Abstract
Early rehospitalization after kidney transplantation (KT) is common and may predict future adverse outcomes. Previous studies using claims data have been limited in identifying preventable rehospitalizations. We assembled a cohort of 753 adults at our institution undergoing KT from January 1, 2003—December 31, 2007. Two physicians independently reviewed medical records of 237 patients (32%) with early rehospitalization and identified 1) primary reason for and 2) preventability of rehospitalization. Mortality and graft failure were ascertained through linkage to the Scientific Registry of Transplant Recipients. Leading reasons for rehospitalization included surgical complications (15%), rejection (14%), volume shifts (11%), and systemic and surgical wound infections (11% and 2.5%). Reviewer agreement on primary reason (85% of cases) was strong (kappa=0.78). Only 19 rehospitalizations (8%) met preventability criteria. Using logistic regression, weekend discharge (OR 1.59, p=0.01), waitlist time (OR 1.10, p=0.04), and longer initial length of stay (OR 1.42, p=0.03) were associated with early rehospitalization. Using Cox regression, early rehospitalization was associated with mortality (HR 1.55; p=0.03) but not graft loss (HR 1.33; p=0.09). Early rehospitalization has diverse causes and presents challenges as a quality metric after KT. These results should be validated prospectively at multiple centers to identify vulnerable patients and modifiable processes-of-care.
Keywords: Kidney, rehospitalization, survival, preventability
Introduction
Early rehospitalization following kidney transplantation (KT) is common, conferring high costs to the United States (US) health care system. An analysis of Medicare data from 2003 – 2006 found that 28.5% of KT recipients had Medicare claims for a readmission within 30 days (1) a considerably higher rate than for patients undergoing other intra-abdominal surgeries (10–16%) (2) or patients in the general population (19.6%) (3). The mean cost of each transplant rehospitalization was nearly $10,000 (1). Recent changes in Medicare reimbursement penalize hospitals for early rehospitalization after certain admissions, and excess rehospitalization rates are scrutinized as a quality-of-care indicator (4–6). However, high rehospitalization rates may also reflect a patient population of greater medical complexity and acuity, characteristics that may be incompletely captured by risk-adjustment methods available to Medicare (7, 8). Despite the relatively high frequency and cost associated with early rehospitalization following KT, little remains known about the reasons for these events and which rehospitalizations are unplanned or potentially preventable.
KT recipients are uniquely vulnerable to adverse events following discharge from transplantation, especially given the large burden of comorbidities in this population (including diabetes, hypertension, and vascular disease) (9), and more elderly patients being transplanted than ever before (10, 11). Therefore, some early rehospitalizations following transplant may be seen as part of the acceptable risk of a major surgical procedure in patients with significant co-morbidities and the prospect of long-term clinical benefit (12), while others may be preventable, such as those due to failures in the process of transitioning care (5, 13). In 2012, McAdams-De-Marco et al. examined early rehospitalization rates for Medicare-covered KT recipients. This important study revealed variation in early rehospitalization rates between centers, which may be explained not only by differences in patient populations but also by varying quality in transitions-of-care between transplant centers (14). With the exception of initial hospitalization length of stay, the study lacked detailed data about process-of-care measures that might lead to this outcome.
To our knowledge, only one prior study has examined preventability of rehospitalizations after KT. In an analysis of over 400,000 rehospitalizations using Florida Medicare claims data, Goldfield et al. estimated a potentially preventable rehospitalization rate (PPR) of 20.6% following KT, compared to an average surgical PPR rate of 7.9% (15). However, the PPR rates provided limited clinical insight, given they were calculated with a complex algorithm utilizing diagnosis related group (DRG) codes to determine whether readmissions were unplanned and/or related to the previous admission. Closer scrutiny of these events is needed to achieve a better understanding of the preventability of KT rehospitalizations.
In light of the limitations of previous studies, the goals of this study were to 1) identify reasons for early rehospitalization following KT by chart review, 2) adjudicate potential preventability of these rehospitalizations, 3) examine associations of recipient, donor, allograft and process-of-care variables with early rehospitalization, and 4) examine the associations of early rehospitalization with mortality and all-cause graft loss.
Materials and Methods
Study Population
The study population included all adults (≥ 18 years of age) undergoing KT at the University of Pennsylvania from January 1, 2003 – December 31, 2007. We excluded multi-organ transplant recipients, and recipients who died prior to discharge from KT. Early rehospitalization was defined as the first hospitalization within 30 days of discharge from KT. To ensure ascertainment of our primary outcome of early rehospitalization, we reviewed extensive center records during the 30 day timeframe, including clinic notes and transplant coordinator communications that describes hospitalizations occurring at other hospitals. Donor, recipient, and transplant variables were abstracted from patient records and were linked to the Scientific Registry of Transplant Recipients (SRTR) for verification of graft survival. The SRTR includes data on all donor, wait-listed candidates, and transplant recipients in the US, submitted by members of the Organ Procurement and Transplantation Network (OPTN), and has been described elsewhere. The Health Resources and Services Administration (HRSA), US Department of Health and Human Services provides oversight to the activities of the OPTN and SRTR contractors. Mortality was ascertained through center records and linkage to the Social Security Death Master File. Follow-up information was available for patients on death and graft loss until December 31 2011. Median follow-up was six years.
