Abstract
Purpose
Age of the target audience at time of intervention is thought to be a critical variable influencing the effectiveness of adolescent sexual risk reduction interventions. Despite this postulated importance, to date studies have not been designed to enable a direct comparison of outcomes according to age at time of intervention delivery.
Methods
We examined outcomes of 598 youth who were sequentially involved in two randomized controlled trials of sexual risk prevention interventions, the first one delivered in grade 6 [Focus on Youth in the Caribbean (FOYC)] and the second one in grade ten [Bahamian Focus on Older Youth (BFOOY)]. Four groups were examined, including those who received: 1) both treatment conditions, FOYC and BFOOY; 2) FOYC in grade 6 and the control condition in grade 10; 3) the control condition in grade 6 and BFOOY in grade 10; and 4) both control conditions. Intentions, perceptions, condom-use skills as well as HIV-related knowledge were assessed over 60 months.
Results
Data showed that those who received both interventions had the greatest increase in condom-use skills. Youth who received FOYC in grade 6 had greater scores in knowledge and intention.
Conclusion
These results suggest that youth receive the most protection with early and repeated exposure to interventions. These findings suggest that educators should consider implementing HIV prevention and risk reduction programs as a fixed component of education curriculum beginning in the pre-adolescent years and if possible also during the adolescent years.
Keywords: HIV Prevention Intervention, Adolescence, Condom-use skills, Randomized Controlled Trials, Risk Reduction Behavior
Introduction
The prominence of adolescents and young adults in the context of the global HIV epidemic is uncontested. Adolescents and young adults between the ages of 13-29 constitute over one-third of all new HIV infections in the US [1]. Focusing on those who are most vulnerable, such as youth, should be a primary aim of prevention programs [2]. A robust literature based on randomized, controlled trials testifies to the effectiveness of a substantial number of HIV prevention interventions targeting adolescents and young adults [3,4].
Despite these successes, many basic questions regarding adolescent risk reduction interventions remain. A review of 66 group-based risk reduction interventions targeting adolescents observed that the reviewed studies did not provide “consistent evidence of differential effects on outcome for any of the 12 critical moderator variables (gender, virginity status, age, race/ethnicity, setting, dosage, focus, multicomponent, targeting, study design and comparison group type” [3](p288). The probable importance of each of these variables on outcomes is well recognized. Age and virginity status have received considerable attention in the literature for a variety of reasons. For several decades concerns were raised that risk reduction interventions by describing safer sexual practices could accelerate the initiation of sex and/or increase sexual activity if they were delivered to youth prior to the initiation of sex [4-6]. This aspect of the variables “age” and “virginal status” have been exhaustively studied, with an overwhelming preponderance of the literature indicating that sexual risk reduction interventions do not hasten the onset of sex or increase sexual activity [3,4,6,7].
However, the question as to the best timing for delivery of adolescent sexual risk reduction interventions in terms of age (which is confounded with sexual debut status) remains open. An extensive literature exists describing the myriad physical, cognitive and emotional changes occurring over the course of adolescence which could influence likelihood of being infected, of engaging in risk behavior and/or of responding to a risk reduction intervention. [8]. The adolescent's propensity to egocentric thinking and pre-occupation with short-term over long-term consequences may negatively impact decision-making. The early adolescent's reliance on concrete rather than abstract reasoning as well as the older adolescent's tendency to revert to concrete thinking when confronted with an emotion-laden situations continues to allow them to wander into harm's way [9]. Evidence from imaging studies has revealed that a surge of neural proliferation occurs in the brain around pre-adolescence and a wave of neural pruning occurs over the first few years after puberty. This “remodeling” of the brain is important and consistent with the observation that neural connections appear to be strengthened, weakened and/or revised during adolescence [10].
This question as to most propitious time(s) during a child's development for an intensive HIV prevention intervention remains unanswered. Currently there are several risk reduction interventions targeting youth in mid-to late adolescence that have been demonstrated to be effective [11]. A much smaller number of interventions targeting pre-adolescents and early adolescents have been demonstrated to be effective [12-15]. However, direct statements about relative effectiveness of intervention delivery according to age of the child—or the advantage of multiple intervention exposures [2]—remain speculative.
