Abstract
Context
Ambulance diversion, a practice in which emergency departments (EDs) are temporarily closed to ambulance traffic, might be problematic for patients suffering from time-sensitive conditions. However, there is little empirical evidence to show whether diversion is associated with worse patient outcomes.
Objective
Analyze whether temporary ED closure on the day a patient suffers from acute myocardial infarction (AMI), as measured by ambulance diversion hours of the nearest ED, is associated with increased mortality rates among AMI patients.
Study Design and Main Outcome Measures
Data include 100% Medicare claims data that cover admissions between 2000 and 2005, linked with date of death until 2006, and daily ambulance diversion logs from four California counties between 2000 and 2006. We compared the percentage of AMI patients who die within 7, 30, up to 365 days of admission when their nearest ED is not on diversion and when that same ED is exposed to <6, 6-12, and ≥12 hours of diversion out of 24 hours on the day of admission. We control for underlying differences in patient population by estimating ED fixed-effects multivariate regression models that also include time-varying patient and hospital characteristics and seasonal trends adjustment.
Population Studied
The study included 13860 Medicare AMI patients from 508 zip codes whose admission date was within the relevant time period. Among the hospital universe, 149 EDs were identified as the nearest ED to these patients.
Results
Between 2000 and 2006, the mean daily diversion duration was 7.9 hours (SD=6.1 hours). Based on analysis of 11652 patients who were admitted to the ED between 2000 and 2005 and whose nearest ED had at least 3 diversion exposure levels (n=3541, 3357, 2667, and 2060 for no exposure, exposure to <6, 6-12, and ≥12 hours of diversion, respectively), there is no statistically significant differences, at the 5% level, in mortality rates between no diversion and exposure to diversion under 12 hours. Exposure to 12 or more hours of diversion is associated with higher 30-day mortality compared to no diversion status (actual mortality rate: 19% [n=392] vs. 15% [n=545]; regression adjusted difference: 3.24 percentage point [95% Confidence Interval, CI: 0.6-5.88]); higher 90-day mortality (26% [n=537] vs. 22% [n=762]; regression adjusted difference: 2.89 percentage point [CI: 0.13-5.64]); higher 9-month mortality (33% [n=680] vs. 28% [n=980]; regression adjusted difference: 2.93 percentage point [CI: 0.15, 5.71]); and higher 1-year mortality (35% [n=731] vs. 29% [n=1034]; regression adjusted difference: 3.04 percentage point [CI: 0.33-5.75]).
Conclusions
Among Medicare patients with acute MI in 4 populous California counties, exposure to at least 12 hours of diversion by the nearest ED was associated with increased 30-day, 90-day, 9-month, and 1-year mortality.
Introduction
A recent synthesis study by the Robert Wood Johnson Foundation and a report by the Institute of Medicine describe the state of emergency departments (ED) in the US as reaching a breaking point: the ED system experiences increased utilization but decreased capacity.1, 2 These trends have led to a milieu of problems for patients, such as longer waiting times,3-5 overextended staff,6, 7 and disruptions to ambulance services.8, 9 Ambulance diversion, a practice in which EDs are temporarily closed to ambulance traffic due to overcrowding or lack of available resources, might be especially problematic for patients suffering from time-sensitive conditions such as acute myocardial infarction (AMI). Ambulance diversion occurs for a variety of reasons, including overcrowding, shortage of ED staff, and lack of specialty services (e.g., trauma, neurosurgery), staffed inpatient beds, or specialty facilities (CCU, ICU beds, or major equipment failures).2, 8 Regardless of the reason for diversion, an ED on diversion effectively creates a temporary decrease in ED access.
While there are many anecdotal reports or single-hospital case studies suggesting the adverse effects of ambulance diversion and closures on patient care, 10, 11 there is little systematic empirical evidence to demonstrate these claims.12, 13 A recent ecological study based on data from New York City found that high levels of diversion were associated with increased AMI mortality rates.14 Because this study was not conducted at the individual patient level, however, the authors could not ascertain whether the differences in mortality rates were due to diversion or due to unobserved individual patient and hospital characteristics. As emphasized by the most prominent health service researchers in emergency medicine, there is a need to document whether decreased access as measured by diversion affects the quality of care or outcomes and, if so, the extent of such effects. 8, 15
In this study, we use 100% of Medicare claims and daily ambulance diversion logs from four California counties’ local emergency medical services to analyze the relationship between ambulance diversion and health outcomes of patients suffering from AMI. Specifically, we address the following research question: Is temporary ED closure on the day a patient suffers from AMI, as measured by ambulance diversion hours of the nearest ED, associated with increased mortality rates among patients with AMI?
Methods
Conceptual Model
An emergency department on diversion can be considered as a signal that available resources are unable to match demand or a proxy (albeit imperfect) of crowding.16-18 Conceptually, diversion could have implications for both patients who are diverted to other hospitals and non-diverted patients within the diverting hospital. For patients who had to be diverted elsewhere, ambulance diversion increases transport time,8 likely causing delays in receiving treatment and potentially worse prognosis of AMI. Even if the increased transport time is trivial, the patients might end up in a less desirable setting (for example, ED without cath capacity if the one with cath capacity is on diversion). For non-diverted patients in an ED that is on divert (either because these patients were admitted before the status change, arrived by private vehicles, or were brought in under exception), their outcome could still be affected as they are in an ED during a time when providers or resources are limited in such a way to prevent optimal patient care.2
Moreover, diversion in one hospital can potentially affect patients in nearby hospitals, as nearby hospitals would receive diverted patients. This increased patient load could similarly cause treatment delays. As our data will show in detail, many EDs are on divert for short periods of time on a given day, and in many instances have multiple episodes of diversion throughout a day. Our patient data contain date of admission, but not the exact time of admission. While we cannot verify that a patient was diverted or not, the conceptual model described here hypothesizes that longer exposure to diversion hours would be associated with worse outcome for both the diverted and non-diverted patients in the affected area.
Data Sources
The primary data sources for ambulance diversion were the daily diversion logs from four California counties: Los Angeles, San Francisco, San Mateo, and Santa Clara. Together, these four counties represent 63% of California's population, based on 2000 US Census data. We obtained detailed daily diversion logs for the years 2000-2006 from each county by directly contacting their local emergency medical services (LEMS) agencies and securing permission. The first available date of each county's data varies: San Mateo starts Jan 2000, San Francisco March 2000, Los Angeles June 2001, and Santa Clara Jan 2003. All counties have daily logs available until Nov 2006. We only included patients from the relevant months/years when data for the corresponding county is available.
