Abstract
Patient: Female, 42
Final Diagnosis: Acute pulmonary embolism
Symptoms: Chest pain • dyspnea
Medication: Streptokinase • Warfarin
Clinical Procedure: —
Specialty: Cardiology and Neoplasm
Objective:
Management of emergency care
Background:
Deep venous thrombosis (DVT) and subsequent pulmonary embolism (PE) caused by pelvic vein compression are rare and life-threatening complications of leiomyoma of the uterus.
Case Report:
We report a 42-year-old virgin woman with a history of leiomyoma who presented to the emergency department with complaints of dyspnea and pleuritic chest pain with transient spotting. On physical examination, she had a non-tender abdomen with a 20-week size uterus. Imaging investigations revealed an acute DVT in her left leg and a huge uterine-derived mass compressing the common iliac veins. Transesophageal echocardiography (TEE) demonstrated an echogenic mass in her right pulmonary artery consistent with thrombosis. The patient was completely cured using thrombolytic therapy and myomectomy, and was well at 1 year after thrombolysis.
Conclusions:
PE caused by pelvic vein compression is a rare complication of leiomyoma, which should be considered. Thrombolytic therapy associated with myomectomy can be implemented for treating such cases, and TEE can be used for diagnosing suspected high-risk PE.
MeSH Keywords: Echocardiography, Leiomyoma, Pulmonary Embolism, Thrombolytic Therapy
Background
Pulmonary embolism (PE) is a life-threatening condition occurring about 23–69 patients per 100 000 population. It can range from an asymptomatic patient to a massive PE. The implementation of its appropriate treatment at presentation is usually effective and life-saving. PE is also recognized in about 50% of patients with deep venous thrombosis (DVT) and nearly 80% of those who are being diagnosed with PE have DVT [1–3].
Some main predisposing factors, either acquired or inherited, of DVT and the resultant PE include deficiencies of blood coagulation agents, immobilization, hypercoagulable states caused by cancer, pregnancy, trauma, oral contraceptives, and major surgery [2]. A rarely reported cause for developing thromboembolism is uterine leiomyoma contributing to pelvic venous compression, and thus the occurrence of PE in some cases [4].
We present a rare case of DVT and subsequent massive PE caused by a huge uterine leiomyoma, which was treated without any complications.
Case Report
A 42-year-old, non-smoking, virgin woman presented to our institution with complaints of dyspnea and pleuritic chest pain since 2 days ago along with 2-month transient spotting. She had a history of leiomyoma since 5 months ago, and was hospitalized due to vaginal bleeding, and had been undergone therapy by a gonadotropin-releasing hormone (GnRH) agonist and medroxyprogesterone acetate, intramuscularly. To control her anemia, she was given oral ferrous sulfate. There was no relevant familial history of the same condition. On physical examination, she was anxious and tachypneic on admission, with body mass index of 24.7 kg/m2, body temperature 37°C, blood pressure 100/70 mmHg, heart rate 120 beats per min, respiratory rate of 24 breaths per min, and 96% oxygen saturation while breathing room air. Other findings included regular heart beat with a 2/6 systolic murmur in the left sternal border, clear lung sound, and a non-tender abdomen with a 20-week size uterus. There was no swelling in her lower limbs.
An electrocardiogram revealed a sinus tachycardia and inverted T waves in v1 to v3 and inferior leads. Hematologic testing revealed hemoglobin of 11.3 g/dL and other results were within normal limits. Coagulation factors were also unremarkable. A chest radiograph showed Westermark sign without pleural effusion. An ultrasound investigation revealed an acute DVT in the popliteal and superficial femoral veins of her left leg and an enlarged leiomyoma of the uterus. Thereafter, transesophageal echocardiography (TEE) demonstrated normal left ventricle systolic function, severe right ventricle enlargement, McConnell sign, moderate tricuspid regurgitation, severe pulmonary hypertension of 110 mmHg, and dilatation of the main pulmonary artery. In addition, a 2.6 1.6 cm echogenic mass was detected in the left pulmonary artery, consistent with thrombosis (Figure 1). Given her leiomyoma history, she underwent magnetic resonance imaging (MRI), which revealed a huge uterine-derived mass compressing both common iliac veins (Figure 2).
