Abstract
Background
Disasters are destructive, potentially traumatic events that affect millions of youth each year.
Objective
The purpose of this paper was to review the literature on depressive symptoms among youth after disasters. Specifically, we examined the prevalence of depression, risk factors associated with depressive symptoms, and theories utilized in this research area.
Methods
We searched MEDLINE, PsycInfo, and PubMed electronic databases for English language articles published up to May 1, 2013. Reference lists from included studies were reviewed to capture additional studies. Only quantitative, peer reviewed studies, conducted with youth under the age of 18 years, that examined postdisaster depressive symptoms were included. Seventy-two studies met inclusion criteria. Prevalence of depressive symptoms, disaster type, correlates of depressive symptoms, and theories of depressive symptoms were reviewed.
Results
Only 27 studies (38%) reported on prevalence rates among youth in their sample. Prevalence rates of depression among youth postdisaster ranged from 2% to 69%. Potential risk factors were identified (e.g., female gender, exposure stressors, posttraumatic stress symptoms). Theories were examined in less than one-third of studies (k = 21).
Conclusions
Given the variability in prevalence rates, difficulty identifying a single profile of youth at risk for developing depressive symptoms, and lack of a unifying theory emerging from the studies, recommendations for future research are discussed. Use of established batteries of assessments could enable comparisons across studies. Merging existing theories from children’s postdisaster and depression literatures could aid in the identification of risk factors and causal pathways.
Keywords: disaster, children, depression, review, theory
Disasters are destructive, potentially traumatic events. Disasters may include events that are natural (e.g., tornadoes, floods, hurricanes) or man-made (e.g., 9/11, nuclear explosions; Furr, Comer, Edmunds, & Kendall, 2010). Unfortunately, disasters are common and affect millions of children each year (Guha-Sapir, Vos, Below, & Ponserre, 2012; Seballos, Tanner, Tarazona, & Gallegos, 2011).
After disasters, many youth (i.e., children and adolescents) report posttraumatic stress (PTS) symptoms (Bal, 2008; Comer et al., 2010; Dyb, Jensen, & Nygaard, 2011; La Greca et al., 2013; La Greca, Silverman, Lai, & Jaccard, 2010; Yelland et al., 2010) and/or depressive symptoms (Goenjian et al., 1995; 1996; Grant, Hardin, Pesut, & Hardin, 1997; Hardin, Weinrich, Weinrich, Hardin, & Garrison, 1994; Lai, La Greca, Auslander, & Short, 2013; Papadatos, Nikou, & Potamianos, 1990). Several metaanalyses and reviews have summarized the literature on youth PTS symptoms postdisaster (Alisic, Jongmans, van Wesel, & Kleber, 2011; Furr et al., 2010; Trickey, Siddaway, Meiser-Stedman, Serpell, & Field, 2012). However, no reviews of youth postdisaster depressive symptoms exist. Thus, we have limited knowledge about prevalence rates of youth postdisaster depression and risk factors that contribute to depressive symptoms. This information is needed, as depressive symptoms are associated with negative life outcomes (e.g., poor academic functioning, substance use, suicide attempts; Birmaher et al., 1996; Horowitz & Garber, 2006). The purpose of this paper was to review the literature on youth postdisaster depressive symptoms, in order to understand how depression is elicited by trauma exposure (Galea, Nandi, & Vlahov, 2005; Trickey et al., 2012) and to inform future directions for research and treatment.
Our first aim was to examine prevalence rates of youth postdisaster depression. These rates have not yet been assessed. We characterized prevalence rates of youth depression by disaster type (i.e., natural or man-made), as man-made disasters may have different consequences for mental health (Galea et al., 2005).
Our second aim was to identify risk factors for youth postdisaster depressive symptoms. This knowledge is important for understanding youth postdisaster depression and its causes. Clinically, this information is needed to create tailored postdisaster interventions. Risk factors for postdisaster depressive symptoms may differ from those identified in the general depression literature. For example, among youth studied after a terrorist bombing in Israel, bombing-related perceived stress was associated with youth depressive symptoms (Shahar, Cohen, Grogan, Barile, & Henrich, 2009). Thus, specific disaster-related risk factors may need to be considered when designing postdisaster interventions.
In this study, we examined the following risk factors: child characteristics (i.e., age and gender), disaster exposure stressors (e.g., perceiving you might die during the disaster, actual life-threatening events such as a tree falling on your home, seeing someone be hurt or injured), and PTS symptoms. We expected that older age might be a risk factor for depressive symptoms, given that adolescence is a “critical period” of vulnerability for depression (Jacobs, Reinecke, Gollan, & Kane, 2008). We also expected that female gender would be a risk factor for depressive symptoms, based on research in the general depression literature identifying female gender as a risk factor (Cole, Peeke, Martin, Truglio, & Seroczynski, 1998). Further, we expected disaster exposure stressors to be associated with greater depressive symptoms, given associations between stressors and depressive symptoms generally (Hyde, Mezulis, & Abramson, 2008). We also expected PTS symptoms to be associated with depressive symptoms, as these symptoms are often comorbid postdisaster (Goenjian et al., 2011; Lai et al., 2013).
As our final aim, we summarized theories utilized to understand postdisaster depressive symptoms in youth. Currently, it is unclear whether youths’ postdisaster depressive symptoms are best understood from a general depressive symptom framework, a disaster framework, or both. Numerous conceptual theories have been developed to understand depression generally (Abramson, Metalsky, & Alloy, 1989; Beck, 1993), but these theories may not apply postdisaster, due to factors unique to the postdisaster environment. At the same time, postdisaster frameworks of youth functioning after disasters have focused on PTS symptoms (Ehlers & Clark, 2000; La Greca, Silverman, Vernberg, & Prinstein, 1996). It is unknown whether these frameworks may apply to postdisaster depressive symptoms. A summary of current conceptual theories being tested in this area are needed to guide future research.
Method
This review followed current guidelines on reporting systematic reviews (Moher, Liberati, Tetzlaff, & Altman, 2009). We conducted a literature search for studies examining disasters and depressive symptoms; we included any article published up to May 1, 2013. The initial search was conducted using MEDLINE, PsycInfo, and PubMed. Searches were conducted by crossing two sets of keywords: 1) disaster*, brushfire*, earthquake*, fire*, flood*, hurricane*, manmade disaster*, natural disaster*, posttraumatic stress*, PTSD, terrorism, tornado*, trauma*, tsunami*, or bomb; and 2) adolescent*, child*, schoolchild*, youth, and depress*.
Next, the following journals were searched for studies regarding trauma, youth psychopathology, and depression in youth: Journal of Traumatic Stress, American Journal of Psychiatry, Archives of General Psychiatry, Journal of Consulting and Clinical Psychology, Journal of Abnormal Child Psychology, Journal of Abnormal Psychology, Journal of Affective Disorders, Journal of Anxiety Disorders, Behaviour Research and Therapy, British Journal of Psychiatry, Depression and Anxiety, Development and Psychopathology, European Child and Adolescent Psychiatry, Journal of the American Academy of Child and Adolescent Psychiatry, Journal of Child Psychology and Psychiatry, Journal of Clinical Child and Adolescent Psychology, and Pediatrics.
