Abstract
Aims
To examine the associations between youth poly-tobacco use and substance use disorders.
Design
Analysis of data from the 2007–2011 U.S. National Survey on Drug Use and Health.
Setting
Randomly selected, household-dwelling adolescents from the noninstitutionalized, civilian population of the U.S.A.
Participants
A total of 91,152 adolescents (ages 12–17).
Methods
Logistic regression models were used to examine the associations between type of tobacco user (non-user, users of alternative tobacco products only, users of cigarettes only, and users of cigarettes plus alternative tobacco products) with past year alcohol, marijuana, or other illicit drug use disorders, adjusting for demographic and social variables.
Findings
Compared with non-users of tobacco, the greatest risk for substance use disorders was among users of cigarettes plus alternative tobacco products (alcohol disorder adjusted odds ratio [aOR] 18.3, 95% confidence interval [CI] 16.2–20.6; marijuana disorder aOR 37.2, 95% CI 32.5–42.7; other drug disorder aOR 18.4, 95% CI 15.4–21.8), followed by users of cigarettes only (alcohol disorder aOR 9.6, 95% CI 8.8–10.6; marijuana disorder aOR 20.4, 95% CI 18.1–23.0; other drug disorder aOR 9.4, 95% CI 7.8–11.4), then users of alternative tobacco products only (alcohol disorder aOR 8.1, 95% CI 6.7–9.6; marijuana disorder aOR 9.2, 95% CI 7.5–11.4; other drug disorder aOR 3.2, 95% CI 2.4–4.3).
Conclusions
Tobacco use in adolescence is associated with higher rates of substance use disorders across all tobacco users, especially among those who use cigarettes plus other tobacco products.
Keywords: substance use disorders, poly-tobacco use, risk perceptions, youth tobacco use
INTRODUCTION
Less progress has been made in reducing the use of alternative (non-cigarette) tobacco products relative to cigarette use in the U.S., especially among underage youth (<18 years of age). In 2001, ~30% of high-school youth in the U.S. were current cigarette smokers versus 18% in 2011 [1]. In contrast, the prevalence of youth using alternative tobacco products has remained static for nearly a decade with 12% of youth currently using alternative tobacco products [2, 3]. Alternative tobacco products are not currently regulated by the U.S. Food and Drug Administration and they are inexpensive versus conventional cigarettes [4–7]. In addition, the popular notion that alternative tobacco products are less harmful than conventional cigarettes likely contributes to their popularity [2, 4–11]. Still, many of these products contain a substantial amount of nicotine and are associated with serious health risks [12–14].
The combination of cigarette smoking with alcohol and illicit drug use behaviors has been well-documented [15–18]. Rates of cigarette smoking in the U.S. are quite high among those with substance use disorders with estimates up to 80% [19, 20]. Tobacco use is associated with poorer treatment outcomes for substance use disorders. For instance, youth with substance use disorders have a high relapse rate of up to 50% within 3 months of completing substance use treatment [21]. Youth who continue or initiate smoking cigarettes during or following substance use treatment are even more likely to relapse [22] and report heavier use of alcohol and drugs following relapse than non-tobacco users [23].
Deleterious health consequences are greater for youth poly-tobacco users who are more likely to engage in alcohol and illicit drug use versus users of one tobacco product [24, 25]. In a study that examined characteristics of tobacco use in a large population of Air Force recruits, poly-tobacco users reported more total alcohol use and binge drinking [26]. In a related national study, youth poly-tobacco users were most likely to have used alcohol, marijuana, and/or cocaine in the last 30 days versus non-tobacco users and users of one tobacco product [27]. Taken together, the findings underscore the clustering of substance use behaviors that are more pronounced for poly-tobacco users.
Therefore, while it is clear that tobacco use is more frequent and heavier among individuals with alcohol and other drug problems [28, 29], the extent to which these associations vary across different types of tobacco users (i.e., non-users versus alternative tobacco users only, conventional cigarette users only, poly-tobacco users who combine alternative tobacco products plus conventional cigarettes) is unknown. In the present study, we examine the associations between different types of youth tobacco users and substance use disorders using data from a nationally representative sample. We also focus our analysis on clinically diagnosable substance use behaviors because tobacco has a strong contemporaneous relationship with alcohol and illicit drug use behaviors and potentially impedes abstinence following substance use treatment. Given the changing tobacco use landscape among U.S. youth we distinguish between conventional cigarette users and alternative tobacco product users. Moreover, because alternative tobacco products can be viewed as “less harmful” than conventional cigarettes [2, 4–11], we additionally examine if youth who use alternative tobacco products are more conscientious of the adverse outcomes for substance misuse, in general, versus users of conventional cigarettes.
METHODS
Survey setting and tools
The analyses presented in this study utilized public use files of the 2007–2011 National Survey on Drug Use and Health (NSDUH) [30]. The NSDUH is an annual nationwide cross-sectional survey that provides population estimates of substance use and health status of the noninstitutionalized U.S. civilian population aged 12 or older. Independent, multistage area probability samples are collected for each of the 50 states and the District of Columbia. Informed consent was obtained from all participants. A total of 283,216 respondents completed the survey in 2007–2011 and present analyses include subjects that are ages 12–17 years old at the time of participation (n=91,152). We used five recent years of NSDUH data in order to increase the total sample size of youth tobacco users, specifically alternative tobacco users, thus increasing power for analyses.
Measures
Past month tobacco use was assessed for the following products: cigarettes, cigars, pipe, chew, and snuff. Youth were classified into tobacco user groups representing a) non-tobacco users (did not use any of the above tobacco products in the past month), b) users of alternative products (cigars, chew, snuff, and/or pipe) but not cigarettes in the past month, c) users of only cigarettes in the past month, and d) users of cigarettes plus alternative products (cigars, chew, snuff, and/or pipe) in the past month.
