Abstract
Previous research has shown that two dimensions of temperament referred to as neuroticism/behavioral inhibition (N/BI) and extraversion/behavioral activation (E/BA) are key risk factors in the development and maintenance of anxiety and mood disorders (Brown & Barlow, 2009). Given such findings, these temperamental dimensions may represent promising treatment targets for individuals with emotional disorders; however, to date, few studies have investigated the effects of psychological treatments on temperamental constructs generally assumed to be “stable, inflexible, and pervasive” (American Psychiatric Association, 2000).
The present study addresses this gap in the literature by examining the effects of the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP; Barlow et al., 2011), a cognitive-behavioral therapy designed to target core processes of N/BI and E/BA temperaments, in a sample of adults with principal anxiety disorders and a range of comorbid conditions. Results revealed small effects of the UP on N/BI and E/BA compared with a waitlist control group at post-treatment. Additionally, decreases in N/BI and increases in E/BA during treatment were associated with improvements in symptoms, functioning, and quality of life. Findings provide preliminary support for the notion that the UP treatment facilitates beneficial changes in dimensions of temperament.
Keywords: Temperament, anxiety, depression, treatment, cognitive-behavioral
Temperament refers to a biologically based tendency to experience a particular constellation of emotions, as well as characteristic levels emotional intensity and reactivity to specific types of stimuli (Allport, 1937; Barlow, Sauer-Zavala, Carl, Ellard, & Bullis, 2013). Contemporary research suggests overlap between temperament and two higher order dimensions of personality that reflect fundamental emotional tendencies, namely: neuroticism and extraversion (Clark & Watson, 1999). Neuroticism, on a continuum with emotional stability, is defined as the tendency to experience frequent and strong negative emotional responses, including anxiety, fear, irritability, anger, sadness, and the like. This exaggerated negative emotionality is often accompanied by beliefs that the world is a threatening place and that one is unable to cope with or control negative events (Barlow, 2002; Eysenck, 1947; Goldberg, 1993). In contrast, extraversion is characterized by a willingness to engage with one’s environment with energy, cheerfulness, sociability, and confidence, whereas introversion refers to the tendency to be more reserved and solitary (Eysenck, 1967; McCrae & Costa, 1987).
There are a number of closely related constructs including “negative affectivity/emotionality,” “behavioral inhibition,” “trait anxiety,” or “harm avoidance” for neuroticism and “positive affectivity/emotionality,” “behavioral activation” or “surgency” for extraversion. Although these different temperamental constructs overlap substantially, there are subtle differences among them. While these constructs can all span continua of adaptive to maladaptive functioning, they vary in the degree to which they aim to assess more normative (i.e., positive affect) versus pathologic (i.e., interpersonal surgency) features of temperament or personality. Relatedly, they maintain slightly different associations with psychological symptoms (Jorm et al., 1999; Naragon-Gainey, Gallagher, & Brown, 2013). Behavioral inhibition, for example, is less strongly correlated with symptoms of anxiety and depression than neuroticism and negative affectivity (Jorm et al.,1999). This is in line with the theoretical conceptualization of behavioral inhibition and behavioral activation as representing basic motivational tendencies in response to cues of threat and reward that are relatively stable and independent of symptoms (Carver & White, 1994; Jorm et al., 1999). In fact, the authors of the most commonly used assessment of the behavioral inhibition and activation (BIS/BAS; Carver & White, 1994), which is utilized in the present study, selected language for the measure items that would facilitate differentiation of fundamental motivational tendencies from symptoms of anxiety or depression (Carver & White, 1994; Jorm et al., 1999). There are also slightly varying associations between the specific temperament constructs and different psychological disorders (Naragon-Gainey et al., 2013). For example, positive affectivity, an affective component of temperament, is more strongly (inversely) associated with unipolar depression than social anxiety, whereas extraversion, reflecting more of an interpersonal component of temperament, is more strongly (inversely) associated with social anxiety than unipolar depression (Watson & Naragon-Gainey, 2010).
Although the differences among these temperamental constructs are important, particularly for measurement considerations, the close conceptual and empirical overlap of these variables has led many researchers to view them as assessing largely common processes of temperament. Consistent with this perspective, we refer to the dimensions of temperament as neuroticism/behavioral inhibition (N/BI) and extraversion/behavioral activation (E/BA), reflecting the most commonly used, stable measures of temperament (Brown, 2007; Brown & Barlow 2009; Campbell-Sills, Liverant, & Brown, 2004; Carver & White, 1994).
A substantial literature underscores the role of N/BI in accounting for the onset, overlap, and maintenance of anxiety, depressive, and related disorders. N/BI is implicated in the full range of emotional disorders, including depression (DEP), generalized anxiety disorder (GAD), social anxiety (SOC), obsessive compulsive disorder (OCD), panic disorder (PD), and posttraumatic stress disorder (PTSD; Brown, 2007; Brown & Barlow, 2009; Gershuny & Sher, 1998; Kessler et al., 2011; Watson, Clark, & Tellegen, 1988). Elevated N/BI appears to function as a common, higher order vulnerability factor that explains a substantial portion of the covariance and comorbidity among these disorders. In addition, higher levels of N/BI are associated with decreased treatment response for several disorders (Brown, 2007). Overall, these data suggest that N/BI is important to consider in the context of emotional disorders, as it impacts etiology, symptomatology, and treatment.
Although less empirical attention has been paid to the relationships between E/BA and psychological health, emerging research suggests this construct may also have implications for a variety of psychological outcomes (Garland et al., 2010; Pressman & Cohen, 2005). Structural models have indicated that low E/BA is associated with unipolar depression (Clark & Watson, 1991), social anxiety (Brown, Chorpita, & Barlow 1998), and agoraphobia (Rosellini, Lawrence, Meyer, & Brown, 2010). Low E/BA has also been associated with posttraumatic stress disorder (Trull & Sher, 1994), and in fact, a recent meta-analytic study indicated low E/BA is a characteristic of most individuals with anxiety or mood disorders (Kotov, Gámez, Schmidt, & Watson, 2010). On the other end of the spectrum, high levels of E/BA are associated with risk for or diagnoses of bipolar disorders (Johnson, Gruber, & Eisner, 2007; Gruber, Johnson, Oveis, & Keltner, 2008). Together, N/BI and E/BA account for a large portion of the shared variance across anxiety and mood disorders (Brown, 2007; Krueger, 1999).
