Introduction
Anxiety disorders are the most common of all psychiatric conditions (Kessler et al. 2005) and are up to twice as common among women as men (Kessler et al. 1994; Kessler et al. 2005; Somers et al. 2006). Nearly one in three women will experience an anxiety disorder during her lifetime, often with a chronic or recurrent course (Kessler et al. 1994). It is not surprising therefore that anxiety disorders are common during pregnancy (Ross and McLean 2006). While there has been considerable focus on perinatal depression, our understanding of perinatal anxiety disorders is still in early stages. Prevalence estimates for anxiety disorders during pregnancy vary widely, with reported rates of women meeting diagnostic criteria for one or more specific anxiety disorders during pregnancy ranging from 12.2% to 39% (Adewuya et al. 2006; Borri et al. 2007; Giardinelli et al. 2012; Mota et al. 2008; Sutter-Dallay et al. 2004; Uguz et al. 2010; Zar et al. 2002). With the exception of specific phobia, which typically does not interfere with a woman’s day-to-day functioning, generalized anxiety disorder (GAD) is the most prevalent of the anxiety disorders among pregnant women, with reported rates up to 10.5% (Adewuya et al. 2006).
In addition to anxiety that meets diagnostic criteria for a disorder, an even greater proportion of pregnant women experience sub-threshold yet clinically relevant levels of anxiety (Andersson et al. 2006; Faisal-Cury and Menezes 2007; Lee et al. 2007; Heron et al. 2004). Several studies indicate rates of anxiety symptoms may be higher during pregnancy than in the postpartum period (Evans et al. 2001; Goodman and Tyer-Viola 2010; Heron et al. 2004; Lee et al. 2007) and may be more common during pregnancy than depression (Lee et al. 2007). Comorbidity between perinatal anxiety and depression is high (Grigoriadis et al. 2011), however anxiety also occurs without depression, and many women may experience more than one anxiety disorder concurrently (Kroenke et al. 2007). There are many reasons why pregnancy may contribute to vulnerability to increased anxiety; these include physiological and hormonal changes, physical discomfort, increased stress, uncertainty, fear regarding the possibility of pregnancy and birth complications, concerns for health of self and baby, significant life changes, and exacerbation or recurrence of pre-existing psychiatric disturbance (Wenzel 2011).
Maternal anxiety during pregnancy is associated with negative consequences for mothers and children, including increased pregnancy-related symptoms (e.g., nausea and vomiting), higher alcohol and tobacco use, greater number of medical visits, obstetric complications, shorter fetal gestation, compromised fetal neurodevelopment, and later child behavioral-emotional problems (Alder et al. 2007; Alvik et al. 2006; Andersson et al. 2004; Dunkel and Tanner 2012; Glover and O’Connor 2006; Goodwin et al. 2007; Hurley et al. 2005; Swallow et al. 2004; Teixeira et al. 1999; Van den Bergh et al. 2005). Furthermore, elevated anxiety during pregnancy is a major risk factor for postpartum depression (e.g. Britton 2008; Heron et al. 2004; Lee et al. 2007; Sutter-Dallay et al. 2004), independent of antenatal depression (Coelho et al. 2011; Heron et al. 2004; Mauri et al. 2010; sutter-Dallay et al. 2004), conferring further risks for mother and child. Nevertheless, anxiety during pregnancy is frequently undetected and untreated (Alder et al. 2007; Coleman et al. 2008; Goodman and Tyer-Viola 2010).
Psychotropic medications such as antidepressants and benzodiazepines are often used to treat anxiety, however the potential risks of fetal exposure make the development of efficacious non-pharmacologic approaches particularly urgent in this context (e.g., Hayes et al. 2012; Udechuku et al. 2010). Notably, pregnant women are reluctant to take medication due to potential risks to the developing fetus (Goodman 2009). Psychological therapies, particularly cognitive behavioral therapy (CBT), effectively reduce anxiety in patients with anxiety disorders (Otte 2011), yet such therapies have not been tested for treatment of anxiety in pregnant women. Despite a great need for effective, non-pharmacological interventions, research specifically addressing treatment of anxiety disorders during pregnancy is seriously lacking, with no published studies of psychotherapeutic treatments for anxiety in pregnancy to date.
Mindfulness based interventions (MBIs) offer a promising development for the treatment of anxiety, with numerous studies demonstrating the effectiveness of MBIs in reducing anxiety, depression and stress in clinical and non-clinical populations (for reviews see Chiesa and Serretti, 2009 & 2011; Fjorback et al. 2011; Grossman et al. 2004; Hoffman et al. 2010; Keng et al. 2011; Khoury et al. 2013; Toneatto and Ngyuen 2007). One of the most established and studied MBIs is mindfulness-based stress reduction (MBSR) which was developed by Kabat-Zinn (1990) in the 1980s. MBSR teaches mindfulness as a way to alleviate pain and improve physical and emotional well-being for individuals suffering from a variety of diseases and disorders. MBSR is a highly structured 8-week intensive group training in which participants are taught mindfulness practices such as a body-scan, formal sitting meditation, and mindful yoga. Through use of these practices, participants are taught to observe thoughts, feelings, and bodily sensations objectively and in the present moment without judging, clinging to, or pushing away their experience (Kabat-Zinn 1990). Mindfulness Based Cognitive Therapy (MBCT) is an adaptation of MBSR developed by Segal, Williams, and Teasdale (2002; 2013). MBCT integrates aspects of CBT with MBSR and is similarly offered in an 8-session group format over eight weeks. MBCT teaches mindfulness meditation as its core therapeutic practice with cognitive techniques to target specific symptoms of psychological dysfunction. Although originally designed for the prevention of relapse in patients in remission from depression, early studies suggest that MBCT may be helpful for a broad range of mental health problems (Sipe and Eisendrath 2012).
Intensive training in mindfulness meditation via MBSR or MBCT may reduce anxiety and associated symptoms in patients with anxiety disorders (Arch et al., 2013; Kabat-Zinn et al. 1992; Miller et al. 1995; Vollestad et al. 2011) and a meta-analytic review indicated that MBIs were associated with large effect sizes for improving anxiety in patients with anxiety disorders (Hoffman et al. 2010). MBCT has shown positive effects in panic (Kim et al. 2009), GAD (Craigie et al. 2008; Evans et al. 2008; Hoge et al. 2013; Majid et al. 2010), and in social anxiety disorder (Koszycki et al. 2007). Other interventions in which mindfulness training is an integral component of treatment have also shown favorable results as a clinical intervention for GAD (Hayes-Skelton et al. 2013; Roemer et al. 2008; Roemer and Orsillo 2007).
Mindfulness-based interventions may have beneficial effects for pregnant women. Three small studies have demonstrated that MBIs are effective in reducing stress, anxiety, depressive symptoms, and emotional distress during pregnancy in healthy, non-clinical populations (Duncan and Bardacke 2010; Dunn et al. 2012; Vieten and Astin 2008). However, MBIs have not yet been tested as a treatment for clinically significant distress, including anxiety disorders or depressive disorders in pregnant or postpartum women.
There are several reasons to hypothesize that MBCT may be particularly applicable to the treatment of both subclinical and clinical levels of GAD in pregnant women: (1) Women overwhelming prefer non-pharmacological interventions during pregnancy. MBCT provides a safe and potentially effective alternative to psychotropic medication. (2) Rumination is a predominant feature of GAD. MBCT has been shown to reduce maladaptive rumination (Heeren and Philippot 2011; Michalak et al. 2011). (3) The nature of worry in GAD is future directed and therefore training in present-focused mindful awareness may provide a useful alternative way of responding for individuals with GAD (Roemer and Orsillo 2002). (4) Individuals with GAD have difficulty in regulating their emotions, as shown by greater negative reactivity to and poorer understanding of emotions (Mennin et al. 2005; Tull et al. 2009). Practicing mindfulness with non-judging awareness may increase distress tolerance, and promote emotional self-regulation (Greeson and Brantley, 2009). (5) Individuals with GAD typically have a habituated pattern of avoiding distressing internal experiences (Hayes et al. 1999; Orsillo et al. 2010). According to Greeson and Brantley (2009), “Mindfulness practice offers a fundamentally different way of responding to anxiety in which it is “deliberately noticed, allowed, and responded to with openness, curiosity, acceptance, and self-compassion. Therefore, practicing mindfulness may interrupt habitual avoidance, increase distress tolerance, and promote greater behavioral flexibility in response to anxiety, ultimately leading to less anxiety and overall distress” (Greeson and Brantley 2009 p. 176).
