Biofilms develop from the initial surface attachment of bacteria to structured ‘slime cities’ within which bacteria are up to 1000 times more resistant to antibiotic treatment.[1] Biofilms can cause failure for a wide range of medical devices including urinary and venous catheters.[1] Impaired device function is also associated with biofilm formation on water filters and ship hulls.[2,3] Controlling bacterial biofilms remains a key aim across many disciplines. One strategy to achieve this is the use of switchable materials[4,5] to trigger the removal of biofilms from surfaces,[6–10] which would enable intermittent ‘cleaning’ of surfaces or filters. In this study we apply two switchable materials to achieve up to 96% detachment of a uropathogenic Escherichia coli (UPEC) strain upon a reduction in temperature. Furthermore, an assessment of the changes in surface chemistry of the switchable materials following the temperature switch provides new insights into bacteria-surface interactions, which are important for understanding polymer surface resistance to bacterial attachment. Specifically, we demonstrate that bacterial attachment cannot be explained by a simple correlation with WCA.
Two polymer samples were selected from a number of switchable materials discovered using a combinatorial screen of polyacrylates.[11] These two materials exhibited the largest increase or decrease in water contact angle (WCA) when the temperature was reduced from all materials in the screened library.[11] The first co-polymer, which exhibited a decrease in WCA with a reduction in temperature, was a 70:30 cross-linked copolymer of poly(PG) diacrylate (PPGdA) and trimethylolpropane ethoxylate (1 EO/OH ) methyl ether diacrylate (TMPEMEdA) which will be referred to as PPGdA 70:30 TMPEMEdA. The chemical structures of the monomers are shown in Figure 1a. The second material, which exhibited an increase in WCA with a reduction in temperature, was a linear 70:30 copolymer of 2-[[(butylamino)carbonyl]oxy]ethyl acrylate (BACOEA) and 2-(2-methoxyethoxy)ethyl methacrylate (MEEMA), which will be referred to as BACOEA 70:30 MEEMA. In addition, homopolymers of the 4 monomer components were prepared for comparison. Polymers were prepared using a photo-initiated free radical polymerization mechanism similar to the on slide polymerization utilized by the high throughput materials discovery methodology.[11,12] Glass was used as a non-thermally responsive control.
Figure 1.
(a) Chemical structures of monomers. (b–c) Confocal images of SYTO17 stained UPEC on (b) PPGdA 70 :30 TMPEMEdA or (c) BACOEA 70:30 MEEMA at 37 °C (left) and 4 °C (right). Each image is 160 × 160 µm. Images from controls are shown in Figure SI1. (d) Coverage of UPEC on polymer coupons or a glass coverslip grown at 37 °C ( ) and grown at 37 °C then incubated at 4 °C (
) and grown at 37 °C then incubated at 4 °C ( ) for 4 h. Error bar equals ± one standard deviation, n = 3. The coverage of bacteria on homopolymers of the 4 monomers after 72 h incubation is also shown. (e) By analysis of the supernatant and sonication of the substrates the –total number of bacterial cells on the substrate(
) for 4 h. Error bar equals ± one standard deviation, n = 3. The coverage of bacteria on homopolymers of the 4 monomers after 72 h incubation is also shown. (e) By analysis of the supernatant and sonication of the substrates the –total number of bacterial cells on the substrate( ) and in the supernatant (
) and in the supernatant ( ) on glass or PPGdA 70 :30 TMPEMEdA respectively was determined when either maintaining the temperature at 37 °C or reducing it to 4 °C.
) on glass or PPGdA 70 :30 TMPEMEdA respectively was determined when either maintaining the temperature at 37 °C or reducing it to 4 °C.
