Abstract
Study Objectives:
Patients with obstructive sleep apnea (OSA) on established positive airway pressure (PAP) treatment are often advised routine annual follow-up visits to assess ongoing effectiveness and address problems associated with therapy. This study evaluates the clinical utility of annual face-to-face follow-up visits.
Design:
We performed a retrospective chart review of OSA patients on PAP who had completed a routine annual follow-up visit. Demographics, polysomnography, PAP compliance, Epworth Sleepiness Scale (ESS), subjective complaints (efficacy and interface issues, equipment malfunction, prescription renewal), objective findings (efficacy or leak issues, equipment problems), and visit-specific interventions were recorded. We determined relationships between patient provided information and likelihood of therapeutic versus administrative interventions.
Setting:
Academic sleep center.
Measurements and Results:
Among 716 patients who met study criteria, we abstracted data on 180 randomly selected patients. On multivariate analyses, only subjective complaints or objective findings by providers were associated with a therapeutic intervention (p < 0.0001). Though most patients (55 of 63 patients, 87.3%) who required therapeutic interventions had objective findings, without subjective complaints, the odds of such findings were only 0.12 (95% CI = 0.06-0.24, p < 0.0001). Without subjective complaints, the likelihood of a therapeutic intervention was 0.07 (95% CI = 0.03-0.15, p < 0.001).
Conclusion:
Our data suggests that in the absence of a subjective complaint, an annual follow-up is more likely to require administrative rather than face-to-face clinical intervention. Designing a clinic model to account for this might reduce resource utilization. However, the value and optimal timing of “routine” annual follow-up visits requires further evaluation.
Citation:
Nannapaneni S, Morgenthaler TI, Ramar K. Assessing and predicting the likelihood of interventions during routine annual follow-up visits for management of obstructive sleep. J Clin Sleep Med 2014;10(8):919-924.
Keywords: obstructive sleep apnea, follow-up, clinic visits, CPAP, complaints
The most common treatment option for patients with obstructive sleep apnea (OSA) is the use of continuous positive airway pressure (CPAP). Occasionally, patients who are unable to tolerate CPAP may need a different form of positive airway pressure (PAP) to treat OSA such as bilevel positive airway pressure (BPAP).1 The short-term and long-term positive effects of PAP therapy in OSA patients are well established.2 Adherence to PAP therapy is important to obtain and maintain these expected positive benefits. However, studies have shown that the overall adherence is suboptimal.3–5 The suboptimal PAP adherence may be related to various factors such as nasal congestion, rhinorrhea, dryness, mask interface problems such as lack of fitting, mask leak issues, pressure related problems such as exhaling against high pressure, or PAP machine related symptoms.6–8 Close follow-up to monitor and address compliance issues in OSA patients is recommended to establish effective utilization patterns and remediate any problems related to the PAP or the mask, and thereby improve PAP adherence.9 This is especially important during the first few weeks of PAP use, as adherence to PAP therapy is more likely to be established within the first few months of PAP use.9,10 Accordingly, CMS and third party payers require an initial face-to-face follow-up visit with a physician to assess PAP adherence and benefits of PAP use between 31 and 90 days after the start of PAP therapy.11 Subsequently, patients on PAP therapy for OSA are frequently advised annual follow-up visits by trained health care providers in order to continue to troubleshoot and manage issues that may arise with the use of PAP devices and renew PAP prescriptions as requested by vendors.12 Changes in PAP may also be needed as the patient's weight changes or as new side effects related to therapy emerge, not to mention the possible occurrence of mechanical malfunctions of PAP equipment.10 Therefore, most sleep centers, based on the current guidelines advise OSA patients on PAP therapy, to return for an annual clinic follow up visit.9,10,12 Despite these reasonable considerations, the value of such annual routine visits has not been scrutinized.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Though patients with obstructive sleep apnea (OSA) on positive airway pressure (PAP) are routinely advised annual follow-up visits to assess ongoing effectiveness and address problems related to PAP use, there is no available data to support the value of this practice, particularly in an era of decreasing costs of care and improving patient access with appropriate resource utilization.
