Abstract
There have been several recent efforts in the UK and the Netherlands to describe the harms of psychoactive substances based on ratings of either experts or drug users. This study aimed to assess the perceived benefits as well as harms of widely used recreational drugs, both licit and illicit, in an international sample of drug users. The survey was hosted at https://www.internationaldrugsurvey.org/ and was available in three languages. Residents reported their experience of 15 commonly used drugs or drug classes; regular users then rated their harms and benefits. In all, 5791 individuals from over 40 countries completed the survey, although the majority were from English speaking countries. Rankings of drugs differed across 10 categories of perceived benefits. Skunk and herbal cannabis were ranked consistently beneficial, whilst alcohol and tobacco fell below many classified drugs. There was no correlation at all between users’ harm ranking of drugs and their classification in schedules of the USA or ABC system in the UK. Prescription analgesics, alcohol and tobacco were ranked within the top 10 most harmful drugs. These findings suggest that neither the UK nor US classification systems act to inform users of the harms of psychoactive substances. It is hoped the results might inform health professionals and educators of what are considered to be both the harms and benefits of psychoactive substances to young people.
Keywords: Alcohol, benefits, cannabis, drug abuse, ecstasy, harms, legal status
Introduction
Worldwide alcohol causes 2.5 million deaths per year (World Health Organisation, 2011) whilst tobacco is implicated in twice this number (Mackay et al., 2006), collectively accounting for 12% of all deaths. The health costs of tobacco smoking total $96 billion per year in the USA and £2.25 billion in the UK (Mackay et al., 2006). The cost of alcohol is an accumulation of health, social and crime-related spending and can total up to £20 billion in the UK and $200 billion in the USA (Global Status Report on Alcohol and Health, 2011). Recently, there has been an increase in non-medical use of prescription analgesics (or painkillers), with a growing trend of ‘pill mills’ and ‘doctor shopping’. In the USA, the non-medical use of these drugs by 12 million people made them the second most common form of illicit drug use after cannabis in 2010 (Substance Abuse and Mental Health Services Administration, 2011). Deaths from prescription analgesics in the USA are greater than those from heroin and cocaine combined, with rates tripling in the last 10 years (Centre for Disease Control and Prevention, 2011), which is perhaps unsurprising given their much larger number of consumers.
Illicit drugs are only used by a minority of the world’s population, with between 3.5% and 5.7% having used an illicit substance at least once (United Nations Office on Drugs and Crime, 2010). Around 10–15% of these are classed as ‘problematic users’. Cannabis has the highest prevalence of use followed by amphetamine, cocaine and heroin. In the UK, problem drug use of Class A substances costs society £15.4 billion a year, of which £13.9 billion is attributable to criminal offences. The US Department of Justice National Drugs Intelligence Centre (2011) reported that the total impact of illicit substances on society amounted to over $193 billion, with crime and incarceration accounting for over $100 billion of these costs.
Current approaches aimed at reducing illicit drug use include prohibition of supply, education and treatment. Most countries and international agencies (such as the United Nations and World Health Organisation), classify drugs according to how dangerous or harmful they are. For example, under the UK Misuse of Drugs Act 1971, drugs are segregated into three classes (A, B and C) which are meant to (i) reflect their relative harms and (ii) determine the penalties for possessing and trafficking each drug. In the USA drugs are classified into five schedules reflecting their ‘potential for abuse’. It has been argued that these systems have evolved in an unsystematic way according to social, political and historical concerns rather than being based on any scientific evidence.
Recently, attempts have been made to develop a ‘rational’ scale to assess and compare the overall harms of psychoactive drugs (Nutt et al., 2007). Their ‘harm matrix’ included three categories of harm: ‘physical’, ‘dependence-related’ and ‘social’, each with three sub-levels, allowing currently used and new psychoactive substances to be more objectively compared on the basis of experts’ ratings. Nutt et al.’s findings showed no relationship with the rank ordering by experts and categorisation of drugs under the UK Misuse of Drugs Act, and caused considerable controversy within the government and media.
Subsequently we used the same harm matrix to survey over 1500 UK drug users and found significant correlations between their harm rankings and those of Nutt et al.’s experts, but none between users’ rankings and the current classification of drugs under the UK Misuse of Drugs Act (Morgan et al., 2010b). These findings were then replicated in the Netherlands, where a two-class classification systems is employed (van Amsterdam et al., 2010), and a recent web-based survey of drug users (predominantly mephedrone users) which provided a very similar profile of rankings to the studies outlined above based on harm ratings of 13 psychoactive substances (Carhart-Harris, 2011). Once again alcohol and tobacco were rated to be highly harmful whilst cannabis, ecstasy and magic mushrooms were rated as relatively safe. In response to doubts raised about the differential weighting and choice of criteria used, Nutt et al. (2010) used ‘multicriteria decision analysis’ to develop a weighted model, based again on ratings by experts. Their results supported their previous findings – again, there was no correlation between rated harms and UK ABC classification.
A debate has ensued, with some disputing whether it is logically possible to rank drugs on any single dimension of harm (Caulkins et al., 2011; Cohen, 2010). It is argued that no model would ever be perfect because ratings of harm to others and harms to self are neither objective nor measureable, as they will always be influenced by expertise and personal biases; indeed, Nutt et al. used a small number of experts with uncertain knowledge of drug-related harms outside of their area of expertise (Coulson and Caulkins, 2012). Furthermore, the principle of combining individual and aggregate harm measures to create a weighted total ‘harm score’ may be flawed, in that the relationship between these two types of harm may not be additive. The latter authors further suggested that even perfect calculation of harm scores cannot determine how a new drug should be scheduled. Scheduling systems are interrelated with some drugs being precursors to others, and thus it is difficult for them to be considered on a drug-by-drug basis. In addition the consequences of scheduling, changes depend on context of use of the drug; for example, alcohol is highly harmful to use whilst driving. Nutt et al. (2010) also did not take into account either differential availability of illegal substances or poly drug use. Caulkins et al. (2011) proposed alternative ‘harm matrices’ which would take into account the context of drug use, so each substance in each context would be associated with harm-type ratings. However, although this process would be an interesting one to explore, it was deemed too lengthy and complex for an internet survey, and thus we adopted the Nutt et al. framework, for parsimony and ease of use.