To allow for bacterial attachment and subsequent biofilm formation PPGdA 70:30 TMPEMEdA and BACOEA 70:30 MEEMA were inoculated with strains of UPEC (strain 536), Pseudomonas aeruginosa (strain PAO1) or Staphylococcus aureus strain (8325-4). E.coli is a significant cause of water contamination[13] and all three bacterial species are responsible for significant levels of human infection.[14,15] The polymers and bacteria were incubated for 72 h at 37 °C, above the switching temperature of the polymers,[11] in protein free media (RPMI) prior to a 4 h incubation at either 4 °C (below the switching temperature of the polymers [11]) or 37 °C. Bacterial surface coverage was determined by staining the washed polymers with SYTO17, as previously described,[16] and quantifying the fluorescence output. Representative confocal microscopy images of bacteria on the polymers when the incubation was maintained at 37 °C are contrasted with those where it was reduced to 4 °C (see Figure 1b and c for PPGdA 7030 TMPEMEdA and BACOEA 70:30 MEEMA, respectively). Figure 1d shows the quantification of UPEC surface coverage on the homopolymerand glass surfaces. The morphology of the bacterial biofilms on the two materials differed; on BACOEA 70:30 MEEMA fewer but larger colonies were observed (Figure 1b) while on PPGdA 70 :30 TMPEMEdA a larger number of smaller colonies was observed (Figure 1c). Upon a reduction in temperature to 4 °C both PPGdA 70 :30 TMPEMEdA and BACOEA 70:30 MEEMA showed a significant decrease in bacterial attachment (compare Figures 1b and 1c right hand panels). On PPGdA 70:30 TMPEMEdA, bacterial coverage was reduced from 2.0% to 0.10%, corresponding to the release of 96% of the attached bacteria, whilst on BACOEA 70:30 MEEMA bacterial coverage was reduced from 5.3% to 1.0%, corresponding to the release of 81% of attached bacteria (Figure 1d). A bacterial coverage of 0.05% after 72 hours incubation was observed on the polymer from our recently discovered new class of materials resistant to bacterial attachment with the best resistance to UPEC.[17] No switchable detachment was observed for either P. aeruginosa or S. aureus (data not shown) suggesting the thermally induced release of bacteria may be specific for E. coli. Previously, the release of up to 98% of Halomonas marina and Staphylococcus epidermidis attached to the polymer poly(N-isopropyl acrylamide) (PNIPAAm) was achieved by lowering the temperature of PNIPAAm to below its lower critical solution temperature.[18]
In our studies, low UPEC coverage was observed on the homopolymer of TMPEMEdA, PPGdA and BACOEA at both temperatures, with bacterial coverage measured in the range of 0.1–0.3%. Only the homopolymer of MEEMA showed a significant (p<0.37) change in bacterial coverage with a change in temperature (Figure 1d). For this material bacterial coverage increased from 0.3% to 0.9% with a reduction in temperature. An increase in WCA of 7° was observed for the homopolymer of MEEMA (Figure 2a), and for this case an increase in hydrophobicity resulted in an increase rather than a reduction in bacterial attachment. The bacterial coverage on glass was 53% at 37 °C, which was not significantly different (p<0.90) to that at 4 °C, 58%.
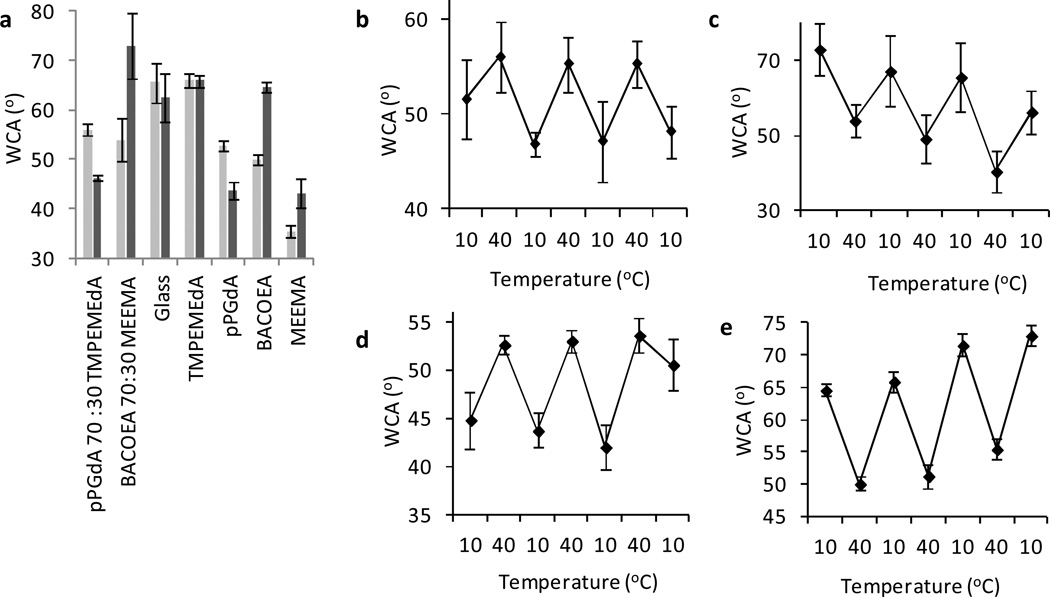
Figure 2.
