Abstract
Background: The present study was conducted to assess the relationship between drinking water fluoride (F) levels, dental fluorosis and dental caries among 9-12 years old school children of Nelakondapally Mandal, Khammam district, Andhra Pradesh. Materials and Methods: A cross-sectional analytical study was conducted on 1500 school children aged 9-12 years, selected by stratified random sampling from different areas with different levels of naturally occurring F in drinking water. The children were assessed for dental fluorosis according to WHO basic survey guidelines. The overall oral health status of the child was assessed by decayed missing filled teeth (DMFT)/dmft index. Statistical analysis was done using mean, standard deviation, standard error, Z-test, ANOVA test, and Chi-square test. Results: The results of the present study revealed that the prevalence of fluorosis was 74.9%. Number of children having dental fluorosis was highest in children who consume water from bore wells. Caries prevalence in the study population was about 56.5%. Caries prevalence and mean DMFT/dmft scores were least in children with optimal F areas and highest in children with below optimal F areas. Conclusion: There was moderate prevalence of fluorosis in Nelakondapally Mandal of Khammam district, and caries prevalence is high in areas below optimal F areas. How to cite the article: Shanthi M, Reddy BV, Venkataramana V, Gowrisankar S, Reddy BV, Chennupati S. Relationship between drinking water fluoride levels, dental fluorosis, dental caries and associated risk factors in 9-12 year old school children of Nelakondapally Mandal of Khammam district, Andhra Pradesh, India: A cross-sectional survey. J Int Oral Health 2014;6(3):106-10.
Key words: : Child dental caries, Dean’s fluorosis index, DMFT/dmft index, dental fluorosis, fluoride
Introduction
Dental caries remains a major public health problem in most of the industrialized countries, affecting 60-90% of school children and the vast majority of adults according to WHO report. It is also the most prevalent oral disease in several Asian and Latin American countries. The incidence of dental caries is increasing due to high consumption of sugars and inadequate exposure to fluoride (F). 1
Among all the caries-preventive strategies, discovery of F and its remarkable properties in the prevention of dental caries is a classic example of extensive epidemiological research conducted in various parts of the world. The cariostatic effect of F occurs when F gets incorporated into the enamel during tooth development, whereas dental fluorosis results in the hypo mineralization of tooth enamel due to the continuous ingestion of the excessive amount of F during tooth development. This results in a variety of pathological changes in the structure of teeth. If this is not prevented during childhood it can hamper dental esthetics and psychological well-being of the child. 2 In such scenario dental fluorosis is regarded as an unfortunate side-effect to F’s caries-protective benefits. 3
Over the last decade, there has been some concern about the prevalence of fluorosis all over the world, India being one of them. 4 , 5 Fluorosis is endemic in 20 states of India and it continuous to remain a challenging national dental health problem. Nelakondapally Mandal of Khammam district is one such endemic fluorosis area of Andhra Pradesh, where most of the habitations have high F levels in the drinking water. Until today, no data is available on the prevalence of fluorosis and caries in this district. This makes Nelakondapally Mandal an ideal place for the present descriptive epidemiological study, to determine the caries experience in children having dental fluorosis and the correlation between these two interrelated oral afflictions.
Materials and Methods
Study design
A cross-sectional analytical study was conducted among 9-12 years old school children of nelakondapally mandal, Khammam district, Andhra Pradesh. Data were collected using a pre-tested and structured questionnaires followed by intra oral examination. The questionnaire that was used to collect information consists of two parts. First part consisted of information on demographic data, permanent residential address, and source of drinking water, staple food, liquids routinely consumed and oral hygiene aids. Second part consisted of tables to record dental caries and dental fluorosis 6 (WHO criteria).
Sample size and sampling technique
A stratified random sampling technique was used. The entire geographical area of Nelakondapally mandal was divided into 3 strata, based on the concentrations of naturally occurring F in drinking water ( Table 1 ). The F levels in drinking water for the purpose of stratifying the district were obtained from the documented records of the office of the chief engineer, department of rural water supply, Khammam and were correlated with water analysis done at Panchayatraj internal water quality monitoring laboratory, Zilla Parishad (Z.P.), Nalgonda.