The LEMS agencies govern and track diversion in all hospitals under each county's jurisdiction. The daily diversion log is specific to ED and trauma centers, and contains information regarding date and exact time diversion began and ended for every hospital as well as the reason for diversion in each instance (i.e., whether the ED diversion is due to ED saturation, if only trauma care is on divert, lack of neurosurgeon, equipment downtime). During the study period, there were no policies to selectively divert AMI patients to PCI-equipped hospitals in these four counties. For the purpose of this analysis, we excluded diversion that only applied to trauma center or psychiatric emergency departments and diversion due to lack of neurosurgeon or CT scan downtime, since these types of diversion would not affect the admission of AMI patients. To capture the relevant hospital universe for matching patients to the correct EDs (as hospitals not on divert would not appear in the diversion logs), we merged the daily diversion logs with California Office of Statewide Health Planning and Development (OSHPD) and Medicare Healthcare Cost Report Information System (HCRIS) datasets to obtain additional facility data.
Patient data from the four California counties, including patients’ mailing zip codes, were obtained from the Medicare Provider Analysis and Review (MedPAR). We linked each patient's zip code with longitude and latitude coordinates of each zip code using Mailer's software.19 We also obtained the longitude and latitude coordinates of the hospital's physical address or heliport (if one exists).20 We identified the nearest ED for each patient's zip code as follows: (1) we calculated the driving time between each patient's zip code and all EDs; 21, 22 and (2) we designated the ED with the shortest driving time as the nearest ED. Finally, we identified the diversion level of the nearest ED on the day a patient suffered from AMI by merging the ED diversion data to the patient data based on admission date and provider ID. The study was approved by the Naval Postgraduate School Institutional Review Board (IRB#20080043-IREP7-A).
Patient Population
We identified the AMI population by extracting from 100% MedPAR records that had 410.x0 or 410.x1 as the principal diagnoses, admission occurring between 2000 and 2005, and county of residence as one of the four counties for which we have diversion data. These patients’ Medicare records were linked to death certificates, if deceased, up until the end of March 2006. We applied several exclusion criteria to the patient sample. First, we followed McClellan et al's exclusion criteria to minimize selection bias; 23 the list excludes patients who had a prior AMI admission within the past 12 months, had a length of stay of 1 day (as they may not be real AMI patients), and patients without continuous Medicare part A coverage within the past 12 months. We also excluded 24 percent of the patient population who were not admitted through the ED, since admission through the ED is the relevant population. Furthermore, we excluded 11 percent of patients whose admitted hospital is more than 100 miles away from their mailing ZIP codes, as those patients likely do not reside at their mailing address or were admitted to hospitals while away from home.
Defining AMI Outcomes
The dependent variables in the analysis are whether a patient died within X days from his ED admission (X=7, 30, 90, 270, and 365 days). For example, the dependent variable that captures 7-day mortality takes on the value 1 if a patient died within 7 days from his date of admission and 0 otherwise.
Statistical Methods
Our statistical model follows the same principle as the case-crossover design, while controlling for time-dependent variables. In essence, we compare the percent of AMI patients who die within 7, 30, 90, 270 and 365 days when their nearest ED is in normal operation (i.e., no exposure to diversion, the control group) and when the same ED is exposed to different levels of diversion (i.e., the same ED crosses over to higher exposure of diversion--we define level of diversion exposure below). By using each ED as its own matched control, we can eliminate any inherent differences across EDs, such as possible differences in baseline mortality rates, quality of care, case-mix of the patient population, teaching status, or other unobserved characteristics that might be confounded with mortality rates.24 This is done by estimating a linear probability model with fixed effects for each ED that was identified as the closest ED for each patient (this is equivalent to including indicators for each ED in the model), and the key variable of interest is the level of diversion each ED experiences on every day (additional control variables are described below).
We define 4 diversion exposure levels: 0 hours (reference group), <6 hours, 6-12 hours (not including 12 hours), and ≥12 hours. These cutpoints were determined before we linked the daily diversion data to patient outcomes by dividing the empirical distribution of the daily ambulance diversion hours into quartiles. The cutoffs for the quartiles are 3, 6.6, and 11.6 hours. We combine the first two quartiles since a priori we did not expect to see an association with inpatient mortality at lower levels of diversion and wanted to account for only practically meaningful thresholds. We therefore use 6 and 12 hours (instead of 6.6 and 11.6 hours) for easier exposition of the thresholds for the two upper quartiles.
The ED fixed-effects removes any time-invariant unobserved differences across EDs, and the three diversion exposure indicators allow us to compare AMI mortality rates when the same ED is exposed to different levels of diversion. Because each ED serves as its own matched-control to compare mortality rates across different levels of diversion, we exclude patients from hospitals in which we observe fewer than 3 levels of exposure.
Even though a logistic model is the natural choice for estimating a dichotomous dependent variable for cross-sectional data, it would result in an inconsistent estimator in a panel data setting as we are including a significant number of fixed effects. On the other hand, a linear probability model can provide consistent estimates.25, 26 In addition to the key diversion variables, we include fully interacted patient demographic co-variates (5-year age groups, gender, white, black or other race, and counts of comorbidities). We also included a list of disease related risk adjustment following the work by Skinner and Staiger that uses the same patient data source.27 Specifically, risk adjustments were made if patients had peripheral vascular disease, chronic pulmonary disease, dementia, chronic renal failure, diabetes, liver disease, or cancer at the time of admission. In addition, we included hospital characteristics of the admitted hospital, including whether the hospital has catheterization capacity, hospital ownership (for-profit, government), and size (measured by log transformed total available beds). Finally, we controlled for year trends (overall mortality rates have decreased steadily over time) and monthly (seasonal) trends within each year. For all models, we estimated heteroskedasticity-robust standard errors28 that allow for intra-ED correlation among patients who lived closest to the same ED . All estimations were performed using Stata 11 (Stata Corp, College Station, TX), and we used the conventional 5% level of significance with 2-sided testing. Our sample size was sufficient, by conventional standard of 0.8 power, to detect a minimum of 10 percent differences in mortality rates—the estimated study power for the analysis was >0.90 for all dependent variables.