(a) WCA at both 40 °C ( ) and 10 °C (
) and 10 °C ( ). Error bars equal ± one standard deviation unit, n = 9. WCA measurements of (b) PPGdA 70 :30 TMPEMEdA and (c) BACOEA 70:30 MEEMA and homopolymers (d) PPGdA and (e) BACOEA taken at 10 °C and 40 °C. The temperature of the materials was changed between the 10 °C and 40 °C 3 times. The error bars equal ± 1 standard deviation, n = 9.
). Error bars equal ± one standard deviation unit, n = 9. WCA measurements of (b) PPGdA 70 :30 TMPEMEdA and (c) BACOEA 70:30 MEEMA and homopolymers (d) PPGdA and (e) BACOEA taken at 10 °C and 40 °C. The temperature of the materials was changed between the 10 °C and 40 °C 3 times. The error bars equal ± 1 standard deviation, n = 9.
Bacterial cells adapt rapidly to physico-chemical changes in their growth environment including temperature and hence a reduction from 37 °C to 4 °C will induce a cold adaptive response. In E. coli, almost 300 genes showed differential expression when the temperature was reduced from 37 °C to 23 °C[19] Hence it is possible that the reduced attachment/detachment of the E.coli strain used in these studies to PPGdA 70 :30 TMPEMEdA and BACOEA 70:30 MEEMA respectively is a consequence of the microbe’s response to temperature rather than to any changes in the bacteria-material interaction. However, since we observed no differences in the surface coverage of E. coli on glass at 4 °C compared with 37 °C (Figure SI1e), we conclude that changes observed are indeed due to modification of the bacteria-polymer interactions.
The monomer constituents of the two switchable copolymers acted synergistically to produce a biological response that would not be predicted based upon the response observed for the respective homopolymers. For PPGdA 70 :30 TMPEMEdA the combination of monomer constituents supported much higher bacterial attachment at 37 °C than was observed for the homopolymers of PPGdA and TMPEMEdA. For BACOEA 70:30 MEEMA the combination of the two monomers resulted in an increase in bacterial attachment at 37 °C that was reversible upon a reduction in temperature. This switch was not observed for the respective homopolymers. At 4 °C the bacterial coverage of the PPGdA 70 :30 TMPEMEdA (0.01%) was lower than the coverage on the homopolymers of PPGdA (0.14%) and TMPEMEdA (0.23%), whilst the bacterial coverage at 4 °C for BACOEA 70:30 MEEMA (1.0%) was similar to the homopolymer of MEEMA (0.9%), but higher than the homopolymer of BACOEA (0.2%).
