Abstract
Objective
Explore alcohol involvement trajectories and associated factors during the year post-high school (HS) graduation among emerging adults with type 1 diabetes.
Methods
Youth (N=181) self-reported alcohol use at baseline and every 3 months for 1 year post-HS graduation. Data were also collected on parent-youth conflict, diabetes self-efficacy, major life events, living and educational situations, diabetes management, marijuana use, cigarette smoking, and glycemic control. Trajectories of alcohol use were modeled using latent class growth analysis. Associations between trajectory class and specific salient variables were examined using analysis of variance, chi square, or generalized linear mixed model, as appropriate.
Results
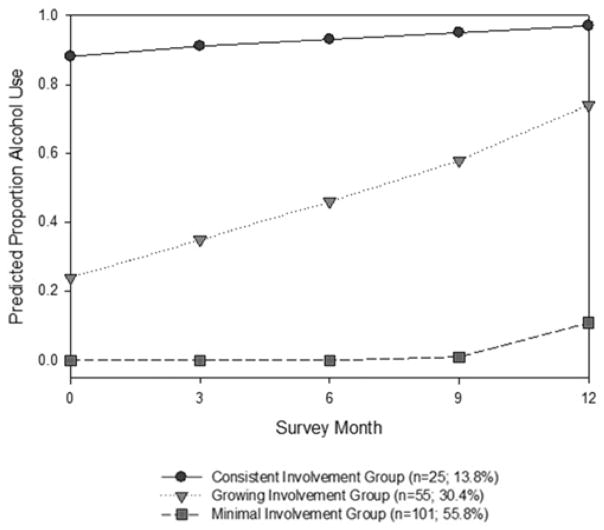
Identified alcohol involvement trajectory classes were labeled as: 1) Consistent Involvement Group (n=25, 13.8%) with stable, high use relative to other groups over the 12 months; 2) Growing Involvement Group (n=55, 30.4%) with increasing use throughout the 12 months; and 3) Minimal Involvement Group (n=101, 55.8%) with essentially no involvement until month nine. Those with minimal involvement had the best diabetes management and better diabetes self-efficacy than those with consistent involvement. In comparison to those minimally involved, those with growing involvement were more likely to live independently of parents; those consistently involved had more major life events; and both the growing and consistent involvement groups were more likely to have tried marijuana and cigarettes.
Conclusions
This sample of emerging adults with type 1 diabetes has 3 unique patterns of alcohol use during the first year after high school.
Implication and Contribution
Among youth with type 1 diabetes in the year post-HS graduation, alcohol involvement knowledge was extended by identifying patterns of such use. Further research of alcohol use patterns is needed to guide health care professionals in their assessments and researchers in testing interventions that target unique patterns.
Keywords: alcohol involvement, emerging adults, diabetes
Youth with type 1 diabetes use alcohol [1] and may be similar to their emerging adult peers who use alcohol more than other age groups [2]. Arnett [2] hypothesizes that emerging adults’ substance use may be associated with the freedom to experiment with substances as part of seeking their identity, the lack of expectations for adult behavior, the lack of perceptions of substance use consequences, and self-medication in response to the stress of the many changes in their life, confusion about their identity and/or pessimism about their future. Congruent with various underlying reasons for alcohol use, experts have described patterns such as “abstainers”, “light drinkers” and “very heavy drinkers” among youth in the general population [3]. However, a paucity of research exists on alcohol use patterns among those with diabetes. Some could be abstainers, especially if they are methodical managers of their diabetes [4], who likely would not want to risk severe hypoglycemic events and poor glycemic control, known to be associated with alcohol use [5]. Others could be light drinkers who feel free to experiment with alcohol use. Finally, some could be relatively heavy drinkers who are self-medicating with alcohol in response to stress.
Identification of factors that discriminate various patterns of alcohol use is essential to intervene with individuals with various underlying reasons for alcohol use [3]. Congruent with salient behavioral, social, psychological and socio-demographic factors noted for the general population [3], alcohol use among emerging adults with type 1 diabetes is proposed to be associated with environmental and individual characteristics, transitional events, other health behaviors, and health outcomes [6]. Examination of such factors during the year after high school (HS) graduation would be important because it is known as a critical year for substance use [7]. Salient environmental characteristics during this time period include relationships with parents such as parent-youth conflict [8]; individual characteristics of diabetes-specific self-efficacy [9]; health behaviors that are diabetes-related such as diabetes management [10] and typical youth behaviors such as marijuana use and cigarette smoking [11]; the health outcome of glycemic control [10]; and life events, major ones such as deaths and divorce in the family [12] and ones specific to this age group, such as moving out of parental homes, and enrolling in school [13].
An examination of alcohol involvement trajectories and associated factors would increase understanding of these youth’s alcohol use, guiding development of interventions specific for unique patterns. An exploratory study of emerging adults with type 1 diabetes during the first year post-HS was conducted to: 1) identify alcohol involvement trajectories and 2) examine associations between the identified trajectories and environmental characteristics (parent-youth conflict), individual characteristics (diabetes-self-efficacy), health behaviors (diabetes management, marijuana use, and cigarette smoking), health outcomes (glycemic control), and life events (major life events, living independently of parents and school enrollment) as well as socio-demographic and diabetes-related factors.
