Abstract
Background
Reducing readmissions is a clinical and policy priority, but little is known about variations in readmission rates after major surgery and whether a hospital's surgical readmission rates are related to other markers of high-quality surgical care.
Methods
Using national Medicare data, we calculated 30-day readmission rates after hospitalization for coronary artery bypass graft (CABG), pulmonary lobectomy, endovascular abdominal aortic aneurysm repair (EVAR), open abdominal aortic aneurysm repair (AAA), colectomy, and hip replacement. We used bivariate and multivariable techniques to assess the relationship between readmission rates and other measures of surgical quality, including performance on surgical process measures, procedure volume, and mortality.
Results
There were 479,471 discharges following one of the six index procedures from 3,004 hospitals. The median risk-adjusted six-procedure composite 30-day readmission rate was 13.1% [interquartile range, IQR 9.9%-17.1%}. Adjusting for hospital characteristics, we found that hospitals in the highest quartile of surgical volume had lower readmission rates than the lowest-volume hospitals (12.7% vs. 16.8%, p<0.001), and hospitals with the lowest mortality rates had significantly lower readmission rates than hospitals with high mortality rates (13.3% vs. 14.2%, p<0.001). High performance on surgical process of care performance measures was only marginally associated with readmission rates (13.1% versus 13.6%, p=0.021). Patterns were similar when each of the six major surgeries was examined individually.
Conclusion
Nearly one in seven patients is readmitted within 30 days of discharge following a major surgical procedure. High volume and low mortality hospitals have lower surgical readmissions than other hospitals.
Introduction
Reducing readmissions is a priority for both policy makers and clinical leaders. The focus on readmissions has been driven by a belief that reducing the frequency with which patients return to the hospital can both improve care and lower costs. To date, much of the focus has been on readmissions after hospitalizations for medical conditions, where discharge planning and care coordination are often suboptimal.1-4 The Centers for Medicare and Medicaid Services (CMS) plans to include surgical procedures as it expands its readmissions penalty program.5
Using medical readmissions as a measure of hospital quality is controversial. While hospitals vary substantially in their medical readmission rates, these rates are generally uncorrelated (or even inversely correlated) with metrics often used to identify high quality hospitals, including volume, mortality, and performance on process measures.6 When coupled with evidence that hospitals with the sickest and poorest patients have the highest readmission rates,7,8 some have questioned whether readmission rates for medical conditions actually measure hospital quality, or if they instead capture social and clinical factors unrelated to hospital care.1,7
The relationship between readmission rates and surgical care may be different. Given that most patients have non-urgent major surgeries when they are clinically stable, surgical readmissions may more likely result from complications of the care the patient received during the index hospitalization. As such, one would expect hospitals that excel in surgical care to generally have fewer readmissions. However, we have relatively little information on the types of hospitals that perform well or poorly on this metric; one prior study found inconsistent relationships between volume and readmissions after surgery during the 1990s.9 The patterns of surgical care have changed substantially since then. Whether high-quality hospitals, as defined by commonly-used metrics of hospital surgical performance, have lower surgical readmission rates based on current patterns of care is largely unknown. Given that the extension of the Hospital Readmission Reduction Program to surgical patients is predicated on the notion that inadequate inpatient care and poor transition from inpatient to post-acute care are responsible for surgical readmissions, understanding the degree to readmissions are related to quality would be immensely helpful.
In this study we sought to answer three key questions: first, what are the patterns of surgical readmissions among Medicare patients across a set of major procedures in a national sample of hospitals? Second, are key structural characteristics of hospitals, such as size or teaching status, associated with higher surgical readmission rates? And finally, to what extent is a hospital's performance on well-established measures of surgical quality, such as adherence to surgical process measures, procedure volume or mortality, correlated with its surgical readmission rate? We hypothesized that hospitals with greater adherence to the surgical quality measures and higher volume would each lead to fewer readmissions. Finally, we predicted that hospitals with lower 30-day perioperative mortality would have lower readmission rates.
Methods
Data
We linked three data sources: 1) the 2009 Medicare Inpatient 100% file and the 2010 Medicare Provider Analysis and Review (MedPAR) file; 2) the American Hospital Association (AHA) annual survey on hospital characteristics; and 3) Hospital Compare data containing Hospital Quality Alliance (HQA) Surgical Care Composite Scores.