Searches for authors identified as experts in the field of disasters and depressive symptoms among youth were then conducted. Finally, we manually searched the reference lists of each study included in the review.
Study Selection
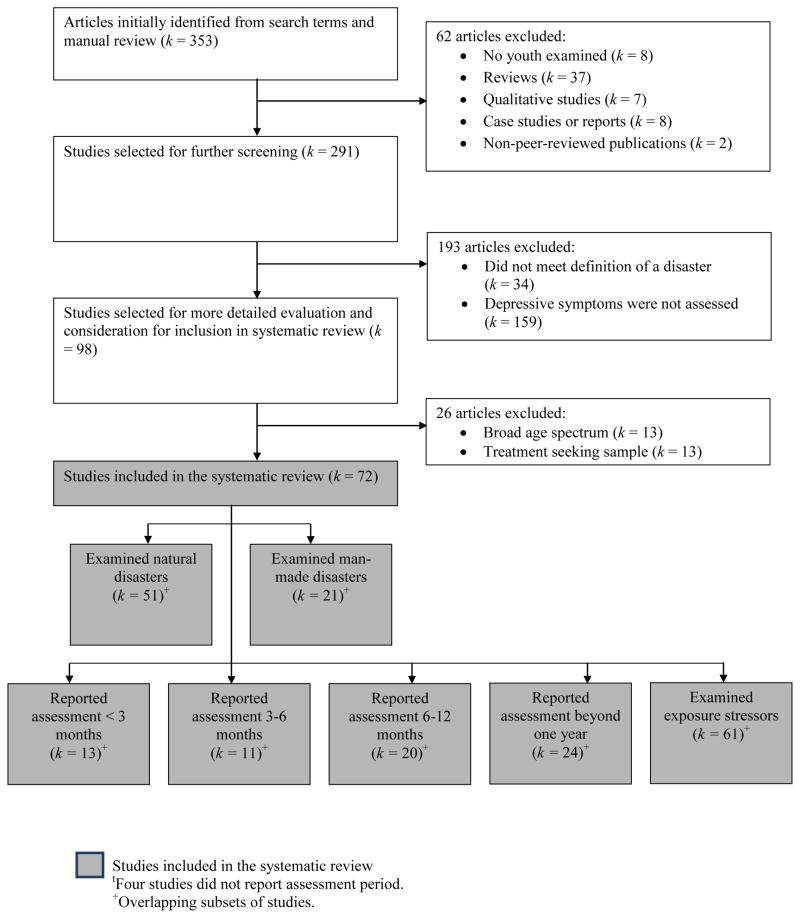
The initial search identified 353 articles. Abstracts of these articles were examined to determine if articles met inclusion criteria (Figure 1). Criteria were derived from a metaanalysis on youth PTS symptoms postdisaster (Furr et al., 2010). Tier 1. Only quantitative, peer reviewed studies conducted with youth were included. Studies had to include youth under the age of 18 years as part of their sample. Reviews, qualitative studies, case studies, non-peer reviewed publications, and reports were excluded. Tier 2. All studies had to examine depressive symptoms (demonstrated by including a measure of depression) after exposure to distinct, identifiable disasters, which we defined as “events that are relatively sudden, highly disruptive, and time-limited (even though the effects may be longer lasting), and public (affecting youth from more than one family)” (Vogel & Vernberg, 1993). Studies examining child abuse, war, or political violence were excluded. Tier 3. To ensure that findings were generalizable to youth exposed to disasters, studies examining a broad age spectrum that did not look at youth specifically were eliminated. In addition, studies that examined a highly specialized, treatment seeking population (e.g., depressive symptoms among treatment seeking youth) were excluded. This process yielded 72 studies that met inclusion criteria.
Figure 1.
Flow chart of candidate articles.
Data Synthesis
For the current study, we chose a narrative synthesis of the literature, which allowed for a summary of the current state of the literature on youth postdisaster depressive symptoms. Utilizing a narrative synthesis also allowed us to identify and examine relevant studies in more detail, so that we could make recommendations for future research specifically as it relates to the measurement and prevalence of depression, evaluation of risk factors, and use of theories.
Funding
There was no funding body involved in the decision to submit this paper for publication. Research time for the preparation of this manuscript was supported by a training grant from the National Institute of Child Health and Human Development (NICHD; T32HD07510).
Coding of Studies
Criteria used in this study were derived from criteria used in past metaanalyses examining children’s PTS reactions to traumatic events (Alisic et al., 2011; Furr et al., 2010). Each study was examined for reported prevalence rates of depressive symptoms. Type of disaster was coded as natural or man-made.
Due to the lack of unifying conceptualizations regarding postdisaster depressive symptoms among youth, we utilized a conservative approach and recorded all potential risk factors that were examined in relationship to depressive symptoms. To identify theories utilized, we examined whether studies included statements about theories, aims, or hypotheses related to depressive symptoms (following methodology outlined by Alisic et al., 2011). A study was coded as including theory when it referred to “theory,” “conceptualization,” “framework,” “grounded,” and “underpinnings” in the title, abstract, or introduction. A study was coded as including aims when it utilized words such as “purpose,” “aim,” “objective,” and “this study sought to.” Finally, a study was coded as including hypotheses when the terms “hypothesis” or “we expected” were utilized.
Results
Aim One: Prevalence Rates of Depression
Across the 72 studies examined in this review, 18 (25%) studies utilized a categorical definition for assessing depression (e.g., presence or absence of clinically significant depression assessed through the Kiddie Sads), 39 (54%) utilized a continuous measure of depression (e.g., the Revised Child Anxiety and Depression Scale), and 15 (21%) utilized both a categorical and a continuous definition for assessing depression (e.g., utilizing the Children’s Depression Inventory and a cutoff score for clinically significant depression). Only 27 studies (38% of the 72 studies examined) reported prevalence rates of depression among youth in their sample. Of these studies, 20 reported on depressive symptom prevalence rates after a natural disaster, and 7 studies reported on prevalence rates after a man-made disaster.
After exposure to a natural disaster, prevalence rates varied widely, from 4% at 18 months post-hurricane among youth (ages 4–17 years) in Puerto Rico (Felix et al., 2011), to 69% among youth (male M age=18.25 years; female M age=17.23 years) assessed two weeks after an earthquake in Greece (Papadatos et al., 1990). Generally, prevalence rates of depression were higher among children assessed less than three months after the natural disaster (k=4), when compared to children assessed at time points later than three months postdisaster. For example, in addition to the 69% prevalence rate just reported, prevalence rates were 10% among displaced children (M age=15.51 years) two months after an earthquake in Turkey (Vehid, Alyanak, & Eksi, 2006), 13% among displaced children (ages 7–14 years) two months after the 2004 Tsunami in Thailand (Thienkrua et al., 2006), and 32% among children (ages 7–12 years) assessed less than one month after exposure to Hurricane Gustav (Salloum, Carter, Burch, Garfinkel, & Overstreet, 2011). In contrast, depression prevalence rates were lower when youth were assessed one year or more after a natural disaster. For example, 6% of youth (peak age was 9–10 years) assessed one year after a tsunami reported clinically significant depressive symptoms (Piyasil et al., 2008), and 5.5% of youth (grades 4–9) reported clinically significant depression when assessed one year after a tsunami (Piyasil et al., 2008).