Determination of Reasons for and Preventability of Early Rehospitalization
Using preliminary data from a chart review analysis of a separate one-year cohort of KT recipients at our institution between 2010–2011, we identified categories of reasons for early rehospitalization (16). We adapted a chart review instrument previously validated in general medicine patients to adjudicate reasons for and preventability of early rehospitalization (17, 18). We reviewed instrument content with a panel of five experts including transplant nephrologists, transplant surgeons, and an expert on survey instrument development (JAS). We trained two physicians (EL and AP) in the use of the survey instrument and completed a pilot phase of 20 patients outside the study cohort. The physician reviewers then independently reviewed the medical records, including inpatient and outpatient charts and transplant coordinator records, of KT recipients who were rehospitalized within 30 days. The reviewers categorized early rehospitalizations according to four patterns described in prior studies of preventability (15): 1) unplanned and related to KT, 2) unplanned and unrelated to KT, 3) planned and related to KT, and 4) planned and unrelated to KT. The reviewers then identified the 1) reason for rehospitalization and 2) preventability of each rehospitalization. Preventability was determined based on specific criteria (see Table 1 for specific criteria; see Appendix for complete survey instrument). Only if an early rehospitalization event met one or more of these criteria could an event be categorized as potentially preventable. The clinician experts were blinded to each other’s assessments.
Table 1.
Criteria for Preventable Rehospitalizations
| Criteria: Rehospitalization would have been prevented if: | Number of individuals meeting criteria |
|---|---|
| 1) The patient had an outpatient physician/NP assessment prior to being admitted. | 7 |
| 2) The patient had received prescribed medications. | 0 |
| 3) The patient had been compliant with their medication regimen. | 3 |
| 4) The patient had understood their discharge instructions. | 0 |
| 5) Communication had been better between inpatient and outpatient providers. | 0 |
| 6) Outpatient diagnostic or therapeutic procedures had been available. | 2 |
| 7) An alternative medical regimen had been prescribed at discharge. | 6 |
| 8) The patient lived closer and could have been treated as an outpatient. | 0 |
| 9) The patient had a clinical parameter or surgical issue appropriately addressed during their index hospitalization. | 1 |
| 10) The patient had adequate support at home. | 0 |
Statistical Analysis
All analyses were performed using STATA/MP for Mac (College Station, TX, USA). Categorical variables (e.g., gender, ethnicity) were described by their frequencies. Continuous variables (e.g., age, cold ischemia time) were described by their mean, median, range, and standard deviation. Binary variables were compared between groups using the chi-square test or Fisher’s exact, as appropriate. To compare continuous variables between groups, we used Wilcoxon rank-sum tests or Student’s t-tests, as appropriate.
Analysis of Inter-rater Reliability – Reasons for and Preventability of Rehospitalization
We used the Cohen’s kappa statistic to quantify inter-rater reliability regarding the primary reason for hospitalization or the assessment of preventability. When the initial two reviewers disagreed, the principal investigator (MN) reviewed medical records and the team of reviewers formed a consensus.
Model-Building Strategy
Our goal was to build parsimonious explanatory models for early rehospitalization, all-cause graft loss, and mortality. This modeling approach has the advantage of presenting easily interpretable results for clinicians, and identifies the strongest associations for our outcomes of interest. In order to generate a multivariable logistic regression model for the outcome of rehospitalization and Cox proportional hazards regression models for the outcomes of death and all-cause graft loss, we initially entered all variables significant at the 20% level on bivariate analysis, and retained the covariates that improved model fit using the Akaike information criterion (AIC). The AIC penalizes models with additional numbers of variables, thus favoring parsimony (19). We then removed, one by one, variables that did not significantly contribute to the multivariable model on the basis of the Wald test (p-value threshold 0.05) or change the coefficients of the remaining variables in the model (change threshold 20%) (20). For the Cox proportional hazards models, we examined Schoenfeld residuals and inspected log-log plots to confirm the proportional hazards assumption. We also built a multinomial logistic model examining number of early rehospitalizations as the outcome.
The following variables were considered as potential covariates:
recipient age category at transplant, sex, race (black or non-black), body mass index (BMI), dialysis vintage (0 years, ≤1 year, ≤2 years, >2 years), time on the waitlist, causes of end stage renal disease, socioeconomic status (a score derived from census data and recipient zip code (21)), history of diabetes, cardiovascular disease (defined as prior myocardial infarction, coronary artery bypass grafting, positive stress test, coronary angioplasty, or documented systolic or diastolic heart failure), peripheral vascular disease, previous solid organ transplant, primary medical payor (private vs. other), cytomegalovirus (CMV) seropositivity, and hepatitis C seropositivity;
donor age, sex, race (black or non-black), CMV status, and donor type (live vs. deceased donor, expanded criteria deceased donor);
allograft variables of delayed graft function, cold ischemia time and human leukocyte antigen mismatch (zero mismatch or not); and
process-of-care variables of length of initial transplant hospitalization (long stay defined as >4.5 days given median hospitalization of four days), intensive care unit stay during index hospitalization, weekend (defined as Saturday or Sunday) discharge, discharge on insulin, number of total discharge medications, and discharge on narcotics.
Only two variables had missing observations (BMI [n=5] and cold ischemia time [n=17]). To confirm that the missingness in these variables did not bias our estimates, we performed sensitivity analyses assuming the missing observations were at either extreme of their distributions. These analyses did not alter the associations observed in our final models.
Results
Study Population
A total of 753 adults were discharged following KT at our institution during the study period. Two additional patients received a KT but died prior to discharge, and were not included in the analysis. As shown in Table 2, the median age was 51 years (13.3); 34% were black, 64% were male, and 66% received deceased donor transplants. A total of 237 (32%) experienced the primary outcome of rehospitalization within 30 days. Specifically, 180 (24%) recipients experienced one early rehospitalization, 43 (5.7%) recipients had two rehospitalizations and 14 (1.9%) recipients had three rehospitalizations. The median time to first early rehospitalization was nine days (interquartile range 5–15 days). The median duration of patient follow-up was six years. For comparison, the median age of the US national cohort of KT recipients over the study period (n=74, 475) was 50 years (13.6); 24% were black, 60% were male, and 60% were deceased donor transplants.
Table 2.
