Abstract
Objective
To describe the current status of institutional facilities and the supporting research infrastructure of surveyed health research institutions in Africa, including information on communication technologies and connectivity, library resources, and laboratory operations and resources.
Design
A structured questionnaire was used to solicit information on institutional facilities at health research institutions.
Setting
Health research institutions in 42 sub-Saharan African countries.
Participants
Key informants from 847 health research institutions.
Main outcome measures
The availability of laboratory, information and communication, and library facilities in health research institutions.
Results
Less than half of the respondent health research institutions had computer laboratories (49%), network computers (50%) and information technology support (38%). More than two-thirds (67%) had a library. Electronic subscriptions to international journals were observed to be very low, with an average of three subscriptions per institution. Almost two-thirds of the surveyed institutions (69%) reported having laboratories, about half of which (55%) were accredited nationally. Linkages and research collaborations were generally weak, particularly those with other laboratories in the Region. Challenges included financial and human resource constraints and the inability to communicate effectively with partners.
Conclusions
Health research institutions in the Region have insufficient access to essential facilities such as laboratories, libraries, computers and the Internet to generate, access and share information.
Keywords: research systems, research facilities, Africa research, health research
Introduction
Over the past few years, there has been a growing interest in promoting health research systems, and a consensus has been formed that stronger health research systems are key to achieving improved health outcomes globally1 and in African countries in particular. The World Health Organization (WHO)2 defines a health research system as:
‘… the people, institutions and activities whose primary purpose is to generate high-quality knowledge that can be used to promote, restore and/or maintain the health status of populations. It can include mechanisms adopted to encourage the utilization of research.’
Deriving from this definition, critical factors for the creation and strengthening of robust health research systems include the availability of financial resources, sufficient human competencies and supporting health research infrastructure and facilities.
This paper provides an insight, based on survey data, into the current status of institutional facilities and supporting research infrastructure of surveyed health research institutes in Africa. Along with filling the gap in published African studies on research infrastructure and institutional facilities in health research organizations, the paper provides empirical data to aid decision-making on policies and strategies to strengthen health research systems in Africa.
Methods
The methods followed to assess national health information systems are described elsewhere3 but are summarized briefly here.
This paper analyses survey data collected from health research organizations in 42 countries in the WHO African Region. The survey used Tool 6 from the Health Research System Analysis Initiative: Methods for Collecting Benchmarks and Systems Analysis Toolkit.4 Within the institutional survey, seven questionnaires, representing separate ‘modules’, were completed by the respondent institutions. This report draws on data from one those questionnaires: Module 6000 – Institutional facilities and field sites.
The questionnaire was designed to elicit relevant information on the status and availability of facilities and infrastructure that were identified as critical for the optimal functioning of these research organisations.
The questionnaires were completed by senior personnel such as administrative officials or research directors at the health research institutions, who were considered to be well-informed key informants. Health research organisations were identified to include government agencies, hospitals, non-governmental organisations or charities, pharmaceutical companies, medical schools, other universities and independent research institutions. A total of 847 health research organisations were surveyed, and these formed the basis of the empirical analysis presented in this paper. Table 1 summarises the distribution of each respondent group. Government agencies constituted the highest proportion (30%) of respondents, followed by hospitals (18%).
Table 1.
Characteristics of health research institutions in 42 sub-Saharan African countries, 2009.
| Characteristics | Health research institutions |
|
|---|---|---|
| n* | % | |
| Age of institution (years) (n = 694) | ||
| <30 | 426 | 61 |
| 30–59 | 200 | 29 |
| ≥60 | 68 | 10 |
| Sector the institution belong to (n = 762) | ||
| Public | 536 | 70 |
| Private not-for-profit | 132 | 17 |
| Para-state | 37 | 5 |
| Private for-profit | 26 | 3 |
| Other | 31 | 4 |
| Type of institution (n = 847) | ||
| Government agencies | 257 | 30 |
| Hospitals | 154 | 18 |
| Medical schools | 108 | 13 |
| Independent research institutions | 106 | 13 |
| Other research institutions (non-governmental organisations, charities) | 105 | 12 |
| Other universities | 95 | 11 |
| Other | 22 | 3 |
| Level at which institution functions (n = 751) | ||
| National | 483 | 64 |
| Local | 140 | 19 |
| Regional | 60 | 8 |
| International | 55 | 7 |
| Other | 13 | 2 |
| Primary functions of institution (n = 697) | ||
| Conduct research on health topics | 374 | 54 |
| Academic | 373 | 54 |
| Provide health services | 338 | 48 |
| Conduct research on non-health topics | 122 | 18 |
| Product development or distribution | 74 | 11 |
| Other | 128 | 18 |
| National official or working language (n = 847) | ||
| French | 445 | 53 |
| English | 285 | 34 |
| Other | 117 | 14 |
| Institution has mandate on | ||
| Research of all types | 571 | 79 (n = 723) |
| Health research | 563 | 77 (n = 731) |
*Number of respondent health institutions, out of the 847 surveyed.
