Abstract
Background
Anterior odontoid screw fixation (AOSF) has been one of the most popular treatments for odontoid fractures. However, the true efficacy of AOSF remains unclear. In this study, we aimed to provide the pooled rates of non-union, reoperation, infection, and approach related complications after AOSF for odontoid fractures.
Methods
We searched studies that discussed complications after AOSF for type II or type III odontoid fractures. A proportion meta-analysis was done and potential sources of heterogeneity were explored by meta-regression analysis.
Results
Of 972 references initially identified, 63 were eligible for inclusion. 54 studies provided data regarding non-union. The pooled non-union rate was 10% (95% CI: 7%–3%). 48 citations provided re-operation information with a pooled proportion of 5% (95% CI: 3%–7%). Infection was described in 20 studies with an overall rate of 0.2% (95% CI: 0%–1.2%). The main approach related complication is postoperative dysphagia with a pooled rate of 10% (95% CI: 4%–17%). Proportions for the other approach related complications such as postoperative hoarseness (1.2%, 95% CI: 0%–3.7%), esophageal/retropharyngeal injury (0%, 95% CI: 0%–1.1%), wound hematomas (0.2%, 95% CI: 0%–1.8%), and spinal cord injury (0%, 95% CI: 0%–0.2%) were very low. Significant heterogeneities were detected when we combined the rates of non-union, re-operation, and dysphagia. Multivariate meta-regression analysis showed that old age was significantly predictive of non-union. Subgroup comparisons showed significant higher non-union rates in age ≥70 than that in age ≤40 and in age 40 to <50. Meta-regression analysis did not reveal any examined variables influencing the re-operation rate. Meta-regression analysis showed age had a significant effect on the dysphagia rate.
Conclusions/Significances
This study summarized the rates of non-union, reoperation, infection, and approach related complications after AOSF for odontoid factures. Elderly patients were more likely to experience non-union and dysphagia.
Introduction
Odontoid fractures account for 10%–15% of all cervical spine fractures [1]. Despite of the frequency of odontoid fractures, its management remains controversial and ranges from conservative treatment to surgical intervention [2]–[7]. Conservative treatment consists of skull traction, cervical collar, brace, and halo vest. However, such methods are unpopular for unstable odontoid fractures (type II and shallow type III based on the classification of Anderson and D'lonzo [8]) because of the high non-union rate [2], [3]. Moreover, they are often poorly tolerated in the elderly and in the multiply injured patients [6]. Posterior C1–C2 fusion has been advocated as it significantly increases the fusion rate [9], [10]. Nevertheless, this technique is associated with extensive surgical exposure, autogenous bone harvest, and compromise of the cervical movement [2]–[6]. Anterior odontoid screw fixation (AOSF) has been one of the surgical treatments for unstable odontoid fractures since it was independently introduced by Bohler and Nakanishi [11], [12]. This technique seems an ideal treatment as it preserves C1–C2 movement and obviates bone graft harvest.
To date, many clinical studies have evaluated the effectiveness of AOSF for odontoid fractures [12]–[77]. Nevertheless, clinicians may be confused about the true efficacy of this technique because of the wide variability of these reports. Previous reviews were mostly narrative or were investigations that did not weight the results of the single studies according to the number of participants [2], [4]–[6]. Therefore, it is important to combine the results from different studies for clinical reference. In this study, we aimed to provide pooled rates of non-union, re-operation, infection, and approach related complications after surgical treatment of unstable odontoid fractures using AOSF. Furthermore, we tried to explore potential factors that affected these outcomes.
Materials and Methods
Search strategy and inclusion criteria
A computerized systematic search was conducted up to August 2013 using MEDLINE database. We screened all fields by the term “odontoid fracture” or “odontoid screw” or “odontoid fixation”. Articles were limited to those published in English. We also searched the reference lists and relevant journals by hand. This meta-analysis was performed in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (when appropriate) (Checklist S1).
We included studies which were carried out on humans. The studies that discussed fusion results, and/or re-operations, and/or infections, and/or approach related complications after odontoid screw fixation for type II or type III odontoid fractures were selected. We also required a minimum sample size of five to ensure quality and comparability of data. Biomechanical studies, cadaveric studies, animal studies, case report, duplications, and review articles were excluded. Clinical studies with inadequate information or incomplete data were also excluded. We carefully reviewed the department/institute of each potential eligible study to screen whether there were any papers from the same surgical team. For papers that had overlapping patients determined through the overlapping research time, we only included the paper with the largest sample size for analysis.
Data extraction
Two investigators reviewed all identified articles to determine if an individual study was eligible for inclusion. Data from each study was extracted using a standardized form. Disagreements on eligibility and data between reviewers were resolved by consensus with the third reviewer. Studies were categorized into levels of evidence according to those published in the Journal of Bone and Joint Surgery (American) [78].
Data extracted consisted of study year, country, level of evidence, patients' mean age, sex proportion, mean follow-up duration, classification of the odontoid fracture, number of patients, number of non-unions, number of re-operations, number of infections, and number of approach related complications. Fusion status should be assessed according to radiological (static or dynamic) and/or computed tomography (CT) examinations. Because the fusion criteria might be different among the included studies, we used a universal definition of fusion for data extraction. Criteria for fusion success included formation of trabecular and cortex bony bridges through the fracture site, absence of sclerotic borders adjacent to the fracture site, and absence of movement of the fracture site confirmed on radiographs and/or CT scan. Radiolucent cleft, clear fracture line, fibrous union, or any movement at the fracture site were considered as non-union. Re-operation represented secondary surgical intervention for any reason after odontoid screw fixation. Infections indicated only those located at the surgical site including both superficial and deep ones. We extracted data on five types of approach related complications including postoperative dysphagia, postoperative hoarseness, esophageal /retropharyngeal injury, wound hematomas, and spinal cord injury. In this meta-analysis, data regarding the study characteristics and the outcomes of interest were extracted based on the average value of each study. For studies with overlapping patients, only the one with the largest sample size was entered into meta-analysis.
Statistical analysis
Meta-analyses were performed to pool the rates of non-union, re-operation, infection, and approach related complications. A Freeman-Tukey Double arcsine transformation was implemented to calculate the overall proportion. A test of heterogeneity was carried out, and cut-off p value of 0.1 was established as a threshold of homogeneity. Pooled estimates and 95% confidence intervals (CIs) were summarized by forest plots. Fixed-effect models were applied unless statistical heterogeneity was significant, in which case random-effect models were used. We further investigated potential sources of heterogeneity by arranging groups of studies according to relevant characteristics (year of publication, level of evidence, patients' mean age, sex, follow-up duration, fracture type, and study sample size) and by meta-regression analysis. Factors were examined both individually and in multiple-variable models. To avoid model instability, only factors that showed significant effects individually were enrolled into a multiple regression model. Publication bias was assessed using Egger test. All analyses were done in the statistical software R 3.0.1.
