Abstract
Objective
Minority populations in the United States are disproportionally affected by Human Papillomavirus (HPV) infection and HPV-related cancer. We sought to understand physician practices, knowledge and beliefs that affect utilization of the HPV vaccine in primary care settings serving large minority populations in areas with increased rates of HPV-related cancer.
Study Design
Cross-sectional survey of randomly selected primary care providers, including pediatricians, family practice physicians and internists, serving large minority populations in Brooklyn, N.Y. and in areas with higher than average cervical cancer rates.
Results
Of 156 physicians randomly selected, 121 eligible providers responded to the survey; 64% were pediatricians, 19% were internists and 17% were family practitioners. Thirty-four percent of respondents reported that they routinely offered HPV vaccine to their eligible patients. Seventy percent of physicians reported that the lack of preventive care visits for patients in the eligible age group limited their ability to recommend the HPV vaccine and 70% of those who reported this barrier do not routinely recommend HPV vaccine. The lack of time to educate parents about the HPV vaccine and cost of the vaccine to their patients were two commonly reported barriers that affected whether providers offered the vaccine.
Conclusions
Our study found that the majority of providers serving the highest risk populations for HPV infection and HPV-related cancers are not routinely recommending the HPV vaccine to their patients. Reasons for providers' failure to recommend the HPV vaccine routinely are identified and possible areas for targeted interventions to increase HPV vaccination rates are discussed.
Keywords: Human Papillomavirus Vaccine, HPV vaccine barriers, HPV vaccine and primary care providers
Introduction
Infection with human papillomavirus (HPV), the most common sexually transmitted infection, may result in cervical cancer and cancers of the anus, penis, vulva, vagina, and oropharynx, among others. From 2004-2008, there were approximately 33,000 cases of HPV-associated cancers diagnosed annually in the United States1. There are currently two HPV vaccines available and both are effective against the HPV types that cause up to 70% of HPV-related cancer cases1,2. Despite the availability of these safe and effective vaccines, HPV vaccine series initiation and completion rates remain low2. According to the 2012 National Immunization Survey-Teen (NIS-Teen), the overall initiation rate for the HPV vaccine series (first dose) was 54% for females with only 33% of girls completing the recommended three doses3. These rates were essentially unchanged from 20114. Of significance, eighty-four percent of unvaccinated girls reported a healthcare encounter where they received a vaccine other than the HPV vaccine3. A study based on 2008-2009 NIS-Teen data reported that white girls had a completion rate of 60% compared to 45% for blacks and 40% for Hispanics5. A trend analysis of NIS-Teen data for 2008 through 2011 reported that minority and below-poverty adolescents had consistently higher HPV vaccine series initiation than white and above-poverty adolescents. In this analysis, all race/ethnicity groups had completion percentages ranging from 32% to 40%6. Overall, these current HPV vaccination rates are well below the Healthy People 2020 goal of an 80% coverage level of 3 doses of HPV vaccine by age 13 to 15 years7. Although HPV vaccination rates among males are also low, coverage for boys who received at least one dose of HPV vaccine increased from 8.3% in 2011 to 20.8% in 2012, the first year after HPV vaccine was routinely recommended for boys8.
The cost of the HPV vaccine in the United States is approximately $130 per dose, $390 for the series and is covered by most private health insurance companies9. The HPV vaccine is included in the Vaccines for Children (VFC) Program which covers vaccine costs for children and teens without health insurance and for some children and teens who are underinsured9.
Understanding the reasons for disparities in HPV vaccination rates is crucial because the populations that exhibit lower rates of HPV vaccination completion, African-Americans, Hispanics, and those living below the federal poverty level, have higher HPV related cancer rates10-12. Failure to increase vaccine uptake in these groups may worsen the disparities in HPV-related cancers and fail to prevent many HPV related cancer cases.
Prior research has documented the important influence of the medical provider on vaccine decision making among parents and adults, and recent studies have confirmed the importance of the providers' role in parental consent for the HPV vaccine13-20 Given the significant link between provider recommendation and vaccine acceptance and completion, we sought to understand physician practices, beliefs and barriers that could affect their utilization of the HPV vaccine among their racial/ethnic minority patients at higher risk for HPV infection and HPV related cancer10-12,21.