Table 1: Three strata with different F levels in drinking water inclusion criteria.8
| Levels/strata | F content in ppm |
| Level 1 | <0.7 |
| Level 2 | 0.71.2 |
| Level 3 | 1.33.5 |
F: Fluoride
Collection and analysis of water samples
Collection of water samples was done based on the methodology followed in National Oral Health survey and F Mapping 2002-2003. 7 Sufficient numbers of plastic bottles were carried to the schools. Water was collected from drinking source, which was used by children. All the bottles were labeled. The water samples were sent to the laboratory of “Panchayat Raj internal water quality monitoring laboratory, Z.P Nalgonda,” to confirm the F levels, before the commencement of clinical examination. The F concentration of water was analysed using pH/ion meter (720A Orion, Thermo Fisher Scientific Inc., Waltham, MA, 2005 model) coupled with an ion specific electrode for fluoride (Model 9609BN, Orion Research Inc., MA, USA).
The children who satisfied the following criteria were included in the study.
School children, aged 9-12 years irrespective of sex, race, and socioeconomic status who were residents of that particular region and using the same source of drinking water
Children with more than 50% of the crown erupted and no fillings on the facial surface of anterior teeth
Children who were cooperative.
Exclusion criteria
The children who had the following characteristics were excluded from the study.
Children who had migrated from some other place or who were not the permanent residents of that particular area
Children who obtained their drinking water from more than one source
Children with orthodontic brackets were excluded as this hindered diagnosis of enamel defects
Children with severe extrinsic stains on their teeth in whom assessing fluorosis is not possible
Children with any communicable or systemic diseases and fractured anterior teeth.
Prior permission was obtained from the district educational officer, Khammam. Informed consent was obtained from the school heads, on behalf of students and their parents before the intra-oral examinations.
Clinical examination
Type-III clinical examination, 9 as recommended by American Dental Association was followed throughout the study for intra oral examinations.
Data analysis
The information collected from questionnaires, clinical examinations and F analysis was computed and subjected to statistical analysis using the Statistical Package for Social Sciences (SPSS version 10, SPSS Inc., Chicago, USA-1983). Quantitative data was summarized using means and standard deviations. ANOVA test was used to find significant differences between different groups. Student’s test was used to compare two means. Qualitative data was analyzed for differences in proportions by using Chi-square test for independence. The level of significance was set at 0.05%. If P < 0.05, the results were considered as statistically significant.
Results
Among the total population of 1500 children, 324 belonged to the age group 9-10 years, 652 belonged to the age group 10-11 years, and 524 belonged to the 11-12 years. 822 (54.8%) were boys and 678 (45.2%) were girls. Majority of respondents (87.3%) used bore well water for drinking purpose ( Figure 1 ). The main staple food of the study
Figure 1: Distribution of study population according to source of drinking water.
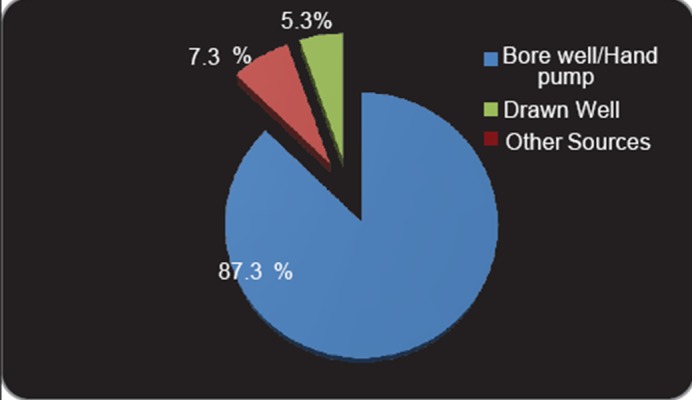
population was rice (88.6%). Apart from drinking water, tea was the most frequently consumed beverage (77.5%). The consumption of sugar in the study population was about (61.3%) in boys and (38.7%) in girls.
