Abstract
Objective Little data exist on short-term quality-of-life (QOL) outcomes, specifically sinonasal measures, after endoscopic pituitary surgery.
Design Prospective case series assessed sinonasal QOL before and after the transnasal endoscopic approach to the sella with resection of nasal cavity and sinus tissues.
Setting/Participants/Main Outcome Measures A total of 39 adults scheduled to undergo resection for a pituitary mass preoperatively completed the Sinonasal Outcome Test-22 (SNOT-22). Rating various QOL issues, testing repeated postoperatively at 1 month by 37 patients and 3 months by 35 patients, was analyzed (paired Student t test).
Results SNOT-22 scores (5-point scale; total: 110) averaged 23.4 preoperatively and 27.6 at 1 month but had significantly improved to 16.2 at 3 months (p = 0.03). Emotional well-being parameters (e.g., sadness, frustration, concentration, productivity, fatigue) significantly improved 3 months postoperatively (p < 0.05). Physiologic parameters (e.g., olfaction, obstruction, postnasal drainage) that had worsened at 1 month (< 0.05) then normalized at 3 months.
Conclusion Total ratings for sinonasal QOL shows that SNOT scores were comparable between preoperative and 1-month testing but were improved significantly at 3 months. Individual questions showed marked improvement in emotional well-being and temporary physiologic changes after surgery. Our findings give surgeons information about what patients can expect immediately after transnasal endoscopic pituitary surgery.
Keywords: quality of life, sphenoid sinus, pituitary surgery, endoscopy
Introduction
Although mentioned as long as 100 years earlier, the concept of modern endoscopic pituitary surgery was introduced in France in 1992 and the United States in 1997.1 2 Owing to its improved visibility beyond the capabilities of microscopy, endoscopic approaches are well established and used by many institutions throughout the world. In the treatment of pituitary adenomas, the endoscopic approach provides a panoramic view of the sella turcica. In comparing endoscopic versus microscopic approaches to the sella turcica for pituitary adenomas, several institutions have reported similar oncologic and endocrinology results, improved visualization, and shorter hospital stays.3 4 5 6 As more institutions adopt endoscopy, larger studies are examining long-term oncologic and endocrinology outcomes as well as measures related to quality of life (QOL) specific for sinonasal disorders, such as the patient-reported Sino-Nasal Outcome Test (SNOT) and its variations.
In comparison with the sublabial approach to the sella turcica, major concerns related to the use of the transnasal endoscopic approach are its problematic effects on sinonasal function because of the creation of a large sphenoidotomy and often partial removal of the superior turbinates and posterior septum. Specifically, removal of these structures may disturb olfactory epithelium and sinus physiology. In a 2009 study about the effects of endoscopic pituitary surgery on olfaction in 57 consecutive patients, Hart et al noted olfactory ability decreased 1 month after surgery but changes uniformly normalized 2 months later.7 Although Wang et al confirmed these results, the use of a nasal septal flap for closure of the sellar defect may have long-term deleterious effects on olfaction.8 9
Little has been published to date on the short-term QOL outcomes, specifically sinonasal measures, after endoscopic pituitary surgery. In three retrospective studies that compared endoscopic and sublabial approaches specific to sinonasal QOL, no differences were found between the two groups, although no preoperative baseline data had been included.9 10 11 12 13 In this prospective study in patients with pituitary tumors, we quantify the postoperative effects of endoscopic transsphenoidal pituitary surgery on sinonasal QOL by using the modified SNOT-22, obtaining patient-reported ratings before and 1 and 3 months after surgery.
Methods
With approval from the University of Cincinnati institutional review board, 39 consecutive patients ≥18 years with pituitary adenomas between October 2010 and November 2011 were included; those excluded had underwent previous endoscopic sinus or pituitary surgery, planned extended transnasal approaches requiring nasal septal or other local flaps, or were unable to complete the questionnaire. Among 18 women and 21 men who ranged from 19 to 76 years of age (mean: 48 years), there were 26 (67%) with nonsecreting macroadenomas, 10 (26%) with hormone-active adenomas (5 growth hormone, 4 prolactinomas, 1 Cushing), and 3 (7%) with Rathke cleft cysts.