Whilst drug harms may not be sufficient to determine policy (Kalant, 2010) the belief that policies informed by science are better than those with no scientific basis at all has been expressed by several researchers (e.g. Fischer and Kendall, 2011; Obot, 2011; Room and Lubman, 2010). The value of informing policy makers of the relative harm of drugs is not opposed even by critics (Caulkins et al., 2011). As well as harms, however, recreational drugs have perceived benefits, otherwise they would not be used. There are a variety of historical and emerging beneficial uses of various compounds that are illicit substances; for example cannabis, once used as a sedative and anti-convulsant in the UK and US (Walton, 1938), has recently been explored in its organic form and components as an analgesic, anti-emetic and appetite stimulant. Renewed efforts have also been made to demonstrate the efficacy of illicit drugs as adjuncts to psychotherapy, either as psycholytics or psychedelics, with promising results (see Sessa, 2005 for a review). For example, in two small studies, MDMA has been found to be effective as an adjunct to exposure therapy for post-traumatic stress disorder (PTSD) and therapy-resistant anxiety disorders (Johansen and Krebs, 2009; Mithoefer, 2006; Sessa, 2007). In addiction treatment with single dose of LSD, in the context of alcohol treatment programmes in the 1960s and 1970s, is associated with a decrease in alcohol misuse (Krebs and Johansen, 2012), whilst ketamine has improved rates of abstinence in the treatment of heroin addicts (Krupitsky et al., 2002).
A wide literature has detailed the benefits of recreational drugs to users (e.g. Griffiths et al., 2006, 2008, 2011; Móró and Noreika, 2011; Müller and Schumann, 2011; Tart 1971). However, only two studies to date have compared the potential benefits of illicit drugs to the harms (Carhart-Harris and Nutt, 2010; Morgan et al., 2010b). The latter assessed the perceived acute and long-term benefits of 21 substances in over 1500 drug users whilst the former compared the benefits of four types of substances in 626 users. Users presumably make a complex cost/benefit judgement when taking recreational drugs. Understanding both the harms and benefits of taking drugs for users is important for the uptake of health education, and therefore it is important to collect accurate and up-to-date data on regular users’ perspectives of the benefits of taking drugs.
The current study aimed to provide a more comprehensive account of the perceived benefits as well as harms of 18 psychoactive substances (11 illicit and seven legal). As previous surveys have been limited to UK or the Netherlands, it also aimed to obtain an international sample of users with diverse cultural and legal approaches to psychoactive substances.
Methods
A website was designed using Web II software and was distributed internationally via a link on Erowid in three optional languages (English, Spanish and French). Participants were required to provide informed consent and confirm they were over 18 before entering the survey. Withdrawal from the survey was permitted at any time using a button at the bottom of the page, and participants were informed that in this instance their data would not be saved.
Psychoactive substance use was recorded first to establish which of the 18 drugs each participant would then be able to rate. The following drugs were grouped into three classes once data on substance use had been entered; Hallucinogens: 2-CB/ 2-CI, ayahuasca, DMT, GHB, LSD, Mescaline/ Peyote, mushrooms, salvia divinorum; Amphetamines: amphetamine/methamphetamine, prescribed stimulants (e.g. Dexedrine, Ritalin); Opiates: heroin, methadone, opium (prescription analgesics were kept in their own separate group).
Only participants who regularly used the drugs went on to rate their benefits and harms, except in the case of hallucinogens where all those reporting any prior use of the drugs were included on the assumption that few people would take hallucinogens ‘regularly’. This was an unfortunate practical consideration to limit the length of the survey for respondents. Because of very low numbers of users (less than 0.7% of the total sample), three drugs (crack, anabolic steroids, solvents: aromatic and aliphatic hydrocarbons, ketones and haloalkanes such as benzene, m-xylene, ethylbenzene, propylbenzene, 1,1,1-trichlorethane (TCE) and nitrites e.g. Poppers) were not included in the analyses.
Measures (for the full survey see supplementary online material)
Harms
Participants were asked to rate the harms associated with each drug on the basis of seven risk factors;
Short-term physical risk: Participants were asked to think about how much short-term physical risk they thought was associated with taking a single dose of a drug. They were instructed that a ‘single dose’ meant one bottle of beer, one ecstasy tablet or one line of coke. They were then asked ‘when someone is under the effects of a drug how likely are they to cause themselves some physical damage. For example, if someone is likely to die from an overdose this would be considered ‘extreme risk’, or if someone is likely to have an accident this would be ‘moderate risk’.’
Long-term physical risk: Participants were asked to rate how much long-term physical risk they thought would be associated with regular use each of the drugs.
Risk of injecting: Participants were asked, ‘how likely do you think people are to inject the following drugs?’ Although injection is not a harm in itself, it is an indicator of a higher likelihood of dependence, due to the rapid onset of effects and is also associated with risk of a range of serious secondary health outcomes, for example hepatitis C and HIV transmission.
Risk of physical dependence: this was assessed by asking the question ‘If someone takes the drugs below on a regular basis, what is the risk that they will become physically reliant on them and experience physical side effects if they stop?’.
Risk of psychological dependence: This was assessed by the question ‘what is the risk if someone takes the drugs below on a regular basis that they will develop cravings?’.
Risk to society: Participants were told that some drugs are seen to have a negative impact on society by damaging family relationships, damage to property, or through the cost of policing. They were then asked to rate the level of risk to society which they thought each drug posed.
Risk of bingeing: Participants were asked to rate the likelihood of bingeing. Bingeing means the tendency to repeatedly dose with a substance, and is an indicator of the dependence-forming properties of a drug, hence it presence as an indicator of harm .When a person takes an excessive amount of a drug, for example more than 10 units of alcohol in a single session, this is considered ‘bingeing’.
Participants were asked to score each substance on a four-point scale, with 0 no risk, 1 some risk; 2 moderate risk and 3 extreme risk. The scores for these seven factors were averaged to give a mean harm score.
Benefits
Participants rated 10 benefits, defined below. Five benefits comprised multiple items. The number of participants who rated a drug as having a particular benefit was calculated as a proportion of the total number of participants who rated that drug.
Sociability (4 items; Lose inhibitions/ be more sociable, Feel more confident, Feel closer to people/ more empathy, Feel part of a social group)
Enjoyment (5 items; Enhance activities, Enhance sense of fun/humour, Help with creativity/ abstract thinking, Increase sexual function/ enjoyment, Feel elated/ euphoric)
State of mind (6 items; Open up to new experiences, Altered senses, Increase existential awareness, Find meaning in the self and the world, Help alter consciousness, To get out of my head/ escapism)
Pain (2 items; Relieve symptoms of disease/ illness, Relieve physical pain)
Relieve anxiety/ depression (1 item)
Feel more relaxed/ relieve stress (1 item)
Change appearance of body (bulk up/ lose weight) (1 item)
Help wake up/ have more energy (1 item)
Help to get to sleep (1 item)
Improve attention, memory and concentration (1 item)
Participants were also asked to report their first and second preference for drugs.