Results
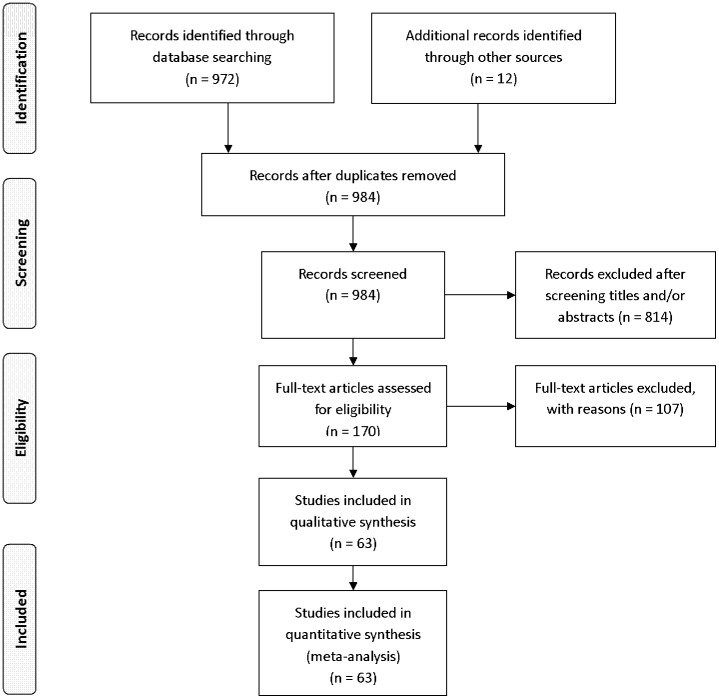
In the initial screening, 972 potential studies were selected according to the search strategy. Hand-searching resulted in 12 additional papers. After reviewing titles and abstracts, 814 papers were found to be unrelated to the current topic. Of the remaining 170 papers, the full texts were read and 104 publications which did not meet eligibility criteria were excluded. Further three papers [71], [73], [76] were excluded due to potential overlapping patients. Consequently, sixty three papers met all inclusion criteria and were selected (Figure 1) [12]–[70], [72], [74], [75], [77]. Based on the level of evidence, there were 1 level II, 17 level III, and 45 level IV studies. The mean age ranged from 35 to 85.4 years. We divided the studies into five age subgroups (age ≤40, age 40 to <50, age 50 to <60, age 60 to <70, and age ≥70). The male to female ratio was 1.74. The follow-up duration ranged from 1.5 months to 9 years. 88.9% of the injuries were type II dens fractures according to Anderson and D'Alonzo's classification [8]. The characteristics of selected studies were summarized in Table S1 and Table S2.
Figure 1. Selection of relevant publications, reasons for exclusion.
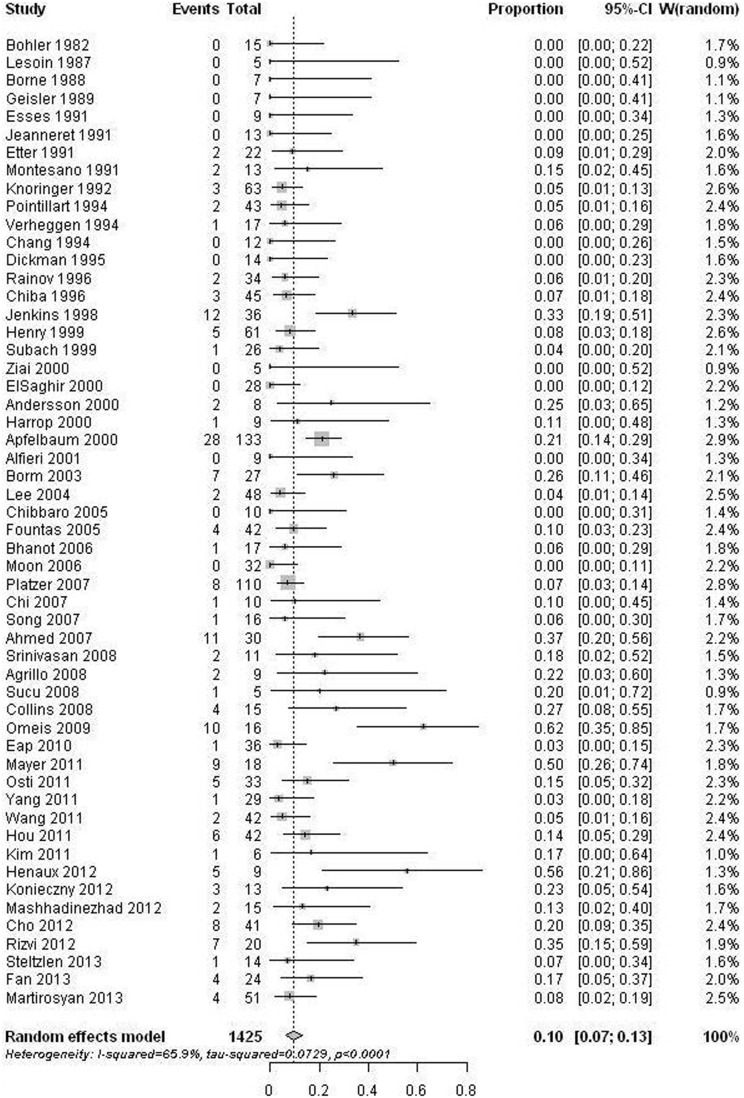
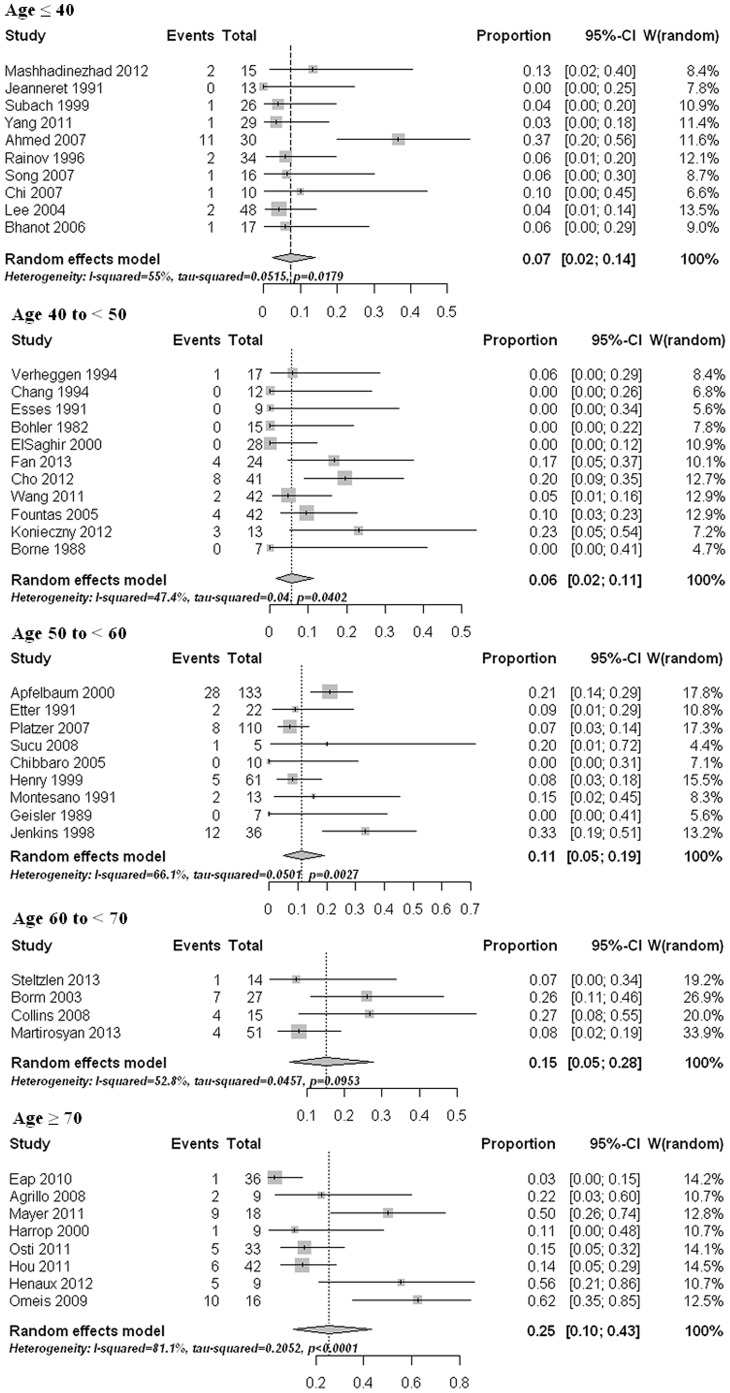
54 studies [12]–[20], [22]–[29], [31]–[51], [53]–[60], [62], [63], [65]–[70] that reported fusion results were pooled. Six studies [21], [52], [61], [72], [74], [75] were excluded from data synthesizing because of potential patients overlapping. Imaging methods used for fusion assessment included radiograph (static and/or dynamic) and CT scan. Radiograph was used in fifty two studies. CT scan was used in twenty six papers. Twenty five studies used both methods. In selected studies, a total of 1425 patients were evaluated. The non-union rates ranged from 0% to 62%. The pooled estimate for all studies was 10% (95% CI: 7%–13%). However, the estimate was associated with substantial heterogeneity (p<0.001) (Figure 2). We observed that the pooled non-union rate based on CT scan (12%, 95% CI: 7%–17%) was higher than that based on only X-rays (8%, 95% CI: 4%–13%). Nevertheless, the difference was statistically insignificant (p = 0.234) after univariate meta-regression analysis. Therefore, we combine both image modalities into one database. Univariate meta-regression analysis showed that old age (p = 0.002), less than one year follow-up (p = 0.017), and publication after 2000 (p = 0.012) were significantly predictive of non-union. The non-union rate increased with age, as estimates in the five age groups were 7%, 6%, 11%, 15%, and 25%, respectively (Figure 3). Subgroup comparisons showed that the non-union rate in age ≥70 was significant higher than that in age ≤40 (p = 0.015) and in age 40 to <50 (p = 0.015). After multivariate meta-regression analysis, only age (p = 0.016) remained significant. No significant publication bias was detected (p = 0.699).
Figure 2. Forest plots showing the non-union rates (boxes) with 95% confidence of intervals (CIs; bars).
Figure 3. Forest plots showing the non-union rates (boxes) with 95% confidence of intervals (CIs; bars) in different age groups.
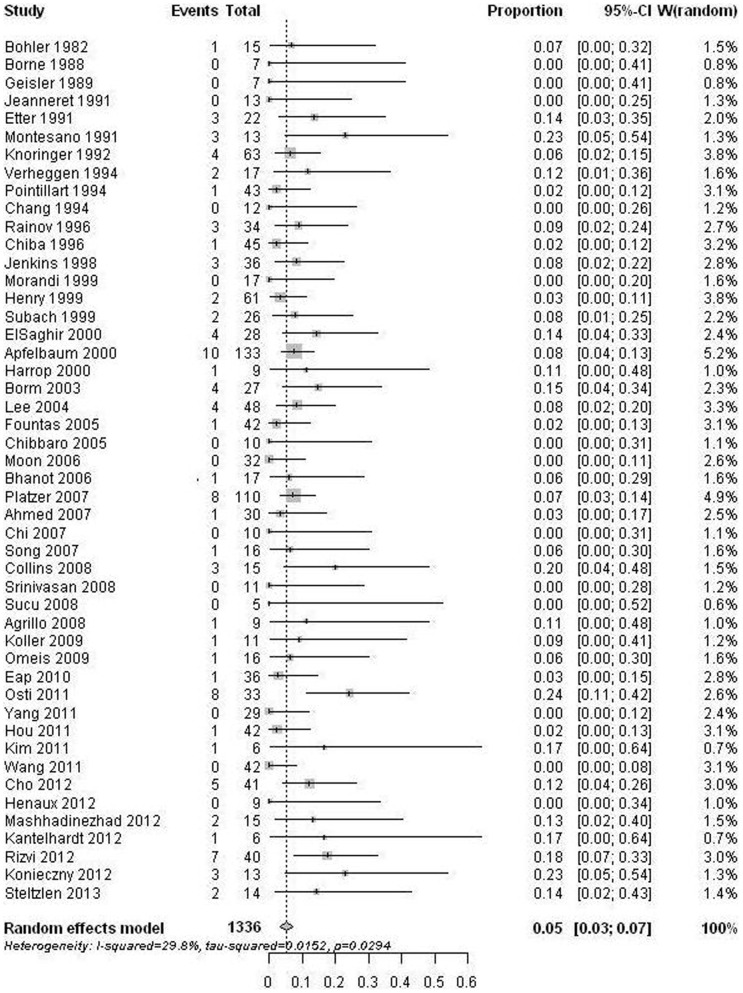
48 citations [12], [14], [15], [17]–[20], [22]–[24], [26]–[31], [33]–[35], [38]–[56], [58]–[60], [62]–[67], [69] provided re-operation information following odontoid screw fixation. Reasons for re-operation included screw loosening/pullout/cut-out/mal-position, fracture re-dislocation, unstable non-union, hematoma, and so on. The re-operation rates ranged from 0% to 24%. The random-effect pooled proportion was 5% (95% CI: 3%–7%) with pronounced heterogeneity (p = 0.029) (Figure 4). Meta-regression analysis revealed that none of the examined variables (year of publication, age, gender, follow-up duration, fracture type, or sample size) significantly influenced the re-operation rate. Egger test for publication bias showed no significant evidence for bias (p = 0.343).