Material and Methods
Study Design and Sampling Method
We conducted a cross-sectional study of primary care providers serving large minority populations at higher risk for HPV infection in Brooklyn, New York between November 2010 and January 2012. The provider population included pediatricians, family practitioners, and internal medicine physicians serving neighborhoods identified from the American Community Survey22 as having large minority populations (greater than 30%) and higher than the average rates of HPV related cancer cases according to the New York State Cancer Registry. Other inclusion criteria were: 1) New York State licensed general pediatrician, internal medicine or family practitioner, 2) minimum one-half of their patient population belong to minority populations (physician-reported), and 3) minimum one-third of their patient population were between the ages of 9 and 26 years old (physician-reported).
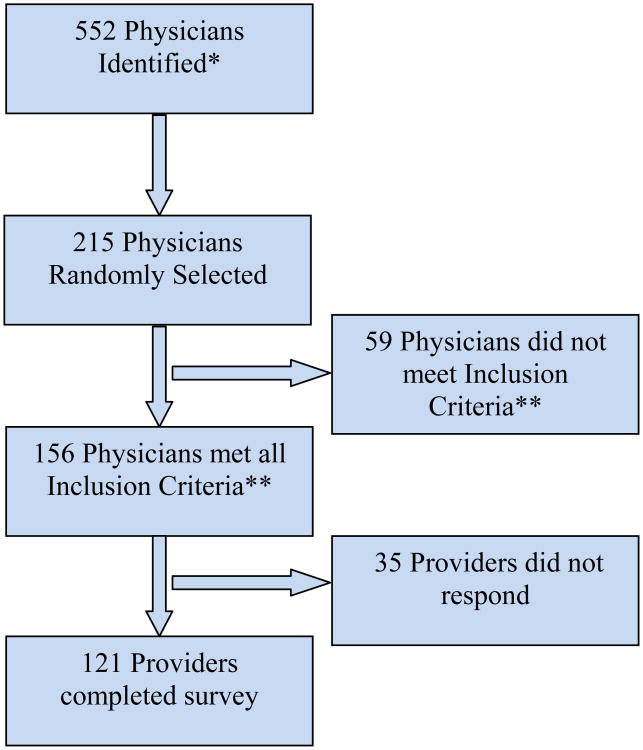
An inventory of providers was created from the New York State Department of Health provider database and professional medical organization membership lists (i.e. the local Chapters of the American Academy of Pediatrics). Multiple sources were used to increase the accuracy of this provider list to assure the inclusion of only actively practicing physicians, accurate practice location and specialty. This initial inventory was created based on practice location (zip code) and specialty (pediatrics, internal medicine, family practice). In total, 552 providers were identified. A stratified randomization using zip code of practice and type of provider (pediatrician, family practitioner or internist) was used to obtain a proportionally distributed number of providers in the study. A random sample of 120 was generated and then, based on number of refusals/ineligibles, generated again until the sample size was reached. The sample size was calculated using a 95% confidence interval and proportions of the different outcome (vaccination rates) ranging from 0.20 to 0.80. 59 providers randomly selected from the list to participate in the study did not meet the inclusion criteria described above (minimum one-half of their patient population belong to minority populations and minimum one-third of their patient population were between the ages of 9 and 26 years old). This information was not accessible before randomization and was self reported by providers or assessed by the research assistant (see figure 1).
Figure 1. Provider Recruitment Flow Chart.
* A list of 552 physicians was compiled from data obtained from the New York State Department of Health provider database (http://www.nydoctorprofile.com/dispatch) and Local Chapters of the American Academy of Pediatrics, and included pediatricians, family practitioners, and internal medicine physicians serving neighborhoods identified from the American Community Survey as having large minority populations (greater than 30%) and higher than the average rates of HPV related cancer cases according to the New York State Cancer Registry.
**Inclusion criteria: 1) New York State licensed general pediatrician, internal medicine or family practitioner, 2) minimum one-half of their patient population belong to minority populations (physician-reported), and 3) minimum one-third of their patient population were between the ages of 9 and 26 years old (physician-reported).