Results
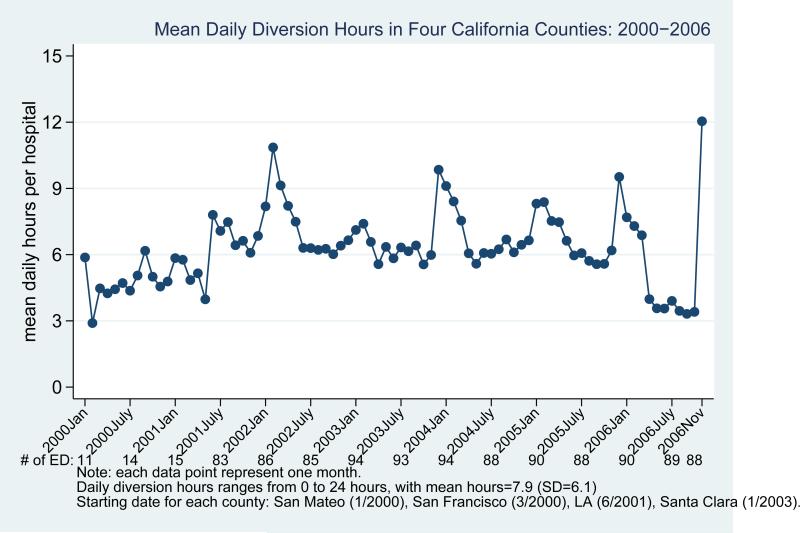
The final sample consisted of 13,860 patients from 508 zip code areas whose admission date was within the relevant time period where ED diversion data is available. Among the hospital universe, 149 EDs were identified as the nearest ED to these patients. Figure 1 shows the mean hours of diversion per day between 2000 and 2006 among hospitals that reported positive diversion hours. The mean duration was 7.9 hours (SD=6.1 hours), but Figure 1 shows a seasonal trend where the hours of diversion tend to peak in winter.
Figure 1.
Mean Diversion Hours in Four California Counties: 2000-2006
Merging the diversion information to the patient data, we exclude 2235 patients whose closest ED is not exposed to at least 3 levels of diversion and we exclude diversion logs from 2006 because the last matched admission date is Dec 2005. The multivariate analysis consists of 11,625 patients. Among them, 3541, 3357, 2667, and 2060 patients were admitted for AMI when their closest ED was not exposed to diversion, exposed to <6, 6-12, and ≥12 hours, respectively. Table 1 shows that 29 percent of patients (n=1034) in the no-diversion category died within 1 year of ED admission. The percent of patients who died within 1 year of admission in the <6, 6-12, and ≥12 hours diversion categories are 31 percent (n=1028), 30 percent (n=794), and 35 percent (n=731), respectively.
Table 1.
Descriptive Statistics of Patient and Hospital Characteristics
| Nearest ED was not diverted on the day of admission | Nearest ED's exposure to diversion on the day of admission |
|||||||
|---|---|---|---|---|---|---|---|---|
| <6 hr | 6-12 hours | ≥12 hours | ||||||
| % or Mean | (N or SD) | % or Mean | (N or SD) | % or Mean | (N or SD) | % or Mean | (N or SD) | |
| Share of patients who die within: | ||||||||
| 7-day | 9% | (305) | 9% | (300) | 8% | (222) | 10% | (208) |
| 30-day | 15% | (545) | 16% | (538) | 17% | (451) | 19% | (392) |
| 90-day | 22% | (762) | 23% | (760) | 23% | (605) | 26% | (537) |
| 9-month | 28% | (980) | 29% | (978) | 28% | (751) | 33% | (680) |
| 1-year | 29% | (1034) | 31% | (1028) | 30% | (794) | 35% | (731) |
| Patient demographics | ||||||||
| Female | 50% | (1757) | 50% | (1677) | 51% | (1354) | 52% | (1065) |
| African American | 6% | (203) | 6% | (191) | 6% | (169) | 11% | (231) |
| Other non-white races | 19% | (662) | 20% | (663) | 20% | (522) | 20% | (414) |
| Age distribution | 12% | (432) | 11% | (373) | 13% | (342) | 14% | (294) |
| 65-69 | 15% | (531) | 15% | (499) | 15% | (398) | 15% | (313) |
| 70-74 | 19% | (656) | 20% | (669) | 19% | (520) | 20% | (403) |
| 75-79 | 22% | (773) | 22% | (729) | 22% | (580) | 22% | (445) |
| 80-84 | 19% | (670) | 18% | (592) | 17% | (445) | 17% | (344) |
| 85+ | 14% | (479) | 15% | (495) | 14% | (382) | 13% | (261) |
| Patient comorbid conditions | ||||||||
| Peripheral vascular disease | 7% | (245) | 7% | (249) | 7% | (192) | 7% | (142) |
| Chronic pulmonary disease | 19% | (680) | 20% | (667) | 19% | (501) | 21% | (436) |
| Dementia | 4% | (150) | 5% | (167) | 4% | (110) | 5% | (99) |
| Chronic renal failure | 2% | (72) | 2% | (66) | 2% | (52) | 2% | (42) |
| Diabetes | 25% | (874) | 25% | (837) | 27% | (726) | 28% | (572) |
| Liver disease | 0% | (12) | 1% | (17) | 1% | (15) | 0% | (5) |
| Cancer | 6% | (224) | 5% | (177) | 5% | (141) | 5% | (107) |
| Patient treatment | ||||||||
| Catheterization | 49% | (1750) | 45% | (1506) | 46% | (1239) | 42% | (860) |
| cath on day of admission | 43% | (756) | 42% | (628) | 40% | (491) | 40% | (340) |
| PCI | 31% | (1105) | 26% | (885) | 28% | (752) | 24% | (489) |
| PCI on day of admission | 52% | (578) | 53% | (466) | 51% | (381) | 49% | (239) |
| Thrombolytic therapy | 1% | (51) | 2% | (58) | 1% | (38) | 2% | (32) |
| Thrombolytic therapy on day of admission | 82% | (42) | 76% | (44) | 82% | (31) | 94% | (30) |
| Admission hospital characteristics | ||||||||
| has cath lab | 87% | (3066) | 81% | (2730) | 80% | (2130) | 78% | (1611) |
| for-profit | 7% | (259) | 13% | (431) | 15% | (411) | 17% | (346) |
| Government | 9% | (336) | 9% | (298) | 10% | (276) | 12% | (255) |
| Share admitted to nearest ED | 42% | (1478) | 40% | (1334) | 41% | (1091) | 41% | (844) |
| Mean distance between admitted and nearest ED (in miles) | 2.34 | (7.49) | 2.65 | (7.22) | 2.57 | (7.42) | 2.34 | (6.80) |
| Mean total beds in hospital | 325.29 | (281.00) | 317.78 | (264.04) | 319.20 | (189.01) | 314.30 | (251.41) |
| Number of patients | 3541 | 3357 | 2667 | 2060 | ||||
The rest of Table 1 shows the key variable's descriptive statistics by the four diversion exposure categories (no diversion, <6 hours, 6-12 hours, and ≥12 hours). Patient demographics and comorbid characteristics (2nd and 3rd panels of Table 1) generally do not differ by levels of diversion. The only exception is that there is a higher share of African-American patients in the 12-plus-hour category (6% [n=203] in no-diversion vs. 11% [n=231] in ≥12 hours category). Once admitted, patient treatment patterns differ in two dimensions (4th panel of Table 1): percent of patients receiving cath is 42 percent (n=860) in ≥12 hours exposure group compared to 49 percent (n=1750) in the no-diversion group; percent of patients receiving PCI is 24 percent (n=489) in ≥12 hours exposure group compared to 31 percent (n=1105) in the no-diversion group.
