Abstract
Background
Measures of social context, such as marriage and religious participation, are associated with remission from alcohol use disorders (AUD) in population-based and treatment samples, but whether these associations hold among individuals at high familial risk for AUD is unknown. This study tests associations of measures of social context and treatment with different types of remission from DSM-5 AUD in a high-risk sample.
Methods
Subjects were 686 relatives of probands (85.7% first-degree) who participated in a high-risk family study of alcohol dependence. All subjects met criteria for AUD at baseline and were re-interviewed 5 years later. Follow-up status was categorized as persistent AUD, high-risk drinking, remitted low-risk drinking, and abstinence. Social context measures were defined as stable or changing from baseline to follow-up, and their bivariate and multivariate associations with follow-up status were tested.
Results
At follow-up, 62.8% of subjects had persistent AUD, 6.4% were high-risk drinkers, 22.2% were remitted low-risk drinkers, and 8.6% were abstinent. Birth of first child during the interval was the only measure of social context associated with remitted low-risk drinking and was significant for women only. Abstinent remission was characterized by being stably separated or divorced for women, new marriage for both sexes, experiencing low levels of family support and high levels of friend support, and receiving treatment. High-risk drinkers were more likely than individuals with persistent AUD to have a stable number of children and to have been recently unemployed.
Conclusions
The social contexts accompanying different types of remission in this high-risk sample resemble those found in population-based and clinical samples. Low-risk drinkers resemble natural remitters from population-based samples who change their drinking habits with life transitions. Abstainers resemble clinical samples in marital context, support from friends, and treatment. High-risk drinkers appear to continue to experience negative consequences of heavy drinking.
Keywords: alcohol use disorder, social context, treatment, remission, recovery
Introduction
The role of social connection in remission from alcohol use disorders (AUDs) has been documented in a wide variety of samples. In treatment samples, alcohol-specific supports such as Alcoholics Anonymous (AA) or other social networks that support recovery are associated with reduced alcohol consumption and lower rates of relapse (Ellis et al., 2004; Longabaugh et al., 2010; Project MATCH Research Group, 1998; Stout et al., 2012). In population-based samples, social connections not specific to alcohol use, such as marriage and religious participation, are associated with better drinking outcomes in both treated and untreated individuals (Avalos and Mulia, 2012; Dawson et al., 2012; Dawson et al., 2005; Kelly et al., 2011a). The consistency of these findings across samples with varying levels of AUD severity and treatment experience (Fein and Landman, 2005) suggests that social connection is a key component of recovery regardless of severity of alcohol problems.
In population-based samples, measures of social context like marriage can mark significant life transitions that accompany natural reductions in drinking (Dawson et al., 2006), consistent with evidence that more than 50% of individuals who remit from AUD do so without formal treatment (Cunningham et al., 2000; Sobell et al., 1996). In clinical samples, similar measures are associated with treatment outcome and can also mark changes associated with recovery (reviewed in Adamson et al., 2009). Whether this relationship between social context and remission holds in samples with high familial risk for AUD is unknown. The increased genetic and environmental risks for AUD which accompany high-risk samples (e.g., Jacob et al., 2003) might decrease the relative salience of social context for remission. Increased familial risk for AUD, however, seems not to contribute to decreased likelihood of remission. In 40 years of longitudinal birth cohort data from sons of fathers with AUDs, for example, only 18 of 361 carefully selected, biologically-based, premorbid predictors of alcohol dependence were associated with failure to remit, suggesting remission is subject to social influences even in high-risk samples (Penick et al., 2010). In the current study we examine more definitively whether measures of social context are associated with remission in individuals from families with high risk for alcoholism, and whether social context differs by type of remission. Our aims were to (1) examine AUD status at follow-up among individuals with AUD at baseline who were re-interviewed 5 years later, and (2) examine measures of social context and treatment as a function of AUD status at follow-up.
Materials and Methods
Participants
Subjects for this study were 686 relatives of probands, from 460 families, from the Collaborative Study on the Genetics of Alcoholism (COGA) who met criteria for DSM-5 alcohol use disorder (AUD; American Psychiatric Association, 2013) in the year preceding the baseline interview and who participated in a follow-up interview 5 years later. As described elsewhere (Bucholz et al., 1996; Culverhouse et al., 2005; Nurnberger et al., 2004; Reich, 1996), COGA is a multi-site, high-risk family study of alcohol dependence. Probands for COGA were recruited from treatment settings at 6 sites across the United States and were required to meet criteria for DSM-III-R-defined alcohol dependence (American Psychiatric Association, 1987) and Feighner definite alcoholism (Feighner et al., 1972). Probands were also required to have at least two first-degree relatives living in one of the COGA catchment areas available for study. All of these first-degree relatives were sought for baseline interviews and for follow-up interviews approximately 5 years later. The protocol was approved by the institutional review board at each site, and written informed consent was obtained from all subjects. Of the subjects studied in the present report, 85.7% were first-degree relatives of the proband (father, mother, sibling, offspring). The sample was 80.0% White, 12.5% African American, 4.5% Hispanic, and 3.0% was classified as Native American, Pacific Islanders and “other.”
Assessment
The Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA) was used to interview all subjects. The SSAGA is a comprehensive diagnostic interview with documented reliability and validity (Bucholz et al., 1994; Bucholz et al., 1995; Hesselbrock et al., 1999) developed specifically for the COGA study and accommodates several diagnostic systems, including information that allowed classification of AUD by the recent Fifth Diagnostic and Statistical Manual (DSM5) of the American Psychiatric Association (2013).
Alcohol use disorder
Lifetime AUD was defined as at least 2 symptoms occurring within any 12-month period (American Psychiatric Association, 2013). Current AUD at baseline was defined as AUD within one year of interview, based on reported age at the most recent symptom. At follow-up, AUD status was determined using recency data for each symptom; persistent AUD required at least one symptom to be present within a year of this second interview.