Survey
The survey utilized in this study was developed by a group of 3 physicians (2 pediatricians and an internist) and 2 behavioral scientists. The survey included the following domains: knowledge about HPV, HPV vaccine and cervical cancer, attitudes and beliefs towards the HPV vaccine, physician barriers to recommending HPV vaccines, perceived patient barriers for the HPV vaccine and systems that could improve current HPV vaccination rates. The survey also included information on demographic variables, medical training history and a description of the respondents' patient populations. The survey was piloted with a group of six physicians, including pediatricians, family practitioners and internists who had patient populations similar to the study populations of interest. The survey was piloted for readability and clarity of survey items. Based on the pilot results, questions were revised prior to implementation. In December 2011, the Advisory Committee on Immunization Practices' (ACIP's) recommendations on the routine use of HPV vaccine for boys were adopted. In December 2011 and January 2012 (when data collection concluded) we received responses from 5 providers. We assessed the HPV recommendation practices of these providers and compared them to those that responded to the survey before December 2011 to assess the potential effect of this policy change.
Physician perceived barriers to HPV vaccine recommendation
Potential perceived barriers to recommending HPV vaccine to an eligible patient and the frequency of this occurrence included the following options: lack of time, cost, competing priorities, language, cultural barriers, cultural beliefs, and concern about offending parents/guardians due to link between HPV vaccine and sexual transmission. Surveyed logistical barriers included equipment, personnel, office space, office staff, and availability of language- appropriate, comprehensive patient education materials.
Physicians' perceived patient barriers
Physicians' perceived patient barriers to HPV vaccine included responses of always, very often, sometimes, rarely, never, don't know/not sure to questions on cost to patient/insurance reimbursement, patient pain or discomfort, patient or parent views vaccine as unnecessary, parent believes all vaccines are unnecessary or dangerous, patient doesn't want to discuss HPV infection due to embarrassment or other reasons, parent doesn't have the time, national guidelines are unclear or don't apply to my patient population, Physician perceived barriers to patients' following through with vaccine recommendation included the following choices: concerns about vaccine safety, relationship of HPV to sexual activity, lack of compliance with preventive care visits in patient population and frequency of these perceived barriers in minority patient population.
Data Collection
Providers who were randomly selected to participate in the study received the survey by mail, together with an information sheet that explained the study, eligibility criteria and an incentive. The incentive, the most recent edition of the “Epidemiology and Prevention of Vaccine-Preventable Diseases: The Pink Book: Course Textbook,” was mailed at the same time as the survey with the goal of increasing response rates, as proposed by Delnevo et al.23,24 Providers were also given a pre-paid return envelope as part of the packet. If we did not receive the completed questionnaire approximately two weeks after the initial mailing, we contacted the physician by mail and by phone. This process was repeated at weeks 4 and 6 if there was no response. If there was no response after 8 weeks, we considered that provider a “non-responder”.
Data was manually entered into an access database by a research assistant and quality control was performed by the principal investigator to find and address any potential data entry problem. Analysis was performed using IBM SPSS Statistics® version 19. This study was approved by the State University of New York, Downstate Medical Center Institutional Review Board.
Results
We randomly selected 156 physicians from the list compiled and 121 (78%) returned a completed survey (see figure 1); 52% of respondents were female, and the average age was 54 (range 34-80). Sixty-one percent were born abroad and 33% reported a primary language other than English. Table 1 shows other characteristics of the study population. The 35 non-respondents were distributed similarly among the three provider type specialties.
Table 1. Socio-demographic characteristics of Brooklyn, New York physicians serving minority youth, 2010-2012 (N=121).
| Region of Origin | ||
| Latin America | 4% | |
| Caribbean | 10% | |
| Eastern Europe | 13% | |
| Asia | 18% | |
| United States | 38% | |
| Other | 17% | |
|
| ||
| Ethnicity | ||
| Hispanic | 12% | |
| Non-Hispanic | 47% | |
| Other* | 41% | |
|
| ||
| Race | ||
| Afro-Caribbean | 8% | |
| Black/African American | 14% | |
| Asian | 28% | |
| White | 50% | |
|
| ||
| Primary Language | ||
| Spanish | 6% | |
| Russian | 9% | |
| English | 62% | |
| Other** | 23% | |
|
| ||
| Ability to Speak English (n=46)*** | ||
| Well | 17% | |
| Very Well | 83% | |
|
| ||
| Graduate Medical School | ||
| US | 40% | |
| Outside the US | 60% | |
Reponses include any ethnicity the subject self reported.