Figure 4. Forest plots showing the re-operation rates (boxes) with 95% confidence of intervals (CIs; bars).
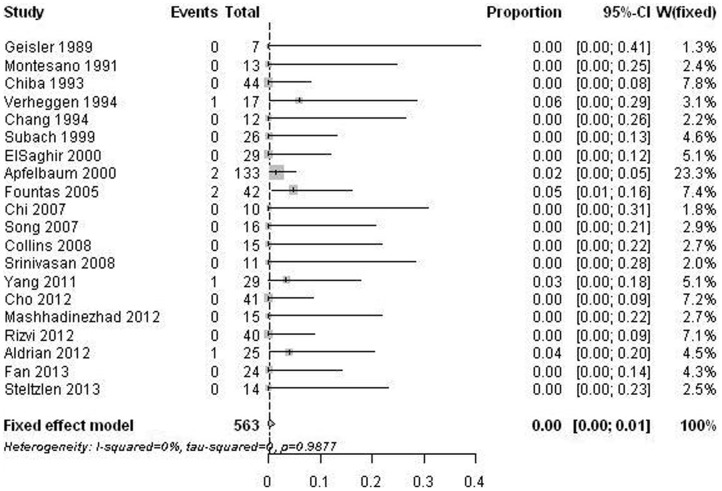
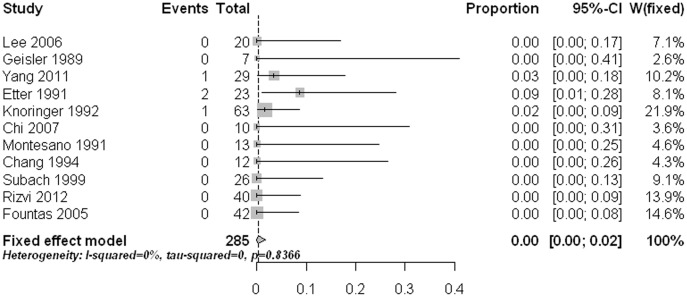
Surgical site infection was assessed in 20 studies [15], [19], [21], [22], [24], [31], [33], [34], [41], [45], [47], [49], [50], [60]–[62], [66], [67], [69], [70] with 563 surgeries. The reported infection rate was low, with estimates varied from 0% to 6%. The overall infection rate of all included studies was 0.2% (95% CI: 0%–1.2%) (Figure 5). As there was no substantial significant heterogeneity, further meta-regression analysis was not carried out. There was no significant publication bias (p = 0.549).
Figure 5. Forest plots showing the infection rates (boxes) with 95% confidence of intervals (CIs; bars).
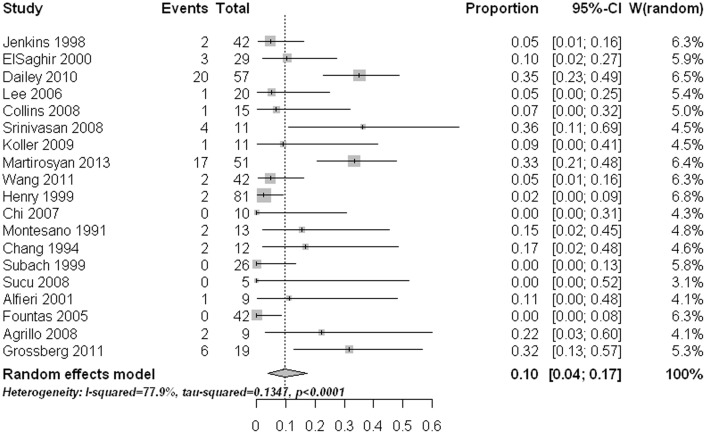
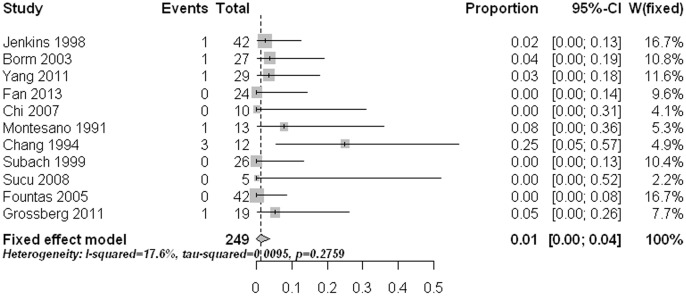
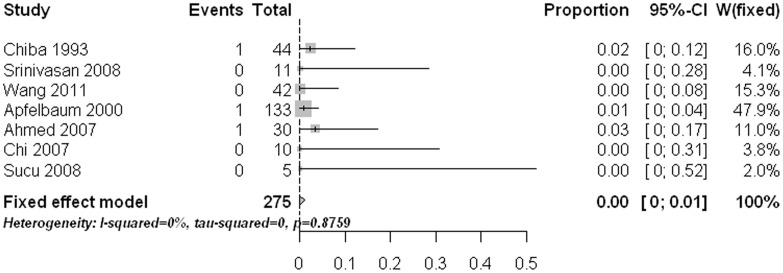
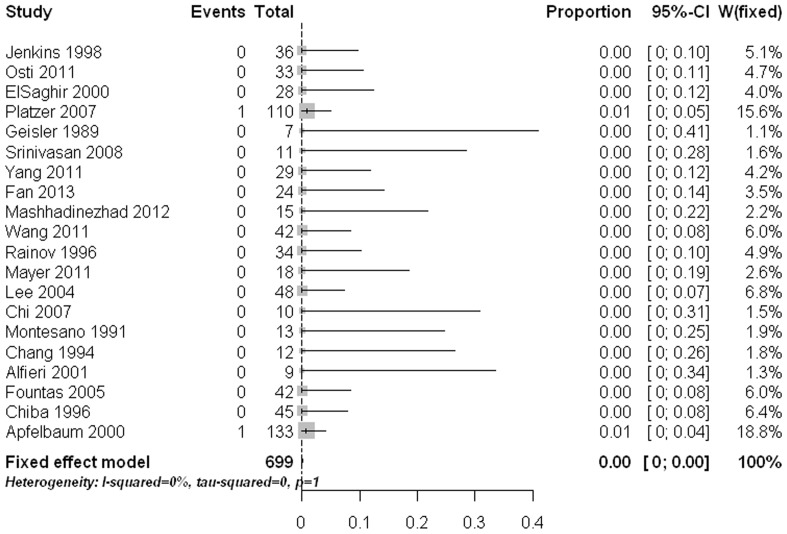
The main approach related complication was postoperative dysphagia. The pooled rate was 10% (95% CI: 4%–17%) with statistically significant heterogeneity (Figure 6). Meta-regression analysis revealed that age had a significant effect on the estimate (p<0.0001). Subgroup comparisons indicated that the two old age groups (age 60 to <70 yrs and age ≥70 yrs) had significant higher dysphagia rates than those in the other three age groups (age ≤40, age 40 to <50, and age 50 to <60) (p<0.05). Pooled proportions for the other approach related complications like postoperative hoarseness (1.2%, 95% CI: 0%–3.7%) (Figure 7), esophageal /retropharyngeal injury (0%, 95% CI: 0%–1.1%) (Figure 8), wound hematomas (0.2%, 95% CI: 0%–1.8%) (Figure 9), and spinal cord injury (0%, 95% CI: 0%–0.2%) (Figure 10) were very low. No significant publication bias was detected (p>0.1)
Figure 6. Forest plots showing the rates of dysphagia (boxes) with 95% confidence of intervals (CIs; bars).