Several years ago (2008) we concluded follow-up through grade nine of youth who had participated in a randomized controlled HIV prevention trial (Focus on Youth in the Caribbean, or FOYC) in grade 6. Also in 2008, we initiated a randomized controlled trial of a version of FOYC adapted for older adolescents—Bahamian Focus On Older Youth (BFOOY) among grade 10 students. Because a subset of the grade 10 students enrolled in the BFOOY evaluation had also participated in the grade 6 trial (FOYC), we are in a position to address some of the questions regarding timing of a skills-based group HIV prevention intervention. The data in this study are from the 12-month follow-up of the grade 10 study—and, therefore, a five year follow-up from the grade 6 study. Specifically, these intersecting datasets enable us to explore several questions. Does an additive or booster effect result if the grade 10 intervention (BFOOY) is given to youth who previously received the grade 6 intervention (FOYC), or have these youth already gained maximum benefit from its earlier receipt? Do youth who previously had received the control condition experience a sharper response to the grade 10 intervention than do their peers who had received the grade 6 intervention?
Methods
Data
The data utilized for these analyses are from youth who participated in two randomized, controlled trials evaluating the effectiveness of the adolescent sexual risk reduction interventionFocus on Youth in the Caribbean (FOYC). FOYC is a 10-session program (plus two booster sessions) targeting adolescents which was adapted from Focus on Youth (FOY), an evidence-based risk reduction intervention targeting US mid-adolescents that is part of the Centers’ for Disease Control and Prevention portfolio of evidence-based HIV prevention programs [16]. FOYC and FOY are based on a social cognitive model, Protection Motivation Theory [17], which posits that decision making is a balance of the perceived benefits and risks associated with the risky or protective behavior. In brief, the model suggests that if the individual: 1) believes that the protective maneuver is likely to work (“response efficacy”) and 2) that she is able to enact the protective maneuver (“self-efficacy”). She determines that 3) the disadvantages of employing the protective maneuver (“response costs”) are relatively small while 4) the adverse consequences of the risky behavior are significant (severity) and 5) likely to happen to the individual (“vunerability). Finally, she feels that the positive feedback that she will enjoy from engaging in the risky behavior both from an 6) external audience (“extrinsic rewards”) and 7) her own physical or emotional pleasure “intrinsic rewards”) are small. Protection Motivation Theory would predict that this person is likely to intend to engage (“intention”) in the protective action rather than the risky action, a critical step in the pathway to “action”. The intervention contains exercises designed to increase skills regarding risk avoidance, communication, negotiation and condom-use as well as HIV-related knowledge. The intervention format includes lectures, interactive discussions, games and exercises to reinforce main messages, and a fictional family story to contextualize decision-making [13]. During its adaptation from FOY, subsequently, FOYC was modified to be developmentally appropriate for grade 10 students (see below). The grade 10-version of FOYC, called Bahamian Focus on Older Youth (BFOOY) also contains 10-sessions (with the same order and general content of the grade 6 version, FOYC), but the discussions, exercises and games reflect the older age of the participants. Youth and parents provided assent and consent to participate in each trial. Human Research Protection Boards for Wayne State University and the Ministries of Health and Education in the Bahamas approved consenting procedures and study protocols.
Grade 6 intervention (FOYC) evaluation
The grade 6 effectiveness trial of FOYC involved 15 of the 26 government elementary schools located on the island of New Providence, The Bahamas which were selected based on geographic distribution and willingness of the school administrators to accept randomization [13]. The control comparison for FOYC was a 10-session ecology curriculum, “The Wondrous Wetlands” (WW) [12-14]. The WW curriculum, which was developed for The Bahamas, emphasizes the preservation of the wetlands and provided applied knowledge and skills regarding water conservation. Approximately two-thirds of the students in grade 6 in the participating schools returned assent/consent forms before the desired sample size was reached and enrollment was completed. Enrolled students completed baseline measures, prior to randomization, which was conducted at the level of the school. The FOYC curriculum was delivered to all students enrolled in grade 6 in the 10 schools randomized to FOYC, (and five schools were randomized to WW) regardless of whether a student was or was not participating in the evaluation of the interventions. A questionnaire assessing HIV knowledge and condom-use skills, self-efficacy, intentions and self-reported behaviors [The Bahamian Youth Health Risk Behavioral Inventory (BYHRBI) [13,18], was administered to youth participating in the study at baseline and at five follow-up assessments (6, 12, 18, 24 and 36 months post intervention); students not enrolled in the study did not complete the questionnaire.
FOYC was found to be effective in increasing HIV knowledge and condom-use skills, condom-use self-efficacy, and intentions to use condoms through 36 months post-intervention [12-14].
Grade 10 intervention (BFOOY) evaluation
A randomized, controlled evaluation of BFOOY (an adaptation of FOYC for grade 10 students as described above) among youth attending grade 10 was conducted among all eight of the government high schools in New Providence, The Bahamas. The control condition was “standard-of-care”, the existing Bahamian Health and Family Life Education (HFLE) Curriculum, which focuses on a range of health topics, including a factual presentation of HIV and pregnancy prevention. The 2564 participating students were randomized by class to one or the other of the two student curricula (BFOOY and HELE) and two parent interventions [13,19] (which were not the focus of the current analysis). The power of the current study was insufficient to allow us to look at all the possible parent and youth intervention exposure combinations. However, to control for any possible effects we included a variable in the model coded as having received the parental monitoring intervention or not.
