Abstract
Background
HIV infection occurs in 30% of children with severe acute malnutrition in sub-Saharan Africa. Effects of HIV on the pathophysiology and recovery from malnutrition are poorly understood.
Methods
We conducted a prospective cohort study of 75 severely malnourished Ugandan children. HIV status/CD4 counts were assessed at baseline; auxologic data and blood samples were obtained at admission and after 14 days of inpatient treatment. We utilized metabolomic profiling to characterize effects of HIV infection on metabolic status and subsequent responses to nutritional therapy.
Findings
At admission, patients (mean age 16.3 mo) had growth failure (mean W/H z-score −4.27 in non-edematous patients) that improved with formula feeding (mean increase 1.00). 24% (18/75) were HIV-infected. Nine children died within the first 14 days of hospitalization; mortality was higher for HIV-infected patients (33% v. 5%, OR = 8.83). HIV-infected and HIV-negative children presented with elevated NEFA, ketones, and even-numbered acylcarnitines and reductions in albumin and amino acids. Leptin, adiponectin, insulin, and IGF-1 levels were low while growth hormone, cortisol, and ghrelin levels were high. At baseline, HIV-infected patients had higher triglycerides, ketones, and even-chain acylcarnitines and lower leptin and adiponectin levels than HIV-negative patients. Leptin levels rose in all patients following nutritional intervention, but adiponectin levels remained depressed in HIV-infected children. Baseline hypoleptinemia and hypoadiponectinemia were associated with increased mortality.
Conclusions
Our findings suggest a critical interplay between HIV infection and adipose tissue storage and function in the adaptation to malnutrition. Hypoleptinemia and hypoadiponectinemia may contribute to high mortality rates among malnourished, HIV-infected children.
Introduction
Malnutrition is a major determinant of morbidity and mortality in the developing world and is the underlying cause of 3.5 million child deaths each year [1]. Poor nutrition increases greatly a child's risk of dying from diarrhea, pneumonia, measles, and malaria and is associated with decreased adult height, lower educational achievement, lower socioeconomic status, and a possible increase in chronic diseases during adulthood [2], [3]. Worldwide, malnutrition represents 35% of the burden of disease in children less than five years of age and 11% of disability-adjusted life years (DALYs) [1].
In sub-Saharan Africa, 30% of children with severe acute malnutrition (SAM) are infected with HIV, which increases mortality rates substantially; those with CD4 count <20% are at greatest risk [4], [5]. However, the factors underlying the increased risk of mortality from HIV are poorly understood. Rates of pneumonia (68%), urinary tract infection (26%), and bacteremia (18%) are comparable in severely malnourished HIV-infected and HIV-negative children [6]. Furthermore, among those who survive, the rates of nutritional recovery are similar [7]. There is consequently a critical need to elucidate the pathophysiology of SAM in children with concurrent HIV infection.
In a previous study we used metabolomic profiling to characterize changes in various hormones, growth factors, cytokines, and metabolites during nutritional rehabilitation of severely malnourished Ugandan children [8]. Here we characterized differences in baseline metabolic and hormonal status between HIV-infected and HIV-negative children with SAM and compared their subsequent responses to nutritional therapy. We hypothesized that HIV infection would modify the hormonal and metabolic responses to malnutrition and nutrient therapy and that hormones and metabolites measured at baseline might be associated with mortality in HIV-infected children.
Methods
Study Cohort
The study was conducted at Mwanamugimu Nutrition Unit at Mulago Hospital, in Kampala, Uganda. Children ages six months to five years who met WHO criteria for SAM were eligible for enrollment. SAM was defined as having a weight-for-height z-score (W/H z) <−3, mid-upper arm circumference (MUAC) <11.5 cm, or bilateral pitting edema. Referrals came from the Mulago pediatric acute care unit (emergency department) and community clinics in and around Kampala.
Study Variables
A complete medical and diet history, sociodemographic profile, and physical exam including anthropometric data were obtained at time of enrollment. Lab studies included CBC and differential, blood smear, and CD4/CD8 counts (FACSCalibur, BD Biosciences, USA). HIV status was assessed using an HIV rapid antibody test (Determine, Abbott, USA; STAT-Pak, Chembio Diagnostics, USA; Uni-Gold, Trinity Biotech, Ireland) for patients >18 months of age and HIV DNA PCR (AMPLICOR HIV-1 Monitor Test version 1.5, Roche, USA) for patients <18 months. Children whose mothers had a documented negative HIV test within the previous 30 days were presumed to be HIV negative. Children with known HIV infection did not have repeat HIV testing. Those with malaria were treated with anti-malarials. All patients received counseling from a trained HIV counselor at Mwanamugimu Nutrition Unit before delivering results; HIV-infected patients were referred for appropriate HIV-related care.
Nutritional Interventions
Nutrition rehabilitation and management of medical complications were carried out according to WHO guidelines for inpatient treatment of SAM by medical house officers at Mwanamugimu Nutrition Unit [9]. Inpatient therapy was administered in two phases according to WHO guidelines: an initial stabilization phase during which acute medical conditions were managed; and a longer rehabilitation phase once clinical status improved. Patients were fed F75 mild-based liquid formula (75 kcal and 0.9 g protein/100 mL) during the first phase and F100 (100 kcal and 2.9 g protein/100 mL) during the rehabilitation phase. Micronutrient deficiencies were corrected with vitamin A, folic acid, zinc, and iron. All patients received empiric antibiotics [9]. Patients were followed from time of enrollment until death or discharge from the inpatient unit.
Metabolomic Analysis
Blood samples (maximum 5 mL) were collected at time of enrollment (within 24 h of admission). A second blood sample was collected after 14 days of inpatient treatment or at time of discharge from the inpatient unit, whichever occurred first. Aprotinin (500 KIU/mL of blood; Sigma-Aldrich, USA) was added to prevent protein degradation. Blood samples were collected on ice and processed promptly; EDTA plasma was stored at −70°C and shipped in bulk to the Duke University Stedman Nutrition Center for analysis. Detailed methods of the metabolic and hormonal analyses are described in the Supporting Information (Methods S1).
Statistical Analysis
Sample size was based on commonly reported concentrations and variability of classical hormones (insulin, growth hormone, cortisol) in infants and children. We evaluated pre-treatment anthropometric variables and biomarkers using non-parametric Wilcoxon Rank-Sum and absolute change during treatment using Wilcoxon Signed-Rank based on variables of interest (HIV status, mortality). The association between HIV status and mortality was assessed utilizing an odds ratio. We performed multivariable logistic and linear regression to evaluate associations between biomarkers levels, HIV status, and mortality. Analysis of leptin and total and high molecular weight (HMW) adiponectin excluded patients taking antiretroviral drugs (ARVs), given the known effects of these medications on these hormones [10]–[14]. Edematous children were excluded from analysis of anthropometric variables based on weight. All analyses were conducted using JMP Pro 9.0 (Cary, NC); a two-sided p-value<0.05 was considered statistically significant for all tests.