The NSDUH substance use disorder assessment queries past year alcohol, marijuana, or other illicit drug use disorder and is specified to be consistent with DSM-IV criteria; this instrument has been clinically validated [31]. Given the new diagnostic criteria for DSM-5, we developed an algorithm to make these diagnoses. Participants were identified as having a DSM-5 diagnosis for a substance use disorder if they endorsed two or more criteria within a 12-month period which included hazardous use, social/interpersonal problems related to use, neglected major roles to use, withdrawal, tolerance, used larger amounts/longer, repeated attempts to quit/control use, much time spent using, physical/psychological problems related to use, activities given up to use. The craving symptom was not included in the NSDUH assessment. Legal problem(s) is a DSM-IV symptom but is not a symptom to meet criteria for a DSM-5 diagnosis and was therefore excluded from our analysis of DSM-5 diagnoses. Illicit drug disorder (other than marijuana) was defined based on criteria for cocaine, heroin, pain relievers, sedatives, stimulants, hallucinogens, inhalants, or tranquilizer disorders.
The NSDUH asks participants aged 12 to 17 how much people risk physical and other harm when they smoke one or more packs of cigarettes per day, drink four to five alcoholic drinks nearly every day, use marijuana once or twice a week, use cocaine, use LSD, and/or use heroin once or twice a week. Risk perceptions of cocaine, LSD, and heroin use were the only illicit drugs (other than marijuana) queried in the NSDUH. Response choices are (1) no risk, (2) slight risk, (3) moderate risk, and (4) great risk. We collapsed responses for moderate, slight, and no risk to dichotomize responses in order to measure great risk for harm versus all others. We combined the perceived risk scores for cocaine, LSD, and heroin into one illicit drugs (other than marijuana) score by averaging the risk score across the three substances; then if the average score was 3.5 or more, the respondent was coded as perceiving great risk for harm.
We controlled for participants’ sex, race/ethnicity, age, annual family income, and the population density of the county in which the respondent resided. Population density was classified into large metropolitan areas (population ≥1 million), small metropolitan areas (population < 1 million), and non-metropolitan areas (outside a standard metropolitan statistical area).
Statistical Analysis
The prevalence of substance use disorders (alcohol, marijuana, other illicit drugs) and belief that regular use of substances was not of great risk was compared among the tobacco user types (non-user (reference), alternative products only, cigarettes only, cigarettes plus alternative products) using chi square tests of independence. P<.05 was considered statistically significant.
Logistic regression models were used to examine the association between type of tobacco user with each type of substance use disorder (alcohol, marijuana, other illicit drugs), adjusting for social and demographic variables described above and year. We first assessed the substance use disorders as defined by DSM-IV criteria, then used the DSM-5 criteria described above. Model results were nearly identical for participants with a DSM-IV substance use disorder diagnosis versus a DSM-5 substance use disorder diagnosis; therefore, we present results on the DSM-5 diagnoses only for brevity. Next we assessed the associations between type of tobacco user (non-user as the reference) with the perception that use of each substance was not of great risk, adjusting for the same social and demographic variables described above and survey year. All models were additionally run, excluding non-tobacco users and using cigarette users only as the reference group. To account for the potential impact of users of blunts (cigars with marijuana in them) on the associations between type of tobacco user and marijuana use disorder or marijuana risk perceptions, we also ran these models excluding current (past 30 day) blunt users. Odds ratios and 95% confidence intervals are presented.
The NSDUH uses a complex sampling design employing a 50-state design with an independent multistage area, deeply stratified, probability sample for each of the 50 states and the District of Columbia. Sample weights are provided to obtain unbiased estimates for survey outcomes [32]. The sample design must be incorporated into the analysis because it affects estimation of standard errors [33]. Thus, all analyses were performed using SAS-callable SUDAAN version 11.0.0, a software program that uses Taylor series linearization to adjust for design effects of complex sample surveys and apply survey weights [34].
RESULTS
Most of the participants were non-tobacco users (88.8%, 95% confidence interval [CI] 88.5–89.0%); 2.4% (95% CI 2.3–2.6%) were alternative tobacco users only; 5.6% (95% CI 5.4–5.8%) were conventional cigarette users only; 3.2% (95% CI 3.1–3.4%) were users of conventional cigarettes and alternative tobacco products. Among users of only alternative tobacco products, the most popular products used were cigars only (45.3%, 95% CI 42.6–48.0%), followed by snuff only (22.0%, 95% CI 20.0–24.2%), both chew and snuff (10.8%, 95% CI 9.4–12.4%), and pipe only (6.8%, 95% CI 5.6–8.1%). Among those that used both cigarettes and at least one alternative tobacco product, the most common combinations of other products used were cigars only (53.1%, 95% CI 50.8–55.4%), snuff only (10.3%, 95% CI 9.1–11.7%), chew and snuff (6.0%, 95% CI 5.0–7.3%), and cigars and pipe (6.0%, 95% CI 4.8–7.4%).
Slightly more than half of participants were male, nearly 60% were Caucasian, and roughly 1/3 fell into each of the age groups of 12–13 years, 14–15 years, and 16–17 years (Table 1 contains additional demographic characteristics).
Table 1.
