Abstract
In the present study, 10 patients with ischemic stroke in the left hemisphere and six healthy controls were subjected to acupuncture at right Waiguan (TE5). In ischemic stroke subjects, functional MRI showed enhanced activation in Broadmann areas 5, 6, 7, 18, 19, 24, 32, the hypothalamic inferior lobe, the mamillary body, and the ventral posterolateral nucleus of the left hemisphere, and Broadmann areas 4, 6, 7, 18, 19 and 32 of the right hemisphere, but attenuated activation of Broadmann area 13, the hypothalamic inferior lobe, the posterior lobe of the tonsil of cerebellum, and the culmen of the anterior lobe of hypophysis, in the left hemisphere and Broadmann area 13 in the right hemisphere. In ischemic stroke subjects, a number of deactivated brain areas were enhanced, including Broadmann areas 6, 11, 20, 22, 37, and 47, the culmen of the anterior lobe of hypophysis, alae lingulae cerebella, and the posterior lobe of the tonsil of cerebellum of the left hemisphere, and Broadmann areas 8, 37, 45 and 47, the culmen of the anterior lobe of hypophysis, pars tuberalis adenohypophyseos, inferior border of lentiform nucleus, lateral globus pallidus, inferior temporal gyrus, and the parahippocampal gyrus of the right hemisphere. These subjects also exhibited attenuation of a number of deactivated brain areas, including Broadmann area 7. These data suggest that acupuncture at Waiguan specifically alters brain function in regions associated with sensation, vision, and motion in ischemic stroke patients. By contrast, in normal individuals, acupuncture at Waiguan generally activates brain areas associated with insomnia and other functions.
Keywords: neural regeneration, acupuncture and moxibustion, Waiguan (TE5), ischemic stroke, specificity of acupoints, functional MRI, cerebral function imaging, acupuncture, motion brain areas, grants-supported paper, photographs-containing paper, neuroregeneration
Research Highlights
(1) In ischemic stroke patients, acupuncture at Waiguan (TE5) specifically alters function in brain areas associated with sensation, vision, and motion.
(2) In normal controls, acupuncture at Waiguan generally activates brain areas directly associated with its main treatment effects including insomnia.
Abbreviations
SPM, Statistical Parametric Mapping; BA, Brodmann areas
INTRODUCTION
There is strong EVIDENCE that acupuncture at different acupoints, combination of acupuncture at acupoints, and acupuncture and sham-acupuncture at acupoints can induce both activation and deactivation of functional areas of the brain under physiological or pathological conditions[1,2,3,4,5,6]. However, there are limited data on changes in functional brain areas in response to acupuncture at one acupoint, and only few studies comparing cerebral function imaging of acupuncture at Shenmen (HT7) and Neiguan (PC6)[7,8,9]. Studies of Shenmen acupoint are also typically based on two cerebral functional imaging modalities, functional MRI and positron emission tomography, which are not comparable. Further, to our knowledge there are no studies comparing brain area functions after acupuncture at one acupoint under physiological or pathological conditions. Thus, further studies are required to investigate the effects of acupuncture at one acupoint on negative activation using related imaging and data processing detection methods.
Functional MRI is used to detect blood oxygen level changes in response to activity in functional areas of the brain to indirectly investigate brain function[9,10]. The general linear model Statistical Parametric Mapping (SPM) software package has been frequently used in functional MRI[11]. SPM2 software package is regarded as authoritative analysis software for cerebral function imaging processing[5,6,7,8]. Acupuncture therapy has been reported to improve outcomes after stroke[12,13,14]. Thus, using fMRI, we examined changes in activation/deactivation in functional brain areas induced by acupuncture at Waiguan (TE5) in ischemic stroke patients and healthy controls.
RESULTS
Quantitative analysis of participants
A total of 10 ischemic stroke patients and six healthy participants were included in the study.