Figure 7. Forest plots showing the rates of hoarseness (boxes) with 95% confidence of intervals (CIs; bars).
Figure 8. Forest plots showing the rates of esophageal /retropharyngeal injury (boxes) with 95% confidence of intervals (CIs; bars).
Figure 9. Forest plots showing the rates of wound hematomas (boxes) with 95% confidence of intervals (CIs; bars).
Figure 10. Forest plots showing the rates of spinal cord injury (boxes) with 95% confidence of intervals (CIs; bars).
Discussion
We conducted this study to provide a better understanding of the frequency of non-union, infection, re-operation, and approach related complications after anterior screw fixation for type II and type III odontoid fractures. Non-union can be one of the most important outcomes, because it may lead to spinal cord injury due to atlantoaxial instability. Pooled analysis from our study showed that the non-union rate after AOSF was 10%. It seemed that the fusion rate of AOSF (90%) was better than that of the conservative treatment (60%–80%) [3], and was comparable to that of the posterior fixation (89%–100%) [5]. Therefore, AOSF might be a good choice for type II and type III odontoid fractures in selected patients. This study revealed that the re-operation rate was 5% after AOSF. The reasons for re-operation included non-union, screw failure, fracture re-dislocation, and occasionally hematoma. Since non-union accounted for fifty percent of the cases undergoing re-operation, obtaining bony fusion becomes the first priority in AOSF. Not all of the non-unions underwent second surgical interventions, because some of them (fibrous unions) were radiologically stable. For these cases, long term follow up was still essential. The infection rate in surgical site was very low with only seven cases identified during our review [24], [33], [41], [60], [61]. The pooled estimate was 0.2% without significant heterogeneity among the studies. All infection cases were superficial and were resolved without sequelae.
Our study revealed that age had a significant impact on the non-union rate. The non-union rate in patients younger than 50 years was 6%. Therefore, AOSF seems to be a good choice for young patients. Although the non-union rate reached 11% to 25% in patients aged 50 years or older, this rate was still acceptable as the non-union rate of conservative treatment for the elderly patients was very high (60% in Nourbakhsh' review [3], and 56%–72% in Huybregts' review [7]). Subgroup comparisons showed that age ≥70 had a significant higher non-union rate than the young had. Our findings were consistent with those reported by Platzer et al [46]. They observed that patients older than 65 years had a significantly higher non-union rate of 12% compared with that of 4% in younger individuals [46]. However, two other observational studies reported that age was not associated with fusion failure [38], [62]. It was generally agreed that old patients had a higher chance to experience osteoporosis and diminished bone quality which might have an important effect on the fusion outcome. As none of the studies directly assessed osteoporosis of surgical patients, the bone quality information in different age groups was not clear. This could be one reason to explain the controversial results from different studies. Therefore, it is important for further studies to clarify the relationships among age, osteoporosis, and fusion outcomes after AOSF. Since elderly patients were more likely to experience non-unions, measures should be adopted to enhance the bony fusion in this population. Dailey et al [75] retrospectively analyzed the efficacy of AOSF in a group of patients with age over 70. They observed a significantly higher stabilization rate of 96% in patients when 2 screws were placed, compared with that of 56% in patients with only one screw used. However, in another group of relatively young patients, the difference became statistically insignificant [28]. Younger patients have better bone quality which could provide more stability at the surgical site. Thus, placing one screw may be sufficient. Nevertheless, the elderly patients might benefit from an additional screw which added rotational stability in the osteopenic bone [75].
Postoperative dysphagia was the main approach related complication after AOSF with pooled estimate of 10%, followed by postoperative hoarseness (1.2%). Esophageal /retropharyngeal injury, wound hematomas, and spinal cord injury were rare approach related complications. Noteworthy was that age also had a significant effect on postoperative dysphagia rate. Dysphagia is a known complication of anterior cervical spine surgery. A recent systematic review showed that female gender, advanced age, multilevel surgery, longer operating time and severe pre-operative neck pain may increase the risk of postoperative dysphagia after cervical spine surgery [79]. During our review, there was no study directly comparing the dysphagia rates among different age groups. Through this meta-analysis, we observed that age ≥60 had a significant higher dysphagia rate than the age <60 had. The possible reason for this fact was that the elderly patient's esophagus was less tolerant to retraction due to fibrosis [75]. Considering the relatively high dysphagia rate in the elderly after AOSF, strategies, such as using of perioperative methylprednisolone, monitoring of endotracheal tube cuff pressure, and preoperative tracheal/esophageal traction exercise, may be employed to reduce the risk of this complication [79].