Characteristics of sample, NSDUH 12–17 year olds, 2007–2011 (N= 91,152)
| Variable | N | Weighted % (95% CI) |
|---|---|---|
| Tobacco use | ||
| Non-user | 80,118 | 88.8 (88.5–89.0) |
| Cigars, smokeless tobacco a, and/or pipe only | 2,345 | 2.4 (2.3–2.6) |
| Cigarettes only | 5,452 | 5.6 (5.4–5.8) |
| Cigarettes + cigars, smokeless tobacco a, and/or pipe | 3,237 | 3.2 (3.1–3.4) |
|
| ||
| Alcohol use disorder symptoms b | ||
| 0–1 symptoms | 83,967 | 94.5 (94.3–94.7) |
| ≥ 2 symptoms | 5,161 | 5.5 (5.3–5.7) |
|
| ||
| Marijuana use disorder symptoms b | ||
| 0–1 symptoms | 86,032 | 95.4 (95.3–95.6) |
| ≥ 2 symptoms | 4,365 | 4.6 (4.4–4.8) |
|
| ||
| Other illicit drug use disorder symptoms b | ||
| 0–1 symptoms for one or more classes of drugs | 84,553 | 97.7 (97.6–97.9) |
| ≥ 2 symptoms for one or more classes of drugs | 2,016 | 2.3 (2.1–2.4) |
|
| ||
| Sex | ||
| Male | 46,573 | 51.1 (50.7–51.5) |
| Female | 44,579 | 48.9 (48.5–49.3) |
|
| ||
| Race | ||
| Caucasian | 53,808 | 58.1 (57.4–58.8) |
| African American | 12,529 | 14.9 (14.5–15.3) |
| Hispanic | 16,110 | 19.8 (19.2–20.4) |
| Other | 8,705 | 7.3 (7.0–7.6) |
|
| ||
| Age | ||
| 12–13 years | 28,558 | 31.7 (31.3–32.1) |
| 14–15 years | 30,603 | 33.9 (33.5–34.3) |
| 16–17 years | 31,991 | 34.4 (34.0–34.8) |
|
| ||
| Income | ||
| <$20,000 | 15,595 | 16.6 (16.2–17.1) |
| $20,000 – $49,999 | 29,199 | 31.1 (30.5–31.7) |
| $50,000 – $74,999 | 17,175 | 17.8 (17.4–18.1) |
| $≥75,000 | 29,183 | 34.5 (33.8–35.2) |
|
| ||
| County metro status | ||
| Large metro | 39,732 | 53.5 (52.7–54.2) |
| Small metro | 31,361 | 30.4 (29.6–31.3) |
| Non-metro | 20,059 | 16.1 (15.6–16.6) |
|
| ||
| Year | ||
| 2007 | 17,727 | 20.4 (19.9–20.8) |
| 2008 | 17,842 | 20.1 (19.6–20.6) |
| 2009 | 17,705 | 19.8 (19.4–20.3) |
| 2010 | 18,614 | 19.6 (19.1–20.1) |
| 2011 | 19,264 | 20.1 (19.7–20.6) |
Smokeless tobacco products include chewing tobacco or snuff.
Missing data not included in frequency calculations. 2,024 (2.2%) missing data for alcohol use disorder symptoms, 755 (0.8%) missing data for marijuana use disorder, 4,583 (5.0%) missing data for other drug use disorder.
Type of tobacco user and substance use disorders
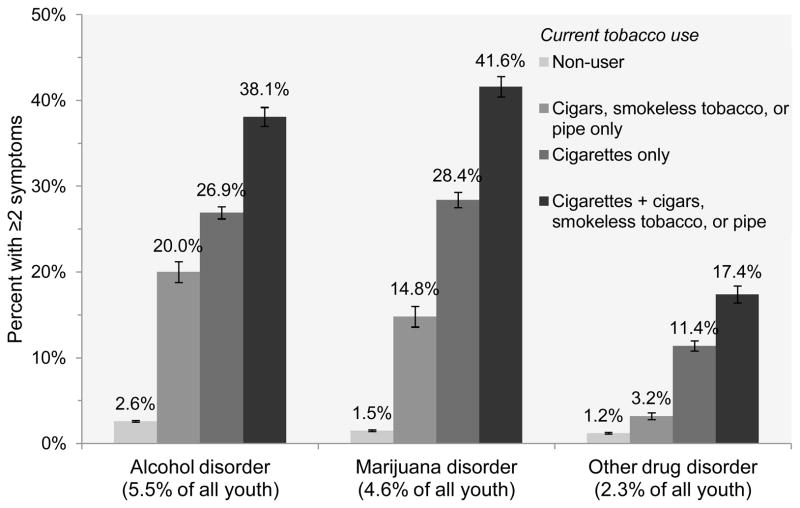
Approximately 5.5% (95% CI 5.3–5.7%) of participants exhibited ≥2 symptoms for an alcohol use disorder; 4.6% (95% CI 4.4–4.8%) exhibited ≥2 symptoms for a marijuana use disorder; 2.3% (95% CI 2.1–2.4%) exhibited ≥2 symptoms for other illicit drug use disorders. Of the 9.5% (95% CI 9.2–9.7%) of youth who had one or more substance use disorder, over half (57.0%, 95% CI 55.7–58.3%) were current tobacco users. Of youth with alcohol disorder, over half (58.5%. 95% CI 56.9–60.1%) used some type of tobacco. Of those with marijuana use disorder, 71.2% (95% CI 69.4–73.0%) used tobacco. Of those with drug use disorder other than marijuana, 54.2% (95% CI 51.0–57.3%) used tobacco. The prevalence of substance use disorders was highest among users of cigarettes and alternative tobacco products, followed by users of cigarettes only, alternative tobacco products only, and non-tobacco users (alcohol use disorder Wald F=608.0, p<.001; marijuana use disorder Wald F=603.7, p<.001; other drug use disorder Wald F=153.0, p<.001) (Figure 1).
Figure 1.
Percent of DSM-5 substance use disorders, by type of tobacco user among youth age 12–17 years, NSDUH 2007–2011. Percentages +/− standard errors are shown.
95% confidence intervals are as follows. Alcohol use disorder: non-users 2.4–2.7%, cigars, smokeless tobacco or pipe only 17.7–22.5%, cigarettes only 25.4–28.4%, cigarettes plus other products 36.0–40.3%. Marijuana use disorder: non-users 1.4–1.6%, cigars, smokeless tobacco or pipe only 12.7–17.3%, cigarettes only 26.6–30.1%, cigarettes plus other products 39.3–44.1%. Other drug use disorder: non-users 1.1–1.3%%, cigars, smokeless tobacco or pipe only 2.5–4.2%, cigarettes only 10.1–12.7%, cigarettes plus other products 15.5–19.5%.