Patient Characteristics (n=753)
| Full sample N=753 | Not Rehospitalized N=516 | Rehospitalized N=237 | p-value | |
|---|---|---|---|---|
| Recipient Variables | ||||
| Age (years) | 51.38 (13.3) | 51.95 (13.4) | 50.61 (13.1) | 0.783 |
| Sex | 0.251 | |||
| Female | 270 (36%) | 178 (35%) | 92 (39%) | |
| Male | 483 (64%) | 338 (65%) | 145 (61%) | |
| African American | 255 (34%) | 174 (34%) | 81 (34%) | 0.902 |
| Cause of ESRD | 0.76 | |||
| Diabetes Type I | 46 (6%) | 30 (6%) | 16 (7%) | |
| Diabetes Type II | 124 (16%) | 84 (16%) | 40 (17%) | |
| Hypertensive Nephrosclerosis | 104 (14%) | 75 (15%) | 29 (12 %) | |
| FSGS | 79 (11%) | 49 (10%) | 30 (12%) | |
| IgA Nephropathy | 35 (5%) | 26 (5%) | 9 (4%) | |
| Non-FSGS, Non-IgA Glomerunephropathy | 135 (18%) | 93 (18%) | 42 (17%) | |
| Allograft Nephropathy | 2 (0.2%) | 1 (0.2%) | 1 (0.4%) | |
| ADPKD | 83 (11%) | 60 (12%) | 23 (10%) | |
| Congenital Nephropathy | 42 (6%) | 27 (5 %) | 15 (6%) | |
| Hepatorenal Syndrome | 3 (0.4%) | 3 (0.6%) | 0 (0.0%) | |
| Other | 100 (12%) | 64 (13%) | 37 (15%) | |
| Body Mass Index | 27.37 (5.6) | 27.5 (5.7) | 27.1 (5.5) | 0.35 |
| History of Hypertension | 640 (85%) | 438 (86%) | 202 (83%) | 0.65 |
| History of Diabetes | 210 (28%) | 143 (27%) | 67 (28%) | 0.133 |
| History of Prior Solid Organ Transplant | 94 (13%) | 56 (11%) | 38 (16%) | 0.046 |
| Primary Payor | ||||
| Private Insurance | 345 (46%) | 243 (48%) | 102 (42%) | 0.329 |
| Public Insurance | 408 (54%) | 268 (52%) | 140 (58%) | |
| Socioeconomic Index Score (21) | 51.4(4.27) | 51.0(4.38) | 50.9(4.01) | 0.661 |
| Time on the Wait List (years) | 1.58 (1.66) | 1.50 (1.6) | 1.75 (1.8) | 0.015 |
| CMV Status | 0.341 | |||
| R−/D+ | 156 (21%) | 109 (21%) | 47 (19%) | |
| R+/D+ | 222 (30%) | 143 (28%) | 79 (36%) | |
| R+/D− | 154 (21%) | 100 (20%) | 54 (22%) | |
| R−/D− | 166 (7%) | 122 (24%) | 44 (18%) | |
| HCV Antibody Positive | 69 (9%) | 47 (9%) | 22 (9%) | 0.939 |
| History of CVD * | 136 (18%) | 95 (18%) | 41 (17%) | 0.713 |
| History of PVD | 8(1%) | 3(0.6%) | 5(2%) | 0.069 |
| Dialysis Vintage (years) | 0.724 | |||
| 0 | 306 (41%) | 211 (42%) | 95 (39%) | |
| <1 | 128 (17% | 87 (17%) | 41 (17%) | |
| ≥1, <2 | 69 (9%) | 49 (10%) | 20 (8%) | |
| ≥2 | 250 (33%) | 163 (32%) | 87 (36%) | |
| Donor Variables | ||||
| Age (years) | 41.83 (14.9) | 41.49 (14.9) | 42.42 (14.9) | 0.423 |
| African American | 198 (26%) | 128 (25%) | 70 (30%) | 0.731 |
| Zero Antigen Mismatch | 56 (7%) | 43 (8%) | 13 (6%) | 0.167 |
| Deceased Donor | 500 (66%) | 327 (64%) | 173 (72%) | 0.036 |
| Extended Criteria Deceased Donor | 39 (5%) | 26 (5%) | 13 (5%) | 0.875 |
| Delayed Graft Function | 140 (19%) | 85 (16%) | 55 (23%) | 0.039 |
| Process of Care Variables | ||||
| Index Hospitalization Length of Stay (days) | 5.19 (3.24) | 5.05 (3.15) | 5.5 (3.41) | 0.038 |
| Number of Discharge Medications | 13.60 (2.6) | 13.54 (2.6) | 13.82(2.6) | 0.16 |
| Discharged on Insulin | 226 (30%) | 155 (30%) | 71 (30%) | 0.767 |
| Discharged on Narcotics | 635 (84%) | 432 (84%) | 203 (84%) | 0.769 |
| Cold Ischemia Time (hours) | 10.58 (9.5) | 10.11 (9.3) | 11.52 (10.0) | 0.061 |
| ICU Stay | 75 (10%) | 46 (9%) | 29 (13%) | 0.158 |
| Discharged on the Weekend | 189 (25%) | 118 (23%) | 71 (30%) | 0.037 |
Abbreviations: ESRD – End Stage Renal Disease; FSGS –Focal Segmental Glomerulosclerosis; ADPKD—Autosomal Dominant Polycystic Kidney Disease; CMV—Cytomegalovirus; HCV—Hepatitis C Virus; R—Recipient; D—Donor; CVD—Cardiovascular Disease; PVD—Peripheral Vascular DiseaseThe following variables had missing data: Body Mass Index (N=748), Cold Ischemia Time (N=736)
CVD defined as prior myocardial infarction, coronary artery bypass grafting, positive stress test, coronary angioplasty, or documented systolic or diastolic heart failure.