The burden and consequences of anxiety during pregnancy is substantial and there is a recognized need for effective alternatives to pharmacological treatment of anxiety in pregnancy. Thus we developed the Coping with Anxiety through Living Mindfully (CALM) Pregnancy intervention, an application of MBCT adapted specifically to pregnant women with anxiety. The content of the CALM Pregnancy intervention derives primarily from MBCT developed by Segal, Williams, and Teasdale (2002; 2013), which has its foundation in Kabat-Zinn’s (1990) MBSR program. CALM Pregnancy also draws upon the recent work of Neff (2012) and Germer (2012) regarding self-compassion, Roemer and Orsillo’s mindfulness/acceptance-based approach to the treatment of GAD (Hayes-Skelton et al. 2013; Roemer et al. 2008; Treanor et al. 2011; Orsillo and Roemer 2011), and Bardacke’s (2012) application of MBSR to preparation for childbirth. The intervention is further informed by the general literature regarding conceptualizations of GAD (e.g., Behar et al. 2009; Garfinkle and Behar 2012; Roemer & Orsillo 2002), and from consultation with experts in the areas of MBIs, CBT, and interventions with pregnant women.
The CALM Pregnancy intervention teaches alternative ways of responding to anxiety symptoms and includes mindfulness techniques, cognitive approaches, education about anxiety and depression and cognitive distortions specific to anxiety and depressive disorders, along with homework to encourage the use of mindfulness in everyday life through regular practice. Box 1 provides an overview of the intervention content. Content related to anxiety is the main focus of the CBT component; however, due to the high co-occurrence of depression with anxiety, depression-related content is also included, and content focused on anxieties commonly experienced by pregnant women, such as anxiety regarding delivery, the health of the fetus/infant, and the responsibilities of motherhood are included. Explicit self-compassion meditation is included in the CALM Pregnancy curriculum based on recent research suggesting that self-compassion may be a particularly important component in mindfulness-based treatments and that it is significantly correlated with less anxiety and depression and overall greater psychological health (Davis and Hayes 2011; Neff 2003; Kuyken et al. 2010; van Dam et al. 2011). Lastly, mindful yoga and postures for sitting and lying down meditations are adapted to accommodate pregnant women’s comfort and some of the class and home practice meditations incorporate mindfulness of the developing fetus.
Box 1. Content of the CALM Pregnancy program.
-
Psychoeducation about:
Stress physiology, anxiety, and depression
Mindfulness
How mindfulness can be utilized in pregnancy, labor and delivery, and parenting, and in everyday life to facilitate more adaptive responses to challenges and distress
-
Mindfulness practices
Body scan
Mindful yoga
Various sitting meditations
Walking meditation
Mindfulness in everyday life practices
Mindfulness of baby practices
-
Cognitive exercises
Self-observation and self-monitoring skills development
Decentering from automatic thoughts
Self-compassion meditation
Home practice – 30 to 45 minutes 6 days a week
Reading material provided from a variety of sources on aspects of mindfulness practice
The purpose of this open-treatment pilot study was to: (a) evaluate the feasibility and acceptability of delivering the CALM Pregnancy intervention to pregnant women with GAD or high levels of anxiety or worry symptoms, (b) determine the preliminary efficacy of the intervention on reduction of anxiety, worry, and depression and on increasing mindfulness and self-compassion, (c) assess the relationship between mindfulness and anxiety and depression over time, and (d) elicit participant feedback about the intervention.
Methods
Participants
Participants were 24 pregnant women recruited from the prenatal clinic of a large urban teaching hospital, local obstetric and mental health provider referral, and self-referral. Potential participants were initially screened via questionnaire to determine initial eligibility. Screen-positive women were subsequently interviewed in person for final eligibility determination. Eligibility criteria at screening were: (a) 1 to 27 weeks gestation at the start of the study intervention, (b) age 18 or above, (c) English-speaking, (d) elevated anxiety symptoms as determined by either a score of ≥ 45 on the Penn State Worry Questionnaire (PSWQ: Meyer et al. 1990) or ≥ 10 on the GAD-7 (Spitzer et al. 2006), (e) no greater than moderate level of depression as determined by a score of < 15 on the Patient Health Questionnaire -9 (PHQ-9; Kroenke et al. 2001); (f) no suicidal ideation as indicated on question 9 on the PHQ-9; and (g) agreed to be contacted for follow-up interview.
Final eligibility was determined by interview by the study psychologist and included the following criteria: (a) Beck Anxiety Inventory (BAI: Beck and Steer 1990) severity score of ≥ 11 indicating elevated level of anxiety symptoms and/or PSWQ ≥ 45 indicating elevated worry symptoms and/or met criteria for GAD as determined by the MINI International Neuropsychiatric Interview (MINI; Sheehan et al. 1998); and (b) willing and able to participate in at least seven of the eight CALM Pregnancy intervention sessions. Exclusion criteria included the following: (a) met DSM-IV-TR criteria for bipolar disorder, substance dependence disorder, or psychotic disorder (current or lifetime); (b) met DSM-IV-TR criteria for an Axis I anxiety disorder other than GAD that was more problematic or severe than GAD symptoms or diagnosis. (c) initiated pharmacological treatment for depression and/or anxiety within past 6 weeks or, if currently on medication for anxiety and/or depression, had increased dose within past 6 weeks or planned to increase dose or change medications during study time frame; (d) was currently participating in psychotherapy > 2 times per month; (e) had received cognitive behavior therapy in the past 12 months; or (f) had participated in any formal stress reduction program that included regular meditation practices in the past 12 months.
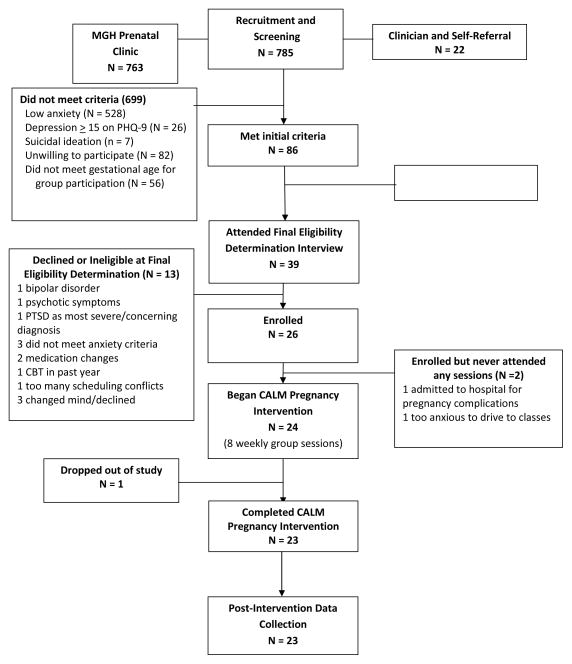
A total of 785 women completed the screening questionnaire during the time period from September 2012 through January 2013, 763 from the hospital clinic and 22 from clinician- or self-referral. Of those screened, 257 were positive for anxiety and/or worry (elevated PSWQ or GAD-7). Of these, 171 were excluded according to additional eligibility criteria and 47 were unable to be contacted. Thus, 39 women were eligible and agreed to the diagnostic interview. Thirteen women were ineligible following the diagnostic interview and final eligibility determination, or declined further participation in the study. Twenty-six women were enrolled in the study. Two women never attended any of the intervention sessions: one due to hospitalization for pregnancy complications and one because she felt too anxious to drive to the classes. A third woman withdrew from the study after attending two sessions stating that she no longer wanted to participate. Diagram 1 shows the flow of study participants from recruitment through post-intervention.
Diagram 1.