Figure 1.
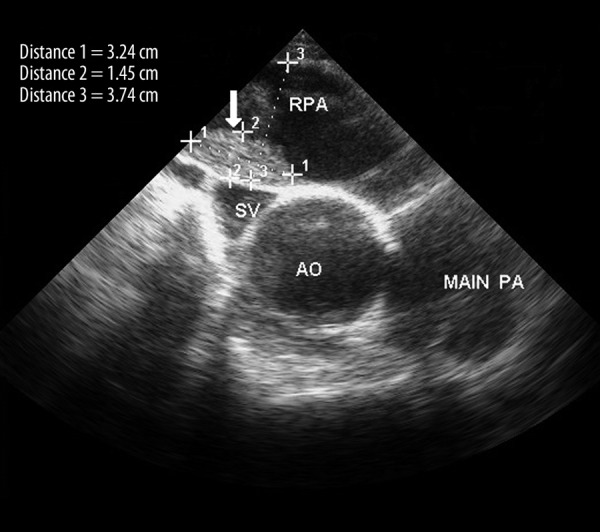
A clot in the right pulmonary artery diagnosed by transesophageal echocardiography. AO – aorta, MPA – main pulmonary artery, RPA – right pulmonary artery.
Figure 2.

Uterine leiomyoma and the compression of both common iliac veins. The arrows show the venous compression (white arrows) and the uterine mass (black arrows).
Due to massive PE, the patient was administered loading dose of 250 000 units of streptokinase and the infusion of 100 000 units per hour during 24 h. After undergoing thrombolysis, her general condition significantly improved, and then she underwent anticoagulation therapy. One unit of packed red blood cells was also transfused. Examination by TEE on the fourth day revealed the disappearance of the pulmonary artery thrombosis. After achieving a therapeutic range of international normalized ratio (range 2.0–3.0), she was discharged on warfarin 5 mg daily.
The patient was followed for 3 months and then evaluated again and examined using TEE and ultrasonography, which demonstrated normal findings. After withholding warfarin preoperatively, she underwent myomectomy instead of hysterectomy due to her uterus preservation. Warfarin therapy commenced again following surgery, and she was discharged in stable condition on warfarin therapy. Nine months after myomectomy, she was well, without evidence of thromboembolism.
Discussion
PE commonly originates from DVT and can rapidly result in death, although appropriate treatment can reduce the risk of mortality. Despite the increase in guidelines on this issue, the optimal therapy, including thrombolysis and catheter-based therapies, has remained unclear, and it seems that we should consider using other factors, including patient wishes, age, quality of life, and comorbidities for implementing proper therapy [2,5].
Uterine leiomyoma is the most common benign pelvic tumor in women over age 30. Some of its well-known acute complications are thromboembolism, torsion of subserosal pedunculated leiomyoma, urinary retention, and hemorrhage. It is usually asymptomatic; however, as it increases in size, symptoms may present due to compression of the surrounding anatomic structures, resulting in significant increase in the incidence of thromboembolism [4,6]. In cases with thrombosis, hysterectomy is the criterion standard treatment, but in patients who want to preserve their fertility, myomectomy provides a conservative option together with using inferior vena cava filters and anticoagulant agents [4].
In our literature review, we found some cases similar to ours, but there were some differences regarding presentations, etiologies, and implemented therapies due to patient condition. Among reported cases, lower limb DVT and PE were most commonly diagnosed, and anticoagulant associated with hysterectomy was the most-implemented therapy. Only 1 report stated that taking progesterone was the etiology of thrombosis. In addition, a vena cava filter was used upon either extensive lower limb or iliac vein thrombosis, and embolectomy was performed in 2 cases (Table 1).
Table 1.