Study Impact: Our study found that in the absence of subjective symptoms, OSA patients on CPAP are less likely to need an intervention during their annual follow-up face-to-face visit. Our findings suggest an opportunity for future studies to investigate screening tools that would assess predictive factors prospectively to determine the need for and timing of face-to-face follow-up visits for this patient population.
Our anecdotal observations suggest that significant changes to PAP therapy were made infrequently during routine annual follow-up visits. Often, it seemed that the appointments were mostly congratulatory on their CPAP use, and that only administrative tasks such as prescription refills that might be accomplished without a face-to-face visit were accomplished. In an era of increasing emphasis on appropriate resource utilization and efforts towards decreasing costs of care, we considered a review of our current clinical practice of utmost importance, particularly as it pertains to the requirement of these routine annual follow-up visits for all patients with OSA on PAP therapy. A literature search on this topic did not reveal any studies to date. The goal of this study was therefore to evaluate the clinical utility of routine annual face-to-face follow-up visits for OSA patients on PAP therapy and determine which clinical predictors are associated with a need for clinically significant interventions during such visits.
METHODS
Study Design
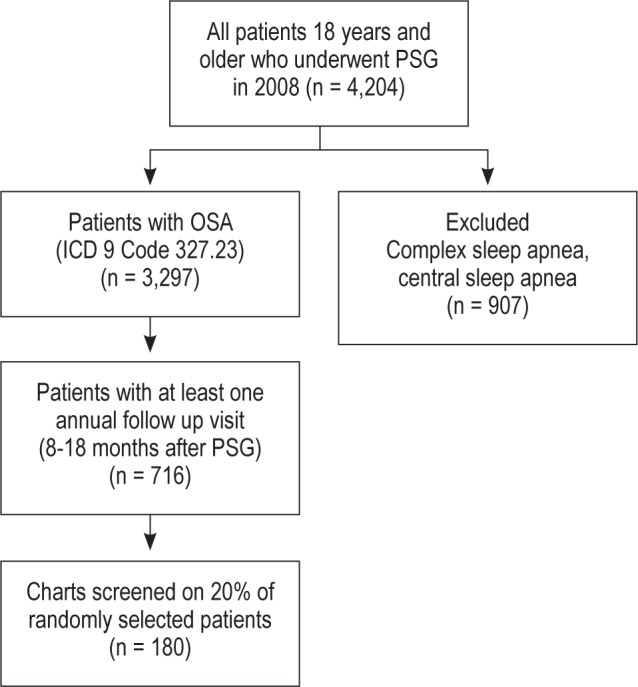
A retrospective chart review was conducted on patients 18 years and older seen at our center who had a clinical diagnosis of OSA (ICD-9 Code 327) and underwent a baseline polysomnography (PSG) in the year 2008. Of the 4,204 patients who had a PSG performed, 3,297 patients were confirmed to have a diagnosis of OSA (ICD-9 Code 327.23). Patients with central sleep apnea and complex sleep apnea were excluded from the study. Of the patients with OSA, we screened for patients who had at least one routine annual follow-up visit. We considered “routine follow up visits” as those that occurred 12-18 months after the initial PAP visit; the initial PAP visit usually occurred 2-12 weeks following PAP prescription to help with initial adaptation. Based on these criteria, 716 patients were eligible and included in the study group. Of the 716 patients, data were abstracted on 180 (20%) randomly selected patients (Figure 1).
Figure 1. Patient selection algorithm.