Although temperamental and personality factors are often thought to be “stable, inflexible, and pervasive” (American Psychiatric Association, 2000), there is increasing evidence that these traits may be responsive to some treatments. Several naturalistic studies have investigated the malleability of temperament as a function of time and treatment in samples of patients with emotional disorders. Brown (2007) modeled changes in temperament variables and symptoms in adults with anxiety and mood disorders over a period of 2 years, during which time approximately 76% of the sample received treatment of some kind (psychotherapy and/or pharmacotherapy). Results indicated N/BI improved substantially as a result of treatment, whereas E/BA did not. However, another study found no discernible effect of treatment on N/BI or E/BA in a sample of patients with major depressive disorder who were followed over an 8-month period in which the majority of them received some combination of psychological and/or pharmacological treatment (Kasch, Rottenberg, Arnow, & Gotlib, 2002). The contrasting findings of these two studies highlight the potential variability in treatment effects on temperament, which may be a result of different treatment approaches. These results suggest the need for research into the effects of specific treatments on temperament.
In fact, research on pharmacological treatments and temperament suggests that certain therapeutic agents may differentially modify specific temperament dimensions. For example, serotonergic medications (i.e., selective serotonin reuptake inhibitors [SSRIs]) appear to suppress N/BI (e.g., Fu et al., 2004; Harmer et al., 2009), and to a lesser extent also suppress E/BA (McCabe, Mishor, Cowen, & Harmer, 2010). These effects may be due to serotonergic-induced decreases in amgydalal reactivity in response to threat cues and blockage of dopaminergic neurotransmission prefrontal cortex regions (Soskin, Carl, Alpert, & Fava, 2012). Conversely, catecholaminergic (i.e., noradrenergic/dopaminergic) drugs appear to preferentially enhance E/BA (McCabe et al., 2010; Tomarken, Dichter, Freid, Addington, Shelton, 2004) through increases in noadrenergic and dopaminergic neurotransmission in mesolimbic reward circuits (Soskin et al., 2012). These results further suggest that specific treatment approaches have the potential to produce differential effects on dimensions of temperament.
However, few studies have investigated changes in temperament in response to specific psychological treatments. Rapee, Kennedy, Ingram, Edwards & Sweeney (2005) developed a parent-focused, cognitive-behavioral prevention program for preschool-age children with elevated N/BI. In an initial randomized-controlled trial, results revealed no differences in temperamental change in the intervention versus control group (Rapee et al., 2005). But in a subsequent investigation using a sample of children with higher levels of N/BI and a more intensive program structure, the intervention significantly reduced N/BI (Kennedy, Rapee, & Edwards, 2009).
Among adults with major depressive disorder, Tang and colleagues (2009) investigated the effect of pharmacological treatment with paroxetine (an SSRI), cognitive therapy (CT), or placebo on symptoms of depression, N/BI, and E/BA. Patients taking paroxetine, compared to those taking placebo, demonstrated greater changes in N/BI and E/BA, even when controlling for changes in depressive symptoms. In contrast, although CT resulted in greater change in N/BI and E/BA than placebo, after controlling for depressive symptom change, this difference was only significant for E/BA. Together, these results indicate that temperamental variables can be modified as a result of SSRI or CT interventions, and that corresponding changes may be independent from symptom functioning.
One psychological treatment that may be relevant in a more systematic exploration of how psychotherapeutic components impact temperament dimensions is the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP; Barlow et al., 2011). The UP is a cognitive-behavioral intervention developed to address core temperamental processes in emotional disorders; as such, it is suited to treat a broad range of anxiety, mood, and related disorders, and accompanying comorbid conditions. Specifically, this treatment aims to address maladaptive emotion response tendencies that contribute to both N/BI and E/BA, and is based on the notion that individuals’ reactions to their emotions influence the frequency and intensity of their future emotions and emotion response tendencies. The UP treatment consists of five core treatment modules that directly target maladaptive reactions to the experience of emotions. Several modules provide skills for relating more adaptively to emotional experiences including: increasing present-focused awareness and acceptance of all emotions (both negative and positive) perceived as uncomfortable, enhancing cognitive flexibility regarding the meanings and consequences of emotions, and reducing emotional avoidance behaviors. Other modules facilitate the extinction of anxiety and distress to emotional experience through interoceptive and in vivo exposure exercises, giving patients the opportunity to practice tolerating emotions using the range of skills acquired during earlier modules. While the UP addresses fundamental characteristics of N/BI and E/BA, there may be certain facets of these temperaments that are not explicitly addressed, such as well-being and social connectedness components of E/BA.
While the efficacy of UP in treating anxiety and comorbid disorders has been evaluated in several preliminary studies (Ellard et al., 2010; Farchione et al., 2012) and a large, ongoing randomized-controlled trial, the current study examines whether the UP indeed produces improvements in N/BI and E/BA. We hypothesized that there would be decreases in N/BI and increases in E/BA as a function of participation in the UP as compared with a waitlist control. An additional goal of this study was to assess whether changes in temperamental variables are related to improvements in treatment outcomes. Based on research described above (e.g., Brown et al., 1998; Brown, 2007; Clark & Watson, 1991; Watson & Naragon-Gainey, 2010), we hypothesized that decreases in N/BI would be related to decreased anxiety and depressive symptoms, and that increases in E/BA would be primarily associated with decreased depression, and to a lesser extent, with decreased anxiety. We also expected that decreased N/BI and increased E/BA would predict improved functional impairment and quality of life.