Flow of Participants through Study
Outcomes and Measures
The baseline questionnaire set included questions regarding demographics, current stressors, health, and past mental health treatment. The post-intervention questionnaire set included updates to the baseline questions, as well as three open-ended questions to elicit participants’ qualitative feedback concerning their participation in the intervention. Participants were asked: “What, if anything, do you think you learned from the CALM Pregnancy program?” “What aspects of the program were most and least helpful?” and “What suggestions do you have for improving the program?”
To assess feasibility and acceptability of the intervention and study protocol, we recorded participant attendance at intervention sessions and assessed home practice adherence rates via weekly participant homework logs. Post-intervention qualitative data provided further data regarding the acceptability of the intervention and protocol.
The following instruments were utilized for screening and data collection:
The Penn State Worry Questionnaire (PSWQ; Meyer et al. 1990) is a widely used 16-item self-report questionnaire designed to assess the generality, excessiveness and uncontrollability of worry. The PSWQ has been reported to discriminate patients with GAD from community controls and patients with other anxiety disorders (Brown et al. 1992) and has demonstrated sensitivity to change across both 6-week and 12-week therapeutic interventions for GAD (Borkovec and Costello 1993). Higher scores represent a greater degree of worry. The PSWQ was administered at screening, baseline, and post-intervention. In this sample, the internal consistency as assessed by Cronbach’s alpha yielded coefficients of 0.84 at screening and 0.83 at both baseline and post-intervention.
The GAD-7 (Spitzer et al. 2006) is a seven-item self-report questionnaire designed to screen for and measure anxiety severity in GAD. Items are scored on a 0 to 3 scale, with aggregate scores ranging from 0 to 21. Scores ≥10 indicate the possibility of an anxiety disorder (Spitzer et al. 2006; Kroenke et al. 2007). The GAD-7, with a Cronbach’s alpha of 0.89 for the scores of this sample, was used for initial eligibility screening.
The Patient Health Questionnaire – 9 (PHQ-9; Kroenke et al. 2001) is a nine-item self-report scale based on the nine diagnostic criteria for major depressive disorder in the DSM-IV-TR. The PHQ-9 score ranges from 0 to 27 with a score ≥ 15 indicating a moderately severe level of depressive symptoms. The PHQ has been validated for use in pregnant populations (Spitizer et al. 2000). It was administered at screening with a Cronbach’s alpha of 0.71.
The MINI International Neuropsychiatric Interview (MINI; Sheehan et al. 1998) is a structured psychiatric diagnostic interview for use in determining Axis I DSM-IV-TR diagnoses. The MINI has demonstrated concurrent validity with the much longer Structured Clinical Interview for DSM Diagnoses (Sheehan et al. 1997) as well as with the Composite International Diagnostic Interview for ICD-10 (Lecrubier et al. 1997). The MINI was administered by the study psychologist at both baseline and at post-intervention to determine psychiatric diagnoses.
The Beck Anxiety Inventory (BAI; Beck and Steer 1990) is a 21-item self-report scale developed to measure clinical anxiety level while reliably discriminating anxiety from depression. Each item is scored on a 4-point Likert-type scale with total scores ranging from 0 to 63. A cut-off score of 11 is recommended as the most appropriate cutoff for identifying clinically relevant subthreshold anxiety (Karsten et al. 2011). The BAI was administered at baseline, at weeks 3, 5, and 7, and at post-intervention with reliability coefficients of 0.89, 0.72, 0.85, 0.71, and 0.82 for the five time points respectively.
The Beck Depression Inventory – Second Edition (BDI-II; Beck et al. 1996) is a well-established 21-item self-report instrument designed to assess the presence and severity of depressive symptoms during the past two weeks in correspondence with criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (4th ed, text rev; DSM-IV-TR; American Psychiatric Association, 2000). The BDI-II was administered at baseline, at weeks 3, 5, and 7, and at post-intervention with reliability coefficients of 0.85, 0.75, 0.90, 0.88, and 0.91 for the five time points respectively.
The Self-Compassion Scale (SCS; Neff 2003) is a 26-item self-report measure of self-compassion with acceptable test-retest reliability (Neff 2003; Neff et al. 2007). The SCS assesses both the positive and negative aspects of the three main components of self-compassion: (a) self-kindness versus self-judgment, (b) common humanity versus isolation, and (c) mindfulness versus over-identification. Responses are rated on a five-point scale with higher scores indicating greater self-compassion. Internal consistencies for the current study were .82 at baseline and .85 at post-intervention.
The Mindfulness Attention Awareness Scale (MAAS; Brown and Ryan 2003) is a 15-item scale purported to measure dispositional mindfulness, with higher scores indicating higher mindfulness levels. The MAAS was administered at baseline, weeks 3, 5, and 7, and at post-intervention. Internal consistencies for the five time points were 0.88, 0.91, 0.92, 0.95, and 0.94 respectively.
Procedures
Screening and recruitment
All study procedures were approved by the hospital internal review board prior to the start of the study. Participants were recruited via two strategies. The first entailed screening at the prenatal clinic of Massachusetts General Hospital. Pregnant women were given a recruitment screening packet by the unit clerk upon visit check-in. The packet contained a brief description of the study, a screening consent form with permission to be contacted for a follow-up interview if responses to the questionnaire indicated initial study eligibility, and a screening questionnaire that included screens for anxiety and depression. In the second recruitment strategy, women were recruited via self- or clinician referral through advertisements placed in large obstetric practices in the Boston area. Study information was also provided to mental health clinicians appropriate to the target population. Clinicians in all sites were encouraged to refer potentially eligible women. A screening packet was sent to interested women who contacted the study office.
Screen-positive women who gave permission to be contacted were scheduled for a final eligibility determination visit with the study psychologist. After obtaining signed informed consent, the psychologist administered a final eligibility interview that included the BAI and the MINI. Women who met final eligibility criteria were given a set of baseline questionnaires to complete and were scheduled to receive the CALM Pregnancy intervention.
Intervention description
The CALM Pregnancy intervention was provided in eight weekly two-hour group sessions following the basic MBCT session structure described by Segal et al. (2002; 2013). Three groups of 6 to 12 women per group were conducted. Sessions were held in a large carpeted room at an academic institution, with yoga mats, meditation cushions, chairs arranged in a circle, and healthy snacks provided. Sessions included didactic presentations, group exercises aimed at cognitive skill development, formal meditation practices, and leader-facilitated group inquiry and discussion. Approximately 30–40 minutes of daily home practice of formal and informal mindfulness practices was assigned and encouraged between classes. MP3s of formal meditations were provided for home practice and relevant readings were provided. In addition to daily formal practice, for five of the weeks, participants were encouraged to also practice an abbreviated mindfulness practice (the Three-Minute Breathing Space) three times per day. During the last three weeks of the intervention they were encouraged to also utilize the Three-Minute Breathing Space “whenever they noticed unpleasant thoughts or feelings.” The CALM Pregnancy intervention was delivered by a licensed independent clinical social worker (LK) with over ten years’ experience in leading mindfulness groups and who had completed MBSR training as well as a five-day MBCT training course. All sessions were audiotaped and reviewed for the purposes of treatment fidelity monitoring and ongoing supervision by the principal investigator (JHG), an experienced psychiatric/mental health advanced practice nurse with expertise in treating perinatal anxiety and depression and who also completed professional-level training in both MBSR and MBCT.
Data collection
The MINI was administered by the study psychologist at baseline and at one week post-intervention to determine psychiatric clinical diagnoses. Participants completed the PSWQ, BAI, BDI-II, SCS, and MAAS at baseline and post-intervention. The BAI, BDI-II, and MAAS were also administered at weeks 3, 5, and 7 of the intervention in order to assess the relationship of mindfulness to the anxiety and depression over time. Session attendance was recorded and weekly home practice logs were completed by participants and collected weekly. Qualitative feedback regarding participants’ experiences in the CALM Pregnancy intervention was collected via questionnaire at one week post-intervention.