To confirm that the bacterial cells were being released into the supernatant, total bacterial numbers were determined for both the supernatant and the substrate for PPGdA 70 :30 TMPEMEdA before and after a temperature reduction. Cells were released from the coating by sonication before counting. After 4 h incubation at 37 °C, approximately 70% of the seeded bacteria remained on the surface whilst 30% of the bacteria were present in the supernatant for both the polymer and glass (Figure 1e). Dispersal occurs naturally in mature bacterial biofilms but may be triggered by different environmental cues including nutrient levels, oxygen tension, temperature and bacterial signal molecules.[20] In our experiments, the consistent release observed from both glass and polymer at 37 °C suggests that these particular surfaces do not influence dispersal. When the sample temperatures were reduced the percentage of bacteria attached to the glass sample decreased to 63% with a corresponding increase in planktonic bacteria within the supernatant (Figure 1e). This suggests an increase in bacteria dispersal from biofilm at the low temperature compared with higher temperature. In Neisseria subflava and several other oral bacteria a temperature-dependent dispersal pattern from a cool medium towards a warm medium has been observed.[21] The possible mechanism involved in driving temperature-dependent dispersal is likely to depend on the intracellular levels of the second messenger cyclic diguanylate which controls the balance between a sessile surface attached lifestyle and a free living planktonic lifestyle .[20]
On PPGdA 70 :30 TMPEMEdA, a significant release of bacteria from the surface was observed, with the proportion of bacteria in the supernatant increasing from 28% to 69% and the number of bacteria on the surface correspondingly reduced from 72% to 31% (Figure 1e). This equates to the release of 59% of the attached bacteria upon the reduction of temperature, confirming that bacteria are released from the surface of the polymer into the supernatant. The difference in the magnitude of the proportion of released bacteria between total cell counts and confocal microscopy methods is due to the different parameters being measured. In particular, the surface coverage measurements obtained via confocal microscopy do not resolve individual surface attached bacterial cells especially within biofilms,.
The surface properties of the polymers, as measured by time-of-flight secondary ion mass spectrometry (ToF-SIMS) and surface wettability analysis, were assessed to provide insight into the surface chemical changes associated with the bacterial release. Both PPGdA 70 :30 TMPEMEdA and BACOEA 70:30 MEEMA showed a reversible switch in WCA (Figure 2a–c), with an average change in WCA of −10° ± 1° and 19° ± 5°, respectively, when the temperature was reduced from 40 °C (above the switching temperature of the polymers [11]) to 10 °C (below the switching temperature of the polymers [11]). The glass transition temperature of the polymers was not in this range (Figure SI2). A similar reversible switch in WCA was observed for the homopolymers of PPGdA and BACOEA (Figure 2d–e). No statistically significant change (p<0.90) in the WCA was measured on glass upon dropping the temperate (Figure 2a). Upon reduction in temperature below 37 °C, a decrease in WCA of 15° from 60° to 45° has been previously observed for PNIPAAm,[18] and a decrease of 5° from 55° to 50° has been observed for an ethylene glycol based switchable surface.[22]
For ToF-SIMS analysis, the 2 switchable copolymers were introduced to the spectrometer at room temperature, cooled and analyzed at −5 °C before warming to 37 °C and reanalyzing. Samples were held at a temperature for at least 1 h before analysis. The reversibility of any switches was also assessed (Figure SI3 and 4). These experiments were performed in vacuum, thus, any switching in the polymer surface structure is unlikely to occur by the same mechanism as when in a solvent. However, any changes in surface composition observed by ToF-SIMS may provide insight into the molecular mobility within the polymer and thus, can inform how any changes to the polymer surface may occur in water.
The relative change in each of the hundreds of secondary ions in the positive and negative spectra was calculated and when this change was statistically significant across 3 replicates (p<0.05) the ions with the largest (either negative or positive) change in intensity were identified, shown in Table SI1 for PPGdA 70 :30 TMPEMEdA and BACOEA 70:30 MEEMA. For reference the intensities of each of these ions measured from the homopolymers of each material’s monomer constituents are also shown. ToF-SIMS spectra of the two copolymers at −5 °C and 37 °C as well as the homopolymer controls are shown in Figure SI5 and 6. X-ray photoelectron spectroscopy (XPS) was also used to quantify the surface chemistry of the two switchable polymers (Table SI2).
The secondary ions with the largest positive change in intensity on reduction of temperature on PPGdA 70 :30 TMPEMEdA, and were therefore surface enriched at −5 °C, were all hydrocarbon fragment ions. The switching of these ions was partially reversible. These secondary ions were not specific to one monomer and likely originate from polymer backbone environments common to both monomers. The secondary ions with the largest negative change in intensity, which indicates surface enrichment at an elevated sample temperature, were associated with PPGdA by comparison of the homopolymer spectra of TMPEMEdA and PPGdA (Table SI1). The switching of these ions was non-reversible. There was no significant difference between the O/C ratio as measured by XPS compared with the value calculated from the molecular structure of this polymer (Table SI2).