Methods
Design
To control for the transitional event of HS graduation and the year after, a critical time for substance use [7], this report is of 181 HS graduates out of 204 participants from a larger exploratory-descriptive longitudinal study. The larger study, described elsewhere [14–18], described changes in salient outcomes in the contexts of education and living situations and examined key factors associated with specified outcomes during the transitional time of emerging adulthood. This transition has been little explored, yet extremely important for youth with type 1 diabetes who are expected to assume diabetes care responsibility [19] and known to have poor glycemic control [5].
Procedures
This Institutional Review Board-approved study obtained consents from youth 18 years of age or older and parental consent/youth assent from those less than 18 years of age. HS seniors with type 1 diabetes were recruited in 4 consecutive years from outpatient clinics providing diabetes care in the Midwest. Study information was sent to a potential pool of 17–19 year-olds with type 1 diabetes. Study staff screened interested youth for: being 17–19 years of age and in the last 6 months of HS; diagnosed with type 1 diabetes for at least one year; ability to speak and read English; living with their parent or guardian; and being without a serious psychiatric disorder or a second chronic illness that would interfere with becoming independent. Only 3% of participants were permanently lost to follow-up (3 requested to be withdrawn, 2 died, and 2 were lost to contact by staff after 6 or 9-month data collection points). Participants who missed a data collection point were not considered withdrawn because they often completed later data collection points.
Data Collection
Youth self-completed questionnaires via the format of their choice (Web-based system or paper and pencil). Baseline-only data included socio-demographics and diabetes-related information. Data collected at baseline and every 3 months over the 12 months post-HS graduation included parent-youth conflict, diabetes self-efficacy, major life events, living situation, school enrollment, diabetes management, marijuana use, cigarette smoking, alcohol use, and glycemic control. Glycemic control values were obtained from the medical records of their health care providers and were, on average, within 41.8 days (SD=48.7) of the completion of questionnaires.
Socio-demographic and Diabetes-related Information
Data were collected on gender, mother’s and father’s education level, years with diabetes diagnosis and method of insulin administration, either continuous subcutaneous insulin infusion (CSII) or multiple daily injections (MDI). Because only a few of the mothers (n = 7) and fathers (n = 8) had less than a HS education, these data were collapsed to college or no-college categories.
Environmental Characteristics
Parent-Youth Conflict was measured by the 15-item Parent-Adolescent Diabetes Conflict Scale, with known reliability and validity [20]. Although a revised scale exists [21], the version used was the one available at initiation of the study. Participants were asked the frequency of arguments around diabetes management over the last 3 months from 1 (never) to 5 (all the time). Responses were summed for a total score (potential range from 15–75), with higher scores reflecting greater conflict. The Cronbach coefficient was .94.
Individual Characteristics
Diabetes-specific Self-efficacy was measured by a revised 8-item Diabetes Self-efficacy Scale [22], an assessment of confidence in one’s ability to perform diabetes management tasks. Revisions involved addition of an item differentiating hypoglycemia and hyperglycemia management and to better reflecting contemporary treatment. Participants were asked how well they could do the tasks, grading themselves from an “A+” (could not do better) to an “F” (you are a disaster). A summed total score was calculated (potential scores ranging from 8–72), with higher scores indicating better self-efficacy. The Cronbach alpha value was 0.84.
Health Behaviors
Diabetes Management was measured by the study-devised 24-item Emerging Adult Diabetes Management Self-Report. This measure is an adaptation of the Diabetes Self-Management Profile (DSMP) [23] from an interview format to self-completion on a Web-based program. Participants noted how often they had performed and made changes in diabetes management tasks in the last 3 months. The summed total score could range from 0–84, with higher scores indicating better management. The Cronbach alpha coefficient was .81.
Alcohol Use, Marijuana use, and Cigarette Smoking were measured in terms of the last 3 months with items from the Health Behavior Questionnaire [24], with binge drinking being 5+ drinks for males and 4+ drinks for females [25]. Participants were first asked about drinking frequency from not at all, once or twice in past 3 months, 2–3 times in past 3 months, about once a month, 2 or 3 days a month, once a week, 2 or 3 days a week, 4 or 5 days a week, and every day. If participants had had a drink, they were asked questions on binge drinking, getting drunk, and quantity consumed. Participants were first asked if they had ever tried marijuana, with potential responses being never, yes once, and yes more than once. If participants had ever tried marijuana, they were asked questions on frequency of marijuana use. Participants were first asked if they had ever smoked a cigarette, with potential responses being never, yes only once, yes a few times, and yes more than a few times. If participants had ever smoked a cigarette, they were asked questions on the quantity smoked.
Responses to the questions on alcohol use frequency, ever tried marijuana and ever smoked cigarette were respectively dichotomized into: being involved in alcohol use or not, ever tried or not tried marijuana, and ever or never smoked cigarettes at each time point. These data were dichotomized because 70–78% of participants responded that they were not involved when asked the initial questions on alcohol use frequency, ever tried marijuana and ever smoked cigarette. Only a minority responded to follow-up questions on binge drinking, getting drunk, quantity consumed, frequency of marijuana use and quantity of cigarettes smoked.
Health Outcome
Glycemic control (HbA1c) was obtained from medical records of the youth’s health care providers. To control for differing assay methods used by providers, adjusted HbA1c values were calculated by taking the original HbA1c value and subtracting the assay-specific bias value per the College of American Pathologists [26].
Life Events
Major Life Events were measured by the Losses and Transition Subscales of the Adolescent-Family Inventory of Life Events & Changes, with documented test-retest reliability of .80–.82 [27]. Participants were asked 12 months after enrollment to note yes or no if specific life events such as a death, divorce and marriage had occurred in their family in the last 12 months. The total numbers of losses and transition events were summed for a total score.