We focused on patients undergoing any one of six major surgical procedures: coronary artery bypass grafting (CABG), pulmonary lobectomy, endovascular aortic aneurysm repair (EVAR), open abdominal aortic aneurysm repair (AAA), colectomy, and hip replacement (Appendix Table1). These procedures were selected because they are common and costly operative procedures for Medicare beneficiaries and reflect a distribution of surgical subspecialties—cardiac, thoracic, vascular, colorectal, and orthopedic—that aids the generalizability of results across the spectrum of surgical care and hospitals. Additionally, cardiovascular procedures such as CABG and AAA repairs may be included in the CMS readmissions reduction penalties by 2015, and understanding patterns of readmissions in these procedures will provide specific insight on the implications of federal policy efforts.
Patients undergoing concurrent valve repairs were excluded from the CABG sample. Lobectomy, EVAR, AAA, and colectomy procedures were restricted by ICD-9 diagnosis codes for lung cancer, non-ruptured aneurysms, and colorectal cancer, respectively, to preserve homogeneity of the samples (see Appendix Table S1 for a complete list of International Classification of Diseases, Ninth Revision (ICD-9) codes used to identify each procedure Patients undergoing procedures performed during December of each year were also excluded because we lacked the data to capture readmissions occurring in the following calendar year.
Of the 4,650 hospitals providing acute-care services to Medicare patients, 3,004 performed at least one of our six selected procedures, and thus were included in our analyses. Our final patient-level cohort was composed of 479,471unique discharges undergoing one of the six procedures of interest.
Variables
Our primary predictors were hospital structural characteristics and measured surgical quality. Structural characteristics included hospital size, teaching status, region, and ownership (non-profit, for-profit, and public) from the AHA dataset. We followed the AHA convention of categorizing hospitals with fewer than 100 beds as small, between 100 and 400 beds as medium, and greater than 400 beds as large. The percentage of the population living below poverty based on beneficiary zip-code was linked from US census data and an average was calculated for each individual hospital based on its patient census.
We used three well-established measures of surgical quality: the HQA surgical process score, procedure volume, and 30-day operative mortality. The HQA surgical process score includes the evidence-based Surgical Care Improvement Project (SCIP) measures, which are designed to reduce perioperative surgical complications (Appendix, Table S2). These measures are included in the CMS hospital value-based purchasing program.10
We calculated each hospital's 30-day procedure-specific mortality rates using the Elixhauser risk-adjustment scheme, a well-validated tool developed by the Agency for Healthcare Research and Quality (AHRQ).11,12 We then applied indirect standardization to create a composite mortality rate across these six conditions.13 For each of these three established indicators of surgical quality, we divided hospitals into quartiles of performance for ease of presentation.
Our primary outcome measure was a hospital-level composite of the six procedure-specific risk-adjusted 30-day readmission rates as well as procedure-specific readmission rates. We used the Elixhauser risk-adjustment approach to calculate expected procedure-specific odds of 30-day readmission for each hospital. To calculate the final risk-adjusted procedure-specific readmission rate for each hospital, we multiplied that hospital's observed-to-expected ratio by the overall readmission rate for that operation from our national sample. We used indirect standardization to calculate each hospital's six-procedure composite readmission rate by averaging each hospital's observed-to-expected readmission ratio for each procedure, weighting each ratio based on the number of cases for that procedure.
Analyses
We compared patient characteristics of those patients who were readmitted within 30 days of discharge from an index procedure with those patients who were not readmitted. We next compared the characteristics of the hospitals above the median six-procedure composite readmission rate, including hospital size, region, teaching status, and ownership status, to the characteristics of hospitals that were below the median.
The distribution of risk-adjusted six-procedure composite readmission rates was plotted to illustrate variations in readmission rates across hospitals, and we superimposed a plot of hospital volume. Next, we examined bivariate associations between hospital structural characteristics, including hospital size, teaching status, region, location, poverty, and ownership status and the six-procedure composite 30-day readmission rates. We subsequently built a multivariate model that adjusted for all of the hospital characteristics.
Next, we built three separate multivariable models (one for each of the three quality metrics), each adjusting for all the hospital characteristics described above. Finally, we built a “fully-adjusted” model that adjusted for all three quality metrics (HQA scores, volume, and mortality) simultaneously to identify the independent relationship between each of these quality measures and readmissions. All regression models were weighted by hospital-level procedure volume.