In the multivariable logistic regression models (Table 2), compared to non-tobacco users (lowest risk group), users of alternative tobacco products only were much more likely than non-tobacco users to have a substance use disorder (alcohol use disorder adjusted odds ratio [aOR] 8.1, 95% CI 6.7–9.6; marijuana use disorder aOR 9.2, 95% CI 7.5–11.4; other drug use disorder aOR 3.2, 95% CI 2.4–4.3). The odds of substance use disorders were even higher among cigarette smokers (only) compared to non-tobacco users (alcohol use disorder aOR 9.6, 95% CI 8.8–10.6; marijuana use disorder aOR 20.4, 95% CI 18.1–23.0; other drug use disorder aOR 9.4, 95% CI 7.8–11.4). Furthermore, users who combined cigarettes with alternative tobacco products had the greatest odds of substance use disorders (alcohol use disorder aOR 18.3, 95% CI 16.2–20.6; marijuana use disorder aOR 37.2, 95% CI 32.5–42.7; other drug use disorder aOR 18.4, 95% CI 15.4–21.8). For marijuana and other drug use disorders, the non-overlapping confidence intervals for the odds ratios associated with the different types of tobacco users indicated that risks were highest among users of cigarettes and alternative tobacco products, followed by cigarettes only, and users of alternative tobacco products only. For alcohol use disorders, the odds associated with users of cigarettes and alternative products was significantly greater than users of cigarettes only and users of alternative products only (indicated by non-overlapping confidence intervals).
Table 2.
Associations between type of tobacco user and substance use disorder, adjusted for demographic covariates
| Alcohol use disorder: a ≥2 vs 0–1 symptoms aOR (95% CI) |
Marijuana use disorder: b ≥ 2 vs 0–1 symptoms aOR (95% CI) |
Other drug use disorder: c ≥ 2 vs 0–1 symptoms aOR (95% CI) |
|
|---|---|---|---|
| Tobacco use | |||
| Non-user | Ref. | Ref. | Ref. |
| Cigars, smokeless tobacco d, and/or pipe only | 8.1 (6.7, 9.6) | 9.2 (7.5, 11.4) | 3.2 (2.4, 4.3) |
| Cigarettes only | 9.6 (8.8, 10.6) | 20.4 (18.1, 23.0) | 9.4 (7.8, 11.4) |
| Cigarettes + cigars, smokeless tobacco d, and/or pipe | 18.3 (16.2, 20.6) | 37.2 (32.5, 42.7) | 18.4 (15.4, 21.8) |
| Sex | |||
| Female | Ref. | Ref. | Ref. |
| Male | 0.6 (0.56, 0.7) | 1.1 (1.0, 1.3) | 0.5 (0.48, 0.6) |
| Race | |||
| Caucasian | Ref. | Ref. | Ref. |
| African American | 0.7 (0.6, 0.8) | 1.1(0.9, 1.3) | 0.7 (0.6, 0.9) |
| Hispanic | 1.4 (1.2, 1.5) | 1.3 (1.1, 1.5) | 1.2 (1.0, 1.4) |
| Other | 0.9 (0.7, 1.1) | 1.1 (0.9, 1.3) | 1.0 (0.8, 1.2) |
| Age | |||
| 12–13 years | Ref. | Ref. | Ref. |
| 14–15 years | 4.1 (3.5, 4.8) | 4.7 (3.7, 5.9) | 1.6 (1.3, 2.0) |
| 16–17 years | 6.4 (5.6, 7.4) | 6.2 (4.9, 7.8) | 1.5 (1.3, 1.9) |
| Income | |||
| ≥$75,000 | Ref. | Ref. | Ref. |
| $50,000 – $74,999 | 0.9 (0.8, 1.04) | 1.0 (0.9, 1.2) | 1.0 (0.8, 1.2) |
| $20,000 – $49,999 | 0.9 (0.8, 0.95) | 1.3 (1.2, 1.5) | 1.1 (0.96, 1.3) |
| <$20,000 | 1.0 (0.8, 1.1) | 1.5 (1.2, 1.8) | 1.3 (1.1, 1.6) |
| County metro status | |||
| Non-metro | Ref. | Ref. | Ref. |
| Large metro | 1.1 (0.96, 1.2) | 1.8 (1.6, 1.9) | 1.2 (1.02, 1.5) |
| Small metro | 1.0 (0.9, 1.1) | 1.7 (1.5, 2.0) | 1.2 (1.04, 1.5) |
| Year | |||
| 2007 | Ref. | Ref. | Ref. |
| 2008 | 1.0 (0.8, 1.1) | 1.3 (1.1, 1.5) | 1.0 (0.8, 1.2) |
| 2009 | 0.8 (0.7, 0.9) | 1.1 (0.97, 1.3) | 0.9 (0.8, 1.2) |
| 2010 | 0.8 (0.7, 0.98) | 1.4 (1.2, 1.6) | 1.1 (0.9, 1.3) |
| 2011 | 0.7 (0.6, 0.8) | 1.5 (1.3, 1.7) | 0.9 (0.7, 1.1) |
Model N=89,128.
Model N=90,397,
Model N=86,569,
Smokeless tobacco products include chewing tobacco and/or snuff.
Compared to users of cigarettes only, users of alternative tobacco products only had significantly lower odds of substance use disorders (aOR 0.8, 95% confidence interval (CI) 0.7–0.98; marijuana aOR 0.5, 95% CI 0.4–0.6; other drugs aOR 0.3, 95% CI 0.2–0.5). Conversely, users of cigarettes plus alternative tobacco products had approximately twice the odds of substance use disorders than cigarette users only (alcohol aOR 1.9, 95% CI 1.7–2.2; marijuana aOR 1.9, 95% CI 1.6–2.2; other drugs aOR 2.0, 95% CI 1.6–2.4).
Type of tobacco user and risk perceptions
Approximately half of respondents (50.2%, 95% CI 49.7–50.7%) believed that using marijuana once or twice a week does not have great risk of physical or other harm. Approximately one-third of respondents believed that people do not risk great physical and other harm when they smoke one or more packs of cigarettes per day (32.9%, 95% CI 32.5–33.4%) or drink 4–5 alcoholic drinks per day (35.0%, 95% CI 34.5–35.4%). Fewer believed that people do not risk great harm from using other illicit drugs (cocaine, LSD and/or heroin) once or twice a week (22.0%, 95% CI 21.5–22.4%). The prevalence of believing regular cigarette, alcohol, and marijuana use does not have great risk was highest among users of cigarettes plus alternative tobacco products and lowest among non-tobacco users (cigarettes Wald F=284.3, p<.001; alcohol Wald F=316.6, p<.001; marijuana Wald F=681.4, p<.001) (Figure 2). Although statistically significant (Wald F=7.2, p<.001), percentage of youth believing that using other illicit drugs once or twice a week does not pose great risk for harm was relatively similar across tobacco user groups (Figure 2).
