Abstract
Context
Varied nursing home quality improvement programs have been implemented over the last decade; their implications for racial disparities in quality are unknown.
Objective
To determine the longitudinal trend of racial disparities in pressure ulcer prevalence among long-term nursing home residents during 2003-2008, and whether persistent disparities are related to where residents received care.
Design
Using US nursing home resident assessment files, On-line Survey, Certification, and Reporting files, and Area Resource Files, we examined pressure ulcer rate for high-risk residents. We categorized nursing homes according to their proportions of black residents. We determined risk-adjusted racial disparities between and within sites of care, and the risk-adjusted odds of pressure ulcers for black and white residents receiving care in different facilities.
Setting and participants
Observational cohort of 2,136,764 white and 346,808 black residents in 12,473 certified nursing homes.
Main outcome measure
Risk-adjusted odds of pressure ulcers of stages 2 to 4.
Results
Overall pressure ulcer rates decreased over years but black residents showed persistently higher rates than white residents: 16.8% (95% confidence interval [CI] 16.6-17.0%) vs 11.4% (95% CI 11.3-11.5%) in 2003, and 14.6% (95% CI 14.4-14.8%) vs 9.6% (95% CI 9.5-9.7%) in 2008 (p>0.05 for trend of disparities). Both black (unadjusted rate 15.5% in 2008; adjusted odds ratio [OR]=1.59, 95% confidence interval [CI] 1.52-1.67) and white (unadjusted rate 12.1%; adjusted OR=1.33, 95% CI 1.26-1.40) residents in nursing homes with the highest concentrations of black residents (≥35%) showed higher risk of pressure ulcers than white residents (unadjusted rate 8.8%) in nursing homes serving essentially white residents (black residents<5%).
Conclusions
From 2003 to 2008, the prevalence of pressure ulcers among high-risk nursing home residents was higher in black residents that in white residents. This disparity was in part related to the site of nursing home care.
Keywords: pressure ulcer, racial disparity, nursing home, long-term care, trend
INTRODUCTION
Pressure ulcers are a common health problem among nursing home residents that increases morbidity, mortality, and costs of care substantially1,2. Racial disparities in pressure ulcer prevalence are well documented in nursing homes3-6. To achieve the national priority of reducing and eliminating healthcare disparities7, it is imperative to understand the reasons underpinning such disparities. Previous studies suggest that a disproportionate share of minority residents reside in a small number of nursing homes with limited clinical and financial resources8,9. Therefore, site of care may play an important role and the higher pressure ulcer rate in black residents may be because of their receiving care at lowest-quality nursing homes in addition to race itself.
Since late 2002, national nursing home quality improvement and public-reporting programs have been launched10-12. During similar period of time, varied state13,14 and local5,15 initiatives have also been implemented. These programs aimed to improve overall quality including reducing pressure ulcers, but focused little attention to widespread racial disparities. Therefore, they may have no effect on reducing disparities despite overall improvement over time. Prior research focuses on overall improvements shortly after program implementations or the documentation of cross-sectional disparities, shedding little light on the longitudinal trend of disparities.
This study analyzed the trend of pressure ulcer prevalence in nursing homes by race and site of care during 2003-2008. We further sought to determine whether disparities are primarily related to race or the race-mix of the nursing home where resident care is delivered, and whether site-of-care disparities are associated with nursing home managerial, financial, and geographic features.
METHODS
Study sample
We used the 2003-2008 nursing home Minimum Data Set (MDS) files to identify long-term care residents, and their pressure ulcer rate was calculated annually using similar methodology developed by the Centers for Medicare and Medicaid Services (CMS) for publicly released quality measures16. The MDS is a nationally mandated tool for patient assessment and care planning in all nursing homes certified by the CMS17. Over 90% of nursing homes in the US are so certified18. For long-term care residents, full MDS assessments are performed at admission, annually thereafter, and when a significant change of health status occurs, while abbreviated assessments are performed on a quarterly basis. MDS diagnostic, functional, and other common assessments are shown to be of high validity and internal consistency for research purposes19-21. Specifically, a multistate study confirms the validity and inter-rater reliability (weighted kappa>0.8) of the MDS pressure ulcer assessments20. [Au: what specifically is the validity of the pressure ulcer measure?]
We analyzed the annual and “significant change” full assessments which contain over 350 items related to each resident's demographics, physical and mental health status, and disease diagnoses. Race and ethnicity was identified at admission by nursing home staff and was categorized as non-Hispanic white, Black, Hispanic, Asian/Pacific islander, or American Indian/Alaskan native. We confirmed that targeted residents had one or more prior quarterly assessments, i.e., they had stayed in the nursing home for at least 90 days.
Residents were included in the study if they (1) required extensive assistance or were totally dependent on staff assistance with bed mobility or moving between surfaces; (2) were in coma; or (3) had malnutrition (ICD-9-CM codes 260-262, 263.0-263.2, 263.8, or 263.9). These residents are believed to be at high risk for developing pressure ulcers16, and cross-sectional racial disparities were reported in previous studies. Pressure ulcers of any stage (stages 1 to 4) for these residents were determined by nurse assessment or physician diagnosis (ICD-9-CM codes 707.21 to 707.24 for stages 1 to 4, respectively). For the purpose of analyzing racial disparities, we retained only non-Hispanic white and Black residents in analyses, and excluded the small number (<6%) of residents of other race/ethnicity.
Variables
Our primary outcome was whether the resident had pressure ulcer of stage 2 or higher in each year. The unit of analysis was the resident-year or each assessment. The independent variables were race (white or black) and type of nursing homes in terms of racial composition. For each nursing home, we calculated the proportion of all its long-term care residents who are black and performed preliminary analyses on its association with pressure ulcer rate. We then categorized facilities into 4 groups: nursing homes with high concentration of Blacks (black residents ≥35%), medium-high concentration of Blacks (black residents 15-34.9%), medium concentration of Blacks (black residents 5-14.9%), and low concentration of Blacks (black residents <5%). In sensitivity analyses we examined alternative cutoff points for categorization; the results were similar and thus are not presented here.