Remission categories and high-risk drinking
Remission from AUD was defined in accordance with DSM-5 sustained remission as having met none of the AUD criteria for at least one full year at the follow-up interview. Remitted individuals who reported not having drunk any alcohol for at least one full year were classified as “abstinent remitted”. Individuals who were still drinking were considered “remitted low-risk drinkers” if their current alcohol consumption fell within NIAAA-defined low-risk drinking guidelines (men: no more than 4 drinks in one day and no more than 14 drinks per week; women: no more than 3 drinks in one day and no more than 7 drinks per week ; National Institute on Alcohol Abuse and Alcoholism, 2010). Finally, subjects with no current AUD symptoms but whose alcohol consumption exceeded low risk drinking were classified as high-risk drinkers. Follow-up status was represented by a 4-level variable: (1) persistent AUD (1 or more current AUD symptoms), (2) high-risk drinking, (3) remitted low-risk drinking, and (4) abstinent remitted. Although DSM-5 criteria state that craving may be present in remission, none of the remitted subjects in this sample reported craving.
Alcohol treatment
A 3-level variable representing individuals who had no treatment, who received professional treatment with or without AA attendance (cell counts were too small to create a separate category for professional treatment only) or who received AA-only was created for baseline and follow-up based on lifetime history at each assessment. Individuals whose treatment category was the same at both time points were categorized as stable for that treatment category. Individuals who endorsed no treatment at baseline and AA at follow-up were coded as receiving “new AA-only” and those who endorsed no treatment or AA-only at baseline and professional treatment at follow-up were coded as having received “new professional treatment.”
Marital status
Individuals who reported the same marital status at baseline and follow-up were coded as being (1) stably married, (2) stably separated, divorced, or widowed (only 1.0% of the sample reported being widowed at either phase; given the small number of individuals affected, this group was combined with those reporting separation or divorce), or (3) stably never married. Individuals who had never married or were separated, divorced, or widowed at baseline, and who at follow-up were married were coded as newly married. Individuals who were married at baseline and separated, divorced or widowed at follow-up were coded as newly separated or divorced.
Children
Variables representing individuals who reported the same number of children at both time points (including no children), or who had their first or an additional child between assessments, were created.
Religious attendance
At each assessment, respondents who indicated a religious preference were asked “In the past twelve months how many times did you attend religious services?” Variables representing attendance fewer than 12 times, 12 to 51 times, and 52 or more times (at least weekly) were created. These frequencies were used to create variables representing stable, increasing, and decreasing attendance frequency from baseline to follow-up.
Social support
Two questionnaires about the perceived level of social support received from family and friends were completed at the follow-up assessment (Procidano and Heller, 1983). Each questionnaire had 20 questions with responses on a 4-level Likert scale ranging from “Generally false” to “Generally true,” with higher scores indicating higher levels of support. Representative questions were “I have a deep sharing relationship with a number of members of my family/friends,” “I rely on my family/friends for emotional support.” Missing data for 93 individuals were imputed at the median score (60 for both family and friend support), and a dummy variable was created to represent individuals with missing data. This variable was not significantly associated with follow-up status, indicating that individuals without questionnaire data were not disproportionately from one category. Binary variables representing above-median scores on family and friend support were used in analyses.
Drug use and nicotine habitual use or dependence
Illicit drug use was defined as lifetime use 11 or more times of marijuana, cocaine, stimulants, sedatives, opiates, PCP, hallucinogens, solvents, or other illicit drugs. Not all wave 1 participants were assessed for nicotine dependence (Bierut et al., 2008), therefore habitual smoking (at least 20 cigarettes daily for at least 6 months) was used as the nicotine use measure at wave 1. At wave 2, all participants were assessed for nicotine dependence. For both drug and nicotine measures, current use was defined as occurring within the last year. Remitted use at follow-up was divided into 2 categories based on most recent use from 1 to 5 years ago or more than 5 years ago.
Data analysis
Bivariate associations with remission status at follow-up for demographics, alcohol and drug use, social measures and treatment were tested using multinomial logistic regression, with current AUD as the reference group. Variables from bivariate analyses with p-values of .25 or less in relation to the outcome category being evaluated were selected for initial inclusion in the multivariate model (Hosmer and Lemeshow, 2000). Multivariate models were developed using logistic regression, rather than multinomial regression, because bivariate models showed that few variables were associated with all outcome categories; therefore a multinomial model would not provide a good fit to the data. Separate logistic regression models were fit for high-risk drinking, remitted low-risk drinking, and abstinence, using persistent AUD as the reference group for each. This method approximates a multinomial model in cases such as this where covariates are significant in some categories but not in others (Hosmer and Lemeshow, 2000). Variables that were not associated with the outcome category and that did not contribute to model fit based on comparison of fit statistics were eliminated from the model if they were not necessary for interpretation. Once final models were identified, interactions of gender with marital status were tested, based on evidence that marriage is differentially associated with gender in individuals with AUDs (Schneider et al., 1995), and that women who are regular drinkers are more likely than their male counterparts to select partners with alcohol dependence (Agrawal et al., 2006). All statistical tests were adjusted for familial clustering using the Huber-White robust variance estimator in the Stata statistical program (StataCorp, 2009).