15 other Primary languages were reported, the maximum number of physicians reporting each of those languages was 2.
Physicians who reported English as their primary language did not respond to this question.
Sixty-four percent reported pediatrics as their specialty, 19% internal medicine and 17% family practice. These rates were similar to the distribution of specialties in the compiled list of all providers in the area. In terms of practice setting, 36% of physicians worked in a private practice setting, 27% in a small group setting, 12% in community clinics and 25% in large public hospitals. Seventy percent of providers in the study reported having a patient population comprised of 75% or more of minorities, and 55% reported that at least 30% of their patient populations were immigrants. The largest minority populations served by these physicians included Hispanics or Latinos and Black or African Americans.
Only 41 (34%) reported recommending the HPV vaccine routinely (always or very often) to their eligible patients, 73 (60%) reported recommending the vaccine sometimes or rarely and 7 (6%) reported never recommending the HPV vaccine to their eligible patients. Five providers responded to the survey after the ACIP recommended the HPV vaccine for boys. Of these, 2 (40%) reported recommending the vaccine routinely, a similar rate to those who reported routinely recommending the vaccine before ACIP's new recommendations. Of the providers that reported recommending the HPV vaccine routinely (always or very often) 66% were pediatricians, 27% family practitioners and 7% internists (p=0.005). Providers that reported recommending the vaccine routinely were more likely to perceive a higher risk of HPV among the patient population (35% vs 24%), reported knowing the rates of HPV- related cancer in their population (29% vs 18%), reported having a lower rate of uninsured patients (7 % vs 14%) and reported a lower rate of immigrant patient populations (20% or less) although none of these were statistically significant. There were no associations between provider gender and routinely recommending the HPV vaccine (51% female, 48% male), provider age (mean age 54 vs. 54.2 years), primary language (61% English primary language, 65% other than English)) or country of origin (44% for those born in the US, 56% for those born abroad). Physician practices, beliefs and barriers by frequency of recommendation of the HPV vaccine are reported in Table 2. Ninety-five percent of providers in the study thought that HPV infection and its complications were serious enough to warrant a vaccine. All of the providers that recommended the vaccine routinely believed the HPV vaccine is “safe”, versus 88% of those that do not recommend the vaccine routinely (p=0.303). Of the 22% of providers that thought that children receive too many vaccines, 63% were pediatricians, 30% family practitioners and 7% internists (p=0.029).
Table 2. Provider Reported HPV Vaccine Knowledge, Beliefs, Practices and Barriers.
| Providers' reported Knowledge, Beliefs and Barriers for HPV vaccine | Overall % (n=121) | % of Providers Who Recommend Vaccine Routinely (n= 41) | % of Providers Who Do Not Recommend Vaccine Routinely (n= 80) | P Value |
|---|---|---|---|---|
| Knowledge and Beliefs | ||||
|
| ||||
| HPV infection and its complications are serious enough to warrant a vaccine | 95% | 100% | 93% | 0.07 |
| Offering the HPV vaccine provides an opportunity to discuss sex education | 88% | 87% | 88% | 0.88 |
| Not sure or thinks it is not yet known if vaccine provides long lasting immunity | 72% | 76% | 70% | 0.51 |
| Children receive too many vaccines | 22% | 10% | 29% | 0.10 |
|
| ||||
| Provider Barriers | ||||
|
| ||||
| No time to educate parents or patients about the vaccine | 66% | 59% | 70% | 0.44 |
| Cost of the vaccine is a barrier to recommending it | 46% | 49% | 45% | 0.69 |
| National or local guidelines for HPV vaccine are not clear | 45% | 49% | 43% | 0.59 |
|
| ||||
| Perceived Patient Barriers | ||||
|
| ||||
| Lack of preventive care visits impede HPV vaccine recommendation | 71% | 70% | 69% | 0.92 |
| Concerns with the safety of the vaccine or side effects | 53% | 40% | 60% | 0.25 |
| Parents/Patient would not like to discuss because HPV is a sexually transmitted infection | 48% | 42% | 49% | 0.45 |
Seventy-two percent of providers were unsure about, or thought the information was not yet known on, the long lasting immunity provided by the HPV vaccine. These providers who were unsure about long lasting immunity were less likely to recommend the vaccine routinely (70% vs 30%, p=0.335). When asked about the sexual component of HPV and its impact on HPV vaccine recommendation practices, 88% of providers in the study thought that offering the HPV vaccine provides an opportunity to discuss sex education with their patients between the ages of 9-17. Five percent thought that the vaccine might make their patients more likely to initiate sex, and 7% thought that condom use would decrease among their sexually active patients after receiving the HPV vaccine.