After exposure to a man-made disaster, prevalence rates of depressive symptoms also varied widely, from 2% among an exposed sample of children (M age=11.7 years) assessed five years after a fireworks explosion (Boer, Smit, Morren, Roorda, & Yzermans, 2009) to 34% of youth (M age at follow-up was 21.3 years) assessed 5 to 8 years after the Jupiter disaster (Bolton, O’Ryan, Udwin, Boyle, & Yule, 2000). However, prevalence rates reported were generally under 10% (Boer et al., 2009; Breton, Valla, & Lambert, 1993; Comer et al., 2010; Dirkzwager, Kerssens, & Yzermans, 2006; Hoven et al., 2005).
Aim Two: Correlates of Depressive Symptoms
Child Characteristics
Seven articles examined relationships between age and depressive symptoms (see Table 2). No clear relationships between age and depressive symptoms emerged from these studies. Some studies found that younger age was associated with higher levels of depressive symptoms (Kronenberg et al., 2010; McDermott & Palmer, 2002), while other studies found that older age was associated with higher levels of depressive symptoms (Bokszczanin, 2002; Liu et al., 2011; Thienkrua et al., 2006).
Table 2.
Aim Two: Correlates of Depressive Symptoms
Specific associations between gender and depressive symptoms were examined in 18 articles (Table 2). The majority of these studies (k=11; 61% of these articles) found that female gender was associated with higher levels of depression (Aber et al., 2004; Bokszczanin, 2002; Fan et al., 2011; Gershoff et al., 2010; Giannopoulou et al., 2006; Goenjian et al., 2011; Hardin et al., 1994; Kronenberg et al., 2010; Roussos et al., 2005; Warheit et al., 1996; Weems et al., 2007). However, two studies found the converse, that male gender was associated with higher levels of depressive symptoms (Ekşi et al., 2007; Kolaitis et al., 2003), and four studies found no association between gender and depressive symptoms (Kar & Bastia, 2006; Lai et al., 2013; McDermott & Palmer, 1999; Tang et al., 2010). Finally, one study found an interaction between gender and age in a sample of youth (grades 4–12) assessed six months after the Sutherland Bushfire (McDermott & Palmer, 2002). Younger males reported lower levels of depressive symptoms, but there was no main effect of gender in that study. Overall, it appears that female gender may be a major risk factor for depressive symptoms postdisaster.
Disaster Exposure Stressors
Relationships between a general concept of “exposure” and depressive symptoms were examined in 24 studies (Table 2). Of these articles, 16 found significant associations between exposure and depression symptoms, while 8 studies found no difference in depressive symptom levels between those exposed to a disaster and those not exposed.
Across studies, several specific exposure stressors were examined in relationship to depressive symptoms: being injured (Ekşi et al., 2007; Jia et al., 2010), witnessing the disaster (Fan et al., 2011), losing a family member or loved one (Ekşi et al., 2007; Fan et al., 2011; Goenjian et al., 2009; Jia et al., 2010), knowing someone who was hurt or ill (Goenjian et al., 2011; Jia et al., 2010), perceived life threat (i.e., fear during the earthquake; C. Kilic, Kilic, & Aydin, 2011; McDermott & Palmer, 2002; Thienkrua et al., 2006), and loss/disruption (Kolaitis et al., 2003; Lai et al., 2013; Shahar et al., 2009).
In addition, other significant life events or stressors, not necessarily related to disasters, emerged as risk factors for depression. Significant relationships to depression have been reported for the following risk factors: community violence (Salloum et al., 2011), life stressors (Fan et al., 2011; Kronenberg et al., 2010; Roussos et al., 2005; Salloum et al., 2011; Warheit et al., 1996; Wickrama & Kaspar, 2007), adversity (Giannopoulou et al., 2006), and restricted travel after a disaster (Comer et al., 2010).
PTS symptoms
Overall, 20 studies directly examined PTS symptoms as a factor associated with youth depressive symptoms postdisaster (Table 2). All of these studies reported significant, positive associations between PTS and depressive symptoms. For example, Goenjian and colleagues (1995) assessed youth with varying levels of exposure to the Spitak Earthquake. When youth were assessed 1½ years after the earthquake, PTS and depressive symptoms were correlated at r=.55. Similarly, PTS and depressive symptoms were correlated at r=.54 in a sample of youth assessed four months after the Asian Tsunami (Wickrama & Kaspar, 2007).
Aim Three: Theories Utilized in Disaster Research
Most studies contained stated aims (k=57; Table 1). Some aims were broad. For example, one study aimed “[t]o determine prevalence and correlates of probable mental disorders among New York City, public school students 6 months following the September 11, 2011, World Trade Center attack” (Hoven et al., 2005). Other aims were more specific. One study aimed “to investigate the effects of parental psychopathology on the traumatic stress and depression of earthquake survivor-children 4 years after the earthquake” (Kilic et al., 2011).
Table 1.
Synthesis of study characteristics.
| Characteristic | k (%) | |
|---|---|---|
| All Studies (k = 72) | ||
| Note that these characteristics are not mutually exclusive. | Aim | 57 (79%) |
| Hypotheses | 22 (31%) | |
| Explicitly Stated Theory | 21 (29%) | |
| Included Aims, Hypotheses and Theory | 10 (14%) | |
|
| ||
| Natural Disaster Studies (k = 51) | ||
| Earthquake | 26 (51%) | |
| Hurricane | 13 (25%) | |
| Tsunami | 7 (14%) | |
| Flood | 3 (6%) | |
| Bushfire/Wildfire | 2 (4%) | |
|
| ||
| Man-Made Disaster Studies (k = 21) | ||
| Terrorism | 9 (43%) | |
| Boat Disaster | 3 (14%) | |
| Nuclear Waste Disaster | 3 (14%) | |
| Sniper Attack/Shooting | 1 (5%) | |
| Other Explosion | 5 (24%) | |
Hypotheses about depressive symptoms were explicitly stated in less than one-third of the studies examined (k=22). As an example of stated hypotheses, Salloum and colleagues (2011) “hypothesized that…exposure to Hurricane Gustav…will be associated with increased symptoms of PTSD and depression.”
Theories were examined in less than one-third of studies (k=21; see Tables 1 and 3). Sixteen different theories were described (Table 3). Two theories were derived directly from general depression theories (e.g., appraisal theories, reduced response-contingent theories, attribution theory); ten distinct theories were framed in the disaster and traumatic stressor literature (e.g., a developmental approach to disasters; trajectories of distress; stress models of disasters, stress vulnerability hypothesis; disaster contextual ecological model; conversation of resources; secondary depression; dose exposure models; a model by Hardin et al., 1994; a model by La Greca et al., 1996). Finally, four theories fell into an “other” category, and covered biological models of allostatic load, developmental models (i.e., Bronfenbrenner model), and stressor models (e.g., social support stress buffering, Skinner hierarchical coping). Overall, 10 studies (14%) included aims, hypotheses, and an explicit theory.