Results
Remission
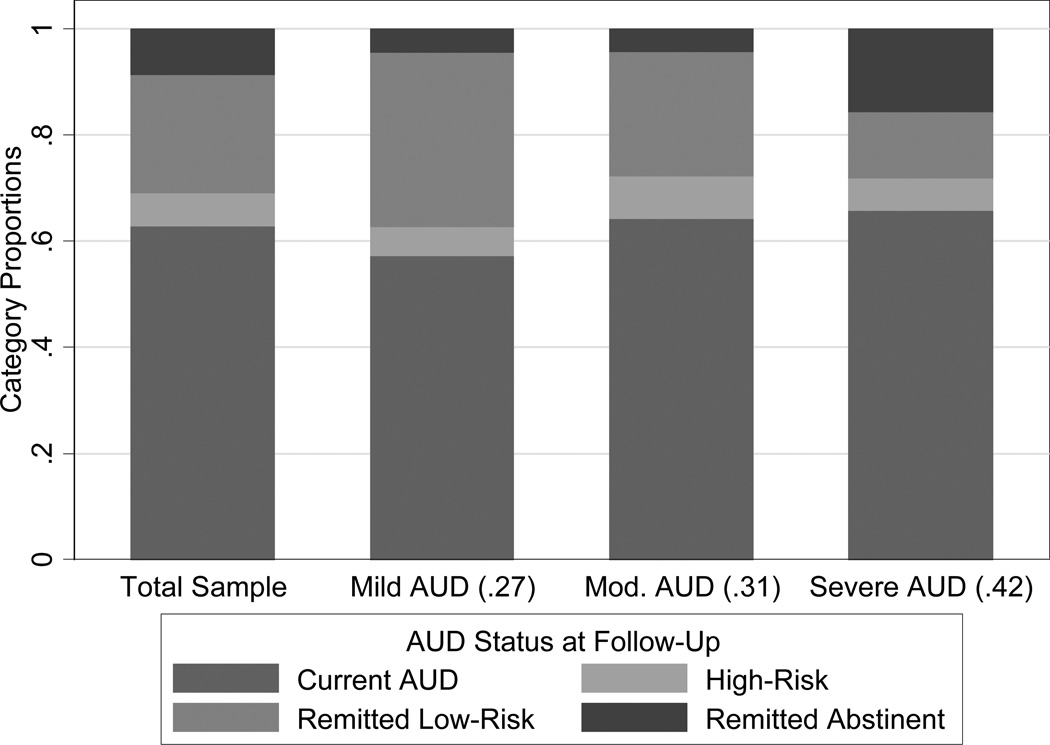
At follow-up, 30.8% of the sample was remitted. Remitted low-risk drinking was more prevalent than abstinent remission (22.2% and 8.6%, respectively), and high-risk drinkers comprised 6.4% of the sample (Figure 1). Thirty-seven percent of individuals with mild lifetime AUD severity at baseline (2–3 symptoms) had remitted by follow-up; most were remitted low-risk drinkers. Individuals with moderate (4–5 symptoms) and severe (6–11 symptoms) lifetime severity at baseline had similar remission rates at follow-up (27.8% and 28.0%, respectively) but differed in remission type, with low-risk drinking more common among individuals with moderate than severe AUD (23.6% versus 12.3%, respectively; X2(1) = 15.0, p<.01), and abstinence more common among individuals with severe than moderate AUD (15.7% versus 4.2%, respectively; X2(1) = 12.5, p<.01).
Figure 1.
Proportion of sample with mild (2–3 symptoms), moderate (4–5 symptoms) and severe (6 or more symptoms) lifetime AUD at baseline in parentheses.
AUD/Remission Status at Follow-Up in Total Sample and by Lifetime Severity at Baseline
Bivariate results
Demographics and substance use
Compared to individuals with persistent AUD, remitted low-risk drinkers were more likely to be female (Table 1). The persistent AUD group was youngest, and the mean age gradually increased from high-risk drinkers to remitted low-risk drinkers to abstainers. All non-persistent groups began regular drinking (i.e., once a month or more for at least 6 months) at a significantly later age than the persistent AUD group. Compared to individuals with persistent AUD, remitted low-risk drinkers had fewer lifetime AUD symptoms and fewer years from onset to recency of AUD, and abstinent individuals had more lifetime symptoms. Last week’s alcohol consumption among remitted low-risk drinkers decreased from baseline to follow-up, and at follow-up was well within low-risk drinking guidelines (National Institute on Alcohol Abuse and Alcoholism, 2010). A majority of all groups reported lifetime illicit drug use. Current drug use was highest in the persistent AUD group and was significantly lower in the remitted low-risk drinking and abstinent groups. High-risk drinkers and abstainers were more likely than the persistent AUD group to have remitted from drug use more than 5 years before the follow-up. Abstainers had the highest rate of lifetime nicotine habitual use or dependence (72.9%) and remitted low-risk drinkers the lowest (40.8%). Current nicotine habitual use or dependence was significantly lower among high-risk drinkers and remitted low-risk drinkers than among individuals with persistent AUD. Remitted low-risk drinkers were less likely to have remitted within the 5 years before follow-up, and abstainers were more likely to have remitted more than 5 years previous.
Table 1.
Demographic, alcohol and drug use characteristics of individuals with AUD at baseline, by remission status at follow-up
| Status at Follow-Up | ||||
|---|---|---|---|---|
| Remitted | ||||
| Persistent AUD R |
High-Risk Drinkers |
Low-Risk Drinkers |
Abstinent | |
| N=431 | N=44 | N=152 | N=59 | |
| Female,% | 37.3 | 47.7 | 53.9‡ | 45.8 |
| African American,% | 13.2 | 13.6 | 11.8 | 8.5 |
| Age at baseline, M(SD) | 30.5 (9.5) | 31.3 (9.6) | 32.2 (10.8) | 35.4 (10.5)‡ |
| Age regular drinking, M(SD) | 16.8 (3.4) | 18.0 (5.1)† | 17.5 (3.3)† | 17.9 (5.3) |
| Age AUD onset, M(SD) | 19.5 (5.7) | 19.7 (6.3) | 20.1 (5.4) | 20.9 (7.1) |
| AUD symptoms, lifetime, M(SD) | 6.5 (2.8) | 5.9 (2.8) | 4.8 (2.5)‡ | 8.5 (2.7)‡ |
| Years from AUD onset to AUD recency, % | ||||
| < 15 years R | 46.4 | 61.4 | 69.7 | 44.1 |
| 15 or more years | 53.6 | 38.6 | 30.3‡ | 55.9 |
| Drinks last week at baseline and follow-up, M(SD)1 | ||||
| Male, baseline | 20.4 (22.5) | 21.6 (21.4) | 11.5 (22.9)‡ | 18.5 (25.8) |
| Male, follow-up | 19.0 (21.7) | 13.8 (17.2) | 3.2 (3.9)‡ | 0 (0)a |
| Female, baseline | 13.6 (22.2) | 7.4 (8.6) | 5.7 (8.0)‡ | 4.5 (8.4)‡ |
| Female, follow-up | 10.1 (14.5) | 4.3 (4.9)† | 1.1 (1.6)‡ | 0 (0)a |
| Illicit Drug Use 2, % | ||||
| NoneR | 25.5 | 22.8 | 44.0 | 25.4 |
| Current (within 1 year) | 41.5 | 25.0 | 14.5‡ | 11.9‡ |
| Remitted (more than 1 year to 5 years ago) | 19.0 | 20.4 | 13.2‡ | 28.8 |
| Remitted (more than 5 years ago) | 13.9 | 31.8† | 28.3 | 33.9† |
| Nicotine Habitual Use or Dependence, %3 | ||||
| NoneR | 41.1 | 43.2 | 59.2 | 27.1 |
| Current (within 1 year) | 26.9 | 4.5† | 13.8‡ | 30.5 |
| Remitted (more than 1 year to 5 years ago) | 19.7 | 31.8 | 11.2‡ | 22.0 |
| Remitted (more than 5 years ago) | 12.3 | 20.4 | 15.8 | 20.3† |
Note: High-risk drinking, men: >4 drinks/day or >14 drinks/week; women: >3 drinks/day or >7 drinks/week; Low-risk drinking = drinking below high-risk levels.