Method
Participants
Data were derived from a randomized controlled trial of the UP compared with a waitlist control (see Farchione et al., 2012). A total sample of N = 37 participants were recruited from individuals seeking treatment at the Center for Anxiety and Related Disorders at Boston University (CARD). Inclusion criteria were: (a) a principal (most severe) anxiety disorder diagnosis, determined by the Anxiety Disorders Interview Schedule for DSM-IV – Lifetime Version (ADIS-IV-L; DiNardo, Brown, & Barlow, 1994), (b) able to provide informed consent, (c) able to attend all study-related appointments, (d) over the age of 18, (e) fluency in English. Participants were excluded if they presented with a condition necessitating immediate alternative treatment or co-existing treatment that may have interfered with the study treatment, or had undergone a recent, adequate course of CBT (defined as 8 or more sessions).
Principal anxiety disorder diagnoses in the sample were social anxiety disorder (n=8), obsessive compulsive disorder (n=8), panic disorder with agoraphobia (n=8), generalized anxiety disorder (n=7), anxiety disorder NOS (n=2), and posttraumatic stress disorder (n=1). Three participants received co-principal diagnoses (principal diagnoses of equal severity); the average total number of diagnoses was 2.16 (SD = 1.19). Among the sample, nine patients were diagnosed with comorbid depression (MDD, depressive disorder NOS or dysthymia). Participants were, on average, 29.67 years of age (SD = 9.43); 40.5% (n=15) were male and 94.6% (n=35) were Caucasian. Participants were randomized to either an immediate-treatment (n=26) or delayed-treatment following a 16-week wait-list (n=11). For information regarding attrition, see Farchione et al. (2012). All analyses in the present study are based on the intent-to-treat sample (N=37).
Measures
Anxiety Disorders Interview Schedule for DSM–IV: Lifetime Version (ADIS– IV–L; DiNardo, Brown, & Barlow, 1994)
Intake diagnoses were assessed using the ADIS– IV–L, a semi-structured interview designed to ascertain reliable diagnosis of the DSM–IV anxiety, mood, somatoform, and substance use disorders. All clinical interviewers were required to complete a rigorous training and certification process in use of this instrument prior to conducting assessments. The ADIS-IV-L has shown excellent inter-rater reliability in previous research (Brown, 2007).
Behavioral Inhibition and Behavioral Activation Scales (BIS/BAS; Carver & White, 1994)
Levels of N/BI and E/BA were assessed using the BIS/BAS, a 20-item self-report measure. These scales were designed to assess two temperaments identified in Gray's (1987) biobehavioral theory of emotion, namely behavioral inhibition and behavioral activation. Seven BIS subscale items tap into individuals’ emotional responses to impending negative events (e.g., “I feel worried when I think I have done poorly at something important”). Thirteen BAS items assess individuals’ behavioral and emotional responses to potentially positive events (e.g., “When I get something I want, I feel excited or energized”). Participants are asked to respond to each item using a 4-point Likert scale ranging from 1 (quite untrue of you) to 4 (quite true of you). Empirically, the BIS/BAS exhibit stronger associations with other measures of temperament (i.e., neuroticism/negative affectivity and extraversion/positive affectivity, respectively) than with measures of anxiety or depressive disorder constructs, suggesting they have good convergent and discriminant validity as indicators of temperament (Campbell-Sills, Liverant, & Brown, 2004). Additionally, the BIS/BAS has demonstrated good reliability in a large sample of individuals with emotional disorders (α = .73 to .92; Campbell-Sills et al., 2004).
Hamilton Anxiety Rating Scale (HAM-A; Hamilton, 1959)
The HAM-A, administered with the Structured Interview Guide for the Hamilton Anxiety Rating Scale (SIGH-A; Shear et al., 2001), was used to measure general symptoms of anxiety. The SIGH-A has shown excellent inter-rater reliability (r = .99), test-retest reliability (r = .89), and internal consistency (α = .82; Shear et al., 2001).
Hamilton Depression Rating Scale (HAM-D; Hamilton, 1960)
The HAM-D, administered with the Structured Interview Guide for the Hamilton Depression Ratings Scale (SIGH-D; Williams, 1988), was assessed general depressive symptoms. The SIGH-D has evidenced good reliability in previous studies (r = .82; Williams, 1988).
Quality of Life Inventory (QOLI; Frisch, 1994)
The QOLI is a 32-item measure of life satisfaction, well-being, and positive mental health. This scale assesses life satisfaction among 16 domains, and also generates a global QOL score (equal to the sum of individual satisfaction ratings, weighted by their importance to the individual). The QOLI demonstrated high internal consistency and 1 month test-retest reliability in a detailed psychometric study of three clinical and three nonclinical samples (all >0.75; Frisch et al., 1992). Research also indicates that the QOLI accurately measures subjective QOL in patients with anxiety and depressive disorders (Frisch et al., 1992; Gladis et al., 1999).
Work and Social Adjustment Scales (WSAS-C, Mundt et al., 2002)
The clinician-rated version of the Work and Social Adjustment Scale was used to measure overall functioning. The WSAS quantifies the interference caused by patients’ symptoms in work, home management, private leisure, social leisure, and family relationships. This measure has shown sensitivity to disorder severity and change related to treatment (Mataix-Cols et al., 2005; Mundt et al., 2002) and acceptable internal consistency in previous research (WSAS-C, α = .70 – 94).
Procedure
The Boston University Institutional Review Board approved all study procedures and all participants provided informed consent. Independent evaluators, blind to treatment condition, administered diagnostic clinical interviews focusing on the current symptomatology of disorders identified at the intake assessment. In the immediate-treatment condition, assessments were conducted at pre-treatment, post-treatment, and at a 6-month follow-up (6MFU) time point. In the delayed-treatment condition, participants were assessed pre- and post-16 week wait-list; for between-condition analyses, the post-waitlist assessment was used as the baseline assessment for the delayed-treatment group. At the end of the 16-week waitlist, delayed-treatment participants immediately received the UP treatment protocol; additional assessments were then conducted at both post-treatment and 6MFU time points.