Differences in activated brain areas between stroke patients and healthy controls after acupuncture at Waiguan
In stroke patients, acupuncture at Waiguan enhanced activation in the left Brodmann areas (BA) 5, 6, 7, 18, 19, 24, and 32, hypothalamus, and the ventral posterolateral nucleus, and the right BA4, 6, 7, 18, 19, and 32, compared with controls (Table 1, Figure 1A).
Table 1.
Comparison of enhanced activated brain areas, Brodmann areas, Montreal Neurological Institute Talairach, and activation intensity between stroke patients and healthy controls following acupuncture at Waiguan (TE5)
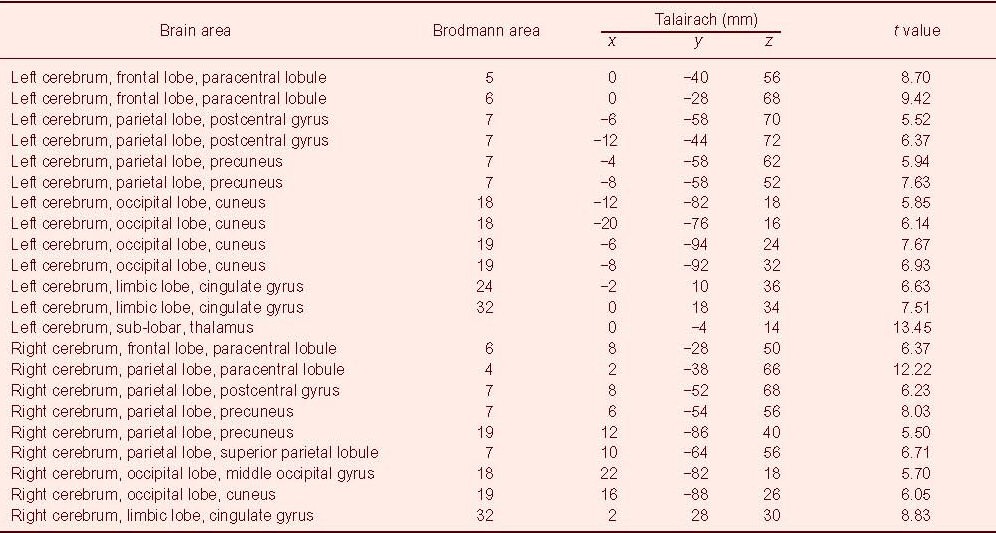
Figure 1.
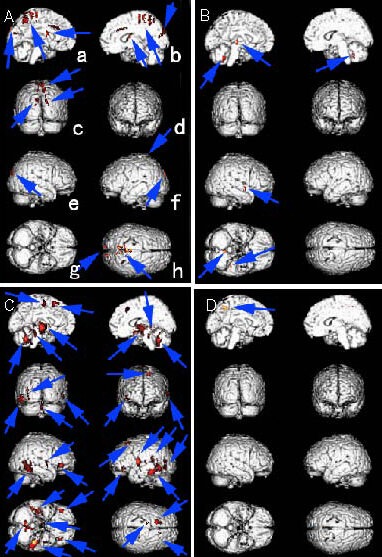
Activation/deactivation differences in functional areas of the brain between stroke patients and healthy controls following acupuncture at Waiguan (TE5).
Red region (arrows): differences in activation/deactivation.
a: Left sagittal plane of the median brain; b: right sagittal plane of the median brain; c: posterior plane of the brain; d: anterior plane of the brain; e: left view of the brain; f: right view of the brain; g: normal inferior of the brain; h: apical view of the brain (a–h in all pictures represent the same plane as Figure A).
(A) Enhanced activated brain areas in ischemic stroke patients compared with normal controls.
(B) Attenuated activated brain areas in ischemic stroke patients compared with normal controls.
(C) Enhanced deactivated brain areas in ischemic stroke patients compared with normal controls.
(D) Attenuated deactivated brain areas in ischemic stroke patients compared with normal controls.
