Abstract
Background
The aim of this study was to evaluate visual performance, contrast sensitivity, and patient satisfaction in patients undergoing cataract surgery with bilateral implantation of the Tecnis ZMB00 diffractive multifocal IOL (intraocular lens).
Material/Methods
This was a prospective study of 40 eyes of 20 patients with an age range from 48 to 67 years and undergoing cataract surgery with implantation of the diffractive 1-piece IOL Tecnis ZMB00 (Abbott Medical Optics) in 1 eye and 3 weeks later in the other eye. The following parameters were evaluated at 3 and 6 months after the operation: binocular uncorrected distance, intermediate and near visual acuity (UDVA, UIVA, UNVA), uncorrected binocular photopic and mesopic distance and photopic near contrast sensitivity (CSV-1000), subjective symptoms, and patient satisfaction (VF-14).
Results
No significant change was observed in logMAR UDVA between 3 and 6 months postoperatively (−0.11±0.14 vs. −0.10±0.13, p>0.05). In contrast, UNVA (0.06±0.12 vs. −0.02±0.12, p=0.004) and UIVA (0.12±0.15 vs. 0.07±0.11, p=0.005) in this period improved significantly. At 3 and 6 months after surgery, 85% of patients no longer needed to wear corrective lenses. Contrast sensitivity under different conditions was within normal age-matched limits, with significant improvements for some spatial frequencies at 3 and 6 months after surgery (p<0.04). Mean overall patient satisfaction was 9.39±1.06 and 9.19±1.20 (scale from 1 to 10, with 10 being the best score) at 3 and 6 months, respectively. Low level of halo perception was reported in 75% of patients.
Conclusions
The Tecnis ZMB00 IOL provides an effective restoration of the distance, intermediate, and near visual function, allowing patients to be totally free of need to wear corrective lenses and providing high levels of patient satisfaction.
MeSH Keywords: Cataract Extraction, Lenses, Intraocular, Visual Acuity
Background
The goal of modern cataract surgery is not only to remove the opacified lens, but also to restore visual function at various distances. This can be achieved by implanting specific models of multifocal intraocular lenses (IOLs). Refractive, diffractive, and hybrid apodized (refractive/diffractive) multifocal IOLs are currently available for clinical use [1,2]. One relatively new design of multifocal IOL is the 1-piece IOL Tecnis ZMB00 (Abbott Medical Optics), which combines diffractive and aspheric optics. This IOL is CE-marked and obtained FDA approval in 2010. Specifically, the aspheric surface of this IOL induces a controlled amount of negative spherical aberration that compensates for the positive spherical aberration usually present in the cornea. Furthermore, chromatic dispersion induced by this relatively new IOL is low and can result in an improvement in contrast sensitivity of up to 12% in comparison with other IOLs made of hydrophobic acrylic materials (e.g., Zhao H, Piers PA, Mainster MA). The additive effects of different optical design elements contribute to contrast loss in pseudophakic eyes implanted with different aspheric IOLs (presented at the XXVII Congress of the ESCRS, Barcelona, 2009). To date, the results of 2 reported studies have shown that this type of multifocal IOL is able to provide excellent objective and subjective results, with effective restoration of near and distance visual function [3,4]. The aim of the current study was to evaluate binocular visual outcomes, including the analysis of intermediate visual function, with this diffractive multifocal IOL at 3 and 6 months after surgery.
Material and Methods
Patient selection
The study included 40 eyes of 20 patients (16 females, 4 males), with a mean age of 56.10±6.8 years (range 48–67 years) undergoing cataract surgery with implantation of the diffractive 1-piece IOL Tecnis ZMB00 in 1 eye and 3 weeks later in the other eye. Patients were included if they were between 40 and 70 years old and had bilateral cataracts, preoperative corneal astigmatism of less than 1.0 D, strong motivation for independence from wearing corrective lenses, and who agreed to attend the scheduled follow-up visits. Exclusion criteria included subjects under 40 or over 70 years of age, with unrealistic visual outcome expectations or with a profession demanding visual precision (e.g., an architect), psychiatric diseases, stroke, dyslexia, dissatisfaction with progressive glasses, or the need for an IOL power beyond the available diopter range (+5.0 to +34 D). This study was approved by the local ethics committee and was performed in accordance with the ethical standards laid down in the Declaration of Helsinki.