There are some limitations existing in this study. First, this meta-analysis only focused on the rates of non-union, re-operation, infection, and approach related complications. We did not pool other outcomes like functional results and patient satisfactory outcome because they were not always reported or were reported in various forms. Even the outcomes we combined were not always available. Second, during the extraction of fusion data, we found the fusion status was assessed using different imaging modalities and non-union was defined according to different standards. Thus, pooling of relevant data might lead to bias even though we had predefined unified criteria for non-union. Third, extensive and significant heterogeneities were detected when we combined the rates of non-union, re-operation, and dysphagia. We had explored the heterogeneity through meta-regression analysis according to several study characteristics, but we only found age had a significant effect on the non-union and dysphagia rate. After subgroup analysis, we still observed heterogeneity in each age group, which meant there were potential other factors influencing the two outcomes. For re-operation, we failed to find potential factors which could explain the heterogeneity. The factors we analyzed represented the average value of each study, which could limit the exploration of the heterogeneity. Moreover, the heterogeneity might also be ascribed to various factors, such as other patient characteristics, fracture subtypes, and surgical techniques used. Lastly, the level of evidence of our analysis is low as none of the enrolled studies were randomized controlled trials. Despite these weaknesses, our study obtains some clinical significance since we pooled estimates based on a relatively large sample. This study provides a quantitative description of the frequencies of non-union, re-operation, infection, and approach related complications after AOSF for odontoid fractures. These data can be helpful in making informed surgical decisions. Further studies may be necessary to pool the functional outcomes of using this technique and to determine the factors affecting the efficacy.
Supporting Information
Characteristics of the studies included for analyzing non-union, re-operation, and infection.
(DOC)
Characteristics of the studies included for analyzing approach related complications.
(DOC)
PRISMA Checklist.
(DOC)
Funding Statement
This work is supported by grants of National Natural Science Foundation of China (No. 81372014) and Natural Science Foundation of Zhejiang Province for Distinguished Young Scholars (No. LR12H06001). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Husby J, Sorensen KH (1974) Fracture of the odontoid process of the axis. Acta Orthop Scand 45: 182–192. [DOI] [PubMed] [Google Scholar]
- 2. Maak TG, Grauer JN (2006) The contemporary treatment of odontoid injuries. Spine (Phila Pa 1976) 31: S53–60 discussion S61. [DOI] [PubMed] [Google Scholar]
- 3. Nourbakhsh A, Shi R, Vannemreddy P, Nanda A (2009) Operative versus nonoperative management of acute odontoid Type II fractures: a meta-analysis. J Neurosurg Spine 11: 651–658. [DOI] [PubMed] [Google Scholar]
- 4. Harrop JS, Hart R, Anderson PA (2010) Optimal treatment for odontoid fractures in the elderly. Spine (Phila Pa 1976) 35: S219–227. [DOI] [PubMed] [Google Scholar]
- 5. Patel AA, Lindsey R, Bessey JT, Chapman J, Rampersaud R (2010) Surgical treatment of unstable type II odontoid fractures in skeletally mature individuals. Spine (Phila Pa 1976) 35: S209–218. [DOI] [PubMed] [Google Scholar]
- 6. Pal D, Sell P, Grevitt M (2011) Type II odontoid fractures in the elderly: an evidence-based narrative review of management. Eur Spine J 20: 195–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huybregts JG, Jacobs WC, Vleggeert-Lankamp CL (2013) The optimal treatment of type II and III odontoid fractures in the elderly: a systematic review. Eur Spine J 22: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Anderson LD, D'Alonzo RT (1974) Fractures of the odontoid process of the axis. J Bone Joint Surg Am 56: 1663–1674. [PubMed] [Google Scholar]
- 9. Brooks AL, Jenkins EB (1978) Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am 60: 279–284. [PubMed] [Google Scholar]
- 10. Grob D, Jeanneret B, Aebi M, Markwalder TM (1991) Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg Br 73: 972–976. [DOI] [PubMed] [Google Scholar]
- 11. Nakanishi T, Sasaki T, Tokita N, Hirabayashi K (1982) Internal fixation for the odontoid fracture. Orthop Trans 6: 176. [Google Scholar]
- 12. Bohler J (1982) Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am 64: 18–27. [PubMed] [Google Scholar]
- 13. Lesoin F, Autricque A, Franz K, Villette L, Jomin M (1987) Transcervical approach and screw fixation for upper cervical spine pathology. Surg Neurol 27: 459–465. [DOI] [PubMed] [Google Scholar]
- 14. Borne GM, Bedou GL, Pinaudeau M, Cristino G, Hussein A (1988) Odontoid process fracture osteosynthesis with a direct screw fixation technique in nine consecutive cases. J Neurosurg 68: 223–226. [DOI] [PubMed] [Google Scholar]
- 15. Geisler FH, Cheng C, Poka A, Brumback RJ (1989) Anterior screw fixation of posteriorly displaced type II odontoid fractures. Neurosurgery 25: 30–37 discussion 37–38. [DOI] [PubMed] [Google Scholar]
- 16. Esses SI, Bednar DA (1991) Screw fixation of odontoid fractures and nonunions. Spine (Phila Pa 1976) 16: S483–485. [DOI] [PubMed] [Google Scholar]
- 17. Etter C, Coscia M, Jaberg H, Aebi M (1991) Direct anterior fixation of dens fractures with a cannulated screw system. Spine (Phila Pa 1976) 16: S25–32. [DOI] [PubMed] [Google Scholar]
- 18. Jeanneret B, Vernet O, Frei S, Magerl F (1991) Atlantoaxial mobility after screw fixation of the odontoid: a computed tomographic study. J Spinal Disord 4: 203–211. [DOI] [PubMed] [Google Scholar]
- 19. Montesano PX, Anderson PA, Schlehr F, Thalgott JS, Lowrey G (1991) Odontoid fractures treated by anterior odontoid screw fixation. Spine (Phila Pa 1976) 16: S33–37. [DOI] [PubMed] [Google Scholar]
- 20.Knöringer P (1992) Internal fixation of dens fractures by double-threaded screws. Orthopedics and Traumatology: 231–245