Living Independently of Parents and School Enrollment were study-devised questions about with whom they lived (parents, friends, boyfriend or girlfriend, college roommate, alone, or relatives) and their current educational situation in relation to HS (graduated, dropped out, or repeating last year), General Education Diploma/General Equivalency Degree (GED) (working on or completed), and enrollment in school (not enrolled, vocational school, 2-year college, or 4-year college). Living situation and school enrollment were dichotomized as either living independent of parents or not and whether or not they were enrolled in school or not after HS graduation/completion of a GED.
Statistical Analysis
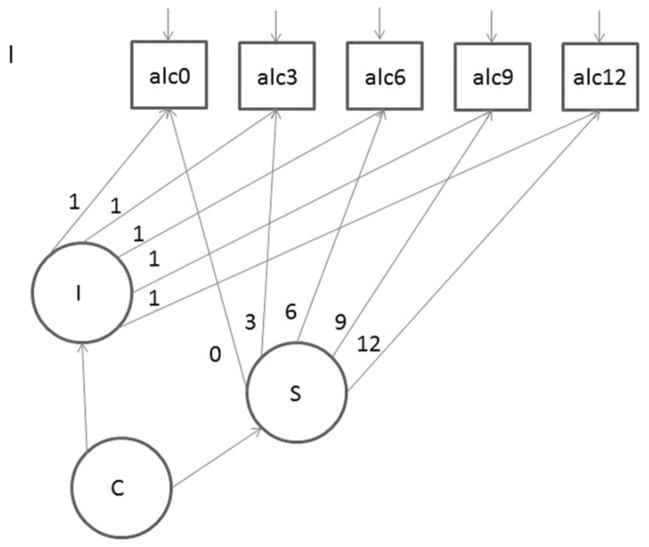
The trajectory of alcohol involvement was modeled using latent class growth analysis [28] using methods implemented in MPLUS version 5.2 [29]. Specifically, alcohol involvement (No/Yes) at each of the time points (graduation through 12 months post-graduation) was modeled. Longitudinal growth mixture models were used to identify latent classes (or participant groups) defined by trajectories of the alcohol involvement. See Figure 1 for a diagram of the model. Mplus software [29] was used to estimate model with full-information maximum likelihood estimation and the MLR estimator (robust standard errors). Intercept and linear slope growth factors were included. To match the timing of the interviews, fixed time scores were used at 0, 3, 6, 9, and 12 months with the intercept of the model set at baseline (time=0). Model selection information and classification diagnostics [30] appear in Table 1. Model selection began by specifying a single latent class, then 2 classes, 3 classes and so on. Determination of a final model was based on smallest BIC value, a non-significant Lo-Mendell-Rubin test, good entropy (>.70) and conceptual judgment. Associations between latent class and selected baseline-measured variables were tested using analysis of variance (ANOVA) or contingency tables with chi squared for continuous and nominal variables, respectively. General linear mixed models (GLMM) were used to test associations between latent alcohol involvement classes and selected dependent variables over repeated measurement points, using each possible value from each visit; thus, although time itself was not used in the analysis, the repeated measures gave a mean value for each participant. Generalized estimating equation (GEE) models were used to test associations between latent alcohol involvement class and selected dichotomous variables over repeated measurement points [31]. Statistically significant (P < .05) overall tests were followed up with post-hoc paired comparisons to identify patterns of differences between latent classes. All variables were examined to ensure that analytic assumptions were met. Descriptive, ANOVA, GLMM, and GEE analyses were performed using SAS v9.3 [32].
Figure 1. Path diagram for latent class growth model.
Latent variables are indicated by circles: I = intercept factor; S=slope factor; C=categorical class factor. Observed alcohol use indicators at each time point are shown by squares: alc0=baseline; alc3=3mo; alc6=6mo; alc9=9mo; alc12=12mo.
Table 1.
Model selection information and classification diagnostics for 3-class model.
| Number of Classes | BIC | Entropy | LMR pval | ||||
|---|---|---|---|---|---|---|---|
| 2 | 712.904 | 0.851 | p=0.0000 | ||||
| 3 Class 1 Class 2 Class 3 |
708.658 | 0.755 | p=0.0009 |
π̂k (CI95) 0.319 (0.28, 0.36) 0.163 (0.13, 0.20) 0.517 (0.50, 0.53) |
mcaPk 0.304 0.138 0.558 |
AvePPk 0.850 0.900 0.914 |
OCCk 12.10 46.21 57.07 |
| 4 | 720.237 | 0.753 | p=0.0874 | ||||
BIC = Bayes Information Criterion
LMR = Lo-Mendell-Rubin test.
π̂k = Model-predicted proportion in Class k; CI is bias-corrected bootstrap value.
mcaPk = Modal class assignment proportion for class k.
AvePPk = Average Posterior Class Probability.
OCCk = Odds of correct classification ratio for class k.
Results
Sample Characteristics
The 181 youth for this report were HS graduates for whom we had alcohol use data. At baseline, they were, on average 18.3 (SD = 0.4) years old, were predominately white (93%), 44% were male and 56% females, most lived in homes with married parents (64%), and less than 5% of parents had less than a HS education. Participants administered their insulin via MDI (51%) or CSII (49%) and, on average, had been diagnosed with diabetes for 8.6 (SD = 4) years and had a bias-adjusted HbA1c value of 8.9% (SD=1.7). Although these youth were in HS and were living with parents/guardians at baseline, 155 (86%) were enrolled in school beyond HS and 114 (64%) lived independently of parents during the 12 months post-HS graduation. As can be seen in Table 2, the portion involved in alcohol, marijuana, and cigarette smoking was relatively low at HS graduation and during the year after graduation and relatively lower than portions in the general population [33, 34].