The summary of literature review.
| Author | No. of cases | Age | Diagnosis | Etiology | Implemented therapies |
|---|---|---|---|---|---|
| Bonito et al. 2007 [10] | 1 | 49 y/o | Lower limb DVT + PE | Pelvic vein compression | Anticoagulant + Hysterectomy |
| Nishikawa et al. 2000 [11] | 1 | 51 y/o | Iliac vein thrombosis + PE | Pelvic vein compression | Vena cava filter + Anticoagulant + Hysterectomy |
| Chong et al. 1998 [8] | 2 | 43 y/o 49 y/o |
Extensive Lower limb DVT Lower limb DVT |
Pelvic vein compression Taking progesterone |
Vena cava filter + Anticoagulant + Hysterectomy Anticoagulant + Unspecified surgery |
| Ogawa et al. 1992 [12] | 1 | 49 y/o | Lower limb DVT + PE | Pelvic vein compression | Embolectomy + Thrombectomy + Hysterectomy |
| Dekel et al. 1998 [13] | 1 | 45 y/o | Iliac vein thrombosis | Pelvic vein compression | Vena cava filter + Anticoagulant + Hysterectomy |
| Pakiz et al. 2009 [14] | 1 | 39 y/o | Lower limb DVT | Pelvic vein compression | Anticoagulant + Hysterectomy |
| Stanko et al. 2001 [7] | 1 | 49 y/o | Iliofemoral thrombosis | Pelvic vein compression | Vena cava filter + Anticoagulant + Hysterectomy |
| Unosawa et al. 2009 [15] | 1 | 53 y/o | Lower limb DVT + PE | Pelvic vein compression | Embolectomy + Hysterectomy |
| Falcone et al. 2005 [16] | 1 | 39 y/o | Lower limb DVT + PE | Pelvic vein compression | Anticoagulant + Hysterectomy |
| Chandra et al. 2010 [17] | 1 | 47 y/o | Lower limb DVT + Iliac vein thrombosis | Pelvic vein compression | Anticoagulant + Hysterectomy |
DVT – deep vein thrombosis; PE – pulmonary embolism.
Concurrent incidence of venous thromboembolism and uterine leiomyoma usually developed in women with no other known risk factors of thromboembolism, and most of them were accompanied by compressed pelvic veins, contributing to pelvic and/or lower-limb thrombosis, with the left leg more commonly affected. These conditions were usually treated using anticoagulation and/or thrombolysis along with hysterectomy [7]. However, 1 case has previously been reported in which DVT may have been caused by administering progesterone agents for controlling vaginal bleeding [8]. In addition, as previously known, the use of hormone replacement therapy is associated with the high rate of venous thromboembolism (both DVT and PE) in women [9].
In the present case, we used thrombolysis therapy, which resulted in thrombosis resolution. Given the patient’s condition and her virginity, delayed myomectomy was performed instead of hysterectomy. Furthermore, TEE was also used as a diagnostic tool for identifying suspected PE in this setting for the first time. It is reasonable to assume that the venous stasis caused by leiomyoma was the main cause of DVT and subsequent PE. Administration of medroxyprogesterone acetate may have been another precipitating factor in our case.
Despite the successful therapy and 1-year survival, some questions remain unanswered, including the optimal treatment of PE, the true indication of using vena cava filters, and the proper and safe treatment strategy to decrease the leiomyoma size in such patients. Further prospective studies and clinical trials are needed to clarify these findings.
Conclusions
DVT and subsequent PE caused by the compression of pelvic veins is a rare complication of leiomyoma of the uterus. Thrombolytic therapy associated with myomectomy can be considered in treating such cases, and TEE can be used for diagnosing suspected high-risk PE and prognostic assessment in this setting. We should pay much attention to the rare complications of uterus leiomyoma, including thromboembolism and the implementation of proper therapy based on patient condition.