The secondary ions that increased in intensity on BACOEA 70:30 MEEMA when the temperature was elevated originated from both monomer components. Ions associated with MEEMA switched reversibly. The secondary ions with the largest reduction in intensity when the temperature was raised were all at a higher intensity in the homopolymer of MEEMA compared to the homopolymer of BACOEA and thus likely originate from MEEMA (Table SI1).
A number of studies have previously explored reversible bacterial attachment on switchable materials.[6,7,18] In all these cases initial bacterial attachment occurred on materials with a WCA in the range of 50–70°, and bacterial release was triggered by a decrease in WCA brought on by a reduction of temperature. In this study, bacterial attachment occurred when the WCA of the materials was in the range of 53°–56°; however, bacterial release was induced when the WCA was switched either above or below this range upon the reduction of temperature. This suggests that bacterial attachment cannot be explained by a simple correlation with WCA. Consistent with this observation, resistance to bacterial attachment has been observed previously on both superhydrophobic and superhydrophilic surfaces.[23,24]
Our data suggest that the surface composition of the polymers in this study plays the key role. For PPGdA 70 :30 TMPEMEdA, ToF-SIMS analysis suggests that the PG moieties of PPGdA are surface enriched at 37 °C whilst the polymer backbone becomes preferentially exposed at reduced temperature with an accompanying decrease in the abundance of PG groups. The WCA analysis suggests the polymer’s hydrophilicity and potentially its solvation increased with a reduction in temperature. Together, these results suggest that at 37 °C and in solution the PPG sidegroups are collapsed, resulting in the PG moiety covering the surface and thus reducing the surface density of TMPEMEdA. However, at 4 °C the polymer absorbs water, resulting in the extension of the polymer’s side groups. This causes the bacteria to detach. This is a similar mechanism to that proposed for the switchable behavior of PNIPAAm,[25] ethylene glycol and PG based materials.[26]
For BACOEA 70:30 MEEMA, ToF-SIMS analysis suggests the surface enrichment of MEEMA at 37 °C, suggesting that the side groups are extended and possibly solvated. This is supported by the comparatively low WCA of the material at 37 °C. Large hydrocarbon fragments were detected for BACOEA 70:30 MEEMA using ToF-SIMS (Table SI1), such as C9H20+, that are presumably derived from the polymer backbone. This is supported by the comparatively lower O/C ratio as measured by XPS (0.32) compared with the value calculated from the molecular structure of this polymer (0.41) (Table SI2). These fragments were also observed for the homopolymer of MEEMA, suggesting that the polymer BACOEA 70:30 MEEMA contains sections with repeated MEEMA units at its surface. The bacteria may have a specific affinity for the pendant group of MEEMA through hydrogen bonding of surface carbohydrates. Upon lowering of the temperature as the surface concentration of MEEMA is reduced the bacteria are released. The inclusion of BACOEA creates a surface more permissable for cell attachment at 37 °C.
In summary, two co-polymers previously identified by high throughput screening to have thermo-responsive properties have been found to cause the detachment of UPEC by up to 96% when the temperature is reduced from 37 °C to 4 °C. The two polymers selected for this study were chosen because one exhibited an increase and the other a decrease in WCA when the temperature was dropped. The equivalent response of bacteria to these two materials despite their disparate change in WCA demonstrates that bacterial attachment cannot be explained by a simple correlation with WCA. This insight is important for understanding the mechanisms governing antifouling properties against bacterial attachment. ToF-SIMS and WCA analysis highlighted changes in the polymers’ surface chemistry that accompanied the detachment of E.coli, suggesting that the polymers both undergo conformationally driven surface chemical changes when the temperature is altered. The switchable polymer strategy utilized in this study could be applied for a variety of uses including self-cleaning bacterial filtration systems.