The analysis in this paper is based on three variables identified as playing a critical role in enhancing the proper and optimal functioning of health research centres in Africa:
Availability of, and connectivity to, information and communication technologies (ICT)
Library resources
Laboratory operations and resources
Concerning the ICT variable, we asked the surveyed institutions to provide information concerning the availability of ICT infrastructure. The indicators for ICT infrastructure included computing equipment and facilities such as data storage servers, Internet access, individual staff email addresses, institutional websites, network connectivity and the availability of information technology (IT) help at the institution.
Regarding the library resource variable, we asked institutions whether they had a library and, if so, the types of library resources that were available. The library resources indicators considered were the availability of Internet access in the library and the use of online resources such as online catalogues and electronic subscriptions to journals. We also investigated the level of subscriptions to locally and regionally published journals, the availability of a reference desk and interlibrary loan facilities.
For the laboratory operations and resources variable, we investigated the availability of laboratories in the surveyed health research institutions. We further investigated if these laboratories were accredited and whether they had adequate capacities and facilities to handle infectious agents safely. We also investigated the extent to which laboratories had linkages with other laboratories within the country, regionally and globally. Finally, we identified the main obstacles hindering the effective functioning of these laboratories.
For responses to questions where institutions were asked to rank items in the questionnaire, we used weighting schemes to arrive at composite ranks. For example, where the response required ranking an item on a 1–5 scale, a weight of five was given to the first rank, four to the second rank and so on, with the fifth rank getting the least weight of one. The average of these was used to derive a composite rank of items.
We used IBM® SPSS® Statistics Version 19 statistical software to analyse the data.
Results
This section provides the results obtained from the analyses of the three key variables that were identified as critical in enhancing research capacity at African health research institutions: ICT use and connectivity, library resources, and laboratory operations and resources.
ICT use and connectivity
The availability and use of ICT facilities in the surveyed institutions was low (Table 2). Only half the respondent institutions (50%) had networked computers, and less than half had computer laboratories (49%) and IT support (38%). Less than half of the respondent institutions (46%) had daily Internet access while only 54–63% provided staff with a computer (Table 3).
Table 2.
Availability of IT connectivity, facilities and software in health research institutions in the WHO African Region, 2009.
| IT facility, conductivity and software | Health research institutions |
|
|---|---|---|
| n* | % | |
| Facility | ||
| Computer laboratory | 197 | 49 (n = 404) |
| Meeting/conference room | 235 | 58 (n = 404) |
| Classroom/seminar room | 314 | 78 (n = 404) |
| Networks and support | ||
| Networked computers | 226 | 50 (n = 449) |
| IT support | 169 | 38 (n = 444) |
| Access to Internet | ||
| Daily access to Internet | 386 | 75 (n = 515) |
| Unique email address provided | 258 | 51 (n = 508) |
| Institutional website | 239 | 41 (n = 586) |
| Software packages available | ||
| Spreadsheets | 423 | 98 (n = 434) |
| Databases | 293 | 68 (n = 431) |
| Bibliographic referencing | 126 | 29 (n = 433) |
| Statistical packages | 220 | 51 (n = 434) |
| Epidemiological packages | 212 | 49 (n = 434) |
| Qualitative analysis | 65 | 15 (n = 433) |
| Project management | 95 | 22 (n = 434) |
| Algorithmic | 27 | 6 (n = 434) |
| Simulation | 31 | 7 (n = 434) |
| Geographic information system | 93 | 21 (n = 434) |
*Number of respondent health institutions, out of the 847 surveyed.
Table 3.