Patients were informed about the risks and benefits of surgery including stroke, visual loss, cerebrospinal fluid leak, and epistaxis, and about short-term postoperative olfactory and taste disturbance, nasal cavity crusting, foul nasal odor, and postnasal drainage lasting from 4 to 12 weeks after surgery. Preoperatively, all 39 patients completed the Sino-Nasal Outcome Test 22 (SNOT-22), a validated test for QOL that is preferred for its reliability, responsiveness, and ease of use (5-point scale; total: 110).10 Postoperatively, 37 patients (19 men, 18 women) completed a 1-month and 35 (17 men, 18 women) completed a 3-month SNOT-22 evaluation.
Surgical Approach
All patients underwent a transnasal, transsphenoidal removal of pituitary tumors by the senior authors (L.A.Z. and P.V.T.) with preservation of the middle turbinates and partial resection of the inferior third of the superior turbinates with a sinus shaver. Wide bilateral sphenoidotomies was performed with Kerrison rongeurs. Addition of a posterior septectomy increased the working space by elevating the septal mucosa in a subperiosteal plane with a Cottle elevator from the anterior edge of the middle turbinate posterior to the sphenoidotomy. The underlying septal bone was removed with endoscopic scissors. The elevated mucosa was removed with a shaver preserving ∼ 1 cm of superior mucosa for olfactory preservation and anterior and inferior septal mucosa to cover the remaining septal bone (Fig. 1A). The cut edges of the sphenoid sinus and septal mucosa was cauterized with bipolar. The intersinus septum was then removed with rongeurs; the sellar face opened with Kerrison rongeurs or a high-speed diamond drill (Fig. 1B). After removal of the tumor and sellar face reconstruction with abdominal fat and septal bone, DuraSeal (Covidien, Mansfield, Maryland, United States) was sprayed over the sellar reconstruction, and a bioresorbable nasal dressing was placed between the middle turbinate and septum to prevent synechiae.
Fig. 1.
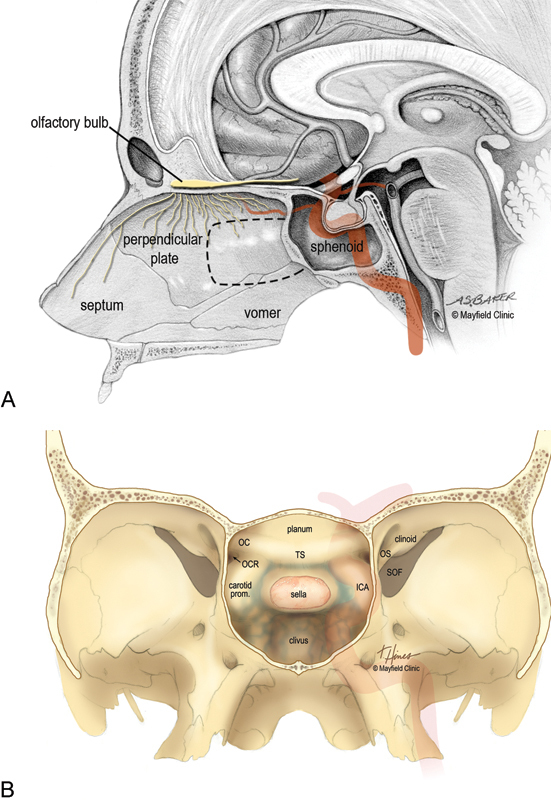
Endoscopic pituitary surgery. (A) Sagittal view of the nasal septum. Dashed line shows portion of septum removed during surgery and preservation of olfactory fibers along the superior septum. (B) Coronal view after wide bilateral sphenoidotomy exposes the optic prominences, internal carotid arteries (ICAs), clival recess, and planum sphenoidale. OC, optic chasm; OCR, opticocarotid recess; OS, optic strut; SOF, superior orbital fissure; TS, tuberculum sella. (Printed with permission from Mayfield Clinic; all rights reserved.)