The prevalence and severity of dental fluorosis among the study population using Dean’s index criteria in areas with different F levels in drinking water is presented in Figure 2 . The prevalence of fluorosis was 74.8% of which majority had fluorosis in strata 3. The association was found to be significant using ANOVA test for multiple group comparisons. The results of Mann–Whitney U-test for group wise comparisons were also highly significant (P < 0.001 [highly significant]). The Dean’s scores increased with increased F levels in drinking water. Prevalence and severity of dental fluorosis among children with different sources of drinking water and group wise comparison using Mann–Whitney U-test showed children who consumed water from bore wells suffered more from fluorosis than who consumed water from other source. Table 2 illustrates the prevalence of dental caries among the study population. Mean decayed missing filled teeth (DMFT) and dmft of the study population was about 1.28 ± 1.82 and 0.85 ± 0.16, respectively. Table 3 represents the prevalence of dental caries with different water F concentrations and one-way ANOVA for comparison of means is highly significant. Table 4 represents prevalence of dental caries with different source of drinking water. The greatest mean DMFT and dmft was observed in the area with F concentration of 0.0-0.6 ppm. The prevalence and severity of dental caries was not significant among children, who consumed sweets at different frequencies and who used different oral hygiene aids. There was statistically significant association between drinking water F concentration with dental fluorosis and dental caries. Results were presented as mean ± standard deviation for quantitative data and number and percentage for categorical data.
Figure 2: Prevalence and severity of fluorosis in study population according to Dean’s fluorosis index (WHO criteria) scores.
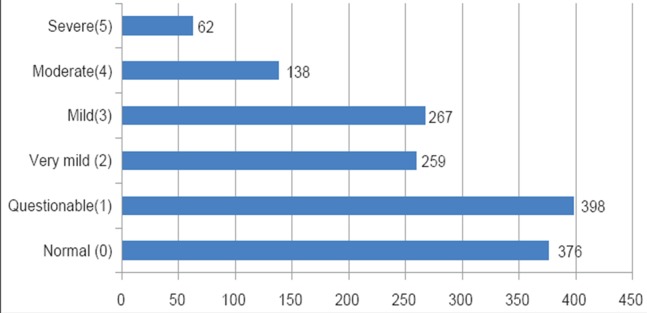
Table 2: Prevalence of dental caries among study population.
| Range | Total score | Mean±SD | |
| DT | 014 | 1662 | 1.27±0.73 |
| MT | 01 | 11 | 0.008±0.02 |
| FT | 02 | 12 | 0.009±0.12 |
| DMFT | 014 | 1685 | 1.28±1.82 |
| Dt | 014 | 83 | 0.43±0.06 |
| Mt | 05 | 59 | 0.31±0.08 |
| Ft | 02 | 22 | 0.11±0.04 |
DMFT: Decayed missing filled teeth, DT, Dt: Decayed teeth, MT, Mt: Missing teeth, FT, Ft: Filled teeth, SD: Standard deviation
Table 3: Prevalence of dental caries with different water fluoride concentration.
| Stratum (ppm) | Mean±SD | |
| DMFT | dmft | |
| 1 (0.00.6) | 3.8±1.65 | 0.12±0.45 |
| 2 (0.71.2) | 0.33±0.34 | 0.3±0.43 |
| 3 (1.33.5) | 1.03±0.19 | 0.6±0.37 |
| Total | 2.49±0.18 | 0.26±0.11 |
Kruswal-Wallis ANOVA test: χ2=185.4; P<0.005 (HS). Mann-Whitney Utest for group wise comparison are highly significant. SD: Standard deviation, HS: Highly significant, DMFT, dmft: Decayed missing filled teeth
Table 4: Prevalence of dental caries with different sources of drinking water.
| Source of drinking water | Mean±SD | |
| DMFT | dmft | |
| Bore well | 0.85±0.21 | 0.26±0.14 |
| Draw well | 1.07±0.88 | 0.75±0.11 |
| Other sources | 0.53±1.41 | 0.13±0.08 |
| Total | 0.49±0.18 | 0.26±0.11 |
Kruwal-Wallis ANOVA test: χ2=173.5; P<0.005 (HS). Mann-Whitney Utest for group wise comparison are significant. DMFT, dmft: Decayed missing filled teeth, SD: Standard deviation, HS: Highly significant
Discussion
A number of studies 10 - 13 have been conducted in various parts of India to collect epidemiological data on fluorosis and dental caries, but still current update is required. This was one of the main reasons for selecting this area for the present investigation. School children were selected for the study because they can be easily examined and also review can be carried out if necessary.
