Abstract
Objective:
Cell-based therapies are being investigated as an adjunct to IV thrombolysis or mechanical thrombectomy in ischemic stroke. This review summarizes the potential applications as well as challenges of intravascular cell delivery in ischemic stroke.
Method:
We conducted a search of Medline as well as the clinicaltrials.gov Web site for all ongoing human clinical studies using stem cells in ischemic stroke patients.
Result:
The pros and cons of the various donor cell types and routes of cell delivery, including intravascular delivery, in ischemic stroke are discussed. In addition, the potential challenges in translation from bench to bedside, the optimal techniques for intravascular cell delivery, and an updated comprehensive list of ongoing clinical trials in ischemic stroke are highlighted.
Conclusions:
Stem cells have shown a promising role in ischemic stroke, in preclinical studies as well as initial pilot studies. Further studies are needed to assess intravascular cell therapy as a potential adjunct to thrombolysis or mechanical thrombectomy in ischemic stroke.
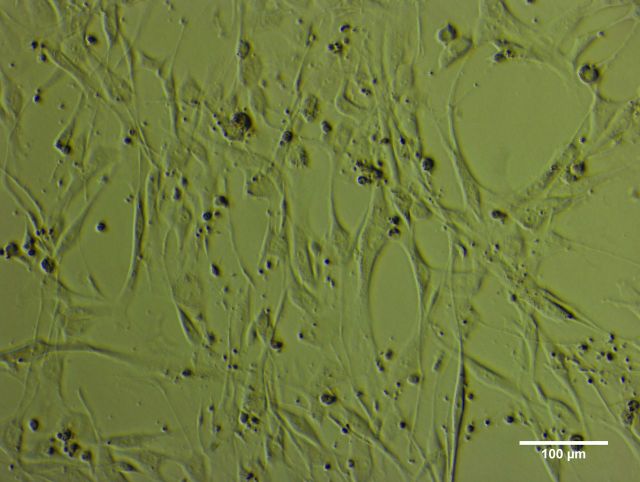
Cell therapy is emerging as a promising new modality for enhancing neurologic recovery in ischemic stroke.1 Numerous basic science studies have demonstrated positive results in animal models of ischemic stroke following implantation of progenitor cells derived from various sources, including adipose, human fetal/embryonic tissue, bone marrow, peripheral, and umbilical cord blood (figure).2 These animal studies have utilized various methods of cell delivery or implantation (table 1), including direct intracerebral (IC) injection, intracisternal/cerebro-ventricular (ICV), or intravascular routes of delivery such as IV or intra-arterial (IA) infusion.
Figure. Phase contrast image of human umbilical cord blood stem cells.
Table 1.
Routes of cell delivery
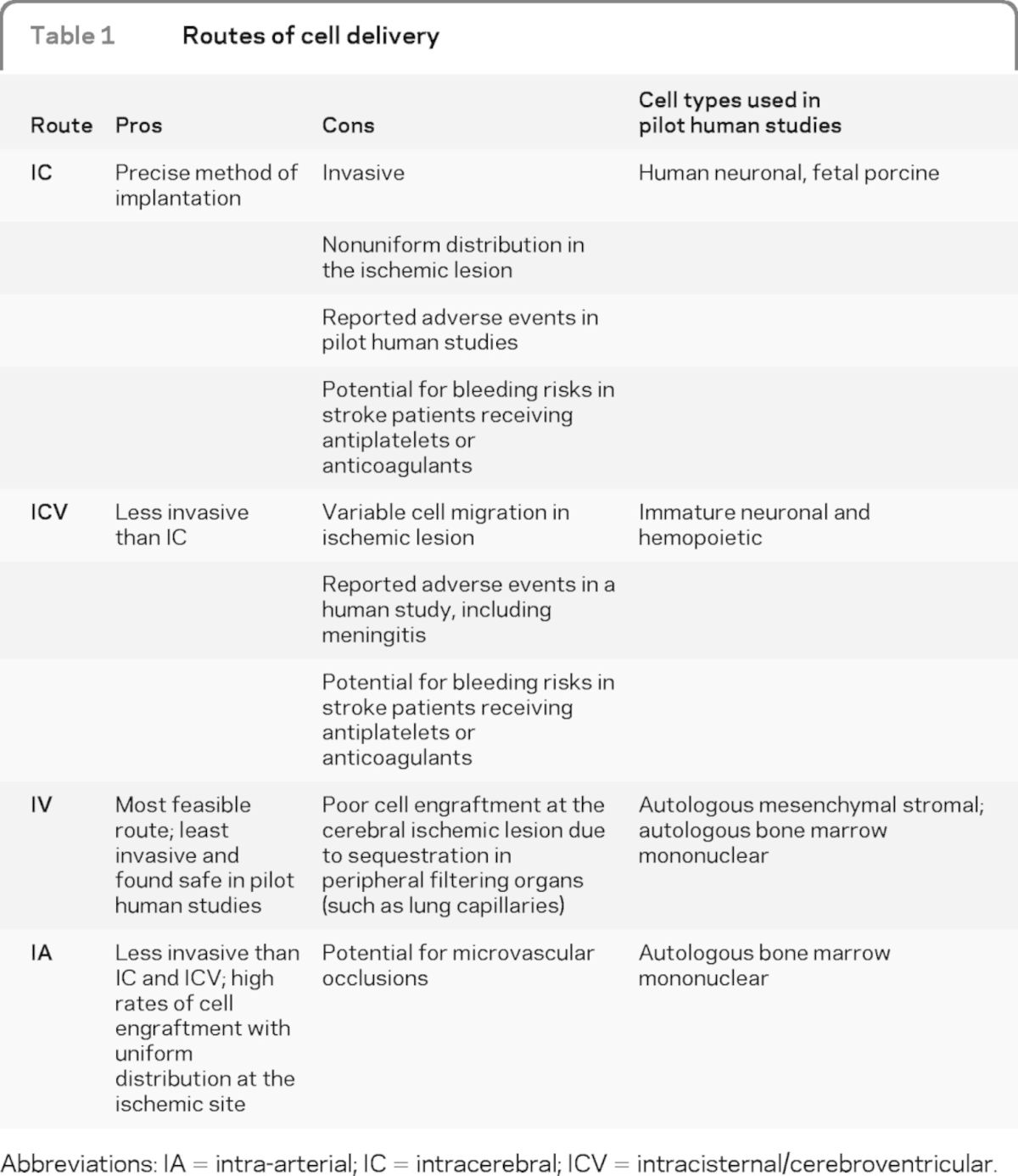
Abbreviations: IA = intra-arterial; IC = intracerebral; ICV = intracisternal/cerebroventricular.
Methods of cellular delivery and implantation.
Intracerebral.
Direct injection is invasive, and despite being a precise method of cellular delivery and implantation, it results in a poor distribution of cells in the target lesion.3 Initial pilot human studies investigating stereotactic IC cell implantation in patients with chronic stroke also reported adverse events, including seizures, syncope, asymptomatic subdural hematoma, transient motor worsening, and enhancing lesions on MRI.4,5