Table 2.
Alcohol use, cigarette smoking, and marijuana use for current study for various time points and for national samples of high school students and emerging adults.
| Youth with Type 1 Diabetes during the First Year Post HS Graduation in Study Sample | National Sample: 9–12 graders in the U.S. [33] | National Sample: 18–25 year olds in the U.S. [34] | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total Sample: Dichotomized |
Baseline # (%) | 3 month # (%) | 6 month # (%) | 9 month # (%) | 12 month # (%) | ||||
|
| |||||||||
| Alcohol Use | |||||||||
|
| |||||||||
| Frequency in past 3 months | N = 181 | N=170 | N = 154 | N = 152 | N = 139 | Use past 30 days | % | Use past month | % |
|
| |||||||||
| Not involved: 0 times | 141 (78%) | 132 (78%) | 105 (68%) | 95 (63%) | 78 (56%) | < 1 drink on 1 day | 61% | no | 39% |
|
| |||||||||
| Involved: ≥ 1 times | 40 (22%) | 38 (22%) | 49 (32%) | 57 (37%) | 61 (44%) | ≥ 1 drink on 1 day | 39% | yes | 61% |
|
| |||||||||
| Cigarette Use | |||||||||
|
| |||||||||
| Ever tried in past 3 months | N = 181 | N = 171 | N = 155 | N = 152 | N = 139 | Use past 30 days | Use past month | ||
|
| |||||||||
| Never | 127 (70%) | 115 (67%) | 103 (66%) | 99 (65%) | 86 (62%) | < 1 in a day | 82% | no | 67% |
|
| |||||||||
| Ever | 54 (30%) | 56 (33%) | 52 (34%) | 53 (35%) | 53 (38%) | ≥ 1 in a day | 18% | yes | 33% |
|
| |||||||||
| Marijuana use | |||||||||
|
| |||||||||
| Ever tired in past 3 months | N = 179 | N = 169 | N = 153 | N = 152 | N = 138 | Use past 30 days | Use past month | ||
|
| |||||||||
| Never | 138 (77%) | 133 (79%) | 117 (76%) | 114 (75%) | 103 (75%) | Used < 1 time | 77% | no | 81% |
|
| |||||||||
| Ever | 41 (23%) | 36 (21%) | 36 (24%) | 38 (25%) | 35 (25%) | Used ≥ 1 time | 23% | yes | 19% |
|
| |||||||||
| Alcohol Use for Groups | |||||||||
|
| |||||||||
| Consistent Involvement | |||||||||
|
| |||||||||
| Frequency | |||||||||
| Every day | 0 | 0 | 0 | 0 | 0 | ||||
| 4–5 days/week | 0 | 0 | 0 | 1 (5) | 0 | ||||
| 2–3 days/week | 2 (8) | 4 (19) | 6 (29) | 4 (20) | 6 (29) | ||||
| 1/week | 6 (24) | 7 (33) | 4 (19) | 2 (10) | 3 (14) | ||||
| 2–3 days/month | 6 (24) | 3 (14) | 4 (19) | 6 (30) | 4 (19) | ||||
| 1/month | 3 (12) | 1 (5) | 0 | 0 | 2 (10) | ||||
| 2–3 times/past 3 months | 3 (12) | 1 (5) | 3 (14) | 1 (5) | 3 (14) | ||||
| 1–2 times/past 3 months | 5 (20) | 5 (24) | 3 (14) | 6 (30) | 3 (14) | ||||
| Not at all | 0 | 0 | 1 (5) | 0 | 0 | ||||
|
| |||||||||
| Usual Amount Drank | |||||||||
| ≥ 9 | 2 (8) | 2 (10) | 1 (5) | 0 | 0 | ||||
| 7–8 | 4 (16) | 5 (24) | 2 (10) | 3 (15) | 3 (14) | ||||
| 6 | 3 (12) | 3 (14) | 5 (25) | 3 (15) | 0 | ||||
| 5 | 5 (20) | 3 (14) | 4 (20) | 4 (20) | 4 (19) | ||||
| 4 | 4 (16) | 3 (14) | 4 (20) | 3 (15) | 6 (29) | ||||
| 3 | 1 (4) | 3 (14) | 2 (10) | 1 (5) | 6 (29) | ||||
| 2 | 4 (16) | 1 (5) | 1 (5) | 3 (15) | 1 (5) | ||||
| 1 | 0 | 1 (5) | 1 (5) | 1 (5) | 0 | ||||
| <1 drink | 2 (8) | 0 | 0 | 1 (5) | 1 (5) | ||||
| Refused | 0 | 0 | 0 | 1 (5) | 0 | ||||
|
| |||||||||
| Growing Involvement | |||||||||
|
| |||||||||
| Frequency | |||||||||
| Every day | 1 (2) | 0 | 0 | 1 (2) | 2 (5) | ||||
| 4–5 days/week | 0 | 0 | 0 | 0 | 0 | ||||
| 2–3 days/week | 0 | 0 | 0 | 2 (4) | 4 (10) | ||||
| 1/week | 2 (4) | 1 (2) | 3 (6) | 2 (4) | 2 (5) | ||||