Access to computers and IT services in health research institutions in the WHO African Region, 2009.
| Access to computers and IT service | Health research institutions |
|
|---|---|---|
| n | % | |
| Provision of computer | ||
| Researcher with < 5 years of experience | 217 | 54 (n = 403 |
| Researcher with 5–10 years of experience | 251 | 62 (n = 403) |
| Researcher with 10–20 years of experience | 252 | 63 (n = 403) |
| Director or head of the institute | 345 | 86 (n = 403) |
| Does not provide computer | 37 | 9 (n = 403) |
| Provision of computer printer | ||
| Researcher with < 5 years of experience | 182 | 47 (n = 387) |
| Researcher with 5–10 years of experience | 208 | 54 (n = 387) |
| Researcher with 10–20 years of experience | 223 | 58 (n = 387) |
| Director or head of the institute | 320 | 83 (n = 387) |
| Does not provide computer printer | 40 | 10 (n = 386) |
| Provision of Internet access | ||
| Researcher with < 5 years of experience | 208 | 57 (n = 366) |
| Researcher with 5–10 years of experience | 230 | 63 (n = 366) |
| Researcher with 10–20 years of experience | 233 | 64 (n = 366) |
| Director or head of the institute | 299 | 82 (n = 366) |
| Does not provide Internet | 45 | 12 (n = 375) |
Library resources
More than two-thirds (69%) of respondent institutions had a library (Table 4). Electronic subscriptions to international journals were observed to be very low, with an average of three subscriptions per institution. These observations indicate that, despite access to ICT infrastructure, health research institutions in Africa do not use ICT infrastructure for library services.
Table 4.
Availability and accessibility of library resources in health research institutions in the WHO African Region, 2009.
| Availability and accessibility of library resource | Health research institutions |
|
|---|---|---|
| n | % | |
| Presence of a library | 428 | 69 (n = 624) |
| Library | ||
| Is part of a consortium | 52 | 12 (n = 409) |
| Participates in interlibrary loans | 75 | 18 (n = 427) |
| Has a professional information specialist | 167 | 39 (n = 426) |
| Has a reference desk | 265 | 63 (n = 419) |
| Access to the library | ||
| All staff of institution | 386 | 98 (n = 395) |
| Researchers from other institutions | 338 | 86 (n = 395) |
| General public | 201 | 51 (n = 395) |
| External consultants | 291 | 74 (n = 395) |
| Other | 75 | 19 (n = 394) |
| n | Mean (95% confidence interval lower, upper limit) | |
| Library collections | ||
| Books/volumes in the collection | 298 | 7588 (4601, 10,576) |
| Computers | 389 | 9 (1.5, 17) |
| Paid electronic subscriptions | 268 | 3 (0, 7) |
| Print subscriptions | 307 | 30 (4, 56) |
| Scientific journals subscriptions | 301 | 46 (4, 87) |
The data show that interlibrary loan facilities were not commonly used (18%) and that most libraries had manned reference desks (63%). There were, on average, over 7500 books in a library collection, about 30 print subscriptions and 46 scientific journal subscriptions per respondent institution (Table 4).
Laboratory operations and resources
Close to two-thirds (69%) of the respondent institutions reported having laboratories and about half of these (55%) were accredited nationally (Table 5). On the question of the presence of linkages with other laboratories within the country, regionally and globally, about half of the respondent institutions (48%) had laboratories with links to other laboratories within the country, about one-third (35%) had laboratories with links to other laboratories in the world, but only one-quarter reported linkage with other laboratories in neighbouring countries.
Table 5.
Availability of laboratory facilities in health research institutions in the WHO African Region, 2009.
| Laboratory characteristics | Health research institutions |
|
|---|---|---|
| n* | % | |
| Presence of at least one laboratory in the institution | 363 | 61 (n = 597) |
| Linked with other laboratories in country | 163 | 47 (n = 348) |
| Linked with other laboratories in neighbouring countries | 96 | 27 (n = 351) |
| Linked with other laboratories in the world | 126 | 35 (n = 356) |
| Recognised as a national reference | 164 | 45 (n = 361) |
| Accredited nationally | 205 | 55 (n = 373) |
| Laboratory resources | ||
| Line budget for staff training on safety issues | 127 | 36 (n = 355) |
| Line budget for staff training on technical aspects | 162 | 44 (n = 366) |
| Written safety procedures and policies | 177 | 49 (n = 360) |
| Laboratory able to handle any infectious agents | 198 | 57 (n = 346) |
| Line budget for equipment maintenance | 243 | 65 (n = 373) |
| Line budget for equipment purchase | 253 | 68 (n = 374) |
| Line budget for equipment supplies | 260 | 70 (n = 374) |
| Highest risk group of infectious agents that laboratory can handle | ||
| No or low individual and community risk | 49 | 23 (n = 213) |
| Moderate individual risk, low community risk | 70 | 33 (n = 213) |
| High individual risk, low community risk | 40 | 19 (n = 213) |
| High individual and community risk | 54 | 25 (n = 213) |
*Number of respondent health institutions, out of the 847 surveyed.