Categories of and Reasons for Rehospitalization
Reviewers agreed on rehospitalization patterns (i.e., planned and related, unplanned and unrelated, etc.) in 90% of cases (kappa=0.68, p=0.04). Among the 237 patients with early rehospitalization, 214 (90%) experienced unplanned early rehospitalization events. The majority of these unplanned early rehospitalizations (n=201 of 214, 94%) were graded as related to KT. In contrast, only 21 early rehospitalizations (9% of all rehospitalizations) were graded as planned and related to KT (e.g., peritoneal dialysis catheter removal), and two rehospitalizations were deemed planned but unrelated to KT. As shown in Table 3, the leading causes of the 201 early rehospitalization that were unplanned and related to KT were post-surgical complications including systemic thrombosis (e.g., deep vein thrombosis) and pain (15%), rejection (14%), volume overload or depletion (11%), and systemic and surgical wound infections (11% and 2.5%, respectively). Agreement on the primary reason for rehospitalization was strong; reviewers agreed in 84.5% of cases (kappa=0.78, p=0.03).
Table 3.
Reasons for Unplanned Early Rehospitalizations Related to KT by Preventability
| Total | Preventable | Not Preventable | |
|---|---|---|---|
| Post-Surgical Complications* | 34 | 3 | 31 |
| Rejection | 28 | 1 | 27 |
| Volume Overload or Depletion | 22 | 2 | 20 |
| Infection | 21 | 2 | 19 |
| Graft Dysfunction - Not Rejection | 14 | 0 | 14 |
| Drug Toxicity or Interaction | 8 | 0 | 8 |
| Electrolyte Abnormalities | 11 | 4 | 7 |
| Symptomatic Anemia | 4 | 2 | 2 |
| Other** | 59 | 5 | 54 |
| N= | 201 | 19 | 182 |
Complications included venous thrombosis (e.g., DVT and PE), uncontrolled pain, fluid collections, abdominal hernia, and wound dehiscence.
Reasons in this category included: removal of a pituitary adenoma, chest pain, neuropathic pain, and autonomic dysfunction.
Preventability of Rehospitalization
Reviewers agreed on the assessment of preventability in 85% of cases (kappa=−0.06, p=0.84) based on previously used criteria (17). Rehospitalizations that met criteria for preventability were rare (n=19 cases), representing 9% of all unplanned rehospitalizations and 3% of the entire cohort.
Risk Factors for Early Rehospitalization
As shown in Table 2, in univariate analysis, rehospitalized patients were more likely to have had longer median time on the waiting list prior to KT (1.75 vs. 1.5 years, p=0.015), to have received deceased donor kidneys (72% vs. 64%, p=0.036), to have delayed graft function (23% vs. 16% p=0.039) and to have experienced longer initial length of stay (median 4.8 vs. 4.0 days, p = 0.03). Discharge from KT on a weekend (30% vs. 23%, p=0.037) was also associated with early rehospitalization, but a number of other process-of-care variables including discharge on insulin, discharge on narcotics, and the total number of discharge medications were not associated with the outcome.
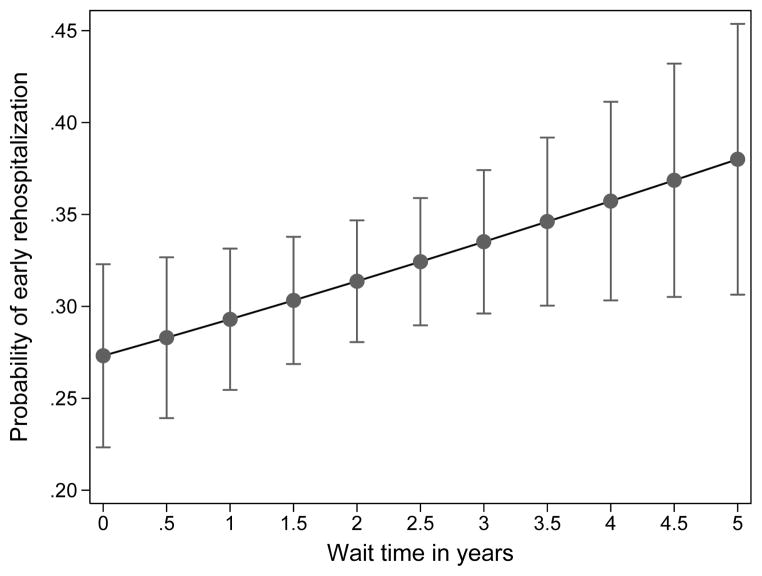
As shown in Table 4, in multivariable logistic regression, time on the waitlist (OR 1.10 per additional year [1.00–1.21], p=0.04), weekend discharge (OR 1.59 [1.12–2.28], p=0.01), and long initial length of stay defined as >4.5 days (OR 1.42 [1.02–1.98], p=0.03) were independently associated with early rehospitalization. The addition of recipient demographics including age, race, and sex increased (worsened) the AIC and these variables were not statistically significant in our final model. The dose-response relationship between additional years on the waiting list and early rehospitalization is illustrated in Figure 3.
Table 4.
Results of Multivariable Logistic Regression for the Outcome of Early Rehospitalization
| Demographics | Final Model | Model + | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Wait Time (per additional year) | 1.10 | [1.00,1.21] | 0.041 | 1.12 | [1.01,1.23] | 0.031 |
| Weekend Discharge | 1.59 | [1.12,2.28] | 0.01 | 1.63 | [1.13,2.33] | 0.008 |
| Long LOS ( > 4.5 days) | 1.42 | [1.02,1.98] | 0.034 | 1.46 | [1.05,2.04] | 0.024 |
| Age | ||||||
| 18–40 | -ref- | |||||
| 41–55 | 1.12 | [0.74,1.68] | 0.619 | |||
| >55 | 0.93 | [0.62,1.41] | 0.731 | |||
| African American | 0.86 | [0.61,1.22] | 0.383 | |||
| Male | 0.83 | [0.60,1.15] | 0.263 | |||
|
| ||||||
| N | 753 | 753 | ||||
| AIC | 930.00 | 934.89 | ||||
Abbreviations: OR—Odds Ratio; CI—Confidence Interval; LOS—Length of Stay; AIC—Akaike Information Criterion
Figure 3.