Figure 2.
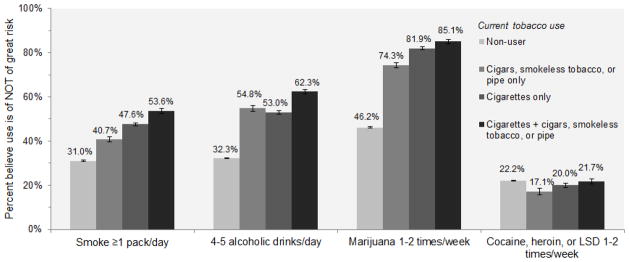
Percent who believe regular substance use is NOT of great risk for harm, by type of tobacco user among youth age 12–17 years, NSDUH 2007–2011. Percentages +/− standard errors are shown.
95% confidence intervals are as follows. Smoke ≥1 pack/day: non-users 30.5–31.5%, cigars, smokeless tobacco or pipe only 38.4–43.1%, cigarettes only 46.1–49.1%, cigarettes plus other products 51.2–55.9%. 4–5 drinks/day: non-users 31.8–32.8%, cigars, smokeless tobacco or pipe only 52.0–57.5%, cigarettes only 51.2–54.7%, cigarettes plus other products 60.2–64.3%. Marijuana 1–2 times/week: non-users 45.7–46.7%%, cigars, smokeless tobacco or pipe only 71.8–76.6%, cigarettes only 80.5–83.2%, cigarettes plus other products 83.0–87.0%. Cocaine, heroin, or LSD 1–2 times/week: non-users 21.8–22.7%, cigars, smokeless tobacco or pipe only 14.5–20.1%, cigarettes only 18.2–21.8%, cigarettes plus other products 19.5–24.0%.
Results of multivariable logistic regression models predicting the belief that the substances do not present great risk is shown in Table 3. Compared to non-tobacco users, cigarette smokers (only) and users who combined cigarettes with alternative tobacco products had two to three times the odds of believing that regular use of cigarettes (cigarettes only aOR 2.2, 95% CI 2.0–2.3; cigarettes and alternative products aOR 2.5, 95% CI 2.3–2.8) and alcohol (cigarettes only aOR 2.4, 95% CI 2.2–2.6; cigarettes and alternative products aOR 3.1, 95% CI 2.8–3.4) is not of great risk for harm, and approximately five times the odds of believing regular marijuana use does not pose great risk (cigarettes only aOR 4.7, 95% CI 4.3–5.2; cigarettes and alternative products aOR 5.6, 95% CI 4.8–6.7). Although the odds of believing frequent illicit drug use (other than marijuana) does not pose great harm was significantly higher among these tobacco user groups (compared to non-tobacco users), the magnitude of the increased risk was lower than that for the other substances (cigarettes only aOR 1.2, 95% CI 1.1–1.4; cigarettes and alternative products aOR 1.4, 95% CI 1.2–1.6). Users of only alternative tobacco products had 1.5 to 3 times the odds of believing that regular cigarette (aOR 1.5, 95% CI 1.3–1.6), alcohol (aOR 2.2, 95% CI 2.0–2.5), and marijuana use (aOR 2.8, 95% CI 2.4–3.2) is not of great risk for harm versus non-tobacco users. Their perceptions of risk of regular illicit drug use (other than marijuana) did not differ significantly from non-tobacco users (aOR 1.0, 95% CI 0.9–1.3).
Table 3.
Associations between type of tobacco user and perceptions of risk of regular substance use, adjusted for demographic covariates
| Belief that use of the following substances is NOT of great risk for harm
|
||||
|---|---|---|---|---|
| Smoke ≥ 1 pack/day a aOR (95% CI) |
4–5 Alcoholic drinks/day b aOR (95% CI) |
Marijuana 1–2 times/week c aOR (95% CI) |
Cocaine/heroin/LSD 1–2 times/week d aOR (95% CI) |
|
| Tobacco use | ||||
| Non-user | Ref. | Ref. | Ref. | Ref. |
| Cigars, smokeless tobacco d, and/or pipe only | 1.5 (1.3, 1.6) | 2.2 (2.0, 2.5) | 2.8 (2.4, 3.2) | 1.0 (0.9, 1.3) |
| Cigarettes only | 2.2 (2.0, 2.3) | 2.4 (2.2, 2.6) | 4.7 (4.3, 5.2) | 1.2 (1.1, 1.4) |
| Cigarettes + cigars, smokeless tobacco d, and/or pipe | 2.5 (2.3, 2.8) | 3.1 (2.8, 3.4) | 5.6 (4.8, 6.7) | 1.4 (1.2, 1.6) |
| Sex | ||||
| Female | Ref. | Ref. | Ref. | Ref. |
| Male | 1.44 (1.38, 1.49) | 1.65 (1.59, 1.71) | 1.38 (1.33, 1.43) | 1.02 (0.98, 1.07) |
| Race | ||||
| Caucasian | Ref. | Ref. | Ref. | Ref. |
| African American | 1.04 (0.98, 1.11) | 0.80 (0.75, 0.84) | 1.54 (1.46, 1.62) | 1.59 (1.48, 1.70) |
| Hispanic | 0.99 (0.92, 1.06) | 0.99 (0.95, 1.04) | 1.24 (1.17, 1.32) | 1.54 (1.43, 1.65) |
| Other | 0.94 (0.86, 1.03) | 0.77 (0.70, 0.84) | 0.95 (0.87, 1.03) | 1.31 (1.18, 1.46) |
| Age | ||||
| 12–13 years | Ref. | Ref. | Ref. | Ref. |
| 14–15 years | 0.95 (0.91, 1.00) | 1.11 (1.06, 1.17) | 1.51 (1.44, 1.59) | 0.63 (0.59, 0.67) |
| 16–17 years | 0.85 (0.81, 0.90) | 1.00 (0.95, 1.05) | 2.12 (2.02, 2.23) | 0.38 (0.37, 0.40) |
| Income | ||||
| ≥$75,000 | Ref. | Ref. | Ref. | Ref. |
| $50,000 – $74,999 | 1.09 (1.04, 1.15) | 1.12 (1.06, 1.19) | 1.03 (0.97, 1.09) | 1.11 (1.04, 1.19) |
| $20,000 – $49,999 | 1.31 (1.24, 1.39) | 1.29 (1.22, 1.35) | 1.21 (1.16, 1.26) | 1.28 (1.20, 1.37) |
| <$20,000 | 1.55 (1.46, 1.64) | 1.49 (1.39, 1.59) | 1.39 (1.30, 1.49) | 1.62 (1.51, 1.75) |
| County metro status | ||||
| Non-metro | Ref. | Ref. | Ref. | Ref. |
| Large metro | 0.92 (0.87, 0.97) | 0.78 (0.74, 0.81) | 1.35 (1.29, 1.42) | 1.02 (0.95, 1.09) |
| Small metro | 0.92 (0.88, 0.97) | 0.87 (0.83, 0.91) | 1.25 (1.19, 1.32) | 1.01 (0.94, 1.08) |
| Year | ||||
| 2007 | Ref. | Ref. | Ref. | Ref. |
| 2008 | 0.95 (0.90, 1.00) | 0.98 (0.93, 1.04) | 1.09 (1.02, 1.17) | 1.00 (0.92, 1.08) |