Many studies in the past have proved the direct link between the degree of dental fluorosis and the amount of F in drinking water
in different countries. 14 - 17 The important milestone discovery by Dean et al. 1942 (as cited by Tiwari A ,1986) 18 states that, 1 ppm of F in drinking water has maximum reduction of caries and very mild dental fluorosis. The recommended level of water fluoridation for optimal dental caries reduction is 0.7-1.0 ppm, with 4.0 ppm being the maximum contaminant level allowed by the environmental protection agency. 19
Neither the socioeconomic status, age, nor the gender of the child had any influence on the prevalence of dental fluorosis in our study group (P > 0.05). Furthermore, no significant association was found between the various oral hygiene measures, diet intake and sea food consumption with dental fluorosis. Tea 20 is a rich source of F, and its intake is supposed to cause fluorosis. The contrary observation in the present study can be attributed to the limited consumption of tea and also changing habits of beverage consumption with age.
Water obtained from different water sources, located closely in a same village showed different concentrations of F in the present study. Similar observations were reported by El-Nadeef and Honkala (1998) 21 in Nigeria and Gopalakrishnan et al. (1999) 22 in Kerala. Where, superficial layers of water in bore wells contain less F content than deeper layers, and it was again proved in this study. These findings were similar from various studies conducted by Ng’ang’a and Valderhaug 23 in Nairobi, Kenya; and Bårdsen et al. 24 in Western Norway.
Fluorosis was moderate to high prevalent among the present study population (74.9%). The prevalence could be explained by Susheela’s explanation. 25 In endemic fluorosis area, a great amount of F is incorporated into food materials and ingested into the body. Higher temperatures of Nelakondapally, which necessitates greater intake of water, could also be one reason. The fluorotic changes showed bilateral symmetry in our study, which is similar to the findings from the study conducted by Manji et al. 26 in Kenya which indicate systemic origin and characteristic of dental fluorosis. The severity of enamel changes is greater in higher F areas than low F areas.
Caries prevalence among the study population was about 56.5%, which is slightly higher than Andhra Pradesh average caries prevalence of 41.5% in the permanent dentition as reported by National Oral Health survey and F mapping 2002-2003. According to Subba Reddy and Tewari 27 the mutilated morphology of fluorotic teeth facilitates plaque accumulation and food lodgment that leads to initiation of dental caries. There was a positive correlation between fluorosis and dental caries in the present study. Shourie 28 has reported that where F level ranged from 0.20 to 7.00 ppm from Lahore district showed a lower incidence of dental caries. Englander and Wallace 29 have reported overall reduction in DMFT of 40% in residents with F level of 1.20. Gill and prasad 30 have reported 48.03% of clinical caries at 0.55 ppm level. The DMFT was 1.60 in children in the age group of 13-14 years. In the present study, strata 1 mean DMFT and dmft increased with low water F levels, and this increase was statistically significant. Strata 1 (0.0-0.6 ppm) representing about 33.3% study population, 5.87% had fluorosis and caries prevalence high as 50.8%. In strata 2 (0.7-1.2 ppm) representing about 37.3% study population, 9.07% had fluorosis and caries prevalence was found 32%. In strata 3 (1.3-3.5 ppm) representing about 29.4% study population, 85.04% had fluorosis and caries prevalence was 39.5%. It was observed from the study that caries prevalence was high in strata 1 with 0.0-0.6 water F concentration, followed by least in optimal water F concentration and caries prevalence was slightly high in strata 3 compared with strata 2. This indicates the fact that fluorosis renders the teeth more susceptible for dental caries, and this is more so, at greater concentrations of F in the drinking water.
Conclusion
Epidemiological surveys in other areas of Khammam district would further enhance our knowledge on the prevalence of dental fluorosis, and dental caries and correlation between these two prevalence oral afflictions. Dental fluorosis is present in Khammam District, and caries were seen in conjunction with fluorosis in all the age group of children. It is important to have rigorous control of oral health educative and preventive programs on dental fluorosis and caries, its effects on oral health. Since children and adolescents are most commonly affected by dental fluorosis and caries therefore, constant update of the prevalence of dental fluorosis and caries with a larger sample is required, and preventive programs need to be focused on them.
Footnotes
Source of Support: Nil
Conflict of Interest: None
Contributor Information
M Shanthi, Department of Paediatric Dentistry, Mahsa University, Malaysia.