| 2–3 days/month | 0 | 0 | 7 (15) | 12 (26) | 9 (21) | ||||
| 1/month | 0 | 5 (9) | 2 (4) | 3 (6) | 3 (7) | ||||
| 2–3 times/past 3 months | 4 (7) | 2 (4) | 4 (8) | 6 (13) | 3 (7) | ||||
| 1–2 times/past 3 months | 8 (15) | 9 (17) | 13 (27) | 10 (21) | 7 (17) | ||||
| Not at all | 40 (74) | 35 (66) | 18 (38) | 11 (23) | 12 (29) | ||||
| Refused | 0 | 1 (2) | 1 (2) | 0 | 0 | ||||
|
| |||||||||
| Usual Amount Drank | |||||||||
| ≥ 9 | 1 (7) | 0 | 1 (3) | 1 (3) | 1 (3) | ||||
| 7–8 | 2 (13) | 1 (6) | 1 (3) | 3 (8) | 3 (10) | ||||
| 6 | 0 | 1 (6) | 3 (10) | 5 (14) | 6 (20) | ||||
| 5 | 2 (13) | 0 | 3 (10) | 4 (11) | 0 | ||||
| 4 | 2 (13) | 2 (12) | 2 (7) | 6 (17) | 3 (10) | ||||
| 3 | 0 | 3 (18) | 3 (10) | 4 (11) | 7 (23) | ||||
| 2 | 3 (20) | 1 (6) | 7 (24) | 2 (6) | 3 (10) | ||||
| 1 | 1 (7) | 3 (18) | 4 (14) | 7 (19) | 3 (10) | ||||
| <1 drink | 4 (27) | 6 (35) | 5 (17) | 4 (11) | 4 (13) | ||||
| Refused | 0 | 0 | 0 | 0 | 0 | ||||
|
| |||||||||
| Minimal Involvement | |||||||||
|
| |||||||||
| Frequency | |||||||||
| Every day | 0 | 0 | 0 | 0 | 0 | ||||
| 4–5 days/week | 0 | 0 | 0 | 0 | 0 | ||||
| 2–3 days/week | 0 | 0 | 0 | 0 | 0 | ||||
| 1/week | 0 | 0 | 0 | 0 | 0 | ||||
| 2–3 days/month | 0 | 0 | 0 | 0 | 0 | ||||
| 1/month | 0 | 0 | 0 | 0 | 0 | ||||
| 2–3 times/past 3 months | 0 | 0 | 0 | 0 | 2 (3) | ||||
| 1–2 times/past 3 months | 0 | 0 | 0 | 1 (1) | 8 (11) | ||||
| Not at all | 101 (100) | 97 (100) | 86 (100) | 84 (99) | 66 (87) | ||||
|
| |||||||||
| Usual Amount Drank | |||||||||
| ≥ 9 | 0 | 0 | 0 | 0 | 0 | ||||
| 7–8 | 0 | 0 | 0 | 0 | 0 | ||||
| 6 | 0 | 0 | 0 | 0 | 0 | ||||
| 5 | 0 | 0 | 0 | 0 | 0 | ||||
| 4 | 0 | 0 | 0 | 0 | 1 (10) | ||||
| 3 | 0 | 0 | 0 | 1 (100) | 1 (10) | ||||
| 2 | 0 | 0 | 0 | 0 | 2 (20) | ||||
| 1 | 0 | 0 | 0 | 0 | 4 (40) | ||||
| <1 drink | 0 | 0 | 0 | 0 | 2 (20) | ||||
Trajectories of Alcohol Involvement
Three alcohol involvement categories best fit the data based on latent class analysis (See Figure 2). The 3-class model best fit the data (χ2=32.4, DF=23, P=.092; BIC=708.7; Adjusted Lo-Mendell-Rubin for 3 vs. 4 classes p=.087) of the 5 (1–5 classes) models were examined. The 3-class model’s precision of latent class assignment was adequate (Table 1). Those in the Consistent Involvement Group (n=25, 13.8%) were using alcohol at HS graduation, had the highest estimated probability of use relative to other groups at all data points, and were fairly stable in their involvement over the 12-month study period. The Minimal Involvement Group (n=101, 55.8%) had a negligible estimated probability of alcohol use until nine months into the study period, at which time it grew slightly, but was still extremely low. At baseline, the Growing Involvement Group (n=55, 30.4%) had a very low estimated probability of alcohol use, gradually increased with a more brisk increase between the 9 and 12-month periods. Alcohol use covariance coverage (bivariate proportion of non-missing data) ranged from 58% to 100%, acceptable for MPLUS full information maximum likelihood estimation methods. A test for randomness in missing value patterns indicated that the pattern may be missing completely at random (p=0.76) [35].
Figure 2. Latent class model-estimated probabilities for alcohol involvement, baseline to 12 months.