Ethical considerations
The study protocol was approved by the institutional review boards at Duke University, Makerere University School of Public Health, and the Uganda National Council of Science and Technology. Sponsors of the study assisted with data interpretation but had no role in study design, data collection, or data analysis.
Written informed consent (in English and Luganda) to participate in the study and all its components was obtained from all guardians. Each patient received an insecticide-treated bed net at enrollment and transportation money to return home at the time of discharge as compensation for participation.
Results
Study Population
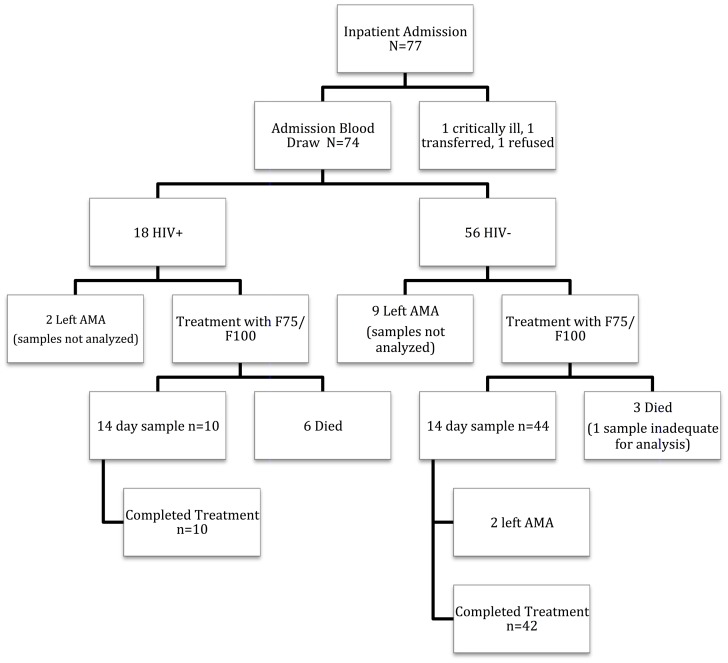
A total of 77 patients were referred to Mwanamugimu Inpatient Nutrition Unit and screened for study enrollment between December 2010 and March 2011. One patient refused to participate, another was deemed clinically unstable by the medical house officer for extra blood draws, and a third was transferred from the ward after only HIV status was assessed. Therefore, 75 patients had known HIV status and 74 had complete admission anthropometry. Analyses of hormones, metabolites, and cytokines were performed on blood samples from 62 patients at admission (16 HIV-infected including three on ARVs and 46 HIV-negative); 54 of these patients had repeat samples analyzed after 14 days of hospitalization and eight patients died before the second sample was obtained. Initial samples were insufficient in one additional patient (who died) and were not analyzed in 11 patients who left the ward prior to completing at least 14 days of treatment (including two HIV-infected patients, one of whom was on ARVs) ( Figure 1 ).
Figure 1. Flowchart of Patient Outcomes.
The patient population was 57.3% male; mean age was 16.3±1.0 months (mean±SE). 56.8% (42/74) presented with edematous malnutrition. Non-edematous children had an initial W/H z-score −4.27±0.24 and MUAC 9.8±0.2 cm. Mean length-for-age (L/A) z-score was −2.97±0.18; head circumference-for-age (HC/A) z-score was −1.15±0.18. 9.5% (7/74) had malaria; one HIV-infected patient had concurrent malaria ( Table 1 ).
Table 1. Baseline Anthropometric and Hematologic Characteristics of HIV-infected and HIV-negative Patients.
| HIV-infected (n = 18) | HIV-negative (n = 56) | ||
| Number (%) | p-value | ||
| Male Sex | 10/18 (55.6) | 32/56 (57.1) | 1.00 |
| Edema Present | 9/18 (50) | 33/56 (58.9) | 0.589 |
| Positive Malaria Smear | 1/18 (5.6) | 6/56 (10.7)) | 0.555 |
| Newly Diagnosed HIV infection | 12/18 (66.7) | - | - |
| Current ARV treatment | 4/6 (66.7) | - | - |
| Mortality | 6/18 (33.3) | 3/56 (5.4) | 0.0051 |
| Mean±SEM | |||
| Age | 19.2±2.6 | 15.4±1.1 | 0.315 |
| Days in Treatment | 26.4±3.9 | 24.9±1.5 | 0.850 |
| Admission Anthropometry | |||
| W/H % (nonedematous) | 70.5±2.4 | 71.3±1.4 | 0.571 |
| W/H Z-Score (nonedematous) | −4.44±0.48 | −4.20±0.28 | 0.615 |
| W/A Z-Score (nonedematous) | −5.14±0.61 | −4.87±0.33 | 0.870 |
| MUAC (nonedematous) | 9.6±0.5 | 9.9±0.2 | 0.599 |
| L/A Z-score (all patients) | −3.17±0.40 | −2.90±0.20 | 0.492 |
| H/C Z-score (all patients) | −0.72±0.32 | −1.25±0.21 | 0.246 |
| Hematology | |||
| Abs CD4 Count | 644±103 | 2734±253 | <0.0001 |
| CD4% | 14.6±2.1 | 34.8±1.2 | <0.0001 |
| Abs CD8 Count | 1724±387 | 1610±120 | 0.638 |
| CD8% | 37.3±2.6 | 21.3±1.0 | <0.0001 |
| CD4/CD8 Ratio | 0.44±0.08 | 1.83±0.10 | <0.0001 |
| WBC (103/µl) | 8.5±1.2 | 13.2±1.0 | 0.0082 |
| Hemoglobin (g/dL) | 7.7±0.4 | 9.0±0.2 | 0.0130 |
| Platelets (103/µl) | 267±37 | 371±24 | 0.0231 |
As previously reported, overall mortality was 12.2% (9/74). Of those who successfully completed inpatient nutritional rehabilitation, mean length of stay was 25.2 days. During hospitalization, mean W/H z-score increased 1.00±0.18 in non-edematous children. Among surviving patients, 80% (52/65) were followed until discharge and 20% (13/65) left the ward against medical advice before achieving nutritional stability.
Baseline Characteristics of HIV-infected and HIV-negative Patients
HIV prevalence in the study population was 24% (18/75); two-thirds (12/18) of these were newly diagnosed HIV infections. Four of the six previously diagnosed patients were being treated with ARVs upon admission ( Table 1 ).