Intracisternal/cerebroventricular.
The ICV route of cell delivery is less invasive than direct IC implantation but is also associated with variable cell migration to the ischemic site.6,7 In a pilot human study investigating ICV delivery in 10 chronic stroke patients (7 ischemic and 3 hemorrhagic), some patients developed fever and meningeal signs 48 hours after cellular delivery via ICV route.8
IV.
Infusion is the least invasive method, allowing wide distribution of cells with exposure to chemotactic signals that potentially guide them toward the target ischemic lesion. This method, however, results in cells being trapped by peripheral organs, including the lungs, liver, and spleen, thereby limiting potential engraftment in the ischemic lesion in the brain.2 Since patients with ischemic stroke commonly have associated cardiac and renal impairment, there is also a potential for the cells reaching these organs, with further reduction in cell delivery to the ischemic brain.9,10 Given that IV cell delivery is least invasive, this method of delivery has been investigated in patients with chronic stroke. In a placebo-controlled phase I/II trial of 30 patients with chronic stroke, 5 in the treated group received autologous mesenchymal stromal cells at 1 to 2 months from the onset of symptoms. This method was reportedly safe and feasible in the short term,11 as well as on long-term follow-up, with improved neurologic recovery in those patients receiving cellular therapy.12 Another unblinded single-arm study demonstrated safety and feasibility with IV infusion of autologous mesenchymal cells in 12 patients post–stroke onset (range, 36–133 days).13 Until recently, all human studies had reported results in chronic stroke patients. Recently, an open-label prospective human study demonstrated safety and feasibility with IV mononuclear cell infusion in 10 patients with acute stroke.14 Patients in this study underwent bone marrow harvest and subsequent IV cell infusion within 24 to 72 hours of stroke onset. This methodology is supported by a preclinical study in which rats with common carotid artery/middle cerebral artery occlusion performed better on neurologic tests with IV mononuclear cells infused up to 72 hours, compared with 1 week from stroke onset.15 However, similar to prior animal experiments, this study also found cells sequestered in the spleen, lung, liver, and kidney.
Intra-arterial.
