Case Presentation
A 16-year-old male was referred for recurrent episodes of drug-resistant symptomatic palpitations. He had successful ablation of a concealed para-Hisian accessory pathway (AP) 7 years previously.
At baseline, 12-lead ECG showed frequent atrial premature beats (APB) in a bigeminal pattern with inferior axis in the frontal plane and a fixed coupling interval to the preceding QRS complex. There was no evidence of pre-excitation. APBs were conducted to the ventricles with a functional left posterior fascicular delay, causing shift in the frontal QRS axis from +60° to +120°. Nonsustained, narrow complex tachycardia initiated by the APB is shown in Figure 1A.
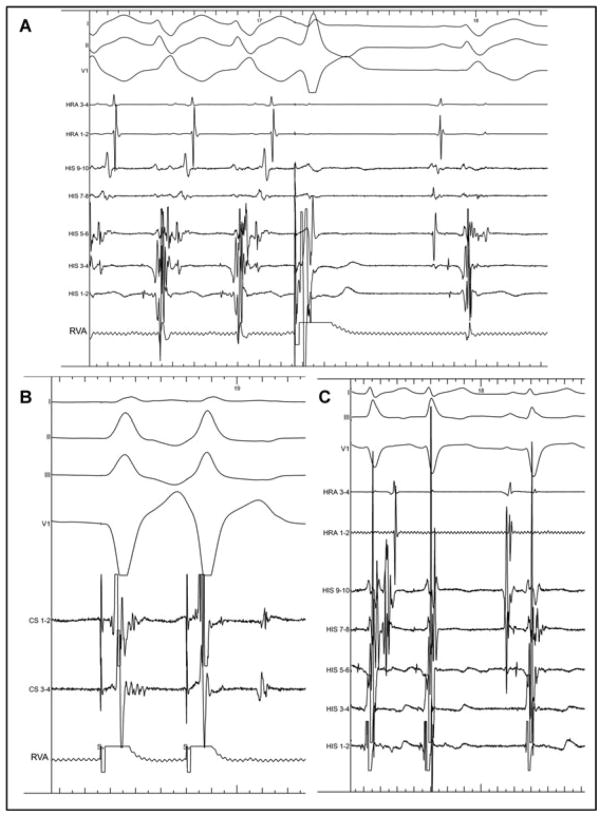
Figure 1.
A: Initial surface ECG. The surface ECG shows frequent atrial premature beats (APB). Ectopic short duration positive P waves can be identified on top of T waves in the inferior leads and V1 during atrial bigeminy and narrow complex tachycardia initiation. B: Intracardiac recordings during spontaneous initiation of the tachycardia. Shown are surface electrograms and intracardiac recordings from the mid lateral wall of the right atrium (HRA), para-Hisian region (HIS). The first beat is a normal sinus beat. The second HRA recording is an APB that is conducted with an increased AH delay to 192 ms. The 3rd and 4th beats are normal sinus beats. The narrow complex tachycardia is then initiated with the same A-H-V sequence as the APB. For all nonsinus beats, the earliest atrial activity is recorded on His 5-6. There is a continuous activity after most of ventriculograms on His 5-6.
An electrophysiological study was performed, using a deflectable decapolar catheter (Xtrem, ELA Medical, Le-Plessis-Robinson, France) for His bundle recording, a deflectable quadripolar catheter (Xtrem, ELA Medical) at the high right atrium, and a 4-mm nonirrigated tip ablation catheter (Celcius, BiosenseWebster, Diamond Bar, CA, USA).
Intracardiac recordings in sinus rhythm showed normal AH (68 ms) and HV (44 ms) intervals. APBs conducted through the atrioventricular (AV) node in a decremental fashion causing an increase in A–H interval to 192 ms. On mapping the APBs, the earliest site of atrial activation was recorded just proximal to the His bundle. The activation of the right atrium and the coronary sinus was concentric during the APB. Intermittently, APBs initiated narrow complex tachycardia with 1:1 AV relationship at a cycle length (CL) of 366 ms (Fig. 1B). What are the diagnostic possibilities of this tachycardia?
Discussion
The surface ECG shows a narrow complex tachycardia with a 1:1 AV relationship. The diagnostic possibilities include (1) atrial tachycardia (AT), (2) an atypical form of atrioventricular nodal reentrant tachycardia (AVNRT), and (3) orthodromic reentrant tachycardia (ORT) possibly utilizing a para-Hisian AP. AVNRT was excluded by definition because typical AVNRT has very short VA.1 Interestingly, at the onset of the tachycardia variability in the CL was observed. On the surface, ECG changes in RR interval preceded changes in PP interval, which was confirmed by intracardiac recordings (Fig. 1), making atrial tachycardia unlikely. On this basis the only possible diagnosis was ORT.