Table 3.
Aim Three: Theories Utilized in Disaster Research
| Article Type | Articles |
|---|---|
| General Depression Theories (k = 2) | Grant et al., 1997; Jeney-Gammon et al., 1993 |
| Disaster and Trauma Theories (k = 15) | Bokszczanin, 2002; Comer, 2010; Felix et al., 2011; Goenjian et al., 1995, 2001; Hardin et al., 1994; Karabekiroglu et al., 2008; Kilic et al., 2003; Kronenberg et al., 2010; Lai et al., 2013; McDermott & Palmer, 2002; Warheit et al., 1996; Weems et al., 2007; Whalen et al., 2004; Yule et al., 1990 |
| Other Theories (k = 4) | Fernando et al., 2010; Salloum et al., 2011; Shahar et al., 2009; Wang et al., 2010 |
Discussion
This study is the first to systematically document the burden of depression among disaster-exposed youth. Disasters are associated with elevated rates of depression among youth. Prevalence rates in this review ranged from 2% to 69% (Boer et al., 2009; Papadatos et al., 1990). Prevalence rates for depression among youth in the general population range from 1% to 9% (Costello, Erkanli, & Angold, 2006; Horowitz & Garber, 2006). However, it is clear that there is wide variability in reported prevalence rates of youth postdisaster depression. This variability may be partly due to differences in disasters, methodology, or due to challenges associated with conducting research after disasters (Bonanno, Brewin, Kaniasty, & La Greca, 2010). Nevertheless, this review establishes the importance of assessing depressive symptoms as part of children’s potentially broad range of reactions to disasters. This is not currently common practice among postdisaster studies of youth. For example, 159 of the original 353 articles identified in this review did not include a measure of depression.
Regarding risk factors, no single profile of youth at risk for developing depressive symptoms emerged. This may indicate that we have not identified the best predictors of depressive symptoms, or it may indicate that many risk factors lead to postdisaster depressive symptoms. Wide variability of depression prevalence rates observed in this review may provide additional evidence that many factors influence the development of youth postdisaster depressive symptoms.
When we examined child characteristics, findings were mixed. In line with hypotheses, there was a body of evidence that female gender is a risk factor for depressive symptoms postdisaster. At the same time, we expected older age to be a risk factor for depressive symptoms in this study. However, some studies found associations between younger age and depressive symptoms, while other studies reported that older age was a risk factor for depressive symptoms. Although findings for child characteristics were mixed, child characteristics have been found to have small to medium effect sizes in relationship to PTS symptoms after disasters (Trickey et al., 2012). It may be an important area to continue to assess in order to determine how postdisaster interventions might be targeted towards different age and gender groups.
Regarding stressors, disaster exposure was a risk factor for depressive symptoms in many, but not all of the studies reviewed. Also, several nonspecific exposure stressors (non-disaster related) were identified as risk factors for depressive symptoms. Finally, PTS symptoms were a risk factor for depressive symptoms. Based on information from this study, clinical interventions might consider including a focus on helping children cope with stressors after disasters. This is not currently common practice (Comer et al., 2010). Interventions might also consider assessing and targeting comorbid symptoms, as PTS symptoms emerged as a risk factor for depressive symptoms.
This review is the first to identify current theories being utilized to understand youth depressive symptoms postdisaster. No unifying theory emerged from the studies that were synthesized. Thus, the etiology of youth postdisaster depression remains unclear. A variety of theories were examined across articles, and theories were predominantly adapted from the disaster and traumatic stress literature. In contrast, only two studies utilized general depression theories. However, no studies tested competing theories within the same article. Thus, it remains an important question in the field as to whether postdisaster depressive symptoms are unique from or similar to general depressive symptoms. Future studies that test disaster/trauma theories against depression theories are needed in order to elucidate this question. However, given that numerous studies have found a significant association between youth PTS and depressive symptoms postdisaster, it is likely that disaster/trauma theories best explain the presence of postdisaster depressive symptoms in youth. Further, a unifying theory for child reactions to disasters will need to incorporate the multiple risk factors this review identified as associated with depressive symptoms: child characteristics, exposure stressors, and broad psychological symptoms (e.g., PTS). The role of environmental factors (e.g., social support) will also need to be considered.
Several limitations should be considered when evaluating this paper. First, causality is difficult to determine in the relationship between risk factors and depressive symptoms. Many studies in this review were cross-sectional, and few studies contained pre- and post-disaster ratings of depressive symptoms. This is common in the disaster literature, due to the unpredictable nature of all disasters. However, this limited our ability to draw conclusions about the timing of risk factors and depressive symptoms. Although risk factors may contribute to depressive symptoms, it is also possible that depressive symptoms may increase the presence of some stressors such as non-disaster related stressors (e.g., loss of friends). Second, study selection decisions may have influenced findings. For example, in this study we excluded studies that included highly specialized, treatment seeking populations. Thus, we may have identified depressive symptoms with a more limited range and variability than exists in the larger population of youth exposed to disasters. It is also possible that we failed to identify articles that are germane to this systematic review, either through articles falling after our inclusion date of May, 2013 (e.g., Weems et al., 2013), or through articles being overlooked. This would affect findings by failing to include pertinent information. Finally, findings were limited by heterogeneity in disaster research designs, and this likely contributed to variability in our findings. For example, not all of the studies reviewed in this article reported prevalence rates of depression, limiting our ability to comment on prevalence rates across all studies. Further, studies examined various risk factors for depressive symptoms postdisaster, limiting comparisons across studies.
To move the disaster research field forward, researchers might consider using established batteries of assessments to enable comparisons across studies and build consensus. At a minimum, studies should include a measure of depressive symptoms. Further, it would be helpful if studies utilized similar measures of depressive symptoms. This would allow direct comparisons of means and variability between samples.
In summary, this review has yielded key findings regarding youth postdisaster depression. This review highlights that any unifying theory of child reactions to disasters will need to include depressive symptoms. However, should this theory be built from a depression theory or from a postdisaster theory? Based on this review, this remains an open question. No studies jointly tested these types of theories against each other. This type of testing is needed to guide theory. For example, researchers from fields of depression and disasters should consider collaborating on investigations. Depression cognitive appraisal theorists (e.g., Grant et al., 1997) could assess youth negative appraisals, while postdisaster depression theorists who focus on disaster and recovery stressors (e.g., Felix et al., 2011) would assess stressors. If these factors were studied jointly, relative contributions of these factors in predicting youth postdisaster depression could be assessed and form the bases of theory testing. A second open question in creating a unifying theory of child reactions to disasters is whether depression arises as a symptom secondary to PTS in youth after disasters, or whether depression develops independently of PTS symptoms. This review suggests that depression may arise as a symptom secondary to PTS symptoms after disasters. However, more longitudinal studies are needed that assess youth PTS and depression at multiple timepoints close to a disaster, in order to better understand the etiology and timing of youth distress.