Analysis
Descriptive statistics were used to describe sample demographics, prevalence of specific DSM-IV-TR diagnoses, and participant intervention attendance and adherence rates. Means and standard deviations were computed for all scores at relevant study time points. A series of repeated ANOVAs were conducted to assess changes from baseline to post-intervention on each of the outcome variables. A series of Pearson correlations between the MAAS scores and the anxiety symptom levels and between MAAS and depression symptom levels were conducted at each of the five time points (baseline; weeks 3, 5, and 7 of the intervention; and post-intervention). Clinical significance at post-intervention was operationalized by the recommended reliable change index and cut-off points (Jacobson and Truax 1991; Vollestad et la. 2011) for the BAI, BDI-II, and PSWQ. See Table 1. Qualitative data were analyzed by the principal investigator (JHG) using qualitative content analysis (Sandelowski 2000). First the researcher read the answers to the open-ended questions and assigned a code to each concept. Second, similar concepts were identified and collapsed into categories. Exemplar quotes that captured the essence of each category were identified.
Table 1.
Reliable change index and recommended cut-off points for the BAI, PSWQ, and BDI-II
| Instrument | Reliable Change Index | Cut-Off Point |
|---|---|---|
| BAI | 10 | ≤ 10 |
| PSWQ | 7 | ≤ 47 |
| BDI-II | 8.46 | ≤ 14 |
Results
Baseline Characteristics
Of the 24 participants who attended any of the intervention sessions, 16 (66.7%) were recruited via the hospital screening method and eight (33.3%) were clinician- or self-referred. Mean age at baseline was 33.5 years (SD 4.40), range 27 to 45 years. Number of weeks pregnant at baseline ranged from 6 to 27 weeks (Mean = 15.54; SD 5.83). Seven women were in the first trimester and 17 in the second trimester at baseline. Eighteen were pregnant with their first child, and six with their second child. The majority of participants were white/non-Hispanic (n = 18, 75%), three (12.5%) were Asian, two (8.3%) were Hispanic, and one indicated “other” as her racial/ethnic group. One participant was single and the rest were married or living with the father of the baby. Participants were well-educated, with 15 (62.5%) holding a graduate or professional degree, six (25%) holding a college degree, and 3 (12.5%) having some college.
Of the 24 participants, 17 (70.8%) met criteria for GAD at baseline. GAD was the sole diagnosis for 11 of them, whereas six participants also met criteria for the following comorbid diagnoses (although GAD symptoms were reported as most severe or concerning for all): two major depressive disorder and specific phobia, one dysthymia, one post-traumatic stress disorder, one agoraphobia, one specific phobia, and one dysthymia, agoraphobia, and social phobia. Seven participants did not meet criteria threshold for any current DSM-IV-TR Axis I disorder and were included due to burden of generalized anxiety symptoms or worry symptom levels that met inclusion criteria. Seven of the 24 study participants had a history of psychotropic medication use prior to the current pregnancy and one had taken psychotropic medication early in the pregnancy but had discontinued it prior to the study onset. Two participants were on selective serotonin reuptake inhibitors (SSRIs) throughout their study participation: One had started a SSRI seven weeks prior to enrollment and continued on the same dose throughout the study, and another continued on a stable dose of an SSRI which she had been on for the past 10 years. Nine additional participants reported a history of psychotropic medication use prior to the current pregnancy but were not currently taking medication during the study time frame. Sixteen participants reported a history of receiving psychotherapy in the past. Four participants (including one who dropped out of the study), all of whom had been in psychotherapy for the past year or longer, were continuing during the current pregnancy at a frequency of less than twice per month.
Feasibility and Acceptance of Intervention and Procedures
Most participants (n = 21; 87.5%) attended at least six of the eight intervention sessions. Two participants attended five sessions, and one participant dropped out after attending two classes. The mean number of sessions attended by the 23 completers was 6.96 sessions. With the exception of the one drop-out, all participants completed the study intervention and all data collection points. Participants completed home practice of formal meditation practice an average of 4.12 out of six days per week (range 1.9 to 6.6 days per week). Participants practiced the scheduled Three-Minute Breathing Space an average of 12.3 times per week (range 1 to 23 times per week) during the course of the study, and an average of 6 times over the course of the last three weeks “whenever they noticed unpleasant thoughts or feelings” with a wide range of 0 to 63 times. Responses to the qualitative questions at post-intervention revealed that women regarded their experiences in the CALM Pregnancy intervention to be overwhelmingly positive. All 23 completers expressed that they enjoyed participating and all noted several aspects of the program which they found helpful.
Efficacy of the Intervention
Pre/post analyses included only the 23 women who completed the study. Results of the repeated measures ANOVA indicated statistically significant improvements (p < .01) on the BAI, PSWQ, BDI-II, SCS, and MAAS, with strong effect sizes (eta-squares) for all outcomes. Means, standard deviations, eta-squared, significance levels, and percent change are presented in Table 2. Pearson correlations between the MAAS and the BAI at the five time points (baseline; weeks 3, 5, and 7 of the intervention; and post-intervention) indicated that the only time-point with a significant meaningful relationship was at post-intervention (r = −.482, p = .020). Pearson correlations between the MAAS scores and BDI-II levels at the five time-points demonstrated a quadratic effect. There were no significant relationships at the first three time points. However, at week seven of the intervention, a statistically significant inverse relationship (r = − .54; p = .01) occurred, demonstrating a 128% increase in the strength of the correlation from week five to week seven of the intervention. This significant correlation was maintained to the post-intervention time point (see Table 3).
Table 2.
Results of Repeated Measures ANOVAs
| Variable | Cronbach’s α | M (SD) | p. | η2 | % Δ |
|---|---|---|---|---|---|
| BAI* | <.001 | .36 | −47.65 | ||
| BL | .88 | 12.13 (8.56) | |||
| Post | .82 | 6.35 (4.95) | |||
| PSWQ | <.001 | .50 | −14.87 | ||
| BL | .83 | 59.30(8.92) | |||
| Post | .83 | 50.48(10.23) | |||
| MAAS | .019 | .22 | +15.34 | ||
| BL | .88 | 51.04(9.50) | |||
| Post | .94 | 54.87(10.62) | |||
| SCS | < .001 | .58 | +14.87 | ||
| BL | .81 | 31.44(7.92) | |||
| Post | .90 | 39.65(9.63) | |||
| BDI-II | < .001 | .56 | −46.16 | ||
| BL | .85 | 11.87(5.67) | |||
| Post | .91 | 6.39(6.36) |
BL = Baseline, Post = Post-Intervention
Table 3.
MAAS Correlations with BDI-II and BAI
| Time | BDI-II | BAI | ||
|---|---|---|---|---|
| r | p | r | p | |
| Baseline | −.37 | .07 | −.17 | .43 |
| Week 3 | −.11 | .62 | −.14 | .52 |
| Week 5 | −.36 | .09 | −.06 | .80 |
| Week 7 | −.54 | .01 | −.28 | .21 |
| Post-Intervention | −.52 | .01 | −.48 | .02 |
In regards to psychiatric diagnoses, of the 16 completers who met diagnostic criteria for GAD at baseline, only one continued to meet criteria at post-intervention. In addition, the two participants who also met criteria for major depression at baseline no longer met criteria at post-intervention. Comorbid baseline diagnoses of agoraphobia, PTSD, social phobia, specific phobia, and dysthymia diagnoses remained at post-intervention. One participant who had no diagnosis at baseline met criteria for social anxiety disorder at post-intervention. Clinical significance of effects at post-intervention is presented in Table 4 with percentages of participants who recovered, improved, showed no change, or deteriorated.
Table 4.
