
Aim
This article outlines the rationale for a family-focused psychoeducational intervention for individuals at risk for psychosis and explains the design of a randomized multisite trial to test its efficacy.
Methods
Adolescents and young adults that meet criteria for a psychosis risk syndrome at eight participating North American Prodromal Longitudinal Study sites are randomly assigned to a 6-month, 18-session family-focused treatment for prodromal youth or a 3-session psychoeducational enhanced care control intervention and followed over 1 year.
Results
The results will determine whether the use of a family intervention is able to significantly improve functional outcomes, decrease the severity of positive symptoms and possibly prevent the onset of full psychosis, compared with enhanced care alone. Levels of familial criticism at baseline are hypothesized to moderate responses to family intervention. Improvements in knowledge about symptoms, family communication and problem solving will be tested as mediators in the pathways between treatment assignment and clinical or psychosocial outcomes in high-risk youth.
Conclusions
The ongoing trial evaluates whether a non-invasive psycho-social approach can significantly enhance functional outcomes and prevent the ultra high risk patients from developing psychosis. The results will provide an important stepping stone in the movement of the field from refining early detection strategies to developing efficacious preventative treatments.
Keywords: family therapy, prodrome, psychosis, schizophrenia, treatment
Introduction
The aim of preventing schizophrenia and other psychotic disorders has led researchers to focus on early identification of individuals at risk for psychosis. The ‘ultra high risk’ (UHR) syndrome refers to a set of clinical criteria to detect individuals exhibiting risk factors for developing psychosis. The UHR criteria are characterized by attenuated psychotic symptoms and/or a family history of psychosis with functional deterioration.1 Approximately 35% of individuals identified as UHR develop a psychotic disorder within 2.5 years.2–4 Although the UHR construct represents one of the strongest predictors of psychosis to date, the majority of UHR subjects do not develop a psychotic disorder, and conversion rates have dropped in recent years in some studies/locations.5 Although not all UHR subjects transition to psychosis, many suffer from poor social and role functioning and are subsequently at significant risk for school failures and long-term social and occupational disabilities.6 In addition, many UHR subjects experience clinically significant levels of anxiety and depression. Thus, it is critical to develop early, minimally invasive interventions.
Researchers have tested the efficacy of antipsychotic medications in an effort to address the clinical needs of UHR patients. The two randomized controlled trials (RCTs) that have tested the prophylactic effects of antipsychotic medications on UHR patients have produced inconclusive results.7,8 Given the lack of evidence supporting the use of antipsychotic medications, there is a need to develop efficacious treatments to stave off the full onset of psychosis and improve functioning. A recent RCT of long-chain omega-3 fatty acids versus placebo, with each UHR group receiving up to nine sessions of need-based psychosocial intervention, found significant improvement on measures of positive symptoms, negative symptoms and functioning in the group receiving fatty acids.9 Low-risk interventions are well suited to address the unique challenges of treating a UHR population, such as the need to limit exposure to adverse events in potentially false positive cases.
Various cognitive behavioural treatment (CBT) manuals have been developed for the UHR population and tested in several RCTs.7,10,11 First, in an RCT of risperidone and CBT versus a needs-based intervention administered for 6 months, McGorry and colleagues7 established that those receiving the combination of medications and CBT had lower rates of conversion at the end of the treatment. The group differences were not significant at 6-month follow-up, nor were there differences between groups on measures of functional outcome. A second study found that patients who completed a 6-month trial of CBT had significantly reduced rates of transition to psychosis compared with patients who received monitoring alone.10 Although those differences were not maintained at the 3-year follow-up, those patients who received CBT were less likely than those in the control condition to require treatment with antipsychotics at follow-up.11 In a third RCT comparing CBT to supportive therapy,12 there was a rapid decline in positive symptoms for both treatment groups but no significant improvement in negative symptoms or social functioning. Taken together, these studies demonstrate the potential efficacy of psychosocial interventions at the early phase of illness, whereas also challenging the field to develop interventions that can improve functional outcomes.