Acknowledgments
Source of Funding: Research time for the preparation of this manuscript was supported by the National Institute of Child Health and Human Development (NICHD; T32 HD07510).
We thank Constance Ogokeh, Brooke Beaulieu, and Victoria Novinger for their administrative assistance with this article.
References
*Articles marked with an asterisk were reviewed in this systematic review.
- *.Aber JL, Gershoff ET, Ware A, Kotler JA. Estimating the effects of September 11th and other forms of violence on the mental health and social development of New York City’s youth: A matter of context. Applied Developmental Science. 2004;8(3):111–129. doi: 10.1207/s1532480xads0803_2. [DOI] [Google Scholar]
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96(2):358. [Google Scholar]
- Alisic E, Jongmans MJ, van Wesel F, Kleber RJ. Building child trauma theory from longitudinal studies: A meta-analysis. Clinical Psychology Review. 2011;31(5):736–747. doi: 10.1016/j.cpr.2011.03.001. [DOI] [PubMed] [Google Scholar]
- *.Asarnow J, Glynn S, Pynoos RS, Nahum J, Guthrie D, Cantwell DP, Franklin B. When the earth stops shaking: Earthquake sequelae among children diagnosed for pre-earthquake psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(8):1016–1023. doi: 10.1097/00004583-199908000-00018. [DOI] [PubMed] [Google Scholar]
- Bal A. Post-traumatic stress disorder in Turkish child and adolescent survivors three years after the Marmara earthquake. Child and Adolescent Mental Health. 2008;13(3):134–139. doi: 10.1111/j.1475-3588.2007.00469.x. [DOI] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy: Past, present, and future. Journal of Consulting and Clinical Psychology. 1993;61(2):194. doi: 10.1037//0022-006x.61.2.194. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, Nelson B. Childhood and adolescent depression: A review of the past 10 years. Part I. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(11):1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- *.Boer F, Smit C, Morren M, Roorda J, Yzermans J. Impact of a technological disaster on young children: A five-year postdisaster multiinformant study. Journal of Traumatic Stress. 2009;22(6):516–524. doi: 10.1002/jts.20461. [DOI] [PubMed] [Google Scholar]
- *.Bokszczanin A. Long-term negative psychological effects of a flood on adolescents. Polish Psychological Bulletin. 2002;33(1):55–61. [Google Scholar]
- *.Bolton D, O’Ryan D, Udwin O, Boyle S, Yule W. The long-term psychological effects of a disaster experienced in adolescence: II: General psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000;41(4):513–523. doi: 10.1111/1469-7610.00636. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Brewin CR, Kaniasty K, La Greca AM. Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest. 2010;11(1):1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- *.Breton JJ, Valla JP, Lambert J. Industrial disaster and mental health of children and their parents. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32(2):438–445. doi: 10.1097/00004583-199303000-00028. [DOI] [PubMed] [Google Scholar]
- *.Bromet EJ, Goldgaber D, Carlson G, Panina N, Golovakha E, Gluzman SF, Schwartz JE. Children’s well-being 11 years after the chornobyl catastrophe. Archives of General Psychiatry. 2000;57(6):563–571. doi: 10.1001/archpsyc.57.6.563. [DOI] [PubMed] [Google Scholar]
- *.Brown EJ, Goodman RF. Childhood traumatic grief: An exploration of the construct in children bereaved on September 11. Journal of Clinical Child and Adolescent Psychology. 2005;34(2):248. doi: 10.1207/s15374424jccp3402_4. [DOI] [PubMed] [Google Scholar]
- *.Catani C, Jacob N, Schauer E, Kohila M, Neuner F. Family violence, war, and natural disasters: A study of the effect of extreme stress on children’s mental health in Sri Lanka. BMC Psychiatry. 2008;8(1):33. doi: 10.1186/1471-244x-8-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole DA, Peeke LG, Martin JM, Truglio R, Seroczynski AD. A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of Consulting and Clinical Psychology. 1998;66(3):451–460. doi: 10.1037//0022-006x.66.3.451. [DOI] [PubMed] [Google Scholar]
- *.Comer JS, Fan B, Duarte CS, Wu P, Musa GJ, Mandell DJ, Hoven CW. Attack-related life disruption and child psychopathology in New York City public schoolchildren 6-months post-9/11. Journal of Clinical Child and Adolescent Psychology. 2010;39(4):460–469. doi: 10.1080/15374416.2010.486314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello JE, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? Journal of Child Psychology and Psychiatry. 2006;47(12):1263–1271. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- *.Dirkzwager AJE, Kerssens JJ, Yzermans CJ. Health problems in children and adolescents before and after a man-made disaster. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(1):94–103. doi: 10.1097/01.chi.0000186402.05465.f7. [DOI] [PubMed] [Google Scholar]
- Dyb G, Jensen TK, Nygaard E. Children’s and parents’ posttraumatic stress reactions after the 2004 tsunami. Clinical Child Psychology and Psychiatry. 2011;16(4):621–634. doi: 10.1177/1359104510391048. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38(4):319–345. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- *.Ekşi A, Braun KL, Ertem-Vehid H, Peykerli G, Saydam R, Toparlak D, Alyanak B. Risk factors for the development of PTSD and depression among child and adolescent victims following a 7.4 magnitude earthquake. International Journal of Psychiatry in Clinical Practice. 2007;11(3):190–199. doi: 10.1080/13651500601017548. [DOI] [PubMed] [Google Scholar]
- *.Eksi A, Braun KL. Over-time changes in PTSD and depression among children surviving the 1999 Istanbul earthquake. European Child & Adolescent Psychiatry. 2009;18(6):384–391. doi: 10.1007/s00787-009-0745-9. [DOI] [PubMed] [Google Scholar]
- *.Fan F, Zhang Y, Yang Y, Mo L, Liu X. Symptoms of posttraumatic stress disorder, depression, and anxiety among adolescents following the 2008 Wenchuan earthquake in China. Journal of Traumatic Stress. 2011;24(1):44–53. doi: 10.1002/jts.20599. [DOI] [PubMed] [Google Scholar]
- *.Felix E, Hernandez LA, Bravo M, Ramirez R, Cabiya J, Canino G. Natural disaster and risk of psychiatric disorders in Puerto Rican children. Journal of Abnormal Child Psychology. 2011;39(4):589–600. doi: 10.1007/s10802-010-9483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Fernando GA, Miller KE, Berger DE. Growing pains: the impact of disaster-related and daily stressors on the psychological and psychosocial functioning of youth in Sri Lanka. Child Development. 2010;81(4):1192–1210. doi: 10.1111/j.1467-8624.2010.01462.x. [DOI] [PubMed] [Google Scholar]