log-transformed for regression;
inestimable due to zero cell;
drug use=lifetime use 11 or more times of marijuana, cocaine, stimulants, sedatives, opiates, PCP, hallucinogens, solvents, combination or other illicit drugs; drug use history = most recent drug use at least one year ago;
nicotine habitual use (20 cigarettes or more daily for at least 6 months) was used in wave 1 data, since nicotine dependence added late in wave 1 and thus was not available for all participants;
Significance tests conducted using multinomial logistic regression with AUD as reference category and robust variance estimator to correct for clustering of family data.
= reference category;
p ≤ .05,
p ≤ .01
Social context
High-risk drinkers were more likely than their counterparts with persistent AUD to have increased their religious attendance between baseline and follow-up (Table 2). Compared to the persistent AUD group, remitted low-risk drinkers were more likely to be stably or newly married, to have had a first child since baseline, to report stable religious attendance and higher levels of family support. The abstinent group, relative to the persistent AUD group, was more likely to be separated /divorced (stable or new), to have a stable number of children or an additional child since baseline, and to report being stably unemployed since baseline.
Table 2.
Social context measures and alcohol treatment at follow-up among individuals with past-year AUD at baseline, by follow-up remission status
| Status at Follow-Up | ||||
|---|---|---|---|---|
| Remitted | ||||
| Persistent AUD |
High-Risk Drinkers |
Low-Risk Drinkers |
Abstinent | |
| N=431 | N=44 | N=152 | N=59 | |
| Marital status | ||||
| Stable 1 | ||||
| Never MarriedR | 40.8 | 27.3 | 25.7 | 22.0 |
| Married | 21.6 | 25.0 | 31.6‡ | 22.0 |
| Separated/Divorced/Widowed | 15.1 | 18.2 | 11.8 | 28.8‡ |
| New 2 | ||||
| Marriage | 13.0 | 20.4 | 24.3‡ | 13.6 |
| Separated/Divorced/Widowed | 9.5 | 9.1 | 6.6 | 13.6† |
| Children | ||||
| Stable | ||||
| No childrenR | 37.8 | 29.5 | 27.6 | 20.3 |
| One or more children | 39.7 | 54.5 | 42.8 | 61.0‡ |
| First child since baseline | 11.1 | 6.8 | 21.7‡ | 3.4 |
| Additional child since baseline | 11.4 | 9.1 | 7.9 | 15.2† |
| Employment | ||||
| Stably/newly employedR | 77.0 | 68.2 | 77.6 | 71.2 |
| Stably unemployed | 12.8 | 13.6 | 11.2 | 23.7† |
| Newly unemployed | 10.2 | 18.2 | 11.2 | 5.1 |
| Religious attendance | ||||
| Stable | ||||
| NoneR | 31.3 | 18.2 | 21.7 | 23.7 |
| Any (less than monthly to weekly or more) | 27.8 | 25.0 | 32.2‡ | 22.0 |
| Increased | 20.9 | 34.1† | 23.7 | 30.5 |
| Decreased | 20.0 | 22.7 | 22.4 | 23.7 |
| High perceived support, Family3 | 40.1 | 45.4 | 49.3† | 28.8 |
| High perceived support, Friends3 | 39.3 | 36.4 | 46.7 | 52.5 |
| Alcohol treatment history | ||||
| Stable | ||||
| No treatmentR | 56.8 | 59.1 | 75.7 | 25.4 |
| AA-only | 3.0 | 4.5 | 2.6 | 10.2‡ |
| Professional treatment with/without AA attendance | 22.9 | 22.7 | 12.5‡ | 40.7‡ |
| New | ||||
| First AA attendance (no professional treatment) | 6.7 | 6.8 | 6.6 | 6.8 |
| First professional treatment | 10.4 | 6.8 | 2.6‡ | 16.9‡ |
stable = same at both waves
new = changed between baseline and follow-up
reported at follow-up only
Significance tests conducted using multinomial logistic regression with AUD as reference category and robust variance estimator to correct for clustering of family data.
= reference category
p ≤ .05,
p ≤ .01
At follow-up, 58.4% of the sample had never accessed alcohol treatment, 31.2% had accessed professional treatment (with or without AA attendance), and 10.4% had attended AA without professional treatment. Relative to the persistent AUD group, the abstinent group was more likely to have attended AA-only prior to baseline and to have accessed professional treatment before or after the baseline interview, and the low-risk remitted group was less likely to have accessed professional treatment (Table 2).