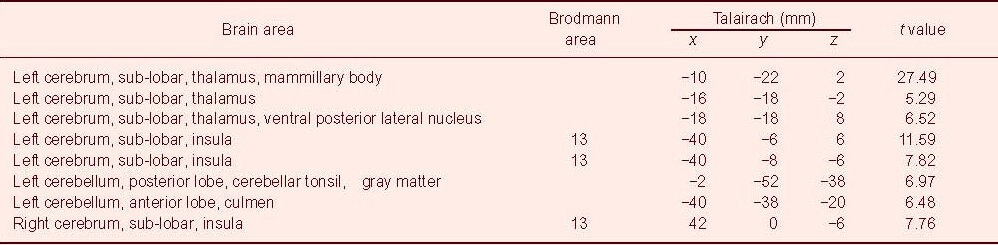
In addition, acupuncture at Waiguan attenuated activation in the left hemisphere, mainly including BA13, the hypothalamus, posterior lobe of the tonsil of cerebellum, and the culmen of the anterior lobe of hypophysis, and attenuated the activation in BA13 in the right hemisphere, in stroke patients compared with healthy controls (Table 2, Figure 1B).
Table 2.
Comparison of attenuated activated brain areas, Brodmann areas, Montreal Neurological Institute Talairach, and activation intensity between stroke patients and healthy controls following acupuncture at Waiguan (TE5)
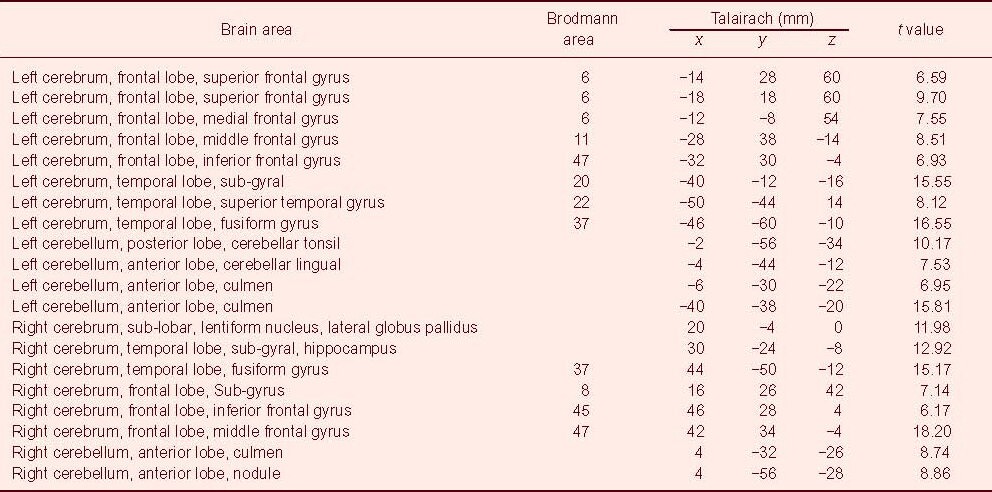
Differences in deactivated brain areas between stroke patients and healthy controls after acupuncture at Waiguan
In stroke patients, acupuncture at Waiguan enhanced deactivation in both hemispheres, including the left BA6, 11, 20, 22, 37, and 47, the culmen of the anterior lobe of hypophysis, alae lingulae cerebella, and the posterior lobe of the tonsil of cerebellum, and the right BA8, 37, 45, and 47, the culmen of the anterior lobe of hypophysis, nodule of the anterior lobe of hypophysis, inferior border of the lentiform nucleus, lateral globus pallidus, and the parahippocampal gyrus, compared with controls (Table 3, Figure 1C). In addition, acupuncture at Waiguan attenuated deactivation in BA7 (brain areas: left cerebrum, parietal lobe, precuneus, x/y/z (mm): –8/–54/46; t value: 6.65; Figure 1D) in stroke patients compared with controls.
Table 3.