Trajectories of Alcohol Involvement and Associated Variables
Associations were examined between alcohol involvement class and select variables (Table 3). There were no statistically significant associations between alcohol involvement class and gender, years with diabetes and insulin administration method, but groups were significantly associated with mothers’ and fathers’ education. College-educated parents had higher than expected proportions of youth in the growing involvement class. Alcohol involvement classes were similar in terms of glycemic control, parent-youth conflict and enrollment in school. Alcohol use classes demonstrated statistically significant differences in terms of diabetes self-efficacy, diabetes management, ever tried marijuana or ever smoked cigarettes, major life events, and living independently of parents. Pairwise tests showed that the Minimal Involvement Group had higher diabetes self-efficacy than the Growing Involvement Group (P=.021) and higher diabetes management than the Consistent Involvement Group (P=.030) and the Growing Involvement Group (P=.049). In addition, the Minimal Involvement Group had much lower odds for ever trying marijuana or ever smoking cigarettes than either the Consistent Involvement or Growing Involvement individuals (P < .001). The Growing Involvement Group was more likely to live independently of parents than the Minimal Involvement Group (P=.013). The Consistent Involvement Group tended to have more of major life events than growing involvement and minimal involvement groups (paired comparison P < .01).
Table 3.
Alcohol trajectory class differences on selected variables: Means (SD) or frequency (%) for tests with socio-demographic and diabetes-related factors and least square means (SE) or Odds Ratio (95%CI) from mixed model tests for test with environmental and individual characteristics, health behaviors, health outcomes and life events.
| Variables | Consistent Involvement Group (n=25) | Growing Involvement Group (n=55) | Minimal Involvement Group (n=101) | P-value |
|---|---|---|---|---|
|
| ||||
| Socio-demographic and Diabetes-related | ||||
|
| ||||
| Gender (Male) | 16 (64.0%) | 24 (43.6%) | 39 (38.6%) | 0.077a |
|
| ||||
| Years with Diabetes | 7.29 (3.48) | 9.23 (3.56) | 8.08 (3.97) | 0.1672b |
|
| ||||
| Insulin Administration Method (CSII) | 12 (48.0) | 23 (41.8) | 54 (53.5) | 0.3774a |
|
| ||||
| Mother’s Education | 0.011a | |||
| No College | 14 (56.0%) | 17 (30.9%) | 55 (55.0%) | |
| College | 11 (44.0%) | 38 (69.1%) | 45 (45.0%) | |
|
| ||||
| Father’s Education | 0.017a | |||
| No College | 15 (60.0%) | 19 (34.6%) | 56 (57.1%) | |
| College | 10 (40.0%) | 36 (65.5%) | 42 (42.9%) | |
|
| ||||
| Environmental Characteristic | ||||
|
| ||||
| Parent-Youth Conflict | 22.35 (1.35) | 23.44 (0.91) | 21.74 (0.67) | 0.323c |
|
| ||||
| Individual Characteristic | ||||
|
| ||||
| Diabetes Self-Efficacy | 51.24 (1.94) | 51.25 (1.31) | 55.03 (0.97) | 0.035c |
|
| ||||
| Health Behaviors | ||||
|
| ||||
| Diabetes Management | 49.02 (2.08) | 50.68 (1.40) | 54.10 (1.04) | 0.034c |
|
| ||||
| Ever Tried Marijuana | 47.45 (15.06–149.51) | 5.87 (2.39–14.42) | * | < 0.001d |
|
| ||||
| Ever Smoked Cigarettes | 15.51 (6.17–38.98) | 3.07 (1.60–5.88) | * | < 0.001c |
|
| ||||
| Health Outcome | ||||
|
| ||||
| Bias-adjusted HbA1C | 8.94 (0.32) | 8.93 (0.22) | 9.10 (0.17) | 0.788c |
|
| ||||
| Life Events | ||||
|
| ||||
| Major Life Events | 3.72 (2.78) | 2.38 (1.87) | 2.44 (2.02) | 0.017b |
|
| ||||
| Enrolled in School | 0.38 (0.13–1.08) | 1.21 (0.43–3.37) | * | 0.145d |
|
| ||||
| Living Independently of Parents | 0.63 (0.26–1.51) | 2.43 (1.14–5.17) | * | 0.013d |
Note.
exact p values based on likelihood ratio chi squared;
p values based on 1-way ANOVA;
p values based on GLMM least squares means;
p values based on GEE and odds ratio; and
referent category is minimal involvement group.
Discussion
This study extends the existing knowledge of alcohol use among emerging adults with type 1 diabetes by identifying 3 unique patterns of involvement during the year after HS graduation. On the surface, emerging adults with diabetes do use alcohol, with less than a quarter reporting use at HS graduation and less than half reporting use 1 year after graduation. The portion of youth with diabetes using alcohol appear to be lower than the portion of national samples of youth, with slight more than a third of HS school students [33] and more than half of 18–25 year olds [34] using alcohol. However, 3 unique patterns of alcohol use were identified, providing a richer understanding of individual’s use during the year after HS.
“Minimal Involvement” was one pattern, with over half of these youth having essentially no alcohol involvement up to 9 months post-graduation when they had a greater, but still very low, probability of using alcohol between 9 and 12 months. These individuals are likely similar to “Abstainers” in the general population [3]. These individuals had the best self-reported diabetes management. As part of a methodical management style [4], these youth could be avoiding alcohol, known to be associated with severe hypoglycemic events and poorer glycemic [5]. In comparison to the growing involvement group, these individuals also had better diabetes self-efficacy, known to be associated with better diabetes management [36]. It is likely that these youth had greater confidence in their abilities to perform their diabetes tasks even when there was a temptation to drink with friends.