In the present study, the UP was administered according to a manual (Barlow et al., 2011). The four study therapists included one licensed doctoral-level psychologist with seven years of experience and three doctoral students with two to four years of experience. Adherence to the treatment was closely monitored during the trial through supervision. Maximum treatment duration was 18 one-hour sessions, with patients completing an average of 15.26 sessions of treatment (SD=4.60; Farchione et al., 2012).
Results
The Effects of the Unified Protocol on Temperament
Between-Conditions
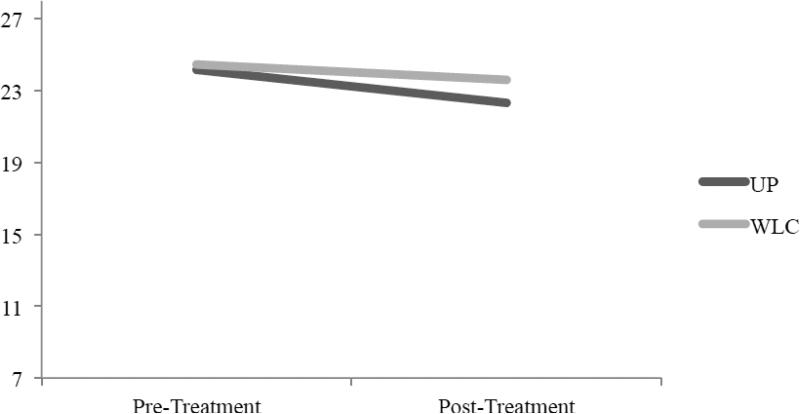
Hedges’ g effect sizes, adjusted for a small sample, were utilized to compare the magnitude of the differences in pre- and post-treatment temperament levels between conditions. As hypothesized, the treatment group (n = 26) exhibited greater decreases in N/BI and increases in E/BA from pre- to post-treatment than the waitlist control group (n=11; see Figures 1 and 2), and these differences were associated with small effect sizes (see Table 1; Cohen [1988] proposed an effect size of 0.2 - 0.3 is “small,” 0.5 is “medium,” and 0.8 and higher is “large.”) These effects were not statistically significant in the present sample. Although the treatment group showed lower N/BI (g = 0.33, 95% CI [−0.42, 1.08]) and higher E/BA (g = − 0.72, 95% CI [−1.48, 0.04]) at post-treatment than the waitlist group, slightly higher N/BI (g = 0.09, 95% CI [−0.38, 1.04]) and moderately lower E/BA (g = −0.42, 95% CI [−1.43, −0.01]) in the waitlist group at pre-treatment contributed to less comparative change between groups from preto post-treatment.
Figure 1.
Mean BIS scores at pre- and post-treatment in the treatment (UP) and waitlist control (WLC) groups. The possible total score range on the BIS measure is 7-28.
Figure 2.
Mean BAS scores at pre- and post-treatment in the treatment (UP) and waitlist control (WLC) groups. The possible total score range on the BAS measure is 13-52.
Table 1.
Between-Condition Descriptive Statistics and Effect Sizes (Hedges’ g)
| Unified Protocol | Waitlist Control | Between Condition Effect Size | Confidence Interval g | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Hedges’ g | SEg | LL | UL | |
| Pre-treatment BIS | 26 | 24.15 | 3.41 | 11 | 24.46 | 2.16 | 0.09 | 0.36 | −0.38 | 1.04 |
| Post-treatment BIS | 22 | 22.32 | 4.15 | 10 | 23.60 | 2.80 | 0.33 | 0.38 | −0.42 | 1.08 |
| Pre-treatment BAS | 26 | 38.09 | 6.55 | 11 | 35.18 | 7.18 | −0.42 | 0.36 | −1.43 | −0.01 |
| Post-treatment BAS | 22 | 40.27 | 5.78 | 10 | 35.40 | 8.13 | −0.72 | 0.39 | −1.48 | 0.04 |
Note. Positive effect sizes denote higher scores in the waitlist condition; negative effect sizes denote higher scores in the UP condition. BIS = Behavioral Inhibition Scale; BAS = Behavioral Activation Scale.
Within-Treatment
Next, intraindividual changes in temperament were examined for a combined group of participants (n = 35) that included both those randomized to immediate treatment (n = 26), as well as waitlist patients who completed the delayed treatment condition following the waitlist phase (n = 9, as 2 participants from the initial 11 in the waitlist condition did not participate in the delayed treatment phase). Standardized Mean Gain effect sizes (ESsg) were used to assess the magnitude of within-participant changes in temperament during treatment. ESsg measures changes in mean scores on a variable over time following a standardized metric, which allows for comparison of change across different outcome variables. As hypothesized, patients receiving treatment with the UP experienced significant decreases in N/BI and increases in E/BA from pre- to post-treatment (see Table 2). Effect sizes for decreases in N/BI (ESsg = 0.51, 95% CI [0.24, 0.78]) and increases in E/BA (ESsg = −0.53, 95% CI [−0.82, −0.24]) were both in the moderate range. Contrary to expectations, levels of N/BI and E/BA did not continue to improve between post-treatment and 6MFU. Rather, results revealed small, non-significant increases in N/BI (ESsg = −0.10, 95% CI [−0.35, 0.15]) and small, significant decreases in E/BA (ESsg = 0.28, 95% CI [0.07, 0.49]) during this time.
Table 2.