Similar proportions of HIV-infected and HIV-negative patients presented with edematous malnutrition (p = 0.589). Non-edematous HIV-infected and HIV-negative patients presented with similar degrees of wasting (W/H z-score −4.44 vs. −4.20, p = 0.615). HIV-infected children had lower absolute CD4 counts (644 vs. 2734, p<0.0001), WBC counts, hemoglobin, and platelets ( Table 1 ).
HIV-infected patients had increased mortality rates: 33.3% for seropositive children compared with 5.4% for seronegative children (OR = 8.83, CI 1.93–40.43, p = 0.0051). Among those who survived, there were similar improvements in W/H z in (non-edematous) HIV-infected and HIV-negative patients after 14 days (0.85 vs. 0.43, p = 0.412).
Effects of HIV Infection on Baseline Metabolic Profile
Both HIV-infected and HIV-negative patients presented in a severe catabolic state with exaggerated lipolysis, fatty acid oxidation, and hypoaminoacidemia ( Table 2 and 3 ). Non-esterified fatty acids (NEFA), ketones, C2 acyl (acetyl)carnitine, and even-chained acylcarnitine molar sum were elevated in both groups at presentation, though ketones (p = 0.039), acetylcarnitine (p = 0.0103), and even-chained acylcarnitine molar sum (p = 0.0108) were higher in HIV-infected patients. Levels of albumin, amino acids, and C3 acyl (propionyl)carnitine, a byproduct of branched chain amino acid catabolism, were comparably low in both groups. Yet blood glucose levels were maintained in the normal range. Triglycerides were higher in HIV-infected patients (p<0.001). Moreover, a number of inflammatory markers, including CRP, IL-2, IL-6, IL-8, and TNF-α were higher in HIV-infected patients, with IL-2 (p = 0.016) and TNF-α (p = 0.025) reaching statistical significance ( Table 2 ). Edematous patients had higher alanine amino transferase (ALT) and gamma glutamyl transpeptidase (GGT) levels and lower albumin and amino acid levels than non-edematous patients (data not shown); these metrics did not differ among the HIV-infected and HIV-negative groups. Edematous patients also had lower total and HMW adiponectin levels; however, edema did not modify the association between HIV status and hypoadiponectinemia.
Table 2. Baseline Metabolic Profile of HIV-infected and HIV-negative Patients.
| HIV-infected (n = 16) | HIV-negative (n = 46) | ||
| Mean±SEM | p-value | ||
| Fatty Acid Metabolites | |||
| NEFA (mmol/L) | 0.65±0.10 | 0.54±0.06 | 0.285 |
| Total Ketones (µmol/L) | 826±259 | 424±95 | 0.0387 |
| Acylcarnitines | |||
| C2 (µmol/L) | 22.3±3.5 | 14.4±2.4 | 0.0103 |
| C3 (µmol/L) | 0.47±0.07 | 0.38±0.04 | 0.179 |
| C2/C3 Ratio | 54.3±9.7 | 44.7±5.7 | 0.195 |
| Even-Chain Acylcarnitine Molar Sum (µmol/L) | 24.0±3.7 | 16.0±2.6 | 0.0108 |
| Hormones | |||
| Insulin (µIU/ml) | 1.81±0.48 | 2.45±0.45 | 0.321 |
| Growth Hormone (ng/ml) | 12.4±2.7 | 11.0±1.3 | 0.380 |
| IGF-1 (ng/ml) | 13.3±4.4 | 9.4±1.7 | 0.597 |
| Total Ghrelin (pg/ml) | 3577±566 | 4040±320 | 0.435 |
| GLP-1 (pg/ml) | 128.8±21.3 | 96.0±12.8 | 0.106 |
| PYY (pg/ml) | 1195±160 | 1202±105 | 0.866 |
| Cortisol (µg/dl) | 54.0±3.2 | 46.0±2.7 | 0.106 |
| Adipocytokines * | n = 13 | n = 46 | |
| Leptin (pg/ml) | 69.8±26.6 | 292±52 | 0.0163 |
| Total Adiponectin (ng/ml) | 8049±1081 | 15268±1133 | 0.0017 |
| HMW Adiponectin (ng/ml) | 4409±757 | 9356±761 | 0.0014 |
| Amino Acids | |||
| Amino Acid Molar Sum (µmol/L) | 1230±62 | 1190±51 | 0.417 |
| Inflammatory Cytokines | |||
| IL-2 (pg/ml) | 7.7±2.7 | 3.6±1.2 | 0.0158 |
| IL-6 (pg/ml) | 96.3±58.4 | 25.6±15.9 | 0.139 |
| IL-8 (pg/ml) | 299.3±191.0 | 75.2±25.9 | 0.060 |
| TNF-α (pg/ml) | 43.0±5.5 | 37.4±9.5 | 0.0248 |
| Other | |||
| Glucose (mg/dl) | 77.1±7.9 | 85.9±3.9 | 0.474 |
| Creatinine (mg/dl) | 0.30±0.04 | 0.27±0.03 | 0.296 |
| Phosphorus (mg/dl) | 2.99±1.40 | 3.28±1.02 | 0.390 |
| Albumin (g/dl) | 2.0±0.2 | 2.0±0.1 | 0.847 |
| CRP (mg/L) | 63.7±16.5 | 26.8±5.3 | 0.0730 |
| Triglycerides (mg/dl) | 177.6±14.0 | 122.9±12.2 | 0.0008 |
*Excludes patients on ARVs.
Table 3. Baseline Amino Acid Levels of HIV-infected and HIV-negative patients.
| HIV-infected (n = 16) | HIV-negative (n = 46) | ||
| Mean±SEM | p-value | ||
| Glycine (µmol/L) | 235±21.4 | 237±12.6 | 0.866 |
| Alanine | 153±27.4 | 217±16.2 | 0.0330 |
| Serine | 99.2±99.5 | 113±5.6 | 0.464 |
| Proline | 152±14.4 | 153±8.5 | 0.904 |
| Valine | 100±10.7 | 75.6±6.3 | 0.0248 |
| Leucine/Isoleucine | 82.0±8.9 | 70.5±5.2 | 0.237 |
| Methionine | 16.1±1.7 | 15.6±1.0 | 0.742 |
| Histidine | 69.1±7.0 | 53.3±4.1 | 0.250 |
| Phenylalanine | 79.6±7.7 | 43.0±4.5 | 0.0067 |
| Tyrosine | 30.1±4.6 | 22.6±2.7 | 0.207 |
| Aspartate | 39.2±4.8 | 36.5±2.8 | 0.853 |
| Glutamate | 111±10.5 | 91.3±6.2 | 0.435 |
| Ornithine | 27.4±3.5 | 26.2±2.1 | 0.381 |
| Citrulline | 8.9±1.2 | 8.2±0.7 | 0.421 |
| Arginine | 28.3±3.3 | 27.7±1.9 | 0.323 |
Insulin and IGF-1 levels were low in both HIV-infected and HIV-negative subjects, while growth hormone (GH), ghrelin, cortisol, GLP-1, and peptide YY (PYY) were high (compare levels to those in references [15]–[18]). Excluding analysis of three patients taking ARVs, which are known to affect adipose tissue function, the levels of leptin (p = 0.016), total adiponectin (p = 0.0017), and high molecular weight (HMW) adiponectin (p = 0.0014) were significantly lower in HIV-infected than in HIV-negative subjects ( Table 2 ). Multivariate logistic regression controlling for the degree of wasting (as assessed by W/H z-score) established that HIV infection was associated with lower total adiponectin (p = 0.0113) and HMW adiponectin (p = 0.009), but not lower leptin (p = 0.157) ( Table 4 ).