Multivariate results
Multivariate results are shown in Table 3 and described below for each outcome category. Persistent AUD at follow-up is the reference group for all categories.
Table 3.
Results of multivariate equations showing correlates of high-risk drinking, remitted low-risk drinking, and abstinent remission
| High–Risk Drinking versus Persistent AUD |
Remitted Low–Risk Drinking versus Persistent AUD |
Abstinent Remission versus Persistent AUD |
|
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Social context | |||
| Stable separation/divorce, Women | NS | NS | 6.0 (1.8–19.7) |
| Men | NS | NS | 0.5 (0.2–1.7) |
| New marriage | 1.9 (0.7–4.8) | NS | 3.0 (1.1–8.2) |
| New separation/divorce | NS | NS | 2.9 (0.9–9.1) |
| Stable number children | 2.5 (1.1–5.7) | NS | NS |
| New first child, Women | 0.5 (0.1–1.8) | 4.4 (1.8–10.6) | 0.2 (0.05–0.64) |
| Men | 1.1 (0.5–2.3) | ||
| New additional child | NS | NS | NS |
| Increased religious attendance | 2.3 (0.9–5.3) | NS | 1.8 (0.8–4.0) |
| Decreased religious attendance | 1.7 (0.7–4.4) | 1.3 (0.6–3.0) | |
| High family support 1 | NS | NS | 0.4 (0.2–0.9) |
| High friend support 1 | NS | NS | 3.1 (1.3–7.3) |
| Newly unemployed | 2.4 (1.0–5.7) | NS | NS |
| Alcohol treatment | |||
| Stable AA-only | NS | NS | 9.1 (2.7–31.0) |
| Stable professional treatment | NS | NS | 2.5 (1.0–6.4) |
| New AA-only | NS | NS | 2.3 (0.7–7.8) |
| New professional treatment | NS | NS | 3.2 (1.1–9.7) |
| Alcohol/drug use covariates | |||
| Severe lifetime AUD (≥ 6 symptoms) | 0.8 (0.4–1.8) | 0.5 (0.3–0.7) | 3.9 (1.6–9.4) |
| 15 or more years from onset to recency | 0.2 (0.1–0.5) | 0.2 (0.1–0.4) | 0.4 (0.2–0.9) |
| Current drug use | 1.2 (0.4–3.4) | 0.4 (0.2–0.7) | 0.2 (0.1–0.5) |
| Remitted drug use, 1–5 years | 1.7 (0.6–4.8) | 0.7 (0.3–1.3) | 1.5 (0.6–3.7) |
| Remitted drug use, > 5 years | 4.2 (1.6–11.1) | 1.8 (1.0–3.3) | 2.7 (1.0–6.9) |
| Current nicotine dependence | 0.1 (0.0–0.7) | 0.5 (0.2–1.0) | 0.9 (0.4–2.0) |
NS = parameter not significant, not estimated in multivariate model;
above median; adjusted for age, ethnicity, and gender, significant associations (p ≥ .05) bolded
High-risk drinking
High-risk drinkers were more likely to have a stable number of children and to have become unemployed since baseline, compared to individuals with persistent AUD. They also had a shorter duration of AUD, were more likely to have quit using drugs more than 5 years previous, and were less likely to have current nicotine dependence.
Remitted low-risk drinking
Women (but not men) who were remitted low-risk drinkers were more likely than women with persistent AUD to have had a first child between the baseline and follow-up interviews (26.8% and 7.4%, respectively). The women who had a first child were significantly younger than those who did not (age at baseline, M (min, max) = 23.8 (18, 36) and 33.1 (18, 55), t(80) = 4.6, p < .001). Compared to individuals with persistent AUD, remitted low-risk drinkers also had fewer lifetime AUD symptoms, fewer years from AUD onset to recency, were less likely to be current drug users and more likely to have remitted from drug use more than 5 years ago, and were less likely to have remitted from nicotine habitual use or dependence within the last 5 years. The associations of stable and new marriage, religious attendance, and family support with remitted low-risk drinking were non-significant in the multivariate model.
Abstinence
Abstinent women were more likely than women with persistent AUD to be stably separated or divorced (44.4% and 18.6%, respectively); this was not true for men. Men and women in abstinent remission were more likely than those with persistent AUD to be newly married and less likely to have had a first child during the follow-up interval. They reported lower levels of support from family and higher levels of support from friends than individuals with persistent AUD. They had greater AUD severity, a shorter duration of AUD, were less likely to be current drug users, and more likely to have remitted from drug use more than 5 years ago. A history of AA attendance or professional treatment at baseline, and new professional treatment during the interval, were associated with abstinent remission.
Discussion
We examined remission, measures of social context and treatment five years after a current AUD diagnosis in a sample of men and women from families with histories of alcohol dependence. Thirty-one percent of the sample was remitted at follow-up and 6.4% of the sample had no AUD symptoms but was drinking at high-risk levels. The most common form of remission was low-risk drinking, but among individuals with greatest AUD severity, abstinence was more common. The social contexts accompanying high-risk drinking and remitted low-risk drinking differed from the context of persistent AUD, with high-risk drinkers more likely to have a stable number of children and to have become unemployed during the follow-up interval, and female remitted low-risk drinkers more likely to have had a first child during the interval. The context of abstinent remission showed the greatest differentiation from persistent AUD, with differences in marital status, children, family and friend support, and treatment.