Postoperatively, patients were instructed to use saline nasal spray every 2 hours during the day for 1 week. Saline rinses, twice a day beginning 1 week postoperatively, were continued until the nasal cavity and sphenoid sinus had healed. Patients were examined monthly in the office by an otolaryngologist until healing was complete. Beginning 1 month postoperatively, the nasal cavity and sphenoid were examined; the nasal cavity was debrided as necessary. Patients repeated SNOT-22 testing 1 and 3 months after surgery; use of debridement, antibiotics, and/or complications was documented.
Statistical Analysis
Paired Student t tests were used to compare pre- and postoperative scores. A power analysis indicated that a sample size of 35 was adequate to detect a 10% change with 90% power.
Results
All 39 patients underwent successful removal of the pituitary adenoma via the transsphenoidal endoscopic approach; there were no postoperative mortalities. Postoperative magnetic resonance imaging at day 1 revealed eight subtotal resections; six were planned because of cavernous sinus extension lateral to the carotid artery, and two were unintentional (i.e., one suprasellar and one intrasellar case). During follow-up examination in office, debridement for nasal crusting and odor was performed for all patients at 1-month follow-up, 32 patients at 2 months, and 7 patients at 3 months; no debridements were performed after 3 months. One patient who presented with epistaxis 3 weeks after surgery subsequently underwent cautery of the posterior septal artery, and one patient received antibiotics 6 weeks after surgery for culture-confirmed Staphylococcus aureus of the sphenoid sinus.
Sinonasal Quality-of-Life Testing
Of a total possible 110 points, SNOT-22 scores (total ± standard deviation) averaged 23.4 ± 18.2 preoperatively for 39 patients, 27.6 ± 17.3 at 1 month for 37 patients, and 16.2 ± 12.6 at 3 months for 35 patients. Therefore, improvements were significant between preoperative and 3-month scores (p < 0.05) but were unchanged at 1-month scores (p = 0.4) (Table 1). Mean changes were 4.22 higher (95% confidence interval [CI], −1.5 to 9.94; p = 0.4) between the preoperative and 1-month postoperative scores and 7.19 lower (95% CI, 3.01–11.37; p < 0.05) between the preoperative and 3-month postoperative scores. Three months after surgery, patients rated emotional well-being questions, such as lack of good sleep, waking tired, fatigue, reduced productivity, reduced concentration, dizziness, and frustration as significantly improved (p < 0.05). Patients' ratings for physiologic factors, such as need to blow nose, sneezing, runny nose, postnasal drip, thick nasal discharge, congestion, and olfaction, decreased at 1 month (< 0.05) and returned to baseline at 3 months (Table 1).
Table 1. SNOT-22 scores for 39 patients preoperatively, 37 patients at 1-month postoperatively, and 35 patients at 3-month follow upa .