Experimental
Preparation of polymer samples
Polymer coupons (10 mm diameter) were prepared by casting 5 µL of monomer solution (75% (v v−1) monomer, 25% (v v−1) dimethyl formamide (DMF) and 1% (w v−1) 2,2-dimethoxy-2-phenyl acetophenone) onto epoxy-functionalized slides (Xenopore), previously dip-coated into 4% (w v−1) poly(2-hydroxyethyl methacrylate) in ethanol. Samples were irradiated with a long wave UV source for 10 mins, O2<2000 ppm. Samples were dried at <50 mTorr for 7 days. The monomers used were 2-(2-methoxyethoxy)ethyl methacrylate, 2-[[(butylamino)carbonyl]oxy]ethyl acrylate, poly(propylene glycol) diacrylate and trimethylolpropane ethoxylate (1 EO/OH) methyl ether diacrylate (Sigma).
Bacterial attachment assay
UPEC strain 536, P. aeruginosa PAO1 and S. aureus 8325-4 [16] were routinely grown on LB (Luria-Bertani, Oxoid, UK) agar plates at 37 °C. Prior to incubation with the bacteria, the polymer coupons were washed in distilled H2O for 10 min, UV sterilized and air-dried. Samples were incubated in 15 mL RPMI-1640 medium (Sigma) inoculated with bacteria (OD600 = 0.01) from overnight cultures and grown at 37 °C with 60 rpm shaking for 72 h. One set of coupons (n = 3) was then transferred to a 4 °C incubator, while another set (n = 3) was maintained at 37 °C for a further 4 h. The coupons were then washed three times with 15 mL phosphate buffered saline (PBS, Oxoid, UK) for 5 min, stained with 20 µM SYTO17 dye (Invitrogen, UK) for 30 min, dried and then examined using a Carl Zeiss LSM 700 Laser Scanning Microscope with ZEN 2009 imaging software (Carl Zeiss, Germany). Bacterial surface coverage was analyzed using open source Image J 1.44 software (National Institute of Health, US).
To calculate the percentage of bacteria released from the polymer surface, a similar method was performed as above. Briefly, after 72 h incubation in bacterial culture coupons were removed and washed three times with 15 mL PBS (Oxoid, UK) for 5 min. One set of coupons (n = 3) was transferred to 2 mL PBS with 0.2% (w v−1) D-(+)-glucose (Sigma) at 4 °C for 4 h, whilst another set of coupons (n = 3) were transferred to the 2 mL PBS/glucose solution and maintained at 37 °C for 4 h. Both surface adherent and aggregated bacteria were released and dispersed by sonication in PBS/glucose solution on ice 5 times for 10 s at 20% output power of W-380 Sonicator (Heat Systems-ultrasonics Inc.), followed by vortexing at maximum velocity for 15 s at room temperature. The sonication procedure did not adversely affect bacterial viability as confirmed by plating samples of bacterial liquid cultures before and after sonication. The bacterial cell numbers were determined using a Z30000 Helber Counting Chamber (Hawksley, UK) in conjunction with a Carl Zeiss Axio Observer phase contrast microscope (Carl Zeiss, Germany).
Polymer characterization
Picolitre volume sessile WCA measurements were made on each polymer as previously described [27]. The temperature of an aluminium stage was regulated using a FBC 735 Temperature Controller (Fisherbrand) and held the samples (n = 9) at a constant temperature for 120 mins before WCA measurements were taken using a piezo picolitre-dosing instrument (Krüss DSA100). The ToF-SIMS analysis was performed on an ION-TOF IV instrument (IONTOF GmbH, Münster, Germany) fitted with a heating and cooling stage. Measurements of independent samples (n = 3) were taken at temperatures of −5 °C and 40 °C. A pulsed 25-kV Bi3+ primary ion source was used at a target current of approximately 1 pA to raster two randomly selected 100 × 100 µm areas of the coupon to collect both positive and negative secondary ions. Charge compensation of the samples was accomplished with a pulsed electron flood gun. The mass of secondary ions was determined using a time-of-flight mass analyzer. The typical mass resolution (at mz−1 41) was just over 6000. XPS was carried out on a Kratos Axis Ultra instrument using monochromated Al Kα radiation (1486.6 eV), 15 mA emission current, 10 kV anode potential and a charge-compensating electron flood. High resolution core levels were acquired at a pass energy of 20 eV. The takeoff angle of the photoelectron analyzer was 90°. All spectra were acquired using an aperture of 110 mm diameter.