- *.Foa EB, Johnson KM, Feeny NC, Treadwell KRH. The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology. 2001;30(3):376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Furr JM, Comer JS, Edmunds JM, Kendall PC. Disasters and youth: A meta-analytic examination of posttraumatic stress. Journal of Consulting and Clinical Psychology. 2010;78(6):765–780. doi: 10.1037/a0021482. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiologic Reviews. 2005;27(1):78–91. doi: 10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- *.Gershoff ET, Aber JL, Ware A, Kotler JA. Exposure to 9/11 among youth and their mothers in New York City: Enduring associations with mental health and sociopolitical attitudes. Child Development. 2010;81(4):1142–1160. doi: 10.1111/j.1467-8624.2010.01459.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Giannopoulou I, Strouthos M, Smith P, Dikaiakou A, Galanopoulou V, Yule W. Post-traumatic stress reactions of children and adolescents exposed to the Athens 1999 earthquake. European Psychiatry. 2006;21(3):160–166. doi: 10.1016/j.eurpsy.2005.09.005. [DOI] [PubMed] [Google Scholar]
- *.Goenjian AK, Molina L, Steinberg AM, Fairbanks LA, Alvarez ML, Goenjian HA, Pynoos RS. Posttraumatic stress and depressive reactions among Nicaraguan adolescents after hurricane Mitch. American Journal of Psychiatry. 2001;158(5):788–794. doi: 10.1176/appi.ajp.158.5.788. [DOI] [PubMed] [Google Scholar]
- *.Goenjian AK, Pynoos RS, Steinberg AM, Najarian LM, Asarnow JR, Karayan I, Fairbanks LA. Psychiatric comorbidity in children after the 1988 earthquake in Armenia. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(9):1174–1184. doi: 10.1097/00004583-199509000-00015. [DOI] [PubMed] [Google Scholar]
- *.Goenjian AK, Roussos A, Steinberg AM, Sotiropoulou C, Walling D, Kakaki M, Karagianni S. Longitudinal study of PTSD, depression, and quality of life among adolescents after the Parnitha earthquake. Journal of Affective Disorders. 2011;133(3):509–515. doi: 10.1016/j.jad.2011.04.053. [DOI] [PubMed] [Google Scholar]
- *.Goenjian AK, Walling D, Steinberg AM, Roussos A, Goenjian HA, Pynoos RS. Depression and PTSD symptoms among bereaved adolescents 6(1/2) years after the 1988 Spitak earthquake. Journal of Affective Disorders. 2009;112(1–3):81–84. doi: 10.1016/j.jad.2008.04.006. [DOI] [PubMed] [Google Scholar]
- *.Goenjian AK, Yehuda R, Pynoos RS, Steinberg AM, Tashjian M, Yang RK, Fairbanks LA. Basal cortisol, dexamethasone suppression of cortisol, and MHPG in adolescents after the 1988 earthquake in Armenia. The American Journal of Psychiatry. 1996;153(7):929–934. doi: 10.1176/ajp.153.7.929. [DOI] [PubMed] [Google Scholar]
- *.Grant SM, Hardin SB, Pesut DJ, Hardin T. Psychological evaluations, referrals, and follow-up of adolescents after their exposure to Hurricane Hugo. Journal of Child and Adolescent Psychiatric Nursing. 1997;10(1):7–16. doi: 10.1111/j.1744-6171.1997.tb00207.x. [DOI] [PubMed] [Google Scholar]
- Guha-Sapir D, Vos F, Below R, Ponserre S. Annual disaster statistical review 2011. The numbers and trends. 2012 from www.emdat.be.
- *.Hardin SB, Weinrich M, Weinrich S, Hardin TL, Garrison C. Psychological distress of adolescents exposed to Hurricane Hugo. Journal of Traumatic Stress. 1994;7(3):427–440. doi: 10.1007/BF02102787. [DOI] [PubMed] [Google Scholar]
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74(3):401. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- *.Hoven CW, Duarte CS, Lucas CP, Wu P, Mandell DJ, Goodwin RD, Bin F. Psychopathology among New York City public school children 6 months after September 11. Archives of General Psychiatry. 2005;62(5):545–551. doi: 10.1001/archpsyc.62.5.545. [DOI] [PubMed] [Google Scholar]
- *.Hsu CC, Chong MY, Yang P, Yen CF. Posttraumatic stress disorder among adolescent earthquake victims in Taiwan. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(7):875–881. doi: 10.1097/00004583-200207000-00022. [DOI] [PubMed] [Google Scholar]
- Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review. 2008;115(2):291. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- Jacobs RH, Reinecke MA, Gollan JK, Kane P. Empirical evidence of cognitive vulnerability for depression among children and adolescents: A cognitive science and developmental perspective. Clinical Psychology Review. 2008;28(5):759–782. doi: 10.1016/j.cpr.2007.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Jeney-Gammon P, Daugherty TK, Finch AJ, Jr, Belter RW, Foster KY. Children’s coping styles and report of depressive symptoms following a natural disaster. The Journal of Genetic Psychology. 1993;154(2):259–267. doi: 10.1080/00221325.1993.9914739. [DOI] [PubMed] [Google Scholar]
- *.Jia Z, Tian W, He X, Liu W, Jin C, Ding H. Mental health and quality of life survey among child survivors of the 2008 Sichuan earthquake. Quality of Life Research. 2010;19(9):1381–1391. doi: 10.1007/s11136-010-9703-8. [DOI] [PubMed] [Google Scholar]
- *.Joseph SA, Brewin CR, Yule W, Williams R. Causal attributions and post-traumatic stress in adolescents. Journal of Child Psychology and Psychiatry. 1993;34(2):247–253. doi: 10.1111/j.1469-7610.1993.tb00982.x. [DOI] [PubMed] [Google Scholar]
- *.Kar N, Bastia BK. Post-traumatic stress disorder, depression and generalised anxiety disorder in adolescents after a natural disaster: A study of comorbidity. Clinical Practice and Epidemiology in Mental Health: CP & EMH. 2006;2:17–17. doi: 10.1186/1745-0179-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kar N, Mohapatra PK, Nayak KC, Pattanaik P, Swain SP, Kar HC. Post-traumatic stress disorder in children and adolescents one year after a super-cyclone in Orissa, India: Exploring cross-cultural validity and vulnerability factors. BMC Psychiatry. 2007;7(1):8. doi: 10.1186/1471-244X-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Karabekiroglu K, Akbas S, Tasdemir GN, Karakurt MN. Post-traumatic stress symptoms in adolescents after two murders in a school: A controlled follow-up study. International Journal of Psychiatry in Medicine. 2008;38(4):407–424. doi: 10.2190/PM.38.4.b. [DOI] [PubMed] [Google Scholar]