Preoperative and postoperative examination
Before surgery, all patients had a comprehensive ophthalmological examination, including uncorrected and best corrected visual acuity, subjective refraction, corneal topography (Corneal Videokeratography Zeiss), slitlamp biomicroscopy, Goldman tonometry, biometry (IOLMaster500, Carl Zeiss Meditec AG), and binocular indirect ophthalmoscopy through a dilated pupil.
At 3 and 6 months after surgery, the clinical evaluation included the following tests: binocular uncorrected distance visual acuity (UDVA) (logMAR ETDRS chart at 4 m), uncorrected near visual acuity (UNVA) (logMAR at 35 cm), uncorrected intermediate visual acuity (UIVA) (logMAR at 60 cm), manifest refraction, binocular photopic (85 cd/m2) and mesopic (3 cd/m2) distance (2.5 m), binocular photopic near (35 cm) contrast sensitivity (1.5, 3, 6, 12, and 18 cycles/degree, CSV-1000, FACT), screening stereoscopic test (Lang Stereotest II), subjective symptoms (halo, glare), and patient satisfaction evaluation (Visual Function questionnaire VF-14) [5].
Surgical technique
All surgeries were performed by the same surgeon (WL) under general anaesthesia through a 2.8-mm incision. Continuous curvilinear capsulorrhexis of approximately 5 mm of diameter was performed. After cataract removal, the Tecnis ZMB00 IOL was inserted into the capsular bag by using the Emerald AR Unfolder (Abbott Medical Optics, Santa Ana, CA). The IOL power was calculated using optical biometry (IOLMaster, Carl Zeiss-Meditec, Jena, Germany), the SRK-T formula, and the A-constant recommended by the manufacturer (118.8). Target refraction was emmetropia in all cases.
Statistical analysis
Statistica software (IBM, Armonk, NY, USA) was used for statistical analysis. All of the data samples analyzed followed a normal distribution according to the results of the Kolmogorov-Smirnov test. Therefore, non-parametric statistical tests were used. Specifically, the Wilcoxon rank sum test was used to assess the significance of differences between 3-month and 6-month postoperative visual, contrast sensitivity, and patient satisfaction data, using the same level of significance (p<0.05) in all cases.
Results
Preoperatively, 13 eyes were hyperopic with a spherical equivalent (SE) ranging from +1.00 to + 3.50 D, a mean value of +2.04±0.74 D, and a median of 2.00 D. Ten eyes were myopic with an SE range from −1.00 to −7.00 D, a mean value of −3.73±1.90 D, and a median of −4.0 D. The remaining 17 eyes presented a SE of 0.00 D. For the whole sample, mean and median preoperative SE were −0.26±2.40 D and 0.00 D, respectively. Mean preoperative binocular logMAR UDVA was 0.43±0.28 and mean binocular logMAR corrected distance visual acuity (CDVA) was 0.12±0.17.
At 3 and 6 months after surgery, mean SE was 0.20 D for distance and near vision. No significant improvement of binocular UDVA was observed between 3 months and 6 months postoperatively (logMAR −0.11±0.14 vs. −0.10±0.13, p=NS). In contrast, a small but statistically significant improvement of binocular UNVA was detected (0.06±0.12 vs. −0.02±0.12, p= 0.004) (Table 1).
Table 1.
Binocular 3 and 6-month mean UDVA, UNVA, UIVA, and CIVA (logMAR).
| Parameter | 3 months | 6 months | p-value |
|---|---|---|---|
| UDVA | −0.11±0.14 | −0.10±0.13 | NS |
| UNVA | 0.06±0.12 | −0.02±0.12 | 0.004 |
| UIVA | 0.12±0.15 | 0.07±0.11 | 0.004 |
| CIVA | 0.00±0.05 | −0.06±0.06 | 0.005 |
NS – statistically not significant.