Table 4. Multivariate regression assessing the effect of HIV status on leptin, total adiponectin, and HMW adiponectin when controlling for admission W/H z-score.
| Beta (HIV status) | p-value | Adjusted R2 | |
| Leptin | 63.7±44.4 | 0.1573 | 0.294 |
| Total Adiponectin | 2752±1051 | 0.0113 | 0.274 |
| HMW Adiponectin | 1949±720 | 0.0090 | 0.253 |
Effects of HIV Infection on Metabolic Response to Nutritional Rehabilitation
54 patients had blood samples drawn both at admission and after 14 days of treatment. We were unable to obtain day-14 samples in any of the patients who died.
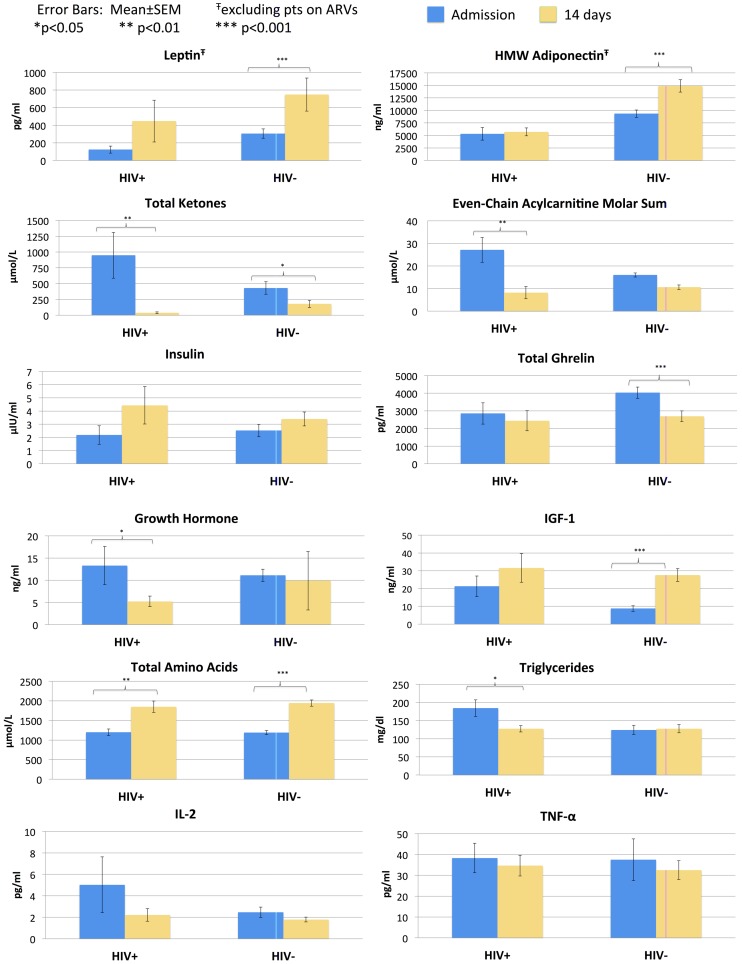
HIV-infected and HIV-negative patients demonstrated similar trends in most metabolites, hormones, and cytokines in response to nutritional treatment. NEFA, total ketones, and even-chained acylcarnitines decreased ( Figure 2 and Table 5 ), while albumin and the majority of amino acids increased ( Table 6 ). There was a rise in the levels of propionylcarnitine (HIV-infected: 0.50 vs. 0.65, p = 0.2754; HIV-negative 0.36 vs. 0.67, p<0.0001), likely reflecting the catabolism of (newly available) dietary branched chain amino acids [19]. Plasma insulin, IGF-1, and leptin increased while plasma ghrelin, GH, and cortisol declined. The majority of inflammatory markers decreased in both groups (statistically significant for IL-6 and CRP). After 14 days of nutritional therapy, there were no significant differences among surviving HIV-infected and HIV-negative patients with respect to NEFA, total ketones, insulin, IGF-1, leptin, ghrelin, GH, cortisol, GLP-1, PYY, IL2, IL6, IL8, or TNF-α levels ( Figure 2 and Table 5 ).
Figure 2. Comparison of metabolic response to inpatient rehabilitation in 54 patients who completed treatment (10 HIV-infected and 44 HIV-negative children).
Analysis of leptin and HMW adiponectin excluded those patients taking ARVs. Data are represented as the mean±SEM.
Table 5. Changes in Metabolic Profiles of HIV-infected (surviving) and HIV-negative patients.