Within-Treatment Descriptive Statistics and Effects Sizes (Estimated Standardized Gain ESsg)
| Pre-treatment | Post-treatment | 6-month follow-up | Pre-Post Effect Size | Post-FU Effect Size | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | ESsg | SEsg | LL | UL | ESsg | SEsg | LL | UL | |
| BIS | 36 | 24.00 | 3.23 | 29 | 22.14 | 3.81 | 27 | 22.30 | 3.81 | 0.51 | 0.14 | 0.24 | 0.78 | −0.10 | 0.13 | −0.35 | 0.15 |
| BAS | 36 | 37.35 | 7.01 | 29 | 39.93 | 5.55 | 27 | 38.41 | 6.38 | −0.53 | 0.15 | −0.82 | −0.24 | 0.28 | 0.11 | 0.07 | 0.49 |
Note. Positive effect sizes denote decreases in scores; negative effect sizes denote increases. BIS = Behavioral Inhibition Scale; BAS = Behavioral Activation Scale.
Relationships Between Temperament and Treatment Outcomes
We next utilized multivariate regression to examine the associations between N/BI and E/BA and the specified treatment outcome variables at post-treatment and 6MFU. Results indicated that the dimensions of temperament were associated with both shared and distinct treatment outcomes. Consistent with hypotheses, at post-treatment, N/BI was significantly associated with anxiety (b = .411, p = .023, 95% CI [0.097, 1.23]) and depression (b = .484, p = .005, 95% CI [0.24, 1.21]) such that lower N/BI at post-treatment was associated with lower levels of anxiety and depressive symptoms. These relationships remained significant after accounting for the influence of post-treatment E/BA. E/BA was significantly associated with depressive (b = −.326, p = .049, 95% CI [−0.67, −0.00]) but not anxiety (b = −.260, p = .139, 95% CI [−0.68, 0.10]) symptoms. Separately N/BI and E/BA accounted for 24.6% and 11.8%, respectively, of the total variance in post-treatment depressive symptoms, while together the temperament predictors explained 35.2% of such variance. E/BA was not a significant predictor of anxiety symptoms at post-treatment either with or without N/BI included as a covariate. N/BI and E/BA together accounted for 24.4% of the total variance in post-treatment anxiety symptoms, and independently explained 17.7% and 7.6% of total variance, respectively.
With regard to broader treatment outcomes, higher E/BA, but not lower N/BI, was associated with higher quality of life at post-treatment (b = .446, p = .014, 95% CI [0.03, 0.22]; b = −.293, p = .095, 95% CI [−0.26, 0.02], respectively). Combined N/BI and E/BA contributed to 29% of the total variance in post-treatment quality of life; separately these predictors accounted for 9.2% and 20.5%, respectively, of such variance. Neither N/BI nor E/BA was a significant predictor of functional impairment at post-treatment (b = .115, p = .545, 95% CI [−0.45, 0.83]; b = −.255, p = .186, 95% CI [−0.73, 0.15], respectively).
At the 6MFU assessment, most of the post-treatment associations between dimensions of temperament and treatment outcomes remained the same as at post-treatment, although there were a few notable changes. Lower N/BI remained a significant predictor of lower anxiety (b = .404, p = .026, 95% CI [0.08, 1.14]) and depressive (b = .379, p = .044, 95% CI [0.07, 1.09]) symptoms. Higher E/BA exhibited stronger associations with lower anxiety symptoms (b = −.431, p = .018, 95% CI [−0.71, −0.07]) and a weaker association with lower depressive symptoms (b = −.353, p = .06, 95% CI [−0.63, 0.01]) at the 6MFU compared with post-treatment, although these changes were not significantly different based on 95% confidence intervals. Independently N/BI and E/BA accounted for 13.1% and 15.3%, respectively, of the total variance in anxiety symptoms at 6MFU; together they explained 31.5% of such variance. Separately, N/BI and E/BA contributed to 11.9% and 10%, respectively, of the total variance in depressive symptoms at 6MFU, while combined they accounted for 24.2% of variance.
At the 6MFU, higher E/BA, but not lower N/BI, was uniquely associated with higher quality of life (b = .635, p = .000, 95% CI [0.09, 0.28]; b = −.201, p = .211, 95% CI [−0.25, 0.06], respectively), which was similar to the results at post-treatment. N/BI and E/BA independently accounted for 1.9% and 37.8%, respectively, of the total variance in quality of life at 6MFU; together these predictors explained 41.9% of such variance. Notably, both lower N/BI and higher E/BA were associated with lower functional impairment at the 6MFU (b = .499, p = .005, 95% CI [0.21, 1.08]; b = −.413, p = .017, 95% CI [−0.58, −0.06], respectively). N/BI and E/BA together explained 37.9% of the total variance in functional impairment outcomes at the 6MFU; separately N/BI and E/BA accounted for 21% and 13.3%, respectively, of such variance.
Discussion
Previous research investigating the effects of psychological treatments for emotional disorders on dimensions of temperament in adults has not featured interventions that have been designed to target core temperamental dimensions. The present results provide preliminary insights into the malleability of temperament in response to treatment with the UP (Barlow et al., 2011), a CBT intervention focused on core temperamental processes, and the impact of changes in temperament on other important treatment outcome variables.
Treatment-related Changes in Temperament
Between-group comparisons revealed greater decreases in N/BI and increases in E/BA at post-treatment in the UP treatment versus waitlist group, although these were associated with small, non-significant effect sizes. Within-participants analyses indicated that, on average, patients receiving treatment achieved moderate decreases in N/BI and increases in E/BA from pre- to post-treatment. Patients exhibited slight losses in such gains between post-treatment and the 6MFU, especially for E/BA. These results suggest that treatment with the UP facilitates improvement in both N/BI and E/BA temperaments, with more stable change shown in N/BI. Although N/BI and E/BA are generally believed to include a moderate degree of mood-state distortion (i.e., conflation of “true” temperamental variance with state dependent variance influenced by current mood or distress; Clark, Vittengl, Kraft & Jarrett, 2003), results from a recent study suggest that these measures primarily capture true temperamental variance even in individuals with emotional disorders (Naragon-Gainey et al., 2013). Thus, although the temperamental changes observed in the present study are small to moderate in magnitude, Naragon-Gainey et al.'s findings suggest that these changes may reflect a substantial degree of actual change in temperament versus solely a reduction in state levels of distress. Nevertheless, it will be important for larger, similar studies in the future to partial out state variance, and evaluate this hypothesis empirically given inconsistencies in the previous literature (e.g., Clark et al., 2003; Naragon-Gainey et al., 2003). It will also be crucial to conduct more robust and fine-grained analyses of the temperamental changes occurring over the follow-up period. It was somewhat surprising that the post-treatment changes in N/BI and E/BA were not maintained at the 6MFU; however, it is unclear whether this was an artifact of the small sample, or whether there are other reasons for the slight loss in gains. One hypothesis is that producing durable changes in temperament will require a greater number of treatment sessions than the standard courses of CBT (i.e., 12- 18 sessions). But more research is needed. In summary, the present findings provide general support for the hypothesis that temperamental constructs can be targeted and modified within treatment, and specifically within a psychological treatment framework.