For intermediate vision, 2 subjects needed to wear corrective lenses ranging from +1.00 D to +1.37 D at the 3-month follow-up visit, and 6 months after surgery 2 subjects needed to ear corrective lenses ranging from +1.37 D to +1.50 D. Seven subjects achieved a corrected intermediate visual acuity (CIVA) of 0.00 logMAR and 19 subjects achieved a logMAR CIVA of 0.10. A binocular logMAR CIVA of 0.00 was achieved in 35% (7/20) of patients. Mean logMAR CIVA was 0.00±0.05 and −0.06±0.06 at 3 and 6 months after surgery, respectively. This change was statistically significant (p=0.005).
At 3 months postoperatively, mean binocular UIVA was 0.12±0.15. Binocular logMAR UIVA was 0.10 or better in 65% (13/20) of patients. At 6 months postoperatively, logMAR UIVA improved significantly (p=0.004), achieving a mean binocular value of 0.07±0.11. The percentage of eyes achieving a logMAR UIVA of 0.10 or better was the same as that obtained at 3 months postoperatively.
Corrective lenses independence outcomes
At 3 and 6 months after surgery, 85% of patients (17/20) were totally free of the need to wear corrective lenses. The best results of corrective lenses independence were obtained for distance (94%–95%), followed by near (85%–90%) and intermediate vision (88%–90%).
Contrast sensitivity (CS) outcomes
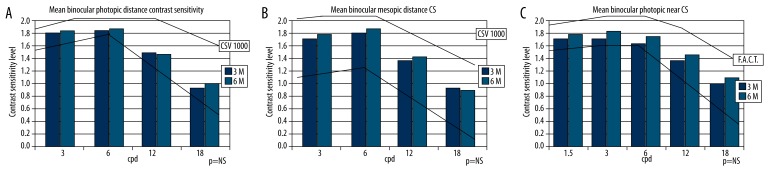
At 3 and 6 months postoperatively, photopic and mesopic CS for distance and photopic CS for near were found to be within normal limits for the normal population in the range of 50 to 75 years [6] (Figure 1A–1C, Table 2). At 6 months postoperatively, significant improvements of mesopic CS for distance (3 cycles/º: 1.76±0.09 vs. 1.83±0.08, p<0.03) and photopic CS for near (1.5 cycles/º: 1.76±0.07 vs. 1.82±0.07, p<0.04; 3 cycles/º: 1.80±0.06 vs. 1.86±0.05, p<0.02; 6 cycles/º: 1.69±0.12 vs. 1.78±0.12, p<0.01) were observed for some spatial frequencies (Table 2).
Figure 1.
Mean uncorrected binocular distance photopic (A) and mesopic (B) CS, as well as mean photopic near CS (C), at 3 and 6 months after surgery in comparison to the normal values for a population aged 50–75 years (continuous line).
Table 2.
Mean uncorrected binocular photopic, mesopic distance and photopic near contrast sensitivity. Comparison of results 3 and 6 month postoperatively.
| 3 months | 6 months | p value | |
|---|---|---|---|
| Photopic distance | |||
| 3 cpd | 1.84±0.10 | 1.87±0.07 | NS |
| 6 cpd | 1.89±0.12 | 1.93±0.13 | NS |
| 12 cpd | 1.56±0.18 | 1.53±0.15 | NS |
| 18 cpd | 0.99±0.19 | 1.04±0.17 | NS |
| Mesopic distance | |||
| 3 cpd | 1.76±0.09 | 1.83±0.08 | <0.03 |
| 6 cpd | 1.84±0.12 | 1.89±0.14 | NS |
| 12 cpd | 1.42±0.18 | 1.47± 0.13 | NS |
| 18 cpd | 0.97±0.27 | 0.95±0.15 | NS |
| Photopic near | |||
| 1.5 cpd | 1.76±0.07 | 1.82±0.07 | <0.04 |
| 3 cpd | 1.80±0.06 | 1.86±0.05 | <0.02 |
| 6 cpd | 1.69±0.12 | 1.78±0.12 | <0.01 |
| 12 cpd | 1.40±0.12 | 1.54±0.11 | NS |
| 18 cpd | 1.04±0.16 | 1.17±0.17 | NS |
NS – statistically not significant.