| HIV-infected (n = 10) | HIV-negative (n = 44) | |||||
| Mean±SEM | p-value | Mean±SEM | p-value | |||
| Admission | 14-day | Admission | 14-day | |||
| Fatty Acid Metabolites | ||||||
| NEFA (mmol/L) | 0.72±0.16 | 0.24±0.06 | 0.0020 | 0.53±0.06 | 0.36±0.037 | 0.0723 |
| Total Ketones (µmol/L) | 948±362 | 39±14 | 0.0098 | 431±99 | 179±56 | 0.0256 |
| Acylcarnitines | ||||||
| C2 (µmol/L) | 25.2±5.2 | 7.2±0.8 | 0.0098 | 14.5±2.6 | 9.3±0.94 | 0.171 |
| C3 (µmol/L) | 0.50±0.11 | 0.65±0.11 | 0.275 | 0.36±0.03 | 0.67±0.06 | <0.0001 |
| C2/C3 Ratio | 60.6±14.7 | 13.4±2.0 | 0.0020 | 45.7±5.9 | 22.5±4.5 | <0.0001 |
| Even-Chain Acylcarnitine Molar Sum (µmol/L) | 27.1±5.5 | 8.2±0.9 | 0.0098 | 16±2.7 | 10.6±1 | 0.216 |
| Hormones | ||||||
| Insulin (µIU/ml) | 2.18±0.70 | 4.43±1.42 | 0.084 | 2.52±0.47 | 3.4±0.53 | 0.108 |
| Growth Hormone (ng/ml | 13.3±4.3 | 5.2±1.2 | 0.027 | 11.2±1.4 | 10.1±1.7 | 0.147 |
| IGF-1 (ng/ml) | 21.3±5.8 | 31.6±8.1 | 0.250 | 8.8±1.6 | 27.6±3.6 | <0.0001 |
| Total Ghrelin (pg/ml) | 2851±603 | 2439±570 | 0.084 | 4029±319 | 2692±303 | <0.0001 |
| GLP-1 (pg/ml) | 116.7±27.5 | 86.0±22.1 | 0.375 | 93.6±13.0 | 88.8±12.4 | 0.863 |
| PYY (pg/ml) | 916±118 | 893±112 | 1.0 | 1144±101 | 1011±78 | 0.100 |
| Cortisol (µg/dl) | 56.6±3.4 | 41.1±6.7 | 0.0625 | 45.3±2.8 | 38.3±3 | 0.0123 |
| Adipocytokines * | n = 7 | n = 44 | ||||
| Leptin (pg/ml) | 123.1±39.7 | 446±238 | 0.128 | 305±53.5 | 748.8±188 | 0.0011 |
| Total Adiponectin (ng/ml) | 8383±1569 | 10154±1815 | 0.297 | 15115±1093 | 20792±1329 | <0.0001 |
| HMW Adiponectin (ng/ml) | 5308±1259 | 5717±795 | 0.625 | 9350±748 | 14895±1245 | <0.0001 |
| Amino Acids | ||||||
| Amino Acid Molar Sum (µmol/L) | 1198±84.4 | 1850±145 | 0.005 | 1192±53.6 | 1944±80.5 | <0.0001 |
| Inflammatory Cytokines | ||||||
| IL-2 (pg/ml) | 5.0±2.6 | 2.2±0.6 | 0.477 | 2.5±0.5 | 1.8±0.2 | 0.255 |
| IL-6 (pg/ml) | 49±32 | 3.4±0.7 | 0.0371 | 9.9±1.5 | 7.8±2.8 | 0.0256 |
| IL-8 (pg/ml) | 344±300 | 29.7±3.4 | 0.0645 | 50.6±9.0 | 41.7±4.4 | 0.638 |
| TNF-α (pg/ml) | 38.3±7.1 | 34.7±5 | 0.922 | 37.5±10 | 32.5±4.5 | 1.0 |
| Other | ||||||
| Glucose (mg/dl) | 72.1±9.3 | 75.4±3.7 | 0.625 | 84.2±3.8 | 77.0±2.2 | 0.0634 |
| Creatinine (mg/dl) | 0.32±0.06 | 0.36±0.11 | 0.910 | 0.25±0.03 | 0.32±0.07 | 0.694 |
| Phosphorus (mg/dl) | 3.2±0.4 | 4.2±0.2 | 0.086 | 3.4±0.2 | 4.6±0.1 | <0.0001 |
| Albumin (g/dl) | 2.03±0.32 | 2.28±0.20 | 0.219 | 2.01±0.17 | 2.51±0.12 | <0.0001 |
| CRP (mg/L) | 70.7±21.1 | 14.2±7.2 | 0.0391 | 26.8±5.7 | 9.9±4.1 | 0.0003 |
| Triglycerides (mg/dl) | 184±22.8 | 127±8.7 | 0.0391 | 124.3±12.7 | 127.7±11.2 | 0.416 |
*Excludes patients on ARVs.
Table 6. Changes in Amino Acid Levels of HIV-infected (surviving) and HIV-negative patients.
| HIV-infected (n = 10) | HIV-negative (n = 44) | |||||
| Mean±SEM | p-value | Mean±SEM | p-value | |||
| Admission | 14-day | Admission | 14-day | |||
| Glycine (µmol/L) | 216±16.6 | 313±28.1 | 0.0020 | 238±13.7 | 305±13.4 | <0.0001 |
| Alanine | 150±18.1 | 409±57.7 | 0.0020 | 218±18.6 | 418±27.5 | <0.0001 |
| Serine | 98.8±4.5 | 125±14.6 | 0.0371 | 113±6.4 | 157±6.9 | <0.0001 |
| Proline | 155±14.5 | 296±42.6 | 0.0098 | 152±9.4 | 282±20.3 | <0.0001 |
| Valine | 102±15.8 | 130±21.3 | 0.375 | 76.8±6.2 | 152±10.2 | <0.0001 |
| Leucine/Isoleucine | 80.1±15.0 | 112±15.2 | 0.106 | 71.0±5.2 | 132±7.3 | <0.0001 |
| Methionine | 16.8±2.8 | 19.7±3.3 | 0.193 | 15.6±1.0 | 24.5±1.6 | <0.0001 |
| Histidine | 64.5±12.7 | 53.9±5.7 | 0.432 | 52.8±3.4 | 50.7±2.7 | 0.954 |
| Phenylalanine | 78.4±18.2 | 59.8±5.3 | 0.432 | 43.3±2.8 | 53.0±2.5 | 0.0184 |
| Tyrosine | 29.8±7.2 | 45.8±10.6 | 0.0840 | 22.6±2.7 | 52.1±5.0 | <0.0001 |
| Aspartate | 31.3±6.3 | 50.4±10.5 | 0.0039 | 35.4±2.7 | 51.0±5.0 | <0.0001 |
| Glutamate | 109±12.7 | 135±17.3 | 0.275 | 91.3±4.7 | 152±8.2 | <0.0001 |
| Ornithine | 29.3±3.1 | 40.2±6.8 | 0.0195 | 26.7±2.3 | 47.9±3.3 | <0.0001 |
| Citrulline | 8.9±1.1 | 16.3±3.4 | 0.0098 | 8.3±0.7 | 19.0±1.6 | <0.0001 |
| Arginine | 29.2±2.4 | 44.5±6.9 | 0.0137 | 27.8±2.2 | 49.7±3.3 | <0.0001 |
However, HIV status was associated with differential effects on adiponectin levels during nutritional recovery. Excluding patients on ARVs, HIV-infected patients had no significant changes in total (8383 vs. 10154, p = 0.2969) or HMW adiponectin (5308 vs. 5717, p = 0.625). In contrast, HIV-negative patients had marked increases in total (15115 vs. 20792, p<0.0001) and HMW adiponectin (9350 vs. 14895, p<0.0001) during recovery. Furthermore, after 14 days of treatment, HIV-infected patients still had significantly lower levels of total (p = 0.0023) and HMW adiponectin (p = 0.0019) than HIV-negative patients ( Figure 2 and Table 5 ).