A pilot study examining the feasibility and acceptability of a 9-month psychoeducational multifamily group (PMFG) treatment for young people at risk for psychosis yielded encouraging results.13 Individuals and families reported benefitting from the intervention and UHR patients improved significantly in positive symptoms and in work/school functioning. Nonetheless, engaging this population in groups was problematic, as reflected by higher than expected treatment refusal rates (45%), often due to concerns about privacy. Also, the relatively small number of families available to a specialized UHR or first-episode treatment centre presents unique challenges for multifamily groups. In one first-episode study, families had to wait 6–12 months on average until a sufficient number of patients were gathered to start a group.14 Although this open trial showed promise, multiple interventions were introduced simultaneously with 56% of the sample receiving antipsychotic medications and 100% receiving individual therapy either concurrently or prior to the PMFG intervention. Thus, conclusions about the efficacy of PMFG await the results of RCTs. In light of the extensive literature on family psychoeducation as a treatment of choice for schizophrenia,15 preliminary success of PMFG in a UHR population, and previous research that has linked the family environment to symptomatic and functional outcomes in schizophrenia,16 first-episode psychosis17 and UHR13,18,19 populations, family therapy is a promising intervention approach worthy of investigating for a UHR population. Miklowitz and colleagues20 developed family-focused treatment (FFT) for patients with bipolar disorder and their families. RCTs testing the efficacy of FFT combined with pharmacotherapy in adult and paediatric bipolar populations resulted in significant recovery rates over 1 year21 (77% of adult patients vs. 52% in a brief treatment control), symptomatic improvement,20 relapse reduction,20–22 and better social and overall functioning.22,23 Adolescents from families that were higher in criticism at baseline showed a greater response to FFT than those from families lower in criticism at baseline.24 In a different study, the positive effect of FFT treatment on adult patients' symptoms was partially mediated by increases in patients' positive interactional behaviour.25 The current project aims to conduct an RCT to determine the efficacy of an adapted version of FFT, family-focused treatment for prodromal youth (FFT-PY) in comparison with a briefer enhanced care (EC) condition in improving functional outcomes, decreasing symptom severity, and reducing transition rates to full psychosis in adolescents and young adults at risk for psychosis. Although other RCTs have focused primarily on reducing symptoms, this family treatment aims to improve functional outcomes due to the broader focus of the intervention on enhancing coping, communication, and problem solving skills that can be applied in the peer, home, school and work environments. Additionally, family members who are in frequent contact with UHR youths may be able to reinforce skills that have been learned in therapy more frequently than would a therapist meeting once per week with a youth.
The following primary hypotheses will be tested:
UHR youths in the FFT-PY condition will experience greater gains in psychosocial functioning and experience less severe subthreshold psychotic symptoms than UHR youths in the EC condition over 1-year follow-up.
UHR youths in the FFT-PY condition will experience reduced rates of conversion to a psychotic disorder relative to UHR youths in the EC condition over 1-year follow-up.
The secondary hypothesis to be tested is the following: Treatment-associated gains in psychosocial functioning and reductions in symptom severity will be moderated by levels of familial criticism at baseline. Specifically, and consistent with prior research,24,25 we expect that youths who are in high-criticism families will show greater benefits than youths in low-criticism families in FFT relative to EC. Further, the treatment-related improvements in youths' and family members' communication and problem-solving skills and knowledge about prodromal symptoms will partially mediate the effectiveness of FFT-PY in enhancing the clinical and functional outcomes of UHR youths.
This article describes the 8-site study, its measurement strategies, and the adaptation and re-manualization of the FFT model to address the needs of UHR youth.
Method
Participants
Adolescents and young adults, aged 12–35, are being recruited from each of eight sites in the North American Prodrome Longitudinal Study (NAPLS), a consortium of UHR research programmes. Once enrolled and consented, participants are approached about the FFT-PY study, consented and provided with a random assignment to one of two treatment conditions (FFT-PY or EC). Consistent with the inclusion criteria for NAPLS, the current study requires that each subject meet the diagnostic criteria of a current ‘psychosis risk syndrome’, as defined by the Structured Interview for Prodromal Syndromes (SIPS).26 A psychosis risk syndrome is defined by the presence of: (i) attenuated positive symptoms; (ii) brief intermittent psychotic symptoms; (iii) decline in functioning and either a diagnosis of schizotypal personality disorder or a first-degree relative with a psychotic disorder; or (iv) a diagnosis of schizotypal personality disorder in participants age 18 or younger. Due to the study's focus on family interventions, subjects must have at least one family member who is willing to participate in the treatment, even if the subject is not living with this family member. A family member can include, but is not limited to, a parent, sibling, caregiver, other relative and/or significant other.
Power calculations conducted in collaboration with a statistician determined the recruitment goal of 96 participants, with 48 in each treatment condition. Assuming the current attrition rate remains at approximately 20%, this sample size would have 80% power to detect a difference in symptomatic and functional outcome of 0.50 standard deviation units or greater and 80% power to detect a reduction of 34% or more in the expected conversion rate.