Increasing Probability of Early Rehospitalization with Longer Waitlist Time (with 95% CIs)
Rehospitalization and the Outcomes of Mortality and Graft Failure
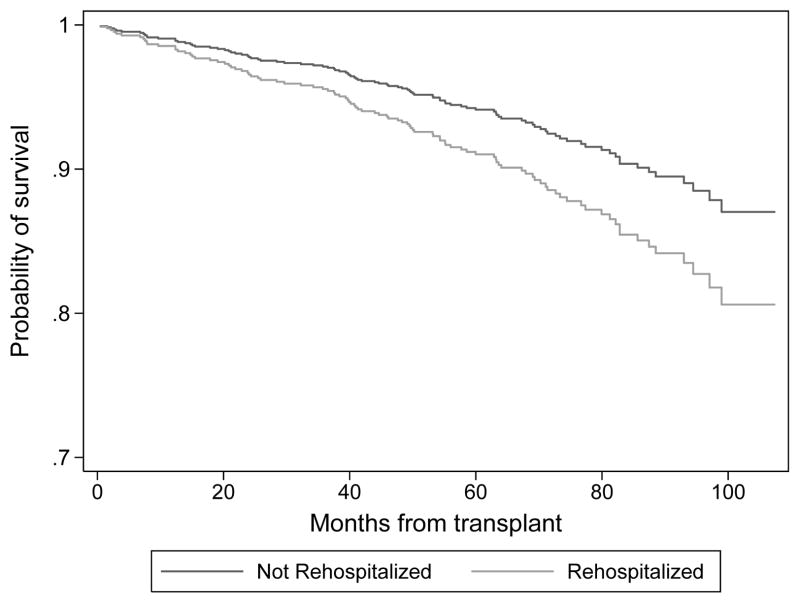
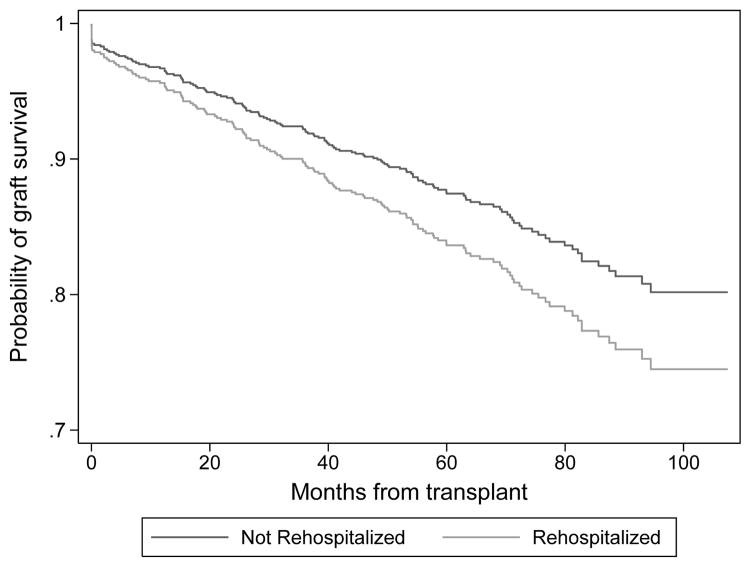
As shown in Figures 1 and 2, early rehospitalization was associated with mortality (HR 1.55 [1.04–2.33], p=0.03) but not with all-cause graft loss (HR 1.33 [0.95–1.85], p=.09). The final multivariable Cox model for mortality (see Table 5) included recipient age, sex, waitlist time in years, delayed graft function, recipient hepatitis C status, and early rehospitalization.
Figure 1.
Multivariable Adjusted Patient Survival by Early Rehospitalization Status
Figure 2.
Multivariable Adjusted All-Cause Graft Loss by Early Rehospitalization Status
Table 5.
Results of Cox Proportional Regression Analysis for the Outcome of Mortality
| HR | 95% CI | p-value | |
|---|---|---|---|
| Recipient Age (years) | |||
| ≥18-≤40 | -ref- | ||
| >40-≤55 | 1.75 | [0.79,3.88] | 0.168 |
| >55 | 4.32 | [2.05,9.14] | < 0.0001 |
| Male | 1.51 | [0.94,2.42] | 0.084 |
| Wait Time (years) | 1.21 | [1.08,1.36] | 0.001 |
| DGF | 1.59 | [1.02,2.46] | 0.04 |
| HCV | 1.97 | [1.13,3.43] | 0.016 |
| ICU | 1.67 | [0.98,2.83] | 0.058 |
| Rehospitalization | 1.55 | [1.04,2.33] | 0.033 |
|
| |||
| N | 753 | ||
| AIC | 1175.97 | ||
Abbreviations: HR-Hazard Ratio; DGF—Delayed Graft Function; HCV—Recipient Hepatitis C Infection; ICU-Intensive Care Unit stay during transplantation
Table 6 shows the results of the final multivariable Cox model for the outcome of all-cause graft loss. Although early rehospitalization did not meet conventional criteria for statistical significance (HR 1.33; p=0.09), we included it in the model because this variable improved model fit by AIC criterion.
Table 6.