Other measures of the quality of a laboratory and its performance may be through the existence of safety procedures and codes and the availability of facilities to handle biological samples of varying risk levels. In order to understand their biosafety capacities, the surveyed institutions were asked to indicate the risk group that their laboratory could handle, varying from the lowest risk to the highest. Table 5 shows that 23% of respondent institutions indicated having laboratories attaining level 1 basic biosafety, 33% had laboratories attaining level 2 basic biosafety and 25% had laboratories attaining the highest risk group 4 for maximum containment.
Institutions were also asked to indicate the laboratory facilities available for handling the highest risk group of infectious agents. Most of the laboratories, though not all, had sterilisation equipment, protective clothing and means for safe disposal of agents (Figure 1). However, these laboratories lacked other critical facilities such as personnel safety monitoring capacity, effluent treatment capability and ante-rooms with airlock and showers.
Figure 1.
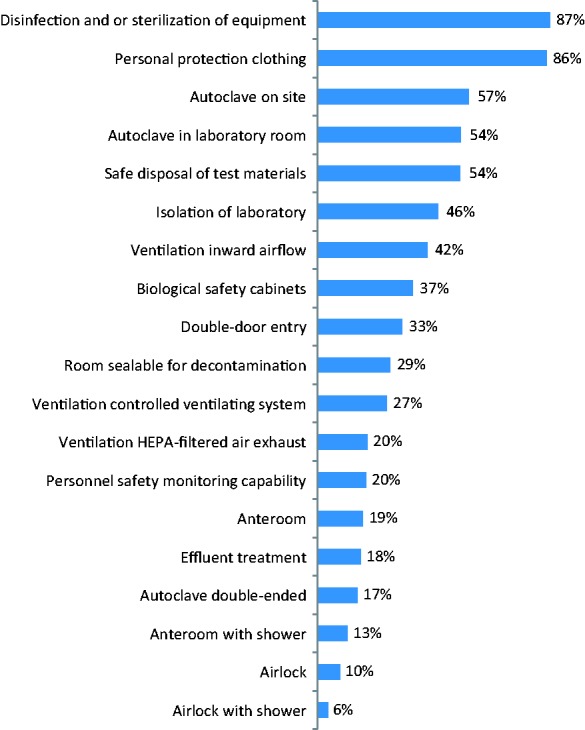
Percentage of health research institutions with biosafety supplies or facilities that handle the highest risk group of infectious agents, WHO African Region, 2009 (n = 239).
The survey identified a number of challenges affecting the institutions’ ability to function effectively, including financial constraints, human resource constraints and the inability to communicate with partners effectively (Figure 2). Financial constraints affecting laboratories were mainly those associated with the purchase and maintenance of laboratory equipment, the purchase of laboratory supplies and consumables, and operational costs. The main human resource obstacles were identified as having inadequate laboratory staff, compounded with the inability to attract and hire well-qualified laboratory staff. Other challenges included the inability to provide on-job training for staff and specimen transportation.
Figure 2.
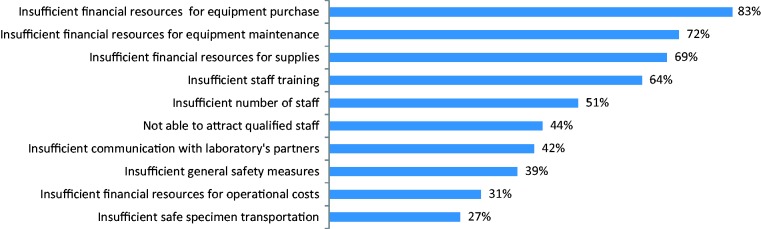
Main obstacles to the effective functioning of laboratories of health research institutions in the WHO African Region, 2009.
Discussion
The results presented in this paper provide an overview of the status of ICT facilities in health research institutions in the Region. We acknowledge the difficulty in making generalised conclusions based on the data presented here but argue that this paper identifies strengths and weakness in institutional infrastructure. By identifying these strengths and weaknesses, the paper highlights ‘problematic’ areas that require immediate policy intervention. The paper also provides sufficient preliminary findings that can provide a basis for future in-depth research on specific questions.
The analysis presented has a number of methodological and data limitations. The main limitation is the inability to conduct a robust comparative analysis of institutional facilities at the country level due to the lack of uniformity in the response rates and distribution of different respondent groups from each country. This is compounded by the fact that health research systems operate in contextual environments that are affected and influenced by different nation-specific factors.