- *.Karakaya I, Agaoglu B, Coskun A, Sismanlar SG, Memik NC, Yildizoc O. Post-traumatic stress reaction symptoms among Turkish students: Assessments one and six months after a terrorist attack in Istanbul. Hong Kong Journal of Psychiatry. 2006;16(2):65–70. [Google Scholar]
- *.Kilic C, Kilic EZ, Aydin IO. Effect of relocation and parental psychopathology on earthquake survivor-children’s mental health. The Journal of Nervous and Mental Disease. 2011;199(5):335–341. doi: 10.1097/NMD.0b013e3182174ffa. [DOI] [PubMed] [Google Scholar]
- *.Kilic EZ, Ozguven HD, Sayil I. The psychological effects of parental mental health on children experiencing disaster: The experience of Bolu earthquake in Turkey. Family Process. 2003;42(4):485–495. doi: 10.1111/j.1545-5300.2003.00485.x. [DOI] [PubMed] [Google Scholar]
- *.Kolaitis G, Kotsopoulos J, Tsiantis J, Haritaki S, Rigizou F, Zacharaki L, Katerelos P. Posttraumatic stress reactions among children following the Athens earthquake of September 1999. European Child and Adolescent Psychiatry. 2003;12(6):273–280. doi: 10.1007/s00787-003-0339-x. [DOI] [PubMed] [Google Scholar]
- *.Korol M, Green BL, Gleser GC. Children’s responses to a nuclear waste disaster: PTSD symptoms and outcome prediction. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(4):368. doi: 10.1097/00004583-199904000-00008. [DOI] [PubMed] [Google Scholar]
- *.Kronenberg ME, Hansel TC, Brennan AM, Osofsky HJ, Osofsky JD, Lawrason B. Children of Katrina: Lessons learned about postdisaster symptoms and recovery patterns. Child Development. 2010;81(4):1241–1259. doi: 10.1111/j.1467-8624.2010.01465.x. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Lai BS, Llabre MM, Silverman WK, Vernberg EM, Prinstein MJ. Children’s postdisaster trajectories of PTS symptoms: Predicting chronic distress. Child & Youth Care Forum. 2013;42(4):351–369. doi: 10.1007/s10566-013-9206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Lai BS, Jaccard J. Hurricane-related exposure experiences and stressors, other life events, and social support: Concurrent and prospective impact on children’s persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Psychology. 2010;78(6):794–805. doi: 10.1037/a0020775. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Vernberg EM, Prinstein MJ. Symptoms of posttraumatic stress in children after hurricane Andrew: A prospective study. Journal of Consulting and Clinical Psychology. 1996;64(4):712–723. doi: 10.1037/0022-006X.64.4.712. [DOI] [PubMed] [Google Scholar]
- *.Lai BS, La Greca AM, Auslander BA, Short MB. Children’s symptoms of posttraumatic stress and depression after a natural disaster: Comorbidity and risk factors. Journal of Affective Disorders. 2013;146(1):71–78. doi: 10.1016/j.jad.2012.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Lau JTF, Yu X, Zhang J, Mak WWS, Choi KC, Lui WWS, Chan EYY. Psychological Distress among Adolescents in Chengdu, Sichuan at 1 Month after the 2008 Sichuan Earthquake. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2010;87(3):504–523. doi: 10.1007/s11524-010-9447-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Lengua LJ, Long AC, Smith KI, Meltzoff AN. Pre-attack symptomatology and temperament as predictors of children’s responses to the September 11 terrorist attacks. Journal of Child Psychology and Psychiatry. 2005;46(6):631–645. doi: 10.1111/j.1469-7610.2004.00378.x. [DOI] [PubMed] [Google Scholar]
- *.Liu M, Li W, Zhanbiao S, Zhen Z, Kan Z, Jianhua S. Mental health problems among children one-year after Sichuan earthquake in China: A follow-up study. PloS One. 2011;6(2):1–6. doi: 10.1371/journal.pone.0014706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.March JS, Amaya-Jackson L, Terry R, Costanzo P. Posttraumatic symptomatology in children and adolescents after an industrial fire. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(8):1080–1088. doi: 10.1097/00004583-199708000-00015. [DOI] [PubMed] [Google Scholar]
- *.McDermott BM, Palmer LJ. Post-disaster service provision following proactive identification of children with emotional distress and depression. Australian and New Zealand Journal of Psychiatry. 1999;33(6):855–863. doi: 10.1046/j.1440-1614.1999.00611.x. [DOI] [PubMed] [Google Scholar]
- *.McDermott BM, Palmer LJ. Postdisaster emotional distress, depression and event-related variables: Findings across child and adolescent developmental stages. Australian and New Zealand Journal of Psychiatry. 2002;36(6):754–761. doi: 10.1046/j.1440-1614.2002.01090.x. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- *.Najarian LM, Goenjian AK, Pelcovttz D, Mandel F, Najarian B. Relocation after a disaster: Posttraumatic stress disorder in Armenia after the earthquake. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(3):374–383. doi: 10.1097/00004583-199603000-00020. [DOI] [PubMed] [Google Scholar]
- *.Papadatos Y, Nikou K, Potamianos G. Evaluation of psychiatric morbidity following an earthquake. International Journal of Social Psychiatry. 1990;36(2):131–136. doi: 10.1177/002076409003600206. [DOI] [PubMed] [Google Scholar]
- *.Pina AA, Villalta IK, Ortiz CD, Gottschall AC, Costa NM, Weems CF. Social support, discrimination, and coping as predictors of posttraumatic stress reactions in youth survivors of Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology. 2008;37(3):564–574. doi: 10.1080/15374410802148228. [DOI] [PubMed] [Google Scholar]
- *.Piyasil V, Ketuman P, Plubrukarn R, Jotipanut V, Tanprasert S, Aowjinda S, Thaeeromanophap S. Post traumatic stress disorder in children after tsunami disaster in Thailand: 2 years follow-up. Journal of the Medical Association of Thailand. 2007;90(11):2370–2376. [PubMed] [Google Scholar]
- *.Piyasil V, Ketumarn P, Prubrukarn R, Pacharakaew S, Dumrongphol H, Rungsri S, Chatchavalitsakul W. Psychiatric disorders in children at one year after the tsunami disaster in Thailand. Journal of the Medical Association of Thailand. 2008;91(Suppl 3):S15–20. [PubMed] [Google Scholar]
- *.Piyavhatkul N, Pairojkul S, Suphakunpinyo C. Psychiatric disorders in tsunami-affected children in Ranong Province, Thailand. Medical Principles and Practice: International Journal of the Kuwait University. 2008;17(4):290–295. doi: 10.1159/000129608. [DOI] [PubMed] [Google Scholar]
- *.Roussos A, Goenjian AK, Steinberg AM, Sotiropoulou C, Kakaki M, Kabakos C, Manouras V. Posttraumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia, Greece. American Journal of Psychiatry. 2005;162(3):530–537. doi: 10.1176/appi.ajp.162.3.530. [DOI] [PubMed] [Google Scholar]