In addition to demographics, we gathered data on PAP compliance (device download), body mass index (BMI), Epworth Sleepiness Scale (ESS), subjective patient symptoms (such as problems related to treatment efficacy, interface issues, PAP equipment malfunction), objective clinical findings (such as lack of efficacy, leak issues around the PAP mask, nasal or mouth dryness despite adequate humidity settings on their PAP device or history of water reservoir emptying overnight during use), and visit-specific interventions. Dryness was evaluated not only by asking for these symptoms but was objectively evaluated by routinely asking patients about: (i) humidity settings on their PAP device and (ii) whether the water reservoir ran empty or had to be refilled in a given night. Additionally, data were gathered on coexisting chronic medical conditions such as diabetes mellitus, hypertension, dyslipidemia, chronic kidney disease, coronary artery disease, and current tobacco use. Data were also obtained on the presence of preexisting or concomitant diagnosis of restless legs syndrome (RLS) and insomnia. The visit-specific interventions were divided into “therapeutic interventions” (that required a licensed care provider for skilled troubleshooting, mask fitting, or patient education) and “administrative interventions” (clerical in nature that might be provided by non-licensed healthcare workers, or management of prescription refills for equipment or established medications that might be taken care of without a visit or on protocol). Therapeutic interventions included changes in mask interface, changes in PAP pressure or modality (e.g., from CPAP to BPAP), addition of oxygen, addition of new medications such as sleep hypnotics, change from PAP therapy (i.e., change from PAP to oral appliance or referral to surgery), or discontinuation of PAP therapy because of patient/clinical reasons. Administrative interventions included PAP prescription refills, established or routine medication refills, education on how to use their current mask and adjusting the straps, or education regarding care and operation of the PAP machine. PAP compliance was evaluated based on the Centers for Medicare and Medicaid services (CMS) definition of use: ≥ 4 h per night on 70% of nights during a consecutive 30-day period anytime between 31 and 90 days of initial use.
Patients at their annual follow-up visit were seen or supervised by sleep physicians, nurse practitioners (NPs)/physician assistants (PAs), or trained registered nurses (RNs). ESS was filled out and device downloads were obtained from the PAP machines before the patients' visit with the providers. During the visit, patients were asked about their subjective symptoms or complaints. Similarly, objective findings were evaluated during the visit and documented based on assessment of PAP devices and masks/straps for problems such as leak issues.
Data Analysis