While we have carried out many analyses which could lead to false positive results through multiple testing, our primary purpose was to investigate the relationship between our composite readmission rate outcome variable and our three quality-related predictors (process quality, volume, and mortality). These three relationships are most accurately captured in our final, fully-adjusted model. In that model, relationships with a Bonferroni-adjusted p-value of 0.0167 were considered significant.
Sensitivity Analyses
In sensitivity analyses, modeling covariates of interest (surgical process quality, volume, and mortality) as continuous variables or with alternate cutoffs did not have a significant effect on the overall findings; therefore, we only present results showing our quality metrics in quartiles. We additionally examined the relationship between quality metrics and readmissions for each of the surgical procedures individually.
For multi-level categorical predictors and covariates, p-values for trend are presented. All analyses were performed using Stata 12. This study was approved by the Office of Human Research Administration at the Harvard School of Public Health.
Results
Patient and Hospital Characteristics
Between 2009 and 2010, there were 3,004 U.S. hospitals that performed at least one of the six surgical procedures in our study (Appendix Table S3). These hospitals accounted for 90.7% of all acute-care Medicare fee-for-service discharges in the U.S. during the study period.
There were 479,471 discharges following our index procedures, and readmission rates ranged from 10.5% to 17.4% across the six procedures (Appendix Table S4). As expected, readmitted patients were older (78.0 years vs. 77.0 years, p<0.001) and had more medical comorbidities (Table 1) than those not readmitted.
Table 1.
Characteristics of patients readmitted within 30 days compared to those that are not
| Patient Characteristics | Patients readmitted within 30 days (n= 61,785) | Patients not readmitted within 30 days (n=417,686) | P-value |
|---|---|---|---|
| AGE | |||
| Age (mean ±SD) | 78.0 ±7.6 | 77 ± 7.6 | <0.001 |
| SEX | |||
| Male | 51.5% | 49.2% | |
| Female | 48.5% | 50.8% | <0.001 |
| RACE | |||
| White | 90.3% | 92.0% | |
| Black | 5.9% | 5.0% | <0.001 |
| Other | 3.8% | 3.0% | |
| COMORBIDITIES | |||
| CHF | 8.2% | 5.5% | <0.001 |
| COPD | 19.7% | 17.1% | <0.001 |
| Hypertension | 55.9% | 61.6% | <0.001 |
| DM | 18.6% | 18.1% | <0.001 |
| Renal Failure | 11.6% | 7.6% | <0.001 |
| Obesity | 5.6% | 5.8% | <0.001 |
| Depression | 4.0% | 4.8% | <0.001 |
| LENGTH OF STAY (DAYS) | |||
| Length of stay | 10.09 | 7.58 | <0.001 |
| DISCHARGE STATUS | |||
| Home | 20.75% | 29.34% | |
| Home with Services | 22.80% | 24.29% | |
| Skilled Nursing Facility | 37.66% | 28.26% | <0.001 |
| Rehab | 13.38% | 11.34% | |
| In-hospital mortality | - | 2.79% | |
| Other | 5.41% | 3.98% | |
| POVERTY | |||
| % below poverty line by patient zip code | 11.2% | 10.9% | <0.001 |
| PROCEDURE | |||
| CABG | 41.60% | 30.60% | |
| Lobectomy | 4.56% | 5.15% | |
| EVAR | 5.26% | 6.36% | <0.001 |
| AAA | 1.37% | 1.35% | |
| Colectomy | 12.77% | 12.26% | |
| Hip Replacement | 34.45% | 44.27% | |
Hospitals with readmission rates below the median were more likely to be non-profit (66.3% vs. 63.6%, p=0.042), non-teaching hospitals (6.8% vs. 10.9%, p<.001) and located in the West (24.1% vs. 14.8%). These hospitals had a higher nurse-to-census ratio (7.2 vs. 6.9, p<0.001) and lower proportion of Medicaid patients (16.2% vs. 17.0%, p=0.005, Table 2) than high readmission rate hospitals.
Table 2.