The last panel of Table 1 reports the hospital characteristics of admitted ED. When the closest ED is on diversion, a lower share of patients is admitted to hospitals with a cath lab (78 percent in ≥12 hours [n=1611] vs. 87 percent in no-diversion category [n=3066]), suggesting that hospitals with cath facilities are on diversion more often than hospitals with no cath facilities. A higher share of patients is admitted to for-profit hospitals (17 percent in ≥12 hours [n=346] vs. 7 percent in no-diversion category [n=259]) and to government hospitals (12 percent in ≥12 hours [n=255] vs. 9 percent in no-diversion category [n=336]). The percent of patients who were admitted to their closest ED and the distance between their admitted ED and their closest ED are similar across the 4 diversion categories. These similar travel patterns might suggest that distance is a minor factor in describing the relationship between diversion and mortality, and that other mechanisms discussed in the conceptual model section play a bigger role.
Table 2 shows the multivariate results, focusing on the diversion variables only (full regression results are included in Appendix A1). The first column shows the mean mortality rates in our control group (no diversion on day of admission). The next three columns show the regression-adjusted differences in mortality rates between each of the exposure groups and the control group. There are no statistically significant differences, at the 5% level, in mortality rates between no diversion status and when the exposure to diversion is under 12 hours. Exposure to 12 or more hours of diversion is associated with higher 30-day mortality compared to no diversion status (actual mortality rate: 19% [n=392] vs. 15% [n=545]; regression adjusted difference: 3.24 percentage points [95% Confidence Interval, CI: 0.6-5.88]); higher 90-day mortality (26% [n=537] vs. 22% [n=762]; regression adjusted difference: 2.89 percentage points [CI: 0.13-5.64]); higher 9-month mortality (33% [n=680] vs. 28% [n=980]; regression adjusted difference: 2.93 percentage points [CI: 0.15, 5.71]); and higher 1-year mortality (35% [n=731] vs. 29% [n=1034]; regression adjusted difference: 3.04 percentage points [CI: 0.33-5.75]).
Table 2.
Association Between Ambulance Diversion of the Nearest ED And AMI Mortality Rates
| Nearest ED not on diversion on the day of admission | Nearest ED's level of exposure to diversion on the day of admission |
|||||||
|---|---|---|---|---|---|---|---|---|
| <6 hr | 6-12 hours | ≥12 hours | ||||||
| Unadjusted mortality rate | Regression adjusted rate difference compared to control group | |||||||
| (N) | % | [95% CI] | [95% CI] | [95% CI] | ||||
| 7-day mortality | (305) | 9 | 0.41 | [−0.95,1.77] | 0.02 | [−1.63,1.66] | 1.45 | [−0.69,3.58] |
| 30-day mortality | (545) | 15 | 0.19 | [−1.59,1.96] | 1.22 | [−0.83,3.26] | 3.24* | [0.60,5.88] |
| 90-day mortality | (762) | 22 | 0.21 | [−1.74,2.15] | 0.17 | [−1.94,2.28] | 2.89* | [0.13,5.64] |
| 9-month mortality | (980) | 28 | 0.34 | [−1.76,2.45] | −1.13 | [−3.55,1.28] | 2.93* | [0.15,5.71] |
| 1-year mortality | (1034) | 29 | 0.16 | [−1.91,2.23] | −1.28 | [−3.73,1.18] | 3.04* | [0.33,5.75] |
| Sample size | 11625 | |||||||
Significant at +p<0.10
p<0.05
**p<0.01
We performed several sensitivity analyses. First, to make sure that our results were not driven by the underlying differences across admitted hospitals, we estimate our model by replacing the nearest ED fixed-effects with admitted ED fixed-effects. Our results were similar and all conclusions remained the same. Second, our sample did not include patients who died upon arrival or in the ED; those patients would have only had outpatient records. We therefore obtained authorization to access 2 years of outpatient records (2000 and 2005), resulting in 63 additional cases. When we added this group to our original sample, our conclusions on the key diversion variables remained the same.
Third, we implemented an additional model by including an additional indicator for patients that bypass their closest ED and interaction terms between the three diversion exposure categories and this bypass indicator. Appendix A2 shows that for the same level of diversion exposure, the point estimate of the mortality rate is indeed higher for people who bypass their closest ED than for those admitted to their closest ED. However, the standard errors are too large to make definitive statements.
Comment
Our study is the first multi-site, multi-county analysis using daily ambulance diversion and patient level data to evaluate the association between diversion and patient outcomes for patients suffering from AMI. We showed that when the nearest ED is on diversion, a lower proportion of patients is admitted to hospitals with catheterization capacity, and a higher proportion is admitted to for-profit and government hospitals. Under a variety of specifications and sensitivity analyses, we found that lengthy periods of ED diversion are associated with higher mortality rates among patients with a time-sensitive condition - acute myocardial infarction. Specifically, when a patient's nearest ED was exposed to diversion for 12 hours or more on the day of admission, he suffered a higher death rate by about 3 percentage points than when that same ED is not on diversion. This adverse relationship persisted even when we examined 1-year mortality rates.
When a hospital's ED is on diversion, it can affect different types of patients: those that were diverted, those receiving care or admitted while the ED is on diversion status, and those in nearby hospitals that have to receive the diverted patients. Although we were able to examine patient and hospital interactions at a more precise level than the community wide ecological analysis, we could not identify individual patients diverted from their ED of choice versus those who were not, or the mode of transportation (those that arrived via private vehicles would be admitted). While this study design is advantageous in that it avoids confounding of patients who are or are not selected to be diverted, our results must be interpreted with caution since we cannot disentangle the precise mechanisms through which diversion affects patient outcomes. Our results should not be interpreted as causal.