Data were analyzed using JMP statistical software (Version 9.0.1, SAS Institute, Cary, NC). Descriptive statistics were performed on baseline characteristics of patients. The t-test statistic was used for 2 group statistics with respect to continuous variables and the Pearson χ2 for categorical values. Nonparametric tests (Wilcoxon) were used to assess data with non-normal distribution. A sum risk factor score (RF score) was developed for each individual patient by adding the total number of cardiovascular risk factors, and an exponential score was generated by multiplying the sum score by itself to assess the additive effect of each clinical condition. From the list of predictors and potential confounders, simple logistic-regression analysis was performed to identify significant covariates that were correlated with intervention. Subsequently, we built multivariate logistic-regression models with therapeutic intervention as the dependent variable using significant covariates identified by simple logistic-regression analysis. Significance was defined with a p-value < 0.05. Next, we tried to determine if there was baseline or patient-provided information that related to the likelihood of specific intervention at the annual follow-up visit. Visit-specific interventions were categorized into higher or lower level interventions as explained above.
In addition, we divided the patients randomly into a derivation group (70%) and a validation group (30%). Recursive partitioning analysis was applied to the derivation group to select factors that predicted a clinically significant intervention at the annual follow-up visits.13 We then checked the performance of those factors in the validation group. We developed receiver operator curves (ROC) for these models.
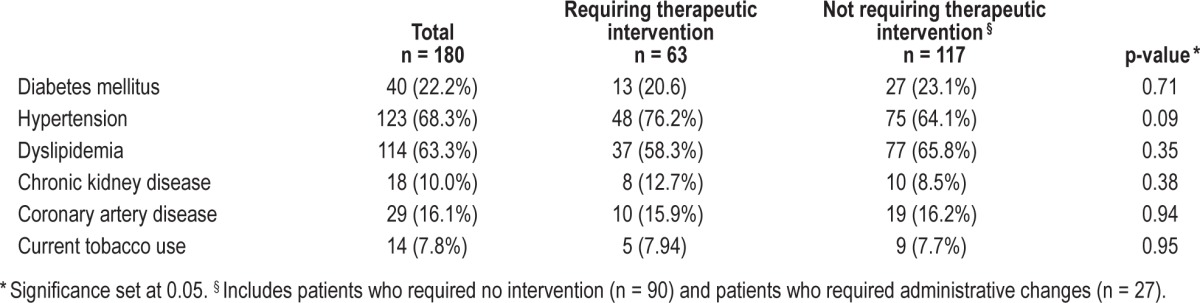
RESULTS
The baseline patient demographics are shown in Table 1. The BMI (Mean ± SD) did not significantly change from baseline to annual follow up visit (35.6 ± 7.7 to 35.5 ± 7.9, p = 0.28). However, there was a significant decrease in ESS from baseline (Mean ± SD) 10.1 ± 5.0 to 6.8 ± 4.1 at follow-up (p = 0.001). At the annual follow-up visit, PAP compliance in the overall study population was 74%. Therapeutic interventions at the annual follow-up were provided to 63 patients (35% of the patients), as listed in Table 2. Information regarding those requiring therapeutic interventions vs not requiring therapeutic interventions is provided in Table 3. The factors that were significantly associated with a therapeutic intervention were the presence of subjective symptoms (interface, efficacy) and objective findings (leak, efficacy, equipment problems, and dryness) (Table 3). Though not statistically significant, univariate analysis demonstrated that patients who were compliant with PAP therapy were less likely to require therapeutic intervention (78.6%, p = 0.08). Also, univariate and multivariate analysis of each individual chronic disease condition did not appear to predict the need for therapeutic interventions at the time of follow-up visit (Table 4). Preexisting sleep related conditions such as RLS and insomnia also did not appear to increase the likelihood of need for therapeutic interventions at the follow-up visit (Pearson χ2 1.48, p = 0.22, and 1.97, p = 0.16, respectively). Duration (in months) from baseline PSG to annual follow-up visit on patients who were on CPAP did not correlate with the need for therapeutic intervention. Further analysis to evaluate for predictive effect of the RF score did not appear significant with either univariate or multivariate analysis.
Table 1.
Baseline patient characteristics
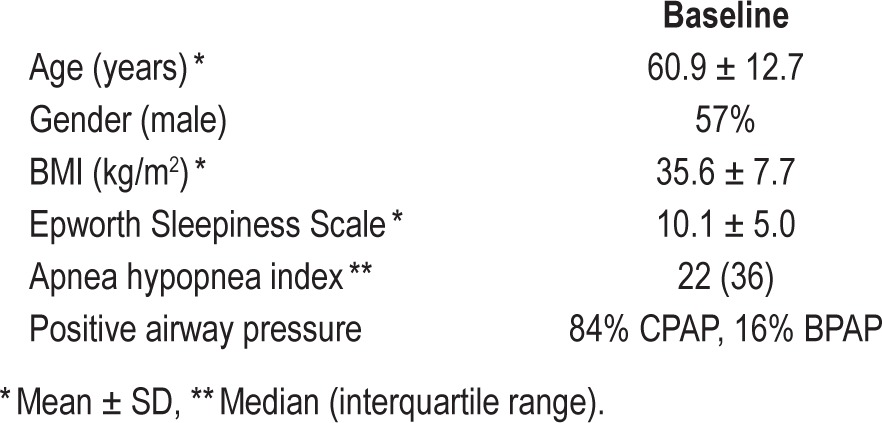
Table 2.
Interventions at annual follow-up of 180 patients
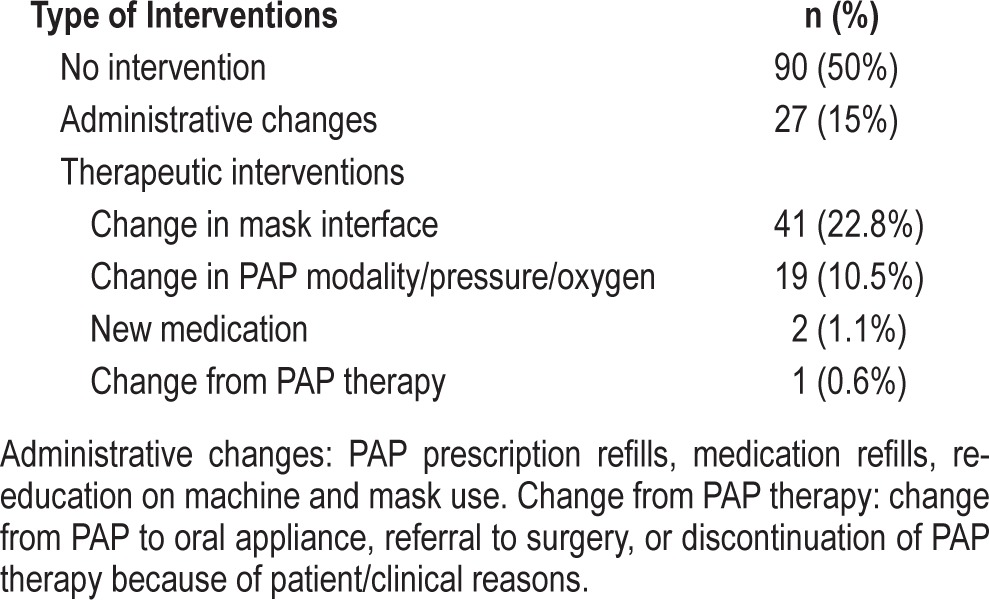
Table 3.