Characteristics of hospitals by performance on readmission rates
| Hospital Characteristics | Hospitals Below Median Readmission Rate | Hospitals Above Median Readmission Rate | P-value |
|---|---|---|---|
| OWNERSHIP | |||
| For Profit | 18.0% | 21.7% | |
| Private Non-profit | 66.3% | 63.6% | 0.042 |
| Public | 15.6% | 14.8% | |
| HOSPITAL SIZE | |||
| Small | 28.0% | 25.7% | |
| Medium | 57.8% | 58.9% | 0.017 |
| Large | 14.3% | 15.5% | |
| TEACHING STATUS | |||
| Major Teaching Hospital | 6.8% | 10.9% | <0.001 |
| RURAL | |||
| % rural | 8.7% | 6.5% | 0.024 |
| REGION | |||
| Northeast | 12.5% | 19.7% | |
| Midwest | 25.9% | 22.2% | <0.001 |
| South | 37.5% | 43.4% | |
| West | 24.1% | 14.8% | |
| INTENSIVE CARE UNIT | |||
| ICU present | 81.3% | 79.1% | 0.129 |
| NURSE-TO-CENSUS RATIO | |||
| Ratio, median (IQR) | 7.2 (6.0, 8.7) | 6.9 (5.8, 8.1) | <0.001 |
| PROPORTION MEDICAID | |||
| Proportion Medicaid (Median, IQR) | 16.2% (11.1%, 20.5%) | 17.0% (11.4%, 21.9%) | 0.005 |
| MEASURES OF QUALITY | |||
| HQA Surgery Score, median (IQR) | 96.6 (95.3, 97.7) | 96.5 (95.0, 97.6) | 0.408 |
| Composite Surgical Volume, median (IQR) | 84.5 (26, 239) | 72 (26, 186) | 0.0205 |
| Composite Surgical Mortality, median (IQR) | 3.3% (1.4%, 5.3%) | 3.7% (1.7%, 5.7%) | <0.001 |
Hospital Structural Characteristics and Readmission Rate
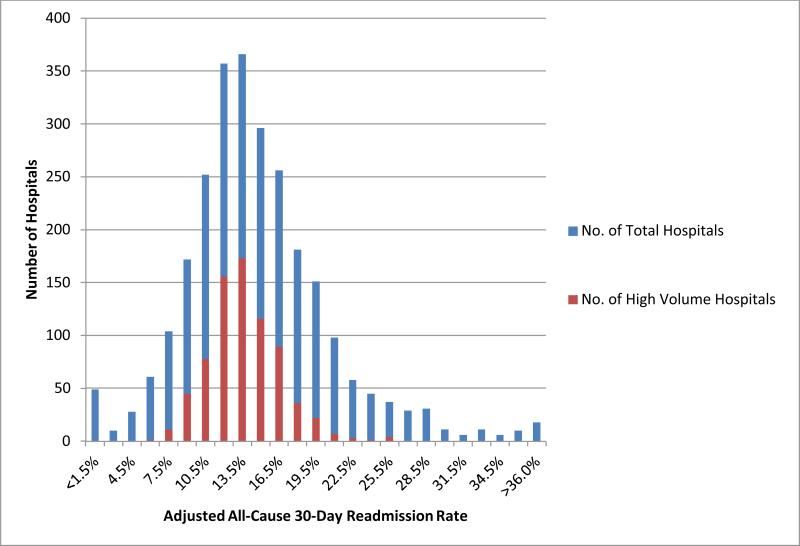
There was marked variability in risk-adjusted six-procedure composite 30-day readmission rates across hospitals (Figure 1). In each of our six procedure-specific analyses, we also found substantial variations in readmissions across hospitals. In multivariable models that accounted for each of the structural characteristics, we found that non-profit hospitals had lower readmission rates than for-profit hospitals (13.1% vs. 13.7%, Table 3). Similarly, major teaching hospitals had lower readmission rates than non-teaching hospitals (12.9% vs. 13.9%, p<0.001). There was no difference in readmission rates between urban and rural hospitals (13.2% versus 13.4%, p=0.987). Hospitals with the highest proportion of patients residing in high-poverty zip-codes had higher readmission rates (14.0% vs. 13.1%, p<0.001). Trends were similar in each of the six procedure-specific analyses.
Figure 1.
Distribution of Risk-Adjusted 30-Day Readmission Rates for Six Surgical Procedures across US Hospitals
Table 3.