- 21. Chiba K, Fujimura Y, Toyama Y, Takahata T, Nakanishi T, et al. (1993) Anterior screw fixation for odontoid fracture: clinical results in 45 cases. Eur Spine J 2: 76–81. [DOI] [PubMed] [Google Scholar]
- 22. Chang KW, Liu YW, Cheng PG, Chang L, Suen KL, et al. (1994) One Herbert double-threaded compression screw fixation of displaced type II odontoid fractures. J Spinal Disord 7: 62–69. [DOI] [PubMed] [Google Scholar]
- 23. Pointillart V, Orta AL, Freitas J, Vital JM, Senegas J (1994) Odontoid fractures. Review of 150 cases and practical application for treatment. Eur Spine J 3: 282–285. [DOI] [PubMed] [Google Scholar]
- 24. Verheggen R, Jansen J (1994) Fractures of the odontoid process: analysis of the functional results after surgery. Eur Spine J 3: 146–150. [DOI] [PubMed] [Google Scholar]
- 25. Dickman CA, Foley KT, Sonntag VK, Smith MM (1995) Cannulated screws for odontoid screw fixation and atlantoaxial transarticular screw fixation. Technical note. J Neurosurg 83: 1095–1100. [DOI] [PubMed] [Google Scholar]
- 26. Chiba K, Fujimura Y, Toyama Y, Fujii E, Nakanishi T, et al. (1996) Treatment protocol for fractures of the odontoid process. J Spinal Disord 9: 267–276. [PubMed] [Google Scholar]
- 27. Rainov NG, Heidecke V, Burkert W (1996) Direct anterior fixation of odontoid fractures with a hollow spreading screw system. Acta Neurochir (Wien) 138: 146–153. [DOI] [PubMed] [Google Scholar]
- 28. Jenkins JD, Coric D, Branch CL Jr (1998) A clinical comparison of one- and two-screw odontoid fixation. J Neurosurg 89: 366–370. [DOI] [PubMed] [Google Scholar]
- 29. Henry AD, Bohly J, Grosse A (1999) Fixation of odontoid fractures by an anterior screw. J Bone Joint Surg Br 81: 472–477. [DOI] [PubMed] [Google Scholar]
- 30. Morandi X, Hanna A, Hamlat A, Brassier G (1999) Anterior screw fixation of odontoid fractures. Surg Neurol 51: 236–240. [DOI] [PubMed] [Google Scholar]
- 31. Subach BR, Morone MA, Haid RW Jr, McLaughlin MR, Rodts GR, et al. (1999) Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery 45: 812–819 discussion 819–820. [DOI] [PubMed] [Google Scholar]
- 32. Andersson S, Rodrigues M, Olerud C (2000) Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J 9: 56–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Apfelbaum RI, Lonser RR, Veres R, Casey A (2000) Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg 93: 227–236. [DOI] [PubMed] [Google Scholar]
- 34. ElSaghir H, Bohm H (2000) Anderson type II fracture of the odontoid process: results of anterior screw fixation. J Spinal Disord 13: 527–530 discussion 531. [DOI] [PubMed] [Google Scholar]
- 35. Harrop JS, Przybylski GJ, Vaccaro AR, Yalamanchili K (2000) Efficacy of anterior odontoid screw fixation in elderly patients with Type II odontoid fractures. Neurosurg Focus 8: e6. [PubMed] [Google Scholar]
- 36. Ziai WC, Hurlbert RJ (2000) A six year review of odontoid fractures: the emerging role of surgical intervention. Can J Neurol Sci 27: 297–301. [DOI] [PubMed] [Google Scholar]
- 37. Alfieri A (2001) Single-screw fixation for acute Type II odontoid fracture. J Neurosurg Sci 45: 15–18. [PubMed] [Google Scholar]
- 38. Borm W, Kast E, Richter HP, Mohr K (2003) Anterior screw fixation in type II odontoid fractures: is there a difference in outcome between age groups? Neurosurgery 52: 1089–1092 discussion 1092–1084. [PubMed] [Google Scholar]
- 39. Lee SC, Chen JF, Lee ST (2004) Management of acute odontoid fractures with single anterior screw fixation. J Clin Neurosci 11: 890–895. [DOI] [PubMed] [Google Scholar]
- 40. Chibbaro S, Benvenuti L, Carnesecchi S, Marsella M, Serino D, et al. (2005) The use of virtual fluoroscopy in managing acute type II odontoid fracture with anterior single-screw fixation. A safe, effective, elegant and fast form of treatment. Acta Neurochir (Wien) 147: 735–739 discussion 739. [DOI] [PubMed] [Google Scholar]
- 41. Fountas KN, Machinis TG, Kapsalaki EZ, Dimopoulos VG, Feltes CH, et al. (2005) Surgical treatment of acute type II and rostral type III odontoid fractures managed by anterior screw fixation. South Med J 98: 896–901. [DOI] [PubMed] [Google Scholar]
- 42. Bhanot A, Sawhney G, Kaushal R, Aggarwal AK, Bahadur R (2006) Management of odontoid fractures with anterior screw fixation. J Surg Orthop Adv 15: 38–42. [PubMed] [Google Scholar]
- 43. Moon MS, Moon JL, Sun DH, Moon YW (2006) Treatment of dens fracture in adults: A report of thirty-two cases. Bull Hosp Jt Dis 63: 108–112. [PubMed] [Google Scholar]
- 44.Ahmed N, Loutfy M, Shershera W, Sleem A (2007) Fixation of Type II Odontoid Fractures with Anterior Single Screw. EJNS 22: 137–146 [Google Scholar]
- 45. Chi YL, Wang XY, Xu HZ, Lin Y, Huang QS, et al. (2007) Management of odontoid fractures with percutaneous anterior odontoid screw fixation. Eur Spine J 16: 1157–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Platzer P, Thalhammer G, Ostermann R, Wieland T, Vecsei V, et al. (2007) Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine (Phila Pa 1976) 32: 1714–1720. [DOI] [PubMed] [Google Scholar]
- 47. Song KJ, Lee KB, Kim KN (2007) Treatment of odontoid fractures with single anterior screw fixation. J Clin Neurosci 14: 824–830. [DOI] [PubMed] [Google Scholar]
- 48. Agrillo A, Russo N, Marotta N, Delfini R (2008) Treatment of remote type ii axis fractures in the elderly: feasibility of anterior odontoid screw fixation. Neurosurgery 63: 1145–1150 discussion 1150–1141. [DOI] [PubMed] [Google Scholar]
- 49. Collins I, Min WK (2008) Anterior screw fixation of type II odontoid fractures in the elderly. J Trauma 65: 1083–1087. [DOI] [PubMed] [Google Scholar]
- 50. Srinivasan U, Dhillon C, Mahesha K, Kumar P (2008) Anterior single lag screw fixation in type II Dens fracture—indian experience. Indian Journal of Neurotrauma 5: 87–91. [Google Scholar]
- 51. Sucu HK, Akkol I, Minoglu M, Gelal F (2008) Percutaneous anterior odontoid screw fixation. Minim Invasive Neurosurg 51: 106–108. [DOI] [PubMed] [Google Scholar]