Providers in the study reported that the most common barrier impeding them from offering the vaccine was lack of time to educate parents or patients (66%). 70% of pediatricians reported this barrier, compared to 47% of family practitioners and 45% of internists (p=0.049) and 70% of those providers that do not recommend the vaccine routinely reported this barrier. Cost of the vaccine to their patients was reported as the next most common barrier to recommending the vaccine by providers in the study (46% reported this barrier); 46% of those that reported this barrier were pediatricians, 35% internists, and 19% family practitioners (p=0.034). Finally, nearly half (45%) of providers in the study thought that the national or local guidelines for HPV vaccine were not clear, and were an impediment for them to recommend the vaccine more often.
When asked about what they perceived as potential patient barriers to obtaining the vaccine, 71% of providers thought that their patient population's lack of preventive care visits limited their ability to recommend the HPV vaccine more often. This provider perceived patient barrier was most prevalent among internists (94%), followed by family practitioners (75%) and pediatricians (63%) (p=0.033). Fifty-three percent of providers believed that patients' and parents' concerns with the safety of the vaccine or side effects are a barrier for vaccination. This barrier was reported similarly across all provider types. Forty-eight percent of providers in the study thought that because HPV is a sexually transmitted infection, their patients or parents will not follow through with the recommendation to obtain the HPV vaccine. Among those that reported this barrier, 74% were pediatricians, 16% internists and 10% family practitioners (p=0.96).
Finally, when providers were asked about the most helpful methods to increase HPV vaccination in their practice, 84% thought that reminders for patients would help increase their HPV vaccine rates, 72% thought that providers would benefit from continuing education/workshops, and 56% thought that reminders for providers to offer the vaccine to their eligible patients would be beneficial.
Discussion
Our study shows that approximately one third of physicians who provide care to populations at high-risk of HPV infection report offering the HPV vaccine routinely to their eligible patients in accordance with national guidelines. These results are in contrast to a national survey of pediatricians and family practice physicians where 98% of pediatricians and 88% of family practice physicians reported offering HPV vaccine to their female patients25. Our results are cause for concern since prior studies have demonstrated that the strongest predictor of HPV vaccination is physician discussion and recommendation14,16. The importance of the provider recommendation is even greater for those with the highest risk of developing HPV-related cancers because many minority and immigrant patients rely on their healthcare provider as their main source of health-related information26,27. Many of the barriers to administering the HPV vaccination identified in our study are consistent with findings in prior studies28,29. However, the results of our study outline the most commonly reported barriers cited by physicians serving populations at high risk for HPV infection and links them to vaccine recommendation practices.
Seventy percent of the physicians in our study reported that the lack of preventive care visits for patients in the eligible age group limited their ability to recommend the HPV vaccine and 70% of those who reported this barrier do not routinely recommend HPV vaccine. Physicians in all three specialties reported this issue as a significant barrier, including 94% of internists, 75% of family practitioners and 63% of pediatricians. This finding is particularly noteworthy given results from the 2012 NIS-Teen Survey, where 84% of unvaccinated adolescent females reported a healthcare provider encounter and received a vaccine other than HPV vaccine. Given the additional preventive care visits required to complete HPV vaccination, primary care practitioners need to recognize every potential opportunity for vaccination and initiate HPV vaccination at any primary care visit.