Cell delivery involves endovascular infusion of progenitor cells directly in the artery perfusing the ischemic tissue. This route of cell delivery also bypasses the peripheral filtering organs, thereby increasing cell delivery to the target ischemic tissue with uniform distribution. Animal studies have demonstrated higher rates of cell engraftment with IA delivery,16,17 as well as a higher concentration of cells in the target ischemic lesion with IA,16 compared with IV cell infusion.18,19 One preclinical study comparing IV and IA autologous bone marrow mononuclear cell (BMMNC) delivery found significant reduction in infarct volume, higher cell engraftment, and improved motor function with IA delivery.20 The authors attributed this “significant neuroprotective effect ” in the IA group to the larger number of implanted cells in the brain during early reperfusion. Despite the advantage of increased cell homing in the ischemic lesion, few animal studies have also raised concern with the potential for microvascular occlusion, worsening ischemia, and higher mortality with IA delivery.19,21 A recent preclinical study investigated the etiology of cerebral blood flow reduction and microvascular occlusion following IA neural progenitor cell infusion.22 The investigators attributed the microstrokes to the prior procedural technique, but that can be overcome with preserved anterograde flow.22
Mechanisms of action of stem cells in ischemic stroke.
Preclinical studies on the use of stem cells for the treatment of stroke have now clearly demonstrated that the administration of different types and sources of stem cells can ameliorate neurologic deficits, and in some cases significantly reduce the size of the infarct. For example, IV administration of human cord blood stem cells into laboratory rodents 2 days after ischemic stroke has been shown to reduce infarct lesion volume by approximately 50% and improve neurologic function by approximately 55%.23
Early studies of stem cell therapy for treating stroke were based on the rationale of replacing neural cells that were lost as a result of ischemic brain injury. These cells could be neuronal, astrocytic, oligodendroglial, or endothelial in phenotype. However, it has now become clear that in spite of improvements in neurologic outcome and reductions in infarct size, the mechanism of cell replacement in stem cell therapy for stroke appears to play a more modest role than originally envisioned. Recent reports have shown that the administration of stem cells in animals with stroke can induce the reinstatement of functional connectivity, as determined by