Supplementary Material
Acknowledgements
Funding from the Wellcome Trust (grant number 085245) and the NIH (grant number R01 DE016516) is kindly acknowledged. Morgan Alexander acknowledges the Royal Society for the provision of a Wolfson Merit Award. Assistance from Ka To Fung and Wong Yunn Shyuan with polymer sample preparation and characterization is kindly acknowledged. Assistance from Emily Smith with XPS measurements is kindly acknowledged. (Supporting Information is available online from Wiley InterScience or from the author).
Contributor Information
Andrew L. Hook, Laboratory of Biophysics and Surface Analysis, School of Pharmacy, University of Nottingham, Nottingham, NG72RD, UK
Chien-Yi Chang, School of Life Sciences, Centre for Biomolecular Sciences, University of Nottingham, Nottingham, NG72RD, UK.
David J. Scurr, Laboratory of Biophysics and Surface Analysis, School of Pharmacy, University of Nottingham, Nottingham, NG72RD, UK
Robert Langer, Department of Chemical Engineering, Harvard-MIT Division of Health Sciences and Technology, David H. Koch Institute for Integrative Cancer Research, Massachusetts Institute of Technology, 500 Main Street, Cambridge, MA 02139, USA.
Daniel G. Anderson, Department of Chemical Engineering, Harvard-MIT Division of Health Sciences and Technology, David H. Koch Institute for Integrative Cancer Research, Massachusetts Institute of Technology, 500 Main Street, Cambridge, MA 02139, USA
Paul Williams, School of Life Sciences, Centre for Biomolecular Sciences, University of Nottingham, Nottingham, NG72RD, UK.
Martyn C. Davies, Laboratory of Biophysics and Surface Analysis, School of Pharmacy, University of Nottingham, Nottingham, NG72RD, UK
Morgan R. Alexander, Laboratory of Biophysics and Surface Analysis, School of Pharmacy, University of Nottingham, Nottingham, NG72RD, UK.
References
- 1.Costerton JW, Stewart PS, Greenberg EP. Science. 1999;284:1318. doi: 10.1126/science.284.5418.1318. [DOI] [PubMed] [Google Scholar]
- 2.Dang HY, Lovell CR. Applied and Environmental Microbiology. 2000;66:467. doi: 10.1128/aem.66.2.467-475.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callow JA, Callow ME. Nature Communications. 2011;2 doi: 10.1038/ncomms1251. [DOI] [PubMed] [Google Scholar]
- 4.Cole MA, Voelcker NH, Thissen H, Griesser HJ. Biomaterials. 2009;30:1827. doi: 10.1016/j.biomaterials.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 5.Hook AL, Voelcker N, Thissen H. Acta Biomaterialia. 2009;5:2350. doi: 10.1016/j.actbio.2009.03.040. [DOI] [PubMed] [Google Scholar]
- 6.Alarcon CDL, Twaites B, Cunliffe D, Smith JR, Alexander C. International Journal of Pharmaceutics. 2005;295:77. doi: 10.1016/j.ijpharm.2005.01.037. [DOI] [PubMed] [Google Scholar]
- 7.Cunliffe D, Alarcon CD, Peters V, Smith JR, Alexander C. Langmuir. 2003;19:2888. [Google Scholar]
- 8.Cunliffe D, Smart CA, Tsibouklis J, Young S, Alexander C, Vulfson EN. Biotechnology Letters. 2000;22:141. [Google Scholar]
- 9.Cheng G, Xite H, Zhang Z, Chen SF, Jiang SY. Angewandte Chemie-International Edition. 2008;47:8831. doi: 10.1002/anie.200803570. [DOI] [PubMed] [Google Scholar]
- 10.Lee J, Jung J, Na K, Heo P, Hyun J. ACS Applied Materials & Interfaces. 2009;1:1359. doi: 10.1021/am9002364. [DOI] [PubMed] [Google Scholar]