Ambulance diversion is common and more likely to occur in urban settings—the National Center for Health Statistics estimated that hospitals divert more than ½ million ambulances a year in the United States– an average of 1 ambulance per minute.29 The estimated association is also not trivial—a 3.24 percentage point increase off a 15 percent 30-day mortality rate indicates a 21.6% increase in overall mortality rate. Fortunately, we only observed the adverse relationship in hospitals that were on divert for at least 12 hours on any given day. In our data, such long diversion days occurred in 25 percent of the daily logs. Notably, such long diversion hours are more likely to occur in winter and in densely populated metropolitan areas --both factors associated with increased ED demand.
These findings point to the need for more targeted interventions to appropriately distribute system-level resources in such a way to decrease crowding and diversion, so that patients with time-sensitive conditions such as myocardial infarction are not adversely affected. It is important to emphasize that while demand on emergency care is increasing as evidenced by increasing utilization, supply of emergency care is decreasing.29-31 If these issues are not addressed on a larger scale, ED conditions will deteriorate, having significant implications for all.
Our study has several limitations that should be considered when interpreting our results. First, we identify the nearest ED for each patient based on the longitude and latitude information of the patient's zip code and the hospital's location. Two patients from the same zip code might have very different distances to the same ED. We believe the problem is minimized for our sample because all four counties are in densely populated Metropolitan Statistical Areas. Second, the patient's zip code on file is based on mailing zip code, which might not reflect the actual residence. We took the standard approach and applied exclusion criteria, dropping patients whose admitted hospital is more than 100 miles away from his zip code. In addition, approximately 80-85% of AMIs have been shown to occur at home.32, 33 More importantly, there is no evidence to suggest that out-of-home MIs (or more specifically, non-residential zip code MIs) would systematically differ across patients who experience more diversion than others, therefore this data limitation should not affect our analyses.
Third, it is possible that some patients’ closest EDs are out of the counties in which we can match diversion logs (for example, a resident in San Francisco county might be closest to an ED in Alameda county). In our method that follows the case-crossover design, those patients would be excluded from the analysis, because we only include patients whose nearest ED experienced multiple levels of diversion. Fourth, there might be reporting errors in the diversion daily logs. As long as the errors do not systematically differ by diversion duration (i.e., there are not more errors for log entries that record longer duration), we do not expect to have a bias in our estimates.
Fifth, the study is limited to elderly populations, which only represent between 50-60% of acute MI patients. Therefore our results should not be generalized to the younger population. Similarly, our results are based on four populous counties in California that collectively represent 63 percent of the state's population. Although these counties are demographically diverse, the proportion of African Americans is substantially lower and the proportion of other non-White minority is substantially higher than those of the U.S. as a whole. Also, these counties have few rural residents. Therefore, our findings may not be readily generalizable to other parts of the U.S., particularly rural areas where a single hospital is the only option for MI care.
Lastly, the exclusion of patients who died before they can generate a hospital admission means our estimated mortality rate differences should be considered a conservative estimate. Suppose we have a hypothetical patient that will die in either case, whether the ED is on diversion or not. In the case-crossover design, he does not contribute to the mortality difference if we can observe his death at all levels of exposure to diversion (i.e., when counting the number of death under different exposure levels, he contributes 1 death in all cases). However, our data limitation is such that when he is diverted and dies en route, he does not show up as an observable death when the ED is exposed to diversion; whereas if he survived just long enough to get admitted when an ED is not on divert, his death would be evident in our data. In other words, he would contribute as 1 death under no diversion, but no death under diversion. The implication of this data limitation means the observed mortality rate is lower than the actual mortality rate when the ED is exposed to diversion, hence making our estimated difference in mortality rate between diversion and no diversion a conservative estimate.
Conclusion
Diversion is a signal of a larger access problem in the health care system, representing resource constraints that are beyond patient factors and related to the hospital and health care system. We show a strong relationship between prolonged ambulance diversion and increased mortality of patients with acute myocardial infarction. While we cannot disentangle the precise mechanisms through which diversion affects patient outcomes, our results suggest that more integrated health care policies from the pre-hospital to in-hospital setting should include provisions that minimize instances where hospitals are on diversion for prolonged periods of time. Furthermore, restructuring of hospital and larger system-level resources to improve care delivery efficiency may be required to improve outcomes of patients with time-sensitive conditions, such as acute myocardial infarction.
Possible policy options to improve such care could include patient flow initiatives that have been implemented in many counties and states with success.34 Diversion bans have been implemented in various regions,35, 36 with the first statewide ban on diversion in Massachusetts in 2009.37, 38 Early evaluation of this recent legislation has not revealed any negative outcomes for patients, at least when measured by waiting times.39 To prevent adverse consequences for patients, however, it is critical that such policies are implemented in conjunction with hospital-level changes beyond the ED that improve inpatient capacity and patient flow.7, 40-42
Lastly, it would be important for future analyses to disentangle the various mechanisms through which diversion might adversely affect patient care, so that policies targeting the right mechanisms can be adapted for better care that translates into better outcomes for patients in need. In addition, it is crucial to examine the relationship between ambulance diversion and the outcomes of non-elderly patients and patients suffering from other time-sensitive illness such as traumatic injuries. Such findings on diversion’s downstream effects on patient outcomes will be vital to drive evidence-based policies.
Acknowledgments
Financial Disclosures:
This publication was supported by the Robert Wood Johnson Foundation's Changes in Health Care Financing and Organization initiative, grant 63974 (YS), NIH/NCRR/OD UCSF-CTSI Grant Number KL2 RR024130 (RYH), and the Robert Wood Johnson Foundation Physician Faculty Scholars (RYH).
Role of the Sponsors:
The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Disclaimer:
The article contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the Robert Wood Johnson Foundation.
Appendix
Appendix A1.