Although the present results are preliminary, they have important implications for anxiety and depressive disorder treatment research. To our knowledge, no previous studies have investigated psychological treatments specifically designed to address temperament-based risk factors in anxious adults. This study suggests that the UP, a psychological treatment that targets core processes of temperament, may facilitate beneficial changes in two dimensions of temperament, which in turn are associated with improvements in a range of treatment outcomes. As temperament is considered a key vulnerability factor for the development of emotional disorders, the ability to therapeutically modify temperament has the potential not only to ameliorate current symptoms, but also to decrease susceptibility to future episodes of disorder. Furthermore, although the present study involved patients diagnosed with current anxiety disorders, our findings in conjunction with prospective data identifying elevated N/BI as a risk factor for subsequent emotional disorders (e.g., Hirshfeld-Becker et al., 2007; Zinbarg et al., in preparation) support the need for early interventions aimed at decreasing vulnerability in at-risk individuals. Of course, further systematic research is necessary to confirm these hypotheses.
Effects of Changes in Temperament on Treatment Outcomes
Treatment-related changes in temperament dimensions were associated with a number of important outcomes at post-treatment and 6MFU. Consistent with predictions, lower N/BI was associated with significantly lower anxiety and depressive symptoms at post-treatment and 6MFU. Although N/BI was not a significant predictor of functional impairment at post-treatment, it was at 6MFU. Counter to predictions, N/BI was not associated with quality of life at either post-treatment or 6MFU. It may be that by these time-points following treatment, N/BI had declined to a level in which it was not substantially impacting quality of life, whereas at higher levels earlier in the course of illness it may have exerted a more direct, negative effect on quality of life. This interpretation may be consistent with research suggesting that N/BI is minimally, if at all, inversely correlated with positive outcomes except when it reaches higher levels where it appears to inhibit positive emotion (Williams, Peeters, & Zautra, 2004).
Based on prior research supporting a specific association between E/BA and depression, and to a lesser extent also between E/BA and social anxiety (Brown, 2007; Brown & Barlow, 2009; Watson & Naragon-Gainey, 2010), we expected that increases in E/BA would be associated most strongly lower depressive symptoms. With regard to this hypothesis, our data yielded mixed findings. At post-treatment, higher E/BA was associated with lower depressive but not anxiety symptoms, while, at 6MFU, higher E/BA was associated with lower anxiety but not depressive symptoms. Similarly, E/BA was not significantly associated with functional impairment at post-treatment, but was at 6MFU. The relatively small sample size of the study may have contributed to these variations, and therefore it will be important to examine these associations within a larger sample in future research.
The specific effects of E/BA on quality of life are also noteworthy. Higher E/BA was associated with higher quality of life at both post-treatment and 6MFU, and contributed to a large portion of the variance (20.5%-37.8%) in quality of life outcomes. These findings suggest that E/BA deserves greater exploration as a possible treatment target for improving quality of life. This is consistent with the theory that higher E/BA confers a specific sensitivity to rewards (versus N/BI to threat) that then results in greater pursuit of positive goals and more frequent experience of positive emotions (Gray, 1991; Lucas, Diener, Grob, Suh, & Shao, 2000). Extensive findings in the personality literature support this theory, showing that higher E/BA reliably predicts greater quality of life and well-being across individuals and life contexts (Diener, Oishi, & Lucas, 2003; Diener, Suh, Lucas, & Smith, 1999). Nevertheless, there is minimal research examining E/BA as a mediator of quality of life in the context of treatment, which seems a promising avenue for investigation. These results in combination with the finding that N/BI was not associated with quality of life at post-treatment or follow-up in the present study further suggest the unique role of E/BA with regard to improving quality of life.
The present findings may be important to consider when conducting future clinical studies given that previous treatment research has focused primarily on the relationship between E/BA and depression, but not with anxiety, functional impairment, and quality of life. Greater attention to E/BA-related processes, including positive emotions, sociability, and approach behaviors, may incrementally enhance acute and long-term treatment outcomes in anxiety and mood disorders (Carl et al., 2013; Ehrenreich, Fairholme, Buzzella, Ellard, & Barlow, 2007), and these preliminary findings support such a hypothesis.
Limitations and Future Directions
This study has several limitations that will be important to address in future research. For one, the study's small sample size limits the precision of the reported effect sizes. A larger study with greater statistical power is needed to obtain more precise estimates of the effects of treatment on temperamental variables. In addition, the small sample size and limited number of assessment time-points did not allow us to control for potential bidirectional effects between changes in symptoms and temperaments. However, notably, results from Naragon-Gainey et al.'s (2013) recent study provide empirical support for our conceptualization that there is a primary effect of temperamental changes on symptom improvement (i.e., pathoplastic model) rather than vice versa. Nevertheless, future research entailing modeling of interactions between symptoms and temperament variables during and following treatment is needed to evaluate the precise directional effects.
Despite these important limitations, the present study marks the first evaluation of the effects of a psychological treatment targeting dimensions of temperament in adults with emotional disorders. The results of this preliminary study indicate that even in a small sample the UP may exert meaningful effects on temperamental dimensions and that these effects are associated with a range of beneficial treatment outcomes. These findings support the need for future research to further evaluate the effects of temperament-focused interventions on temperamental variables and treatment outcomes.