The lack of time to educate parents about HPV and the HPV vaccine was one of the most common barriers reported by physicians that affected whether or not they offered the HPV vaccine to their patients. Sixty-one percent of providers from all specialties reported this barrier, including 70% of pediatricians. Other surveys have identified time to educate parents as a barrier, including a survey of Florida-based physicians serving Medicaid-enrolled adolescents30. Those who reported time constraints were less likely to recommend HPV vaccination to target group adolescent girls. As noted in this study, providing patient-focused educational materials and training to mid-level professionals may help address this barrier30.
The cost of the vaccine was reported as another common barrier that determined whether providers offered the vaccine to their patients. Given that the cost of the HPV vaccine itself, not including administrative fees, can be more than $400 for 3 doses, identifying mechanisms to assure that reimbursement for vaccines and vaccine administration are timely and efficient is imperative. A national survey of primary care providers found that physicians are dissatisfied with insurance payments for vaccine costs and administration fees regardless of payer type. In this study, some providers reported that they may delay offering vaccines due to uncertainty about insurance coverage for new vaccines until most payers are covering them31. Financial issues were also reported as a top barrier in a 2011 survey of a nationally representative sample of physicians practicing family medicine, pediatrics and obstetrics and gynecology32. Physician concerns with reimbursement for vaccine costs must be addressed in order to continue the success of past immunization efforts.
Given the importance of the provider recommendation on vaccine uptake, we have identified areas where targeted interventions may increase HPV recommendation and HPV vaccination rates. There is a need for interventions that address the issue of cost as a barrier to HPV vaccination. Options for obtaining low cost vaccines need to be provided, including provider education about how to obtain the vaccine for patients eligible for the Vaccines For Children program (VFC)9. In addition, issues of vaccine financing/reimbursement must be addressed as providers may be less likely to offer vaccine when reimbursement is uncertain or inadequate. The lack of preventive care visits cited as a barrier by physicians in our study population requires systems changes to reduce missed opportunities for providers to recommend HPV vaccine at all primary care visits. Office and clinic-based systems, such as chart reminders and reminder and recall systems, can maximize all eligible patient encounters as potential HPV vaccination opportunities. Targeted education for patients and parents should be developed that will assist physicians with education about the HPV vaccine and lessen the barrier of time limitations as well as address concerns about vaccine safety. Because almost seventy-five percent of responders felt that they, as providers themselves, would benefit from continuing education or workshops, future interventions must include education that targets providers of high-risk populations and provider strategies for addressing parental concerns.
There are some limitations to this study. The use of self-reported data leads to the possibility that respondents reported socially desirable responses. The survey assessed physician-reported behaviors and did not verify actual practices and the instrument may not have included all key barriers. Since there was a high percentage of foreign-trained physicians in the study population and the sample was limited to a specific geographic location, results may not be generalizable. Also, because the results included information obtained from those providers who chose to complete the survey, responses may be subject to selection bias; those who responded may have strong feelings about the HPV vaccine. The sample size was limited due to resource constraints, however this does not lessen the importance of study findings. Future research could explore these findings in more detail. Despite these limitations, this study identifies several potential opportunities for interventions that could lead to increased HPV vaccination.
Conclusion
Our study showed that the majority of providers serving the highest risk populations for HPV-related cancers are not routinely recommending the HPV vaccine to their patients. We identify specific barriers that can be addressed with targeted interventions that will help promote HPV vaccination in populations at high-risk for HPV-related cancer. Given the importance of the provider recommendation in vaccine uptake, provider-targeted interventions in areas serving patients most at risk for HPV-related cancers provide a significant opportunity to lessen ethnic, racial and economic disparities in HPV-related cancers.
Provider recommendations greatly influence decisions about vaccine acceptance.
We surveyed providers of high-risk patients about HPV vaccine.
Providers caring for high-risk patients are not routinely offering HPV vaccine.
Knowledge of factors that affect HPV vaccine utilization can guide interventions.
Time limitations and cost are reported as common barriers to offering HPV vaccine.
Acknowledgments
Funding Source: All phases of this study were supported by an NIH/NCI grant, 1R03CA144734. The study sponsor was not involved in study design, the collection, analysis, and interpretation of data, the writing of the report or the decision to submit the manuscript for publication.