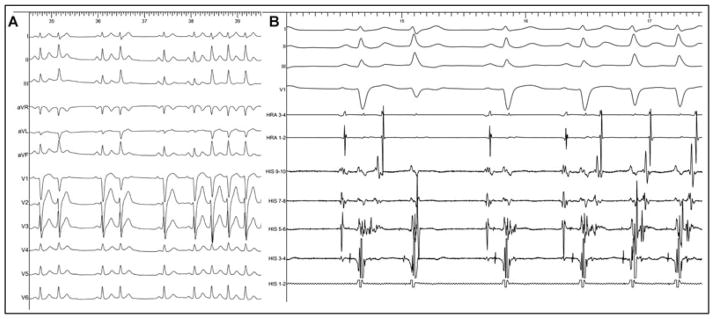
Entrainment from right ventricular apex was performed during sustained tachycardia at a CL 20 ms shorter than that of the tachycardia. Upon cessation of pacing, V-A-V response was reproducibly observed, thus excluding an atrial tachycardia.1 A single ventricular extrastimulus delivered at the time of His refractoriness during tachycardia advanced the following atrial electrogram by 40 ms, demonstrating retrograde activation over an accessory pathway. Of interest, incidentally observed right and left bundle branch block during tachycardia failed to prolong VA time, which is consistent with septal location of the accessory pathway.2 Finally, premature ventricular complexes delivered during His refractoriness reproducibly interrupted the tachycardia without conduction to the atria (Fig. 2A), confirming the diagnosis of orthodromic reentrant tachycardia utilizing a concealed accessory pathway.
Figure 2.
A: Tachycardia interruption with single PVC delivered during His refractoriness. Recordings as per Figure 1B; in addition, a right ventricular apex (RVA) recording is provided. A single premature ventricular beat is delivered in the right ventricle during His refractoriness, which interrupts the tachycardia without retrograde atrial activity on the HRA recording. His 3-4 and 5-6 display a fragmented activity that is in continuity with the ventriculograms during tachycardia. This fragmentation disappears after the last ventriculogram of the tachycardia and reappears in the following sinus beat. B: Single ventricular extrastimuli at basic drive cycle lenth (CL) 600 ms and an extra stimulus at 320 ms. On the basic drive, the retrograde atrial activation initially occurs at His 5-6, preceded by the fractionated low amplitude electrogram. A shorter coupling interval demonstrates a sudden increase in VA interval, with a different retrograde atrial activation sequence. His 3-4 displays a V-H-A pattern and the fractionated activity has disappeared. C: Spontaneous termination of the tachycardia. Again, the fragmented activity found at the end of the electrograms is lacking after the last ventriculogram of the tachycardia.
Endocardial mapping was performed to identify the earliest atrial activation. Low-amplitude continuous fractionated potential following the local ventricular electrogram was recorded near the His bundle during sinus rhythm and tachycardia but not following an isolated APB. During tachycardia, it preceded each retrograde atrial electrogram (Fig. 1B). It was consistently observed prior to each APB. The key element to prove that this fractionated activity was due to an AP was to demonstrate that it did not have a fixed timing relationship to A or to V.
APBs with ventricular conduction were observed as bigeminy if the local ventricular electrogram at the His location was not followed by the fractionated potential. On the other hand, when the APB initiated the tachycardia, the local ventricular electrogram at the His location was consistently followed by the fractionated potential. This observation suggested the obligatory role of the fractionated potential in tachycardia initiation by the APB. During sinus rhythm, spontaneous intermittent block in impulse conduction to the atria occurred after this fractionated activity, thus demonstrating that it was not a local atrial electrogram (Fig. 1B). Retrograde atrial electrogram was never observed without preceding fractionation demonstrating that this signal was linked to the atria. On delivering single ventricular extrastimuli coupled at 400 ms to ventricular pacing drive train of 600 ms, nondecremental conduction to the atria, earliest at His 5-6 and consistently preceded by the low-amplitude fractionated activity, was observed. However, at a coupling interval of 360 ms, AP blocked and conduction occurred over the normal AV conduction system leading to a sudden increase in VH interval (from 136 to 312 ms) with atria being activated retrogradely over the AV node (Fig. 2B). Similarly, when a ventricular premature beat terminated the tachycardia without advancing to the atria, the fractionated activity was characteristically absent (Fig 2A). These observations demonstrated that this activity was also linked to the ventricle but distinct from ventricular electrogram. These findings favor the conclusion that the fractionated potential was indeed an AP potential recording.
For stability and increased safety during ablation, we approached the pathway from the left subclavian venous access.3 Earliest retrograde A and the pathway potential were located anteroseptally on the ventricular side of the tricuspid annulus. Radiofrequency ablation using 25 W for 3 minutes led to the disappearance of the AP potential within few seconds. Sustained sinus rhythm without atrial echo beats ensued. Atrial burst pacing was unable to induce tachycardia.
Footnotes
No disclosures.
References
- 1.Knight BP, Ebinger M, Oral H, Kim MH, Sticherling C, Pelosi F, Michaud GF, Strickberger SA, Morady F. Diagnostic value of tachycardia features and pacing maneuvers during paroxysmal supraventricular tachycardia. J Am Coll Cardiol. 2000;36:574–582. doi: 10.1016/s0735-1097(00)00770-1. [DOI] [PubMed] [Google Scholar]
- 2.Kerr CR, Gallagher JJ, German LD. Changes in ventriculoatrial intervals with bundle branch block aberration during reciprocating tachycardia in patients with accessory atrioventricular pathways. Circulation. 1982;66:196–201. doi: 10.1161/01.cir.66.1.196. [DOI] [PubMed] [Google Scholar]
- 3.Warin JF, Haissaguerre M, Lemetayer P, Guillem JP, Blanchot P. Catheter ablation of accessory pathways with a direct approach. Results in 35 patients. Circulation. 1988;78:800–815. doi: 10.1161/01.cir.78.4.800. [DOI] [PubMed] [Google Scholar]