Patient satisfaction outcomes
No significant changes were observed in the general vision satisfaction score between 3 and 6 months after surgery (9.39±1.06 vs. 9.19±1.20, p=NS, scale ranging from 0 [not satisfied at all] to 10 [completely satisfied]). Furthermore, no significant changes between 3 and 6 months postoperatively were detected in the scores for the different aspects of visual function evaluated with the VF-14 test (Table 3). Patients had mild or no difficulties in performing the different activities evaluated with the VF-14 questionnaire (Table 3). Driving at night was the only activity during which patients experienced little to moderate difficulties.
Table 3.
Visual function test (VF-14); comparison of 3 and 6 month results.
| Activity | 3 months | 6 months | p value |
|---|---|---|---|
| 1. Reading small print | 1.36±0.68 | 1.38±0.84 | NS |
| 2. Reading a newspaper or book | 1.31±0.67 | 1.38±0.69 | NS |
| 3. Reading a large-print book | 1.05±0.23 | 1.00±0.00 | NS |
| 4. Recognizing people close by | 1.00±0.00 | 1.00±0.00 | NS |
| 5. Seeing steps, stairs or curbs | 1.05±0.22 | 1.05±0.23 | NS |
| 6. Reading traffic signs, street names or store signs | 1.16±0.50 | 1.17±0.51 | NS |
| 7. Doing fine handicrafts | 1.26±0.56 | 1.17±0.51 | NS |
| 8. Writing cheques or filling out forms | 1.16±0.37 | 1.11±0.47 | NS |
| 9. Playing cards | 1.00±0.00 | 1.00±0.00 | NS |
| 10. Doing sport activities | 1.00±0.00 | 1.00±0.00 | NS |
| 11. Cooking | 1.10±0.31 | 1.00±0.00 | NS |
| 12. Watching television | 1.26±0.45 | 1.00±0.00 | NS |
| 13. Driving during the day | 1.18±0.40 | 1.22±0.44 | NS |
| 14. Driving at night | 2.54±1.13 | 2.22±1.30 | NS |
(Scale: no difficulties – 1, little difficulties – 2, moderate difficulties – 3, big difficulties – 4, unable to perform activity – 5).
Regarding photic phenomena, a significant reduction in halo-related difficulties at work, as well as in the level of halo perception, was noted at 6 months after surgery (Table 4). Low levels of halo perception were observed in 55% (11/20) and 60% (12/20) of patients at 3 and 6 months after surgery, respectively. No patients complained about any other photic adverse effects such as glare.
Table 4.
Photic adverse effects (halo) – 3 and 6-month comparison (range 0–4; 0 = none, 4 = strong/severe).
| Question | 3 months | 6 months | p value |
|---|---|---|---|
| Work difficulty regarding “halo” | 1.55±0.98 | 0.94±1.11 | <0.003 |
| Level of “halo” perception | 1.33±1.08 | 0.76±1.03 | <0.005 |
Complications
No intra- or postoperative complications were observed. At 6 months, no cases of posterior capsular opacification requiring YAG capsulotomy were detected.
Discussion
Mean binocular logMAR UDVA in the current series was −0.10 at 6 months after surgery, which confirms the ability of this multifocal IOL to successfully restore distance vision, consistent with reports by other authors using the same type of multifocal IOL [3,4]. Specifically, Bautista et al. [3] found a mean postoperative logMAR UDVA of 0.08 at 2 months postoperatively, and Friedrich [4] reported that 94.7% of patients implanted with the same IOL used in our study had a binocular UDVA of 0.1 LogMAR or better. The good distance vision outcome obtained in the current and previous studies is accompanied by a predictable correction of ocular refraction, resulting in minimum residual refractive errors. In comparison with other models of diffractive and zonal refractive multifocal IOLs, the level of binocular distance visual acuity is similar or even better [7–12].