| Questions | Presurgery | 1 mo post | 3 mo post |
|---|---|---|---|
| Need to blow nose | 0.6 ± 0.96 | 1.9 ± 1.61 | 0.9 ± 1.28 |
| Sneezing | 0.5 ± 0.68 | 1.3 ± 1.33 | 0.7 ± 0.99 |
| Runny nose | 0.7 ± 1.05 | 1.4 ± 1.16 | 0.7 ± 0.97 |
| Cough | 0.6 ± 0.99 | 0.6 ± 0.96 | 0.7 ± 1.02 |
| Postnasal drip | 0.7 ± 1.13 | 1.3 ± 1.35 | 0.9 ± 1.30 |
| Thick nasal discharge | 0.4 ± 0.85 | 1.4 ± 1.52 | 0.7 ± 1.27 |
| Ear fullness | 0.5 ± 0.85 | 0.7 ± 0.93 | 0.5 ± 0.74 |
| Dizziness | 0.9 ± 1.29 | 0.4 ± 0.72 | 0.2 ± 0.65 |
| Ear pain | 0.4 ± 0.81 | 0.6 ± 1.00 | 0.1 ± 0.43 |
| Facial pain/pressure | 0.6 ± 1.18 | 1.1 ± 1.52 | 0.3 ± 0.75 |
| Difficulty falling asleep | 1.3 ± 1.85 | 1.2 ± 1.56 | 0.8 ± 1.34 |
| Waking up at night | 1.8 ± 1.70 | 1.6 ± 1.79 | 1.2 ± 1.48 |
| Lack of good night's sleep | 1.9 ± 1.89 | 1.6 ± 1.79 | 1.1 ± 1.47 |
| Waking up tired | 2.4 ± 1.79 | 1.8 ± 1.77 | 1.3 ± 1.34 |
| Fatigue during day | 2.3 ± 1.80 | 1.9 ± 1.68 | 1.2 ± 1.35 |
| Reduced productivity | 1.9 ± 1.79 | 1.6 ± 1.81 | 0.9 ± 1.26 |
| Reduced concentration | 1.7 ± 1.72 | 1 ± 1.51 | 0.7 ± 1.07 |
| Frustrated/restless/irritable | 1.8 ± 1.90 | 1.1 ± 1.55 | 0.7 ± 1.08 |
| Sad | 1.1 ± 1.51 | 0.8 ± 1.33 | 0.5 ± 1.15 |
| Embarrassed | 0.2 ± 0.74 | 0.2 ± 0.71 | 0.1 ± 0.34 |
| Sense of taste and smell | 0.3 ± 0.77 | 2.1 ± 1.53 | 0.7 ± 1.07 |
| Blockage/congestion in nose | 0.6 ± 1.09 | 2.0 ± 1.56 | 0.9 ± 1.26 |
| Total | 23.4 ± 18.20 | 27.6 ± 17.27 | 15.9 ± 12.59 |
Significant changes (p < 0.05) compared with preoperative scores are shown in boldface.
Discussion
Among many variations afforded in the transnasal, transsphenoidal endoscopic approaches to the sella, our 39 consecutive patients underwent successful removal of pituitary adenomas via a large bilateral sphenoidotomy, removal of the posterior septal bone and mucosa, and resection of the inferior third of the superior turbinates bilaterally. Using this approach allowed ample working space for binostril instrumentation and a panoramic view of the posterior wall of the sphenoid sinus from lateral wall to lateral wall, sphenoid floor, and planum sphenoidale. When compared with preoperative patient-reported ratings, 3-month ratings on the SNOT-22 reflected improved emotional well-being and resolution of sinonasal symptoms. Given that the 1-month scores did not show such improvement may be helpful in outlining realistic expectations for immediately after surgery and during the course of healing over several months.
Olfactory neuroepithelium lines the cribriform plate, superior turbinate, superior septum, and some areas of the middle turbinate.14 Although portions of neuroepithelium are permanently removed by our approach to the sella, our patients reported only a temporary, although significant, decrease in olfactory changes at 1 month that had returned to preoperative levels at 3 months. In a prospective study using the University of Pennsylvania Smell Identification Test to evaluate how endoscopic pituitary surgery affected one's sense of smell, Hart et al noted patients experienced a temporary decrease in olfaction at 1 month but had recovered preoperative baseline scores by 3 months.7 This finding contrasts with the observation of longer-term olfactory dysfunction after pituitary surgery using a nasal septal flap.9 Recovery of olfaction in our patients was likely related to the resolution of mucosal edema and abundant nasal crusting caused by the disruption of mucociliary clearance in the sphenoid sinus and along the cut edges of the septum rather than the loss of olfactory neuroepithelium. Indeed, trapped mucosal secretions and nasal crusting that ultimately required nasal cavity debridement occurred in all patients at 1 month but in only 18% of patients at 3 months.