Lifetime AUD severity and rates of treatment were greatest among abstinent individuals and lowest among remitted low-risk drinkers, consistent with evidence that abstinence is a more common form of remission among individuals with severe AUD, and that moderate drinking is the most common form of remission among untreated individuals (Dawson et al., 2005; Sobell et al., 1996). Remission rates in this high-risk sample were higher than those found among alcohol dependent individuals from a population-based sample who were re-interviewed 3 years after meeting criteria for current alcohol dependence (AD; Dawson et al., 2012). In that study, only 11% of the sample was remitted at follow-up. The higher rate of remission in this study may be due to the fact that remission was based on DSM-5 AUD, which has a lower severity threshold than DSM-IV AD, and therefore a lower threshold for remission (i.e., remission of 2, rather than 3, symptoms). Also, related to the sample’s high-risk status, each individual in the current study had at least one family member with lifetime AD who had accessed professional treatment, which may have influenced them to consider reducing their own alcohol use. This possibility is consistent with evidence that the shared familial environment accounts for a significant proportion of variance in treatment seeking (True et al., 1996). In the current study, individuals with no current AUD symptoms who were drinking at risk levels were differentiated from individuals with persistent AUD. In the study by Dawson et al. (2012), these individuals were included in the no recovery group, comprising about 8% of that group (D.A. Dawson, personal communication, July 24, 2013). Designating them as a separate category in the current study revealed that although they were drinking at high-risk levels, they differed in substantive ways from individuals with current AUD, having a shorter duration of AUD, higher rates of remitted drug use and lower rates of current nicotine dependence.
Family context, represented by marital status and children, differentiated high-risk drinking and both types of remission from persistent AUD. A smaller proportion of the persistent AUD group had ever been married or had children compared to high-risk drinkers, remitted low-risk drinkers, and abstainers. This difference is consistent with evidence that heavy drinkers are more likely to delay marriage and children, or to remain single, than individuals who do not drink heavily (Chilcoat and Breslau, 1996; Waldron et al., 2008), or to transition out of heavy drinking as they adopt changing adult roles (Miller-Tutzauer et al., 1991). Similarly, the birth of first child among women who became remitted low-risk drinkers is consistent with adult role transitions and with natural recovery (Dawson et al., 2006; Russell et al., 2001; Sobell et al., 2000), suggesting a group of individuals adjusting their drinking habits to new roles, largely without formal treatment. Abstinent individuals were less likely to have a first child than individuals with AUD, possibly reflecting their older age and, also, the higher likelihood among women of being stably separated or divorced. The higher likelihood of stable separation or divorce among abstinent women, but not men, is consistent with findings which suggest that marriage is more beneficial for men with alcohol problems than similar women. In the current study, women who were separated or divorced at baseline, and stayed that way, were more likely than similar men to be abstinent at follow-up, suggesting that being single increased their chances of recovery from AUD. In a 5-year follow-up of problem drinking women, women who had been separated or divorced between assessments had reduced risk of alcohol problems at follow-up compared to those who remained married (Wilsnack et al., 1991). Similarly, evidence from treatment studies suggests that married men have better outcomes following treatment than unmarried men, whereas for women marriage increases the risk of relapse (reviewed in Walitzer and Dearing, 2006). These gender differences regarding the benefits of marriage for individuals attempting to recover from severe AUDs might be interpreted in light of evidence for positive assortative mating for alcohol use and dependence (Grant et al., 2007), with females more likely than males to choose a partner with a history of alcohol dependence (Agrawal et al., 2006). Investigations in more recent data are needed, however, since the rates of alcohol problems among women are increasing (Grucza et al., 2008) and rates of marriage are decreasing (Copen et al., 2012) in younger cohorts. Perhaps reflecting this shift, a recent meta-analysis of treatment studies found that marital status was a less salient predictor of treatment outcome when samples included included larger proportions of women, suggesting that increasing numbers of women entering treatment may shift the findings from previous research based in predominately male samples (Adamson et al., 2009).
Abstinent individuals reported lower levels of support from family and higher levels of support from friends than did individuals with persistent AUD. These differences may be related to the likelihood in this high-risk sample of active AUD in relatives. Individuals who became abstinent between baseline and follow-up may have distanced themselves from their families and cultivated friends who did not have drinking problems, or who were also trying to abstain, in order to maintain abstinence themselves. It is equally plausible that lower perceived family support is due to the respondent’s behavior, wherein objectionable alcohol-related behaviors alienated family members. Since social support was measured only at follow-up, and alcohol-specific support (e.g., support for remission) was not queried, we cannot examine change in support or determine whether support from friends is related to AA or treatment participation. Treatments designed specifically to increase support for abstinence in the social networks of individuals with AUDs result in drinking outcomes similar to or better than those attained with more traditional treatments (Litt et al., 2007; Litt et al., 2009; UKATT Research Team, 2005). Similarly, drinking outcomes are improved when individuals attend AA as an adjunct to professional treatment (Bond et al., 2003; Kelly et al., 2011b; Stout et al., 2012), consistent with the association of stable AA attendance with abstinence in the current study.
Limitations
This study must be interpreted with several limitations in mind. Foremost is the fact that the sample was selected for its high risk for AUD and therefore cannot be generalized to the larger population. However, the examination of the context of remission in a high-risk sample extends similar findings in population-based and clinical samples. The lack of recency ages for individual symptoms at baseline necessitated basing current AUD status at baseline on a single question about age at most recent symptom. Finally, the sample was primarily white with little power to detect ethnic differences.
Conclusions and future directions
The social contexts accompanying remission patterns in this high-risk sample resemble those found in population-based and clinical samples. Low-risk drinkers resemble natural remitters from population-based samples who change their drinking habits with life transitions. Abstainers resemble clinical samples in marital context, support from friends, and treatment, and high-risk drinkers appear to continue to experience negative consequences of heavy drinking. The social context of remission appears to be as important in this sample with high familial risk for AUD as it is in population-based and clinical samples. Future work will examine whether the remission status of family members is associated with the remission status of subjects, and how these relate to social context.