Finally, participants were asked to assess their own dependence using four binomial yes/no questions taken from the CAGE-AID (‘Cut-Down, Annoyed, Guilty, Eye-Opener’ Adapted to Include Drugs) dependence scale (Brown and Rounds, 1995) The CAGE-AID was developed as a time-saving screening tool for clinicians in primary care and whilst it cannot indicate dependence, it can reflect a likelihood of abuse or dependence, warranting further screening.
The survey was launched on Erowid on the 7 March 2011 and all data up until 17.30 on 5 December 2011 were included in this report.
Statistical analyses
Spearman’s rank correlation coefficient was used to analyse the relationship between UK classifications and US scheduling of illicit substances and the perceived harms of psychoactive drug as rated by users in the UK and US.
Results
Demographics
A total of 5691 individuals, worldwide, completed the online survey. Their demographic data are displayed in Table 1.
Table 1.
Demographic data for the sample: percentage in each category
|
Gender
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | No reply | ||||||
| 76.2 | 23.5 | 0.4 | ||||||
|
Age
| ||||||||
| 18–24 | 25–30 | 31–40 | 41–50 | 51–60 | 61–65 | 66–110 | No reply | |
|
| ||||||||
| 61.53 | 14.40 | 10.53 | 6.75 | 4.87 | 1.00 | 0.43 | 0.48 | |
| Education | ||||||||
| Early leaver | Secondary | Undergraduate | Post-graduate | No reply | ||||
|
| ||||||||
| 6.04 | 35.73 | 42.95 | 14.28 | 1.00 | ||||
| Employment | ||||||||
| Retired | Unemployed | Carer/homemaker | studying | Employed | No reply | |||
| 2.19 | 13.33 | 2.38 | 39.39 | 41.94 | 0.76 | |||
| Ethnicity | ||||||||
| White | African | Indian | East Asian | Mixed Race | Other | No Reply | ||
|
| ||||||||
| 88.36 | 0.64 | 1.33 | 0.35 | 5.61 | 3.16 | 0.55 | ||
| Sexual Orientation | ||||||||
| Heterosexual | Homosexual | Bisexual | No Reply | |||||
|
| ||||||||
| 83.60 | 3.70 | 11.74 | 0.97 | |||||
| Religion | ||||||||
| Christian | Hindu | Muslim | Buddhist | Jewish | Agnostic/Atheist | Sikh | Other | No reply |
|
| ||||||||
| 17.42 | 0.50 | 0.47 | 3.61 | 1.54 | 50.15 | 0.02 | 22.41 | 3.89 |
| Country | ||||||||
| USA | UK | Europe | Canada | Australia/ New Zealand | South/ Central America | Other | No Reply | |
|
| ||||||||
| 54.31 | 15.25 | 11.10 | 7.53 | 4.54 | 2.09 | 4. 59 | 0.59 | |
Number of participants who rated themselves as regular users of a drug and therefore rated their associated harms and benefits are reported in Table 2.
Table 2.
Participants’ experience of drugs.
| Regular users | Occasional users | Ex users | Have tried it | Know someone who has used it | No direct experience /Not heard of it | Total able to rate harms | |
|---|---|---|---|---|---|---|---|
| Alcohol | 2341 | 2472 | 475 | 388 | 54 | 61 | 2341 |
| Amphetamines | 634 | 1236 | 778 | 2653 | 2794 | 3477 | 634 |
| Benzodiazepines | 335 | 792 | 294 | 1281 | 1155 | 1929 | 335 |
| Cannabis: herbal | 2863 | 1302 | 576 | 639 | 243 | 162 | 2863 |
| Cannabis: skunk | 2810 | 1154 | 518 | 570 | 262 | 472 | 2810 |
| Cocaine | 99 | 789 | 506 | 1617 | 1853 | 927 | 99 |
| Ecstasy | 336 | 1353 | 423 | 1332 | 1577 | 765 | 336 |
| Hallucinogens | 1058 | 5202 | 1018 | 7898 | 11606 | 25316 | 14587 |
| Ketamine | 106 | 357 | 106 | 842 | 1739 | 2641 | 106 |
| Nitrous oxide | 126 | 711 | 173 | 1592 | 1016 | 2168 | 12619 |
| Mild stimulants | 3187 | 1524 | 153 | 538 | 113 | 271 | 3187 |
| Opiates | 202 | 441 | 428 | 2168 | 4369 | 9764 | 202 |
| Prescription analgesics | 354 | 952 | 316 | 1783 | 1054 | 1327 | 354 |
| Tobacco | 2107 | 987 | 968 | 1058 | 526 | 145 | 2107 |
| Viagra/Cialis | 43 | 125 | 9 | 412 | 1071 | 4126 | 43 |
‘Mild Stimulants’ = caffeine, khat
Harms
Table 3 presents mean harm ratings of drugs on the seven risk factors. Data for the overall mean harm ratings are presented in Figure 1. They are displayed in terms of the drug’s classification under (a) US schedules and (b) UK Misuse of Drugs Act as they represented the largest number of respondents. Amphetamines and prescription analgesics were excluded from the UK interpretation and opiates/heroin were excluded from the US interpretation, as substances falling within these drug categories had different classifications or scheduling. US ratings of harms were not correlated with their status under the Controlled Substances Act schedule (Spearman’s rank correlation -0.240; p=0.41).
Table 3.