Measures
Condom-use response costs
Perceptions of the perceived “response costs” (the possible exposures, liabilities or losses) associated with using a condom were assessed through five items, with each response measured along a five-point Likert scale (1=Strongly disagree; 3=Don't know; 5=Stongly agree). The items in the grade 6 study and those in the grade 10 studies were either identical or nearly so, although in a few instances the changes might have altered the meaning [e.g., “If a girl carries condoms, people would think she is having sex” (grade 6) compared to “It would be wrong for me to carry a condom because it would mean I am planning to have sex” (grade 10). The internal consistency (alpha) of these items ranged between (0.30- 0.49).
Condom-use response efficacy
The youths’ perceptions of the effectiveness of condoms in preventing HIV and other STIs were assessed along a five-point Likert scale (1=Strongly disagree; 3=Don't know; 5=Strongly agree) through three items: “Condoms are an important way to prevent a pregnancy;” “Condoms are an important way to prevent you from getting AIDS;” and “Condoms are an important way to prevent you from getting a STD.” The grade 6 and grade 10 studies employed identical items. The alpha of these items ranged between (0.48-0.82).
Condom-use self-efficacy
The youth's perceptions as to his/her ability to perform all of the steps required to achieve protection through accessing and negotiating condom-use was assessed through seven items. Specifically, these items assess if the youth believes he/she could “get condoms,” “put on a condom correctly”, “ask for condoms in a store”, “ask for condoms in a clinic”, “convince my partner that we should use a condom even if he/she did not want to’, and “refuse to have sex if my sexual partner will not use a condom.” Responses to each item were measured on a five-point Likert scale (1=Strongly disagree; 3=Don't know; 5=Strongly agree). The both studies employed identical self-efficacy items. The alpha of these items ranged between (0.77-0.87).
Condom-use skills checklist
To assess condom-use skills knowledge, both studies used the Condom-use Skills Checklist [20] consisting of 16 items, eight of which are the correct steps to using a condom while the other eight are incorrect steps of using a condom. The students were asked to mark the eight steps which are correct. The scale was scored giving the youth a point for each item that was correctly marked (1=correct/0=incorrect). The internal consistency of these items ranged between (0.15-0.60).
HIV knowledge
Knowledge regarding disease transmission, prevention, treatment, symptoms and effects of HIV/AIDS were measured through true-false questions in both the grade 6 and grade 10 studies. The number of items and the specific items differed by study, reflecting expectations for age-appropriate increases in knowledge as well as changes in the HIV/AIDS field itself. The grade 6 study included 18 items, while the grade 10 study had 16 items. Therefore, the student mean scores regarding HIV/AIDS knowledge decreased at the onset of the grade 10 study (e.g., between the grade 9 follow-up and the baseline at grade 10) due to the items being more difficult but then rising as the grade 10 study continued. The internal consistency of these items ranged between (0.48-0.82). To accommodate the use of different scales, we included a variable to control for which study each time point was assessed in our mixed model examining HIV/AIDS knowledge. Mixed modeling requires that the data be in long format which presents a data row for each time point for each participant. In this format we are also able to indicate in which study the score was assessed. Therefore, if the data had been generated in the grade 6 study it was scored as “1”; if the data had been generated in grade 10 it was scored as “2”.
Intention to use a condom
Both studies measured youth expectations that he/she would use a condom through a single item along a five-point Likert scale: “How likely is it that you will use a condom if you were to have sex in the next six months?” (5=Yes, I will; 3=Don't know; 1=No, I will not).
Although youth were assessed on whether they had engaged in sexual intercourse in the last six months and whether they had used a condom during their last sexual episode, we were unable to examine self-reported condom-use and sexual behavior because the frequencies of such behaviors were too infrequent when divided among the four groups of students. Therefore, models for these behaviors baseline to five years post-FOYC did not converge.
Data Analysis
Means were obtained for each group and plotted. Baseline differences between groups were measured using ANOVA and Tukey corrections were applied for pair-wise comparisons. Models were analyzed using general mixed modeling using PROC MIXED. All models accounted for the random effects of school clustering with the RANDOM statement. Individual variability was accounted for using the REPEATED statement. The main effects for time, intervention group and gender were included as predictors in addition to the interaction of time by intervention assignment. Statistical analyses were conducted using the software SAS v. 9.2 (SAS Institute Inc, Cary, NC).