Acknowledgements
The Collaborative Study on the Genetics of Alcoholism (COGA), Principal Investigators B. Porjesz, V. Hesselbrock, H. Edenberg, L. Bierut, includes ten different centers: University of Connecticut (V. Hesselbrock); Indiana University (H.J. Edenberg, J. Nurnberger Jr., T. Foroud); University of Iowa (S. Kuperman, J. Kramer); SUNY Downstate (B. Porjesz); Washington University in St. Louis (L. Bierut, A. Goate, J. Rice, K. Bucholz); University of California at San Diego (M. Schuckit); Rutgers University (J. Tischfield); Texas Biomedical Research Institute (L. Almasy), Howard University (R. Taylor) and Virginia Commonwealth University (D. Dick). Other COGA collaborators include: L. Bauer (University of Connecticut); D. Koller, S. O’Connor, L. Wetherill, X. Xuei (Indiana University); Grace Chan (University of Iowa); S. Kang, N. Manz, M. Rangaswamy (SUNY Downstate); J. Rohrbaugh, J-C Wang (Washington University in St. Louis); A. Brooks (Rutgers University); and F. Aliev (Virginia Commonwealth University). A. Parsian and M. Reilly are the NIAAA Staff Collaborators.
We continue to be inspired by our memories of Henri Begleiter and Theodore Reich, founding PI and Co-PI of COGA, and also owe a debt of gratitude to other past organizers of COGA, including Ting-Kai Li, currently a consultant with COGA, P. Michael Conneally, Raymond Crowe, and Wendy Reich, for their critical contributions. This national collaborative study is supported by NIH Grant U10AA008401 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the National Institute on Drug Abuse (NIDA).
References
- Adamson SJ, Sellman JD, Frampton CMA. Patient predictors of alcohol treatment outcome: A systematic review. J Subst Abuse Treat. 2009;36:75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Heath AC, Grant JD, Pergadia ML, Statham DJ, Bucholz KK, Martin NG, Madden PA. Assortative mating for cigarette smoking and for alcohol consumption in female Australian twins and their spouses. Behav Genet. 2006;36:553–566. doi: 10.1007/s10519-006-9081-8. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, editor. Diagnostic and statistical manual of mental disorders (DSM-III-R) Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- American Psychiatric Association, editor. Diagnostic and statistical manual of mental disorders (DSM-5) Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Avalos LA, Mulia N. Formal and informal substance use treatment utilization and alcohol abstinence over seven years: Is the relationship different for blacks and whites? Drug Alcohol Depen. 2012;121:73–80. doi: 10.1016/j.drugalcdep.2011.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierut LJ, Stitzel JA, Wang JC, Hinrichs AL, Grucza RA, Xuei X, Saccone NL, Saccone SF, Bertelsen S, Fox L, Horton WJ, Breslau N, Budde J, Cloninger CR, Dick DM, Foroud T, Hatsukami D, Hesselbrock V, Johnson EO, Kramer J, Kuperman S, Madden PA, Mayo K, Nurnberger J, Jr, Pomerleau O, Porjesz B, Reyes O, Schuckit M, Swan G, Tischfield JA, Edenberg HJ, Rice JP, Goate AM. Variants in nicotinic receptors and risk for nicotine dependence. Am J Psychiatry. 2008;165:1163–1171. doi: 10.1176/appi.ajp.2008.07111711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and Alcoholics Anonymous on abstinence. J Stud Alcohol. 2003;64:579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JIJ, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: A report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Heath AC, Reich T, Hesselbrock VM, Kramer JR, Nurnberger JIJ, Schuckit MA. Can we subtype alcoholism? A latent class analysis of data from relatives of alcoholics in a multicenter family study of alcoholism. Alcohol Clin Exp Res. 1996;20:1462–1471. doi: 10.1111/j.1530-0277.1996.tb01150.x. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Hesselbrock VM, Shayka JJ, Nurnberger JIJ, Schuckit MA, Schmidt I, Reich T. Reliability of individual diagnostic criterion items for psychoactive substance dependence and the impact on diagnosis. J Stud Alcohol. 1995;56:500–505. doi: 10.15288/jsa.1995.56.500. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Alcohol disorders in young adulthood: Effects of transitions into adult roles. J Health Soc Behav. 1996;37:339–349. [PubMed] [Google Scholar]
- Copen CE, Daniels K, Vespa J, Mosher WD. First marriages in the united states: Data from the 2006–2010 national survey of family growth. Natl Health Stat Report. 2012:1–21. [PubMed] [Google Scholar]
- Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JIJ, Porjesz B, Schuckit MA, Reich T, Bierut LJ. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: An evaluation after 5 years. Arch Gen Psychiatry. 2005;62:753–760. doi: 10.1001/archpsyc.62.7.753. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Lin E, Ross HE, Walsh GW. Factors associated with untreated remissions from alcohol abuse or dependence. Addict Behav. 2000;25:317–321. doi: 10.1016/s0306-4603(98)00130-0. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Ruan WJ, Grant BF. Correlates of recovery from alcohol dependence: A prospective study over a 3-year follow-up interval. Alcohol Clin Exp Res. 2012;36:1268–1277. doi: 10.1111/j.1530-0277.2011.01729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Maturing out of alcohol dependence: The impact of transitional life events. J Stud Alcohol. 2006;67:195–203. doi: 10.15288/jsa.2006.67.195. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United states, 2001–2002. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Ellis B, Bernichon T, Yu P, Roberts T, Herrell JM. Effect of social support on substance abuse relapse in a residential treatment setting for women. Eval Program Plann. 2004;27:213–221. [Google Scholar]
- Feighner JP, Robins E, Guze SB, Woodruff RaJ, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry. 1972;26:57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- Fein G, Landman B. Treated and treatment-naive alcoholics come from different populations. Alcohol. 2005;36:19–26. [PMC free article] [PubMed] [Google Scholar]