Resident characteristics that were potentially associated with the risk of developing pressure ulcers were selected a priori3,4,6,22-24. These characteristics included age, sex, difficulties in activities of daily living (ADL), cognitive performance scale (CPS), and the presence or absence of dementia (Alzheimer's disease or other types of dementia), stroke, diabetes, other endocrine disease, cardiovascular disease, musculoskeletal disease, cancer, malnutrition, incontinence (frequent or complete bowel or bladder incontinence), antipsychotic drug use, daily physical restraint use, one or more hospital admissions during past 90 days, or being in end stage (6 months or less) of life. Age was categorized as <65 years, 65-74 years, 75-84 years, and ≥85 years. ADLs included bed mobility, transfer, dressing, eating, toilet use, personal hygiene, and bathing; each ADL item was coded as 0 if the resident was independent or needed staff supervision or limited assistance, and 1 if the resident needed extensive staff assistance or in total dependence. The total range of the aggregate ADL score was between 0 and 7. The CPS was defined using a validated MDS algorithm developed by Morris and colleagues25, which ranges from 0 (cognitively intact) to 6 (very severely impaired in cognition).
We obtained nursing home characteristics from the On-line Survey, Certification, and Reporting (OSCAR) file in each year of 2003-08. The OSCAR is a facility-level database maintained and updated by CMS for annual recertification and public reporting purposes. Facility characteristics included total number of beds, profit status (categorized as for-profit, non-for-profit, or government), chain affiliation (yes/no), a measure of facility financial capability based on percentage of Medicaid-reimbursed residents, registered nurse (RN) hours per resident day, licensed practical or vocational nurse (LPN/LVN) hours per resident day, certified nurse assistance (CNA) hours per resident day, and numbers of total and healthcare-related deficiency citations issued by state regulators during annual inspections26.
Lastly, we used the Area Resource Files of corresponding years to characterize the county where each nursing home is located8. County characteristics included the percentage of elderly population ( ≥ 65 years), a measure of the degree to which each nursing home competes for long-term care patients with all other nursing homes in the county27, and urban versus rural location.
Analysis
We compared racial differences in demographic and clinical factors over the full study period and stratified by 2-year intervals (2003-2004, 2005-2006, and 2007-2008). Bivariate generalized estimating equations28 with binomial distribution and logit link function for race were used for analyses of categorical variables and bivariate linear mixed models were used for continuous variables; models accounted for the repeated assessments of patients over years. We performed similar analyses for the trend of pressure ulcer rate according to race and to race by nursing home categories. Nursing home and county characteristics were compared by nursing home categories using chi-square tests or analyses of variance as appropriate.
We fit multivariate patient-level linear models to compute three types of risk-adjusted racial disparity in pressure ulcer prevalence: overall disparity, the disparity due to residents being cared for in different nursing homes (between sites of care), and the disparity among black and white residents in the same nursing home (within a site of care). For each year, we first fit a model that had race as the independent variable and adjusted for the aforementioned patient characteristics to estimate overall risk-adjusted disparity. We then fit another model that further adjusted for the fixed effects of nursing homes to estimate the within-site disparity29. The between-site disparity was calculated as the difference of the two estimates.
We further categorized all residents into 8 categories according to race and site of care: black residents in facilities with high concentration of blacks, white residents in facilities with high concentration of blacks; black residents in facilities with medium-high concentration of blacks, white residents in facilities with medium-high concentration of blacks; black residents in facilities with medium concentration of blacks, white residents in facilities with medium concentration of blacks; black residents in facilities with low concentration of blacks, and white residents in facilities with low concentration of blacks. For each year, we fit a set of logistic regression models that determined the relationship between these groups and the odds of having pressure ulcers, using white residents in nursing homes with low concentration of blacks as the reference group.
These models sequentially adjusted for the clustering of residents in nursing homes using random effects (model 1); age and gender (model 2); other patient characteristics described above (model 3); nursing home characteristics (model 4); and county characteristics and state indicators (model 5). All models were estimated through the GEE approach28 that assumed a binomial distribution and logit link function for the outcome, and incorporated an exchangeable correlation structure of error terms. All models were checked to confirm that collinearity or over-fitting was not an issue. We also tested interactions between the key independent variables and age, gender, difficulties in ADL, and CPS score, but did not find significant interactive effects. The small number of observations with missing values (<3% in general) were not included in multivariate models.
Sensitivity Analyses
We performed a number of sensitivity analyses. In particular, our primary analyses focused on pressure ulcers at stage 2 or higher due to the concern that stage 1 pressure ulcers are more likely to be under-diagnosed in black residents than in white residents. To confirm the robustness of our analyses, we redefined the outcome as whether a resident had pressure ulcers at any stage and performed similar analyses on racial and site-of-care disparities. We further added back excluded minority residents, and re-categorized nursing homes using the percentage of all nonwhite (not just black) long-term residents and determined the associations of minority race/ethnicity and site of care with the odds of pressure ulcers.
Statistical analyses were performed using SAS software version 9.2 (SAS Institute Inc, Cary, North Carolina) and Stata version 8 (Stata Corp, College Station, Texas). All statistical tests were two-tailed with p<.05 considered to be significant. This study was approved by the Institutional Review Board (IRB) of University of Iowa and the IRB of University of California, Irvine; patient informed consent was waived by both IRBs.
RESULTS
Our sample included 2,136,764 white and 346,808 Black long-term care residents over the period of 2003-2008 who were considered at high risk of having pressure ulcers. They represented a total of 4,341,905 and 704,713 assessments, respectively. During 2003-2008, 49% of residents had one annual assessment, 24% had two assessments, and 27% had between three and six assessments. Our unit of analysis was each assessment. Of white residents, 10.5% (n=455,611 assessments) had pressure ulcers of stage 2 or higher; and of Black residents, 15.9% (n=111,981 assessments) had pressure ulcers of stage 2 or higher, resulting in an overall unadjusted racial difference of 5.4% (95% confidence interval [CI] 5.38-5.42%, p<.001). Among white and black residents, respectively, the rates for stage 1 pressure ulcers were 2.1% and 1.2%, 6.6% and 7.7% for stage 2 pressure ulcers, 1.5% and 2.7% for stage 3 pressure ulcers, and 2.4% and 5.5% for stage 4 pressure ulcers.