Results
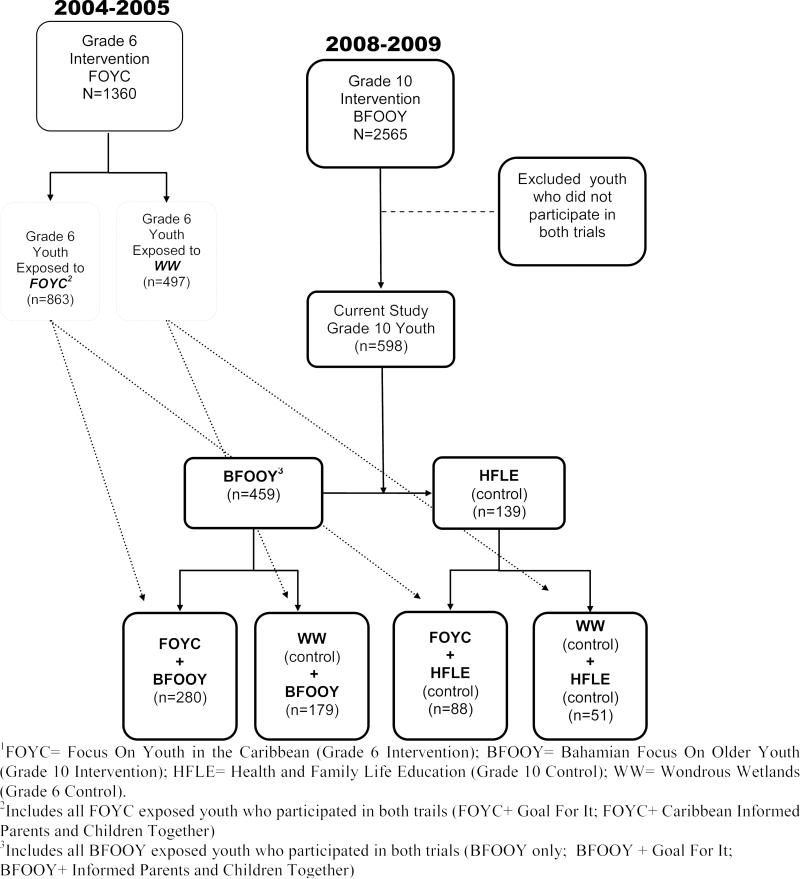
Among the 1360 grade 6 and the 2565 grade 10 study participants, 598 youth were enrolled in both studies; of these youth 51 (39.3% males) had received the control condition in both grades 6 and 10 (WW and HFLE); 280 (46.1% males) received the intervention condition in both grades; 88 (52.3% males) received the intervention in grade 6 and the control in grade 10; and, 179 (40.2% males) received the control in grade 6 and the intervention in grade 10 (See Figure 1). As previously described in detail [21] these youth who were present in both the grade 6 and grade 10 longitudinal trials were comparable with the youth who were only present in the grade six trial. Among the 598 youth enrolled in both studies at baseline of the combined study (e.g., at the time of enrollment of the grade 10 subjects), 486(81%) were still present at the 12 months follow-up combined-study reported herein.
Figure 1.
Intersection of Grade 6 (FOYC1) and Grade 10 (BFOOY) Interventions
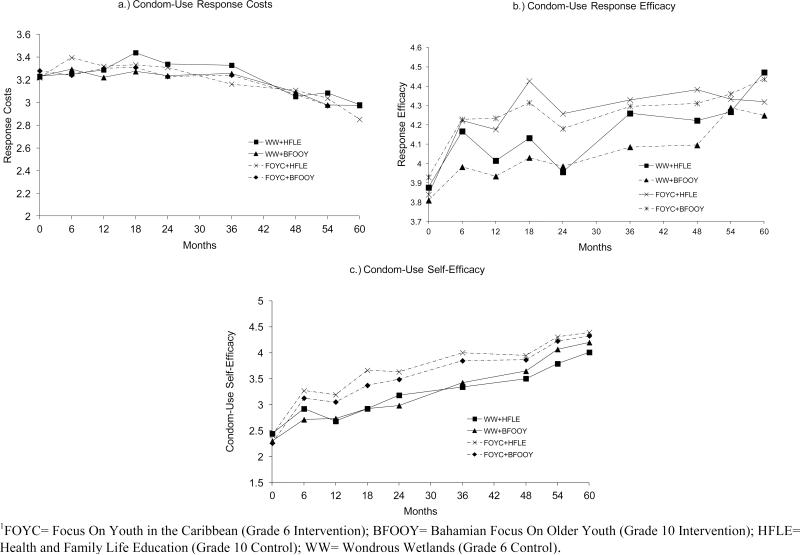
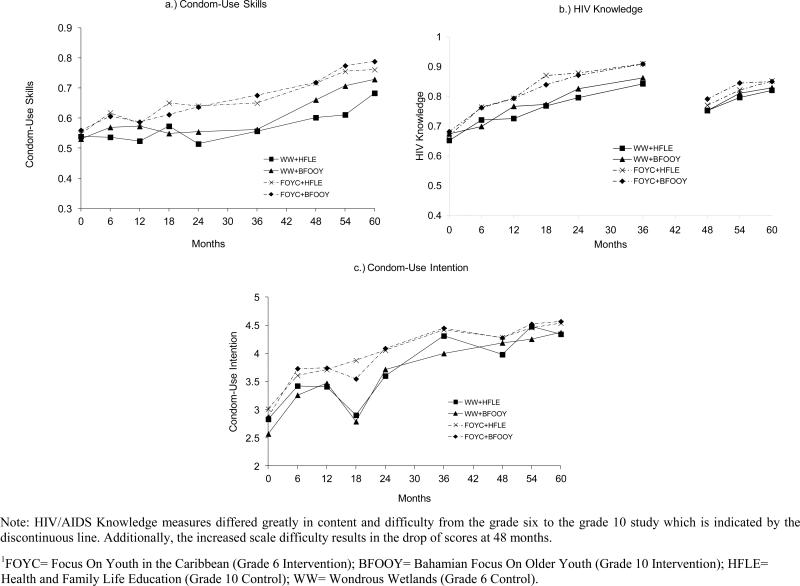
Differences between the four groups in grade 6 prior to any intervention are presented in Table 1. No differences between groups were found prior to intervention exposure. The means of the four groups were plotted in Figure 2A-2C for condom-use self-efficacy, condom-use response efficacy, and condom-use response costs and in Figure 3A –3C for condom-use skills, HIV knowledge, and intention to use a condom at each assessment period beginning with grade 6 baseline up to 60 months post-intervention. The graphs provide a visual depiction of the developmental trajectories for each group which show that after 6 month the FOYC exposed groups have elevated trajectories in comparison to the WW+BFOOY and WW+FOYC
Table 1.
Means and (standard deviations) of items related to condom-use by intervention exposure at baseline.