| 2009 | 1.16 (1.10, 1.23) | 1.04 (0.98, 1.10) | 1.28 (1.20, 1.37) | 1.09 (1.02, 1.17) |
| 2010 | 1.17 (1.10, 1.25) | 1.01 (0.95, 1.07) | 1.42 (1.34, 1.50) | 1.05 (0.99, 1.12) |
| 2011 | 1.13 (1.07, 1.19) | 1.04 (0.97, 1.11) | 1.57 (1.48, 1.66) | 1.13 (1.05, 1.22) |
Model N=90,158.
Model N=90,242.
Model N=89,851.
Model N=85,882.
Compared to cigarette users only, users of alternative tobacco products had lower odds of believing that regular use of cigarettes and marijuana was not of great risk (cigarettes aOR 0.7, 95% CI 0.6–0.8, marijuana aOR 0.6, 95% CI 0.5–0.7); differences in beliefs that regular use of alcohol and other drugs was not of great risk did not reach statistical significance (aOR 0.9, 95% CI 0.8–1.01, and aOR 0.8, 95% CI 0.6–1.04, respectively). However, users of cigarettes plus alternative tobacco products had slightly greater odds than cigarette users to believe that regular use of cigarettes, alcohol and marijuana was not of great risk (cigarettes aOR 1.2, 95% CI 1.03–1.4, alcohol aOR 1.2, 95% CI 1.1–1.4, marijuana aOR 1.2, 95%CI 1.03–1.5). They did not differ from cigarette users in their perception of risk of regular other illicit drug use (aOR 1.1, 95% CI 0.9–1.3).
A “blunt” is a popular term for marijuana rolled with the tobacco-leaf “wrapper” from a cigar. Many blunt users do not consider themselves a tobacco or cigar user but most blunt users do consider themselves to be marijuana users [35–37]. To examine whether use of blunts by tobacco users had any impact on results of models predicting marijuana use disorder or perceptions of risk from marijuana use, we further examined blunt use among our sample. Approximately 4.1% (95% CI 3.9–4.2%) had used a blunt in the past 30 days, and most (92.7%, 95% CI 91.2–93.7%) indicated they had used marijuana in the past 30 days. Approximately 37.4% (95% CI 35.4–39.5%) of users of cigarettes and other tobacco products used blunts, followed by 24.3% (95% CI 23.0–25.6%) of users of cigarettes only, 17.4% (95% CI 15.0–20.0%) of users of alternative tobacco products only, and 1.3% (95% CI 1.1–1.4%) of non-tobacco users (Wald F=741.8, p<.001). When excluding blunt users from the models predicting marijuana use disorder and perceptions of risk from marijuana use, results were similar but with effect sizes slightly smaller than those when using the full sample (data not shown).
DISCUSSION
This study found a clear, stepwise association between youth tobacco use and substance use disorders. Use of alternative tobacco products combined with conventional cigarettes was associated with the highest probability of clinically diagnosable involvement in alcohol, marijuana, and other illicit drug use in a dose-response pattern versus non-users of tobacco and conventional cigarette users only. Furthermore, poly-tobacco users had two times the odds of substance use disorder than users of conventional cigarettes only. Youth users of alternative tobacco products also had consistently higher odds of clinically diagnosable substance use disorders (nearly 10 times higher for alcohol and marijuana use disorders) versus non-tobacco users; however, odds were lower than youth who smoked conventional cigarettes only.
Past research has found users of alternative tobacco products to be less established tobacco users (i.e., less nicotine dependent) than conventional cigarette users [38]. We extend this study by demonstrating that youth alternative tobacco product users are less frequently diagnosed with substance use disorders versus youth who smoke conventional cigarettes. To help explain this association our secondary analysis indicated a stepwise effect across tobacco user type when measuring perceived risk for cigarettes, alcohol, and other illicit drugs. It is probable that non-tobacco users and youth who use alternative tobacco products are more conscientious of their cigarette, alcohol, and/or other drug use behaviors and are consequently less inclined to use all of these substances in comparison to smokers of conventional cigarettes. Prevention efforts are therefore encouraged to focus efforts on increasing youths’ awareness of the harms associated with use of different tobacco products and substance use, in general.
Some of the increased risk for tobacco use combined with heavy use of other substance use could be due to environmental and social risk influences. For instance, youth who endorse heavy co-occurring substance use patterns are more likely to be exposed to a deviant peer group that engages in heavy substance use behaviors and has more approving views towards substance use [39–41]. In addition, the associations may be due to genetic vulnerability to heavy use of different substances that is overlapping [42–44]. The present study underscores the need for future studies to extend such investigations to understanding the strong interrelationship between youth tobacco use and substance use disorders.