The second pattern was “Growing Involvement” for a smaller, but substantial, portion of youth who had a gradually increasing probability of alcohol use after HS graduation. These individuals are similar to the “Light Drinkers” in the general population [3] who likely experiment with alcohol without the constraints of being an adult [2]. Consistent with having freedoms during this period [2], these youth were more likely to live independently of their parents than the minimally involved group. In addition, these youth were 6 times more likely to try marijuana and 3 times more likely to try cigarette smoking in the past 3 months than the minimally involved group. It is likely that they are exploring other substances, consistent with Arnett’s hypothesis [2].
“Consistent Involvement” was the third pattern for a very small minority of individuals steadily using alcohol at HS graduation and during the following year. Relative to the other groups, these youth had the highest alcohol involvement and could be considered heavy drinkers for those with diabetes, similar to heavy drinkers in the general population [3]. Slightly more than two-thirds of consistent involvement individuals drank alcohol relatively frequently, on a weekly or monthly basis, and about 3 quarters consume 3 or more drinks at a time in comparison to the growing involvement group for whom about half drank alcohol relatively infrequently (0 to 3 times in the past 3 months) and consumed relatively few drinks at a time (2 or fewer). This group had more major life events than the minimally involved group which are, which are assumed to be stressful [37]. In addition, these youth were 47 more likely to try marijuana and 15 times more likely to have tried smoking cigarettes in the past 3 months relative to the minimally involved group. It is likely these youth’s alcohol use was associated with self-medication to allay life stress of the many changes in their life as well as confusion about their identity and/or pessimism about their future [2].
It was surprising that alcohol involvement patterns were not associated with parent-youth conflict and gender, both known to be relevant in the general population [6]. However, the lack of association of alcohol classes with glycemic control is consistent with inconclusive associations noted in a recent synthesis of findings among youth with diabetes [1]. The 42 day average between measurement of glycemic control and alcohol use provided considerable time for other factors to influence glycemic control. For example, if an individual had an adaptive management style [4], they could have made diabetes management adjustments to counter the effect of alcohol on glycemic control.
Further research is needed to identify alcohol use patterns and associated factors beyond this sample. Once there is a greater body of evidence, health care professionals can screen emerging adults with type 1 diabetes for alcohol involvement patterns. In addition, researchers can test interventions to target unique alcohol use patterns such as stress management for individuals who are using alcohol to self-medicate.
Study Limitations
The potential limitations of the study need to be considered. This sample generally reflects youth with type 1 diabetes in that they were predominately White [38], relatively equally distributed in terms of males and females [39], and by ADA standards, in relatively poor glycemic control [40]. However, this sample may differ in that most of these youth had parents who were married and had at least a HS education. Further, this sample most likely reflects the more “typical” youth because those with serious mental health issues and co-morbid health conditions were excluded, affecting the portion involved in alcohol use. One also needs to be cautious comparing alcohol use, measured in the past 3 months, in our sample with national samples which measured it in the past month. Finally, the potential for bias in self-reporting of alcohol use exits; however, we provided participants privacy to decrease the potential for this.
Acknowledgments
The project was supported by the National Institute of Nursing Research at the National Institutes of Health (grant #R01NR009810).
Footnotes
Conflicts of Interest: None
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kathleen M. Hanna, Indiana University School of Nursing.
Nathan W. Stupiansky, Indiana University School of Medicine, Adolescent Section.
Michael T. Weaver, Indiana University School of Nursing.
James E. Slaven, Indiana University School of Medicine, Department of Biostatistics.
Timothy E. Stump, Indiana University School of Medicine, Department of Biostatistics.
References
- 1.Barnard K, et al. Alcohol-associated risks for young adults with Type 1 diabetes: a narrative review. Diabetic Medicine. 2012;29(4):434–40. doi: 10.1111/j.1464-5491.2012.03579.x. [DOI] [PubMed] [Google Scholar]
- 2.Arnett JJ. The developmental context of substance use in emerging adulthood. Journal of Drug Issues. 2005;35(2):235–253. [Google Scholar]
- 3.Maggs JL, Schulenberg JE. Trajectories of Alcohol Use During the Transition to Adulthood. Alcohol Research & Health. 2004;28(4):195–201. [Google Scholar]
- 4.Schneider S, et al. Identification of distinct self-management styles of adolescents with Type 1 diabetes. Diabetes Care. 2007;30(5):1107–1112. doi: 10.2337/dc06-2197. [DOI] [PubMed] [Google Scholar]
- 5.Peters A, Laffel L G. American Diabetes Association Transitions Working, . Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association. Diabetes Care. 2011;34(11):2477–85. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanna KM. A framework for the youth with type 1 diabetes during the emerging adulthood transition. Nursing Outlook. 2012;60(6):401–10. doi: 10.1016/j.outlook.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tucker JS, et al. SUBSTANCE USE TRAJECTORIES FROM EARLY ADOLESCECE TO EMERGING ADULTHOOD: A COMPARISON OF SMOKING, BINGE DRINKING, AND MARIJUANA USE. Journal of Drug Issues. 2005;35(2):307–331. [Google Scholar]