B Vishnuvardhan Reddy, Department of Orthodontics, G. Pulla Reddy Dental College & Hospital, G. Pulla Reddy Nagar, Kurnool, Andhra Pradesh, India.
V Venkataramana, Department of Orthodontics, Panineeya Mahavidhyalaya Institute of Dental Sciences, Kamala Nagar, Hyderabad, Andhra Pradesh, India.
S Gowrisankar, Government Dental College and Hospital, Kadapa, Andhra Pradesh, India.
B V Thimma Reddy, Department of Paediatric and Preventive Dentistry, Mamata Dental College and Hospital, Khammam, Hyderabad, Andhra Pradesh, India.
Sireesha Chennupati, Department of Pediatric and Preventive Dentistry, Mamata Dental College & Hospital, Khammam, Hyderabad, Andhra Pradesh, India.
References
- 1.PE Petersen, MA Lennon. Effective use of fluorides for the prevention of dental caries in the 21st century: The WHO approach. Community Dent Oral Epidemiol. 2004;32(5):319–321. doi: 10.1111/j.1600-0528.2004.00175.x. [DOI] [PubMed] [Google Scholar]
- 2.HD Rodd, LE Davidson. The aesthetic management of severe dental fluorosis in the young patient. Dent Update. 1997;24(10):408–411. [PubMed] [Google Scholar]
- 3.M Connet. Science watch: New study challenges old belief on dental fluorosis/tooth decay, Issue 2004. Available at http://fluoridealert.org/articles/science [Google Scholar]
- 4.S Ayoob, AK Gupta. Fluoride in drinking water: A review on the status and stress effects. Crit Rev Environ Sci Technol. 2006;36(6):433–487. [Google Scholar]
- 5.JA Brunelle, JP Carlos. Recent trends in dental caries in U.S. children and the effect of water fluoridation. J Dent Res. 1990;69 Spec No:723–727. doi: 10.1177/00220345900690S141. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Oral Health Survey-Basic Methods. 4th ed. Geneva: WHO. 1997:35–44. [Google Scholar]
- 7.National Oral Health Survey and Fluoride Mapping. New Delhi: DCI. 2000 [Google Scholar]
- 8.KM Sudhir, GM Prashant, VV Subba Reddy, Mohandas U, GN Chandu. Prevalence and severity of dental fluorosis among 13- to 15-year-old school children of an area known for endemic fluorosis: Nalgonda district of Andhra Pradesh. J Indian Soc Pedod Prev Dent. 2009;27(4):190–196. doi: 10.4103/0970-4388.57651. [DOI] [PubMed] [Google Scholar]
- 9.S Peter. Essentials of Preventive and Community Dentistry. 3rd ed. New Delhi: Arya (medi) Publishers. 2003 [Google Scholar]
- 10.JP Ruan, ZQ Yang, ZL Wang, AN Astrøm, A Bårdsen, K Bjorvatn. Dental fluorosis and dental caries in permanent teeth: rural schoolchildren in high-fluoride areas in the Shaanxi province, China. Acta Odontol Scand. 2005;63(5):258–265. doi: 10.1080/00016350510019991. [DOI] [PubMed] [Google Scholar]
- 11.SR Grobler, CW van Wyk, D Kotze. Relationship between enamel fluoride levels, degree of fluorosis and caries experience in communities with a nearly optimal and a high fluoride level in the drinking water. Caries Res. 1986;20(3):284–288. doi: 10.1159/000260947. [DOI] [PubMed] [Google Scholar]
- 12.J Mann, M Tibi, HD Sgan-Cohen. Fluorosis and caries prevalence in a community drinking above-optimal fluoridated water. Community Dent Oral Epidemiol. 1987;15(5):293–295. doi: 10.1111/j.1600-0528.1987.tb00541.x. [DOI] [PubMed] [Google Scholar]
- 13.AI Ismail, JM Brodeur, M Kavanagh, G Boisclair, C Tessier, L Picotte. Prevalence of dental caries and dental fluorosis in students, 11-17 years of age, in fluoridated and non-fluoridated cities in Quebec. Caries Res. 1990;24(4):290–297. doi: 10.1159/000261285. [DOI] [PubMed] [Google Scholar]