Mean harm ratings of drugs on each of the seven risk factors
| Short-term physical risk | Long-term physical risk | Risk of injecting | Risk to society | Risk of bingeing | Risk of reliance | Risk of craving | |
|---|---|---|---|---|---|---|---|
| Opiates | 1.3 | 2.1 | 2.4 | 1.8 | 2.3 | 2.5 | 2.7 |
| Prescription analgesics | 1.1 | 2.0 | 1.6 | 1.5 | 2.3 | 2.4 | 2.5 |
| Cocaine | 1.1 | 2.2 | 1.4 | 1.8 | 2.5 | 1.6 | 2.5 |
| Alcohol | 1.0 | 2.1 | 0.2 | 2.3 | 2.6 | 1.8 | 2.0 |
| Amphetamines | 1.0 | 1.9 | 1.2 | 1.5 | 2.2 | 1.7 | 2.1 |
| Tobacco | 0.9 | 2.4 | 0.1 | 1.1 | 2.0 | 2.3 | 2.6 |
| Benzodiazepines | 0.9 | 1.9 | 0.7 | 1.1 | 2.1 | 2.2 | 2.1 |
| Ketamine | 0.9 | 1.5 | 1.4 | 0.8 | 1.6 | 0.8 | 1.5 |
| Mild stimulants | 0.5 | 1.1 | 0.5 | 0.5 | 1.3 | 1.4 | 1.6 |
| Ecstasy | 0.8 | 1.4 | 0.4 | 0.6 | 1.7 | 0.6 | 1.2 |
| Nitrous oxide | 0.7 | 1.1 | 0.1 | 0.4 | 1.5 | 0.4 | 1.2 |
| Hallucinogens | 1.0 | 1.2 | 0.5 | 0.7 | 1.1 | 0.3 | 0.6 |
| Viagra/ Cialis | 0.3 | 0.6 | 0.3 | 0.3 | 0.9 | 0.6 | 0.4 |
| Skunk cannabis | 0.3 | 0.7 | 0.1 | 0.3 | 0.6 | 0.3 | 1.1 |
| Herbal cannabis | 0.3 | 0.7 | 0.1 | 0.3 | 0.6 | 0.3 | 1.0 |
Figure 1.
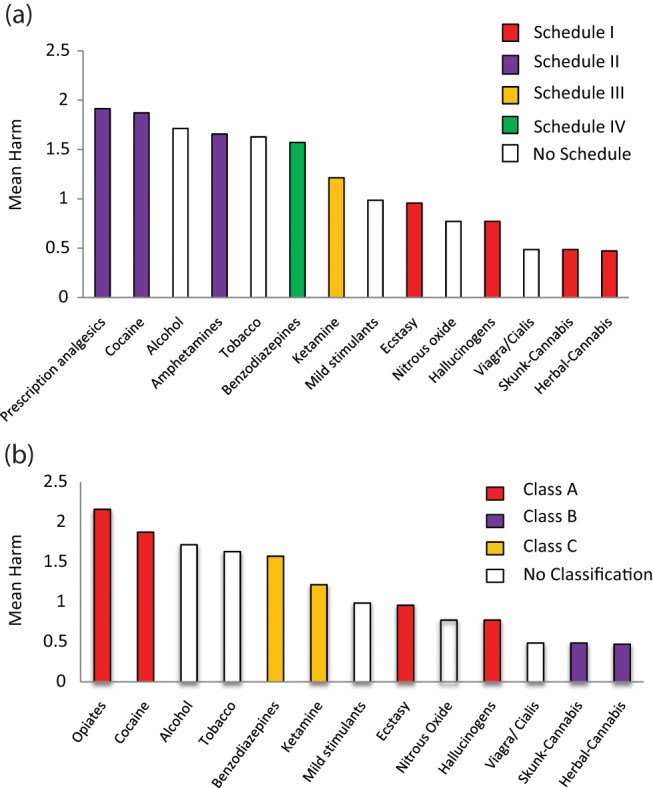
Mean harm ratings of drugs against a) US Schedules under the Controlled Substances Act b) UK legal classifications under the Misuse of Drugs Act.
UK ratings also did not correlate with the legal classifications under the Misuse of Drugs Act, as evidenced in the lack of correlation between ranking of harms by users (Spearman’s rank correlation 0.095; p=0.76).
Benefits
Percentages of participants reporting each of the 10 benefits are shown in Table 4 ranked from highest to lowest percentage. Skunk and herbal cannabis/resin were considered overall to be the most beneficial drugs, followed by prescription analgesics, cocaine and opiates. Sildenafil (Viagra) / Tadalafil (Cialis) and hallucinogens were rated to be least beneficial on these scales. The mean percentage of participants rating each drug as a benefit compared with the mean harm rating of that substance is displayed in Figure 2.
Table 4.
Ranked percentages of participant reporting each of 10 benefits
| Sociability | Enjoyment | State of mind | Relieve pain/ illness | Relieve anxiety/ depression | |||||
|---|---|---|---|---|---|---|---|---|---|
| Ecstasy | 70.6 | Skunk.C | 77.5 | Ketamine | 74.1 | Skunk.C | 71.4 | Benzos | 91.6 |
| Alcohol | 59.3 | Herbal.C | 77.2 | Ecstasy | 71.2 | Herbal.C | 70.7 | Skunk.C | 74.8 |
| Cocaine | 51.8 | Ecstasy | 77.0 | Skunk.C | 62.7 | PPK | 66.8 | Herbal.C | 74.8 |
| Herbal.C | 40.4 | Cocaine | 60.0 | Herbal.C | 62.4 | Opiates | 62.4 | PPK | 70.6 |
| Skunk.C | 40.3 | Ketamine | 54.0 | N2O | 53.8 | Ketamine | 40.1 | Opiates | 64.9 |
| PPK | 39.1 | N2O | 50.2 | PPK | 36.0 | Benzos | 34.0 | Ketamine | 61.3 |
| Benzo | 36.2 | Alcohol | 46.1 | Cocaine | 36.2 | N2O | 24.6 | Ecstasy | 60.0 |
| Opiates | 36.0 | PPK | 45.1 | Opiates | 34.2 | Alcohol | 24.1 | Alcohol | 49.2 |
| Amphet | 31.8 | Amphet | 41.9 | Benzos | 30.3 | Ecstasy | 21.4 | Tobacco | 45.7 |
| Ketamine | 28.8 | Opiates | 39.1 | Alcohol | 28.3 | Cocaine | 19.2 | Cocaine | 45.5 |
| Mild stim | 23.1 | Viagra | 34.0 | Hallucin | 27.6 | Amphet | 15.8 | Amphet | 36.6 |