Limitations of the NSDUH are that it is cross-sectional and causation cannot be determined. The substance use behaviors of youth are a sensitive topic and it is possible that socially desirable responding may be an issue. Youth were not queried on their perceptions of risk for harm that is associated with alternative tobacco product use and such information could be useful for making comparisons of tobacco risk perceptions across different types of youth tobacco users. We contrasted our results using NDSUH DSM-IV diagnostic measures for substance use disorders with our own DSM-5 diagnostic substance use disorder categories and found similar results; nevertheless, we note that the DSM-5 craving symptom was not included in the NSDUH assessment and was therefore excluded from the DSM-5 substance use disorder diagnoses that were used in our analyses.
These limitations notwithstanding, findings from this study have relevant implications for prevention and intervention efforts. This study demonstrates a significant clustering of substance use disorders among youth tobacco users. Specifically, tobacco use clearly distinguished youth at risk for substance use disorders across alcohol, marijuana, and other illicit drugs. This risk is remarkably high for all tobacco users and especially high for poly-tobacco users. This is concerning given the number of new and emerging tobacco products now on the market and the high number of youth tobacco users who experiment with multiple forms of tobacco.
Acknowledgments
Role of funding source: This publication was made possible by Grant Numbers UL1 RR024992 and KL2 RR024994 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research and by K02DA021237 from the NIH. Other support includes K01DA025733 and R01 DA032843 (P.C.R.), K02 DA021237 (L.B.), and R01 DA031288 (R.G.).
Footnotes
Conflicts of Interest: Dr. Bierut is listed as an inventor on Issued U.S. Patent 8,080,371,“Markers for Addiction” covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction.
References
- 1.Centers for Disease Control and Prevention (CDC) Current tobacco use among middle and high school students—United States, 2011. Morb Mortal Wkly Rep. 2012;61:581–585. [PubMed] [Google Scholar]
- 2.O’Connor RJ. Non-cigarette tobacco products: what have we learnt and where are we headed? Tob Control. 2012;21(2):181–90. doi: 10.1136/tobaccocontrol-2011-050281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) National Youth Tobacco Survey [Data file] Office on Smoking and Health; 2011. [Google Scholar]
- 4.Soldz S, Dorsey E. Youth attitudes and beliefs toward alternative tobacco products: Cigars, bidis, and kreteks. Health Educ Behav. 2005;32(4):549–66. doi: 10.1177/1090198105276219. [DOI] [PubMed] [Google Scholar]
- 5.Wray RJ, Jupka K, Berman S, Zellin S, Vijaykumar S. Young adults’ perceptions about established and emerging tobacco products: Results from eight focus groups. Nicotine Tob Res. 2012;14(2):184–90. doi: 10.1093/ntr/ntr168. [DOI] [PubMed] [Google Scholar]
- 6.Delnevo CD. Smokers’ choice: What explains the steady growth of cigar use in the US? Public Health Rep. 2006;121(2):116–9. doi: 10.1177/003335490612100203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wackowski OA, Lewis MJ, Delnevo CD. Qualitative analysis of camel snus’ website message board--users’ product perceptions, insights and online interactions. Tob Control. 2011;20(2):e1. doi: 10.1136/tc.2010.037911. [DOI] [PubMed] [Google Scholar]
- 8.Choi K, Forster J. Awareness, perceptions and use of snus among young adults from the upper Midwest region of the USA. Tob Control. 2012 doi: 10.1136/tobaccocontrol-2011-050383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nyman AL, Taylor TM, Biener L. Trends in cigar smoking and perceptions of health risks among Massachusetts adults. Tob Control. 2002;11:Ii25–8. doi: 10.1136/tc.11.suppl_2.ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loukas A, Batanova MD, Velazquez CE, Lang WJ, Sneden GG, Pasch KE, et al. Who uses snus? A study of texas adolescents. Nicotine Tob Res. 2012;14(5):626–30. doi: 10.1093/ntr/ntr205. [DOI] [PubMed] [Google Scholar]
- 11.Smith JR, Novotny TE, Edland SD, Hofstetter CR, Lindsay SP, Al-Delaimy WK. Determinants of hookah use among high school students. Nicotine Tob Res. 2011;13(7):565–72. doi: 10.1093/ntr/ntr041. [DOI] [PubMed] [Google Scholar]
- 12.Stepanov I, Jensen J, Hatsukami D, Hecht SS. Tobacco-specific nitrosamines in new tobacco products. Nicotine Tob Res. 2006;8(2):309–13. doi: 10.1080/14622200500490151. [DOI] [PubMed] [Google Scholar]
- 13.Stepanov I, Jensen J, Hatsukami D, Hecht SS. New and traditional smokeless tobacco: Comparison of toxicant and carcinogen levels. Nicotine Tob Res. 2008;10(12):1773–82. doi: 10.1080/14622200802443544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Djordjevic M, Doran KA. Nicotine content and delivery across tobacco products. Handbook of Experimental Pharmacology. 2009;192:61–82. doi: 10.1007/978-3-540-69248-5_3. [DOI] [PubMed] [Google Scholar]
- 15.Grucza RA, Bierut LJ. Cigarette smoking and the risk for alcohol use disorders among adolescent drinkers. Alcohol Clin Exp Res. 2006;30(12):2046–54. doi: 10.1111/j.1530-0277.2006.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dani JA, Harris RA. Nicotine addiction and comorbidity with alcohol abuse and mental illness. Nature neuroscience. 2005;8(11):1465–70. doi: 10.1038/nn1580. [DOI] [PubMed] [Google Scholar]