- 14.SO Griffin, ED Beltrán, SA Lockwood, LK Barker. Esthetically objectionable fluorosis attributable to water fluoridation. Community Dent Oral Epidemiol. 2002;30(3):199–209. doi: 10.1034/j.1600-0528.2002.300306.x. [DOI] [PubMed] [Google Scholar]
- 15.AR Al-Shammery, EE Guile, ME Backly. The prevalence of dental fluorosis in Saudi Arabia. Saudi Dent J. 1997;9:58–61. [Google Scholar]
- 16.T Ishii, G Suckling. The severity of dental fluorosis in children exposed to water with a high fluoride content for various periods of time. J Dent Res. 1991;70(6):952–956. doi: 10.1177/00220345910700060801. [DOI] [PubMed] [Google Scholar]
- 17.JJ Warren, SM Levy, MJ Kanellis. Prevalence of dental fluorosis in the primary dentition. J Public Health Dent. 2001;61(2):87–91. doi: 10.1111/j.1752-7325.2001.tb03371.x. [DOI] [PubMed] [Google Scholar]
- 18.A Tiwari. Fluorides and Dental Caries: A Compendium. In: Jalili VP, editor. 1st ed. Indore: Indian Dental Association. 1986:29–43. [Google Scholar]
- 19.AR Prabhakar, OS Raju, AJ Kurthukoti, TD Vishwas. The effect of water purification systems on fluoride content of drinking water. J Indian Soc Pedod Prev Dent. 2008;26(1):6–11. doi: 10.4103/0970-4388.40314. [DOI] [PubMed] [Google Scholar]
- 20.PJ Riordan. Perceptions of dental fluorosis. J Dent Res. 1993;72(9):1268–1274. doi: 10.1177/00220345930720090201. [DOI] [PubMed] [Google Scholar]
- 21.MA El-Nadeef, E Honkala. Fluorosis in relation to fluoride levels in water in central Nigeria. Community Dent Oral Epidemiol. 1998;26(1):26–30. doi: 10.1111/j.1600-0528.1998.tb01920.x. [DOI] [PubMed] [Google Scholar]
- 22.P Gopalakrishnan, RS Vasan, PS Sarma, KS Nair, KR Thankappan. Prevalence of dental fluorosis and associated risk factors in Alappuzha district, Kerala. Natl Med J India. 1999;12(3):99–103. [PubMed] [Google Scholar]
- 23.PM Ng'ang'a, J Valderhaug. Prevalence and severity of dental fluorosis in primary schoolchildren in Nairobi, Kenya. Community Dent Oral Epidemiol. 1993;21(1):15–18. doi: 10.1111/j.1600-0528.1993.tb00711.x. [DOI] [PubMed] [Google Scholar]
- 24.A Bardsen, KS Klock, K Bjorvatn. Dental fluorosis among persons exposed to high- and low-fluoride drinking water in western Norway. Community Dent Oral Epidemiol. 1999;27(4):259–267. doi: 10.1111/j.1600-0528.1998.tb02019.x. [DOI] [PubMed] [Google Scholar]
- 25.AK Susheela. Epidemiology and control of fluorosis in India. J Nutr Found India. Available from: http://www.nutritionfoundationofindia.res.in/pdfs/BulletinArticle/Pages%20from%20nfi_04_84.3.pdf . 1984 [Google Scholar]
- 26.F Manji, V Baelum, O Fejerskov. Dental fluorosis in an area of Kenya with 2 ppm fluoride in the drinking water. J Dent Res. 1986;65(5):659–662. doi: 10.1177/00220345860650050501. [DOI] [PubMed] [Google Scholar]
- 27.VV Subba Reddy, A Tewari. Prevalence of dental caries to different levels of fluoride in drinking water. J Indiana Dent Assoc. 1992;63(11):455–461. [Google Scholar]
- 28.KL Shourie. Prevalence of dental caries to different levels of fluoride in drinking water from Lahore district. J Indiana Dent Assoc. 1953;26(2):4–8. [Google Scholar]
- 29.HR Englander, DA Wallace. Effects of naturally fluoridated water on dental caries in adults: Aurora-Rockford, Illinois, Study III. Public Health Rep. 1962;77(10):887–893. [PMC free article] [PubMed] [Google Scholar]
- 30.PS Gill, BG Prasad. Dental health survey of primary school children in a rural area of Lucknow. J Indiana Dent Assoc. 1968;40(9):227–233. [PubMed] [Google Scholar]