functional MRI.24 This, in turn, may be mediated by the outgrowth of nerve fibers of endogenous neurons.23,25 Other studies have demonstrated that stem cell therapy results in the upregulation of growth factors that may be responsible for the outgrowth of these endogenous fiber processes26 and for the inhibition of inflammatory processes,27 which may lead to secondary cell loss within the brain. These observations offer intriguing alternative mechanisms that may underlie the restorative effects noted with stem cell therapy following stroke and provide a rationale basis for clinical trials.
Challenges in translating intravascular cellular delivery from bench to the bedside.
All routes of cell delivery have appeared promising in animal studies, although the intravascular routes of delivery such as IV and IA are less invasive than IC and ICV routes. Despite promising results in animal studies, several key questions remain to be answered before proceeding to human trials, such as choice of cells for delivery or implantation (table 2), the timing of cellular therapy, and the dose of cells delivered or implanted. Despite these knowledge gaps, initial clinical trials investigating cell therapy in chronic as well as subacute strokes have already begun worldwide (table 3).
Table 2.
Donor cell types
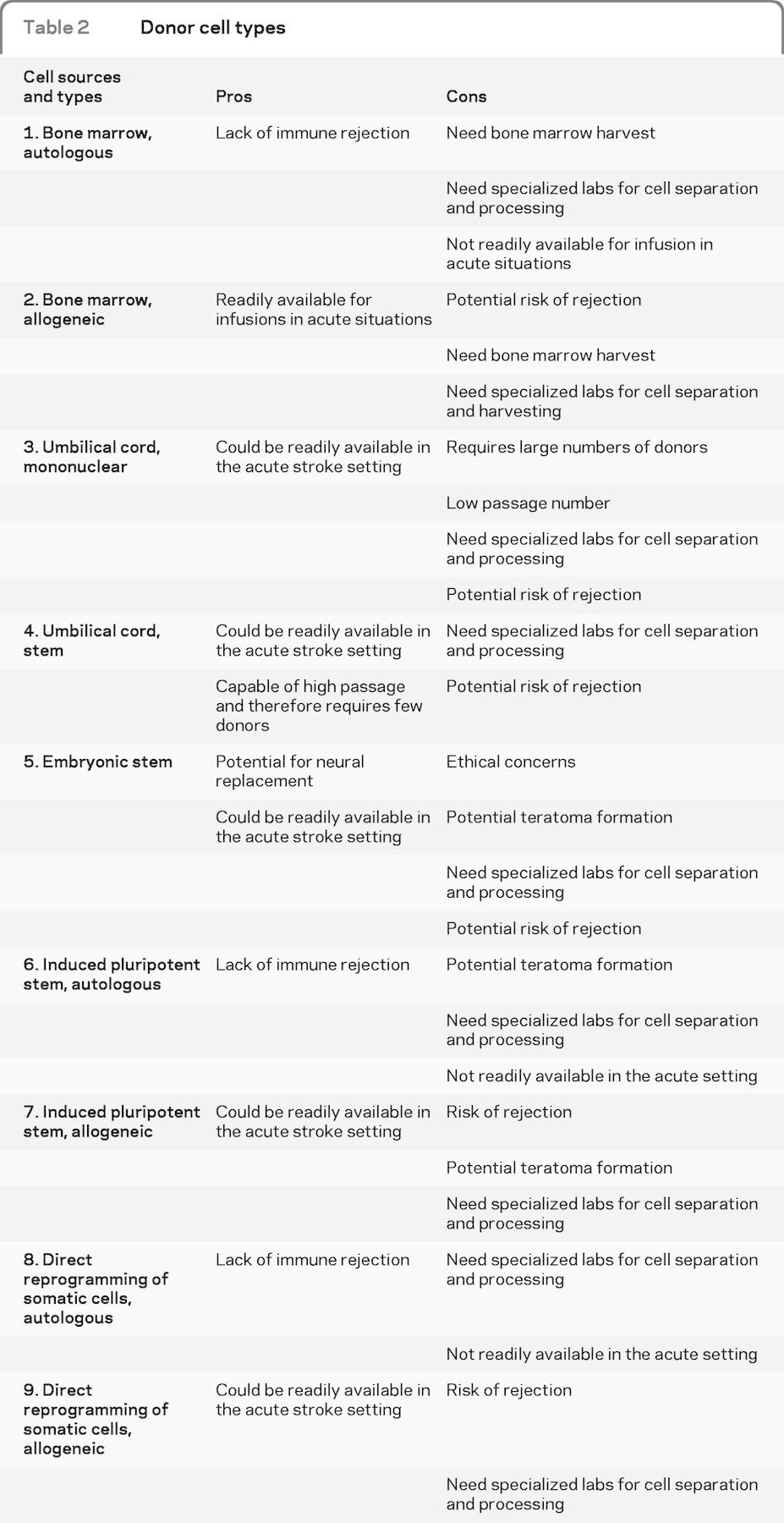
Table 3.
Ongoing clinical trials
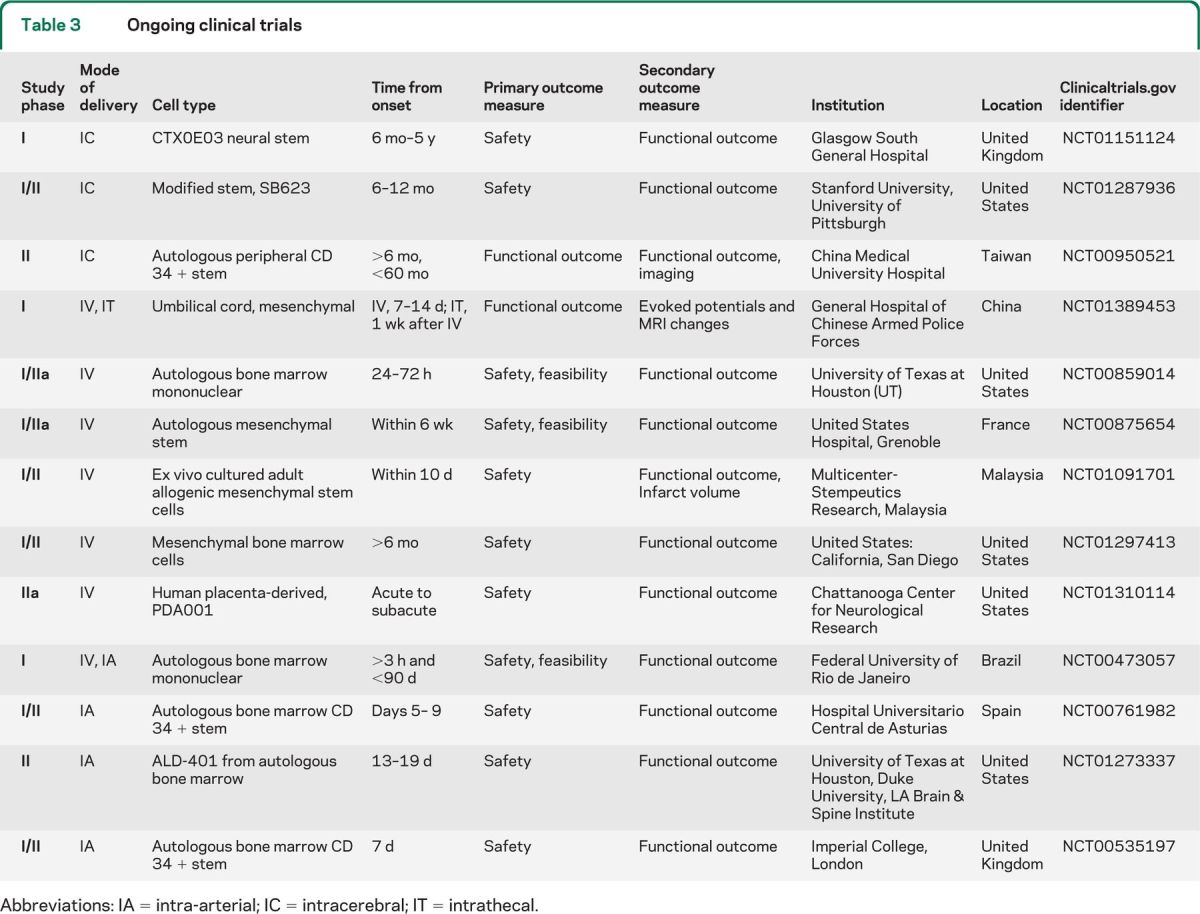
Abbreviations: IA = intra-arterial; IC = intracerebral; IT = intrathecal.
Choice of cells.
The authors describe the pros and cons of the various donor cell types and their relevance to acute ischemic stroke (table 2). The longer timeframe required for obtaining cells from autologous sources limits their potential application in patients with hyperacute strokes. Cells derived from umbilical cord23,28 or placenta29 could be potentially investigated in clinical studies in patients receiving IV or IA thrombolytic therapy in the initial few hours after a stroke.
Timing of cell therapy.
Unlike IV or IA revascularization therapies, there are no clearly defined therapeutic time windows for cell therapy with all routes of delivery. Since most ongoing human studies use cells from autologous sources, these trials are investigating therapeutic windows ranging from a few days to several months.
Dose.
Preclinical studies have demonstrated a dose–response relationship, with higher IV cell dose resulting in smaller infarct volumes.30–31 Given that IV infusion results in sequestration of cells in peripheral organs, it is theoretically conceivable that IA delivery could produce similar results with lesser cell doses; however, the optimal dose for IV or IA therapy is unclear. The initial clinical studies have essentially focused on feasibility of autologous cell procurement and the maximum viable cell dose that could be safely obtained prior to delivery.