At 1-month postsurgery, SNOT-22 aggregate scores had not changed (p = 0.4). These included ratings for need to blow nose, sneezing, runny nose, postnasal drip, thick nasal discharge, and congestion (p < 0.05). As with olfaction, disruption of normal mucociliary flow, edema, and nasal crusting along the cut edges of mucosa and olfactory epithelium increase congestion and thicken mucus secretions. Furthermore, dissolvable products, such as DuraSeal and bioabsorbable nasal dressings, increase the nasal cavity burden and negatively affected SNOT-22 scores. As with olfaction, these scores had improved by 3 months as the nasal lining healed. In comparing ratings with the Rhinosinusitis Disability Index (RSDI) and SNOT-22 between open and endoscopic pituitary surgery, Graham et al noted improved rhinology-specific QOL scores among patients treated by endoscopic surgery; however, no baseline data were available to compare pre- and postoperative values.11 Using the RSDI instrument to evaluate changes in sinonasal QOL before and an average 2 years after surgery, Suberman et al observed no changes in emotional, functional, and physical domains of the RSDI, a finding that agrees with our data.12 In addition, our patients typically rated decreases in physiologic domains, reflecting temporary problematic QOL changes for patients 1 month after surgery. Using these QOL measures is important for patient education in establishing expectations for before and after surgery. Increased difficulty with sinus-specific physiologic parameters was offset by a significant decreased difficulty with feelings of dizziness and trends to improved emotional well-being. By 3 months, all decreases in sinonasal physiology returned to baseline and emotional factors, such as lack of good sleep, waking tired, fatigue, reduced productivity, reduced concentration, dizziness, and frustration, significantly improved (p < 0.05). Our findings agree with several QOL studies in patients with pituitary and other brain tumors, before and after surgical and/or medical intervention, specifically that intervention for the control or cure of brain tumors improves emotional well-being.14 15 16 17 However, these changes may be transient because longer term studies, such as the Suberman RSDI, showed no long-term benefit of emotional domains.
According to the SNOT-22 scores, our 39 patients rated that transnasal endoscopic resection of pituitary tumors does not significantly change sinonasal QOL within the first 3 months after surgery. With no prospective head-to-head comparisons available with the sublabial transseptal approach, these results suggest at least equivalence with the historical mainstay of pituitary surgery. However, improved visibility and shorter hospitalization times strengthen the argument for a purely endoscopic approach. Although initial studies suggest an equal or slight improvement in oncologic outcomes, further large series with long-term outcomes are necessary to consider endoscopy as the gold standard for pituitary surgery.
Conclusion
Among patients who underwent the endoscopic, transsphenoidal approach for pituitary tumors, no differences were measured by SNOT-22 scores between before and 1 month after surgery. At 1 month postoperatively, physiologic changes, likely due to the disruption of mucociliary flow leading to mucus crusting and soft tissue edema, were offset by improvement in emotional scores. At 3 months, SNOT-22 scores had significantly improved, likely due to the resolution of physiologic scores and continued improvement in emotional well-being. Based on our patients' responses and clinical examinations 3 months after surgery, the endoscopic transsphenoidal approach to the sella for pituitary adenomas appears to have no negative impact on sinonasal QOL.
Conflict of Interest The authors have nothing to disclose.
Financial Disclosure
The authors did not receive any financial support for this work.