| Total (n=598) | WW1 +HFLE (n=51) | WW +BFOOY (n=179) | FOYC +HFLE (n=88) | FOYC +BFOOY (n=280) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Gender (Males %) | 266 | (44.5) | 19 | (37.3) | 72 | (40.2) | 46 | (52.3) | 129 | (46.1) |
| Age | 10.40 | (0.68) | 10.45 | (0.73) | 10.34 | (0.59) | 10.35 | (0.64) | 10.44 | (0.73) |
| Response Efficacy | 3.88 | (0.96) | 3.88 | (0.89) | 3.81 | (0.96) | 3.84 | (0.99) | 3.93 | (0.96) |
| Response Cost | 3.25 | (0.55) | 3.23 | (0.58) | 3.23 | (0.53) | 3.22 | (0.63) | 3.28 | (0.54) |
| Self-Efficacy | 2.31 | (1.17) | 2.44 | (1.23) | 2.30 | (1.15) | 2.41 | (1.29) | 2.26 | (1.12) |
| HIV Knowledge | 0.67 | (0.14) | 0.65 | (0.15) | 0.67 | (0.15) | 0.67 | (0.14) | 0.68 | (0.13) |
| Condom-use Skills | 0.55 | (0.13) | 0.54 | (0.13) | 0.53 | (0.13) | 0.55 | (0.14) | 0.56 | (0.12) |
| Intention to use a condom | 2.80 | (1.64) | 2.83 | (1.62) | 2.57 | (1.54) | 3.01 | (1.73) | 2.86 | (1.66) |
* p < 0.05
** p < 0.01
FOYC= Focus On Youth in the Caribbean (Grade 6 Intervention); BFOOY= Bahamian Focus On Older Youth (Grade 10 Intervention); HFLE= Health and Family Life Education (Grade 10 Control); WW= Wondrous Wetlands (Grade 6 Control).
Figure 2.
Means of condom-use perception related constructs over five years of participation in two HIV prevention intervention programs1
Figure 3.
Means of condom-use skills, HIV knowledge, and condom-use intention measured over five years of participation in two HIV prevention intervention programs1
Results of the mixed modeling found differences between groups on some variables, with the FOYC groups showing better performance (see Table 2). Both of the models examining response cost and response efficacy of condoms found significant increases in scores over time, but not for any intervention group(s) or for the interaction of time by intervention group. Condom-use self-efficacy increased over time with a significant effect of time and intervention for the WW+BFOOY group compared to the control group indicating a significant increase after the receipt of BFOOY.
Table 2.