Individual change data for completer sample (n = 23)
| BAI N (%) |
PSWQ N (%) |
BDI-II N (%) |
|
|---|---|---|---|
| In clinical range at baseline | 11 (47.8%) | 23 (100%) | 23 (100%) |
| Recovered | 7 (63.6%) | 9 (39.1%) | 11 (47.8%) |
| Reliably improved | 2 (18.2%) | 7 (30.4%) | 5 (21.7%) |
| No change | 2 (18.2) | 6 (26.1%) | 5 (21.7%) |
| Deteriorated | 0 | 1 ( 4.3%) | 2 (8.7%) |
Participant Feedback
All completers of the study (N = 23) answered open-ended questions regarding their experience participating in the CALM Pregnancy intervention including what, if anything they learned, what aspects of the program were most and least helpful, and what suggestions they had for program improvement. Several common codes were revealed in participants’ overlapping responses to the questions regarding what they learned from the CALM Pregnancy intervention and what aspects of the program were most helpful to them. Analysis of the data revealed seven categories: (1) skill building, (2) connection, (3) universality, (4) acceptance and self-kindness, (5) decreased reactivity, (7) cognitive changes, and (8) insight. Table 5 presents the categories, description of each category, and selected statements exemplifying each category. In response to suggestions for improving the program, six participants proposed having partners included in at least one session so that they could benefit from what was taught and support the women in their new practices. In addition, a few participants recommended ongoing support for their new mindfulness practices. In response to the question “What aspects of the program were least helpful?” several participants reported that the amount of home practice “required” felt like “too much” at times, although some qualified by saying the home practice was never-the-less helpful in learning the practices. One woman remarked that having to do home practice created more anxiety for her.
Table 5.
Categories (presented from most commonly described to less common), description of each category, and selected statements exemplifying each category.
| Category (percentage of sample making statement fitting category) | Description of Category | Selected Examples of Significant Statements |
|---|---|---|
| Skill Building (83.4%) | Learning specific skills to help with anxiety | Program gave me certain tools to help cope with daily stresses and pain that I experience. |
| Learning different techniques to manage stress and anxiety, as one technique doesn’t necessarily fit for all people, or for one person at all times. I like that I have been given the option of doing yoga, a body scan, or just three minutes of breathing depending on what I need at any given time. | ||
| I came away from this group with new techniques and tools to learn safer and calmer ways to deal with stressors and anxiety I experience on a daily basis. | ||
| Connection (66.7%) | Connecting and learning from others | I really enjoyed the interaction in the class and the sharing of ideas and situations. It was great to hear other people talk about their experiences and how they overcame obstacles etc. I felt I could relate to a lot of the other women in the class. |
| I found that the group setting was helpful and comforting. I felt very supported and the other women were nonjudgmental. | ||
| It was great being around women who were in a similar situation to me and I liked being able to talk about my own experiences as well as get insight from them about certain situations and ideas. | ||
| I enjoyed the small and large group discussions the most as they provided an opportunity to relate and connect to the other women in the program. | ||
| Universality (58.3%) | Learning that they were not alone | I found that I’m not alone in my anxious thoughts, which was really helpful. |
| I learned that this a shared human experience and I’m not the only one who suffers from it. | ||
| After the first day I felt significantly better just knowing that there were many other women just like myself that had extremely similar feelings. | ||
| Acceptance and Self-Kindness (58.3%) | Learning to be kinder to self and more accepting of thoughts and feelings, especially those pertaining to anxiety | When I do feel anxious at times, I am more accepting of it as part of who I am rather than beating myself up about it. |
| I’ve learned to be more gentle to myself, to accept my feelings (especially the bad ones. | ||
| I also really appreciated the self-kindness meditation and message – it’s very easy for me to think critically about myself and I’m learning how to be more accepting. | ||
| I learned that by being mindful and willing to experience whatever is happening, the levels of anxiety and stress that normally affect me can diminish. | ||
| When I do feel anxious at times, I am more accepting of it as part of who I am rather than beating myself up about it. | ||
| I accept my thoughts. I accept that they can come and go. I’m aware of them. This new way of dealing with my worries has decreased the “bad” thoughts I used to have a lot! | ||
| Decreased Reactivity (41.7%) | Learning to be less reactive | I used to spiral to a level of loss of control over my feelings, now I can catch it and reel it back in to process better. |
| I learned to deal with stress and pain in a much calmer way. | ||
| The program helped me take a step back and slow down before reacting to certain situations that arise in my daily life. | ||
| If I experienced a stressful moment in the past I would kind of lose composure and react negatively. Now I take space and use tools I learned to keep stress down as best I can | ||
| Cognitive Changes (29.2%) | Learning to think differently | I’ve realized that not all my thoughts are factual. Many times those thoughts create unpleasant feelings and reactions. Before the CALM pregnancy program I would let those thoughts consume me. Now I try to bring myself to the present moment and how I feel at the present. |
| I have realized that my thoughts affect my feelings and reactions so I try to be more aware of thought patterns and also to recognize that my thoughts are not realities. | ||
| I learned better skills for evaluating my thoughts/feelings/emotions and, when they were negative, catching them early before they started to spiral. I realized how much I tended to catastrophize small events and I have gotten much better at looking at the big picture and not focusing in on these small things that tended to stress me out before. | ||
| I don’t let my thoughts cycle in a negative loop. I breathe and let them pass. | ||
| Insight (29.2%) | Developing insight into how they personally cope with anxiety | I am glad I participated as it made me focus on myself and become very reflective of the ways in which anxiety (and how I cope) plays out in my life. |
| I have learned how to better understand my thoughts and body. How my thoughts can trigger feelings and how those thoughts are not always factual. | ||
| I learned about how I personally cope with stress and stressful situations, which in turn will hopefully help inform how I confront them moving forward. (329) |
Discussion
This study, to the best of our knowledge, is the first to examine a treatment specifically designed for, and administered to, pregnant women with GAD or prominent symptoms of generalized anxiety. Results of this open-label study indicate that the CALM Pregnancy intervention is feasible and acceptable to pregnant women with anxiety, and these preliminary results suggest that it may be effective as well. Participants who completed the intervention showed statistically and clinically significant improvements in anxiety, worry and depression severity and concurrent significant increases in self-compassion and mindfulness. In regards to clinical diagnoses, an exceptionally high rate of recovery (15 out of 16; 93.8%) was found for the participants who met GAD criteria at baseline, and the two participants who also met criteria for MDD at baseline were no longer depressed post-intervention. In addition, there were clinically significant improvements on self-report measures. Eighty-two percent of participants who scored in the clinical range for anxiety at baseline (n = 11) showed improvements consistent with recovery or reliable improvement at post-intervention. For those in the clinical range of worry at baseline (n = 23), 69.6% showed recovery or reliable improvement, and for those in the clinical range for depression at baseline (n = 23), 69.6% likewise showed recovery or reliable improvement. These clinically significant results suggest that the CALM Pregnancy intervention constituted a highly effective treatment for participants. The effectiveness of the intervention is further supported by the strong effect sizes found in regards to all study outcomes. Though preliminary, these findings are, as a whole, encouraging.
As an explorative effort to investigate mindfulness as a potential mechanism of action, we analyzed correlations between mindfulness and anxiety, and mindfulness and depression, at five points across the study time frame. Although there were no significant correlations between mindfulness and anxiety or depression at baseline, by the seventh week of the intervention, a statistically significant correlation emerged between mindfulness and depression, and at post-intervention a significant correlation between mindfulness and anxiety emerged. This pattern of an increase in mindfulness as participants progressed through the intervention and the correlated decrease in anxiety and depression observed, suggests that mindfulness may play a role in the reduction of depression and anxiety over time. Research that uses mediational analyses are indicated to further explore the hypothesis that increases in mindfulness are responsible for decreases in anxiety and depression.
Feasibility and acceptability of study intervention and procedures were amply demonstrated by the ability to recruit, screen, enroll, and retain participants. Despite the limited gestational time frame in which women were eligible for participation in the intervention, we were able to recruit adequate numbers of women to run three separate groups during the five months of the study recruitment. Although the majority of participants were recruited through hospital prenatal clinic screening, recruitment through clinician- or self-referral was particularly effective as these women were selectively identified and thus had a much higher rate of eligibility and enrollment. Study participation required a commitment of a weekly two-hour group session for eight weeks, as well as 30 to 40 minutes of home practice daily during the intervention phase of the study. That so many women made this commitment despite busy lives suggests that women are looking for a non-pharmacologic approach for management of their anxiety and are willing to make a commitment to such an intervention. Only one participant dropped out of the study, which further supports the conclusion that this intervention is acceptable to pregnant women. Although there was great variation in amount of home practice completed, qualitative responses indicate that women used home practice in a flexible way corresponding to their time, interest, and, perhaps need. Regardless of amount of home practice, all participants benefitted from the intervention on one or more outcomes, which suggests that effectiveness may be related to factors other than amount of time spent practicing mindfulness. This should be explored in future research.