| Viagra | 20.9 | Mild stim | 31.4 | Amphet | 22.9 | Viagra | 10.8 | N2O | 29.4 |
| Tobacco | 19.6 | Benzos | 26.5 | Mild stim | 13.9 | Mild stim | 8.3 | Mild stim | 22.4 |
| N2O | 15.1 | Hallucin | 22.5 | Viagra | 12.0 | Tobacco | 7.0 | Hallucin | 11.0 |
| Hallucin | 10.9 | Tobacco | 11.2 | Tobacco | 7.1 | Hallucin | 3.7 | Viagra | 9.3 |
| Feel more relaxed/ relieve stress | Help to get to sleep | Help wake up/ have more energy | Improve attention, memory and concentration | Change appearance of body (bulk up/ lose weight) | |||||
| Benzos | 95.8 | Benzos | 90.2 | Cocaine | 84.9 | Amphet | 66.7 | Cocaine | 36.4 |
| Herbal.C | 92.5 | Skunk.C | 78.2 | Mild stim | 83.7 | Mild stim | 63.4 | Amphet | 34.7 |
| Skunk.C | 91.7 | Herbal.C | 77.5 | Amphet | 67.7 | Cocaine | 51.5 | Ecstasy | 22.3 |
| PPK | 86.1 | PPK | 61.3 | Ecstasy | 53.3 | Tobacco | 31.9 | Opiates | 19.8 |
| Tobacco | 82.2 | Opiates | 50.5 | Tobacco | 39.0 | PPK | 28.8 | PPK | 17.5 |
| Alcohol | 81.5 | Alcohol | 43.6 | PPK | 31.9 | Herbal.C | 24.6 | Tobacco | 16.0 |
| Opiates | 67.3 | Ketamine | 17.9 | Opiates | 25.7 | Skunk.C | 23.8 | Mild stim | 14.8 |
| Ketamine | 66.0 | N2O | 16.7 | Ketamine | 17.0 | Opiates | 21.3 | Viagra | 11.6 |
| Ecstasy | 59.5 | Tobacco | 14.2 | Herbal.C | 14.3 | Ecstasy | 16.7 | Herbal.C | 9.2 |
| N2O | 51.6 | Viagra | 4.7 | Skunk.C | 14.0 | Benzos | 14.0 | Ketamine | 9.4 |
| Mild stim | 29.2 | Amphet | 3.2 | Viagra | 9.3 | Viagra | 9.3 | Skunk.C | 8.7 |
| Viagra | 27.9 | Cocaine | 2.0 | Alcohol | 7.3 | Ketamine | 8.5 | Alcohol | 6.2 |
| Cocaine | 25.3 | Mild stim | 2.0 | Benzos | 6.3 | Hallucin | 5.1 | Benzos | 4.8 |
| Amphet | 21.1 | Hallucin | 1.8 | N2O | 4.8 | Alcohol | 1.4 | Hallucin | 1.3 |
| Hallucin | 11.6 | Ecstasy | 1.5 | Hallucin | 4.3 | N2O | 0.8 | N2O | 1.2 |
Herbal.C: herbal cannabis; Skunk.C: skunk cannabis; PPK: prescription painkillers (prescription analgesics); Benzo: benzodiazepines; Amphet: amphetamine; Mild stim: mild stimulants; N2O: nitrous oxide; Hallucin: hallucinogens.
Figure 2.
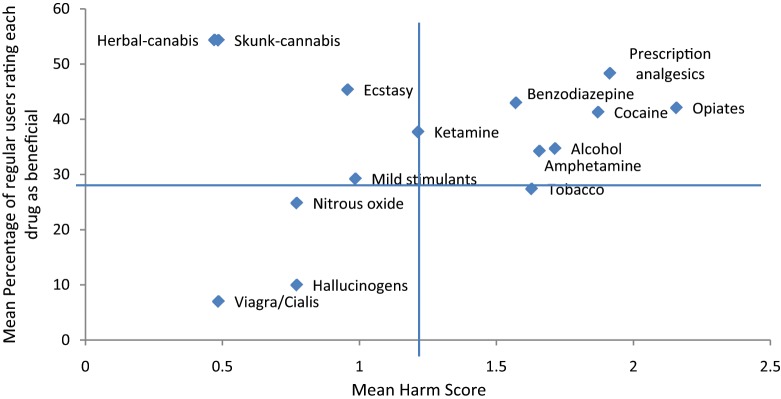
Comparison between mean percentage of participants rating each drug as a benefit and mean harm of drugs.
Drug of choice
Drug preferences of regular users as evidenced by first and second ‘drug of choice’ are displayed in Figure 3. First and second preference profiles for drugs were very different. Skunk, prescription analgesics and opiates were rated highly as first-preference drugs, but were rated relatively low as second preferences. Alcohol, herbal cannabis and benzodiazepines showed the opposite pattern and were rated highly as second preference drugs but not as first preferences. Ecstasy showed consistently high ratings across first and second preferences, whilst tobacco, nitrous oxide (N2O), and hallucinogens were consistently ranked in the bottom 10 drugs.
Figure 3.
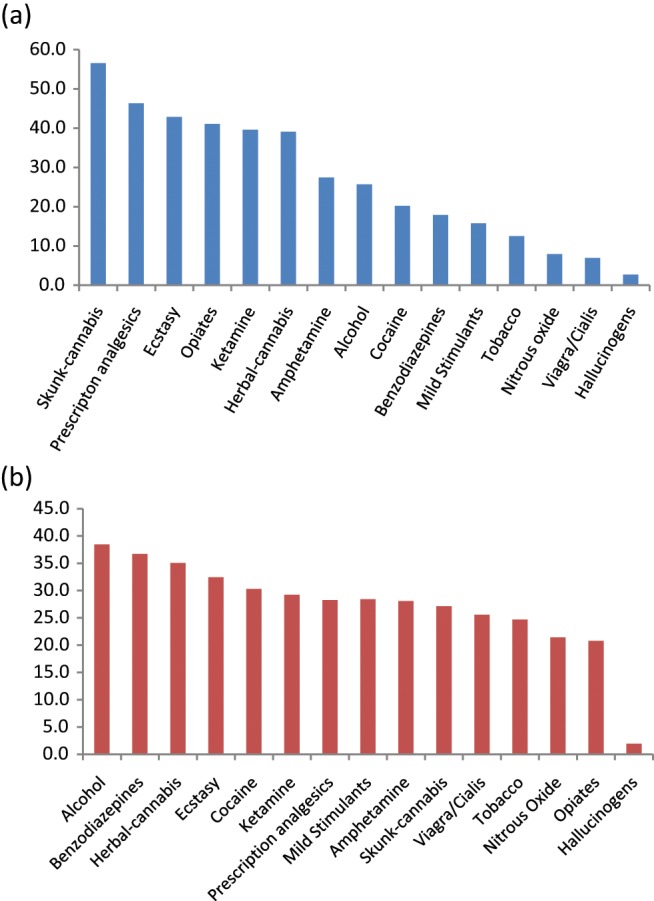
Percentage of participants reporting each drug as a) first preference b) second preference.
Personal use and abuse of drugs
Tobacco consistently had the highest percentage of participants who rated themselves as showing likelihood for abuse or dependence on the CAGE-AID (Table 5).
Table 5.