Intra-arterial cell delivery in cardiac and peripheral vascular disease.
Numerous initial clinical studies investigating IA cell delivery in patients post–myocardial infarction have demonstrated a trend toward improved clinical outcomes as well as physiologic parameters (increased contractility and improved myocardial perfusion, with decreased infarct size and end-systolic volume).32 These studies primarily utilized autologous bone marrow–derived cells and did not report any significant adverse events. Along similar lines, patients with peripheral vascular disease treated in clinical studies with IA or combined IA and IM injections of autologous bone marrow cells have demonstrated favorable outcomes so far.33 These studies also reported no significant adverse events, with improved ankle-brachial index, decreased claudication, and improved walking distance.
Preliminary human experience with intra-arterial cell delivery in ischemic stroke.
In the first reported case of IA cell delivery in ischemic stroke, the authors performed IA autologous BMMNC infusion in a patient with left middle cerebral artery distribution infarct, 3 days after symptom onset.34 Prior to infusion, transcranial Doppler demonstrated intracranial arterial patency. The authors also reported a decrease in hypoperfusion on SPECT as well as increased metabolism in the ischemic tissue, 7 days after IA cell delivery. They subsequently reported another patient who underwent IA autologous BMMNC delivery in the left middle cerebral artery 9 days after stroke onset.35 They also labeled 1% of these cells with Tc-99m by incubating with hexamethylpropylene amine oxime and subsequently performed SPECT scanning, 8 hours following the IA infusion. They reported good clinical recovery and also mentioned that this method of in vivo cell tracking could be safe in humans after IA delivery.
More recently, a pilot study reported safety in IA BMMNC delivery in the middle cerebral artery in patients with chronic stroke.36 They reported no symptomatic worsening or significant adverse effects. One patient developed asymptomatic spike-wave activity following infusion. Two patients developed seizures 6 months after infusion, which were deemed unrelated to the infusion and treated with antiepileptic drugs.
Optimal endovascular techniques for intra-arterial cell delivery in ischemic stroke.