Acknowledgements
This research was supported by a NIMH grant awarded to Dr. David H. Barlow (R34-MH070693).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allport G. Personality: A psychologic interpretation. Holt; New York: 1937. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Author; Washington, DC: 2000. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. Guilford Press; New York: 2002. [Google Scholar]
- Barlow DH, Ellard KK, Fairholme CP, Farchione TJ, Boisseau CL, Allen LB, Ehrenreich-May J. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Client Workbook. Oxford University Press; New York: 2011. [Google Scholar]
- Barlow DH, Sauer-Zavala SE, Carl JR, Ellard KK, Bullis JR. The origins and treatment of neuroticism. Manuscript in preparation. 2013 [Google Scholar]
- Brown TA. Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of Abnormal Psychology. 2007;116:313–328. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Brown T, Barlow D. A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment. 2009;21:256–271. doi: 10.1037/a0016608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, Liverant GI, Brown TA. Psychometric evaluation of the behavioral inhibition/behavioral activation scales in a large sample of outpatients with anxiety and mood disorders. Psychological Assessment. 2004;16:244–254. doi: 10.1037/1040-3590.16.3.244. [DOI] [PubMed] [Google Scholar]
- Carl JR, Soskin DP, Kerns C, Barlow DH. Positive emotion regulation in emotional disorders: A theoretical review. Clinical Psychology Review. 2013;33(3):343–360. doi: 10.1016/j.cpr.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. Journal of Personality and Social Psychology. 1994;67(2):319–333. [Google Scholar]
- Clark LA, Vittengl J, Kraft D, Jarrett RB. Separate personality traits from states to predict depression. Journal of Personality Disorders. 2003;17(2):152. doi: 10.1521/pedi.17.2.152.23990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;103:103–116. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Temperament: A new paradigm for trait psychology. In: Pervin LA, John OP, editors. Handbook of personality. 2nd ed. Guilford Press; New York: 1999. pp. 399–423. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates; New Jersey: 1988. [Google Scholar]
- Diener E, Oishi S, Lucas RE. Personality, culture, and subjective well-being: Emotional and cognitive evaluations of life. Annual Review of Psychology. 2003;54(1):403–425. doi: 10.1146/annurev.psych.54.101601.145056. [DOI] [PubMed] [Google Scholar]
- Diener E, Suh EM, Lucas RE, Smith HL. Subjective well-being: Three decades of progress. Psychological Bulletin. 1999;125(2):276. [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM–IV–Lifetime version. Graywind Publications; Albany, NY: 1994. [Google Scholar]
- Dockray S, Steptoe A. Positive affect and psychobiological processes. Neuroscience and Biobehavioral Reviews. 2010;35:69–75. doi: 10.1016/j.neubiorev.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice. 2010;17(1):88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrenreich JT, Fairholme CP, Buzzella BA, Ellard KK, Barlow DH. The role of emotion in psychological therapy. Clinical Psychology: Science and Practice. 2007;14(4):422–428. doi: 10.1111/j.1468-2850.2007.00102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck HJ. Dimensions of personality. Kegan Paul; Oxford, UK: 1947. [Google Scholar]
- Eysenck HJ. The biological basis of personality. Thomas; Springfield, IL: 1967. [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, Gallagher MW, Barlow DH. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: A randomized controlled trial. Behavior Therapy. 2012;43(3):666–678. doi: 10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisch MB. Quality of Life Inventory: Manual and treatment guide. National Computer Systems; Minneapolis, MN: 1994. [Google Scholar]
- Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. Clinical validation of the Quality of Life Inventory: A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment. 1992;4:92–101. [Google Scholar]
- Fu CH, Williams SC, Cleare AJ, Brammer MJ, Walsh ND, Kim J, Bullmore ET. Attenuation of the neural response to sad faces in major depression by antidepressant treatment: A prospective, event-related functional magnetic resonance imaging study. Archives of General Psychiatry. 2004;61:877–889. doi: 10.1001/archpsyc.61.9.877. [DOI] [PubMed] [Google Scholar]
- Garland EL, Fredrickson B, Kring AM, Johnson DP, Meyer PS, Penn DL. Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review. 2010;30(7):849–864. doi: 10.1016/j.cpr.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershuny B, Sher K. The relation between personality and anxiety: Findings from a 3-year prospective study. Journal of Abnormal Psychology. 1998;107:252–262. doi: 10.1037//0021-843x.107.2.252. [DOI] [PubMed] [Google Scholar]
- Gladis MM, Gosch EA, Dishuk NM, Crits-Cristoph P. Quality of life: Expanding the scope of clinical significance. Journal of Consulting and Clinical Psychology. 1999;67:320–321. doi: 10.1037//0022-006x.67.3.320. [DOI] [PubMed] [Google Scholar]
- Goldberg L. The structure of phenotypic personality traits. American Psychologist. 1993;48:26–34. doi: 10.1037//0003-066x.48.1.26. [DOI] [PubMed] [Google Scholar]
- Gray JA. The psychology of fear and stress. Cambridge University; Cambridge, UK: 1987. [Google Scholar]
- Gray JA. Neural systems, emotion, and personality. In: Madden J IV, editor. Neurobiology of learning, emotion, and affect. Raven Press; New York: 1991. pp. 273–306. [Google Scholar]