The pressure ulcer rate for other white and black long-term residents who were not considered at high risk (a total of 3,773,652 assessments) remained low. Compared to high-risk residents, these low-risk residents tended to be younger and have better physical and cognitive functional performance. Their overall pressure ulcer rates decreased slightly over years (p<0.01 for trend) but did not show clinically significant racial differences: for white and Black residents respectively, the prevalence rates were 2.9% and 2.4% in 2003, 2.8% and 2.4% in 2004, 2.7% and 2.2% in 2005, 2.6% and 2.3% in 2006, 2.4% and 2.0% in 2007, and 2.2% and 1.8% in 2008. The slightly lower rate for low-risk black residents may be partially caused by under-identification of pressure ulcers among patients with darkly-pigmented skin4.
Compared to white residents at high risk, Black residents at high risk were an average of 6 years younger (76 versus 82 years) and more likely to be male (33% versus 26%, Table 1). Black residents were more likely to have stroke and diabetes, less likely to have dementia and musculoskeletal disease, and equally likely to have cardiovascular disease. For both whites and Blacks, the prevalence rates of diabetes increased over years (p<.001), while the rates of dementia and musculoskeletal disease showed decreasing trends (p<.001).
Table 1.
Characteristics of long-term care nursing home residents at high risk for pressure ulcers, 2003-2008
| 2003 - 2004 | 2005 - 2006 | 2007 - 2008 | ||||
|---|---|---|---|---|---|---|
| Characteristic | Blacka | White | Blacka | White | Blacka | White |
| Number of resident assessments | 224,791 | 1,426,678 | 235,961 | 1,454,437 | 243,961 | 1,460,790 |
| Age, y, mean±SD | 76.6±15.7 | 82.3±12.6 | 76.2±15.6 | 82.3±12.5 | 76.0±15.6 | 82.4±12.5 |
| Male gender, number (%) | 71839 (32.0) | 360046 (25.2) | 77712 (32.9) | 374464 (25.8) | 82301 (32.7) | 383293 (26.2) |
| Difficulties in activities of daily living, median (IQR) | 6 (6-7) | 6 (6-7) | 6 (6-7) | 6 (6-7) | 6 (6-7) | 6 (6-7) |
| Cognitive performance score, median (IQR) | 3 (2-6) | 3 (2-5) | 3 (2-5) | 3 (2-5) | 3 (2-5) | 3 (2-5) |
| Disease diagnosis, number (%) | ||||||
| Dementia | 38439 (17.1) | 305309 (21.4) | 36810 (15.6) | 286524 (19.7) | 36350 (14.9) | 273168 (18.7) |
| Stroke | 71708 (31.9) | 291042 (20.4) | 74328 (31.5) | 282161 (19.4) | 75140 (30.8) | 267325 (18.3) |
| Diabetes | 71042 (31.6) | 277257 (19.4) | 80819 (34.3) | 309351 (21.3) | 87935 (36.0) | 333057 (22.8) |
| Other endocrine disease | 6601 (2.9) | 107536 (7.5) | 6703 (2.8) | 106951 (7.4) | 6708 (2.8) | 107591 (7.4) |
| Cardiovascular disease | 66428 (29.6) | 425336 (29.8) | 69685 (29.5) | 434352 (29.9) | 71797 (29.4) | 435192 (29.8) |
| Musculoskeletal disease | 32092 (14.3) | 300125 (21.0) | 30243 (12.8) | 281607 (19.4) | 29196 (12.0) | 270597 (18.5) |
| Cancer | 5170 (2.3) | 42800 (3.0) | 5191 (2.2) | 39270 (2.7) | 4879 (2.0) | 36520 (2.5) |
| Malnutrition, number (%) | 26525 (11.8) | 186895 (13.1) | 27371 (11.6) | 184713 (12.7) | 27080(11.1) | 178216(12.2) |
| Incontinence, number (%) | 199390 (88.7) | 1194129 (83.7) | 208118 (88.2) | 1199911 (82.5) | 213466 (87.5) | 1194926 (81.8) |
| Antipsychotic drug use, number (%) | 47880 (21.3) | 372363 (26.1) | 51204 (21.7) | 385426 (26.5) | 52452 (21.5) | 373962 (25.6) |
| Physical restraint, number (%) | 22254 (9.9) | 164068(11.5) | 19585 (8.3) | 135263 (9.3) | 14638 (6.0) | 97873 (6.7) |
| Hospital admission during the past 90 days, number (%) | 71259 (31.7) | 516457 (36.2) | 67957 (28.8) | 477055 (32.8) | 66845 (27.4) | 452845 (31.0) |
| In end stage of life (<6 mo.), number (%) | 5170 (2.3) | 59920 (4.2) | 6135 (2.6) | 65450 (4.5) | 6343 (2.6) | 71579 (4.9) |
SD=standard deviation; IQR=interquartile rage.
P<.001 for all comparisons to white patients except for cardiovascular disease where p<.05.
Persistent racial disparities
The pressure ulcer (stage 2 or higher) rate among Black residents decreased from 16.8% (95% CI 16.6%-17.0%) in 2003 to 14.6% (95% CI 14.4%-14.8%) in 2008 (Table 2, p<.001 for trend); and the rate among white residents decreased from 11.4% (95% CI 11.3%-11.5%) in 2003 to 9.6% (95% CI 9.5%-9.7%) in 2008 (p<.001 for trend). Despite the lowered rates over time for both races, racial disparity remained relatively unchanged: the unadjusted disparities were 5.4% (95% CI 5.3%-5.5%) in 2003 and 5.0% (95% CI 4.9%-5.1%) in 2008 (p>.05 for trend), and the overall risk-adjusted disparities were 4.5% (95% CI 4.3-4.7%) in 2003 and 3.9% (95% CI 3.6-4.1%) in 2008 (Table 2).