Results of Cox Proportional Regression Analysis for the Outcome of All-Cause Graft Loss
| HR | 95% CI | p-value | |
|---|---|---|---|
| Deceased Donor | 1.95 | [1.25,3.03] | 0.003 |
| Longer LOS | 1.91 | [1.35,2.72] | < 0.0001 |
| Age (years) | |||
| ≥18-≤40 | -ref- | ||
| >40-≤55 | 0.69 | [0.42,1.12] | 0.149 |
| >55 | 1.29 | [0.83,2.02] | 0.249 |
| HCV | 2.31 | [1.47,3.62] | < 0.0001 |
| Discharge Medications (N) | |||
| 0–10 | -ref- | ||
| 11–14 | 0.46 | [0.27,0.76] | 0.002 |
| ≥15 | 0.52 | [0.30,0.90] | 0.019 |
| Rehospitalization | 1.33 | [0.95,1.85] | 0.095 |
|
| |||
| N | 753 | ||
| AIC | 1825.35 | ||
Abbreviations: HR-Hazard Ratio; LOS—Length of Stay during transplant hospitalization; HCV—Recipient Hepatitis C Infection
In a post-hoc analysis, we also investigated predictors of experiencing multiple early rehospitalizations. KT recipients were first categorized as having zero, one, or >1 early rehospitalizations. We estimated a multinomial logistic regression model using no rehospitalizations as the reference category. As the goal of this analysis was explanatory, all covariates associated with rehospitalization (Table 2) were included in this etiologic model. We found that weekend discharge was associated with a single early rehospitalization (relative risk ratio [RRR] = 1.65, 95% CI: 1.12, 2.45, p = 0.012) and a longer initial length of stay was associated with two or more early rehospitalizations (RRR = 2.16, 95% CI: 1.12, 4.16, p = 0.021). None of the other variables associated with the outcome in univariate analyses were significantly associated with having one or multiple early rehospitalizations in the final model.
Discussion
In this study of KT recipients over a five-year period, early rehospitalization was a common event after transplantation, occurring in 32% of our cohort. This rate is consistent with previous studies of early rehospitalization events in the national KT patient population (1, 14). Expert physicians were able to identify that a majority (>90%) of these hospitalizations were unplanned, and to consistently adjudicate the diversity of reasons for these early rehospitalizations by careful chart review. However, only a minority (9%) of these events had evidence of preventability by our criteria (15, 17). While risk-adjustment models are currently implemented by Medicare to attempt to differentiate between rehospitalizations that result from high patient complexity and those that result from lapses in processes-of-care (8), our finding of a low rate of preventability suggests that early rehospitalization after KT may be problematic to implement as a quality-of-care metric.
Interestingly, KT recipients who were rehospitalized early had spent more time on the waiting list and had longer initial length of stay during KT. At our center, transplant candidates are evaluated on a yearly basis after being added to the waiting list and we request constant communication with outside providers for updates on the health status of the candidates. Our evaluation process includes social worker assessments in addition to physician evaluation, and candidates are required to stay current with requested testing including cardiac clearance and cancer screening as appropriate. Candidates who do not meet these requirements are inactivated on the waiting list and further evaluated or de-listed when necessary.
Furthermore, patients who were discharged on a weekend day were more likely to be rehospitalized within 30 days. Per center protocol during the study period, once recipients were discharged from KT they were routinely seen by transplant clinicians including surgeons, nephrologists, and nurse practitioners on Monday mornings for weekly follow-up appointments, with laboratory assessments occurring at least twice weekly in the first post-transplant month. Each recipient was also assigned to a transplant coordinator, with on-call coordinators available after hours and on the weekends. All coordinator communications were charted in the electronic medical record. Therefore, given that patients discharged on the weekend typically had the shortest time to first outpatient follow-up after KT, our finding that these recipients were more likely to experience early rehospitalization suggests that the weekend may represent a period of time when patients may be especially vulnerable to changes in health provider staffing that impact their transitions of care (26). If further multicenter studies confirm these findings, transplant centers may consider augmenting staffing and the oversight related to weekend discharges. Interestingly, advanced recipient age, considered a risk factor for other adverse outcomes following KT (27–29), was not associated with early rehospitalization.
Our expert physicians strongly agreed on reasons for early rehospitalization, as measured by the kappa statistic. We determined that, in addition to primary graft dysfunction, post-operative complications (including pain, bleeding, and systemic thrombosis) and intravascular volume shifts are major causes of early rehospitalization. Our finding that infections are also an important reason for early rehospitalization is consistent with previous findings that KT recipients have a cumulative incidence of infections of >75% by one year after transplantation, with the highest risk in the immediate post-operative period (30). The diversity of reasons for rehospitalization suggest that efforts to reduce rehospitalization rates after KT should not focus on any single cause, but instead should address common pathways that lead to vulnerability during transitions-of-care (e.g., standardizing communication between providers, reducing time between follow up visits, and improving patient education).
Adjudicating preventability of rehospitalization has proven a challenge in previous studies of general medicine patients (31) and is not feasibly achieved using claims data alone. Using detailed chart review and an instrument with many choices for the reason for rehospitalization, our reviewers agreed strongly on reasons for rehospitalization (kappa=0.68). Reviewers also agreed on the preventability of rehospitalization in 85% of cases. However, the discrimination of the kappa statistic is in part dependent on the number of choices raters are offered, and in our study, we offered only two categories of preventability (preventable or not). Also, because preventable rehospitalizations were rare events, the expected proportion of agreement was very high. The resulting kappa statistic indicated that the reviewers did not agree to a greater extent than predicted by chance alone. These results highlight the challenges of adjudicating preventability, and by extension rehospitalization, as a quality-of-care metric in KT recipients using only a retrospective approach, particularly given the diversity of reasons for rehospitalization. We acknowledge that our finding that only 9% of early rehospitalizations were preventable represents a conservative estimate because physician reviewers’ assessments were limited by the variable quality and detail of clinical documentation. Notably, our method of determining preventability required that the physician adjudicator be able to identify a specific reason (e.g. a deficit in a process of care) why the rehospitalization event could have been prevented. Likely due to differences in methodology, our results contrast with the study by Goldfield et al. using claims data that over 20% of rehospitalizations following KT were potentially preventable (15). Prospective studies are needed to fully explore this area.