Mean binocular logMAR UNVA at 6 months after surgery in the current series was −0.02, which is consistent with the results of previous series evaluating the same type of multifocal IOL [3,4]. Bautista et al. [3] found that 94.3% of eyes from a sample implanted with the Tecnis ZMB00 IOL could read 0.00 logMAR without correction at 2 months postoperatively. Similarly, in a sample of patients implanted bilaterally with the same type of multifocal IOL, Friedrich4 reported that 67.7% of eyes could read Jaeger 1+ (0.0 LogMAR) and 93.6% could read Jaeger 1 (0.1 LogMAR) or better at 6 months after surgery. These results indicate that this multifocal IOL is also able to restore the near vision function successfully. These outcomes are similar to or better than those reported for other modalities of aspheric diffractive and zonal refractive multifocal IOLs [7–12]. Tsaousis et al. [7] found a mean postoperative (mean follow-up: 26±6 months) logMAR binocular UNVA of 0.11±0.10 in a sample of eyes implanted with the hybrid apodized diffractive/refractive IOL AcrySof IQ ReSTOR IOL (Alcon, Inc. USA). Alfonso et al. [12] found a mean 6-month postoperative logMAR UNVA of −0.05±0.07 in a sample of eyes implanted with the fully diffractive IOL Acri.Lisa 366D.
Besides distance and near vision outcomes, the current study is the first reporting on intermediate visual outcomes achievable with the Tecnis ZMB00 multifocal IOL. Mean logMAR UIVA was 0.12, a very similar value to those reported by other authors using other types of multifocal IOLs [7–12] (Tsaousis et al. [7] 0.11±0.10 with AcrySof IQ ReSTOR and Alfonso et al. [12] 0.19±0.14 with Acri.Lisa 366D). Likewise, the UIVA outcome obtained in the current series is comparable to that reported for a previous model of the Tecnis multifocal lens (ZM900) [13]. Our results show that the IOL evaluated also provides a functional level of intermediate vision. Furthermore, in the current series, UIVA and UNVA improved significantly from 3 to 6 month postoperatively. Several factors may have contributed to this finding, but patient neuroadaptation to the multifocality induced by the IOL optics seems to have played a major role. Indeed, a similar finding has been reported with other diffractive multifocal IOLs [14,15] and it has even been demonstrated that visual performance after multifocal IOL implantation can be significantly accelerated by training programs [16]. Via the neuroadaptation process (synaptogenesis, neurogenesis) [17], the brain has the ability to select an image related to the object that is being looked at, suppressing other images.
Regarding contrast sensitivity, the results obtained in the current series were well within the normal limits defined for the 50–75 years age range [6], which corresponds to the age range of the sample of patients of the current series. However, the values obtained for higher spatial frequencies were close to the lower limit of the normality range. This outcome is similar to or even better than those reported for other designs of multifocal IOLs, including diffractive and zonal refractive models [9,18,19]. Furthermore, some significant improvements were detected in distance and near contrast sensitivity between the 3-month and 6-month postoperative visits. As with UNVA and UIVA, neuroadaptation may also have played a role in this improvement of visual performance.
As a result of the ability of the IOL to restore the visual acuity and contrast sensitivity, independence from wearing corrective lenses was high, with a total of 85% of patients achieving complete independence. Similar results have also been reported with other models of multifocal IOLs [13,20–22]. Cillino et al. [22], in a comparative study of the clinical outcomes obtained with 4 types of IOL, found that independence from wearing corrective lenses was achieved in 20% of cases implanted with a monofocal IOL (AR40 from AMO), in 43.7% and 53.3% of cases implanted with the multifocal refractive IOLs Array SA40N and ReZoom from AMO, respectively, and in 87.5% of cases implanted with the diffractive multifocal IOL Tecnis ZM900.