Characteristics of patients at annual follow-up
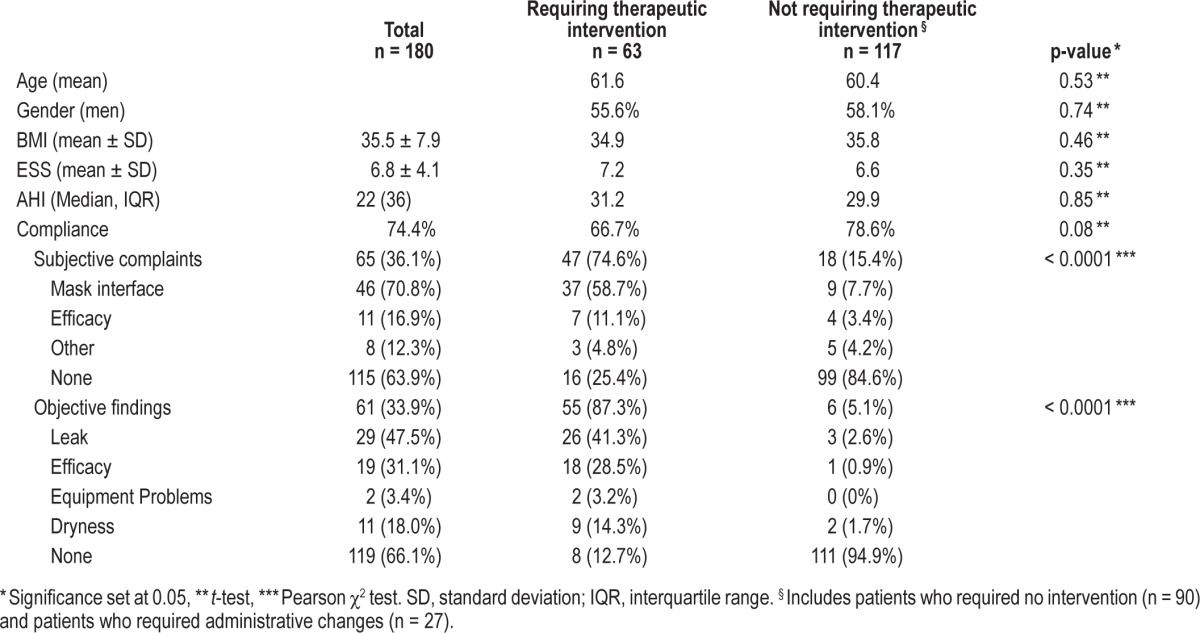
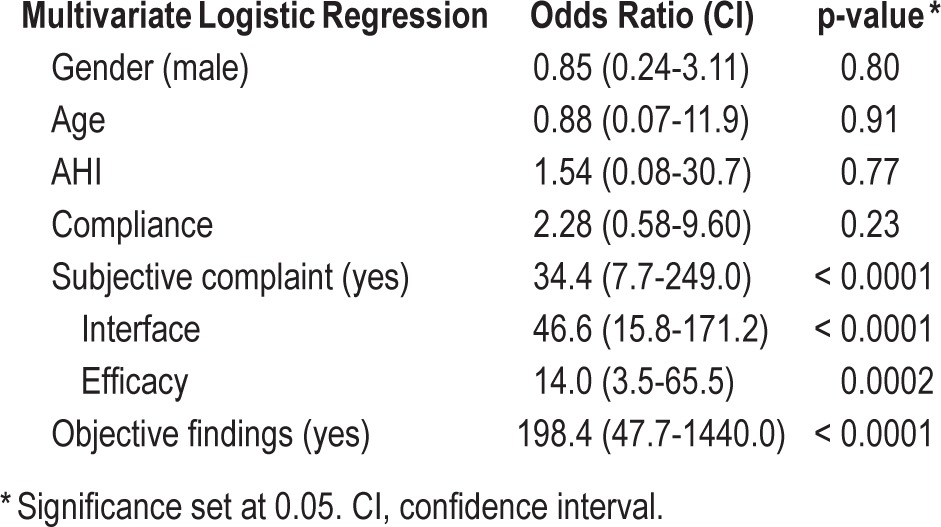
Table 4.