Mixed model results of analyses examining the long term intervention impact of BFOOY and FOYC HIV prevention programs
| Condom-Use Skills | HIV/AIDS Knowledge | Self-Efficacy | Response Efficacy | Response Costs | Intention to use a Condom | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | t | β | SE | t | β | SE | t | β | SE | t | β | SE | t | β | SE | t | |
| Intercept | 0.51 | 0.02 | 33.49** | 0.52 | 0.01 | 22.93** | 2.39 | 0.13 | 18.05** | 3.90 | 0.11 | 36.10** | 3.35 | 0.06 | 55.96** | 2.92 | 0.19 | 15.70** |
| Gender | 0.20 | 0.01 | 3.18** | −0.03 | 0.01 | −4.13** | 0.37 | 12.76 | −6.52** | 0.16 | 0.05 | 3.49** | 0.00 | 0.02 | 0.21 | 0.03 | 0.07 | 0.51 |
| Time | 0.02 | 0.01 | 5.37** | 0.07 | 0.00 | 18.48** | 0.27 | 0.03 | 8.13** | 0.08 | 0.03 | 2.90* | −0.06 | 0.02 | −3.39** | 0.31 | 0.05 | 6.54** |
| Parent Intervention | 0.00 | 0.01 | 0.10 | 0.00 | 0.01 | 0.20 | −0.01 | 0.04 | −0.24 | 0.03 | 0.05 | 0.55 | 0.01 | 0.03 | 0.40 | 0.04 | 0.08 | 0.44 |
| Intervention | ||||||||||||||||||
| FOYC1+BFOOY | 0.04 | 0.02 | 2.40* | 0.06 | 0.02 | 2.72** | 0.14 | 0.16 | 0.88 | 0.12 | 0.13 | 0.94 | −0.01 | 0.07 | −0.21 | 0.33 | 0.22 | 1.56 |
| FOYC+HFLE | 0.05 | 0.02 | 2.68** | 0.04 | 0.02 | 2.63** | 0.27 | 0.16 | 1.66 | 0.09 | 0.14 | 0.63 | 0.03 | 0.08 | 0.43 | 0.07 | 0.23 | 2.01 |
| BFOOY+WW | 0.01 | 0.02 | 0.07 | 0.02 | 0.02 | 0.91 | −0.15 | 0.10 | −1.48 | −0.11 | 0.11 | −1.00 | −0.05 | 0.06 | −0.79 | −0.10 | 0.17 | −0.39 |
| Time*Intervention | ||||||||||||||||||
| FOYC+BFOOY | 0.02 | 0.01 | 3.81** | 0.00 | 0.00 | −0.72 | 0.07 | 0.04 | 1.76 | −0.02 | 0.03 | −0.69 | −0.01 | 0.02 | −0.74 | −0.03 | 0.05 | −0.62 |
| FOYC+HFLE | 0.01 | 0.01 | 2.19* | −0.01 | 0.01 | −1.27 | 0.05 | 0.04 | 1.21 | −0.01 | 0.03 | −0.30 | −0.02 | 0.02 | −1.13 | −0.06 | 0.06 | −1.10 |
| BFOOY+WW | 0.01 | 0.00 | 2.66** | 0.00 | 0.00 | −0.57 | 0.08 | 0.03 | 2.34** | −0.01 | 0.02 | −0.24 | 0.00 | 0.02 | −0.15 | −0.01 | 0.05 | 0.16 |
p<0.01
p<0.05
FOYC= Focus On Youth in the Caribbean (Grade 6 Intervention); BFOOY= Bahamian Focus On Older Youth (Grade 10 Intervention); HFLE= Health and Family Life Education (Grade 10 Control); WW= Wondrous Wetlands (Grade 6 Control).
Results of the mixed models examining HIV/AIDS knowledge and condom-use skills showed improvement by intervention group. Time, intervention group and the interaction of time by intervention group were all significant for condom-use skills. The effect of time indicates that youth show significant increases in condom-use skills as they age, independent of intervention status. When looking at the interaction of time and intervention subgroups, youth who received no intervention exposure (WW+HFLE) showed the least amount of improvement and scored significantly lower than any of the intervention exposed groups, WW+BFOOY, FOYC+HFLE, and FOYC+BFOOY. Time also significantly predicated HIV knowledge, showing an expected increase with age. Although the interaction of intervention group by time was not significant, intervention group effect was significant with the control group (WW+HFLE) having an overall lower mean than either FOYC exposure group (FOYC+BFOOY or FOYC+HFLE).
Significant effects regarding intention to use a condom were found for time and for intervention group. Specifically the FOYC+HFLE group significantly differed compared to the control group WW+HFLE. No significant result was found for the interaction of time and intervention group.