Dr. Denise Bruno wrote the first draft of the manuscript. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tracey E. Wilson, Email: tracey.wilson@downstate.edu.
Francesca Gany, Email: ganyf@mskcc.org.
Abraham Aragones, Email: aragonea@mskcc.org.
References
- 1.CDC. Human Papillomavirus-Associated Cancers - United States, 2004-2008. Morbidity and Mortality Weekly Report. 2012;61:258–261. [PubMed] [Google Scholar]
- 2.CDC. FDA Licensure of Bivalent Human Papillomavirus Vaccine (HPV2, Cervarix) for Use in Females and Updated HPV Vaccination Recommendations from the Advisory Committee on Immunization Practices (ACIP) Morbidity and Mortality Weekly Report. 2010;59(20):626–629. [PubMed] [Google Scholar]
- 3.CDC. Human Papillomavirus Vaccination Coverage Among Adolescent Girls, 2007- 2012, and Postlicensure Vaccine Safety Monitoring 2006-2013 ---United States. Morbidity and Mortality Weekly Report. 2013;62(29):591–595. [PMC free article] [PubMed] [Google Scholar]
- 4.CDC. National and State Vaccination Coverage Among Adolescents Aged 13-17 Years ---United States, 2011. Morbidity and Mortality Weekly Report. 2012;61(34):671–677. [PubMed] [Google Scholar]
- 5.Dorell CG, Yankey D, Santibanez TA, Markowitz LE. Human papillomavirus vaccination series initiation and completion, 2008-2009. Pediatrics. 2011 Nov;128(5):830–839. doi: 10.1542/peds.2011-0950. [DOI] [PubMed] [Google Scholar]
- 6.Bednarczyk RA, Curran EA, Orenstein WA, Omer SB. Health disparities in human papillomavirus vaccine coverage: trends analysis from the National Immunization Survey-Teen, 2008-2011. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2014 Jan;58(2):238–241. doi: 10.1093/cid/cit707. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services. Healthy People 2020. [Accessed May 22, 2012];2012 http://www.healthypeople.gov/2020/topicsobjectives2020.
- 8.http://www.cdc.gov/vaccines/who/teens/vaccination-coverage.html a. October 2, 2012.
- 9.Centers for Disease Control and Prevention. Vaccines for Children Program (VFC) 2013 http://www.cdc.gov/vaccines/programs/vfc/index.html.
- 10.Watson M, Saraiya M, Benard V, et al. Burden of cervical cancer in the United States, 1998-2003. Cancer. 2008 Nov 15;113(10 Suppl):2855–2864. doi: 10.1002/cncr.23756. [DOI] [PubMed] [Google Scholar]
- 11.Vadaparampil ST, Staras SA, Malo TL, et al. Provider factors associated with disparities in human papillomavirus vaccination among low-income 9- to 17-year- old girls. Cancer. 2013 Feb 1;119(3):621–628. doi: 10.1002/cncr.27735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh GK, Miller BA, Hankey BF, Edwards BK. Persistent area socioeconomic disparities in U.S. incidence of cervical cancer, mortality, stage, and survival, 1975- 2000. Cancer. 2004 Sep 1;101(5):1051–1057. doi: 10.1002/cncr.20467. [DOI] [PubMed] [Google Scholar]
- 13.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010 Apr;125(4):654–659. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- 14.Dorell C, Yankey D, Strasser S. Parent-reported reasons for nonreceipt of recommended adolescent vaccinations, national immunization survey: teen, 2009. Clinical pediatrics. 2011 Dec;50(12):1116–1124. doi: 10.1177/0009922811415104. [DOI] [PubMed] [Google Scholar]
- 15.Chi RC, Neuzil KM. The association of sociodemographic factors and patient attitudes on influenza vaccination rates in older persons. The American journal of the medical sciences. 2004 Mar;327(3):113–117. doi: 10.1097/00000441-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19-26: importance of a physician's recommendation. Vaccine. 2011 Jan 29;29(5):890–895. doi: 10.1016/j.vaccine.2009.12.063. [DOI] [PubMed] [Google Scholar]