Measures
All subjects are evaluated using measures from the NAPLS protocol at baseline, 6 and 12 months. The earliest enrolled subjects may also be followed up at 18 and 24 months. Additional measures of family functioning were added. Independent evaluators, blind to treatment assignment, are completing all outcome measures. Trained MA or PhD level clinicians who participated in an in-depth ‘gold-standard’ training programme regarding the administration and scoring of the SIPS and Structured Clinical Interview for the DSM-IV (SCID-I) administer the clinical measures. Additionally, all potential cases must pass consensus agreement via a conference call with NAPLS investigators. In order to ensure the blind and reduce the potential for rating bias, independent supervisors, not involved in the trial, are supervising the clinical assessments administered by independent evaluators. Assessment files and treatment files are kept in separate filing cabinets. The staff members working on the trial and those completing the independent evaluations are instructed to avoid breaking the blind by not discussing the treatment status of individual participants. Additionally, participants involved in the trial are asked not to reveal their condition to the independent evaluators. If an evaluator is unblinded, he/she is replaced with a new blind evaluator.
Clinical measures
The course of attenuated positive symptoms over time and conversion to psychosis is being evaluated with the Scale of Prodromal Symptoms26 at each study visit. The criterion for conversion to psychosis is met when positive symptoms are experienced at a psychotic level of intensity for >1 h per day at an average frequency of 4 days/week over a 1-month period. Psychotic intensity is defined by endorsing full conviction in the experience of a positive symptom and/or experiencing psychotic symptoms that are seriously disorganizing or dangerous. Diagnostic outcomes are measured using the SCID-I. Our study does not contain a formal measure of adverse events, such as increased stigma. However potential negative effects of our treatment ought to be detected by the treating clinicians or the treatment satisfaction questionnaire given at the end of treatment.
Social and role functioning
Psychosocial functioning is based on two domains: interpersonal skills (social functioning) and independent school/employment or homemaking capabilities (role functioning), which is measured by the interview-based Global Functioning Scale (GFS): Social and the GFS: Role. These scales have high inter-rater reliabilities and construct validity.27
Family functioning
Subjects and family members are asked to complete the Knowledge regarding the Prodrome Questionnaire,28 a 32-item questionnaire, before the FFT-PY or EC treatments and again at the end of treatment. Given that this is a psychoeducational intervention, the knowledge that patients and family members acquire over the course of the treatment may mediate clinical and functional outcomes.
To determine whether qualities of the family environment moderate participants' responses to FFT versus EC, and mediate changes in clinical and functional variables, various aspects of the family environment are evaluated at baseline and post-treatment. Family measures include the Perceived Criticism and Perceived Warmth Scales (PCPW),29 the Conflict Behavior Questionnaire (CBQ),30 and a 10-min problem-solving family interaction task.31 The UHR subject and at least one family member complete the PCPW and CBQ. The CBQ is a measure of perceived family conflict that has been widely used with families with children and adolescents.32,33 The PCPW surveys the degree to which a family member perceives criticism and warmth in a key relative and has been used as a reliable predictor of outcomes in the UHR population.18 Lastly, the problem-solving interaction task identifies youth and family members' problem solving and communication skills and shows good concurrent validity with Camberwell Family Interview-measured dimensions of expressed emotion.31
Fidelity measure
Clinicians participate in a 2-day workshop to learn the FFT-PY and EC treatments. They receive weekly individual supervision until standards of competency and treatment adherence are met at which point supervision is provided monthly. Fidelity to the treatment model is measured by the Therapist Competence and Adherence Scale, Revised (TCAS-R).34,35 The TCAS-R is rated by independent observers based on at least three sessions for each study case (at minimum, one from psychoeducation, one from communication enhancement training and one from problem solving). For the EC condition, at least one session is reviewed from every case. Clinicians who score low on the TCAS-R items are offered additional training in the FFT-PY or EC manuals and more intensive supervision.
Procedure
Each participant and his/her family are fully informed about the rationale and procedures for the study. Both the parent and the underage minor must provide consent/assent for the participant and family to be included. If a participant loses capacity to consent, his/her legal guardian would make treatment decisions on the participant's behalf. Participants who lose capacity will not be withdrawn from the protocol. Should a safety issue arise, such as the participant becomes a danger to self/others and/or is seriously disorganized and dangerous, the treating clinician would follow emergency procedures. After the participant is determined to be eligible and consent/assent forms are signed, a random assignment (stratified by antipsychotic use and site) to FFT-PY or EC is determined. The random assignment is made using an automated randomization system and is kept in a secure location by an independent person. The random assignment is relayed directly to the treating clinician through a secure email. The same clinicians are delivering the FFT-PY and EC treatments.