Ranked percentage of participants using each substance who responded ‘yes’ to two or more CAGE questions
| CAGE score ≥2 (%) | |
|---|---|
| Tobacco | 93.2 |
| Prescribed analgesics | 75.7 |
| Cocaine | 69.7 |
| Opiates | 63.4 |
| Cannabis- skunk | 63.3 |
| Alcohol | 61.7 |
| Cannabis - herbal/resin | 61.1 |
| Benzodiazepines | 57.9 |
| Ketamine | 52.8 |
| Mild stimulant | 43.6 |
| Amphetamines | 43.2 |
| Ecstasy | 42.0 |
| Nitrous oxide | 21.0 |
| Viagra/ Cialis | 17.1 |
| Hallucinogens | 6.9 |
Discussion
In terms of harms, there was a lack of any correlation between the rankings of nearly 6000 individuals and the rankings of drugs within either the US Schedules or the UK Misuse of Drugs Act. The findings in terms of UK rankings concur with previous literature (Nutt et al., 2007, 2010; Morgan et al., 2010b) and in terms of the USA scheduling system are consistent with UK findings yet novel in this context. Over 50% of respondents were from the US, with the majority of users being young (18–24), white, educated and currently either employed or studying.
Harms
Under US scheduling, the drugs rated as most harmful were either classed as Schedule II or not classified, whilst several of the drugs rated as least harmful are currently Schedule I. Similarly in the UK, two currently unclassified drugs – alcohol and tobacco – were rated in the top 10 most harmful drugs, whilst ecstasy and hallucinogens (both Class A drugs) were both rated relatively low on harms. Both strains of cannabis were rated as the least harmful drugs despite their Class B status. High harm ratings appeared to be driven by perceived long-term physical risks, risk of bingeing and craving. As expected, alcohol was perceived as a particularly high risk to society and had the highest perceived risk of bingeing, whilst risk of injecting was associated predominantly with opiate use, perhaps unsurprisingly.
Benefits
Whilst cocaine, ecstasy, mild stimulants and amphetamines were linked to ‘help waking up’ and ‘improving attention and memory’, benzodiazepines, prescription analgesics and both types of cannabis were associated with relaxation, decreased depression/anxiety and relief from pain and illness. Although our division is somewhat arbitrary, overall, herbal and skunk cannabis, ecstasy and ketamine were rated as having low harms but high benefits, and tobacco was rated high on harms and low on benefits. Opiates, prescription analgesics and cocaine showed particularly high harms and benefits. Viagra/Cialis and hallucinogens were rated to be of relatively little benefit.
High benefits, low harms
Herbal cannabis and skunk were consistently placed in the top five drugs across the majority of benefits (except for ‘improving attention, memory and concentration’, ‘help waking up/ have more energy’ and ‘changing appearance of body’). In addition, both strains had the highest percentage of participants reporting benefits of ‘enjoyment’ and ‘relief of physical pain/ symptoms of illness or disease’, with skunk showing a slightly higher percentage in both instances. The two strains of cannabis were rated similarly for benefits, both with a primary benefit of relaxation/stress relief followed by their ability to aid sleep and enjoyment. There was little difference between skunk and other forms of cannabis, which is surprising given recent debates about increased harms of high-THC/low-cannabidiol varieties (di Forti et al., 2009; Morgan et al., 2010a,c). Ecstasy was also rated highly across all benefits (except for relaxation, relief from anxiety/ depression, relief of pain and help sleeping). MDMA was the highest ranked drug in the sociability category, with ‘feeling closer to people/empathy’ being the most often reported aspect of sociability. In contrast with both UK and USA classification systems, skunk and herbal cannabis were rated as the least harmful drugs whilst ecstasy was rated as sixth least harmful. These low harm scores were driven by particularly low perceived risk of dependence, risk to society and risk of injecting.
Ketamine was ranked fifth as a drug of choice, and was ranked high on benefits for an individual’s state of mind, enjoyment and pain relief. Ketamine was ranked eighth overall in terms of harms, higher than the two types of cannabis and ecstasy, which appears to be a result of higher ratings on measures of craving, bingeing and long-term physical risk, concurrent with recent reports of dependence on ketamine (Morgan and Curran, 2011).
High benefits, high harms
Cocaine showed consistently high rankings across all benefits but was rated as the third most harmful drug due to high perceived risk of bingeing, dependence and craving as well as long-term physical risk. Prescription analgesics were also ranked in the top 10 drugs across every benefit except ‘help waking up’, and were ranked in the top four in terms of relief from anxiety/ depression, stress and physical pain. As with cocaine, perceived overall harm of prescription analgesics was also extremely high (second most harmful). Opiates were rated as the most harmful drug, but were perceived to be highly beneficial for pain relief, alleviation of anxiety/ depression and stress. Whilst these drugs shared some of the benefits and harms of prescription analgesics, they were less likely to be a drug of choice, which may be due to the higher risk of injecting and craving associated with this group.
Benzodiazepines had the benefits of sedative and anti-depressant/anxiolytic effects and showed similar rankings as opiates in terms of sociability and state of mind. Benzodiazepines were rated as considerably less harmful than opiates; in this respect, the perceptions of these drugs concurs with their legal status. The high preference for prescription analgesics and benzodiazepines by regular users is a profile that has not been reported in any other study and may indicate a relatively unusual sample, or may reflect the recent trend towards prescription drug use in the US.
Low benefits, high harms
Tobacco was consistently ranked in the bottom three drugs in terms of benefits, with the exception of relieving anxiety/ depression or feeling more relaxed/ relieving stress. Whilst tobacco was ranked seventh in overall harms, this drug was unsurprisingly associated with high long-term physical risk and risk of reliance. Tobacco had the highest proportion of likely dependent users as classified by the CAGE.
Amphetamines and alcohol were rated to be of medium benefit. Both were rated as drugs with high risk of bingeing and craving, but amphetamines scored highly on benefits of stimulant effects such as waking up/ having more energy, changing appearance of the body and were ranked as the most beneficial drugs in terms of improving attention, memory and concentration. Alcohol was thought to be highly beneficial for sociability. It was ranked fifth in terms of harms, with particularly high risk to society and risk of bingeing.
Low benefits, low harms
Drugs that were rated as having low harms and low benefits were Viagra, hallucinogens, nitrous oxide and mild stimulants. The low beneficial rating of hallucinogens contradicts the findings of our prior UK drug survey (Morgan et al., 2010b). where hallucinogens were rated as one of the drugs with greatest long-term benefits. Hallucinogens were the least preferred drug, which may reflect the inclusion of a wider group of users compared with all other substances, and along with Viagra/cialis were ranked in the bottom five on all benefits. This is perhaps surprising given the use of Viagra/Cialis as a medicine and previous reports of the positively beneficial effects of hallucinogens (e.g. Griffiths et al., 2006, 2008); this may, however, reflect the very specific benefits of these substances which are not reflected in a mean overall benefits rating on the scale used in this study.