Predictors of Mortality During Inpatient Treatment
Non-edematous patients who died had more striking manifestations of wasting than those who survived, as reflected in lower W/H z-score (−6.28 vs. −3.98, p = 0.0244) and MUAC (7.8 vs. 10.1, p = 0.0019). In all patients, there was a greater degree of stunting in those who died (L/A z-score −4.03 vs. −2.82, p = 0.0454) ( Table 7 ).
Table 7. Baseline Characteristics and Metabolic Profiles associated with Mortality.
| Died (n = 8) | Survived (n = 54) | ||
| Mean±SEM | p-value | ||
| Anthropometry (nonedematous) | |||
| Admission W/H % | 61.1±4.6 | 72.5±1.0 | 0.0121 |
| Admission W/H Z-Score | −6.28±1.05 | −3.98±0.19 | 0.0244 |
| Admission W/A Z-Score | −7.01±0.86 | −4.63±0.26 | 0.0221 |
| Admission MUAC | 7.8±0.3 | 10.1±0.2 | 0.0019 |
| L/A z-score (all patients) | −4.03±0.58 | −2.82±0.18 | 0.0454 |
| Fatty Acid Metabolites | |||
| NEFA (mmol/L) | 0.57±0.15 | 0.56±0.06 | 0.557 |
| Total Ketones (µmol/L) | 539±276 | 526±106 | 0.456 |
| Acylcarnitines | |||
| C2 (µmol/L) | 16.3±2.2 | 16.5±2.3 | 0.139 |
| C3 (µmol/L) | 0.51±0.09 | 0.38±0.03 | 0.128 |
| C2/C3 Ratio | 38.5±7.7 | 48.4±5.5 | 0.858 |
| Even-Chain Acylcarnitine Molar Sum (µmol/L) | 17.9±2.2 | 18.1±2.5 | 0.139 |
| Hormones | |||
| Insulin (µIU/ml) | 1.10±0.97 | 2.46±0.38 | 0.182 |
| Growth Hormone (ng/ml) | 10.5±3.4 | 11.5±1.3 | 0.442 |
| IGF-1 (ng/ml) | 5.6±4.8 | 11.1±1.8 | 0.118 |
| Total Ghrelin (pg/ml) | 4660±771 | 3811±297 | 0.361 |
| GLP-1 (pg/ml) | 149.1±30.3 | 97.9±11.7 | 0.080 |
| PYY (pg/ml) | 1866±227 | 1101±87 | 0.0089 |
| Cortisol (µg/dl) | 52.2±6.2 | 47.4±2.4 | 0.484 |
| Adipocytokines * | n = 8 | n = 51 | |
| Leptin (pg/ml) | 7.1±4.4 | 280±47 | 0.0002 |
| Total Adiponectin (ng/ml) | 10403±3360 | 14191±1017 | 0.075 |
| HMW Adiponectin (ng/ml) | 4894±1922 | 8795±693 | 0.0184 |
| Amino Acids | |||
| Amino Acid Molar Sum (µmol/L) | 1248±70 | 1193±46 | 0.319 |
| Inflammatory Cytokines | |||
| IL-2 (pg/ml) | 16.2±2.8 | 2.9±1.1 | 0.0004 |
| IL-6 (pg/ml) | 223.6±47.9 | 17.2±18.4 | 0.166 |
| IL-8 (pg/ml) | 323±147 | 105±57 | 0.0042 |
| TNF-α (pg/ml) | 46.8±20.2 | 37.6±7.8 | 0.0203 |
*Excludes patients on ARVs.
In addition to HIV infection, factors at baseline associated with subsequent mortality were hypoleptinemia (p = 0.0002), low levels of HMW adiponectin (p = 0.0149), and high levels of PYY (p = 0.0087), IL2 (p = 0.0004), IL6 (p = 0.004), and TNF-α (p = 0.0203) ( Table 7 ) [8]. Multivariate logistic regression analysis controlling for HIV status and admission W/H z showed that hypoleptinemia at baseline remained a significant predictor of mortality (OR 0.906, CI 0.827–0.993, p = 0.035) while HMW adiponectin at baseline became insignificant. Mortality did not vary with other baseline measures including presence of edema, hemoglobin, glucose, creatinine, albumin, phosphorus, other hormones and growth factors, fatty acid metabolites, or amino acid or cytokine levels.
Discussion
Malnutrition remains a major cause of morbidity and mortality, with the greatest impact in low-income countries. HIV infection is detected in 30% of children with SAM and is associated with greatly increased mortality rates [4]. The role of HIV in the pathophysiology of malnutrition is poorly understood. Here we characterized differences in baseline metabolic and hormonal status between HIV-infected and HIV-negative children with SAM and compared their subsequent responses to current WHO recommended nutritional therapy. A major finding of this study is that HIV-infected children with SAM present with significant reductions in the adipocytokines leptin and adiponectin that are associated with mortality during inpatient hospitalization.
In our study the prevalence of HIV infection was 24%, with two-thirds of these representing new diagnoses. Mortality in HIV-infected children was very high (33.3%), similar to results from a previous meta-analysis [4]. HIV-infected and HIV-negative patients presented with similar degrees of wasting and edema, and among those who survived, achieved similar rates of growth and recovery. A previous study found HIV-infected patients to be more wasted at baseline; nevertheless that study, like ours, noted that seropositive and seronegative patients achieve similar rates of catch-up growth during nutritional treatment and that increased wasting at presentation is associated with mortality [7].
Both HIV-infected and HIV-negative children presented in a severe catabolic state characterized by elevated NEFA, total ketones, and even-numbered acylcarnitines (derived from fatty acid oxidation) and striking reductions in serum albumin and amino acids. At the same time, blood glucose levels were maintained in the normal range. Leptin, adiponectin, insulin, and IGF-1 levels were low while growth hormone, cortisol, and ghrelin levels were high. [8] This profile suggests a state in which fat catabolism and glucose production are prioritized above energy storage and growth [8], [20]–[25]. At baseline, serum triglycerides, ketones, and even-chain acylcarnitines were higher and leptin and HMW adiponectin lower in HIV-infected patients than in HIV-negative patients. When controlling for W/H z-score, lower HMW adiponectin levels remained significantly associated with HIV infection, though leptin levels did not.
Nutritional treatment reversed the state of lipid mobilization and fatty acid oxidation and increased the levels of amino acids and C3 acyl (propionyl)carnitine. Insulin and IGF-1 rose while GH, cortisol, and ghrelin declined. HIV status did not modify the effect of treatment on most metabolites, hormones, growth factors, and cytokines. However, nutritional intervention increased HMW and total adiponectin levels in HIV-negative patients but not in HIV-infected patients; their levels remained significantly lower despite high calorie feeds. Leptin, on the other hand, increased in both HIV-infected and HIV-negative subjects.