Readmission rates by select hospital characteristics
| Characteristic | Multivariate Adjusted Composite 30-Day Readmission Rate* | P-value |
|---|---|---|
| HOSPITAL SIZE | ||
| Small (<100 beds) | 13.1% | |
| Medium (100-399 beds) | 13.3% | 0.041 |
| Large (>400 beds) | 13.0% | |
| SETTING | ||
| Rural | 13.4% | 0.987 |
| Urban | 13.2% | |
| MAJOR TEACHING STATUS | ||
| Yes | 13.9% | <0.001 |
| No | 12.9% | |
| OWNERSHIP | ||
| For profit | 13.7% | |
| Private Non-profit | 13.1% | <0.001 |
| Public | 13.5% | |
| ICU | ||
| Yes | 13.1% | 0.118 |
| No | 13.5% | |
| REGION | ||
| Northeast | 14.4% | |
| Midwest | 12.7% | <0.001 |
| South | 13.5% | |
| West | 11.9% | |
| AVERAGE % POVERTY IN PATIENT ZIP CODE | ||
| Lowest | 13.1% | <0.001 |
| Highest | 14.0% | |
Rates are for the 6-procedure composite and are calculated from multivariate analysis that adjust for patient demographics, comorbidities, and each of the hospital characteristics listed above. Model r-squared 0.0570.
Relationship between quality measures and readmission rates
When we examined the relationship between performance on surgical quality measures and readmission rates, after accounting for hospital characteristics, we found that hospitals in the highest quartile of the HQA surgical score had somewhat lower risk-adjusted readmission rates than those in the worst quartile (13.1% vs. 13.6%, p=0.021). Similarly, hospitals with the highest procedure volumes had lower six-procedure composite readmission rates compared to hospitals with the lowest procedure volumes (12.7% in highest volume quartile vs. 16.8% in the lowest volume quartile, p<0.001, Table 4) as did hospitals with the lowest mortality rate (13.3%) compared to hospitals with the highest mortality rate (14.2%, p-value for difference <0.001, Table 4).
Table 4.
Multivariate analysis of predictors for 30-day readmission rates
| Quality And Outcome Predictor | Model I Adjusted Composite 30-Day Readmission Rate* | P-value | Model II Adjusted Composite 30-Day Readmission Rate‡ | P-value |
|---|---|---|---|---|
| HQA SURGICAL PROCESS SCORE | ||||
| Lowest Quartile | 13.6% | 13.5% | ||
| 2nd Quartile | 13.3% | 0.021 | 13.3% | 0.075 |
| 3rd Quartile | 13.0% | 13.0% | ||
| Highest Quartile | 13.1% | 13.1% | ||
| SURGICAL VOLUME | ||||
| Lowest Quartile | 16.8% | 16.5% | ||
| 2nd Quartile | 15.0% | <0.001 | 14.8% | <0.001 |
| 3rd Quartile | 13.7% | 13.6% | ||
| Highest Quartile | 12.7% | 12.8% | ||
| SURGICAL MORTALITY | ||||
| Lowest Quartile | 13.3% | 13.0% | ||
| 2nd Quartile | 12.9% | <0.001 | 13.0% | 0.001 |
| 3rd Quartile | 13.1% | 13.2% | ||
| Highest Quartile | 14.2% | 13.8% |
HQA = Hospital Quality Alliance.
†: Model I rates are for the six-procedure risk-adjusted composite readmission rate. Models are further adjusted for hospital size, teaching status, ownership, region, and location. Model r-squared values are 0.059, 0.085, and 0.0620 for HQA surgical score, volume, and mortality, respectively.
Model II rates are for the six-procedure risk-adjusted composite readmission rate. Models are further adjusted for hospital size, teaching status, ownership, region, and location, as well as the other quality metrics. Model r-squared 0.091.
When we examined our final model that simultaneously accounted for all three quality measures in addition to hospital structural characteristics, we found that volume and mortality remained independently associated with lower readmission rates. Highest-volume hospitals had lower readmission rates than low-volume hospitals (12.8% vs. 16.5%, p<0.001). Lowest-mortality hospitals had lower readmission rates than highest-mortality hospitals (13.0% vs. 13.8%, p<0.001, Table 4). However, the best-performing hospitals on the HQA surgical score had only marginally lower readmission rates compared to poor-performing hospitals (13.1% vs. 13.5%, p=0.075), a difference that was not statistically significant.
When we examined the six individual surgical procedure-specific readmission rates, the overall relationships with hospital quality were consistent. For all three quality measures — compliance with best-practice guidelines, procedure-specific volume, and procedure-specific mortality were generally associated with lower readmission rates, although the differences were not always statistically significant. For open AAA repair, we found no relationship between mortality and readmission rates (Appendix Table S5).