Abuse and dependence
The USA scheduling system is based on the potential for abuse of each substance, hence one might expect it to be mirrored in the proportion of individuals scoring in the abuse range of the CAGE-AID for the different drugs included in this survey. However, in the present study tobacco had the highest proportion of regular users showing possible abuse or dependence, followed by opiates, prescription analgesics, cocaine and alcohol. Thus three drugs in the UK and two in the US which are currently unclassified produce the greatest likelihood of abuse or dependence, albeit on a crude scale. Indeed, in the case of prescription analgesics, opiates, cocaine and alcohol, the overall high harm ratings obtained tended to result from high risks of reliance and craving, whilst tobacco scored particularly high in terms of reliance. Furthermore, ecstasy and hallucinogens, currently Class A and Schedule I, were scored low in the proportion of regular users showing possible abuse on the CAGE-AID.
Limitations
As an internet survey, it was not possible to verify that each respondent was unique, and the sample was inevitably self-selecting. Of the nearly 6000 individuals who completed the survey, the majority were well educated, white, employed or studying. The survey was only translated into English, Spanish and French, and this may have reduced the number of respondents from many countries where other languages predominate. At the same time, this is the first multi-language survey of drug users to date with the largest number of respondents who were spread across 61 countries worldwide.
A further limitation of the current study is that the harms and benefits of polysubstance use, which is becoming the norm amongst the vast majority of drug users, were not addressed. This was beyond the scope of this study and it would be have been a complex task for drug users to rate the effects of multiple substances. Further, research suggests that drug users are aware of the key effects of the drugs they take, even novel compounds such as mephedrone (Carhart-Harris, 2011), despite being taken in combination with other substances. However, future work should aim to explore this interesting issue. Similarly, the study could not assess the context dependence of the benefits or harms or the benefits of the drug effects versus drug culture, for example the benefits of the sociable dance music culture that can occur around ecstasy use. This study also did not distinguish between what were benefits of acute drug effects and longer-term benefits (although we attempted this in our previous UK drug survey, Morgan et al., 2010b). In future work, we would aim to compare harms and benefits on similar scales, and take into account context effects.
Another limitation was that the number of users rating on hallucinogens was much greater than for other substances because, as there are no ‘regular’ users, this included people who had ever tried any of a wide range of hallucinogens. For all other drugs, harms and benefits could only be rated by those who judged themselves regular users and so data for hallucinogens were comparatively skewed. Thirdly, there were low numbers rating some drugs (e.g. crack) and we did not explore the use of different drugs in combination, mainly to restrict the length of the survey so as to increase completion rates. Only regular users of each drug were allowed to rate its benefits and harms in the current study, thus drug benefits may be perceived to be greater than if a sample of ex- or non-users were used. Regular users may downplay risks in their continued use of these substances, much as a car driver plays down the risk of road traffic accidents. Therefore it could be argued that users are not the best people to rate on harms. However, in our previous study of drug users’ views of harms (Morgan et al., 2010b) we found a very high correlation between ‘expert’ and user ratings of harm, therefore it would seem that even if users downplay the risks in their own behaviour, or simply weight the benefits greater than the potential costs, this would not appear to substantially diminish their awareness of the severity of the harms. Further, this sample is unique in its ability to provide extensive knowledge of drug effects, particularly benefits, across a range of psychoactive substances. Given that the literature on drug use has been dominated by research into harms, taking into account the views of these users – even if they might be skewed towards more positive perceptions of recreational drugs – is important if we are to converge on a more balanced position on illicit substance use.
Implications
Our survey expanded upon that of Nutt et al. (2007, 2010) by including a detailed assessment of the perceived benefits of drugs. A full scientific understanding of the relative harms and benefits of recreational drugs is important. In understanding the perceived benefits of illicit substances we may learn about the motivation behind their use, which can prove useful in developing treatment programmes. The lack of correlation between the users’ ranked harms and drug classifications in the UK and USA suggest that current drug policy is not serving to inform those who take drugs of the harms of these substances. Furthermore, the prevalence of use of each substance within this sample suggests that current policy does not influence whether people choose to use the drug. For example, herbal cannabis and skunk, currently Class B in the UK and Schedule I in the USA, were respectively the second and third most regularly used drugs.
The high benefits and low harms of skunk, herbal cannabis and ecstasy do not correspond with their current legal classifications. Further, alcohol and several prescription analgesic drugs are currently not classified in the UK, e.g. Tramadol, but were rated high in harm, whereas in the USA all prescription analgesics have been classified as Schedule II. Whilst these results might be taken to imply that prescription analgesic drugs should be placed in the highest class or schedule, these drugs were also rated as having a wide variety of benefits. Although a system based entirely on drug harms has been suggested to be unworkable (Caulkins et al., 2011), it would seem prudent to produce a full assessment of the relative harms and benefits of psychoactive substances – which perhaps this preliminary study may in some way inform – so that policy makers may more accurately take into account the relative harms and benefits when deciding how to control these substances. Whilst these data, which are simply the opinions of drug users, may not serve to inform policy, they can inform us of the views of drug users on the perceived benefits and harms of psychoactive substances, which may be important for effective drugs education and treatment.
Conclusion
In summary, there are very marked disparities between the rated harms of different drugs by nearly 6000 users and the rankings of these drugs in both UK and USA classification systems. In particular the classification of skunk, herbal cannabis/resin and ecstasy appears arbitrary not only in terms of rated harms but also ranked benefits, preference and dependence. Currently unclassified drugs (alcohol and prescription analgesics (UK)) had high ratings of harms but also relatively high ranking of benefits and high preference. It is therefore important to consider both the perceived consequences and motivations for drug use to better inform both policy and educational programmes.
Acknowledgments
The authors are grateful to those at Erowid (especially Fire) who facilitated the survey. We thank the reviewers of this paper for their insightful comments.
Footnotes
Conflict of interest: The study was funded by the Beckley Foundation which seeks to change global drug policy, therefore we note a potential conflict of interest.
Funding: This study was aided by a small grant from the Beckley Foundation.