Table 2.
Pressure ulcer (stage 2 or higher) rates and racial disparities for high-risk nursing home residents, 2003-2008
| No. of residents | Unadjusted rate (95% CI), % | Risk adjusted racial disparity (95% CI), % | Percent overall risk- adjusted disparity due to sites of care (7)=(6)/(4) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Year | Black | White | Black resident (1) | White resident (2) | Disparity (3)=(1)-(2) | Overalla (4) | Within site of careb(5) | Between sites of care (6)=(4)-(5) | |
| 2003 | 110,935 | 713,872 | 16.8 (16.6-17.0) | 11.4 (11.3-11.5) | 5.4 (5.3-5.5) | 4.5 (4.3-4.7) | 2.0 (1.7-2.3) | 2.5 (2.2-2.8) | 56% |
| 2004 | 113,856 | 712,806 | 16.7 (16.5-16.9) | 11.2 (11.1-11.3) | 5.5 (5.4-5.6) | 4.4 (4.2-4.6) | 2.1 (1.8-2.4) | 2.3 (2.0-2.6) | 52% |
| 2005 | 116,552 | 722,697 | 16.2 (16.0-16.4) | 10.7 (10.6-10.8) | 5.5 (5.4-5.6) | 4.3 (4.1-4.6) | 1.9 (1.7-2.2) | 2.4 (2.1-2.7) | 56% |
| 2006 | 119,409 | 731,740 | 15.9 (15.7-16.1) | 10.2 (10.1-10.3) | 5.7 (5.6-5.8) | 4.5 (4.3-4.7) | 2.2 (1.9-2.4) | 2.3 (2.0-2.6) | 51% |
| 2007 | 120,569 | 731,245 | 15.3 (15.1-15.5) | 9.9 (9.8-10.0) | 5.4 (5.3-5.5) | 4.2 (4.0-4.4) | 2.0 (1.8-2.3) | 2.2 (1.9-2.5) | 52% |
| 2008 | 123,392 | 729,545 | 14.6 (14.4-14.8) | 9.6 (9.5-9.7) | 5.0 (4.9-5.1) | 3.9 (3.6-4.1) | 1.8 (1.5-2.0) | 2.1 (1.8-2.4) | 54% |
CI=confidence interval.
Overall risk-adjusted disparity derived from a patient-level linear model of pressure ulcer status that had race as the independent variable and adjusted for age, gender, difficulties in activities of daily living, cognitive performance scale, disease diagnoses (dementia, stroke, diabetes, other endocrine disease, cardiovascular disease, musculoskeletal disease, and cancer), and whether the resident was in malnutrition, incontinence, antipsychotic drug use, physical restraint use, end stage of life, or had hospital admissions during the past 90 days.
Within-site disparity derived from a similar model that further adjusted for the fixed effects of nursing homes.
Site of care associations
Table 2 also shows that for each year, more than half of the risk-adjusted disparity in pressure ulcer rates between blacks and whites was found between sites, rather than within sites, of care. Table 3 shows that facilities with higher concentration of black residents tended to have lower staffing levels of registered nurse and certified nurse assistance, and to be larger, for-profit, and urban facilities. These facilities may be more financially disadvantaged when caring for predominately Medicaid patients.
Table 3.
Nursing home and county characteristics by type of nursing homes, 2008
| Nursing homes with concentration of black residents that isa | ||||
|---|---|---|---|---|
| Low (<5%) | Medium (5-14.9%) | Medium-high (15-34.9%) | High (>35%) | |
| Nursing home characteristic | ||||
| Number of nursing homes Black residents, mean | 7,231 | 2,322 | 1,603 | 1,317 |
| (median, IQR), % | 1.0(0, 0-1.8) | 9.1(8.6, 6.7-11.3) | 23.1 (22.2, 18.1-27.4) | 56.1 (51.3, 42.4-66.2) |
| Number of beds, mean, (median, IQR) Profit status, number (%) | 100 (94, 60-120) | 124 (118, 88-148) | 130 (120, 91-152) | 137 (120, 95-161) |
| For-profit | 4,363 (60.3) | 1,836 (79.1) | 1,306 (81.3) | 1,032 (78.5) |
| Non-for-profit | 2,332 (32.3) | 394 (17.0) | 238 (14.8) | 207 (15.8) |
| Government | 536 (7.4) | 92 (4.0) | 62 (3.9) | 75 (5.7) |
| Chain affiliated, number (%) | 3,750 (51.9) | 1,381 (59.5) | 996 (62.0) | 766 (58.3) |
| Medicaid residents, mean (median, IQR), % | 57.4 (60.7, 47.5-71.2) | 65.1 (67.1, 56.5-76.1) | 70.6 (72.1, 62.8-80.9) | 77.0 (78.6, 70.9-85.8) |
| RN hours per resident day, mean (median, IQR) | 0.6 (0.6, 0.4-0.8) | 0.5 (0.5, 0.4-0.6) | 0.5 (0.5, 0.3-0.6) | 0.5 (0.4, 0.3-0.6) |
| LPN/LVN hours per resident day, mean (median, IQR) | 0.8 (0.8, 0.6-0.9) | 0.8 (0.8, 0.7-1.0) | 0.9 (0.9, 0.7-1.0) | 0.9 (0.9, 0.7-1.0) |
| CNA hours per resident day, mean (median, IQR) | 2.4 (2.4, 2.1-2.8) | 2.4 (2.3, 2.0-2.7) | 2.3 (2.2, 2.0-2.6) | 2.2 (2.2, 1.9-2.5) |
| Number of government-issued deficiency citations, mean (median, IQR), % Total | 11 (10, 6-15) | 12 (11, 6-16) | 12 (11, 6-16) | 13 (11, 7-17) |
| Health care related | 7 (5, 3-9) | 8 (7, 3-11) | 8 (6, 3-11) | 8 (7, 4-11) |
| County characteristic b | ||||
| Competition of nursing home care, mean (median, IQR) | 0.7 (0.8, 0.7-0.9) | 0.8 (0.9, 0.8-1.0) | 0.8 (0.9, 0.7-1.0) | 0.8 (0.9, 0.7-1.0) |
| Population>65 years, mean (median, IQR), % | 14.6 (14.1, 11.8-16.7) | 13.3 (12.7, 10.7-14.8) | 12.9 (12.6, 10.6-14.4) | 12.5 (12.2, 10.7-13.9) |
| Urban area | 4,339 (60.0) | 1,880 (81.0) | 1,262 (78.6) | 1,037 (78.9) |
IQR=inter-quartile range; RN=registered nurse; LPN=licensed practical nurse; LVN=licensed vocational nurse; CNA=certified nurse assistance.