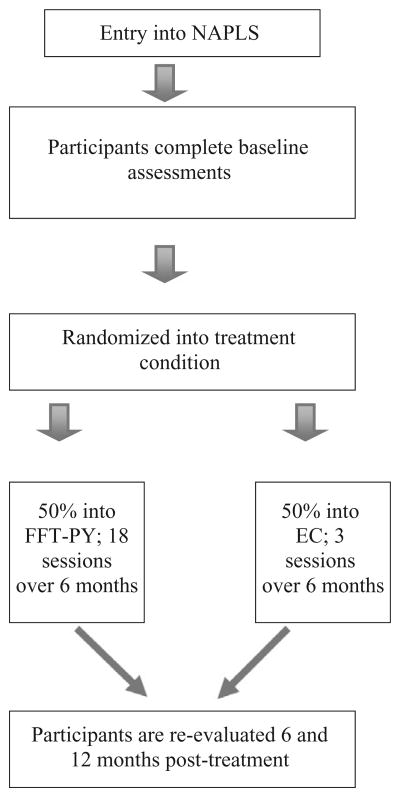
If subjects are assigned to FFT-PY, the family receives 18 sessions over 6 months (12 weekly, 6 biweekly) whereas families in the EC condition receive a total of three weekly sessions over the first 6 months. All subjects in the FFT-PY condition receive the same services offered in the EC condition. Figure 1 outlines the study design.
Figure 1.
FFT-PY study design. EC, enhanced care; FFT-PY, family-focused treatment for prodromal youth; NAPLS, North American Prodrome Longitudinal Study.
Data analysis plan
All analyses will be by intent to treat. The primary outcome variables (functioning and symptom severity), all treated as continuous variables, will be examined as a function of treatment condition and site using mixed effects regression models. Similar approaches will be used to examine the trajectory of functional outcome scores. The advantages of mixed effects models over traditional repeated measures models are that they allow for (i) the inclusion of participants with missing data, (ii) observations that are unequally spread out over time (both within and between participants), and (iii) more flexible modelling of variance and covariance patterns of residuals. Moderators (e.g. family criticism) will be tested through examining the treatment by moderator by time interaction in the mixed models. Changes in knowledge about symptoms, communication and problem-solving skills will be examined in mixed models as mediators of the effects of FFT versus EC on patient outcomes. For evaluation of time to conversion, we will use Cox's proportional hazards model and Kaplan–Meier survival analysis.
For the purposes of this study, we operationally define as ‘clinically significant’ an improvement of 0.5 SDs or larger on the Social and Role Functioning scales or an improvement to an absolute score of 7 or higher on both scales (which corresponds to the normal range of functioning) or both. In terms of positive symptoms, clinically significant change is defined as a reduction in positive symptom severity of 0.5 SDs or larger or a reduction to below the prodromal range of severity (i.e. 2 or lower on all P items) or both.
Treatment Framework
One of the theoretical assumptions of the FFT model is that family members' reactions to the patient's psychiatric symptoms can play either a protective role or contribute to the worsening of symptoms.23 FFT utilizes psychoeducation, stress management and skill-building strategies to address the demands that psychiatric symptoms often impose on families. Notably, the onset of attenuated positive symptoms is often accompanied by functional impairments in the youth, which typically affect family functioning. For example, if a UHR subject is experiencing a high degree of avolition and his grades decline, the family is faced with a decision about how to react. On the one hand, they want to buffer the young person from stress because of his experience with distressing symptoms, yet they also want to stop the decline of academic functioning. In many ways, the onset of symptoms and the family's reactions are seen as developmental challenges in the family. Family members must negotiate the appropriate level of involvement with the UHR subject. The framework of FFT encourages the family to navigate these challenges in a way that meets the needs of each family member, given their newly acquired knowledge (from psychoeducational sessions) about the nature of the UHR syndrome and how it affects the youth. Although the primary goals of the treatment are to decrease the risk of worsening symptoms and enhance social and role functioning, improvement in youths' and family members' communication and problem solving skills is assumed to mediate these changes and hence an important focus of the treatment.
The FFT-PY manual36 was adapted from the FFT manual for children at-risk for bipolar disorder (FFT-A),23 and guided by research on multifamily group therapy,37 and individual, family and group treatment of youth at risk for psychosis.38,39 Adaptations to the manual were made to address the unique clinical issues that affect a UHR population, such as functional deficits, positive symptoms and negative symptoms.