- 17.Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey. Am J Public Health. 2013 Jan;103(1):164–169. doi: 10.2105/AJPH.2011.300600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gerend MA, Weibley E, Bland H. Parental response to human papillomavirus vaccine availability: uptake and intentions. J Adolesc Health. 2009 Nov;45(5):528–531. doi: 10.1016/j.jadohealth.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Bednarczyk RA, Birkhead GS, Morse DL, Doleyres H, McNutt LA. Human papillomavirus vaccine uptake and barriers: association with perceived risk, actual risk and race/ethnicity among female students at a New York State university, 2010. Vaccine. 2011 Apr 12;29(17):3138–3143. doi: 10.1016/j.vaccine.2011.02.045. [DOI] [PubMed] [Google Scholar]
- 20.Guerry SL, De Rosa CJ, Markowitz LE, et al. Human papillomavirus vaccine initiation among adolescent girls in high-risk communities. Vaccine. 2011 Mar 9;29(12):2235–2241. doi: 10.1016/j.vaccine.2011.01.052. [DOI] [PubMed] [Google Scholar]
- 21.Hariri S, Unger ER, Sternberg M, et al. Prevalence of genital human papillomavirus among females in the United States, the National Health And Nutrition Examination Survey, 2003-2006. The Journal of infectious diseases. 2011 Aug 15;204(4):566–573. doi: 10.1093/infdis/jir341. [DOI] [PubMed] [Google Scholar]
- 22.Bureau USC. American Community Survey. http://www.census.gov/acs/www/
- 23.Delnevo CD, Abatemarco DJ, Steinberg MB. Physician response rates to a mail survey by specialty and timing of incentive. Am J Prev Med. 2004 Apr;26(3):234–236. doi: 10.1016/j.amepre.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 24.Atkinson W, Wolfe S, Hamborsky J, McIntyre L, editors. Centers for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases. Washington, DC: Public Health Foundation; 2009. 2009. [Google Scholar]
- 25.Daley MF, Crane LA, Markowitz LE, et al. Human papillomavirus vaccination practices: a survey of US physicians 18 months after licensure. Pediatrics. 2010 Sep;126(3):425–433. doi: 10.1542/peds.2009-3500. [DOI] [PubMed] [Google Scholar]
- 26.Joseph NP, Clark JA, Bauchner H, et al. Knowledge, attitudes, and beliefs regarding HPV vaccination: ethnic and cultural differences between African-American and Haitian immigrant women. Womens Health Issues. 2012 Nov-Dec;22(6):e571–579. doi: 10.1016/j.whi.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Hamlish T, Clarke L, Alexander KA. Barriers to HPV immunization for African American adolescent females. Vaccine. 2012 Oct 5;30(45):6472–6476. doi: 10.1016/j.vaccine.2012.07.085. [DOI] [PubMed] [Google Scholar]
- 28.Keating KM, Brewer NT, Gottlieb SL, Liddon N, Ludema C, Smith JS. Potential barriers to HPV vaccine provision among medical practices in an area with high rates of cervical cancer. J Adolesc Health. 2008 Oct;43(4 Suppl):S61–67. doi: 10.1016/j.jadohealth.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 29.Kahn JA, Zimet GD, Bernstein DI, et al. Pediatricians' intention to administer human papillomavirus vaccine: the role of practice characteristics, knowledge, and attitudes. J Adolesc Health. 2005 Dec;37(6):502–510. doi: 10.1016/j.jadohealth.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 30.Bynum SA, Staras SA, Malo TL, Giuliano AR, Shenkman E, Vadaparampil ST. Factors associated With Medicaid providers' recommendation of the HPV vaccine to low- income adolescent girls. J Adolesc Health. 2014 Feb;54(2):190–196. doi: 10.1016/j.jadohealth.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O'Leary ST, Allison MA, Lindley MC, et al. Vaccine financing from the perspective of primary care physicians. Pediatrics. 2014 Mar;133(3):367–374. doi: 10.1542/peds.2013-2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vadaparampil ST, Malo TL, Kahn JA, et al. Physicians' human papillomavirus vaccine recommendations, 2009 and 2011. Am J Prev Med. 2014 Jan;46(1):80–84. doi: 10.1016/j.amepre.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]