- Grant JD, Heath AC, Bucholz KK, Madden PA, Agrawal A, Statham DJ, Martin NG. Spousal concordance for alcohol dependence: Evidence for assortative mating or spousal interaction effects? Alcohol Clin Exp Res. 2007;31:717–728. doi: 10.1111/j.1530-0277.2007.00356.x. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Bucholz KK, Rice JP, Bierut LJ. Secular trends in the lifetime prevalence of alcohol dependence in the united states: A re-evaluation. Alcohol Clin Exp Res. 2008;32:763–770. doi: 10.1111/j.1530-0277.2008.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA--a comparison with the SCAN. Addiction. 1999;94:1361–1370. doi: 10.1046/j.1360-0443.1999.94913618.x. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Appiled logistic regression. New York: John Wiley & Sons, Inc; 2000. [Google Scholar]
- Jacob T, Waterman B, Heath A, True W, Bucholz KK, Haber R, Scherrer J, Fu Q. Genetic and environmental effects on offspring alcoholism: New insights using an offspring-of-twins design. Arch Gen Psychiatry. 2003;60:1265–1272. doi: 10.1001/archpsyc.60.12.1265. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Pagano ME, Stout RL, Johnson SM. Influence of religiosity on 12-step participation and treatment response among substance-dependent adolescents. J Stud Alcohol Drugs. 2011a;72:1000–1011. doi: 10.15288/jsad.2011.72.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, Magill M, Tonigan JS. The role of alcoholics anonymous in mobilizing adaptive social network changes: A prospective lagged mediational analysis. Drug Alcohol Depen. 2011b;114:119–126. doi: 10.1016/j.drugalcdep.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry N. Changing network support for drinking: Initial findings from the network support project. J Consult Clin Psychol. 2007;75:542–555. doi: 10.1037/0022-006X.75.4.542. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Changing network support for drinking: Network support project 2-year follow-up. J Consult Clin Psychol. 2009;77:229–242. doi: 10.1037/a0015252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zywiak WH, O'malley SS. Network support as a prognostic indicator of drinking outcomes: The combine study. J Stud Alcohol Drugs. 2010;71:837–846. doi: 10.15288/jsad.2010.71.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Tutzauer C, Leonard KE, Windle M. Marriage and alcohol use: A longitudinal study of "maturing out". J Stud Alcohol. 1991;52:434–440. doi: 10.15288/jsa.1991.52.434. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Washington DC: US Department of Health and Human Services; 2010. [Accessed January 28, 2014]. Rethinking drinking: Alcohol and your health. Available at: http://pubs.niaaa.nih.gov/publications/RethinkingDrinking/Rethinking_Drinking.pdf. [Google Scholar]
- Nurnberger JI, Jr, Wiegand R, Bucholz K, O'connor S, Meyer ET, Reich T, Rice J, Schuckit M, King L, Petti T, Bierut L, Hinrichs AL, Kuperman S, Hesselbrock V, Porjesz B. A family study of alcohol dependence: Coaggregation of multiple disorders in relatives of alcohol-dependent probands. Arch Gen Psychiatry. 2004;61:1246–1256. doi: 10.1001/archpsyc.61.12.1246. [DOI] [PubMed] [Google Scholar]
- Penick EC, Knop J, Nickel EJ, Jensen P, Manzardo AM, Lykke-Mortensen E, Gabrielli WF. Do premorbid predictors of alcohol dependence also predict the failure to recover from alcoholism? J Stud Alcohol Drugs. 2010;71:685–694. doi: 10.15288/jsad.2010.71.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Procidano ME, Heller K. Measures of perceived social support from friends and from family: Three validation studies. Am J Community Psychol. 1983;11:1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcohol Clin Exp Res. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Reich T. A genomic survey of alcohol dependence and related phenotypes: Results from the collaborative study on the genetics of alcoholism (COGA) Alcohol Clin Exp Res. 1996;20:133A–137A. doi: 10.1111/j.1530-0277.1996.tb01763.x. [DOI] [PubMed] [Google Scholar]
- Russell M, Peirce RS, Chan AWK, Wieczorek WF, Moscato BS, Nochajski TH. Natural recovery in a community-based sample of alcoholics: Study design and descriptive data. Subst Use Misuse. 2001;36:1417–1441. doi: 10.1081/ja-100106958. [DOI] [PubMed] [Google Scholar]
- Schneider KM, Kviz FJ, Isola ML, Filstead WJ. Evaluating multiple outcomes and gender differences in alcoholism treatment. Addict Behav. 1995;20:1–21. doi: 10.1016/0306-4603(94)00037-y. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: Prevalence in two population surveys. Am J Public Health. 1996;86:966–972. doi: 10.2105/ajph.86.7.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Ellingstad TP, Sobell MB. Natural recovery from alcohol and drug problems: Methodological review of the research with suggestions for future directions. Addiction. 2000;95:749–764. doi: 10.1046/j.1360-0443.2000.95574911.x. [DOI] [PubMed] [Google Scholar]
- Statacorp. Stata statistical software: Release 11.0. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- Stout RL, Kelly JF, Magill M, Pagano ME. Association between social influences and drinking outcomes across three years. J Stud Alcohol Drugs. 2012;73:489–497. doi: 10.15288/jsad.2012.73.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- True WR, Heath AC, Bucholz KK, Slutske W, Romeis JC, Scherrer JF, Lin N, Eisen SA, Goldberg J, Lyons MJ, Tsuang MT. Models of treatment seeking for alcoholism: The role of genes and environment. Alcohol Clin Exp Res. 1996;20:1577–1581. doi: 10.1111/j.1530-0277.1996.tb01702.x. [DOI] [PubMed] [Google Scholar]
- UKATT Research Team. Effectiveness of treatment for alcohol problems: Findings of the randomised UK Alcohol Treatment Trial (UKATT) BMJ. 2005;331:541–544. doi: 10.1136/bmj.331.7516.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldron M, Heath AC, Bucholz KK, Madden PA, Martin NG. Alcohol dependence and reproductive onset: Findings in two australian twin cohorts. Alcohol Clin Exp Res. 2008;32:1865–1874. doi: 10.1111/j.1530-0277.2008.00771.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walitzer KS, Dearing RL. Gender differences in alcohol and substance use relapse. Clin Psychol Rev. 2006;26:128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Wilsnack SC, Klassen AD, Schur BE, Wilsnack RW. Predicting onset and chronicity of women's problem drinking: A five-year longitudinal analysis. Am J Public Health. 1991;81:305–318. doi: 10.2105/ajph.81.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]