Whereas the content of the FFT-PY manual is somewhat different from previous FFT manuals, the approach of clinicians, however, is the same. Clinicians are trained to be active, directive, and to provide an open and ‘down to earth’ approach with patients and families. Although the treatment has a significant psychoeducational component, it is not intended to be purely didactic. Instead, family members are encouraged to interact and practice skills in sessions with the therapist acting as a coach. Although the treatment is manualized, flexibility is emphasized. Therapists are encouraged to meet the needs of each family, which might require a therapist to skip and/or add a topic and adjust the pacing of sessions. This flexibility is afforded by the advantage of an individualized family therapy format.
Treatment structure
Similar to the FFT for bipolar disorder manual, the FFT-PY manual consists of three modules: (i) psychoeducation, (ii) communication enhancement, and (iii) problem solving (Table 1).
Table 1. Family-focused treatment-prodromal youth session overview.
| Session # | Goals for each session |
|---|---|
| I. Family education: Sessions 1–6 | |
| 1 | Overview of treatment and goal setting |
| 2 | Discussion of symptoms and vulnerability-stress model |
| 3 | Identifying and evaluating stress |
| 4 | Mobilizing coping efforts and teach a new skill |
| 5 | Optimizing family support |
| 6 | Prevention planning |
| II. Communication enhancement training: Sessions 7–11 | |
| 7 | Teach skill #1: Expressing positive feelings |
| 8 | Teach skill #2: Active listening |
| 9 | Teach skill #3: Communication clarity |
| 10 | Teach skill #4: Making positive requests for change |
| 11 | Teach skill #5: Expressing negative feelings |
| III. Problem solving 12–18 | |
| 12–17 | Structured problem solving |
| 18 | Termination |
The objectives of the educational sessions are to teach the family about the clinical and functional sequelae of the UHR syndrome, discuss the role of stress in the clinical course, teach skills that can help manage stress, and develop a prevention action plan to be implemented if symptoms and level of functioning worsen. The skill-based approach and focus on family engagement are strategies specifically designed to improve psychosocial functioning. The goals of communication skills training and structured problem solving are to teach the UHR youth to operate at a more effective level in the family, among peers and in an academic/occupational environment. The treatment model encourages flexibility in order to accommodate working with diverse families, such as single/dual parents, gay/straight parents, grandparents as primary caregivers, and couples.
Psychoeducation module
The first six sessions provide education to the family in an interactive format. The family is introduced to the symptoms of the UHR syndrome, associated functional impairments, and other comorbid problems, such as depression and anxiety. Feedback from the subject's clinical assessment is integrated into the discussions of symptoms of the UHR syndrome. The interaction between biological vulnerability and stress is introduced in order to provide the rationale for future work on stress reduction and coping enhancement. When discussing the psychoeducational material, efforts are made to minimize stigma and avoid pathologizing the subject. One of the ways this is done is by normalizing the subject's symptoms. For instance, if a young person is experiencing suspicious thinking, the therapist might say, ‘It's very common to have concerns about what other people think of us, and although this has become increasingly bothersome to you, I think we can all relate to the feelings that this brings up for you’. Additionally, families are informed that the majority of UHR youths do not go on to develop a psychotic disorder.
During the educational sessions, the therapist encourages the family to identify various sources of stress that stem from the individual (e.g. negative self talk, trouble organizing), school/work (e.g. classes are too demanding, deadlines), family (criticism, unclear rules) and the community (e.g. dangerous neighbourhood). The therapist facilitates a discussion regarding the physical (e.g. muscle tension), cognitive (e.g. trouble focusing), behavioural (e.g. withdrawal) and affective (e.g. irritability) signs of stress. Coping strategies are then discussed with the goal of broadening each family member's repertoire of coping options. In order to integrate the material, a ‘prevention action plan’ is developed that includes early warning signs of worsening symptoms or functioning and coping options.
The FFT-PY version of FFT focuses on additional skills that are relevant to a UHR population. Specifically, material was added that addresses social skills deficits, negative and anxiety symptoms, and academic impairments. Based on the clinical and family assessments and initial therapy sessions, the clinician conceptualizes each case and then selects those skills that would provide the most benefit to each individual youth and family. For example, if a subject is experiencing significant social impairment, the social skills training can be provided; if negative symptoms are a significant concern, the therapist can implement pleasant event scheduling or other behavioural activation plans. A new session was added to the FFT-PY manual that works directly on optimizing family support. In this session, the therapist facilitates a discussion regarding how the family members react to stressful events, symptoms and impairments in functioning, and in turn how subjects react to family members' expressions of frustration or attempts to help. Psychoeducation is provided regarding the importance of establishing and maintaining an environment that is low key and non-critical.