Comparison of attenuated deactivated brain areas, Brodmann areas, Montreal Neurological Institute Talairach, and activation intensity between stroke patients and healthy controls following acupuncture at Waiguan (TE5)
DISCUSSION
The present study showed that acupuncture at the right Waiguan had different effects on brain activation/deactivation in ischemic stroke patients versus normal controls. Further, we found that multiple functional areas of the brain were activated or deactivated in both hemispheres in ischemic stroke patients and normal people. This is supported by the observation that when the human brain is conducting tasks (or no task), a variety of functional and anatomically separate areas can interact and coordinate to construct a network[4]. Our data also suggest that the central regulation of acupuncture at acupoints is achieved through network regulation.
Compared with healthy controls, acupuncture at Waiguan in ischemic stroke patients resulted in changes predominantly located in the lesioned hemisphere, including enhanced activation in brain areas associated with somatic sensation (BA5, 7), body movement (BA6), and vision (BA18, 19), but attenuated deactivation of brain areas associated with somatosensory cortices (BA7). These effects are consistent with results from clinical treatment studies[12], where acupuncture improves blood circulation in the cerebral cortex and promotes neurological function in lesioned brain areas.
Interestingly, we found that in stroke patients the enhanced activation and deactivation were predominantly detected in the BA6 region, which is likely associated with the location of the primary motor area[15]. The brain areas with enhanced activation were located near areas representing the forearm and upper arm, while the brain areas with enhanced deactivation were located near the wrist[15]. Acupuncture at Waiguan mainly promotes blood circulation of the cerebral cortex associated with the forearm and upper arm, resulting in reduced blood circulation stress in the cerebral cortex associated with the wrist. We also found evidence of enhanced deactivation in stroke patients in brain areas mainly associated with speech and endocrine function (e.g., BA22 and adenohypophysis, respectively)[15]. It is likely that acupuncture at Waiguan has no direct treatment effects on the improvement of speech function or the regulation of endocrine function as the blood circulation in the associated cortical brain region remained low.
Acupuncture at Waiguan also activated brain areas in the healthy hemisphere of stroke patients, similar to those in the lesioned hemisphere, including regions involved in somatic sensation (BA7), body movement (BA4, 6), and vision (BA18, 19)[15]. This may have contributed to enhanced compensation in the healthy hemisphere. In the stroke patients, the attenuated activation of brain areas following acupuncture at Waiguan mainly occurred in the right hypothalamus and inferior lobe of the insular lobe (BA13), and regions associated with internal organs activity, emotion, and circadian rhythm[15]. These results are similar to positron emission tomography cerebral function imaging of acupuncture at Deqi state[16], suggesting that acupuncture at Waiguan in normal people mainly activates brain areas directly associated with the main treatment effects of Waiguan.
In conclusion, we found that acupuncture at Waiguan exhibited varied effects on activation/deactivation of brain areas under physiological and pathological conditions. In ischemic stroke patients, acupuncture at Waiguan specifically acted on brain areas associated with sensation, vision, and motion. By contrast, in normal controls, acupuncture at Waiguan mainly activated brain areas directly associated with the main treatment effects of Waiguan, such as insomnia. Further studies using larger sample sizes, with observation of the clinical effects, and a control group with a combination of acupoints are required.
SUBJECTS AND METHODS
Design
A block design, neuroimaging study.
Time and setting
The experiment was performed at the MRI Center, Nanfang Hospital, China, from October 2008 to August 2010.
Subjects
Six right-handed healthy volunteers were recruited from the Southern Medical University in Guangzhou, China. The inclusion criteria were: (1) 21–28 years old undergraduate/postgraduate students; (2) non-smokers with regular eating habits without excessive consumption of liquid, tea or coffee, normal sleep, and normal body structure; (3) no acupuncture treatment in the one month prior to the experiment; (4) no metal in his/her body (such as heart stents); (5) no psychiatric history, such as claustrophobia; and (6) no contraindication for acupuncture, such as hemophilia. The subjects included three males and three females, with an average age of 23.33 ± 2.61 years (range 21–27 years).