References
- Brown RL, Rounds LA. (1995). Conjoint screening questionnaires for alcohol and other drug abuse: Criterion validity in a primary care practice. Wis Med J 94:135–140 [PubMed] [Google Scholar]
- Carhart-Harris RL. (2011) A web based survey on mephedrone. Drug Alcohol Depend 118: 19–22 [DOI] [PubMed] [Google Scholar]
- Carhart-Harris RL, Nutt DJ. (2010) User perceptions of the benefits and harms of hallucinogenic drug use: A web-based questionnaire study. J Subst Use 15: 283–300 [Google Scholar]
- Caulkins J, Reuter P, Coulson C. (2011) Basing drug scheduling decisions on scientific ranking of harmfulness: False promise from false premises. Addiction 106: 1886–1890 [DOI] [PubMed] [Google Scholar]
- Centre for Disease Control and Prevention (2011) Vital signs: Overdoses of prescription opioid pain relievers—United States, 1999–2008. Available at: http://www.cdc.gov/vitalsigns (accessed 5 February 2012). [PubMed]
- Cohen P. (2010) The concept of ‘drug harms’. Drug Alcohol Today 10: 10–12 [Google Scholar]
- Coulson C, Caulkins J. (2012) Scheduling of newly emerging drugs: A critical review of decisions over 40 years. Addiction 107: 766–773 [DOI] [PubMed] [Google Scholar]
- Di Forti M, Morgan C, Dazzan P, et al. (2009) High-potency cannabis and the risk of psychosis. Br J Psychiatry 195: 488–491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B, Kendall P. (2011) Nutt et al’s harm scales for drugs – Room for improvement but better policy based on science with limitations than no science at all. Addiction 106: 1891–1892 [DOI] [PubMed] [Google Scholar]
- Griffiths R, Johnson W, Richards W, et al. (2011) Psilocybin occasioned mystical-type experiences: Immediate and persisting dose-related effects. Psychopharmacology 218: 649–665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths R, Richards W, Johnson W, et al. (2008) Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later. J Psychopharmacol 22: 621–632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths R, Richards W, McCann U, et al. (2006) Psilocybin can occasion mystical experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology 187: 268–283 [DOI] [PubMed] [Google Scholar]
- Johansen P, Krebs T. (2009) How could ecstasy help anxiety disorders? A neurobiological rationale. J Psychopharmacol 23: 389. [DOI] [PubMed] [Google Scholar]
- Kalant H. (2010) Drug classification: science, politics, both or neither? Addiction 105: 1146–1149 [DOI] [PubMed] [Google Scholar]
- Krebs T, Johansen P. (2012) Lysergic acid diethylamide (LSD) for alcoholism: Meta-analysis of randomized controlled trials. J Psychopharmacol 26: 994–1002 [DOI] [PubMed] [Google Scholar]
- Krupitsky E, Burakov A, Romanova T. (2002) Ketamine psychotherapy for heroin addiction. J Subst Abuse Treat 23: 273–283 [DOI] [PubMed] [Google Scholar]
- Mackay J, Eriksen M, Shafey O. (2006) The Tobacco Atlas, 2nd Edition. Atlanta, GA: American Cancer Society [Google Scholar]
- Mithoefer M. (2006) MDMA-assisted psychotherapy in the treatment of posttraumatic stress disorder (PTSD): Ninth update on study progress. MAPS Bull 16: 14–15 [Google Scholar]
- Morgan CJ, Curran HV. (2011) Ketamine use: a review. Addiction 107: 27–38 [DOI] [PubMed] [Google Scholar]
- Morgan CJA, Freeman TP, Schafer GL, et al. (2010a) Cannabidiol attenuates the appetitive effects of Δ9-tetrahydrocannabinol in humans smoking their chosen cannabis. Neuropsychopharmacology 35: 1879–1885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan CJ, Muetzelfeldt L, Muetzelfeldt M, et al. (2010b) Harms associated with psychoactive substances: Findings of the UK National Drug Survey. J Psychopharmacol 24: 147–153 [DOI] [PubMed] [Google Scholar]
- Morgan CJA, Schafer G, Freeman TP, et al. (2010c) Impact of cannabidiol on the acute memory and psychotomimetic effects of smoked cannabis: Naturalistic study. Br J Psychiatry 197: 285–290 [DOI] [PubMed] [Google Scholar]
- Móró L, Noreika V. (2011) Sacramental and spiritual use of hallucinogenic drugs. Behav Brain Sci 34: 319–320 [DOI] [PubMed] [Google Scholar]
- Müller C, Schumann G. (2011) Drugs as instruments: A new framework for non-addictive psychoactive drug use. Behav Brain Sci 34: 293–347 [DOI] [PubMed] [Google Scholar]
- Nutt D, King LA, Saulsbury W, et al. (2007) Development of a rational scale to assess the harm of drugs of potential misuse. Lancet 369: 1047–1053 [DOI] [PubMed] [Google Scholar]
- Nutt DJ, King LA, Philips LD. (2010) Drug harms in the UK: A multicriteria decision analysis. Lancet 376: 1558–1565 [DOI] [PubMed] [Google Scholar]
- Obot I. (2011) Improved ranking of drugs on harmfulness can bring sense and order to a failed system. Addiction 106: 1894–1895 [DOI] [PubMed] [Google Scholar]
- Room R, Lubman DI. (2010) Politics and science in classifying the dangers of drugs. Evid Based Ment Health 13: 97–99 [DOI] [PubMed] [Google Scholar]
- Sessa B. (2005) Can psychedelics have a role in psychiatry once again? Br J Psychiatry 186: 456–457 [DOI] [PubMed] [Google Scholar]
- Sessa B. (2007) Is there a case for MDMA-assisted psychotherapy in the UK? J Psychopharmacol 21: 220–224 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2011) Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-41, HHS Publication No. (SMA) 11–4658. Rockville, MD: Substance Abuse and Mental Health Services Administration [Google Scholar]
- Tart C. (1971) On Being Stoned: A Psychological Study of Marijuana Intoxication. Palo Alto: Science and Behavior Books [Google Scholar]
- United Nations Office on Drugs and Crime (2010) World Drug Report (2010). Vienna: United Nations [Google Scholar]
- US Department of Justice National Drugs Intelligence Centre (2011) National Drug Threat Assessment- Executive Summary. Washington, DC: US Department of Justice National Drugs Intelligence Centre [Google Scholar]
- van Amsterdam J, Opperhuizen A, Koeter M, et al. (2010) Ranking the harm of alcohol, tobacco and illicit drugs for the individual and the population. Eur Addict Res 16: 202–207 [DOI] [PubMed] [Google Scholar]
- Walton R. (1938) Marihuana. America’s New Drug Problem. New York: JB Lippincott [Google Scholar]
- World Health Organisation (2011) Global Status Report on Alcohol and Health. Geneva, Switzerland: WHO [Google Scholar]