The results show that a considerable proportion of health research institutions do not have basic access to ICT infrastructure, laboratories, libraries and library facilities. However, an important point that arises from this research is that the ICT connectivity problem in Africa is not just a question of ICT connectivity but also a question of the optimal use of ICT infrastructure for communication and accessing knowledge. The results are not surprising, as coverage for Internet use in the Region is low (16 per 100 inhabitants,5 with lower rates in rural areas, compared with the cities). The quality of connection is also not adequate; very few countries have fibre-optic or satellite broadband connections. The slow connectivity may also discourage use even in situations where Internet connections are available.
There is a dearth of health research libraries in the continent. Over half of the institutions that took part in this survey did not have libraries. The majority of the institutions that did have libraries reported having access to ICT tools, but only a few had online catalogues, subscriptions to online journals or even Internet links in the library, pointing to the poor use of ICT infrastructure in library services. Several initiatives have been implemented to give researchers free online access to the full text of health research papers published in journals. HINARI (Health InterNetwork Access to Research Initiative), a partnership led by WHO involving more than 150 publisher partners is one example (see http://www.who.int/hinari/about/en/).
Among other health services, laboratory services are essential components that must be improved in order to support disease or disorder management in the Region. Several assessments of laboratories in the Region have shown the need for infrastructural and technical capacity strengthening to support HIV/AIDS programmes. The 2007 assessment showed that most African governments were developing their national strategic plans and mobilising resources for laboratory services in both the private and public sectors. The availability of trained, skilled human resources was the main challenge to improving laboratory capacity.6
Laboratory services are essential to identify the agents involved in important public health events, including those which may cause epidemics and pandemics.7 Functional specimen transport systems, combined with strong laboratory biorisk management measures and laboratory quality systems should be in place if laboratories are to release results in a safe, secure, timely and reliable manner. This paper shows that most laboratories operate under severe financial constraints and thus lack the capacity to deal with high levels of risks (i.e. levels 3 and 4). The capability to handle risky agents must be strengthened and enhanced in laboratories in African institutions. Linkages and research collaboration are generally weak, particularly with other laboratories in the Region, and these links should be encouraged since geographically co-located regions tend to have similar health problems.
Conclusions
The study shows that health research institutions in the Region have insufficient access to essential facilities such as laboratories, libraries, computers and the Internet to generate, access and share information. Countries should ensure that adequate financial resources are mobilised and available to improve these facilities in health research institutions.
Declarations
Competing interests
None declared
Funding
WHO Regional Office for Africa
Ethical approval
Not applicable
Guarantor
DK
Contributorship
DK wrote the paper and carried out statistical analyses; CK, PEM, IS and WK reviewed the paper and assisted with fieldwork; PSLD reviewed the initial design of the study and provided support and overall leadership.
Acknowledgements
WHO Country Office focal persons for information, research and knowledge management are acknowledged for their contribution in coordinating the surveys in countries. Their counterparts in ministries of health are also acknowledged. These surveys would not have been possible without the active participation of the head of health research institutions and their department heads who have given their time and effort to fill out and send back the completed modules and questionnaires. We also acknowledge the contribution of the consultant who prepared the background material for this paper.
Provenance
Not commissioned; peer-reviewed by Bruce Currey
References
- 1.Hanney S, González Block MA. Building health research systems to achieve better health. Health Res Policy Syst 2006; 4: 10–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Health Research Systems Analysis (HRSA) Concepts and Indicators. See http://www.who.int/rpc/health_research/concepts/en/index.html (last checked 2 June 2008).
- 3.Kebede D, Zielinski C, Mbondji PE, Sanou I, Kouvividila W, Lusamba-Dikassa P-S. Surveying the knowledge landscape in sub-Saharan Africa: methodology. J R Soc Med 2014; 107(suppl. 1): 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sadana R, Lee-Martin SP, Racelis R, Lee J, Berridge S. Health Research System Analysis (HRSA) Initiative: Methods for Collecting Benchmarks and Systems Analysis Toolkit. Tool #6. Survey of Institutions Contributing to Health Research, Geneva: World Health Organization, 2007. [Google Scholar]
- 5.International Telecommunication Union. The World in 2013: ICT Facts and Figures, Geneva: International Telecommunication Union, 2013. [Google Scholar]
- 6.World Health Organization. HIV and AIDS Laboratory Capacity. Where are We? Overview of Laboratory Capacity in Africa 2005–2007, Brazzaville: World Health Organization Regional Office for Africa, 2010. [Google Scholar]
- 7.World Health Organization. Compendium of Public Health Strategies. Volume 1: WHO Regional Committee for Africa 48th–61st Sessions (1998–2011), Brazzaville: World Health Organization Regional Office for Africa, 2012. [Google Scholar]