Discussion
This study investigates the long-term effects of two similar but age-appropriate HIV prevention intervention programs delivered at grade 6 and/or grade 10. We examined the impact of having received no intervention exposure compared to exposure to both or only one intervention. Because there were no differences between groups at baseline, results suggests that youth who completed the grade 6 interventions, FOYC, demonstrated overall elevated condom-use skills, HIV/AIDS knowledge, self-efficacy and intentions than did the control group (WW and HFLE). Condom-use skills continued to increase over time after receipt of the intervention in either or both grade 6 and 10.
These results suggest that for knowledge- or skill-based constructs, early exposure helps youth acquire and retain information for a longer period of time. Exposure to the intervention in grade 10 did not result in increased knowledge compared to control youth. However, the intervention youth compared to the control youth did show greater facility with condom-use skills. These results are consistent with prior research which found that receiving an intervention in early or both early and later childhood produced greater improvement than receipt only in later childhood [22,23].
The current study did not show an impact on the perceptual constructs (e.g., condom-use response efficacy and response costs) among either the grade 10 and/or grade 10 FOYC/BFOOY recipients compared to the control recipients, although the grade 6 intervention, FOYC, had been impacted perceptual outcomes [12-14]. Diminished impact from a sexual risk reduction intervention delivered later in adolescence may have several causes. The impact may be less apparent among older youth because the majority of youth have acquired sexual health knowledge from multiple sources by the time they have entered high school, producing a ceiling effect that is not present earlier during adolescence. This possibility underscores the importance of early intervention exposure. Younger youth who become sexually active are most vulnerable to sexual risk because they are less equipped with the appropriate knowledge and skills and would benefit the most from early intervention. Additionally, some of the information in the grade 10 intervention, BFOOY, overlaps with the HFLE curriculum (the current standard-of-care) such as HIV/AIDS prevention knowledge. However, the condom-use skills demonstration was specific to the FOYC and BFOOY interventions, which is evident by the consistently lower performance in condom-use skills scores among the control group (WW and HFLE). Outcomes such as intention and self-efficacy are also approaching a ceiling (see Figures 2A and 3C), thus limiting the amount of variation between groups [24].
Potential Limitations
As described under “Methods”, we had insufficient sample size to examine actual condom-use because of the low frequency of sexual intercourse. Although we controlled for parent intervention, the current analysis also did not enable us to disentangle the effects of all the possible parent and youth intervention exposure combinations. The Cronbach alphas were low for some of the scales, which may be attributed to the age of children as the alphas were lowest at the earliest assessments. As previously mentioned, the content of the HFLE curriculum delivered in grade 10 overlaps with some of the content in FOYC and BFOOY curriculum and thus may have diluted the effect. Finally, all youth were exposed to external prevention material outside of the classroom through the media and community in The Bahamas as part of the national HIV prevention campaign, although there is no reason to hypothesize that this exposure would have varied by intervention assignment.
Implications
This study indicates the need to provide youth with early interventions prior to the onset of sexual behavior and, ideally, to offer repeated intervention later in adolescence. Youth did retain knowledge and skills acquired from an intervention delivered during preadolescence, suggesting that early interventions should focus on acquiring knowledge-based skills and changing perceptions and intentions. For more mature youth, the curriculum could revisit knowledge and skills but primarily focus the content on changing perceptions, intentions and behavioral outcomes.
Acknowledgments
The authors thank the National Institute of Mental Health (R01 MH069229) and the Bahamian Ministries of Health and Education for their support.
Footnotes
Contributions and Implications
This study examined the importance of timing and frequency of exposure to risk reduction programs. To our knowledge this is the first study that has examined the effect of having been exposed to two randomized controlled trials of sexual risk prevention interventions at two different developmental periods during adolescence.
References
- 1.Centers for Disease Control and Prevention [August 1, 2008];HIV among youth [Web page] 2013 http://www.cdc.gov/hiv/risk/age/youth/. Published April 24, 2013.