P<.001 for comparisons of all characteristics across nursing home group (chi-square tests for categorical variables and analyses of variance for continuous variables).
Unite of analysis is each nursing home in the county.
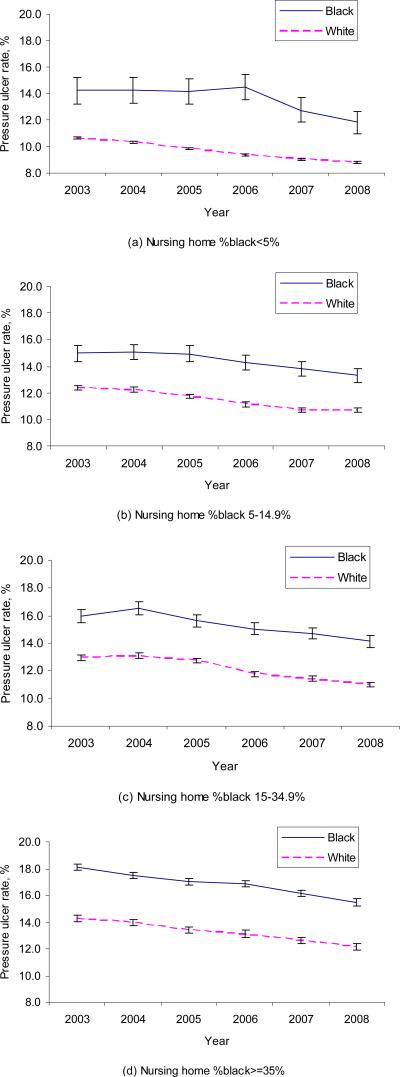
Figure 1 shows that despite the improved pressure ulcer prevalence for each racial and site group, both racial and site-of-care disparities persisted over years. For example, black residents in facilities with highest concentration of blacks had the highest pressure ulcer rate (15.5% in 2008), which was about 7% higher than the rate for white residents in facilities with lowest concentration of blacks (8.8% in 2008), which was the lowest among all groups.
Figure 1.
Pressure ulcer (stage 2+) rate by race and nursing home type (error bars indicate 95% confidence intervals)
Multivariate analyses of 2008 (Table 4) confirmed these disparities: compared with white residents in “essentially white” facilities, the odds ratio was 1.59 (95% CI 1.52-1.67) for black residents in facilities with highest black concentrations. The associations were reduced but largely persisted after adjusting for age, sex and other patient characteristics; further adjusting for nursing home or county and state covariates had minor effects on the associations. Results of multivariate analyses of other years were similar. In a re-estimated model that adjusted for all resident, nursing home, county and state covariates but included facility groups and race as separate variables, the “main effects” of site of care were as follows: compared with nursing homes with low concentration of black residents, the OR was 1.15 (95% CI 1.12-1.19) for facilities with medium concentration of Blacks, 1.20 (95% CI 1.15-1.24) for facilities with medium-high concentration of Blacks, and 1.33 (95% CI 1.28-1.40) for facilities with high concentration of Blacks.
Table 4.
Risk-adjusted odds of pressure ulcers (stage 2+), grouped by race and site of carea, 2008
| No. of residents | Unadjusted rate (95% CI), % | Odds ratio (95% confidence interval)b | |||||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||
| Nursing homes with low concentration of blacks (<5%) | |||||||
| White | 389,150 | 8.8 (8.7-8.9) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Black | 5,395 | 11.8(10.9-12.7) | 1.33 (1.21-1.45) | 1.25 (1.14-1.36) | 1.20 (1.09-1.31) | 1.17 (1.07-1.28) | 1.14 (1.05-1.25)c |
| Nursing homes with medium concentration of blacks (5-14.9%) | |||||||
| White | 128,563 | 10.7 (10.5-10.9) | 1.26 (1.23-1.30) | 1.25 (1.21-1.29) | 1.22 (1.19-1.26) | 1.21 (1.17-1.25) | 1.16 (1.12-1.20) |
| Black | 15,498 | 13.3 (12.8-13.8) | 1.59 (1.39-1.83) | 1.47 (1.29- 1.69) | 1.46 (1.39-1.55) | 1.41 (1.34-1.49) | 1.35 (1.27-1.42) |
| Nursing homes with medium-high concentration of blacks (15-34.9%) | |||||||
| White | 137,656 | 11.0 (10.8-11.2) | 1.27 (1.23-1.32) | 1.27 (1.22-1.31) | 1.22 (1.17-1.26) | 1.22 (1.18-1.27) | 1.19 (1.14-1.24) |
| Black | 27,652 | 14.1 (13.7-14.5) | 1.69 (1.48-1.94) | 1.55 (1.35-1.77) | 1.55 (1.48-1.62) | 1.50 (1.43-1.57) | 1.45 (1.38-1.52) |
| Nursing homes with high concentration of blacks (≥35%) | |||||||
| White | 74,176 | 12.1 (11.8-12.4) | 1.45 (1.39-1.51) | 1.42 (1.36-1.49) | 1.34 (1.28-1.40) | 1.35 (1.29-1.42) | 1.33 (1.26-1.40) |
| Black | 74,847 | 15.5 (15.2-15.8) | 1.84 (1.60-2.11) | 1.71 (1.64-1.77) | 1.66 (1.45-1.90) | 1.62 (1.56-1.69) | 1.59 (1.52-1.67) |
Model 1 adjusted for the clustering of residents in nursing homes alone; model 2 included model 1 plus age and gender; model 3 included model 2 plus difficulties in activities of daily living, cognitive performance scale, disease diagnoses (dementia, stroke, diabetes, other endocrine disease, cardiovascular disease, musculoskeletal disease, and cancer), and whether the resident was in malnutrition, incontinence, antipsychotic drug use, physical restraint use, end stage of life, or had hospital admissions during the past 90 days; model 4 included model 3 plus nursing home covariates (number of beds, non-for-profit facility, government facility, chain affiliation, percent of Medicaid residents, RN hours/resident day, LPN/LVN hours/resident day, CNA hours/resident day, and deficiency citations); and model 5 included model 4 plus county characteristics (competition for nursing home residents, percent of population≥65 years, and urban versus rural county) and state dummies.