In our study, early rehospitalization was associated with mortality but not with all-cause graft loss. Our findings suggest that early rehospitalization may signal unmeasured or unobserved recipient vulnerabilities, such as frailty, that independent of age and allograft quality are associated with mortality. Early rehospitalization could also act as a surrogate measure for factors that are otherwise difficult for clinicians to measure, such as severity of vascular disease (22), socioeconomic status, access to care, level of frailty or limited health literacy (23). These results are also consistent with previous studies in general medicine populations that have identified patient comorbidities, previous health care utilization, and initial hospitalization acuity as strong predictors of 30-day rehospitalization (24, 25). Patients identified as vulnerable from early rehospitalization events may benefit from additional or different forms of monitoring (e.g., more frequent outpatient appointments, phone calls, laboratory checks).
This study has several limitations. A substantial limitation is the generalizability of these single-center results. While our institution’s rehospitalization rate is similar to national rates (1), a recent study did suggest that there is considerable variability in these rates between centers, possibly representing differences in quality of processes-of-care (14). We compared our center to the national cohort of KT recipients and found that distributions of recipient age, gender, race, and donor type were comparable. However, we acknowledge that just as the causes of early rehospitalization are diverse, the measures that will most improve outcomes may be equally diverse between transplant centers. Our center has identified a low rate of preventability based on observable processes-of-care but our results should be validated at multiple transplant centers. Also, while our thorough chart review process enabled adjustment for an extensive list of known, important confounders, we acknowledge that unmeasured confounders or effect modifiers (e.g. level of education, frailty) could prove important in understanding risk factors for rehospitalization. For example, it is possible that in some cases, unmeasured confounders such as lack of social support may necessitate that recipients are discharged on the weekend. Furthermore, the retrospective nature of chart review only allows a limited assessment of the preventability of these rehospitalizations. Despite the fact that our reviewers agreed strongly on reasons for rehospitalization, reviewers only agreed on the preventability of rehospitalization in 85% of cases. It is possible that charted information that is necessary for physicians to ascertain concrete, preventable causes of rehospitalization was systematically missing, but if this were the case, this lack of charted details is a further argument that prospective multicenter studies are needed to completely ascertain systems-based reasons for these diverse events. Additionally, certain recipient risk factors previously found to be predictors of early rehospitalization (e.g., history of cancer, cerebral vascular disease, arrhythmia, and COPD) were not included in this analysis. Given the retrospective nature of the study, we also acknowledge the potential for information bias, though it should not pose a substantial problem for the ascertainment of the primary outcome of early rehospitalization. Most early rehospitalizations are extensively documented by the hospital system, and our single center study had the advantage of the convention that transplant recipients overwhelmingly return to their transplant centers for medical care in the immediate post-operative period. In addition, our KT recipients are instructed to maintain close contact with their transplant coordinators and physicians, which would certainly be expected in the case of rehospitalization in the 30 days after KT. With meticulous review of medical records including all transplant coordinator communications, we are confident in our ascertainment of early rehospitalization events.
Early rehospitalization is common following KT and these events are increasingly scrutinized as a potential quality-of-care indicator. Our rigorous chart review process has identified the diversity of causes for these events and suggests that a minority of these events were preventable. Our retrospective study is, to our knowledge, the first chart review of KT patients who have experienced early rehospitalization seeking to adjudicate preventability. Prospective multicenter studies with detailed recipient-level data are needed to further identify recipient factors and modifiable center-level factors that may potentially reduce the rate of rehospitalization in this vulnerable and unique patient population.
Supplementary Material
Supplementary Figure 1: Chart abstraction form to identify reason for early rehospitalization
Acknowledgments
MH is supported by training grants (5T32DK007006-38 and F32DK096758-01) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The data reported here have been supplied by the Minneapolis Medical Research Foundation (MMRF) as the contractor for the Scientific Registry of Transplant Recipients (SRTR). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government.
Abbreviations
- ADPKD
Autosomal Dominant Polycystic Kidney Disease
- AIC
Akaike Information Criterion
- CI
Confidence Interval
- CMV
Cytomegalovirus
- CVD
Cardiovascular Disease
- DGF
Delayed Graft Function
- ESRD
End Stage Renal Disease
- FSGS
Focal Segmental Glomerulosclerosis
- HR
Hazard Ratio
- HCV
Hepatitis C Virus
- ICU
Intensive Care Unit
- KT
Kidney transplantation
- LOS
Length of Stay
- OR
Odds Ratio
- SRTR
Scientific Registry of Transplant Recipients
- PPR
Potentially Preventable Rehospitalization
- RRR
Relative Risk Ratio
- US
United States
Footnotes
Disclosure
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Additional Supporting Information may be found in the online version of this article.