Communication enhancement training (CET) module
Sessions 7–11 focus on five different communication skills: (i) expressing positive feelings; (ii) active listening; (iii) communication clarity; (iv) making positive requests for change; and (v) expressing negative feelings. The communication clarity session targets disorganized thinking in patients and communication deviance in family members, which has been shown to be stressful for patients and family members.40,41 The therapist teaches skills such as the importance of using concise speech, being specific rather than abstract and bringing up one topic at a time. During the CET module, the bulk of the work in session is conducted using a role-playing format. The therapist facilitates discussions between family members and encourages the use of the new communication skills in within-session rehearsal and between-session homework.
Structured problem-solving module
The final phase of treatment is designed to teach families about the importance of utilizing a structured approach to solving problems. During this module, the therapist explains the different steps of solving problems: (i) define the problem; (ii) identify the goal; (iii) list potential solutions; (iv) evaluate advantages and disadvantages of the solutions; and (v) select a solution and develop a plan. Families learn the skills by using therapist-facilitated role-playing and practicing the skills between sessions. Examples of topics that are brought up include developing strategies to increase activity, improving social skills, decreasing family conflict and managing symptoms.
EC model
To date, there are no standards of usual care for UHR subjects. The EC model was developed to mirror a treatment-as-usual condition that includes case management and family education. The EC manual42 was adapted from the manual for brief psychoeducation with adolescent bipolar patients.35 It consists of: (i) diagnostic assessments with a study evaluator; (ii) psychoeducational sessions focused on the UHR syndrome, risk and protective factors, and an individualized prevention plan that are scheduled after each assessment time point; (iii) ongoing case management and referral for medication management (if needed); and (iv) references for reading materials pertinent to managing UHR symptoms (Table 2). Three additional crisis sessions can be provided if the UHR youth experiences a clinical emergency. In the case of psychiatric emergencies, patient safety is prioritized and clinicians are advised to apply ethical standards of care to mitigate the crisis.
Table 2. Enhanced care session outline.
| Session # | Goals for each session |
|---|---|
| 1 | Discussion of symptoms, vulnerability-stress model |
| 2 | Develop prevention action plan |
| 3 | Provide clinical and neuropsychological feedback |
| Feedback | 6- 12-, 18-, 24-month clinical and neuropsychological feedbacks |
Discussion
This article has outlined the rationale and design of the first RCT testing the efficacy of a family intervention for adolescents and young adults at risk for psychosis. The results will show whether the use of a family intervention is able to significantly enhance functional outcomes, decrease symptoms and prevent the onset of full psychosis. Further, the family environment will be investigated to determine if particular families, such as those who enter treatment with highly conflictual interactions, benefit more from treatment than families who experience lower levels of conflict. The mediating effects of improvements in family communication/problem solving and knowledge of the UHR syndrome on youth clinical and functional outcomes will be examined. The roles of medications and medication adherence will be examined in an exploratory manner.
The current trial is limited by the requirement that subjects have at least one family member who is able and willing to participate in treatment. We will track enrolment to identify the percentage of subjects who are ineligible due to a lack of access to family members and/or an unwillingness to involve family in treatment. The current study has a wide range of age, which might limit the findings, thus the potential effects of age (and other demographic characteristics) will be tested and controlled for as they might affect the intervention outcomes. Additionally, due to some study participants receiving antipsychotic medications, conversion rates might be lower than expected in both treatment conditions. Lastly, since the treatment is being carried out in medical centres, its results may not translate into community mental health settings. It will be important to evaluate how quickly clinicians are able to learn to deliver the treatment, and the factors that impede this process.
In summary, the current study is the first RCT to test the efficacy of a family intervention in a population at significant risk for psychosis. The ongoing trial will determine whether a non-invasive psycho-social approach can significantly enhance functional outcomes and possibly even prevent UHR subjects from developing psychosis. The results will provide an important stepping stone in the movement of the field from refining early detection strategies to developing efficacious early interventions.