As demonstrated by preclinical studies, prespecified endovascular technical details are the key to safety of this route of cell delivery. In patients with myocardial infarction receiving intracoronary cell delivery, the interventionalists used an over-the-wire single balloon catheter that was inflated to occlude flow for a few minutes, during which the cells were infused in the coronaries distal to the occlusion through the lumen of the balloon catheter. This maneuver was performed to allow for adhesion and transendothelial migration of the infused cells.37 The balloon would then be deflated to allow anterograde coronary flow, and this procedure was repeated until all the cells were delivered. Similarly, a double-balloon occlusion technique with ports in between the 2 balloons has been used for IA delivery of a high concentration of chemotherapeutic agents.38 Although the single or double balloon techniques have shown promise,37,38 this might not necessarily be the case in the more fragile cerebral blood vessel.39 As demonstrated recently in a preclinical study, preserved anterograde flow in the parent artery during IA cell delivery might be a safer technique in the craniocerebral vasculature.22
It is critical to have pre-established flow rates that do not affect viability of specific stem cells, with use of different microcatheters, heparinized saline, and angiographic contrast agents. A study has demonstrated that infusion of 10 million cells/mL through the Excelsior SL-10 microcatheter (Boston Scientific, Fremont, CA) at rates of up to 2 mL/min under standard temperature conditions did not affect viability of BMMNCs.40 Cell viability was also unaffected with exposure to Omnipaque (Nycomed, Princeton, NJ) and low-dose heparin (2.5 U/mL) for 1 hour. There was a noticeable reduction in viability of BMMNCs at a concentration of 10 million cells/mL with infusion rates in excess of 2 mL/min and exposure to high-dose heparin (500 U/mL) for 1 hour. Another study demonstrated that infusion of human umbilical cord blood cells through the Excelsior SL-10 microcatheter (Boston Scientific) at concentration of 10 million cells/mL led to a reduction in viability.41 There was no affect on viability of these cells at a concentration of 1 million cells/mL, regardless of flow rates.
DISCUSSION
Cell-based therapy is a potential adjunct therapeutic modality to acute revascularization therapies (IV thrombolysis or mechanical thrombectomy) for improved neurologic recovery in stroke patients. Despite the challenges in clinical translation from basic science studies, initial pilot studies have demonstrated safety and feasibility with IV and IA cell delivery. The ongoing clinical trials using various delivery routes, choice of cells, timing of therapy, and doses of cells are likely to bridge the knowledge gaps that exist with this therapy for patients with ischemic stroke.
GLOSSARY
- BMMNC
bone marrow mononuclear cell
- IA
intra-arterial
- IC
intracerebral
- ICV
intracisternal/cerebroventricular
Footnotes
Go to Neurology.org for full disclosures. Disclosures deemed relevant by the authors, if any, are provided at the end of this article.
AUTHOR CONTRIBUTIONS
Dr. Misra: drafting/revising the manuscript, study concept or design, analysis or interpretation of data. Mr. Ritchie: drafting/revising the manuscript, analysis or interpretation, acquisition of data. Ms. Stone and Dr. Low: drafting/revising the manuscript, study concept or design. Dr. Janardhan: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, study supervision.
DISCLOSURE
Dr. Misra reports no disclosures. Mr. Ritchie holds stock in Novartis AG. Ms. Stone reports no disclosures. Dr. Low holds patents for biomarkers for ovarian cancer and biomarkers for breast cancer; serves as a consultant for Saneron CCEL; receives research support from NIH and HRK Foundation; receives research support from the University of Minnesota, AOSpine, International Organization of Glutaric Aciduria, and Gateway Foundation; and holds stock or stock options or expense compensation for serving on a board of directors from Saneron CCEL. Dr. Janardhan reports no disclosures. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Savitz SI, Chopp M, Deans R, Carmichael ST, Phinney D, Wechsler L. Stem Cell Therapy as an Emerging Paradigm for Stroke (STEPS) II. Stroke 2011;42:825–829 [DOI] [PubMed] [Google Scholar]