Responses to open-ended questions at post-intervention revealed that participants felt that the intervention was helpful to them in several ways. Participants identified that they learned specific skills that helped them increase mindfulness, acceptance and self-kindness, and to decrease reactivity. In addition they reported increased insight and positive cognitive changes. These responses suggest that the intervention is consistent with the theoretical underpinnings of mindfulness training in general and MBCT specifically, both of which aim to cultivate present-moment awareness with an attitude of acceptance, openness, and compassion (Greeson & Brantley 2009). Participants’ suggestion for further ongoing support for mindfulness practice reflects is an important consideration for further development of the intervention. As women move from pregnancy into the postpartum stage and beyond, consolidation and adaptation of mindfulness practices in the context of mothering is important (Bogels et al. 2010; Duncan et al. 2009), and may well benefit from continued support and further learning.
In addition to anxiety/worry criteria required for study entry, all study participants had a substantial burden of depressive symptoms as indicated by elevated BDI-II scores at baseline. This high level of comorbid anxiety and depression among pregnant women should be considered in intervention development and delivery. The CALM Pregnancy intervention seemed to be effective for depression as it was for anxiety and worry, even though depression itself was only minimally addressed. Thus, a variety of symptoms were improved by the mindfulness practices taught in the intervention. Transdiagnostic treatments for anxiety and other emotional disorders have gained increased attention and empirical study in recent years (Farchione et al. 2012; Norton and Barrera 2013; Wilamowska et al. 2010). The transdiagnostic application of MBIs across a range of psychiatric diagnoses and symptoms provides the opportunity for versatility and feasibility of dissemination and accessibility, potentially increasing access to evidence-based treatments for anxiety. Given the effects of the CALM Pregnancy intervention on depression symptoms and diagnoses, further trials should be conducted to test the intervention with women with a primary diagnosis of depression and to specifically trial the intervention with more diagnostically diverse group of pregnant women.
The group format of the CALM Pregnancy intervention has considerable benefits. Effective group interventions are generally more resource- and cost-effective than individual therapy. In addition, the group format may provide added therapeutic benefits as indicated by participant feedback regarding the benefits of connecting and learning from other women going through similar experiences. Future research, however, should include active comparison groups that control for group support in order to examine the contribution of the group support to intervention effectiveness versus mindfulness as the hypothesized key mechanism of action.
Although these findings are promising, it is important to consider the considerable methodological limitations of this pilot study. The study sample was small and lacked sufficient statistical power. The lack of a control or comparison group prevents any definitive attribution of improvements in outcomes to the intervention. Self-report measures are subject to response bias; however the use of diagnostic interviews mitigated this limitation to some degree. The study psychologist was blind to screening results at baseline, but because all women received the intervention, diagnostic assessments were not blind to condition. The sample was made up of predominantly well-educated, older women, and therefore may not be generalizable to other women. Another limitation is the potential confound of current participant treatment: one participant had started on an SSRI eight weeks before entering the trial, and three completers were continuing in psychotherapy (every two weeks or less) which they had been in for between one and ten years. However, inclusion of these women provides some suggestion of a potential adjunctive role of this mindfulness-based intervention to usual treatment. Despite these limitations, there were never-the-less several strengths of the study that increased its external validity and importance. The sample was drawn from a community-based obstetric population and was made up of women who were suffering clinically significant psychiatric distress, the majority of whom were not identified and were not currently receiving mental health care. The use of a structured diagnostic interview in addition to using reliable and valid self-report measures strengthens the study. The qualitative findings add important information regarding how women perceived the intervention and provide dimension and depth to the quantitative findings.
Within the context of these limitations, the current findings are encouraging and further research is warranted to test the intervention in randomized, controlled trials with larger and more diverse samples, and with longer follow-up.
In conclusion, MBCT, in the form of the CALM Pregnancy intervention, shows considerable promise as a feasible, acceptable, and effective treatment option for pregnant women with anxiety. If shown to be effective in more rigorous trails, it could provide a safe, non-pharmacologic alternative to psychotropic medication use in pregnancy or augmentation strategy in women treated with medication, thus filling a critical treatment gap. Pregnancy offers the opportunity to develop mindfulness practices which may be particularly helpful in diminishing distressing cognitive and physiological symptoms of anxiety. Because anxiety and depressive symptoms are associated with negative obstetric and infant outcomes, the CALM Pregnancy intervention could potentially benefit not only on maternal psychological well-being and functioning, but also on the course of pregnancy, the developing fetus/infant, maternal postpartum adjustment, and the development of the mother-infant relationship.
Acknowledgments
This research was funded in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1R21HD065156-01) to Dr. Goodman. We would also like to extend our gratitude to the volunteer staff who facilitated recruitment at Massachusetts General Hospital Obstetrics and to the women who participated in the study. Special thanks to L. Klein for creating the CALM acronym.
Contributor Information
Janice H. Goodman, Email: jgoodman@mghihp.edu, MGH Institute of Health Professions, School of Nursing, 36 1st Ave, Boston, MA 02129, Phone: 617-726-0862, Fax: 617-724-6321
Anthony Guarino, MGH Institute of Health Professions, School of Nursing.
Kerry Chenausky, MGH Institute of Health Professions, School of Nursing.
Lauri Klein, MGH Institute of Health Professions, School of Nursing.
Joanna Prager, MGH Institute of Health Professions, School of Nursing.
Rebecca Petersen, MGH Institute of Health Professions, School of Nursing.
Avery Forget, MGH Institute of Health Professions, School of Nursing.
Marlene Freeman, Massachusetts General Hospital, Harvard Medical School.