Discussion
We found that approximately one in seven patients discharged after undergoing a major surgical procedure is readmitted within 30 days with substantial variations across U.S hospitals. High-performing hospitals, as measured by high procedure volume and low 30-day mortality, had lower surgical readmission rates, and the patterns were consistent across each of the six procedures examined. Adherence to process quality was weakly associated with lower readmission rates, a relationship that markedly diminished when accounting for other quality measures. Taken together, these findings offer evidence that surgical readmission rates are indeed associated with measures of surgical quality.
These findings, although quite different from what has been found for medical readmissions, may not be a surprise. The reasons that bring surgical patients back to the hospital soon after discharge are likely very different than those that drive medical patients to return. While medical patients may come back due to poor social support at home, inability to access primary care, or general poor health, surgical patients more likely to return as a consequence of complications arising from the surgery.14 Hospitals that perform higher volumes of procedures or those with lower mortality are better versed at rescuing patients from postoperative complications.15,16 These “high quality” hospitals may also have systematic approaches to identify when patients are ready for discharge, and to engage in readmission-prevention strategies that may have greater impact for surgical patients than it does for medical ones. Although we could not specifically determine why higher volume or lower mortality hospitals have lower readmission rates, we suspect that these factors may be at play.
We found that adherence to best-practice guidelines was weakly associated with marginally lower readmission rates. The lack of an independent relationship between the HQA score and readmission rates may be because of the small variation in performance on these measures (98.4% among the highest quartile versus 92.0% among the lowest quartile). Further, prior studies have similarly found an inconsistent relationship between process measures and important outcomes such as mortality17,18
Our finding that surgical readmissions have a modest but consistent relationship with measures of surgical quality, especially volume and mortality, should offer some confidence to policymakers who wish to use surgical readmission rates to grade and pay hospitals, especially given that our findings were generally consistent across each of the surgical procedures. However, whether improving surgical outcomes (e.g. mortality) or a greater concentration of surgeries in a few institutions (leading to higher volume) would translate into fewer readmissions is unclear. Although we found statistically significant associations between readmissions and hospital characteristics (such as by ownership), their clinical significance is unclear.
Several prior studies have identified patient-level factors, such as age and severity of underlying illness14,19,20 or length of stay,21-23 that are predictive of readmission. However, the data on the relationship between hospital factors or surgical quality metrics and readmissions are less robust. Prior studies have shown readmission rates following certain high-risk procedures are either inversely related 24 or unrelated to procedure volume.9 Both of these studies focused on patterns of care in the 1990s before widespread use of minimally-invasive approaches and post-surgical algorithms and pathways. We suspect that as surgical care has changed, factors such as volume have become more important for recognizing complications, which may underlie our observed volume-readmissions relationship.
There are limitations to our study beyond those mentioned above. Because we used administrative data, we were unable to adequately account for factors not captured by billing codes. However, we would expect that inadequate risk adjustment would likely either diminish our ability to find an association. Another concern is that some have questioned the value of treating volume as a categorical variable.25-28 Our results did not qualitatively change with various sensitivity analyses, including treating volume as a continuous predictor. Finally, we focused on the Medicare population, and therefore cannot say whether our findings would extend to non-elderly Americans.
Conclusion
We found marked variation in surgical readmission rates across U.S. hospitals. Readmission rates were associated with procedural volume and mortality rates, two well-established metrics of hospital surgical quality. Surgical readmission rates could be a relevant and valid way for policymakers, clinical leaders, and patients to measure the surgical performance of U.S. hospitals.
References
- 1.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. Jama. 2011;305:675–81. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361:2637–45. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]
- 4.Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med. 2011;171:1232–7. doi: 10.1001/archinternmed.2011.278. [DOI] [PubMed] [Google Scholar]
- 5.Readmissions Reduction Program 2012 at http://www.cms.gov/Medicare/Medicare-Feefor-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.)
- 6.Chen LM, Jha AK, Guterman S, Ridgway AB, Orav EJ, Epstein AM. Hospital cost of care, quality of care, and readmission rates: penny wise and pound foolish? Arch Intern Med. 2010;170:340–6. doi: 10.1001/archinternmed.2009.511. [DOI] [PubMed] [Google Scholar]
- 7.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011;4:53–9. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. Jama. 2013;309:342–3. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 9.Goodney PP, Stukel TA, Lucas FL, Finlayson EV, Birkmeyer JD. Hospital volume, length of stay, and readmission rates in high-risk surgery. Ann Surg. 2003;238:161–7. doi: 10.1097/01.SLA.0000081094.66659.c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CMS Issues Final Rule for First Year of Hospital Value-Based Purchasing Program. 2011 (Accessed 4/24/2013, 2013, at http://www.cms.gov/apps/media/press/factsheet.asp?Counter=3947.