Univariate analysis of chronic medical conditions and need for intervention
Of the 65 patients (36%) who presented with subjective complaints, therapeutic interventions were performed in 47 (72.3%). Additionally, when health care providers identified a problem (objective findings; Table 3) such as efficacy problems with PAP (evidenced by high ESS or downloaded AHI estimates), leak issues, or dryness (61 patients, 34%), 55 (90.2%) had a therapeutic intervention performed during their visit (change in interface, change in PAP pressure/modality, addition of oxygen, addition of medications or change from PAP therapy—change from PAP to oral appliance, or referral to surgery, or discontinuation of PAP therapy because of patient/clinical reasons). Of the 115 patients without subjective complaints, only 16 (13.9%) had therapeutic interventions (8 had change in mask interface, 7 had change in PAP type, and 1 had a medication change). In patients without subjective complaints, the likelihood of a needing a therapeutic intervention was 0.07 (95% CI = 0.03-0.15, p < 0.001). If the patient had no subjective complaint, the odds of finding an objective problem at the follow-up visit was 0.12 (95% CI = 0.06-0.24, p < 0.0001). On multivariate logistic regression, the only significant predictors of patients needing clinical intervention during the follow-up visit was the presence of subjective symptoms (found in 36% of the total) or the finding of objective problems (33.9% of patients) by their providers (Table 5).
Table 5.
Predictors of need for therapeutic intervention
In addition to the multivariate analysis, we sought thresh olds for predictors of therapeutic intervention using recursive partitioning analysis, which revealed that the most significant predictors of the need for therapeutic intervention were the presence of a subjective complaint, AHI > 12, age > 55, and BMI < 40.
DISCUSSION
The findings of this study clearly demonstrate that OSA patients on PAP therapy are less likely to need an intervention during their routine annual face-to-face follow-up visit in the absence of subjective symptoms. Therapeutic interventions during prescheduled routine annual visits occurred only in 36% of patients, and the likelihood for an intervention in the absence of a subjective complaint was very low at 0.07 (95% CI = 0.03-0.15, p < 0.001). The presence of subjective complaints, baseline AHI above 12, age older than 55, and a BMI less than 40, were identified as factors predictive for the need of therapeutic intervention. In the era of reducing costs of health care delivery and improving resource utilization, our study provides evidence that select patients such as those with subjective complaints may benefit from face-to-face follow-up visits due to their need for clinical intervention, while the majority might possibly be adequately served in some other manner, such as follow-up via electronic, telephonic, or correspondence methods. However, these findings should not be misconstrued as a guideline or recommendation to follow until future prospective studies at other sleep centers can validate our findings.
From our analysis we were also able to show that the presence of chronic medical conditions and sleep related disorders such as RLS and insomnia were not predictive of a need for therapeutic intervention at the time of a routine annual follow-up visit. This again suggests that the only factors that remain strongly predictive of the higher likelihood of need for interventions at the time of follow-up visits are the presence of a subjective complaint or finding of an objective problem.
Fifty percent of the patients did not require any clinical intervention whatsoever at their annual follow-up visit. In another 15% of cases, patients required an administrative renewal of PAP prescription, refill of routine or established medications, or education regarding proper use of existing equipment. It is likely that many of these latter transactions could be delivered by sleep technologists or performed via telephone or primary care providers, obviating the need for a sleep center intervention. On the other hand, only 15.4% of patients who had subjective complaints did not require therapeutic interventions, such as changes in type of mask interface, changes in PAP modality/ pressure/oxygen, new medication prescription such as a sleep hypnotic, or a change from PAP therapy to different mode such as oral appliance or surgery—all therapeutic changes requiring a licensed provider. Thus, the presence of specific subjective complaints increased the likelihood of a necessary clinical intervention at the follow-up visit (OR 16.1 95% CI 7.6-34.5 p ≤ 0.001).