References
- Adewuya AO, Ola BA, Aloba OO, Mapayi BM. Anxiety disorders among Nigerian women in late pregnancy: a controlled study. Arch Women Ment Health. 2006;9:325–8. doi: 10.1007/s00737-006-0157-5. [DOI] [PubMed] [Google Scholar]
- Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20:189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- Alvik A, Heyerdahl S, Haldorsen T, Lindemann R. Alcohol use before and during pregnancy: a population-based study. Acta Obstet Gynecol Scand. 2006;85:1292–8. doi: 10.1080/00016340600589958. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Publishing; Washington, DC: 2004. text rev. [Google Scholar]
- Andersson L, Sundstrom-Poromaa I, Wulff M, Astrom M, Bixo M. Depression and anxiety during pregnancy and six months postpartum: a follow-up study. Acta Obstetricia et Gynecologica. 2006;85:937–44. doi: 10.1080/00016340600697652. [DOI] [PubMed] [Google Scholar]
- Andersson L, Sundström-Poromaa I, Wulff M, Åström M, Bixo M. Implications of antenatal depression and anxiety for obstetric outcome. Obstet Gynecol. 2004;104:467–76. doi: 10.1097/01.AOG.0000135277.04565.e9. [DOI] [PubMed] [Google Scholar]
- Arch JJ, Ayers CR, Baker A, Almklov E, Dean DJ, Craske MG. Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behav Res Ther. 2013;51:185–96. doi: 10.1016/j.brat.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Bardacke N. Mindful birthing: training the mind, body, and heart for childbirth and beyond. HarperOne; New York: 2012. [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. The Psychological Corporation; San Antonio: 1990. [Google Scholar]
- Beck AT, Steer RA, Brown GK. BDI-II: 2nd Edition Manual. The Psychological Corporation; San Antonio: 1996. [Google Scholar]
- Behar E, DiMarco ID, Hekler EB, Mohlman J, Staples AM. Current theoretical models of generalized anxiety disorder (GAD): conceptual review and treatment implications. J Anxiety Disord. 2009;23:1011–23. doi: 10.1016/j.janxdis.2009.07.006. [DOI] [PubMed] [Google Scholar]
- Bogels SM, Lehtonen A, Restifo K. Mindful parenting in mental health care. Mindfulness. 2010;1:107–20. doi: 10.1007/s12671-010-0014-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. J Consult Clin Psychol. 1993;61:611–9. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- Borri C, Mauri M, Oppo A, Banti S, Rambelli C, Ramacciotti D, Montagnani MS, Camilleri V, Cortopassi S, Bettini A, Ricciardulli S, Rucci P, Montaresi S, Cassano GB. Axis I psychopathology and functional impairment at the third month of pregnancy: results from the Perinatal Depression-Research and Screening Unit (PND-ReScU) Study. J Clin Psychiatry. 2008;69:1617. doi: 10.4088/jcp.v69n1012. [DOI] [PubMed] [Google Scholar]
- Britton JR. Maternal anxiety: course and antecedents during the early postpartum period. Depress & Anxiety. 2008;25:793–800. doi: 10.1002/da.20325. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res. 2011;187:441–53. doi: 10.1016/j.psychres.2010.08.011. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J Altern Complement Med. 2009;15:593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- Coelho HF, Murray L, Royal-Lawson M, Cooper PJ. Antenatal anxiety disorder as a predictor of postnatal depression: A longitudinal study. J Affect Disord. 2011;129:348–53. doi: 10.1016/j.jad.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Coleman VH, Carter MM, Morgan MA, Schulkin J. United States obstetrician-gynecologists’ accuracy in the simulation of diagnosing anxiety disorders and depression during pregnancy. J Psychosom Obstet & Gynecol. 2008;29:173–84. doi: 10.1080/01674820701833265. [DOI] [PubMed] [Google Scholar]
- Craigie MA, Rees CS, Marsh A, Nathan P. Mindfulness-based cognitive therapy for generalized anxiety disorder: a preliminary evaluation. Behav Cog Psychother. 2008;36:553–68. [Google Scholar]
- Duncan LG, Bardacke N. Mindfulness-based childbirth and parenting education: promoting family mindfulness during the perinatal period. J Child Fam Stud. 2010;19:190–202. doi: 10.1007/s10826-009-9313-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan LG, Coatsworth JD, Greenberg MT. A model of mindful parenting: implications for parent-child relationships and prevention research. Clin Child Fam Psychol Rev. 2009;12:255–70. doi: 10.1007/s10567-009-0046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25:141–8. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn C, Hanieh E, Roberts R, Powrie R. Mindful pregnancy and childbirth: effects of a mindfulness-based intervention on women’s psychological distress and well-being in the perinatal period. Arch Women Ment Health. 2012;15:139–43. doi: 10.1007/s00737-012-0264-4. [DOI] [PubMed] [Google Scholar]
- Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. Br Med J. 2001;323:257–60. doi: 10.1136/bmj.323.7307.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness-based cognitive therapy for generalized anxiety disorder. J Anxiety Disord. 2008;22:716–21. doi: 10.1016/j.janxdis.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Faisal-Cury A, Menezes PR. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Women Ment Health. 2007;10:25–32. doi: 10.1007/s00737-006-0164-6. [DOI] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, Gallagher MW, Barlow DH. Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behav Ther. 2012;43(3):666–78. doi: 10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjorback LO, Arendt M, Ørnbøl E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy - a systematic review of randomized controlled trials. Acta Psychiatr Scand. 2011;124:102. doi: 10.1111/j.1600-0447.2011.01704.x. [DOI] [PubMed] [Google Scholar]
- Garfinkle E, Behar E. Advances in psychotherapy for generalized anxiety disorder. Curr Psychiatry Rep. 2012;12:203–10. doi: 10.1007/s11920-012-0263-1. [DOI] [PubMed] [Google Scholar]
- Germer CK. Cultivating compassion in psychotherapy. In: Germer CK, Siegal RD, editors. Wisdom and compassion in psychotherapy: deepening mindfulness in clinical practice. The Guilford Press; New York: 2012. pp. 93–110. [Google Scholar]
- Giardinelli L, Innocenti A, Benni L, Stefanini M, Lino G, Lunardi C, Svelto V, Afshar S, Bovani R, Castellini G, Faravelli C. Depression and anxiety in perinatal period: prevalence and risk factors in an Italian sample. Arch Women Ment Health. 2012;15:21–30. doi: 10.1007/s00737-011-0249-8. [DOI] [PubMed] [Google Scholar]
- Glover V, O’Connor T. Maternal anxiety: its effect on the fetus and the child. Br J Midwifery. 2006;14:663–7. [Google Scholar]
- Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. 2009;36:60–69. doi: 10.1111/j.1523-536X.2008.00296.x. [DOI] [PubMed] [Google Scholar]
- Goodman JH, Tyer-Viola L. Detection, treatment, and referral of perinatal depression and anxiety by obstetrical providers. J Womens Health (Larchmt) 2010;19:477–90. doi: 10.1089/jwh.2008.1352. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Keyes K, Simuro N. Mental disorders and nicotine dependence among pregnant women in the United States. Obstet Gynecol. 2007;109:875–83. doi: 10.1097/01.AOG.0000255979.62280.e6. [DOI] [PubMed] [Google Scholar]
- Greeson J, Brantley J. Mindfulness and anxiety disorders: developing a wise relationship with the inner experience of fear. In: Didonna F, editor. Clinical handbook of mindfulness. Springer; New York: 2009. pp. 171–187. [Google Scholar]
- Grigoriadis S, de Camps Meschino D, Barrons E, Bradley L, Eady A, Fishell A, Mamisachvili L, Cook GS, O’Keefe M, Romans S, Ross LE. Mood and anxiety disorders in a sample of Canadian perinatal women referred for psychiatric care. Arch Womens Ment Health. 2011;14:325–33. doi: 10.1007/s00737-011-0223-5. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Hayes RM, Wu P, Shelton RC, Cooper WO, Dupont WD, Mitchel E, Hartert TV. Maternal antidepressant use and adverse outcomes: a cohort study of 228,876 pregnancies. Am J Obstet Gynecol. 2012;207:49e1–49e9. doi: 10.1016/j.ajog.2012.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hayes-Skelton SA, Roemer L, Orsillo SM. A randomized clinical trial comparing an acceptance-based behavior therapy to applied relaxation for generalized anxiety disorder. J Consult Clin Psychol. 2013 doi: 10.1037/a0032871. (May 6, Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron J, O’Connor TG, Evans J, Golding J, Glover V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80:65–73. doi: 10.1016/j.jad.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010;78:169–83. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, Worthington JJ, Pollack MH, Simon NM. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiatry. 2013 doi: 10.4088/JCP.12m08083. (March 13 Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley KM, Caulfield LE, Sacco LM, Costigan KA, Dipietro JA. Psychosocial influences in dietary patterns during pregnancy. J Am Diet Assoc. 2005;105:963–6. doi: 10.1016/j.jada.2005.03.007. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–9. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Bantam Dell. A Division of Random House, Inc; New York: 1990. Full catastrophe living: using the wisdom of your body and mind to face stress, pain and illness. [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, Lenderking WR, Santorelli SF. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149:936–43. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Karsten J, Nolen WA, Penninx B, Hartman CA. Subthreshold anxiety better defined by symptom self-report than by diagnostic interview. J Affect Disord. 2011;129:236–43. doi: 10.1016/j.jad.2010.09.006. [DOI] [PubMed] [Google Scholar]