References
- 1.Yung AR, McGorry PR. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22:353–70. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
- 2.Cannon TD, Cadenhead KD, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olson KA, Rosenbaum B. Prospective investigations of the prodromal state of schizophrenia: assessment instruments. Acta Psychiatr Scand. 2006;113:273–82. doi: 10.1111/j.1600-0447.2005.00698.x. [DOI] [PubMed] [Google Scholar]
- 4.Ruhrmam S, Schultze-Lutter F, Salokangas RKR, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. 2010;67:241–51. doi: 10.1001/archgenpsychiatry.2009.206. [DOI] [PubMed] [Google Scholar]
- 5.Yung AR, Yuen HP, Berger G, et al. Declining transition rate in ultra high risk (prodromal) services: dilution or reduction of risk? Schizophr Bull. 2007;33:673–81. doi: 10.1093/schbul/sbm015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Correll CU, Hauser H, Auther AM, Cornblatt BA. Research in people with psychosis risk syndrome: a review of the current evidence and future directions. J Child Psychol Psychiatry. 2010;51:390–431. doi: 10.1111/j.1469-7610.2010.02235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGorry PD, Yung AR, Phillips LJ, et al. Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Arch Gen Psychiatry. 2002;59:1–8. doi: 10.1001/archpsyc.59.10.921. [DOI] [PubMed] [Google Scholar]
- 8.McGlashan TH, Zipursky RB, Perkins D, et al. Randomized double-blind clinical trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry. 2006;16:790–9. doi: 10.1176/ajp.2006.163.5.790. [DOI] [PubMed] [Google Scholar]
- 9.Amminger GP, Schafer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychosis disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67:146–54. doi: 10.1001/archgenpsychiatry.2009.192. [DOI] [PubMed] [Google Scholar]
- 10.Morrison AP, French P, Walford L, et al. Cognitive therapy for the prevention of psychosis in people at ultra-high risk. Br J Psychiatry. 2004;184:291–7. doi: 10.1192/bjp.185.4.291. [DOI] [PubMed] [Google Scholar]
- 11.Morrison AP, French P, Parker S, et al. Three-year follow-up off a randomized controlled trial of cognitive therapy for the prevention of psychosis in people at ultra high risk. Schizophr Bull. 2007;33:682–7. doi: 10.1093/schbul/sbl042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Addington J, Epstein I, Liu L, French P, Boydell KM, Zipursky RB. Randomized controlled trial of cognitive behavioral therapy for individuals at clinical high risk for psychosis. Schizophr Res. 2011;125:54–61. doi: 10.1016/j.schres.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 13.O'Brien MP, Zinberg JL, Bearden CE, et al. Psychoeducational multi-family group treatment with adolescents at high risk for developing psychosis. Early Interv Psychiatry. 2007;1:25–32. doi: 10.1111/j.1751-7893.2007.00046.x. [DOI] [PubMed] [Google Scholar]
- 14.Fjell A, Thorsen GB, Friis S, et al. Multifamily group treatment in a program for patients with first-episode psychosis: experiences from the TIPS Project. Psychiatr Serv. 2007;58:171–3. doi: 10.1176/ps.2007.58.2.171. [DOI] [PubMed] [Google Scholar]
- 15.McFarlane WR, Dixon L, Luken E, Lucksted A. Family psychoeducation in schizophrenia: a review of the literature. J Marital Fam Ther. 2003;29:223–45. doi: 10.1111/j.1752-0606.2003.tb01202.x. [DOI] [PubMed] [Google Scholar]
- 16.Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse. Arch Gen Psychiatry. 1998;55:547–52. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- 17.Hooley JM, Richters JE. Expressed emotion: a developmental perspective. In: Cicchetti D, Toth SL, editors. Emotion, Cognition, and Representation. Rochester, NY: University of Rochester Press; 1995. pp. 136–66. [Google Scholar]
- 18.Schlosser DA, Zinberg JL, Loewy RL, et al. Predicting the longitudinal effects of the family environment on prodormal symptoms and functioning in patients at risk for psychosis. Schizophr Res. 2010;113:69–75. doi: 10.1016/j.schres.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Brien MP, Gordon JL, Bearden CE, Lopez SR, Kopelowicz A, Cannon TD. Positive family environment predicts improvement in symptoms and social functioning among adolescents at imminent risk for onset of psychosis. Schizophr Res. 2006;81:269–75. doi: 10.1016/j.schres.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL. A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Arch Gen Psychiatry. 2003;60:904–12. doi: 10.1001/archpsyc.60.9.904. [DOI] [PubMed] [Google Scholar]
- 21.Miklowitz DJ, Simoneau TL, George EL, et al. Family-focused treatment of bipolar disorder: 1-year effects of a psychoeducational program in conjunction with pharmacotherapy. Biol Psychiatry. 2000;48:582–92. doi: 10.1016/s0006-3223(00)00931-8. [DOI] [PubMed] [Google Scholar]