Ten ischemic stroke patients were selected from the First Affiliated Hospital of Guangzhou University of Chinese Medicine. They were diagnosed according to diagnostic criteria in ICD-9 434 and ICD-8 433[17]. The inclusion criteria: (1) ischemic stroke in the left basal ganglia, with typical right hemiataxia (muscle strength of upper limb and lower limb less than four scores[18]) and sensory disability; (2) out of acute stage, with stable condition; (3) non-smokers with regular eating habits without excessive consumption of liquid, tea or coffee, normal sleep, and normal body structure; (4) treated with western medicine treatment within 1 month; (5) aged 40–65 years; and (6) right handed. Exclusion criteria: (1) course of disease longer than 1 year; (2) with acupuncture treatment within 1 month prior to the experiment; (3) with severe heart, liver, or kidney disease, or tumor; (4) severe aphasia or psychiatric history of dementia or claustrophobia; (5) pregnant women or those in lactation; (6) with metal in his/her body (such as heart stents); and (7) with contraindication for acupuncture, such as hemophilia. The patients included 9 males and one female, aged 56.10 ± 5.53 years (range 47–65 years), with course of disease of 5.30 ± 3.71 months (range 1–12 months).
Chinese Stroke Scale scores[18] were 18.20 ± 4.02 points (range 15–27 points). In addition, nine patients had hypertension and two had diabetes mellitus. Informed consent was obtained from all participants.
Methods
Acupuncture
All subjects received acupuncture at Waiguan of the right side. The Waiguan acupoint was located on the forearm, 2 cun (a unit of length that refers to the width of the interphalangeal joint of the thumb) above the transverse crease of the dorsum of the wrist, between the radius and ulna (Figure 2)[19].
Figure 2.
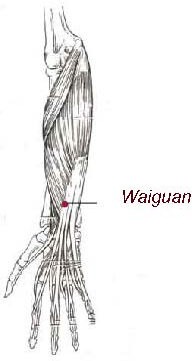
Waiguan (TE5) on the right side.
Acupuncture was performed by one physician, who had engaged in clinical acupuncture for more than three years. The tubes were purchased from Dongbang AcuPrime Co. (Exeter, England) and the 0.3 cm × 40 cm silver needles from Zhongyan Taihe Co. (Beijing, China). After routine sterilization, the physician held the tube using the left hand and tapped the end of the needle using the index finger of the right hand to insert its tip into the tube. The tube was then removed and the needle vertically punctured to a depth of 15 ± 2 mm. The handle of the needle was twirled to induce the needling sensation. Next, the physician manually applied an even reinforcing and reducing manipulation by twirling the needle ± 180°, at 60 times/min.
The acupuncture process was designed using a block method, with twirling and non-twirling stimulation alternated in 30-second blocks, and a total stimulation time of 6 minutes (Figure 3).
Figure 3.
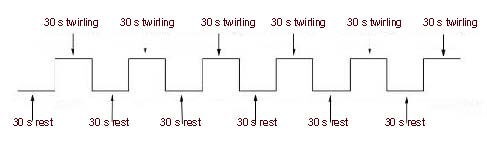
The acupuncture stimulation regime.
s: Second.
fMRI scan
fMRI scanning was performed with a 3.0 T whole-body MRI scanner (GE, Bethesda, MD, USA) and a standard head coil. The subjects used earplugs (Aearo Co., Hartford, CT, USA) and were blindfolded (Xinhua Tourism Co., Hangzhou, China). Each subject rested on the bed for 5–10 minutes before the scan. 3D anatomy images were collected with a T1-weighted 3D gradient echo-pulse fast spin sequence prior to acupuncture, with axial view T1 fluid-attenuated-inversion-recovery scan (repetition time, 2 300 ms; echo time, 21 ms; time of inversion, 920 ms; slice thickness, 6.0 mm; gap 1.0 mm for 20 layers for a total of 2 minutes 45 seconds; field of view, 24 cm × 18 cm; matrix, 320 × 256; number of excitations = 2; field of view echo train length, 9; and band width, 50).