- Gruber J, Johnson SL, Oveis C, Keltner D. Risk for mania and positive emotional responding: Too much of a good thing? Emotion. 2008;8(1):23–33. doi: 10.1037/1528-3542.8.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, & Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmer CJ, O'Sullivan U, Favaron E, Massey-Chase R, Ayres R, Reinecke A, Cowen PJ. Effect of acute antidepressant administration on negative affective bias in depressed patients. American Journal of Psychiatry. 2009;166:1178–1184. doi: 10.1176/appi.ajp.2009.09020149. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Davis S, Harrington K, Rosenbaum JF. Behavioral inhibition in preschool children at risk is a specific predictor of middle childhood social anxiety: A five-year follow-up. Journal of Developmental & Behavioral Pediatrics. 2007;28:225–233. doi: 10.1097/01.DBP.0000268559.34463.d0. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Gruber J, Eisner LR. Emotion and Bipolar Disorder. In: Rottenberg J, Johnson SL, editors. Emotion and psychopathology: Bridging affective and clinical science. American Psychological Association; Washington, DC: 2007. pp. 123–150. [Google Scholar]
- Jorm AF, Christensen H, Henderson AS, Jacomb PA, Korten AE, Rodgers B. Using the BIS/BAS scales to measure behavioural inhibition and behavioural activation: Factor structure, validity and norms in a large community sample. Personality and Individual Differences. 1998;26(1):49–58. [Google Scholar]
- Kasch K, Rottenberg J, Arnow B, Gotlib I. Behavioral activation and inhibition symptoms and the severity and course of depression. Journal of Abnormal Psychology. 2002;111(4):589–597. doi: 10.1037//0021-843x.111.4.589. [DOI] [PubMed] [Google Scholar]
- Kennedy SJ, Rapee RM, Edwards SL. A selective intervention program for inhibited preschool-aged children of parents with an anxiety disorder: Effects on current anxiety disorders and temperament. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(6):602–609. doi: 10.1097/CHI.0b013e31819f6fa9. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Cox BJ, Green JG, Ormel J, McLaughlin KA, Merikangas KR, Zaslavsky AM. The effects of latent variables in the development of comorbidity among common mental disorders. Depression and Anxiety. 2011;28(1):29–39. doi: 10.1002/da.20760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Gámez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Krueger R. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Lucas RE, Diener E, Grob A, Suh EM, Shao L. Cross-cultural evidence for the fundamental features of extraversion. Journal of Personality and Social Psychology. 2000;79(3):452. doi: 10.1037//0022-3514.79.3.452. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Cowley AJ, Hankins M, Schneider A, Bachofen M, Kenwright M, Marks IM. Reliability and validity of the work and social adjustment scale in phobic disorders. Comprehensive Psychiatry. 2005;46(3):223–228. doi: 10.1016/j.comppsych.2004.08.007. [DOI] [PubMed] [Google Scholar]
- McCabe C, Mishor Z, Cowen PJ, Harmer CJ. Diminished neural processing of aversive and rewarding stimuli during selective serotonin reuptake inhibitor treatment. Biological Psychiatry. 2010;67:439–445. doi: 10.1016/j.biopsych.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae RR, Costa PT. Validation of the Five-Factor Model of personality across instruments and observers. Journal of Personality and Social Psychology. 1987;52(1):81–90. doi: 10.1037//0022-3514.52.1.81. [DOI] [PubMed] [Google Scholar]
- Mundt JC, Marks IM, Shear MK, Greist JM. The work and social adjustment scale: A simple measure of impairment in functioning. British Journal of Psychiatry. 2002;180:461–464. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, Gallagher MW, Brown TA. Stable “trait” variance of temperament as a predictor of the temporal course of depression and social phobia. Journal of Abnormal Psychology. 2013;122(3):611. doi: 10.1037/a0032997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Kennedy S, Ingram M, Edwards S, Sweeney L. Prevention and early intervention of anxiety disorders in inhibited preschool children. Journal of Consulting and Clinical Psychology. 2005;73(3):488–497. doi: 10.1037/0022-006X.73.3.488. [DOI] [PubMed] [Google Scholar]
- Rosellini AJ, Lawrence AE, Meyer JF, Brown TA. The effects of extraverted temperament on agoraphobia in panic disorder. Journal of Abnormal Psychology. 2010;119:420–426. doi: 10.1037/a0018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear MK, Vander Bilt J, Rucci P. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A). Depression & Anxiety. 2001;13(4):166–178. [PubMed] [Google Scholar]
- Soskin DP, Carl JR, Alpert J, Fava M. Antidepressant effects on emotional temperament: Toward a biobehavioral research paradigm for major depressive disorder. CNS Neuroscience & Therapeutics. 2012;18(6):441–51. doi: 10.1111/j.1755-5949.2012.00318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang T, DeRubeis R, Hollon S, Amsterdam J, Shelton R, Schalet B. Personality change during depression treatment: A placebo controlled trial. Archives of General Psychiatry. 2009;66:1322–1330. doi: 10.1001/archgenpsychiatry.2009.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomarken AJ, Dichter GS, Freid C, Addington S, Shelton RC. Assessing the effects of bupropion SR on mood dimensions of depression. Journal of Affective Disorders. 2004;78:235–241. doi: 10.1016/S0165-0327(02)00306-3. [DOI] [PubMed] [Google Scholar]
- Trull T, Sher K. Relationship between the Five-Factor Model of Personality and Axis I disorders in a non-clinical sample. Journal of Abnormal Psychology. 1994;103:350–360. doi: 10.1037//0021-843x.103.2.350. [DOI] [PubMed] [Google Scholar]
- Watson D, Naragon-Gainey K. On the specificity of positive emotional dysfunction in psychopathology: Evidence from the mood and anxiety disorders and schizophrenia/schizotypy. Clinical Psychology Review. 2010;30(7):839–848. doi: 10.1016/j.cpr.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- Williams J, Peeters F, Zautra A. Differential affect structure in depressive and anxiety disorders. Anxiety, Stress & Coping: An International Journal. 2004;17(4):321–330. [Google Scholar]
- Zinbarg R, Mineka S, Craske M, Griffith J, Vrshek-Schallhorn S, Wolitzky-Taylor KB, Epstein A. Prospective associations of personality traits and cognitive vulnerabilities with diagnoses of emotional disorders over three years in adolescents. in preparation. [Google Scholar]