This is perhaps not a surprising conclusion. However, what about those patients who have no subjective complaints? We inspect their equipment and download compliance reports at all follow-up visits. Our data indicate that these objective findings contribute relatively rarely to the need for intervention in the absence of subjective complaints. Of the 115 patients without subjective complaints, only 20 (17.4%) were found to have objective findings, and 16 of those required therapeutic interventions. None of the 95 patients out of the total 180 without subjective symptoms or objective findings required therapeutic interventions. These data clearly show the importance of eliciting subjective symptoms, and that the needs of patient without symptoms may not require specialist intervention.
How do we assess for subjective complaints before the patient presents for their annual visit? With no other studies to address this issue, this is a prime area for research. Potential options include a pre-visit questionnaire via phone, internet patient portal, or mail. Recursive partitioning with retrospective validation identified age > 55 years, BMI < 40, and AHI > 12, along with subjective complaints as predictors for clinical intervention at the annual follow-up visit. However, whether these variables can be part of a predictive model to assess the need for clinical intervention and thereby assess the need for an annual follow-up visit will need to be studied prospectively and validated before it can be applied in clinical practice. Higher age and severity of OSA may be associated with comorbidities that can likely increase the need for interventions at annual follow-up visits. For example, it is unclear why a BMI < 40 should be predictive of therapeutic interventions.
At annual follow-up inclusive of compliance downloads and equipment inspection, our overall compliance was 74%, which is slightly higher than other studies.14,15 It is likely that our total patient compliance is much lower than the 74%, since we only included patients who kept routine annual follow-up visits. This may be related to closer monitoring within the first few weeks of PAP use that includes education by our trained nurses, addressing issues related to mask fitting and problems related to PAP. It is therefore possible that the higher adherence overall may have resulted in fewer clinical interventions in the annual follow-up visit, as most issues and problems may have been addressed in the first few weeks of PAP use.
There are several limitations to our retrospective study. Our findings, like all retrospective studies, are likely biased by sample selection. Patients included in the study data were abstracted through a process based on ICD-9 coding. In spite of selecting patients with ICD-9 code 327.23, during chart review we discovered patients with complex sleep apnea in our data set. These patients were secondarily excluded. Additionally, only 22% of the patients (n = 716) with confirmed diagnosis of OSA by PSG were found to have an annual follow up-visit. The likely explanation for the attrition in the number of annual follow up visits are: (a) patients may not have been scheduled for their follow up appointments within the time frame specified by our study parameters (8-18 months), (b) patients may have missed their scheduled appointments, (c) some of our patients who travel long distances probably had their annual follow-up visits closer to home with their physicians, (d) patients may have stopped using their PAP, or non-adherent to the recommendation, (e) patients may not have received recommendation/prescription for the annual visit. The higher than usual compliance rate with PAP therapy at the annual follow-up visit may also be related to the biased sample of patients returning to the clinic for follow-up, which may also affect the actual number of patients requiring a clinical intervention at the annual follow-up visit. Since the likelihood of a therapeutic intervention was not influenced by the years of experience using PAP, it may be that we predominantly were examining established PAP users rather than those who had struggled more to use PAP. The selection bias problems can only be addressed by a prospective study. Additionally, our study population is over 90% Caucasian. Future studies based on patient samples drawn from a more representative sample of the US population could help improve validity.
Our findings may not be generalizable to other sleep centers as this is a single center study that was conducted in an academic sleep center and consisted of highly selected patients who kept their annual scheduled follow-up visits. We classified our interventions as “therapeutic” and “administrative”; this distinction was based on our resources and expertise available at our center and may not necessarily apply to other centers. We chose “administrative” to cover transactions that in our setting were predominantly clerical or that required little or no medical decision-making, and “therapeutic” to describe those transactions that would likely require assessment and medical decision-making. Finally, this study does not allow assessment of the impact of reassurance and minimal education that may have taken place during predominantly administrative visits on long-term adherence. Such factors as patient-doctor relationship, re-emphasis of the importance of managing OSA in the broader clinical picture, and other intangibles are not represented in retrospective assessments and could conceivably be significant in establishing long-term PAP adherence. Despite these limitations, our data show an opportunity to better select which patients would most benefit from routine face-to-face follow up.