- *.Sahin NH, Batigun AD, Yilmaz B. Psychological symptoms of Turkish children and adolescents after the 1999 earthquake: Exposure, gender, location, and time duration. Journal of Traumatic Stress. 2007;20(3):335–345. doi: 10.1002/jts.20217. [DOI] [PubMed] [Google Scholar]
- *.Salloum A, Carter P, Burch B, Garfinkel A, Overstreet S. Impact of exposure to community violence, Hurricane Katrina, and Hurricane Gustav on posttraumatic stress and depressive symptoms among school age children. Anxiety Stress Coping. 2011;24(1):27–42. doi: 10.1080/10615801003703193. [DOI] [PubMed] [Google Scholar]
- *.Scheeringa MS, Zeanah CH. Reconsideration of harm’s way: Onsets and comorbidity patterns of disorders in preschool children and their caregivers following Hurricane Katrina. Journal of Clinical Child & Adolescent Psychology. 2008;37(3):508–518. doi: 10.1080/15374410802148178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seballos F, Tanner T, Tarazona M, Gallegos J. Children and disasters: Understanding impact and enabling agency. Brighton: Institute of Development Studies; 2011. p. 12. [Google Scholar]
- *.Shahar G, Cohen G, Grogan KE, Barile JP, Henrich CC. Terrorism-related perceived stress, adolescent depression, and social support from friends. Pediatrics. 2009;124(2):e235–e240. doi: 10.1542/peds.2008-2971. [DOI] [PubMed] [Google Scholar]
- *.Tang TC, Yen CF, Cheng CP, Yang P, Chen CS, Yang RC, Yu HS. Suicide risk and its correlate in adolescents who experienced typhoon-induced mudslides: A structural equation model. Depression and Anxiety. 2010;27(12):1143–1148. doi: 10.1002/da.20748. [DOI] [PubMed] [Google Scholar]
- *.Telles S, Singh N, Joshi M. Risk of posttraumatic stress disorder and depression in survivors of the floods in Bihar, India. Indian Journal of Medical Sciences. 2009;63(8):330–334. doi: 10.4103/0019-5359.55883. [DOI] [PubMed] [Google Scholar]
- *.Thienkrua W, Lopes Cardozo B, Chakkraband MLS, Guadamuz TE, Pengjuntr W, Tantipiwatanaskul P, van Griensven F. Symptoms of posttraumatic stress disorder and depression among children in tsunami-affected areas in southern Thailand. Journal of the American Medical Association. 2006;296(5):549–559. doi: 10.1001/jama.296.5.549. [DOI] [PubMed] [Google Scholar]
- Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review. 2012;32(2):122–138. doi: 10.1016/j.cpr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- *.Vehid HE, Alyanak B, Eksi A. Suicide ideation after the 1999 earthquake in Marmara, Turkey. The Tohoku Journal of Experimental Medicine. 2006;208(1):19–24. doi: 10.1620/tjem.208.19. [DOI] [PubMed] [Google Scholar]
- *.Vila G, Porche LM, Mouren-Simeoni MC. An 18-month longitudinal study of posttraumatic disorders in children who were taken hostage in their school. Psychosomatic Medicine. 1999;61(6):746–754. doi: 10.1097/00006842-199911000-00005. [DOI] [PubMed] [Google Scholar]
- *.Vila G, Witkowski P, Tondini M, Perez-Diaz F, Mouren-Simeoni M, Jouvent R. A study of posttraumatic disorders in children who experienced an industrial disaster in the Briey region. European Child & Adolescent Psychiatry. 2001;10(1):10. doi: 10.1007/s007870170042. [DOI] [PubMed] [Google Scholar]
- Vogel JM, Vernberg EM. Part 1: Children’s psychological responses to disasters. Journal of Clinical Child Psychology. 1993;22(4):464–484. [Google Scholar]
- Wang HH, Zhang ZJ, Tan QR, Yin H, Chen YC, Wang HN, Li LJ. Psychopathological, biological, and neuroimaging characterization of posttraumatic stress disorder in survivors of a severe coalmining disaster in China. Journal of Psychiatric Research. 2010;44(6):385–392. doi: 10.1016/j.jpsychires.2009.10.001. [DOI] [PubMed] [Google Scholar]
- *.Wang L, Long D, Li Z, Armour C. Posttraumatic stress disorder symptom structure in Chinese adolescents exposed to a deadly earthquake. Journal of Abnormal Child Psychology. 2011;39(5):749–758. doi: 10.1007/s10802-011-9508-4. [DOI] [PubMed] [Google Scholar]
- *.Warheit GJ, Zimmerman RS, Khoury EL, Vega WA, Gil AG. Disaster related stresses, depressive signs and symptoms, and suicidal ideation among a multi-racial/ethnic sample of adolescents: A longitudinal analysis. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 1996;37(4):435–444. doi: 10.1111/j.1469-7610.1996.tb01424.x. [DOI] [PubMed] [Google Scholar]
- *.Weems CF, Pina A, Costa N, Watts S, Taylor L, Cannon M. Predisaster trait anxiety and negative affect predict posttraumatic stress in youths after Hurricane Katrina. Journal of Consulting and Clinical Psychology. 2007;75(1):154–159. doi: 10.1037/0022-006X.75.1.154. [DOI] [PubMed] [Google Scholar]
- Weems CF, Scott BG, Taylor LK, Cannon MF, Romano DM, Perry AM. A theoretical model of continuity in anxiety and links to academic achievement in disaster exposed school children. Development and Psychopathology. 2013;25:729–738. doi: 10.1017/S0954579413000138. [DOI] [PubMed] [Google Scholar]
- *.Whalen CK, Henker B, King PS, Jamner LD, Levine L. Adolescents react to the events of September 11, 2001: Focused versus ambient impact. Journal of Abnormal Child Psychology. 2004;32(1):1–11. doi: 10.1023/B:JACP.0000007576.94501.a0. [DOI] [PubMed] [Google Scholar]
- *.Wickrama KAS, Kaspar V. Family context of mental health risk in Tsunami-exposed adolescents: Findings from a pilot study in Sri Lanka. Social Science and Medicine. 2007;64(3):713–723. doi: 10.1016/j.socscimed.2006.09.031. [DOI] [PubMed] [Google Scholar]
- Yelland C, Robinson P, Lock C, La Greca AM, Kokegei B, Ridgway V, Lai BS. Bushfire impact on youth. Journal of Traumatic Stress. 2010;23(2):274–277. doi: 10.1002/jts.20521. [DOI] [PubMed] [Google Scholar]
- *.Yule W, Udwin O, Murdoch K. The ‘Jupiter’ sinking: Effects on children’s fears, depression and anxiety. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 1990;31(7):1051–1061. doi: 10.1111/j.1469-7610.1990.tb00845.x. [DOI] [PubMed] [Google Scholar]
- *.Zhang Y, Kong F, Wang L, Chen H, Gao X, Tan X, Liu Y. Mental health and coping styles of children and adolescent survivors one year after the 2008 Chinese earthquake. Children and Youth Services Review. 2010;32(10):1403–1409. doi: 10.1016/j.childyouth.2010.06.009. [DOI] [Google Scholar]
- *.Ziaaddini H, Nakhaee N, Behzadi K. Prevalence and correlates of PTSD among high school students after the earthquake disaster in the city of Bam, Iran. American Journal of Applied Sciences. 2009;6(1):130–132. [Google Scholar]