Previous studies have linked decreased levels of leptin and adiponectin to HIV infection, particularly in the context of HIV-associated lipodystrophy, a syndrome characterized by fat redistribution, dyslipidemia, and metabolic syndrome. Many investigations implicate ARVs in the development of this syndrome, citing medication-induced adipose dysregulation and mitochondrial toxicity as potential mechanisms [10]–[14]. Additional studies, however, in untreated adults and mice have shown that HIV infection itself may be associated with adipose tissue dysfunction and decreased levels of adiponectin and leptin [26]–[28].
Adiponectin is produced by mature adipocytes; over-expression of adiponectin increases hepatic insulin sensitivity, while low levels of adiponectin are associated with insulin resistance and the metabolic syndrome [29]. Circulating leptin levels rise in proportion to white adipose tissue mass; higher levels are associated with obesity and lower levels with fasting and malnutrition [22]. The severe hypoadiponectinemia and hypoleptinemia in our HIV-infected children suggest a state of insulin resistance associated with depletion of white adipose tissue reserves.
The pre-existing mass and function of white adipose tissue appear to play roles in the adaptation to, and recovery from, malnutrition because low levels of leptin and adiponectin at baseline were associated with subsequent mortality. Indeed, baseline hypoleptinemia remained a strong predictor of mortality when controlling for HIV infection and W/H z-score in a multivariate analysis. While these findings do not prove that mortality is caused by hypoadiponectinemia and/or hypoleptinemia, there are potential mechanisms by which hypoadiponectinemia and hypoleptinemia might contribute to mortality risk. For example, a lack of pre-existing adipose tissue stores, suggested by hypoleptinemia at presentation, may limit a child's ability to sustain energy production for critical cardiorespiratory function during the initial phases of acute severe malnutrition. Moreover, leptin and adiponectin have immunoregulatory properties that may modulate the response to infectious pathogens. Leptin activates NK cells, induces neutrophil chemotaxis, enhances secretion of pro-inflammatory cytokines, and induces activation and proliferation of T-cells, while adiponectin promotes production of numerous anti-inflammatory cytokines [30], [31]. It is possible that the combined effects of HIV infection and malnutrition on adipose tissue and immune function may increase mortality risk.
There were several limitations to our study. Blood samples were not obtained after fasting, as this could not be justified in critically ill patients. Our small sample size prevented us from conducting potentially important analyses of subgroups including HIV-infected patients who died (n = 6) and those already taking ARVs. Additionally, 17.6% (n = 13) of the original patient population left the ward prior to completing nutritional rehabilitation.
Nevertheless, this study provides a comprehensive analysis of the effects of HIV on the pathophysiology and recovery from SAM in childhood. Our findings suggest a critical interplay between HIV infection and adipose tissue storage and function in the adaptation to malnutrition.
Mortality in malnutrition is predicted by low W/H z and low MUAC. However, these can be difficult or impossible to interpret in infants and children with nutritional edema. Currently, all patients with nutritional edema are categorized as having SAM and treated accordingly. Our finding that hypoleptinemia predicts mortality in edematous as well as non-edematous subjects suggests that leptin assays might in the future be used to identify and target malnourished children at highest risk of death [8].
Finally, it should be noted that the optimal timing for initiating ARV treatment in HIV-infected children with SAM is currently unknown. In some cases, early initiation of therapy may increase the risk of clinical deterioration; in clinically stable children, however, it appears to improve outcomes [12], [32]–[35]. Future studies should determine if the effects of ARVs on adipose tissue metabolism and function influence the clinical response to treatment of severely malnourished children.
Supporting Information
Detailed methods on the assays used for the metabolic and hormonal analyses.
(DOC)
Acknowledgments
The authors gratefully acknowledge the hard work and dedication of the staff of Mwanamugimu Nutrition Unit, particularly Esther, Jane Buyonjo, Justine Nalwadda, and Vicki Nabunnya for their help in completing this study. The authors also thank the staff of the Mulago University–Johns Hopkins University (MU-JHU) Core Lab at the Infectious Disease Institute (IDI).
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. Data are available within the Supporting Information files.
Funding Statement
This work was supported by grants from the Genentech Foundation, PepsiCo, Inc., and the Duke Global Health Institute (to SB, MF, and AM). John A. Bartlett is supported by US National Institutes of Health awards P30AI64518, U01AI067854, D43CA153722, and D43TW06732, and HRSA award T84HA21123. Christopher Newgard and the Stedman Metabolomics Center are supported by NIH grant DK58398. The funders had no role in study design, data collection, decision to publish, or preparation of the manuscript. Dr. St. Peter, who is employed by PepsiCo, Inc., assisted with data analysis and approved the final manuscript as submitted.
References
- 1. Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, et al. (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371: 243–260. [DOI] [PubMed] [Google Scholar]
- 2. Caulfield LE, de Onis M, Blossner M, Black RE (2004) Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr 80: 193–198. [DOI] [PubMed] [Google Scholar]
- 3. Victora CG, Adair L, Fall C, Hallal PC, Martorell R, et al. (2008) Maternal and child undernutrition: consequences for adult health and human capital. Lancet 371: 340–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fergusson P, Tomkins A (2009) HIV prevalence and mortality among children undergoing treatment for severe acute malnutrition in sub-Saharan Africa: a systematic review and meta-analysis. Transactions of the Royal Society of Tropical Medicine and Hygiene 103: 541–548. [DOI] [PubMed] [Google Scholar]
- 5. Chinkhumba J, Tomkins A, Banda T, Mkangama C, Fergusson P (2008) The impact of HIV on mortality during in-patient rehabilitation of severely malnourished children in Malawi. Transactions of the Royal Society of Tropical Medicine and Hygiene 102: 639–644. [DOI] [PubMed] [Google Scholar]
- 6. Bachou H, Tylleskar T, Downing R, Tumwine JK (2006) Severe malnutrition with and without HIV-1 infection in hospitalised children in Kampala, Uganda: differences in clinical features, haematological findings and CD4+ cell counts. Nutrition journal 5: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fergusson P, Chinkhumba J, Grijalva-Eternod C, Banda T, Mkangama C, et al. (2009) Nutritional recovery in HIV-infected and HIV-uninfected children with severe acute malnutrition. Archives of disease in childhood 94: 512–516. [DOI] [PubMed] [Google Scholar]
- 8.Bartz S, Mody A, Hornik C, Bain J, Muehlbauer M, et al.. (2014) Severe acute malnutrition in childhood: hormonal and metabolic status at presentation, response to treatment, and predictors of mortality. J Clin Endocrinol Metab: Epub Feb 27 2014. [DOI] [PMC free article] [PubMed]
- 9.Ashworth A, Khanum S, Jackson A, Schofield C (2003) Guidelines for the inpatient treatment of severely malnourisehd children. Geneva: World Health Organization.