Collection of blood oxygenation level-dependent functional images was conducted during acupuncture with a single provocation echo-planar imaging sequence with a gradient echo/echo-planar imaging/90 (90° pulse) (repetition time, 3 000 ms; echo time, 20 ms; flip angle, 90°; field of view, 24 cm × 24 cm; slice thickness, 6.0 mm; slice gap, 1.0 mm; matrix, 96 × 96; number of excitations = 1; phase per location, 130, 2 600 phases for 6 minutes and 30 seconds).
3D scanning was followed with an axial view 3D T1 fast spoiled gradient echo/20 T1 450 (repetition time, 4.6 ms; echo time, 3.3 ms; flip angle, 20°; field of view, 24 cm × 18 cm; slice thickness, 1.2–0.6 mm; band width, 25; matrix, 256 × 256; number of excitations = 1 for 248 layers in 6 minutes and 2 seconds).
Data analysis
The fMRI data were processed with the software SPM2 (http://www.fil.ion.ac.uk). (1) Slight movements of the head were corrected; (2) the images were normalized to the standard brain template of the Montreal Neurological Institute space; and then (3) smoothed spatially to reduce errors produced during imaging construction and eliminate tiny differences in brain structures among subjects; (4) The smoothed data were analyzed with a generalized linear model voxel by voxel. The t value of each voxel was calculated by two-sample t-tests, and statistical parametric mapping was based on the t values (P < 0.001, uncorrected, K > 30). Significant changes in different brain regions during stimulation and control conditions were identified and superimposed on the standard brain image mode of each subject's anatomic images[20]; (5) the activated/deactivated con file of the model of stroke patients and normal controls was further analyzed using a two-independent sample t-test. The remaining procedures were the same as those reported in (4). Central coordinates from statistical parameters determined using SPM software package were reproduced and input in Talairach Client (download from http://www.talairach.org/client.html) to obtain the anatomical location and the BA range of the functional areas of the brain[21], which were corrected by a physician of the neurological medicine department according to anatomic knowledge and clinical experience.
Acknowledgments:
We thank the support from healthy volunteers, ischemic stroke patients and their families. The authors also thank Yanping Chen and Shanshan Tang at the Imaging Center, Nanfang Hospital, China, for technical support.
Footnotes
Junqi Chen, Studying for doctorate.
Funding: This study was supported by the National Basic Research Program of China (973 Program), No. 2006CB504505, 2012CB518504; and the Third Key Construction Program of “211 Project” of Guangdong Province.
Conflicts of interest: None declared.
Ethical approval: The experiment was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou University of Chinese Medicine. The procedures were registered in the Chinese Clinical Trial Register (No. ChiCTRNRC-00000255).