- 11.Hook AL, Scurr DJ, Anderson DG, Langer R, Williams P, Davies M, Alexander MR. Surface and Interface Analysis. 2013;45:181. doi: 10.1002/sia.4910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hook AL, Anderson DG, Langer R, Williams P, Davies MC, Alexander MR. Biomaterials. 2010;31:187. doi: 10.1016/j.biomaterials.2009.09.037. [DOI] [PubMed] [Google Scholar]
- 13.Swerdlow DL, Woodruff BA, Brady RC, Griffin PM, Tippen S, Donnell HD, Geldreich E, Payne BJ, Meyer A, Wells JG, Greene KD, Bright M, Bean NH, Blake PA. Annals of Internal Medicine. 1992;117:812. doi: 10.7326/0003-4819-117-10-812. [DOI] [PubMed] [Google Scholar]
- 14.Hidron AI, Edwards JR, Patel J, Horan TC, Sievert DM, Pollock DA, Fridkin SK T. Natl Healthcare Safety Network, S. Participating Natl Healthcare. Infection Control and Hospital Epidemiology. 2008;29:996. doi: 10.1086/591861. [DOI] [PubMed] [Google Scholar]
- 15.Schumm K, Lam TB. Cochrane Database Systematic Reviews. 2008;16 doi: 10.1002/14651858.CD004013.pub3. [DOI] [PubMed] [Google Scholar]
- 16.Hook AL, Chang C, Yang J, Luckett J, Cockrayne A, Atkinson S, Mei Y, Bayston R, Irvine DJ, Langer R, Anderson DG, Williams P, Davies MC, Alexander MR. Nature Biotechnology. 2012;30:868. doi: 10.1038/nbt.2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hook AL, Chang C, Yang J, Atkinson S, Langer R, Anderson DG, Davies MC, Williams P, Alexander MR. Advanced Materials. 2013;25:2542. doi: 10.1002/adma.201204936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ista LK, Perez-Luna VH, Lopez GP. Applied and Environmental Microbiology. 1999;65:1603. doi: 10.1128/aem.65.4.1603-1609.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.White-Ziegler CA, Um S, Prez NM, Berns AL, Malhowski AJ, Young S. Microbiology-Sgm. 2008;154:148. doi: 10.1099/mic.0.2007/012021-0. [DOI] [PubMed] [Google Scholar]
- 20.McDougald D, Rice SA, Barraud N, Steinberg PD, Kjelleberg S. Nature Reviews Microbiology. 2012;10:39. doi: 10.1038/nrmicro2695. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan JB, Fine DH. Applied and Environmental Microbiology. 2002;68:4943. doi: 10.1128/AEM.68.10.4943-4950.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wischerhoff E, Uhlig K, Lankenau A, Borner HG, Laschewsky A, Duschl C, Lutz JF. Angewandte Chemie-International Edition. 2008;47:5666. doi: 10.1002/anie.200801202. [DOI] [PubMed] [Google Scholar]
- 23.Epstein AK, Wong TS, Belisle RA, Boggs EM, Aizenberg J. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:13182. doi: 10.1073/pnas.1201973109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kingshott P, Wei J, Bagge-Ravn D, Gadegaard N, Gram L. Langmuir. 2003;19:6912. [Google Scholar]
- 25.Balamurugan S, Mendez S, Balamurugan SS, O'Brien MJ, Lopez GP. Langmuir. 2003;19:2545. doi: 10.1021/la026787j. [DOI] [PubMed] [Google Scholar]
- 26.Synytska A, Svetushkina E, Puretskiy N, Stoychev G, Berger S, Ionov L, Bellmann C, Eichhorn KJ, Stamm M. Soft Matter. 2010;6:5907. [Google Scholar]
- 27.Taylor M, Urquhart AJ, Zelzer M, Davies MC, Alexander MR. Langmuir. 2007;23:6875. doi: 10.1021/la070100j. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.