- 22.Miklowitz DJ, Otto MW, Frank E, et al. Intensive psychosocial intervention enhances functioning in patients with bipolar depression. Am J Psychiatry. 2007;16:1340–7. doi: 10.1176/appi.ajp.2007.07020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miklowitz DJ, Chang KD. Prevention of bipolar disorder in at-risk children: theoretical assumptions and empirical foundations. Dev Psychopathol. 2008;20:881–97. doi: 10.1017/S0954579408000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miklowitz DJ, Axelson DA, George EL, et al. Expressed emotion moderates the effects of family-focused treatment for bipolar adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48:643–51. doi: 10.1097/CHI.0b013e3181a0ab9d. [DOI] [PubMed] [Google Scholar]
- 25.Simoneau TL, Miklowitz DJ, Richards JA, Saleem R, George EL. Bipolar disorder and family communication: effects of psychoeducational treatment program. J Abnorm Psychol. 1999;108:588–97. doi: 10.1037//0021-843x.108.4.588. [DOI] [PubMed] [Google Scholar]
- 26.Miller TJ, McGlashan TH, Rosen JL. Prospective diagnosis of the initial prodrome for schizophrenia based on the structured interview for prodromal syndromes: preliminary evidence of inter-rater reliability and predictive validity. Am J Psychiatry. 2002;159:863–5. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- 27.Cornblatt B, Neindam T, Auther A, Smith C, Johnson JT. Validation of two new measures of functional outcome in the schizophrenia prodrome. Schizophr Bull. 2007;33:688–702. doi: 10.1093/schbul/sbm029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Brien MP, Zinberg JL, Cannon TD. Knowledge Regarding the Prodrome Questionnaire. Los Angeles: UCLA; 2004. [Google Scholar]
- 29.Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. J Abnorm Psychol. 1989;98:229–35. doi: 10.1037//0021-843x.98.3.229. [DOI] [PubMed] [Google Scholar]
- 30.Robin A, Foster SL. Negotiating Parent Adolescent Conflict. New York: Guilford Press; 1989. [Google Scholar]
- 31.O'Brien MP, Zinberg JL, Ho L, et al. Family problem solving interactions and 6-month symptomatic and functional outcomes in youth at ultra-high risk for psychosis and with recent onset psychotic symptoms: a longitudinal study. Schizophr Res. 2009;107:198–205. doi: 10.1016/j.schres.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forehand R, Jones DJ. Neighborhood violence and coparent conflict: interactive influence on child psychosocial adjustment. J Abnorm Child Psychol. 2003;31:591–604. doi: 10.1023/a:1026206122470. [DOI] [PubMed] [Google Scholar]
- 33.Gunlicks-Stoessel M, Mufson L, Jekal A, Turner JB. The impact of perceived interpersonal functioning on treatment for adolescent depression IPT-A versus treatment as usual in school-based health clinics. J Consult Clin Psychol. 2010;78:260–7. doi: 10.1037/a0018935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weisman A, Tompson MC, Okazaki S, et al. Clinicians' fidelity to a manual-based family treatment as a predictor of the one-year course of bipolar disorder. Fam Process. 2002;41:123–31. doi: 10.1111/j.1545-5300.2002.40102000123.x. [DOI] [PubMed] [Google Scholar]
- 35.Miklowitz DJ, Axelson DA, Birmaher B, et al. Family-focused treatment for adolescents with bipolar disorder: results of a 2-year randomized trial. Arch Gen Psychiatry. 2008;65:1053–61. doi: 10.1001/archpsyc.65.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miklowitz DJ, O'Brien MP, Schlosser DA, Zinberg JL, DeSilva S, Cannon TD. Clinician's treatment manual for family-focused therapy of adolescents and young adults at risk for psychosis (FFT-PY) University of California at Los Angeles; 2010. [Google Scholar]
- 37.McFarlane WR. Multifamily Groups in the Treatment of Severe Psychiatric Disorders. New York: Guilford Press; 2002. [Google Scholar]
- 38.O'Brien M, Zinberg J, De Silva S, Nichols CM. Adolescent coping skills enhancement group. University of California at Los Angeles; 2007. [Google Scholar]
- 39.O'Brien M, Zinberg J. Psycho-social treatment manual for prodromal youth and their families. University of California at Los Angeles; 2006. [Google Scholar]
- 40.Wynne LC, Singer M, Bartko J, Toohey M. Schizophrenics and their families: recent research on parental communication. In: Tanner JM, editor. Developments in Psychiatric Research. London: Hodder & Stoughton; 1977. pp. 254–86. [Google Scholar]
- 41.Hooley JM, Hiller JB. Family relationships and major mental disorder: risk factors and preventive strategies. In: Sarason BR, Duck S, editors. Personal Relationships: Implications for Clinical and Community Psychology. New York: John Wiley & Sons; 2001. pp. 61–87. [Google Scholar]
- 42.De Silva S, Zinberg JL, O'Brien MP, Schlosser DA, Miklowitz DJ, Cannon TD. Treatment manual for NAPLS enhanced care condition (EC) University of California at Los Angeles; 2010. [Google Scholar]