CONCLUSION
OSA is a chronic condition that requires ongoing follow-up. However, PAP follow-up may not require face-to-face visits in all cases. Future studies looking at screening tools to assess predictive factors prospectively on this group of OSA patients will help to determine the need for and timing of face-to-face follow-up visits. Avoiding unnecessary while ensuring appropriate annual clinic visits will improve resource utilization and result in increased value of care.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was partially supported by Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Sanders MH, Kern N. Obstructive sleep apnea treated by independently adjusted inspiratory and expiratory positive airway pressures via nasal mask. Physiologic and clinical implications. Chest. 1990;98:317–24. doi: 10.1378/chest.98.2.317. [DOI] [PubMed] [Google Scholar]
- 2.Giles TL, Lasserson TJ, Smith BJ, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;(1):CD001106. doi: 10.1002/14651858.CD001106.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Fleury B, Rakotonanahary D, Tehindrazanarivelo AD, Hausser-Hauw C, Lebeau B. Long-term compliance to continuous positive airway pressure therapy (nCPAP) set up during a split-night polysomnography. Sleep. 1994;17:512–5. doi: 10.1093/sleep/17.6.512. [DOI] [PubMed] [Google Scholar]
- 4.Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147:887–95. doi: 10.1164/ajrccm/147.4.887. [DOI] [PubMed] [Google Scholar]
- 5.Rauscher H, Popp W, Wanke T, Zwick H. Acceptance of CPAP therapy for sleep apnea. Chest. 1991;100:1019–23. doi: 10.1378/chest.100.4.1019. [DOI] [PubMed] [Google Scholar]
- 6.Engleman HM, Martin SE, Douglas NJ. Compliance with CPAP therapy in patients with the sleep apnoea/hypopnoea syndrome. Thorax. 1994;49:263–6. doi: 10.1136/thx.49.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nino-Murcia G, McCann CC, Bliwise DL, Guilleminault C, Dement WC. Compliance and side effects in sleep apnea patients treated with nasal continuous positive airway pressure. West J Med. 1989;150:165–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Pepin JL, Leger P, Veale D, Langevin B, Robert D, Levy P. Side effects of nasal continuous positive airway pressure in sleep apnea syndrome. Study of 193 patients in two French sleep centers. Chest. 1995;107:375–81. doi: 10.1378/chest.107.2.375. [DOI] [PubMed] [Google Scholar]
- 9.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29:375–80. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 10.Gay P, Weaver T, Loube D, Iber C. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29:381–401. doi: 10.1093/sleep/29.3.381. [DOI] [PubMed] [Google Scholar]
- 11.Positive Airway Pressure (PAP) devices. Complying with documentation and coverage requirements. Centers for Medicare and Medicaid Services. [Accessed December, 2010]. http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/PAP_DocCvg_Factsheet_ICN905064.pdf.
- 12.Epstein LJ, Kristo D, Strollo PJ, Jr., et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–76. [PMC free article] [PubMed] [Google Scholar]
- 13.James KE, White RF, Kraemer HC. Repeated split sample validation to assess logistic regression and recursive partitioning: an application to the prediction of cognitive impairment. Stat Med. 2005;24:3019–35. doi: 10.1002/sim.2154. [DOI] [PubMed] [Google Scholar]
- 14.Galetke W, Puzzo L, Priegnitz C, Anduleit N, Randerath WJ. Long-term therapy with continuous positive airway pressure in obstructive sleep apnea: adherence, side effects and predictors of withdrawal–a ‘real-life’ study. Respiration. 2011;82:155–61. doi: 10.1159/000322838. [DOI] [PubMed] [Google Scholar]
- 15.Kohler M, Smith D, Tippett V, Stradling JR. Predictors of long-term compliance with continuous positive airway pressure. Thorax. 2010;65:829–32. doi: 10.1136/thx.2010.135848. [DOI] [PubMed] [Google Scholar]