References
- 1.Englesbe MJ, Dimick JB, Fan Z, Baser O, Birkmeyer JD. Case mix, quality and high-cost kidney transplant patients. Am J Transplant. 2009;9(5):1108–1114. doi: 10.1111/j.1600-6143.2009.02592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martin RC, Brown R, Puffer L, Block S, Callender G, Quillo A, et al. Readmission rates after abdominal surgery: the role of surgeon, primary caregiver, home health, and subacute rehab. Annals of surgery. 2011;254(4):591–597. doi: 10.1097/sla.0b013e3182300a38. [DOI] [PubMed] [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Stone JHG. Service CR, editor. CRS Report for Congress. 2010. Medicare Hospital Readmissions: Issues, Policy Options and PPACA; pp. 1–37. [Google Scholar]
- 5.Epstein AM. Revisiting readmissions--changing the incentives for shared accountability. N Engl J Med. 2009;360(14):1457–1459. doi: 10.1056/NEJMe0901006. [DOI] [PubMed] [Google Scholar]
- 6.Vaduganathan M, Bonow RO, Gheorghiade M. Thirty-day readmissions: the clock is ticking. Jama. 2013;309(4):345–346. doi: 10.1001/jama.2012.205110. [DOI] [PubMed] [Google Scholar]
- 7.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. Jama. 2013;309(4):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 8.Services CfMM. Readmissions Reduction Program. 2012 [cited 2013 September 10]; Available from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- 9.Weinhandl ED, Snyder JJ, Israni AK, Kasiske BL. Effect of comorbidity adjustment on CMS criteria for kidney transplant center performance. Am J Transplant. 2009;9(3):506–516. doi: 10.1111/j.1600-6143.2008.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Axelrod DA, McCullough KP, Brewer ED, Becker BN, Segev DL, Rao PS. Kidney and pancreas transplantation in the United States, 1999–2008: the changing face of living donation. Am J Transplant. 2010;10(4 Pt 2):987–1002. doi: 10.1111/j.1600-6143.2010.03022.x. [DOI] [PubMed] [Google Scholar]
- 11.Huang E, Segev DL, Rabb H. Kidney transplantation in the elderly. Semin Nephrol. 2009;29(6):621–635. doi: 10.1016/j.semnephrol.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363(3):297–298. doi: 10.1056/NEJMc1001882. [DOI] [PubMed] [Google Scholar]
- 13.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 14.McAdams-Demarco MA, Grams ME, Hall EC, Coresh J, Segev DL. Early hospital readmission after kidney transplantation: patient and center-level associations. Am J Transplant. 2012;12(12):3283–3288. doi: 10.1111/j.1600-6143.2012.04285.x. [DOI] [PubMed] [Google Scholar]
- 15.Goldfield NI, McCullough EC, Hughes JS, Tang AM, Eastman B, Rawlins LK, et al. Identifying potentially preventable readmissions. Health care financing review. 2008;30(1):75–91. [PMC free article] [PubMed] [Google Scholar]
- 16.Nair MRL, Chiang C, Abt P, Huverserian A, Mussell A, Schaeffer G, Doll S, Reese P, Levine M. Categories and Predictors of Early Rehospitalization after Kidney Transplantation. American Journal of Transplantation. 2012;12(Supplement s3):27–542. [Google Scholar]
- 17.Oddone EZ, Weinberger M, Horner M, Mengel C, Goldstein F, Ginier P, et al. Classifying general medicine readmissions. Are they preventable? Veterans Affairs Cooperative Studies in Health Services Group on Primary Care and Hospital Readmissions. Journal of general internal medicine. 1996;11(10):597–607. doi: 10.1007/BF02599027. [DOI] [PubMed] [Google Scholar]
- 18.Greenwald JL, Jack BW. Preventing the preventable: reducing rehospitalizations through coordinated, patient-centered discharge processes. Professional case management. 2009;14(3):135–140. doi: 10.1097/NCM.0b013e318198d4e1. quiz 141–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hosmer DLS. Applied Logistic Regression. 2. New York, NY: John Wiley & Sons; 2004. [Google Scholar]
- 20.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. American journal of epidemiology. 1989;129(1):125–137. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- 21.AHRQ AfHRaQ. Chapter 3: Creation of New Race-Ethnicity Codes and SES Indicators for Medicare Beneficiaries. Chapter 3. Agency for Healthcare Research and Quality; Rockville, MD: Jan, 2008. http://www.ahrq.gov/research/findings/final-reports/medicareindicators/medicareindicators3.html. [Google Scholar]
- 22.Ramezani M, Ghoddousi K, Hashemi M, Khoddami-Vishte HR, Fatemi-Zadeh S, Saadat SH, et al. Diabetes as the cause of end-stage renal disease affects the pattern of post kidney transplant rehospitalizations. Transplant Proc. 2007;39(4):966–969. doi: 10.1016/j.transproceed.2007.03.074. [DOI] [PubMed] [Google Scholar]
- 23.Moghani Lankarani M, Noorbala MH, Assari S. Causes of re-hospitalization in different post kidney transplantation periods. Ann Transplant. 2009;14(4):14–19. [PubMed] [Google Scholar]
- 24.Zapatero A, Barba R, Marco J, Hinojosa J, Plaza S, Losa JE, et al. Predictive model of readmission to internal medicine wards. European journal of internal medicine. 2012;23(5):451–456. doi: 10.1016/j.ejim.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Marcantonio ER, McKean S, Goldfinger M, Kleefield S, Yurkofsky M, Brennan TA. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. The American journal of medicine. 1999;107(1):13–17. doi: 10.1016/s0002-9343(99)00159-x. [DOI] [PubMed] [Google Scholar]
- 26.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 27.Meier-Kriesche HU, Ojo A, Hanson J, Cibrik D, Lake K, Agodoa LY, et al. Increased immunosuppressive vulnerability in elderly renal transplant recipients. Transplantation. 2000;69(5):885–889. doi: 10.1097/00007890-200003150-00037. [DOI] [PubMed] [Google Scholar]
- 28.Martins PN, Pratschke J, Pascher A, Fritsche L, Frei U, Neuhaus P, et al. Age and immune response in organ transplantation. Transplantation. 2005;79(2):127–132. doi: 10.1097/01.tp.0000146258.79425.04. [DOI] [PubMed] [Google Scholar]
- 29.Meier-Kriesche HU, Ojo AO, Hanson JA, Kaplan B. Exponentially increased risk of infectious death in older renal transplant recipients. Kidney international. 2001;59(4):1539–1543. doi: 10.1046/j.1523-1755.2001.0590041539.x. [DOI] [PubMed] [Google Scholar]
- 30.Brennan DC, Daller JA, Lake KD, Cibrik D, Del Castillo D. Rabbit antithymocyte globulin versus basiliximab in renal transplantation. N Engl J Med. 2006;355(19):1967–1977. doi: 10.1056/NEJMoa060068. [DOI] [PubMed] [Google Scholar]
- 31.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2011;183(7):E391–402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: Chart abstraction form to identify reason for early rehospitalization