- Keng S, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev. 2011;31:1041–56. doi: 10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mcgonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, Chapleau MA, Paquin K, Hofmann SG. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. 2013;33:763–71. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- Kim YW, Lee SH, Choi TK, Suh SY, Kim B, Kim CM, Cho SJ, Kim MJ, Yook K, Ryu M, Song SK, Yook KH. Effectiveness of mindfulness-based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Dep and Anxiety. 2009;26:601–6. doi: 10.1002/da.20552. [DOI] [PubMed] [Google Scholar]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behav Res Ther. 2007;45:2518–26. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–W77. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, Evans A, Radford S, Teasdale JD, Dalgleish T. How does mindfulness-based cognitive therapy work? Behav Res Ther. 2010;48:1105–12. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Lee AM, Lam SK, SM, Chong CS, Chui HW, Fong DY. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol. 2007;110:1102–12. doi: 10.1097/01.AOG.0000287065.59491.70. [DOI] [PubMed] [Google Scholar]
- Majid SA, Seghatoleslam T, Homan HA, Akhvast A, Habil H. Effect of mindfulness based stress management on reduction of generalized anxiety disorder. Iranian J Publ Health. 2010;41:24–28. [PMC free article] [PubMed] [Google Scholar]
- Mauri M, Oppo A, Montagnani MS, Borri C, Banti S, Camilleri V, Cortopassi S, Ramacciotti D, Rambelli C, Cassano GB. Beyond “postpartum depressions”: specific anxiety diagnoses during pregnancy predict different outcomes: results from PND-ReScU. J Affect Disord. 2010;127:177–84. doi: 10.1016/j.jad.2010.05.015. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Heimberg RG, Turk CL, Fresco DM. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behav Res Ther. 2005;43:1281–1310. doi: 10.1016/j.brat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–95. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Michalak J, Holz A, Teismann T. Rumination as a predictor of relapse in mindfulness-based cognitive therapy for depression. Psychol Psychother. 2011;84:230–236. doi: 10.1348/147608310X520166. [DOI] [PubMed] [Google Scholar]
- Miller JJ, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- Mota N, Cox BJ, Enns MW, Calhoun L, Sareen J. The relationship between mental disorders, quality of life, and pregnancy: findings from a nationally representative sample. J Affect Disord. 2008;109:300–4. doi: 10.1016/j.jad.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Neff KD. The science of self-compassion. In: Germer CK, Siegel RD, editors. Wisdom and compassion in psychotherapy: deepening mindfulness in clinical practice. The Guilford Press; New York: 2012. pp. 79–92. [Google Scholar]
- Neff KD. The development and validation of a scale to measure self-compassion. Self & Identity. 2003;2:223. [Google Scholar]
- Norton PJ, Barrera TL. Transdiagnostic versus diagnosis-specific CBT for anxiety disorders: a preliminary randomized controlled noninferiority trial. Depress Anxiety. 2012;29(10):874–82. doi: 10.1002/da.21974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsillo SM, Roemer L. The mindful way through anxiety. The Guilford Press; New York: 2011. [Google Scholar]
- Otte C. Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues Clin Neurosci. 2011;13:413–21. doi: 10.31887/DCNS.2011.13.4/cotte. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM, Salters-Pedneault K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: evaluation in a randomized controlled trial. J Consult Clin Psychol. 2008;76:1083–9. doi: 10.1037/a0012720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM. An open trial of an acceptance-based behavior therapy for generalized anxiety disorder. Behav Ther. 2007;38:72–85. doi: 10.1016/j.beth.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM. Expanding our conceptualization of and treatment for generalized anxiety disorder: integrating mindfulness/acceptance-based approaches with existing cognitive-behavioral models. Clin Psychol Sci Pract. 2002;9:54–68. [Google Scholar]
- Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: a systematic review. J Clin Psychiatry. 2006;67:1285–98. doi: 10.4088/jcp.v67n0818. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:246–55. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JM, Teasdale JD. Mindfulness-based cognitive therapy for depression. Guilford Press; New York: 2002. [Google Scholar]
- Segal ZV, Williams JM, Teasdale JD. Mindfulness-based cognitive therapy for depression second edition. Guilford Press; New York: 2013. [Google Scholar]
- Seghatoleslam T, Homan H, Akhvast A, Habil H. Effect of mindfulness based stress management on reduction of generalized anxiety disorder. Iran J Public Health. 2011;41:24–8. [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett-Sheenhan K, Janavs J, Weiller E, Bonora LI, Keskiner A, Schinka J, Knapp E, Sheehan MF, Dunbar GC. Reliability and validity of the MINI International Neuropsychiatric Interview (M.I.N.I.): according to the SCID-P. European Psychiatry. 1997;12:224–41. [Google Scholar]
- Sipe WEB, Eisendrath SJ. Mindfulness-based cognitive therapy: theory and practice. Can J Psychiatry. 2012;57:63–9. doi: 10.1177/070674371205700202. [DOI] [PubMed] [Google Scholar]
- Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 2006;51:100–13. doi: 10.1177/070674370605100206. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams J, Lowe B. A brief measure for assessing generalized anxiety disorder - The GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire obstetrics-gynecology study. Obstet Gynecol. 2000;183:759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- Sutter-Dallay AL, Giaconne-Marcesche V, Glatigny-Dallay E, Verdoux H. Women with anxiety disorders during pregnancy are at increased risk of intense postnatal depressive symptoms: a prospective survey of the MATQUID cohort. Eur Psychiatry. 2004;19:459–63. doi: 10.1016/j.eurpsy.2004.09.025. [DOI] [PubMed] [Google Scholar]
- Swallow BL, Lindow SW, Masson EA, Hay DM. Psychological health in early pregnancy: relationship with nausea and vomiting. J Obstet Gynaecol. 2004;24:28–32. doi: 10.1080/01443610310001620251. [DOI] [PubMed] [Google Scholar]
- Teixeira J, Fisk NM, Glover V. Association between maternal anxiety in pregnancy and increased uterine artery resistance index: cohort based study. BMJ. 1999;318:153–7. doi: 10.1136/bmj.318.7177.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toneatto T, Nguyen L. Does mindfulness meditation improve anxiety and mood symptoms? A review of the controlled research. Can J Psychiatry. 2007;52:260–6. doi: 10.1177/070674370705200409. [DOI] [PubMed] [Google Scholar]
- Treanor M, Erisman SM, Salters-Pedneault K, Roemer L, Orsillo SM. Acceptance-based behavioral therapy for GAD: effects on outcomes from three theoretical models. Dep and Anxiety. 2011;28:127–36. doi: 10.1002/da.20766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Stipelman BA, Salters-Pedneault K, Gratz KL. An examination of recent non-clinical panic attacks, panic disorder, anxiety sensitivity, and emotion regulation difficulties in the prediction of generalized anxiety disorder in an analogue sample. J Anxiety Disord. 2009;23:275–82. doi: 10.1016/j.janxdis.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Udechuku A, Nguyen T, Hill R, Szego K. Antidepressants in pregnancy: a systematic review. Aust NZ J Psychiatry. 2010;44:978–96. doi: 10.3109/00048674.2010.507543. [DOI] [PubMed] [Google Scholar]
- Uguz F, Gezginc K, Kayhan F, Sari S, Buyukoz D. Is pregnancy associated with mood and anxiety disorders? A cross-sectional study. Gen Hosp Psychiatry. 2010 Mar-Apr;32:213–5. doi: 10.1016/j.genhosppsych.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Van Dam N, Sheppard SC, Forsyth JP, Earleywine M. Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. J Anxiety Disord. 2011;25:123–30. doi: 10.1016/j.janxdis.2010.08.011. [DOI] [PubMed] [Google Scholar]
- Van den Bergh BR, Van Calster B, Smits T, Van Huffel S, Lagae L. Antenatal maternal anxiety is related to HPA-axis dysregulation and self-reported depressive symptoms in adolescence: a prospective study on the fetal origins of depressed mood. Neuropsychopharmacology. 2007;33:536–545. doi: 10.1038/sj.npp.1301450. [DOI] [PubMed] [Google Scholar]
- Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Womens Ment Health. 2008;11:67–74. doi: 10.1007/s00737-008-0214-3. [DOI] [PubMed] [Google Scholar]
- Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Women Ment Health. 2008;11:67–74. doi: 10.1007/s00737-008-0214-3. [DOI] [PubMed] [Google Scholar]
- Vollestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: evaluation in a randomized controlled trial. Behav Res Ther. 2011;49:281–8. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Wenzel A. Anxiety in childbearing women: diagnosis and treatment. American Psychological Association; Washington, DC: 2011. [Google Scholar]
- Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, Barlow DH. Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depress Anxiety. 2010;27(10):882–90. doi: 10.1002/da.20735. [DOI] [PubMed] [Google Scholar]
- Zar M, Wijma K, Wijma B. Relations between anxiety disorders and fear of childbirth during late pregnancy. Clin Psychol Psychot. 2002;9:122–30. [Google Scholar]