(Edited by Zhang YT, Bai WZ/Su LL/Wang L)
REFERENCES
- [1].Luo YF. Shanghai: Shanghai Science and Technology Press; 2009. Shu Xue Xue. [Google Scholar]
- [2].Liang FR, Zeng F, Zhao L, et al. Specificity of acupoint effects and its fundamental laws. Zhongguo Zhen Jiu. 2009;29(2):129–132. [PubMed] [Google Scholar]
- [3].Lai XS, Huang Y. A cerebral functional definition on the specificity of acupoints, needling sensation and association of acupoints based on the acupoints-brain relation hypothesis? Zhongguo Zhen Jiu. 2007;27(10):777–780. [PubMed] [Google Scholar]
- [4].Su SJ, Zhao XF, Wang S. Application of cerebral function imaging in research on the acupoints specificity. Zhongguo Zhen Jiu. 2010;30(4):293–295. [PubMed] [Google Scholar]
- [5].Huang Y, Li TL, Lai XS, et al. Functional brain magnetic resonance imaging in healthy people receiving acupuncture at Waiguan versus Waiguan plus Yanglingquan points: a randomized controlled trial. Zhongxiyi Jiehe Xuebao. 2009;7(6):527–531. doi: 10.3736/jcim20090607. [DOI] [PubMed] [Google Scholar]
- [6].Xu FM, Xie P, Lv FJ, et al. Study on corresponding areas the liver and lung channels in brain with fMRI. Zhongguo Zhen Jiu. 2007;27(10):749–752. [PubMed] [Google Scholar]
- [7].Fu P, Jia JP, Wang W, et al. Effects of electroacupuncture at neiguan (PC 6) and Shenmen (HT 7) on brain functional imaging. Zhong Guo Zhen Jiu. 2005;25(1):61–63. [PubMed] [Google Scholar]
- [8].Fu P, Jia JP, Zhu J, et al. Effects of acupuncture at Neiguan (PC 6) on human brain functional imaging in different functional states. Zhongguo Zhen Jiu. 2005;25(11):784–786. [PubMed] [Google Scholar]
- [9].Wang K, Zeng XZ, Duan LP. Application of functional magnetic resonance imaging (fMRI) in the study of visceral hypersensitivity of the gut. Beijing Da Xue Xue Bao. 2006;38(6):657–659. [PubMed] [Google Scholar]
- [10].Chen P, Zhao BX, Qin W, et al. Study on the mechanism of acupuncture at Daling (PC7) for mental diseases by fMRI. Zhongguo Zhen Jiu. 2008;28(6):429–432. [PubMed] [Google Scholar]
- [11].Harting NV, Jensen JL. Spatial mixture modeling of fMRI data. Hum Brain Mapping. 2000;11:233–248. doi: 10.1002/1097-0193(200012)11:4<233::AID-HBM10>3.0.CO;2-F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wang QC. Beijing: Chinese TCM Publishing House; 2009. Acupuncture Therapeutics. [Google Scholar]
- [13].Wang LC, Wang ZY, Kang XZ, et al. Comparative study on effects of different acupuncture manipulation methods at Neiguan (PC6) on hand spasm in the patient of stroke. Zhongguo Zhen Jiu. 2008;28(7):503–506. [PubMed] [Google Scholar]
- [14].Chen XJ, Fang Z. Clinical experiences on acupuncture for treatment of cerebellar ataxia after stroke. Zhongguo Zhen Jiu. 2009;29(11):903. [PubMed] [Google Scholar]
- [15].Zhong SZ. Beijing: High Education Press; 2012. Systematic Anatomy. [Google Scholar]
- [16].Zhang GF, Huang Y, Tang CZ, et al. Characteristics of PET cerebral functional imaging during “Deqi” of acupuncture in healthy volunteers. Zhenci Yanjiu. 2011;36(1):46–51. [PubMed] [Google Scholar]
- [17].World Health Organization. WHO Monica Project: MONICA manual. Part IV: Event Registration. 1999 [Google Scholar]
- [18].Sun TK, Chiu SC, Yeh SH, et al. Assessing reliability and validity of the Chinese version of the stroke scale: scale development. Int J Nurs Stud. 2006;43(4):457–463. doi: 10.1016/j.ijnurstu.2005.07.004. [DOI] [PubMed] [Google Scholar]
- [19].General Administration of Quality Supervision, Inspection and Quarantine, the Standardization Administration, People's Republic of China. GB/T12346-2006. Name and location of Acupoints: Chinese National Standards. 2006 [Google Scholar]
- [20].Talairach J, Tournoux P. New York: Thieme; 1988. Co-planar Stereotaxic Atlas of the Human Brain. [Google Scholar]
- [21].Nopperncy U, Price CJ. Functional imaging of the semantic system: Retrieval of sensory-experienced and verbally learned knowledge. Brain Lang. 2003;84(1):120–133. doi: 10.1016/s0093-934x(02)00525-4. [DOI] [PubMed] [Google Scholar]