Full Regression Results on the Association Between Ambulance Diversion of the Nearest ED And AMI Mortality Rates
| (95% CI) | 7-day | 30-day | 90-day | 9-month | 1-year |
|---|---|---|---|---|---|
| Nearest ED Diversion Status on Day of Admission | |||||
| Was not on diversion on the day of admission (reference group) | |||||
| Was exposed to <6 hrs of of diversion | 0.41 [−0.95,1.77] | 0.19 [−1.59,1.96] | 0.21 [−1.74,2.15] | 0.34 [−1.76,2.45] | 0.16 [−1.91,2.23] |
| Was exposed to 6-12 hrs of diversion | 0.02 [−1.63,1.66] | 1.22 [−0.83,3.26] | 0.17 [−1.94,2.28] | −1.13 [−3.55,1.28] | −1.28 [−3.73,1.18] |
| Was exposed to ≥12 hrs of diversion | 1.45 [−0.69,3.58] | 3.24* [0.60,5.88] | 2.89* [0.13,5.64] | 2.93* [0.15,5.71] | 3.04* [0.33,5.75] |
| Patient demographics are included as 36 fully interacted categories (5-year age group, gender, race) | |||||
| Patient comorbid conditions | |||||
| peripheral vascular disease | −0.46 [−2.43,1.50] | −1.65 [−4.31,1.00] | 0.44 [−2.67,3.54] | 0.52 [−2.85,3.90] | 0.49 [−2.99,3.97] |
| chronic pulmonary disease | −1.12+ [−2.39,0.16] | 0.24 [−1.35,1.84] | 1.75+ [−0.14,3.64] | 4.49** [2.52,6.46] | 5.55** [3.52,7.58] |
| dementia | 6.59** [3.24,9.95] | 9.29** [4.76,13.81] | 10.24** [5.67,14.81] | 12.92** [8.48,17.36] | 13.16** [8.67,17.66] |
| chronic renal failure | 7.03** [1.94,12.12] | 12.32** [6.70,17.94] | 14.26** [7.87,20.65] | 12.55** [6.33,18.77] | 12.98** [6.71,19.24] |
| diabetes | −1.08* [−2.14,−0.01] | −2.87** [−4.19,−1.56] | −3.01** [−4.58,−1.44] | −2.33** [−4.04,−0.62] | −1.86* [−3.62,−0.10] |
| liver disease | 8.54 [−1.77,18.85] | 15.05* [1.94,28.17] | 21.04** [7.26,34.83] | 29.49** [15.28,43.70] | 30.74** [16.60,44.88] |
| cancer | 3.64** [1.13,6.15] | 9.15** [6.05,12.24] | 13.76** [10.13,17.39] | 18.60** [14.84,22.37] | 19.78** [16.16,23.41] |
| Year/month Indicators 2000 (reference year) | |||||
| 2001 | 1.55 [−1.49,4.58] | 2.01 [−2.36,6.38] | 0.86 [−4.04,5.76] | 4.44+ [−0.31,9.20] | 4.95* [0.19,9.72] |
| 2002 | 1.09 [−2.07,4.26] | 1.52 [−2.69,5.73] | −0.12 [−4.95,4.72] | 1.42 [−3.32,6.17] | 2.71 [−1.87,7.30] |
| 2003 | −0.36 [−3.27,2.54] | −0.35 [−4.19,3.50] | −2.07 [−6.57,2.42] | −1.89 [−6.39,2.61] | −2.56 [−6.95,1.83] |
| 2004 | −0.27 [−3.40,2.85] | −0.01 [−4.13,4.11] | −1.44 [−6.10,3.22] | −0.80 [−5.52,3.93] | −1.55 [−6.13,3.03] |
| 2005 | −1.02 [−3.83,1.78] | −0.97 [−4.66,2.71] | −3.04 [−7.32,1.24] | −3.61 [−7.97,0.76] | −4.46* [−8.82,−0.10] |
| January (reference month) | |||||
| February | −0.33 [−2.75,2.08] | 1.08 [−2.25,4.41] | 2.47 [−1.41,6.34] | 2.37 [−1.59,6.33] | 2.66 [−1.23,6.55] |
| March | 0.27 [−2.47,3.01] | −0.41 [−3.73,2.91] | −0.49 [−4.16,3.18] | −0.78 [−4.64,3.07] | 0.03 [−3.85,3.92] |
| April | −0.86 [−3.37,1.65] | −1.84 [−5.12,1.44] | −2.18 [−5.88,1.52] | −2.98 [−6.89,0.93] | −4.18* [−8.02,−0.33] |
| May | −0.74 [−3.61,2.13] | −0.36 [−3.87,3.16] | −0.58 [−4.44,3.29] | 0.14 [−3.99,4.28] | −1.15 [−5.22,2.92] |
| June | −0.64 [−3.15,1.87] | 0.01 [−3.43,3.45] | −1.74 [−5.49,2.02] | −3.70+ [−7.77,0.38] | −5.06* [−9.12,−1.01] |
| July | −1.73 [−4.35,0.88] | −2.19 [−5.57,1.20] | −2.68 [−6.75,1.38] | −3.61+ [−7.66,0.43] | −5.72** [−9.70,−1.74] |
| August | −1.87 [−4.39,0.65] | −1.73 [−4.91,1.45] | −3.13+ [−6.78,0.52] | −4.48* [−8.48,−0.47] | −6.54** [−10.49,−2.58] |
| September | −0.61 [−3.24,2.02] | −0.54 [−3.80,2.71] | −1.42 [−4.81,1.96] | −2.81 [−6.46,0.85] | −4.86** [−8.42,−1.30] |
| October | −1.77 [−4.36,0.82] | −2.15 [−5.36,1.07] | −1.84 [−5.39,1.71] | −5.07* [−8.93,−1.21] | −7.38** [−11.22,−3.55] |
| November | −0.40 [−3.03,2.22] | 0.03 [−3.07,3.12] | −0.97 [−4.46,2.51] | −5.15** [−8.80,−1.49] | −7.79** [−11.35,−4.22] |
| December | −1.76 [−4.30,0.78] | −1.91 [−5.15,1.33] | −0.58 [−4.22,3.07] | −5.91** [−9.46,−2.35] | −7.96** [−11.56,−4.37] |
| Hospital Characteristics | |||||
| Admitted to hospital with cath lab | −0.53 [−2.85,1.79] | −0.55 [−3.78,2.67] | −1.79 [−5.26,1.67] | −3.94* [−7.35,−0.54] | −4.01* [−7.32,−0.70] |
| Admitted to for-profit hospital | −0.77 [−3.29,1.75] | −0.55 [−3.70,2.60] | −0.80 [−4.19,2.58] | 0.75 [−2.67,4.18] | 1.61 [−1.84,5.07] |
| Admitted to government hospital | 3.02* [0.55,5.48] | 4.22** [1.23,7.21] | 4.51** [1.37,7.65] | 3.73* [0.23,7.22] | 3.52* [0.09,6.95] |
| Admitted hospital's total beds (log transformed) | −0.90 [−2.84,1.05] | −1.33 [−3.82,1.15] | −1.74 [−4.48,1.00] | 0.73 [−1.95,3.40] | 0.86 [−1.82,3.54] |
| Constant term | 20.37** [9.30,31.43] | 35.28** [21.34,49.23] | 49.19** [33.99,64.39] | 49.03** [34.14,63.91] | 52.94** [38.03,67.86] |
| N | 11625 | ||||
Appendix A2.