References:
- 1.Konstantinides S. Clinical practice. Acute pulmonary embolism. N Engl J Med. 2008;359:2804–13. doi: 10.1056/NEJMcp0804570. [DOI] [PubMed] [Google Scholar]
- 2.Tapson VF. Acute pulmonary embolism. N Engl J Med. 2008;358:1037–52. doi: 10.1056/NEJMra072753. [DOI] [PubMed] [Google Scholar]
- 3.Mansmann EH, Singh A. Pulmonary thromboembolism presenting with abdominal symptoms. Am J Case Rep. 2012;13:137–39. doi: 10.12659/AJCR.883240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta S, Manyonda IT. Acute complications of fibroids: Best Pract Res Clin Obstet Gynaecol. 2009;23:609–17. doi: 10.1016/j.bpobgyn.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Jaff MR, McMurtry MS, Archer SL, et al. Management of massive and sub-massive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011;123:1788–830. doi: 10.1161/CIR.0b013e318214914f. [DOI] [PubMed] [Google Scholar]
- 6.Shiota M, Kotani Y, Umemoto M, et al. Deep-vein thrombosis is associated with large uterine fibroids. Tohoku J Exp Med. 2011;224:87–89. doi: 10.1620/tjem.224.87. [DOI] [PubMed] [Google Scholar]
- 7.Stanko CM, Severson MA, II, Molpus KL. Deep venous thrombosis associated with large leiomyomata uteri. A case report. J Reprod Med. 2001;46:405–7. [PubMed] [Google Scholar]
- 8.Chong YS, Fong YF, Ng SC. Deep vein thrombosis in patients with large uterine myomata. Obstet Gynecol. 1998;92:707. doi: 10.1016/s0029-7844(98)00228-2. [DOI] [PubMed] [Google Scholar]
- 9.Huerta C, Johansson S, Wallander MA, et al. Risk factors and short-term mortality of venous thromboembolism diagnosed in the primary care setting in the United Kingdom. Arch Intern Med. 2007;167:935–43. doi: 10.1001/archinte.167.9.935. [DOI] [PubMed] [Google Scholar]
- 10.Bonito M, Gulemi L, Basili R, et al. Thrombosis associated with a large uterine myoma: case report. Clin Exp Obstet Gynecol. 2007;34:188–89. [PubMed] [Google Scholar]
- 11.Nishikawa H, Ideishi M, Nishimura T, et al. Deep venous thrombosis and pulmonary thromboembolism associated with a huge uterine myoma – a case report. Angiology. 2000;51:161–66. doi: 10.1177/000331970005100210. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa N, Hayashi Y, Maehara T, et al. A surgically treated case of acute pulmonary embolism owing to deep vein thrombosis of the leg mainly caused by uterine myoma. Kyobu Geka. 1992;45:631–34. [PubMed] [Google Scholar]
- 13.Dekel A, Rabinerson D, Dicker D, et al. Thrombosis of the Pelvic Veins Associated With A Large Myomatous Uterus. Obstet Gynecol. 1998;92:646–47. doi: 10.1016/s0029-7844(98)00203-8. [DOI] [PubMed] [Google Scholar]
- 14.Pakiz M, But I. Management of acute deep vein thrombosis due to enlarged symptomatic uterine fibroids. Int J Gynaecol Obstet. 2009;105:177–78. doi: 10.1016/j.ijgo.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Unosawa S, Hata M, Sezai A, et al. Pulmonary embolism with myomatous erythrocytosis syndrome and extreme obesity. Thorac Cardiovasc Surg. 2009;57:313–14. doi: 10.1055/s-2008-1038880. [DOI] [PubMed] [Google Scholar]
- 16.Falcone M, Serra P. Massive pulmonary embolism in a woman with leiomyomatous uterus causing pelvic deep venous thrombosis. Ann Ital Med Int. 2005;20:104–7. [PubMed] [Google Scholar]
- 17.Chandra B, Nibedita C, Ramprasad D, et al. Deep venous thrombosis associated with fibroid uterus in a woman complicated by diabetes, hypertension and hemiparesis. J Obstet Gynaecol India. 2010;60:240–41. [Google Scholar]