References
- 1.Jankowski R, Auque J, Simon C, Marchal J C, Hepner H, Wayoff M. Endoscopic pituitary tumor surgery. Laryngoscope. 1992;102(2):198–202. doi: 10.1288/00005537-199202000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Jho H D, Carrau R L. Endoscopy assisted transsphenoidal surgery for pituitary adenoma. Technical note. Acta Neurochir (Wien) 1996;138(12):1416–1425. doi: 10.1007/BF01411120. [DOI] [PubMed] [Google Scholar]
- 3.Cheng R X, Tian H L, Gao W W, Li Z Q. A comparison between endoscopic trans-sphenoidal surgery and traditional trans-sphenoidal microsurgery for functioning pituitary adenomas. J Int Med Res. 2011;39(5):1985–1993. doi: 10.1177/147323001103900545. [DOI] [PubMed] [Google Scholar]
- 4.Goudakos J K, Markou K D, Georgalas C. Endoscopic versus microscopic trans-sphenoidal pituitary surgery: a systematic review and meta-analysis. Clin Otolaryngol. 2011;36(3):212–220. doi: 10.1111/j.1749-4486.2011.02331.x. [DOI] [PubMed] [Google Scholar]
- 5.Messerer M, De Battista J C, Raverot G. et al. Evidence of improved surgical outcome following endoscopy for nonfunctioning pituitary adenoma removal. Neurosurg Focus. 2011;30(4):E11. doi: 10.3171/2011.1.FOCUS10308. [DOI] [PubMed] [Google Scholar]
- 6.Theodosopoulos P V, Leach J, Kerr R G. et al. Maximizing the extent of tumor resection during transsphenoidal surgery for pituitary macroadenomas: can endoscopy replace intraoperative magnetic resonance imaging? J Neurosurg. 2010;112(4):736–743. doi: 10.3171/2009.6.JNS08916. [DOI] [PubMed] [Google Scholar]
- 7.Hart C K, Theodosopoulos P V, Zimmer L A. Olfactory changes after endoscopic pituitary tumor resection. Otolaryngol Head Neck Surg. 2010;142(1):95–97. doi: 10.1016/j.otohns.2009.09.032. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y Y, Srirathan V, Tirr E, Kearney T, Gnanalingham K K. Nasal symptoms following endoscopic transsphenoidal pituitary surgery: assessment using the General Nasal Patient Inventory. Neurosurg Focus. 2011;30(4):E12. doi: 10.3171/2011.1.FOCUS10319. [DOI] [PubMed] [Google Scholar]
- 9.Rotenberg B W, Saunders S, Duggal N. Olfactory outcomes after endoscopic transsphenoidal pituitary surgery. Laryngoscope. 2011;121(8):1611–1613. doi: 10.1002/lary.21890. [DOI] [PubMed] [Google Scholar]
- 10.Karabatsou K, O'Kelly C, Ganna A, Dehdashti A R, Gentili F. Outcomes and quality of life assessment in patients undergoing endoscopic surgery for pituitary adenomas. Br J Neurosurg. 2008;22(5):630–635. doi: 10.1080/02688690802220379. [DOI] [PubMed] [Google Scholar]
- 11.Graham S M, Iseli T A, Karnell L H, Clinger J D, Hitchon P W, Greenlee J D. Endoscopic approach for pituitary surgery improves rhinologic outcomes. Ann Otol Rhinol Laryngol. 2009;118(9):630–635. doi: 10.1177/000348940911800905. [DOI] [PubMed] [Google Scholar]
- 12.Suberman T A, Zanation A M, Ewend M G, Senior B A, Ebert C S Jr. Sinonasal quality-of-life before and after endoscopic, endonasal, minimally invasive pituitary surgery. Int Forum Allergy Rhinol. 2011;1(3):161–166. doi: 10.1002/alr.20029. [DOI] [PubMed] [Google Scholar]
- 13.Hopkins C, Gillett S, Slack R, Lund V J, Browne J P. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol. 2009;34(5):447–454. doi: 10.1111/j.1749-4486.2009.01995.x. [DOI] [PubMed] [Google Scholar]
- 14.Doty R L. Olfaction. Annu Rev Psychol. 2001;52:423–452. doi: 10.1146/annurev.psych.52.1.423. [DOI] [PubMed] [Google Scholar]
- 15.Gleason J F Jr Case D Rapp S R et al. Symptom clusters in patients with newly-diagnosed brain tumors J Support Oncol 200759427–433., 436 [PubMed] [Google Scholar]
- 16.Ben-Shlomo A, Sheppard M C, Stephens J M, Pulgar S, Melmed S. Clinical, quality of life, and economic value of acromegaly disease control. Pituitary. 2011;14(3):284–294. doi: 10.1007/s11102-011-0310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Klaauw A A, Kars M, Biermasz N R. et al. Disease-specific impairments in quality of life during long-term follow-up of patients with different pituitary adenomas. Clin Endocrinol (Oxf) 2008;69(5):775–784. doi: 10.1111/j.1365-2265.2008.03288.x. [DOI] [PubMed] [Google Scholar]