Association Between Ambulance Diversion of the Nearest ED And AMI Mortality Rates: Compare Patients Who Were Admitted to the Nearest ED and Those Who Bypassed the Nearest ED
| (95% CI) | 7-day | 30-day | 90-day | 9-month | 1-year |
|---|---|---|---|---|---|
| Nearest ED Diversion Status on Day of Admission | |||||
| Was not on diversion on the day of admission (reference group) | |||||
| Was exposed to <6 hrs of diversion | 0.34 [−1.95,2.64] | −1.34 [−4.36,1.69] | −0.55 [−4.06,2.96] | −0.35 [−4.15,3.45] | −0.80 [−4.43,2.84] |
| Was exposed to 6-12 hrs of diversion | 0.63 [−2.09,3.36] | 1.92 [−1.64,5.49] | −0.14 [−3.92,3.63] | −0.49 [−4.69,3.71] | −1.10 [−5.30,3.10] |
| Was exposed to ≥12 hrs of diversion | 1.59 [−1.65,4.83] | 2.14 [−1.90,6.17] | 1.69 [−2.67,6.04] | 1.75 [−2.35,5.85] | 1.66 [−2.47,5.79] |
| Patient bypassed the closest ED | 1.04 [−1.38,3.45] | 0.02 [−3.26,3.30] | −0.06 [−4.17,4.05] | 0.09 [−4.12,4.30] | −0.12 [−4.38,4.15] |
| Interaction Between Bypass indicator and Diversion Exposure Levels | |||||
| Bypass X <6 hours diversion | 0.14 [−2.69,2.96] | 2.59 [−1.28,6.47] | 1.29 [−3.48,6.06] | 1.18 [−4.00,6.35] | 1.62 [−3.50,6.74] |
| Bypass X 6-12 hours diversion | −1.02 [−4.22,2.18] | −1.17 [−5.52,3.18] | 0.54 [−4.41,5.49] | −1.07 [−6.57,4.43] | −0.28 [−5.82,5.26] |
| Bypass X ≥12 hrs of diversion | −0.23 [−4.03,3.57] | 1.90 [−3.09,6.90] | 2.05 [−3.42,7.52] | 2.05 [−3.63,7.74] | 2.38 [−3.24,8.01] |
| N | 11625 | ||||
Footnotes
Author Contributions:
Dr. Shen had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Shen, Hsia.
Acquisition of data: Shen, Hsia.
Analysis and interpretation of data: Shen, Hsia.
Drafting of the manuscript: Shen.
Critical revision of the manuscript for important intellectual content: Shen, Hsia.
Statistical analysis: Shen.
Obtained funding: Shen.
Administrative, technical, or material support: Shen.
Study supervision: Shen.
Additional Contributions:
We especially thank Laurence Baker (Stanford University, Palo Alto CA) for providing constructive suggestions throughout the project; Jean Roth (National Bureau of Economic Research, Cambridge MA) for assisting with obtaining and extracting the patient data; Shoutzu Lin (VA, Menlo Park CA) for excellent programming assistance; Tiffany Wang (UCSF, San Francisco CA) for technical assistance. None received additional compensation other than University salary for their contributions.
Conflict of Interest Disclosures:
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Reference
- 1.Institute of Medicine . Hospital-Based Emergency Care: At the Breaking Point. Institute of Medicine; Washington, DC: 2007. [Google Scholar]
- 2.DeLia D, Cantor J. Research Syntehsis Report. Vol. 17. The Robert Wood Johnson Foundation; Princeton, NJ: 2009. Emergency department utilization and capacity. Available at Available at http://www.rwjf.org/pr/product.jsp?id=45929. [Google Scholar]
- 3.Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009 Jan;16(1):1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 4.Pines JM, Prabhu A, Hilton JA, Hollander JE, Datner EM. The effect of emergency department crowding on length of stay and medication treatment times in discharged patients with acute asthma. Acad Emerg Med. 2010 Aug;17(8):834–839. doi: 10.1111/j.1553-2712.2010.00780.x. [DOI] [PubMed] [Google Scholar]
- 5.Lambe S, Washington DL, Fink A, et al. Waiting times in California's emergency departments. Ann Emerg Med. 2003 Jan;41(1):35–44. doi: 10.1067/mem.2003.2. [DOI] [PubMed] [Google Scholar]
- 6.Schafermeyer RW, Asplin BR. Hospital and emergency department crowding in the United States. Emerg Med (Fremantle) 2003 Feb;15(1):22–27. doi: 10.1046/j.1442-2026.2003.00403.x. [DOI] [PubMed] [Google Scholar]
- 7.Derlet RW, Richards JR. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000 Jan;35(1):63–68. doi: 10.1016/s0196-0644(00)70105-3. [DOI] [PubMed] [Google Scholar]
- 8.Pham JC, Patel R, Millin MG, Kirsch TD, Chanmugam A. The effects of ambulance diversion: a comprehensive review. Acad Emerg Med. 2006 Nov;13(11):1220–1227. doi: 10.1197/j.aem.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 9.Shenoi RP, Ma L, Jones J, Frost M, Seo M, Begley CE. Ambulance diversion as a proxy for emergency department crowding: the effect on pediatric mortality in a metropolitan area. Acad Emerg Med. 2009 Feb;16(2):116–123. doi: 10.1111/j.1553-2712.2008.00317.x. [DOI] [PubMed] [Google Scholar]
- 10.Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Annals of emergency medicine. 2008 Jan 1;51(1):1–5. doi: 10.1016/j.annemergmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Pines JM, Localio AR, Hollander JE, et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Annals of emergency medicine. 2007 Nov 1;50(5):510–516. doi: 10.1016/j.annemergmed.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 12.Schull MJ, Morrison LJ, Vermeulen M, Redelmeier DA. Emergency department gridlock and out-of-hospital delays for cardiac patients. Acad Emerg Med. 2003 Jul;10(7):709–716. doi: 10.1111/j.1553-2712.2003.tb00064.x. [DOI] [PubMed] [Google Scholar]
- 13.Schull MJ, Vermeulen M, Slaughter G, Morrison L, Daly P. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Annals of emergency medicine. 2004 Dec;44(6):577–585. doi: 10.1016/j.annemergmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Yankovic N, Glied S, Green LV, Grams M. The impact of ambulance diversion on heart attack deaths. Inquiry. 2010;47(1):81–91. doi: 10.5034/inquiryjrnl_47.01.81. Spring. [DOI] [PubMed] [Google Scholar]