Finally, patient satisfaction with the outcome of surgery was evaluated using the VF-14 questionnaire. General patient satisfaction was very high and stable, with most of patients scoring their level of satisfaction at between 8 and 10 (0 = not satisfied at all and 10 = completely satisfied), as reported for a previous model of the Tecnis diffractive IOL [21]. The VF-14 test detected only slight to moderate difficulty in driving at night. This effect is mainly attributed to the photic phenomena induced by diffractive optics. This effect is reduced with the introduction of an aspheric optic, minimizing the level of spherical aberration. In contrast, the effect is increased if the multifocal IOL has an additional refractive component [23]. In the current series, a low level of halo perception was reported in 60% of patients at 6 months postoperatively, with no severe complaints of halos. Future studies should confirm if this subjective symptomatology disappears with time, as suggested by many authors based on the short- and medium-term outcomes [15] and according to the significant reduction of the intensity of photic phenomena with time observed in the current series.
Conclusions
The diffractive multifocal IOL Tecnis ZMB00 provides an effective restoration of distance, intermediate, and near vision, promoting a very high level of independence from wearing corrective lenses, as well as high patient satisfaction. Studies should be conducted to evaluate the long-term outcomes obtained with this modality of diffractive multifocal IOL.
Footnotes
Source of support: Departmental sources
Competing interests
The authors have no proprietary or commercial interest in the medical devices that are involved in this manuscript.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Gooi P, Achmed IK. Review of presbyopic IOLs: multifocal and accomodating IOLs. Int Ophthalmol Clin. 2012;52:41–50. doi: 10.1097/IIO.0b013e31824b87be. [DOI] [PubMed] [Google Scholar]
- 2.Lichtinger A, Rootman D. Intraocular lenses for presbyopia correction: past, present, and future. Curr Opin Ophthalmol. 2012;23:40–46. doi: 10.1097/ICU.0b013e32834cd5be. [DOI] [PubMed] [Google Scholar]
- 3.Bautista PC, Gonzales DC, Gomez AC. Evolution of visual performance in 70 eyes implanted with the Tecnis ZMB00 multifocal intraocular lens. Clin Ophthalmol. 2012;6:403–7. doi: 10.2147/OPTH.S24425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freidrich R. IOL multifocality combined with the compensation for corneal spherical aberration: a new concept of presbyopia correcting IOL. Klin Monel Augenheilkd. 2012;229:1108–12. doi: 10.1055/s-0032-1315343. [DOI] [PubMed] [Google Scholar]
- 5.Steinberg EP, Tielsh JM, Schein OD, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol. 1994;112:630–38. doi: 10.1001/archopht.1994.01090170074026. [DOI] [PubMed] [Google Scholar]
- 6.Pomerance G, Evans D. Test-retest reliability of the CSV-1000 contrast test and its relationship to glaucoma therapy. Invest Ophthalmol Vis Sci. 1994;35:3357–61. [PubMed] [Google Scholar]
- 7.Tsaousis KT, Plainis S, Dimitrakos SA, Tsinopoulos IT. Binocularity enhances visual acuity of eyes implanted with multifocal intraocular lenses. J Refract Surg. 2013;29:246–50. doi: 10.3928/1081597X-20130318-03. [DOI] [PubMed] [Google Scholar]
- 8.Lubiński W, Podboraczyńska-Jodko K, Gronkowska-Serafin J, Karczewicz D. Visual outcome three and six months after implantation of Acri.LISA 366D lenses. Klin Oczna. 2012;114:249–54. [PubMed] [Google Scholar]
- 9.Muñoz G, Albarrán-Diego C, Ferrer-Blasco T, et al. Visual function after bilateral implantation of a new zonal refractive aspheric multifocal intraocular lens. J Cataract Refract Surg. 2011;37:2043–52. doi: 10.1016/j.jcrs.2011.05.045. [DOI] [PubMed] [Google Scholar]