- 8.Wysocki T, et al. The psychologic context of pediatric diabetes. Pediatr Clin North Am. 2005;52(6):1755–78. doi: 10.1016/j.pcl.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Glasgow RE, et al. Behavioral science in diabetes. Contributions and opportunities. Diabetes Care. 1999;22(5):832–43. doi: 10.2337/diacare.22.5.832. [DOI] [PubMed] [Google Scholar]
- 10.Hood KK, et al. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics. 2009;124(6):e1171–9. doi: 10.1542/peds.2009-0207. [DOI] [PubMed] [Google Scholar]
- 11.Brown SA, et al. Underage Alcohol Use. Alcohol Research & Health. 2009;32(1):41–52. [PMC free article] [PubMed] [Google Scholar]
- 12.Helgeson VS, et al. Relation of stressful life events to metabolic control among adolescents with diabetes: 5-year longitudinal study. Health Psychology. 2010;29(2):153–159. doi: 10.1037/a0018163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furstenberg FF, Jr, Rumbaut RC, Settersten RA., Jr . On the frontier of adulthood: Emerging themes and new directions. In: Settersten RA, Furstenberg FF, Rumbaut RG, editors. On the frontier of adulthood: Theory, research, and public policy. The University of Chicago Press; Chicago: 2005. pp. 3–25. [Google Scholar]
- 14.Hanna KM, et al. Initial findings: primary diabetes care responsibility among emerging adults with type 1 diabetes post high school and move out of parental home. Child: Care Health and Development. 2013;39(1):61–8. doi: 10.1111/j.1365-2214.2011.01320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanna KM, et al. Readiness for Living Independently Among Emerging Adults With Type 1 Diabetes. The Diabetes Educator. 2013;39(1):92–99. doi: 10.1177/0145721712465341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stupiansky NW, et al. Impulse control, diabetes-specific self-efficacy, and diabetes management among emerging adults with type 1 diabetes. Journal of Pediatric Psychology. 2013;38(3):247–54. doi: 10.1093/jpepsy/jss110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanna KM, Scott LL, Schmidt KK. Meeting Recruitment and Retention Goals in a Longitudinal Study with Emerging Adults. Clinical Nurse Specialist. 2014;28(1):41–45. doi: 10.1097/NUR.0000000000000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanna KM, et al. Emerging Adulthood. Emerging Adults with Type 1 Diabetes during the First Year Post-High School: Perceptions of Parental Behaviors. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wolpert HA, Anderson BJ, Weissberg-Benchell J. Transitions in care: Meeting the challenges of type 1 diabetes in young adults. Alexandria, Virginia: American Diabetes Association; 2009. [Google Scholar]
- 20.Rubin R, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes. 1989;38:7A. [Google Scholar]
- 21.Hood KK, et al. Updated and revised diabetes family conflict scale. Diabetes Care. 2007;30(7):1764–1769. doi: 10.2337/dc06-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Littlefield CH, et al. Relationship of self-efficacy and binging to adherence to diabetes regimen among adolescents. Diabetes Care. 1992;15(1):90–4. doi: 10.2337/diacare.15.1.90. [DOI] [PubMed] [Google Scholar]
- 23.Harris MA, et al. Validation of a structured interview for the assessment of diabetes self-management. Diabetes Care. 2000;23(9):1301–4. doi: 10.2337/diacare.23.9.1301. [DOI] [PubMed] [Google Scholar]
- 24.Jessor R, Donovan J, Costa F. Health behavior questionnaire: High school form. 1992. [Google Scholar]
- 25.Wechsler H, et al. A gender-specific measure of binge drinking among college students. American Journal of Public Health. 1995;85(7):982–5. doi: 10.2105/ajph.85.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pathologists, C.o.A. College of American Pathologists Survey Data. 2012. [Google Scholar]
- 27.McCubbin HI, Thompson AI, McCubbin MA. Family assessment: Resiliency, coping and adaptation. Madison, WI: University of Wisconsin Publishers; 1996. [Google Scholar]
- 28.Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. [Google Scholar]
- 29.Muthen LK, Muthen BO. Mplus usesr’s guide. 5. Muthen & Muthen; Los Angeles: 1998–2007. [Google Scholar]
- 30.Masyn KE. Latent class analysis and finite mixture modeling. In: Little T, editor. The Oxford handbook of quantitative methods in psychology. Oxford University Press; New York, NY: 2013. pp. 551–611. [Google Scholar]
- 31.McCulloch C, Searle S. Generalized, linear, and mixed models. New York, NY: John Wiley & Sons; 2001. [Google Scholar]
- 32.SAS. SAS/STAT User’s Guide. SAS Institute, Inc; Cary, NC: 2011. [Google Scholar]
- 33.Centers for Disease Control and Prevention. Youth Risk Behavior Survelliance - United States, 2011. 2013 [cited 2014 January 25]. Avaialble from: http://www.cdc.gov/yrbss.
- 34.National Institute on Drug Abuse. National Survey on Drug Use and Health. 2013 [cited 2014 January 25]; Avaialble from: http://www.drugabuse.gov/national-survey-drug-use-health.
- 35.Enders C. Applied Missing Data Analysis. New York, NY: Guilford Press; 2010. [Google Scholar]
- 36.Iannotti RJ, et al. Self-efficacy, outcome expectations, and diabetes self-management in adolescents with Type 1 diabetes. Developmental and Behavioral Pediatrics. 2006;27(2):98–105. doi: 10.1097/00004703-200604000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Holmes TH, Rahe RH. The social readjustment rating scale. Journal of Psychosomatic Research. 1967;11(2):213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control. National Diabetes Fact Sheet: national estimates and general information on diabets and rediabetes in the United States. U.S Department of Health and Human Services, Centers of Disease Control and Prevention; Atlanata, GA: 2011. pp. 1–12. [Google Scholar]
- 39.American Diabetes Association. Diabetes statistics for youth. n.d [cited 2005 May 12]; Available from: http://www.diabetes.org/diabetes-statistics/children.jsp.
- 40.Silverstein J, et al. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]