- 11.Fry DE, Pine M, Jordan HS, et al. Combining administrative and clinical data to stratify surgical risk. Ann Surg. 2007;246:875–85. doi: 10.1097/SLA.0b013e3180cc2e7a. [DOI] [PubMed] [Google Scholar]
- 12.Pine M, Jordan HS, Elixhauser A, et al. Enhancement of claims data to improve risk adjustment of hospital mortality. Jama. 2007;297:71–6. doi: 10.1001/jama.297.1.71. [DOI] [PubMed] [Google Scholar]
- 13.Pouw ME, Peelen LM, Lingsma HF, et al. Hospital standardized mortality ratio: consequences of adjusting hospital mortality with indirect standardization. PloS one. 2013;8:e59160. doi: 10.1371/journal.pone.0059160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kassin MT, Owen RM, Perez S, et al. Risk Factors for 30-Day Hospital Readmission among General Surgery Patients. J Am Coll Surg. 2012 doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Birkmeyer JD, Skinner JS, Wennberg DE. Will volume-based referral strategies reduce costs or just save lives? Health Aff (Millwood) 2002;21:234–41. doi: 10.1377/hlthaff.21.5.234. [DOI] [PubMed] [Google Scholar]
- 16.Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81. doi: 10.1097/MLR.0b013e3182329b97. [DOI] [PubMed] [Google Scholar]
- 17.Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals--the Hospital Quality Alliance program. N Engl J Med. 2005;353:265–74. doi: 10.1056/NEJMsa051249. [DOI] [PubMed] [Google Scholar]
- 18.Garcia N, Fogel S, Baker C, Remine S, Jones J. Should compliance with the Surgical Care Improvement Project (SCIP) process measures determine Medicare and Medicaid reimbursement rates? Am Surg. 2012;78:653–6. [PubMed] [Google Scholar]
- 19.Schneider EB, Hyder O, Brooke BS, et al. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg. 2012;214:390–8. doi: 10.1016/j.jamcollsurg.2011.12.025. discussion 8-9. [DOI] [PubMed] [Google Scholar]
- 20.Greenblatt DY, Greenberg CC, Kind AJ, et al. Causes and implications of readmission after abdominal aortic aneurysm repair. Ann Surg. 2012;256:595–605. doi: 10.1097/SLA.0b013e31826b4bfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vorhies JS, Wang Y, Herndon J, Maloney WJ, Huddleston JI. Readmission and length of stay after total hip arthroplasty in a national Medicare sample. The Journal of arthroplasty. 2011;26:119–23. doi: 10.1016/j.arth.2011.04.036. [DOI] [PubMed] [Google Scholar]
- 22.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. Jama. 2012;308:1227–36. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hendren S, Morris AM, Zhang W, Dimick J. Early discharge and hospital readmission after colectomy for cancer. Dis Colon Rectum. 2011;54:1362–7. doi: 10.1097/DCR.0b013e31822b72d3. [DOI] [PubMed] [Google Scholar]
- 24.Hannan EL, Racz MJ, Walford G, et al. Predictors of readmission for complications of coronary artery bypass graft surgery. Jama. 2003;290:773–80. doi: 10.1001/jama.290.6.773. [DOI] [PubMed] [Google Scholar]
- 25.LaPar DJ, Kron IL, Jones DR, Stukenborg GJ, Kozower BD. Hospital procedure volume should not be used as a measure of surgical quality. Ann Surg. 2012;256:606–15. doi: 10.1097/SLA.0b013e31826b4be6. [DOI] [PubMed] [Google Scholar]
- 26.Livingston E, Cao J, Dimick JB. Tread carefully with stepwise regression. Arch Surg. 2010;145:1039–40. doi: 10.1001/archsurg.2010.240. [DOI] [PubMed] [Google Scholar]
- 27.Livingston EH, Cao J. Procedure volume as a predictor of surgical outcomes. Jama. 2010;304:95–7. doi: 10.1001/jama.2010.905. [DOI] [PubMed] [Google Scholar]
- 28.Livingston EH, Elliot A, Hynan L, Cao J. Effect size estimation: a necessary component of statistical analysis. Arch Surg. 2009;144:706–12. doi: 10.1001/archsurg.2009.150. [DOI] [PubMed] [Google Scholar]