- 10.de Vries NE, Webers CA, Montés-Micó R, et al. Visual outcomes after cataract surgery with implantation of a +3.00 D or +4.00 D aspheric diffractive multifocal intraocular lens: Comparative study. J Cataract Refract Surg. 2010;36:1316–22. doi: 10.1016/j.jcrs.2010.01.036. [DOI] [PubMed] [Google Scholar]
- 11.Alfonso JF, Fernández-Vega L, Puchades C, Montés-Micó R. Intermediate visual function with different multifocal intraocular lens models. J Cataract Refract Surg. 2010;36:733–39. doi: 10.1016/j.jcrs.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 12.Alfonso JF, Puchades C, Fernández-Vega L, et al. Visual acuity comparison of 2 models of bifocal aspheric intraocular lenses. J Cataract Refract Surg. 2009;35:672–76. doi: 10.1016/j.jcrs.2008.11.061. [DOI] [PubMed] [Google Scholar]
- 13.Akaishi L, Vaz L, Vilella G, et al. Visual performance of tecnis ZM900 diffractive multifocal IOL after 2500 implants: a 3-year follow-up. J Ophthalmol. 2010;2010 doi: 10.1155/2010/717591. pii: 717591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moreno LJ, Piñero DP, Alió JL, et al. Double-pass system analysis of the visual outcomes and optical performance of an apodized diffractive multifocal intraocular lens. J Cataract Refract Surg. 2010;36:2048–55. doi: 10.1016/j.jcrs.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 15.Palomino Bautista C, Carmona González D, Castillo Gómez A, Bescos JA. Evolution of visual performance in 250 eyes implanted with the Tecnis ZM900 multifocal IOL. Eur J Ophthalmol. 2009;19:762–68. doi: 10.1177/112067210901900513. [DOI] [PubMed] [Google Scholar]
- 16.Kaymak H, Fahle M, Ott G, Mester U. Intraindividual comparison of the effect of training on visual performance with ReSTOR and Tecnis diffractive multifocal IOLs. J Refract Surg. 2008;24:287–93. doi: 10.3928/1081597X-20080301-11. [DOI] [PubMed] [Google Scholar]
- 17.Pepin SM. Neuroadaptation of presbyopia-correcting intraocular lenses. Curr Opin Ophthalmol. 2008;19:10–12. doi: 10.1097/ICU.0b013e3282f31758. [DOI] [PubMed] [Google Scholar]
- 18.Santhiago MR, Wilson SE, Netto MV, et al. Visual performance of an apodized diffractive multifocal intraocular lens with +3.00-d addition: 1-year follow-up. J Refract Surg. 2011;27:899–906. doi: 10.3928/1081597X-20110816-01. [DOI] [PubMed] [Google Scholar]
- 19.Alfonso JF, Fernández-Vega L, Baamonde MB, Montés-Micó R. Prospective visual evaluation of apodized diffractive intraocular lenses. J Cataract Refract Surg. 2007;33:1235–43. doi: 10.1016/j.jcrs.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 20.Zhang F, Sugar A, Jacobsen G, Collins M. Visual function and spectacle independence after cataract surgery: bilateral diffractive multifocal intraocular lenses versus monovision pseudophakia. J Cataract Refract Surg. 2011;37:853–58. doi: 10.1016/j.jcrs.2010.12.041. [DOI] [PubMed] [Google Scholar]
- 21.Gierek-Ciaciura S, Cwalina L, Bednarski L, Mrukwa-Kominek E. A comparative clinical study of the visual results between three types of multifocal lenses. Graefes Arch Clin Exp Ophthalmol. 2010;248:133–40. doi: 10.1007/s00417-009-1177-4. [DOI] [PubMed] [Google Scholar]
- 22.Cillino S, Casuccio A, Di Pace F, et al. One-year outcomes with new-generation multifocal intraocular lenses. Ophthalmology. 2008;115:1508–16. doi: 10.1016/j.ophtha.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 23.Alió JL, Plaza-Puche AB, Piñero DP, et al. Quality of life evaluation after implantation of 2 multifocal intraocular lens models and a monofocal model. J Cataract Refract Surg. 2011;37:638–48. doi: 10.1016/j.jcrs.2010.10.056. [DOI] [PubMed] [Google Scholar]