P<.001 unless otherwise indicated.
P=.003.
Sensitivity analyses
In sensitivity analyses, we found that when the outcome was redefined as pressure ulcers of any stage, the longitudinal trends or disparities across race and site groups did not change substantially (eTable 1 and eFigure 1), and site-of-care disparities persisted after adjustment for resident, facility, county, and state covariates (eTable 2). Analyses comparing white to all nonwhite (Black, Hispanic, Asian/Pacific islander, and American Indian/Alaskan native) high-risk long-term residents showed similar results (eTables 3 and 4, eFigure 2, and eTable 5).
DISCUSSION
We found that among long-term care nursing home residents at high risk for pressure ulcers, black residents had higher prevalence rate than white residents during 2003-2008. The enduring disparity paralleled overall reduced rates across all resident and nursing home groups. Moreover, the disparity was largely related to the site where care was delivered in addition to race itself: residents of both races and in nursing homes with the highest concentration of blacks had at least 30% increased risk-adjusted odds of pressure ulcers compared to residents in nursing homes caring for no or only a small percent of black residents.
Nursing home quality remains to be poor despite the intensified government regulations since late 1980s30-32. In response, current policies have focused greater attention to non-regulatory approaches that rely on the public quality reporting11,12, the QIO (quality improvement organization) technical assistance10,14,33, and more recently pay for performance incentives34,35. To improve the prevention and treatment of pressure ulcers in nursing homes specifically, varied programs have also been implemented and evaluated5,13,15. Existing evidence suggests improved quality of care after program implementations5,10-12,15. Specifically, the national QIO approach and several state programs are found to be successful in improving overall nursing home pressure ulcer care and outcomes10,13,14.
However, concerns arise about the ‘color-blind’ feature of these initiatives, and their potential unintended consequences to sustain or even widen existing racial disparities in nursing home care36,37. Because these quality improvement approaches incorporate no disparity-reducing mechanisms, nursing facilities and local authorities may have no incentive to address disparities beyond global quality improvement38. For example, the CMS’ national quality publications judge all certified nursing homes by overall performance scores calculated from all residents in each facility. Thus, the public reporting tends to provide incentives to improve published scores but not disparities between racial groups or between facilities serving racially or socioeconomically diverse populations.
Research is scarce on the potential impact of generic quality improvement efforts on racial disparities. In particular, evaluations of major CMS and state initiatives have not focused on site-of-care differences, such as differences between nursing homes caring for predominantly white and minority patients. To our knowledge, only one prior study reported that a staff education program implemented in 2 Pennsylvania nursing homes reduced both overall pressure ulcer rate and racial disparities during a 12-week intervention period5. However, findings in this study may not be generalized to other nursing homes or other programs. Our analyses revealed that during the years after major CMS and state nursing home quality initiatives, pressure ulcers among long-term care residents improved overall and across racial and site groups, but disparities persisted.
Given the widespread racial disparities in nursing home care, it is imperative to close the gap beyond industry-wide improvements. The first key step would be understanding why these disparities exist before appropriate efforts can be made to eliminate them. Given that nursing home care for minority residents is concentrated among a small number of nursing homes8,9,39, understanding how outcomes vary as a function of site of care can inform targeted interventions. We found that the enduring racial disparities were largely associated with the type of facilities, and that residents of both races showed substantially increased risk-adjusted odds of pressure ulcers when they received care in minority-concentrated facilities. This suggests that the disparities in pressure ulcer care are largely a system problem, and that the particular nursing home in which a patient is served seems to be more important than patient race itself.
It is not entirely clear why nursing homes highly concentrated by black residents were associated with higher risk-adjusted odds of pressure ulcers. Adjustment for differences in nursing home managerial, staffing, financial, and geographic characteristics did not change these associations. It is possible that these measures were imperfect proxies for facilities’ structural factors that directly affect resident care and outcomes. For example, the absence of appropriate pressure ulcer risk assessment programs may be more common in black-concentrated nursing homes. Thus, this and other underlying organizational, resource, and system-of-care deficits among these nursing homes may persist over time and perpetuate their worsened outcomes relative to other nursing homes.
The findings suggest several policy implications. Importantly, future quality initiatives, such as the renewed CMS QIO program, could consider incorporating disparity-eliminating efforts. For example, Targeting interventions on nursing homes with enduring outcome deficits may promote quality and equity of care more efficiently. Current nursing home quality reporting may contribute to the overall outcome improvement but does not seem to bring a concerted benefit of narrowed disparities. In the long term, the public reporting may show a ‘discouraging’ effect on nursing homes that serve predominantly minority residents, because current report spotlights their worse scores than those of other nursing homes and disregards their similar amount of outcome improvement over time. Indeed, to achieve the same level of reduced pressure ulcer rate, minority-concentrated nursing homes may have devoted more resource and staff inputs given the difficulties of early identification and prevention of pressure ulcers among patients with darkly-pigmented skin. Future report cards should recognize outcome improvements of individual facilities. Similarly, the recently-designed Medicare and Medicaid pay-for-performance programs34,35 in nursing homes could reward both outcome superiority across facilities and secular improvement within a facility.