- 2.Coates TJ, Richter L, Caceres C. HIV Prevention 3 - Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008;372(9639):669–684. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chin HB, Sipe TA, Elder R, et al. The Effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: Two systematic reviews for the guide to community preventive services. Am J Prev Med. 2012;42(3):272–294. doi: 10.1016/j.amepre.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: Their impact on sexual behaviors of young people throughout the world. J Adolesc Health. 2007;40(3):206–217. doi: 10.1016/j.jadohealth.2006.11.143. [DOI] [PubMed] [Google Scholar]
- 5.Wellings K, Wadsworth J, Johnson AM, Field J, Whitaker L, Field B. Provision of sex education and early sexual experience: The relation examined. BMJ. 1995;311(7002):417–420. doi: 10.1136/bmj.311.7002.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: Their impact on sexual behaviors of young people throughout the world. J Adolesc Health. 2007;40(3):206–217. doi: 10.1016/j.jadohealth.2006.11.143. [DOI] [PubMed] [Google Scholar]
- 7.Picot J, Shepherd J, Kavanagh J, et al. Behavioural interventions for the prevention of sexually transmitted infections in young people aged 13-19 years: A systematic review. Health Educ Res. 2012;27(3):495–512. doi: 10.1093/her/cys014. [DOI] [PubMed] [Google Scholar]
- 8.Pedlow CT, Carey M. Developmentally appropriate sexual risk reduction interventions for adolescents: Rationale, review of interventions, and recommendations for research and practice. Ann Behav Med. 2004;27(3):172–184. doi: 10.1207/s15324796abm2703_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinberg L. Risk taking in adolescence - New perspectives from brain and behavioral science. Curr Dir Psychol Sci. 2007;16(2):55–59. [Google Scholar]
- 10.Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. Am J Psychiatry. 2003;160(6):1041–1052. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention [July 5, 2013];Compendium of evidence-based HIV behavioral interventions. 2013 http://www.cdc.gov/hiv/prevention/research/compendium/rr/complete.html.
- 12.Chen XG, Lunn SJ, Deveaux L, et al. A cluster randomized controlled trial of an adolescent HIV prevention program among Bahamian youth: Effect at 12 months post-intervention. AIDS Behav. 2009;13(3):499–508. doi: 10.1007/s10461-008-9511-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deveaux L, Stanton B, Lunn S, et al. Reduction in human immunodeficiency virus risk among youth in developing countries. Arch Pediat Adol Med. 2007;161(12):1130–1139. doi: 10.1001/archpedi.161.12.1130. [DOI] [PubMed] [Google Scholar]
- 14.Gong J, Stanton B, Lunn S, et al. Effects through 24 months of an HIV/AIDS prevention intervention program based on protection motivation theory among preadolescents in the Bahamas. Pediatrics. 2009;123(5):E917–E928. doi: 10.1542/peds.2008-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller KS, Levin ML, Whitaker DJ, Xu XH. Patterns of condom use among adolescents: The impact of mother-adolescent communication. Am J Public Health. 1998;88(10):1542–1544. doi: 10.2105/ajph.88.10.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers For Disease Control and PRevention [CDC] [March 25, 2012];Diffusion of Effective Behavioral Interventions (DEBI) 2012 www.effectiveinterventions.org.
- 17.Rodgers R. Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In: Caaioppi T, Petty R, editors. Social Psychology. Guilford Press; New York, NY: 1983. pp. 153–176. [Google Scholar]
- 18.Stanton B, Black M, Feigelman S, et al. Development of a culturally, theoretically and developmentally based survey instrument for assessing risk behaviors among African-American early adolescents living in urban low-Income neighborhoods. AIDS Educ Prev. 1995;7(2):160–177. [PubMed] [Google Scholar]
- 19.Dinaj-Koci V, Chen X, Deveaux L, et al. Developmental implications of HIV prevention during adolescence: Examination of the long-term impact of HIV prevention interventions delivered in randomized controlled trials in grade six and in grade 10. Youth Soc. 2012 doi: 10.1177/0044118X12456028. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stanton B, Deveaux L, Lunn S, et al. Condom-use Skills Checklist: A proxy for assessing condom-use knowledge and skills when direct observation is not possible. J Health Popul Nutr. 2009;27(3):406–413. doi: 10.3329/jhpn.v27i3.3383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stanton B, Chen XG, Koci V, et al. Effect of a grade 6 HIV risk reduction intervention four years later among students who were and were not enrolled in the study trial. J Adolesc Health. 2012;50(3):243–249. doi: 10.1016/j.jadohealth.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gottlieb G, Blair C. How early experience matters in intellectual development in the case of poverty. Prev Sci. 2004;5(4):245–252. doi: 10.1023/b:prev.0000045358.12782.6b. [DOI] [PubMed] [Google Scholar]
- 23.Hawkins JD, Catalano RF, Kosterman R, Abbott R, Hill KG. Preventing adolescent health-risk behaviors by strengthening protection during childhood. JAMA Pediatr. 1999;153(3):226–234. doi: 10.1001/archpedi.153.3.226. [DOI] [PubMed] [Google Scholar]
- 24.Stucki G, Stucki S, Brühlmann P, Michel BA. Ceiling effects of the health assessment questionnaire and its modified version in some ambulatory rheumatoid arthritis patients. Ann Rheum Dis. 1995;54(6):461–465. doi: 10.1136/ard.54.6.461. [DOI] [PMC free article] [PubMed] [Google Scholar]