- 52. Koller H, Acosta F, Forstner R, Zenner J, Resch H, et al. (2009) C2-fractures: part II. A morphometrical analysis of computerized atlantoaxial motion, anatomical alignment and related clinical outcomes. Eur Spine J 18: 1135–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Omeis I, Duggal N, Rubano J, Cerabona F, Abrahams J, et al. (2009) Surgical treatment of C2 fractures in the elderly: a multicenter retrospective analysis. J Spinal Disord Tech 22: 91–95. [DOI] [PubMed] [Google Scholar]
- 54. Eap C, Barresi L, Ohl X, Saddiki R, Mensa C, et al. (2010) Odontoid fractures anterior screw fixation: a continuous series of 36 cases. Orthop Traumatol Surg Res 96: 748–752. [DOI] [PubMed] [Google Scholar]
- 55. Hou Y, Yuan W, Wang X (2011) Clinical evaluation of anterior screw fixation for elderly patients with type II odontoid fractures. J Spinal Disord Tech 24: E75–81. [DOI] [PubMed] [Google Scholar]
- 56. Kim SK, Shin JJ, Kim TH, Shin HS, Hwang YS, et al. (2011) Clinical outcomes of halo-vest immobilization and surgical fusion of odontoid fractures. J Korean Neurosurg Soc 50: 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mayer M, Zenner J, Auffarth A, Atzwanger J, Romeder F, et al. (2011) Efficacy of anterior odontoid screw fixation in the elderly patient: a CT-based biometrical analysis of odontoid fractures. Eur Spine J 20: 1441–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Osti M, Philipp H, Meusburger B, Benedetto KP (2011) Analysis of failure following anterior screw fixation of Type II odontoid fractures in geriatric patients. Eur Spine J 20: 1915–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, et al. (2011) Comparison of percutaneous and open anterior screw fixation in the treatment of type II and rostral type III odontoid fractures. Spine (Phila Pa 1976) 36: 1459–1463. [DOI] [PubMed] [Google Scholar]
- 60. Yang YL, Fu BS, Li RW, Smith PN, Mu WD, et al. (2011) Anterior single screw fixation of odontoid fracture with intraoperative Iso-C 3-dimensional imaging. Eur Spine J 20: 1899–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Aldrian S, Erhart J, Schuster R, Wernhart S, Domaszewski F, et al. (2012) Surgical vs nonoperative treatment of Hadley type IIA odontoid fractures. Neurosurgery 70: 676–682 discussion 682–673. [DOI] [PubMed] [Google Scholar]
- 62. Cho DC, Sung JK (2012) Analysis of risk factors associated with fusion failure after anterior odontoid screw fixation. Spine (Phila Pa 1976) 37: 30–34. [DOI] [PubMed] [Google Scholar]
- 63. Henaux PL, Cueff F, Diabira S, Riffaud L, Hamlat A, et al. (2012) Anterior screw fixation of type IIB odontoid fractures in octogenarians. Eur Spine J 21: 335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kantelhardt SR, Keric N, Giese A (2012) Management of C2 fractures using Iso-C(3D) guidance: a single institution's experience. Acta Neurochir (Wien) 154: 1781–1787. [DOI] [PubMed] [Google Scholar]
- 65. Konieczny MR, Gstrein A, Muller EJ (2012) Treatment algorithm for dens fractures: non-halo immobilization, anterior screw fixation, or posterior transarticular C1–C2 fixation. J Bone Joint Surg Am 94: e144 (141–146).. [DOI] [PubMed] [Google Scholar]
- 66. Mashhadinezhad H, Samini F, Mashhadinezhad A, Birjandinejad A (2012) Clinical results of surgical management in type II odontoid fracture: a preliminary report. Turk Neurosurg 22: 583–587. [DOI] [PubMed] [Google Scholar]
- 67. Rizvi SA, Fredo HL, Lied B, Nakstad PH, Ronning P, et al. (2012) Surgical management of acute odontoid fractures: surgery-related complications and long-term outcomes in a consecutive series of 97 patients. J Trauma Acute Care Surg 72: 682–690. [DOI] [PubMed] [Google Scholar]
- 68. Martirosyan NL, Kalb S, Cavalcanti DD, Lochhead RA, Uschold TD, et al. (2013) Comparative Analysis of Isocentric 3-dimensional C-arm Fluoroscopy and Biplanar Fluoroscopy for Anterior Screw Fixation in Odontoid Fractures. J Spinal Disord Tech 26: 189–193. [DOI] [PubMed] [Google Scholar]
- 69.Steltzlen C, Lazennec JY, Catonne Y, Rousseau MA (2013) Unstable odontoid fracture: Surgical strategy in a 22-case series, and literature review. Orthop Traumatol Surg Res. Epub ahead of print. [DOI] [PubMed]
- 70.Fan K, Liao J, Niu C, Chen L, Chen W, et al. (2013) Anterior single-screw fixation in 24 patients with Type II odontoid fractures. Formosa n Journal of Musculosk eletal Disorde rs 4: 26–31 [Google Scholar]
- 71. Fujii E, Kobayashi K, Hirabayashi K (1988) Treatment in fractures of the odontoid process. Spine (Phila Pa 1976) 13: 604–609. [PubMed] [Google Scholar]
- 72. Berlemann U, Schwarzenbach O (1997) Dens fractures in the elderly. Results of anterior screw fixation in 19 elderly patients. Acta Orthop Scand 68: 319–324. [DOI] [PubMed] [Google Scholar]
- 73. Fountas KN, Kapsalaki EZ, Karampelas I, Feltes CH, Dimopoulos VG, et al. (2005) Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral type III odontoid fractures. Spine (Phila Pa 1976) 30: 661–669. [DOI] [PubMed] [Google Scholar]
- 74. Lee SH, Sung JK (2006) Anterior odontoid fixation using a 4.5-mm Herbert screw: The first report of 20 consecutive cases with odontoid fracture. Surg Neurol 66: 361–366 discussion 366. [DOI] [PubMed] [Google Scholar]
- 75. Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI (2010) Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine 12: 1–8. [DOI] [PubMed] [Google Scholar]
- 76. Cho DC, Sung JK (2011) Is All Anterior Oblique Fracture Orientation Really a Contraindication to Anterior Screw Fixation of Type II and Rostral Shallow Type III Odontoid Fractures? J Korean Neurosurg Soc 49: 345–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Grossberg J, Spader H, Belknap T, Oyelese A (2011) The use of the Mayfield Frame facilitates trajectory in anterior odontoid screw fixation. 27th annual meeting of the AANS/CNS section on disorder of the spine and peripheral nerves.
- 78. Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A: 1–3. [PubMed] [Google Scholar]
- 79. Cho SK, Lu Y, Lee DH (2013) Dysphagia following anterior cervical spinal surgery: a systematic review. Bone Joint J 95-B: 868–873. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics of the studies included for analyzing non-union, re-operation, and infection.
(DOC)
Characteristics of the studies included for analyzing approach related complications.
(DOC)
PRISMA Checklist.
(DOC)