This study has several limitations. Our analyses focused on pressure ulcer prevalence and its persistent racial disparities; the results may not be generalized to other outcome and process of care disparities in nursing homes40-42. We may have had limited ability in the multivariate risk adjustment to account for variations in resident and site-of-care characteristics. Therefore, the persistent disparities may be partially mediated by unmeasured factors that affect pressure ulcer rates. Finally, we could not determine whether the overall reduced pressure ulcer rate is attributable specifically to the CMS or other quality initiatives in nursing homes, although program-specific effects have been the focus of prior studies10-12.
CONCLUSIONS
This study found that despite the reduced pressure ulcer rates among long-term nursing home residents across all race and nursing home groups during 2003-2008, racial disparities persisted. Persistent risk-adjusted disparities were largely related to the higher rates among nursing homes that disproportionately serve black residents. Future nursing home initiatives may need to devote more attention to disparity reduction efforts beyond global quality improvement.
Supplementary Material
Acknowledgment
This study was funded by the National Institute on Aging (NIA) under grant R01AG032264. The NIA or the Department of Veterans Affairs had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Conflicts of Interests: no conflicts of interest for any authors.
Dr. Yue Li and Ms. Jun Yin had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCE
- 1.Berlowitz DR, Wilking SV. Pressure ulcers in the nursing home. In: Rubenstein LZ, Wieland D, editors. Improving Care in the Nursing Home: Comprehensive Reviews of Clinical Research. Sage; Newbury Park, CA: 1993. [Google Scholar]
- 2.Reddy M, Gill SS, Kalkar SR, Wu W, Anderson PJ, Rochon PA. Treatment of pressure ulcers: a systematic review. JAMA. 2008 Dec 10;300(22):2647–2662. doi: 10.1001/jama.2008.778. [DOI] [PubMed] [Google Scholar]
- 3.Baumgarten M, Margolis D, van Doorn C, et al. Black/White differences in pressure ulcer incidence in nursing home residents. J Am Geriatr Soc. 2004 Aug;52(8):1293–1298. doi: 10.1111/j.1532-5415.2004.52358.x. [DOI] [PubMed] [Google Scholar]
- 4.Lapane KL, Jesdale W, Zierler S. Racial differences in pressure ulcer prevalence in nursing homes. J Am Geriatr Soc. 2005 Jun;53(6):1077–1078. doi: 10.1111/j.1532-5415.2005.53338_5.x. [DOI] [PubMed] [Google Scholar]
- 5.Rosen J, Mittal V, Degenholtz H, et al. Pressure ulcer prevention in black and white nursing home residents: A QI initiative of enhanced ability, incentives, and management feedback. Adv Skin Wound Care. 2006 Jun;19(5):262–268. doi: 10.1097/00129334-200606000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Cai S, Mukamel DB, Temkin-Greener H. Pressure ulcer prevalence among black and white nursing home residents in New York state: evidence of racial disparity? Med Care. 2010 Mar;48(3):233–239. doi: 10.1097/MLR.0b013e3181ca2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.AHRQ . National healthcare disparities report. Agency for Healthcare Research and Quality; Rockville, MD: 2009. [Google Scholar]
- 8.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Aff (Millwood) 2007 Sep-Oct;26(5):1448–1458. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- 10.Rollow W, Lied TR, McGann P, et al. Assessment of the Medicare quality improvement organization program. Ann Intern Med. 2006 Sep 5;145(5):342–353. doi: 10.7326/0003-4819-145-5-200609050-00134. [DOI] [PubMed] [Google Scholar]
- 11.Mukamel DB, Weimer DL, Spector WD, Ladd H, Zinn JS. Publication of quality report cards and trends in reported quality measures in nursing homes. Health Serv Res. 2008 Aug;43(4):1244–1262. doi: 10.1111/j.1475-6773.2007.00829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Werner R, Stuart E, Polsky D. Public reporting drove quality gains at nursing homes. Health Aff (Millwood) 2010 Sep;29(9):1706–1713. doi: 10.1377/hlthaff.2009.0556. [DOI] [PubMed] [Google Scholar]
- 13.Baier RR, Gifford DR, Lyder CH, et al. Quality improvement for pressure ulcer care in the nursing home setting: the Northeast Pressure Ulcer Project. J Am Med Dir Assoc. 2003 Nov-Dec;4(6):291–301. doi: 10.1097/01.JAM.0000094064.06058.74. [DOI] [PubMed] [Google Scholar]
- 14.Rantz MJ, Vogelsmeier A, Manion P, et al. Statewide strategy to improve quality of care in nursing facilities. Gerontologist. 2003 Apr;43(2):248–258. doi: 10.1093/geront/43.2.248. [DOI] [PubMed] [Google Scholar]
- 15.Rosen J, Mittal V, Degenholtz H, et al. Ability, incentives, and management feedback: organizational change to reduce pressure ulcers in a nursing home. J Am Med Dir Assoc. 2006 Mar;7(3):141–146. doi: 10.1016/j.jamda.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Abt. Abt Assoc, Inc. Quality Measures for National Public Reporting: User's Manual. 2004 Nov;1.2 2004. [Google Scholar]
- 17.Mor V. A comprehensive clinical assessment tool to inform policy and practice: applications of the minimum data set. Med Care. 2004 Apr;42(4 Suppl):III50–59. doi: 10.1097/01.mlr.0000120104.01232.5e. [DOI] [PubMed] [Google Scholar]
- 18.Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. Vital Health Stat 13. Jun;2009(167):1–155. [PubMed] [Google Scholar]