- 2.Misra V, Yang B, Sharma S, Savitz SI. Cell-based therapy for stroke. In: Cox C,editor. Progenitor Cell Therapy for Neurological Injury. New York: Springer; 2011:143–162 [Google Scholar]
- 3.Li Y, Chopp M, Chen J, et al. Intrastriatal transplantation of bone marrow nonhematopoietic cells improves functional recovery after stroke in adult mice. J Cereb Blood Flow Metab 2000;20:1311–1319 [DOI] [PubMed] [Google Scholar]
- 4.Kondziolka D, Steinberg GK, Wechsler L, et al. Neurotransplantation for patients with subcortical motor stroke: a phase 2 randomized trial. J Neurosurg 2005;103:38–45 [DOI] [PubMed] [Google Scholar]
- 5.Savitz SI, Dinsmore J, Wu J, Henderson GV, Stieg P, Caplan LR. Neurotransplantation of fetal porcine cells in patients with basal ganglia infarcts: a preliminary safety and feasibility study. Cerebrovasc Dis 2005;20:101–107 [DOI] [PubMed] [Google Scholar]
- 6.Jiang Q, Zhang ZG, Ding GL, et al. Investigation of neural progenitor cell induced angiogenesis after embolic stroke in rat using MRI. Neuroimage 2005;28:698–707 [DOI] [PubMed] [Google Scholar]
- 7.Modo M, Stroemer RP, Tang E, Patel S, Hodges H. Effects of implantation site of stem cell grafts on behavioral recovery from stroke damage. Stroke 2002;33:2270–2278 [DOI] [PubMed] [Google Scholar]
- 8.Rabinovich SS, Seledtsov VI, Banul NV, et al. Cell therapy of brain stroke. Bull Exp Biol Med 2005;139:126–128 [DOI] [PubMed] [Google Scholar]
- 9.Hauger O, Frost EE, van Heeswijk R, et al. MR evaluation of the glomerular homing of magnetically labeled mesenchymal stem cells in a rat model of nephropathy. Radiology 2006;238:200–210 [DOI] [PubMed] [Google Scholar]
- 10.Kraitchman DL, Tatsumi M, Gilson WD, et al. Dynamic imaging of allogeneic mesenchymal stem cells trafficking to myocardial infarction. Circulation 2005;112:1451–1461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bang OY, Lee JS, Lee PH, Lee G. Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol 2005;57:874–882 [DOI] [PubMed] [Google Scholar]
- 12.Lee JS, Hong JM, Moon GJ, Lee PH, Ahn YH, Bang OY;STARTING Collaborators. A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells 2010;28:1099–1106 [DOI] [PubMed] [Google Scholar]
- 13.Honmou O, Houkin K, Matsunaga T, et al. Intravenous administration of auto serum-expanded autologous mesenchymal stem cells in stroke. Brain 2011;134:1790–1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Savitz SI, Misra V, Kasam M, et al. Intravenous autologous bone marrow mononuclear cells for ischemic stroke. Ann Neurol 2011;70:59–69 [DOI] [PubMed] [Google Scholar]
- 15.Yang B, Strong R, Sharma S, et al. Therapeutic time window and dose response of autologous bone marrow mononuclear cells for ischemic stroke. J Neurosci Res 2011;89:833–839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guzman R, De Los Angeles A, Cheshier S, et al. Intracarotid injection of fluorescence activated cell-sorted CD49d-positive neural stem cells improves targeted cell delivery and behavior after stroke in a mouse stroke model. Stroke 2008;39:1300–1306 [DOI] [PubMed] [Google Scholar]
- 17.Shen LH, Li Y, Chen J, et al. Intracarotid transplantation of bone marrow stromal cells increases axon–myelin remodeling after stroke. Neuroscience 2006;137:393–399 [DOI] [PubMed] [Google Scholar]
- 18.Liu H, Honmou O, Harada K, et al. Neuroprotection by PlGF gene-modified human mesenchymal stem cells after cerebral ischaemia. Brain 2006;129:2734–2745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li L, Jiang Q, Ding G, et al. Effects of administration route on migration and distribution of neural progenitor cells transplanted into rats with focal cerebral ischemia, an MRI study. J Cereb Blood Flow Metab 2010;30:653–662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamiya N, Ueda M, Igarashi H, et al. Intra-arterial transplantation of bone marrow mononuclear cells immediately after reperfusion decreases brain injury after focal ischemia in rats. Life Sci 2008;83:433–437 [DOI] [PubMed] [Google Scholar]
- 21.Walczak P, Zhang J, Gilad AA, et al. Dual-modality monitoring of targeted intraarterial delivery of mesenchymal stem cells after transient ischemia. Stroke 2008;39:1569–1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chua JY, Pendharkar AV, Wang N, et al. Intra-arterial injection of neural stem cells using a microneedle technique does not cause microembolic strokes. J Cereb Blood Flow Metab 2011;31:1263–1271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xiao J, Nan ZH, Motooka Y, Low WC. Transplantation of a novel cell line population of umbilical cord blood stem cells ameliorates neurological deficits associated with ischemic brain injury. Stem Cells Dev 2005;14:722–733 [DOI] [PubMed] [Google Scholar]