- 10. Verkauskiene R, Dollfus C, Levine M, Faye A, Deghmoun S, et al. (2006) Serum adiponectin and leptin concentrations in HIV-infected children with fat redistribution syndrome. Pediatr Res 60: 225–230. [DOI] [PubMed] [Google Scholar]
- 11. Hammond E, McKinnon E, Nolan D (2010) Human immunodeficiency virus treatment-induced adipose tissue pathology and lipoatrophy: prevalence and metabolic consequences. Clin Infect Dis 51: 591–599. [DOI] [PubMed] [Google Scholar]
- 12. Musoke PM, Fergusson P (2011) Severe malnutrition and metabolic complications of HIV-infected children in the antiretroviral era: clinical care and management in resource-limited settings. Am J Clin Nutr 94: 1716S–1720S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sweeney LL, Brennan AM, Mantzoros CS (2007) The role of adipokines in relation to HIV lipodystrophy. AIDS 21: 895–904. [DOI] [PubMed] [Google Scholar]
- 14. Tsiodras S, Mantzoros C (2006) Leptin and Adiponectin in the HIV Associated Metabolic Syndrome: Physiologic and Therapeutic Implications. Am J Infect Dis 2: 141–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Feigerlova E, Diene G, Conte-Auriol F, Molinas C, Gennero I, et al. (2008) Hyperghrelinemia precedes obesity in Prader-Willi syndrome. J Clin Endocrinol Metab 93: 2800–2805. [DOI] [PubMed] [Google Scholar]
- 16. Higgins PB, Fernandez JR, Garvey WT, Granger WM, Gower BA (2008) Entero-insular axis and postprandial insulin differences in African American and European American children. Am J Clin Nutr 88: 1277–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lomenick JP, Melguizo MS, Mitchell SL, Summar ML, Anderson JW (2009) Effects of meals high in carbohydrate, protein, and fat on ghrelin and peptide YY secretion in prepubertal children. J Clin Endocrinol Metab 94: 4463–4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lomenick JP, Clasey JL, Anderson JW (2008) Meal-related changes in ghrelin, peptide YY, and appetite in normal weight and overweight children. Obesity (Silver Spring) 16: 547–552. [DOI] [PubMed] [Google Scholar]
- 19. Batch BC, Shah SH, Newgard CB, Turer CB, Haynes C, et al. (2013) Branched chain amino acids are novel biomarkers for discrimination of metabolic wellness. Metabolism 62: 961–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Warren MP (2011) Endocrine manifestations of eating disorders. The Journal of clinical endocrinology and metabolism 96: 333–343. [DOI] [PubMed] [Google Scholar]
- 21. Norrelund H (2005) The metabolic role of growth hormone in humans with particular reference to fasting. Growth hormone & IGF research: official journal of the Growth Hormone Research Society and the International IGF Research Society 15: 95–122. [DOI] [PubMed] [Google Scholar]
- 22. Ahima RS (2006) Adipose tissue as an endocrine organ. Obesity 14 Suppl 5242S–249S. [DOI] [PubMed] [Google Scholar]
- 23. Nonogaki K (2008) Ghrelin and feedback systems. Vitamins and hormones 77: 149–170. [DOI] [PubMed] [Google Scholar]
- 24. Soliman AT, ElZalabany MM, Salama M, Ansari BM (2000) Serum leptin concentrations during severe protein-energy malnutrition: correlation with growth parameters and endocrine function. Metabolism: clinical and experimental 49: 819–825. [DOI] [PubMed] [Google Scholar]
- 25. Manary MJ, Muglia LJ, Vogt SK, Yarasheski KE (2006) Cortisol and its action on the glucocorticoid receptor in malnutrition and acute infection. Metabolism: clinical and experimental 55: 550–554. [DOI] [PubMed] [Google Scholar]
- 26. Villarroya J, Diaz-Delfin J, Hyink D, Domingo P, Giralt M, et al. (2010) HIV type-1 transgene expression in mice alters adipose tissue and adipokine levels: towards a rodent model of HIV type-1 lipodystrophy. Antivir Ther 15: 1021–1028. [DOI] [PubMed] [Google Scholar]
- 27. Giralt M, Domingo P, Guallar JP, Rodriguez de la Concepcion ML, Alegre M, et al. (2006) HIV-1 infection alters gene expression in adipose tissue, which contributes to HIV- 1/HAART-associated lipodystrophy. Antivir Ther 11: 729–740. [PubMed] [Google Scholar]
- 28. Azzoni L, Crowther NJ, Firnhaber C, Foulkes AS, Yin X, et al. (2010) Association between HIV replication and serum leptin levels: an observational study of a cohort of HIV-1-infected South African women. J Int AIDS Soc 13: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Turer AT, Scherer PE (2012) Adiponectin: mechanistic insights and clinical implications. Diabetologia 55: 2319–2326. [DOI] [PubMed] [Google Scholar]
- 30. Carbone F, La Rocca C, Matarese G (2012) Immunological functions of leptin and adiponectin. Biochimie 94: 2082–2088. [DOI] [PubMed] [Google Scholar]
- 31. Procaccini C, Jirillo E, Matarese G (2012) Leptin as an immunomodulator. Mol Aspects Med 33: 35–45. [DOI] [PubMed] [Google Scholar]
- 32. Liu E, Spiegelman D, Semu H, Hawkins C, Chalamilla G, et al. (2011) Nutritional status and mortality among HIV-infected patients receiving antiretroviral therapy in Tanzania. The Journal of infectious diseases 204: 282–290. [DOI] [PubMed] [Google Scholar]
- 33. Prendergast A, Bwakura-Dangarembizi MF, Cook AD, Bakeera-Kitaka S, Natukunda E, et al. (2011) Hospitalization for severe malnutrition among HIV-infected children starting antiretroviral therapy. AIDS 25: 951–956. [DOI] [PubMed] [Google Scholar]
- 34. Heikens GT, Bunn J, Amadi B, Manary M, Chhagan M, et al. (2008) Case management of HIV-infected severely malnourished children: challenges in the area of highest prevalence. Lancet 371: 1305–1307. [DOI] [PubMed] [Google Scholar]
- 35. Kim MH, Cox C, Dave A, Draper HR, Kabue M, et al. (2012) Prompt initiation of ART With therapeutic food is associated with improved outcomes in HIV-infected Malawian children with malnutrition. J Acquir Immune Defic Syndr 59: 173–176. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Detailed methods on the assays used for the metabolic and hormonal analyses.
(DOC)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. Data are available within the Supporting Information files.