- 17.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61(11):1107–15. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lawrence D, Mitrou F, Zubrick SR. Smoking and mental illness: results from population surveys in Australia and the United States. BMC Public Health. 2009;9:285. doi: 10.1186/1471-2458-9-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalman D, Morissette SB, George TP. Co-morbidity of smoking in patients with psychiatric and substance use disorders. Am J Addict. 2005;14(2):106–23. doi: 10.1080/10550490590924728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pagliaro AM, Pagliaro LA. Substance use among children and adolescents. New York: Wiley; 1996. [Google Scholar]
- 22.de Dios MA, Vaughan EL, Stanton CA, Niaura R. Adolescent tobacco use and substance abuse treatment outcomes. J Subst Abuse Treat. 2009;37(1):17–24. doi: 10.1016/j.jsat.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myers MG, Brown SA. Cigarette smoking four years following treatment for adolescent substance abuse. J Child Adolesc Subst Abuse. 1997;7(1):1–15. [Google Scholar]
- 24.Wetter DW, McClure JB, de Moor C, Cofta-Gunn L, Cummings S, Cinciripini PM, Gritz ER. Concomitant use of cigarettes and smokeless tobacco: Prevalence, correlates, and predictors of tobacco cessation. Prev Med. 2002;34(6):638–48. doi: 10.1006/pmed.2002.1032. [DOI] [PubMed] [Google Scholar]
- 25.Schuster RM, Hertel AW, Mermelstein R. Cigar, cigarillo, and little cigar use among current cigarette-smoking adolescents. Nicotine Tob Res. 2012 doi: 10.1093/ntr/nts222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lando HA, Haddock CK, Klesges RC, Talcott GW, Jensen J. Smokeless tobacco use in a population of young adults. Addict Behav. 1999;24(3):431–7. doi: 10.1016/s0306-4603(98)00058-6. [DOI] [PubMed] [Google Scholar]
- 27.Everett SA, Malarcher AM, Sharp DJ, Husten CG, Giovino GA. Relationship between cigarette, smokeless tobacco, and cigar use, and other health risk behaviors among US high school students. J Sch Health. 2000;70(6):234–40. doi: 10.1111/j.1746-1561.2000.tb07424.x. [DOI] [PubMed] [Google Scholar]
- 28.Batel P, Pessione F, Maitre C, Rueff B. Relationship between alcohol and tobacco dependencies among alcoholics who smoke. Addiction. 1995;90(7):977–80. doi: 10.1046/j.1360-0443.1995.90797711.x. [DOI] [PubMed] [Google Scholar]
- 29.John U, Hill A, Rumpf HJ, Hapke U, Meyer C. Alcohol high risk drinking, abuse and dependence among tobacco smoking medical care patients and the general population. Drug Alcohol Depend. 2003;69(2):189–95. doi: 10.1016/s0376-8716(02)00315-0. [DOI] [PubMed] [Google Scholar]
- 30.Odom D, Boman K, Chromy J, Peilan C. 2002 National Survey on Drug Use and Health Sample Design Report, R. International, Editor; Research Triangle Park, NC: 2004. [Google Scholar]
- 31.Jordan BK, Karg RS, Batts KR, Epstein JF, Wiesen C. A clinical validation of the National Survey on Drug Use and Health Assessment of Substance Use Disorders. Addict Behav. 2008;33(6):782–98. doi: 10.1016/j.addbeh.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Substance Abuse and Mental Health Services Administration (SAMHSA) National Survey on drug use and health, 2011 Codebook (ICPSR34481) Rockville, MD: Office of Applied Studies; 2012. [Google Scholar]
- 33.Lee ES, Forthofer RN. Analyzing Complex Survey Data. 2. Thousand Oaks, CA: SAGE Publications, Inc; 2006. [Google Scholar]
- 34.Shah BV, Branwell G, Bieler GS. The SUDAAN User’s Manual, Release 7.5. Research Triangle Institute; Research Triangle Park, NC: 2002. [Google Scholar]
- 35.Sandelowski M. When a cigar is not just a cigar: alternative takes on data and data analysis. Res Nurs Health. 2011;34(4):342–352. doi: 10.1002/nur.20437. [DOI] [PubMed] [Google Scholar]
- 36.Yerger V, Pearson C, Malone RE. When is a cigar not a cigar? African American youths’ understanding of “cigar” use. Am J Public Health. 2001;91:316–317. doi: 10.2105/ajph.91.2.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soldz S, Huyser DJ, Dorsey E. The cigar as a drug delivery device: youth use of blunts. Addiction. 2003;98:1379–1386. doi: 10.1046/j.1360-0443.2003.00492.x. [DOI] [PubMed] [Google Scholar]
- 38.Huh J, Timberlake DS. Do smokers of specialty and conventional cigarettes differ in their dependence on nicotine? Addict Behav. 2009;34(2):204–11. doi: 10.1016/j.addbeh.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 39.Patton GC, Coffey C, Carlin JB, Sawyer SM, Lynskey M. Reverse gateways? Frequent cannabis use as a predictor of tobacco initiation and nicotine dependence. Addiction. 2005;100(10):1518–25. doi: 10.1111/j.1360-0443.2005.01220.x. [DOI] [PubMed] [Google Scholar]
- 40.Dishion TJ, Owen LD. A longitudinal analysis of friendships and substance use: Bidirectional influence from adolescence to adulthood. Dev Psychol. 2002;38(4):480–91. doi: 10.1037//0012-1649.38.4.480. [DOI] [PubMed] [Google Scholar]
- 41.Stormshak E, Comeau C, Shepard S. The relative contribution of sibling deviance and peer deviance in the prediction of substance use across middle childhood. J Abnorm Child Psychol. 2004;32(6):635–49. doi: 10.1023/b:jacp.0000047212.49463.c7. [DOI] [PubMed] [Google Scholar]
- 42.Li MD, Burmeister M. New insights into the genetics of addiction. Nat Rev Genet. 2009;10(4):225–31. doi: 10.1038/nrg2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Agrawal A, Lynskey MT. Are there genetic influences on addiction: evidence from family, adoption and twin studies. Addiction. 2008;103(7):1069–81. doi: 10.1111/j.1360-0443.2008.02213.x. [DOI] [PubMed] [Google Scholar]
- 44.Young S, Rhee SH, Stallings M, Corley R, Hewitt J. Genetic and environmental vulnerabilities underlying adolescent substance use and problem use: General or specific? Behav Genet. 2006;36(4):603–15. doi: 10.1007/s10519-006-9066-7. [DOI] [PubMed] [Google Scholar]
- 45.Elkins I, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Arch Gen Psychiatry. 2007;64(10):1145–52. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]