- 24.Ramos-Cabrer P, Justicia C, Wiedermann D, Hoehn M. Stem cell mediation of functional recovery after stroke. PLoS One 2010;5:e12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daadi MM, Davis AS, Arac A, et al. Human neural stem cell grafts modify microglial response and enhance axonal sprouting in neonatal hypoxic-ischemic brain injury. Stroke 2010;41:516–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang M, Wei X, Li J, Heine LA, Rosenwasser R, Lacovitti L. Changes in host blood factors and brain glia accompanying the functional recovery after systemic administration of bone marrow stem cells in ischemic stroke rats. Cell Transp 2010;9:1973–1984 [DOI] [PubMed] [Google Scholar]
- 27.Walker PA, Letourneau PA, Bedi S, Shah SK, Jimenez F, Cox CS. Progenitor cells as remote “bioreactors”: neuroprotection via modulation of the systemic inflammatory response. World J Stem Cells 2011;3:9–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nan ZH, Grande A, Sanberg CD, Sanberg PR, Low WC. Infusion of human umbilical cord blood ameliorates neurologic deficits in rats with hemorrhagic brain injury. Ann NY Acad Sci 2005;1049:84–96 [DOI] [PubMed] [Google Scholar]
- 29.Kranz A, Wagner DC, Kamprad M, et al. Transplantation of placenta-derived mesenchymal stromal cells upon experimental stroke in rats. Brain Res 2010;1315:128–136 [DOI] [PubMed] [Google Scholar]
- 30.Vendrame M, Cassady J, Newcomb J, et al. Infusion of human umbilical cord blood cells in a rat model of stroke dose-dependently rescues behavioral deficits and reduces infarct volume. Stroke 2004;35:2390–2395 [DOI] [PubMed] [Google Scholar]
- 31.Honma T, Honmou O, Iihoshi S, et al. Intravenous infusion of immortalized human mesenchymal stem cells protects against injury in a cerebral ischemia model in adult rat. Exp Neurol 2006;199:56–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dimmeler S, Zeiher AM. Cell therapy of acute myocardial infarction: open questions. Cardiology 2009;113:155–160 [DOI] [PubMed] [Google Scholar]
- 33.Lawall H, Bramlage P, Amann B. Stem cell and progenitor cell therapy in peripheral artery disease: a critical appraisal. Thromb Haemost 2010;103:696–709 [DOI] [PubMed] [Google Scholar]
- 34.Mendonça ML, Freitas GR, Silva SA, et al. Safety of intra-arterial autologous bone marrow mononuclear cell transplantation for acute ischemic stroke. Arq Bras Cardiol 2006;86:52–55 [DOI] [PubMed] [Google Scholar]
- 35.Correa PL, Mesquita CT, Felix RM, et al. Assessment of intra-arterial injected autologous bone marrow mononuclear cell distribution by radioactive labeling in acute ischemic stroke. Clin Nucl Med 2007;32:839–841 [DOI] [PubMed] [Google Scholar]
- 36.Battistella V, de Freitas GR, da Fonseca LM, et al. Safety of autologous bone marrow mononuclear cell transplantation in patients with nonacute ischemic stroke. Regen Med 2011;6:45–52 [DOI] [PubMed] [Google Scholar]
- 37.Assmus B, Schächinger V, Teupe C, et al. Transplantation Of Progenitor Cells And Regeneration Enhancement in Acute Myocardial Infarction (TOPCARE-AMI). Circulation 2002;106:3009–3017 [DOI] [PubMed] [Google Scholar]
- 38.Terai Y, Kanemura M, Sasaki H, et al. Long-term follow-up of neoadjuvant intraarterial chemotherapy using an original four-lumen double-balloon (4L-DB) catheter for locally advanced uterine cervical cancer. Int J Clin Oncol 2009;14:56–62 [DOI] [PubMed] [Google Scholar]
- 39.Janardhan V, Biondi A, Riina H, Sanelli PC, Stieg PE, Gobin YP. Vasospasm in aneurysmal subarachnoid hemorrhage: diagnosis, prevention, and management. Neuroimaging Clin North Am 2006;16:483–496 [DOI] [PubMed] [Google Scholar]
- 40.El Khoury R, Misra V, Sharma S, et al. The effect of transcatheter injections on cell viability and cytokine release of mononuclear cells. AJNR Am J Neuroradiol 2010;31:1488–1492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Janardhan V, Qureshi AI, Low WC. Intravascular delivery systems for stem cell transplantation for neurological disorders. In: Low WC, Verfaillie CM,eds. Stem Cells and Regenerative Medicine. Singapore: World Scientific Publishing; 2008:355–396 [Google Scholar]