- 15.Magid DJ, Asplin BR, Wears RL. The quality gap: searching for the consequences of emergency department crowding. Ann Emerg Med. 2004 Dec;44(6):586–588. doi: 10.1016/j.annemergmed.2004.07.449. [DOI] [PubMed] [Google Scholar]
- 16.Andrulis DP, Kellermann A, Hintz EA, Hackman BB, Weslowski VB. Emergency departments and crowding in United States teaching hospitals. Annals of emergency medicine. 1991 Sep;20(9):980–986. doi: 10.1016/s0196-0644(05)82976-2. [DOI] [PubMed] [Google Scholar]
- 17.Burt C, Mccaig L, Valverde R. Analysis of Ambulance Transports and Diversions Among US Emergency Departments. Annals of emergency medicine. 2006 Apr 1;47(4):317–326. doi: 10.1016/j.annemergmed.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Advance data. Sep 27;2006(376):1–23. [PubMed] [Google Scholar]
- 19.Mailer's Software . ZIP*Data. Melissa Data; San Clemente, CA: 2006. [Google Scholar]
- 20.Horwitz JR, Nichols A. Hospital ownership and medical services: market mix, spillover effects, and nonprofit objectives. J Health Econ. 2009 Sep;28(5):924–937. doi: 10.1016/j.jhealeco.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 21.Phibbs C. [May 7, 2011];Patient Incurred Cost - How do I estimate travel costs? 2008 http://www.herc.research.va.gov/resources/faq_h02.asp.
- 22.Phibbs C, Luft H. Correlation of travel time on roads versus straight line distance. Med Care Res Rev. 1995;52(4):532–542. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]
- 23.McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. Jama. 1994 Sep 21;272(11):859–866. [PubMed] [Google Scholar]
- 24.Maclure M, Mittleman MA. Should we use a case-crossover design? Annu Rev Public Health. 2000;21:193–221. doi: 10.1146/annurev.publhealth.21.1.193. [DOI] [PubMed] [Google Scholar]
- 25.Buchmueller T, Jacobson M, Wold C. How far to the hospital? The effect of hospital closures on access to care. Journal of Health Economics. 2006 Jul 1;25(4):740–761. doi: 10.1016/j.jhealeco.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 26.Greene WH. Econometric analysis. 6th ed. Prentice Hall; Upper Saddle River, N.J.: 2008. [Google Scholar]
- 27.Skinner J, Staiger DO. Technology diffusion and productivity growth in health care. NBER Working Paper 14865. 2009 Jan 1; doi: 10.1162/REST_a_00535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stock JH, Watson MW. NBER technical working paper series no. t0323. National Bureau of Economic Research; Cambridge, Mass: 2006. Heteroskedasticity-Robust Standard Errors for Fixed Effects Panel Data Regression. http://www.nber.org/papers/t0323. [Google Scholar]
- 29.Burt C, Mccaig L. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Advance data. Sep 27. 2006(376):1–23. [PubMed] [Google Scholar]
- 30.Burt CW, Arispe IE. Characteristics of emergency departments serving high volumes of safety-net patients: United States, 2000. Vital Health Stat. 2004 May 13;(155):1–16. [PubMed] [Google Scholar]
- 31.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and Characteristics of U.S. Emergency Department Visits, 1997-2007. Jama. 2010;304(6):664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008 Sep 24;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Norris RM. Circumstances of out of hospital cardiac arrest in patients with ischaemic heart disease. Heart. 2005 Dec;91(12):1537–1540. doi: 10.1136/hrt.2004.057018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson MJ, Nguyen K. Bursting at the seams: Improving patient flow to help America's emergency departments. The George Washington University Medical Center; Washington, D.C.: 2004. [Google Scholar]
- 35.Rehayem A. Implementing a Statewide Ambulance No-Diversion Policy. Vol. 24. National Association of State EMS Officials; Sep, 2009. p. 2009. [Google Scholar]
- 36.Castillo EM, Vilke GM, Williams M, Turner P, Boyle J, Chan TC. Collaborative to Decrease Ambulance Diversion: The California Emergency Department Diversion Project. J Emerg Med. 2011 Mar;40(3):300–7. doi: 10.1016/j.jemermed.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 37.Auerbach J, Dreyer P. Circular Letter: DHCQ 08-07-494; Changes to ambulance diversion policies. Massachusetts Department of Public Health; Jul 3, 2008. [May 21, 2010]. http://www.mass.gov/Eeohhs2/docs/dph/quality/hcq_circular_letters/hospital_general_0807494.pdf. [Google Scholar]
- 38.Burke L. Ending Ambulance Diversion in Massachusetts. Virtual Mentor. 2010;12(6) doi: 10.1001/virtualmentor.2010.12.6.pfor2-1006. [DOI] [PubMed] [Google Scholar]
- 39.Millard WB. Stand By to Repel Boarders: The Rise of Regional No-Diversion Policies. Annals of Emergency Medicine. 2011;57(5):15A. [Google Scholar]
- 40.Cameron P, Scown P, Campbell D. Managing access block. Aust Health Rev. 2002;25(4):59–68. doi: 10.1071/ah020059. [DOI] [PubMed] [Google Scholar]
- 41.Schneider S, Zwemer F, Doniger A, Dick R, Czapranski T, Davis E. Acad Emerg Med. 11. Vol. 8. a decade of emergency department overcrowding; Rochester, New York: Nov, 2001. pp. 1044–1050. [DOI] [PubMed] [Google Scholar]
- 42.McConnell KJ, Richards CF, Daya M, Bernell SL, Weathers CC, Lowe RA. Effect of increased ICU capacity on emergency department length of stay and ambulance diversion. Ann Emerg Med. 2005 May;45(5):471–478. doi: 10.1016/j.annemergmed.2004.10.032. [DOI] [PubMed] [Google Scholar]