- 19.Lawton MP, Casten R, Parmelee PA, Van Haitsma K, Corn J, Kleban MH. Psychometric characteristics of the minimum data set II: validity. J Am Geriatr Soc. 1998 Jun;46(6):736–744. doi: 10.1111/j.1532-5415.1998.tb03809.x. [DOI] [PubMed] [Google Scholar]
- 20.Mor V, Angelelli J, Jones R, Roy J, Moore T, Morris J. Inter-rater reliability of nursing home quality indicators in the U.S. BMC Health Serv Res. 2003 Nov 4;3(1):20. doi: 10.1186/1472-6963-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mor V, Intrator O, Unruh MA, Cai S. Temporal and Geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0. BMC health services research. 2011 Apr 15;11(1):78. doi: 10.1186/1472-6963-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brandeis GH, Morris JN, Nash DJ, Lipsitz LA. The epidemiology and natural history of pressure ulcers in elderly nursing home residents. JAMA. 1990 Dec 12;264(22):2905–2909. [PubMed] [Google Scholar]
- 23.Berlowitz DR, Ash AS, Brandeis GH, Brand HK, Halpern JL, Moskowitz MA. Rating long-term care facilities on pressure ulcer development: importance of case-mix adjustment. Ann Intern Med. 1996 Mar 15;124(6):557–563. doi: 10.7326/0003-4819-124-6-199603150-00003. [DOI] [PubMed] [Google Scholar]
- 24.Berlowitz DR, Brandeis GH, Anderson JJ, et al. Evaluation of a risk-adjustment model for pressure ulcer development using the Minimum Data Set. J Am Geriatr Soc. 2001 Jul;49(7):872–876. doi: 10.1046/j.1532-5415.2001.49176.x. [DOI] [PubMed] [Google Scholar]
- 25.Morris JN, Fries BE, Mehr DR, et al. MDS Cognitive Performance Scale. J Gerontol. 1994 Jul;49(4):M174–182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 26.Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein DU. Does investor ownership of nursing homes compromise the quality of care? Am J Public Health. 2001 Sep;91(9):1452–1455. doi: 10.2105/ajph.91.9.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grabowski DC, Hirth RA. Competitive spillovers across non-profit and for-profit nursing homes. J Health Econ. 2003 Jan;22(1):1–22. doi: 10.1016/s0167-6296(02)00093-0. [DOI] [PubMed] [Google Scholar]
- 28.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986 Mar;42(1):121–130. [PubMed] [Google Scholar]
- 29.Hsiao C. Analysis of panel data. 2nd version. Cambridge University Press; 2003. [Google Scholar]
- 30.IOM. Institute of Medicine. Improving the quality of care in nursing homes. 2001 [Google Scholar]
- 31.General Accounting Office . Nursing home quality: Prevalence of serious problems, while declining, reinforces importance of enhanced oversight (Publication No. GAO-03-561) Washington, D.C.: 2003. [Google Scholar]
- 32.Harrington C, Mullan JT, Carrillo H. State nursing home enforcement systems. J Health Polit Policy Law. 2004 Feb;29(1):43–73. doi: 10.1215/03616878-29-1-43. [DOI] [PubMed] [Google Scholar]
- 33.Stevenson DG, Mor V. Targeting nursing homes under the Quality Improvement Organization program's 9th statement of work. J Am Geriatr Soc. 2009 Sep;57(9):1678–1684. doi: 10.1111/j.1532-5415.2009.02401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abt. Abt Associates Inc. Quality monitoring for Medicare global payment demonstrations: Nursing home quality-based purchasing demonstration. 2006 Jun; [Google Scholar]
- 35.Werner RM, Tamara Konetzka R, Liang K. State adoption of nursing home pay-for-performance. Med Care Res Rev. 2010 Jun;67(3):364–377. doi: 10.1177/1077558709350885. [DOI] [PubMed] [Google Scholar]
- 36.Casalino LP, Elster A, Eisenberg A, Lewis E, Montgomery J, Ramos D. Will pay-for-performance and quality reporting affect health care disparities? Health Aff (Millwood) 2007 May-Jun;26(3):w405–414. doi: 10.1377/hlthaff.26.3.w405. [DOI] [PubMed] [Google Scholar]
- 37.Konetzka RT, Werner RM. Disparities in long-term care: building equity into market-based reforms. Medical care research and review : MCRR. 2009 Oct;66(5):491–521. doi: 10.1177/1077558709331813. [DOI] [PubMed] [Google Scholar]
- 38.Mukamel DB, Spector WD, Zinn JS, Huang L, Weimer DL, Dozier A. Nursing homes' response to the nursing home compare report card. J Gerontol B Psychol Sci Soc Sci. 2007 Jul;62(4):S218–225. doi: 10.1093/geronb/62.4.s218. [DOI] [PubMed] [Google Scholar]
- 39.Fennell ML, Feng Z, Clark MA, Mor V. Elderly hispanics more likely to reside in poor-quality nursing homes. Health Aff (Millwood) 2010 Jan-Feb;29(1):65–73. doi: 10.1377/hlthaff.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bernabei R, Gambassi G, Lapane K, et al. Management of pain in elderly patients with cancer. SAGE Study Group. Systematic Assessment of Geriatric Drug Use via Epidemiology. Jama. 1998 Jun 17;279(23):1877–1882. doi: 10.1001/jama.279.23.1877. [DOI] [PubMed] [Google Scholar]
- 41.Li Y, Mukamel DB. Racial disparities in receipt of influenza and pneumococcus vaccinations among US nursing-home residents. Am J Public Health. 2010 Apr 1;100(Suppl 1):S256–262. doi: 10.2105/AJPH.2009.173468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Allsworth JE, Toppa R, Palin NC, Lapane KL. Racial and ethnic disparities in the pharmacologic management of diabetes mellitus among long-term care facility residents. Ethn Dis. 2005;15(2):205–212. Spring. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.