Abstract
Background Facial nerve paralysis in a patient with a salivary gland mass usually denotes malignancy. However, facial paralysis can also be caused by benign salivary gland tumors.
Methods We present a case of facial nerve paralysis due to a benign salivary gland tumor that had the imaging characteristics of an intraparotid facial nerve schwannoma.
Results The patient presented to our clinic 4 years after the onset of facial nerve paralysis initially diagnosed as Bell palsy. Computed tomography demonstrated filling and erosion of the stylomastoid foramen with a mass on the facial nerve. Postoperative histopathology showed the presence of a pleomorphic adenoma. Facial paralysis was thought to be caused by extrinsic nerve compression.
Conclusions This case illustrates the difficulty of accurate preoperative diagnosis of a parotid gland mass and reinforces the concept that facial nerve paralysis in the context of salivary gland tumors may not always indicate malignancy.
Keywords: pleomorphic adenoma, facial nerve paralysis, Schwannoma, benign, salivary gland tumor
Introduction
Facial nerve paralysis in a patient with a parotid mass classically suggests a malignant process. The status of the seventh cranial nerve not only is considered a reliable indicator of malignancy but also correlates with the histologic grade and the postoperative prognosis.1 2 Only a few reports in the literature have described facial nerve paralysis due to benign parotid tumors. We report the first case to our knowledge of facial nerve paralysis due to a benign primary parotid tumor with the imaging characteristics of an intraparotid facial nerve schwannoma.
Case Report
A 71-year-old woman was referred to our clinic with a 4-year history of facial nerve paralysis on the left side. Her family first noted lower left facial asymmetry in 2008, and the patient was initially diagnosed with a transient ischemic attack. The facial weakness progressively worsened and eventually resulted in complete paralysis of the left side of the face. At that point, the patient was given a diagnosis of Bell palsy. The patient underwent lower eyelid surgery for ectropion, epiphora, and dry eye. The relevant medical history included previous skin resections for multiple cutaneous malignancies.
On physical examination, grade 5/6 left facial paresis was noted with minimal movement at the oral commissure. The remainder of the neurologic examination was normal. The left eye demonstrated epiphora and mild irritation. No masses of the parotid gland or the neck were detected on palpation, and there was no bulge or displacement of the tonsillar pharyngeal wall. The otologic examination was normal. Audiometry showed bilateral mild to moderately severe downsloping sensorineural hearing loss with excellent discrimination scores. High-resolution computed tomography demonstrated erosion of the stylomastoid foramen on the left side and showed that the stylomastoid foramen on the left side was filled with a mass on the left facial nerve that measured 8 mm in the greatest dimension (Fig. 1). Magnetic resonance imaging confirmed an 8 × 10-mm lesion at the stylomastoid foramen that was enhancing after infusion of contrast material (Fig. 2). These imaging findings were consistent with a possible facial nerve schwannoma. Other disorders to be considered in the differential diagnosis included primary parotid gland tumors, either benign or malignant, perineural spread of cutaneous malignancy, or facial nerve hemangioma. The differential diagnosis is greatly limited considering the long-standing nature of her paralysis, the location of facial nerve enhancement, a normal ear examination, and overall good health.
Fig. 1.
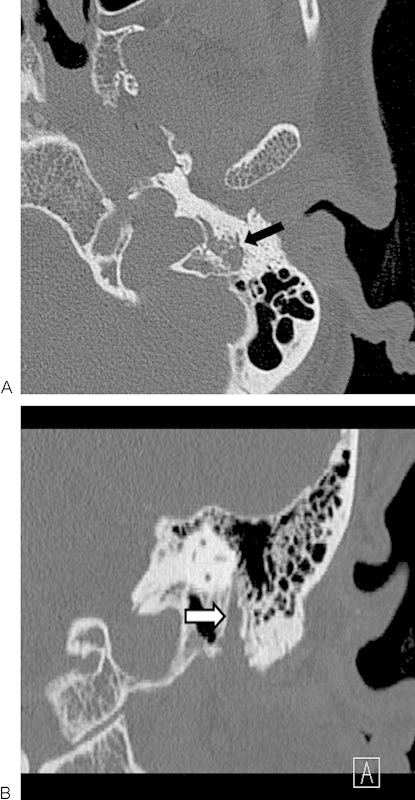
(A) Axial and (B) coronal computed tomographic scans, in bone algorithm, illustrating enlargement and osseous erosion in the region of the stylomastoid foramen (arrows).
Fig. 2.

Axial T1, contrast-enhanced, fat-suppressed magnetic resonance image showing an enhancing mass at the stylomastoid foramen (arrow).
Operative findings included fusiform enlargement of the stylomastoid portion of the facial nerve extending for 13 mm proximally. The vertical portion of the facial nerve was decompressed following a canal-intact mastoidectomy. The facial nerve was followed to the stylomastoid foramen, which was enlarged by the tumor. A superficial parotidectomy was performed, and the affected portion of the facial nerve was included in the specimen. A biopsy of soft tissue surrounding the facial nerve at the stylomastoid foramen was interpreted by the pathologist as suggestive of schwannoma on frozen section analysis. Normal nerve was encountered proximally in the mastoid and at the level of the pes anserinus. Neural reconstruction was performed with a sural nerve cable graft. Final histologic examination revealed encasement of the facial nerve and its arborizing branches by salivary mixed tumor with chondroid and epithelial components compatible with pleomorphic adenoma without any evidence of schwannoma or malignancy (Fig. 3).
Fig. 3.
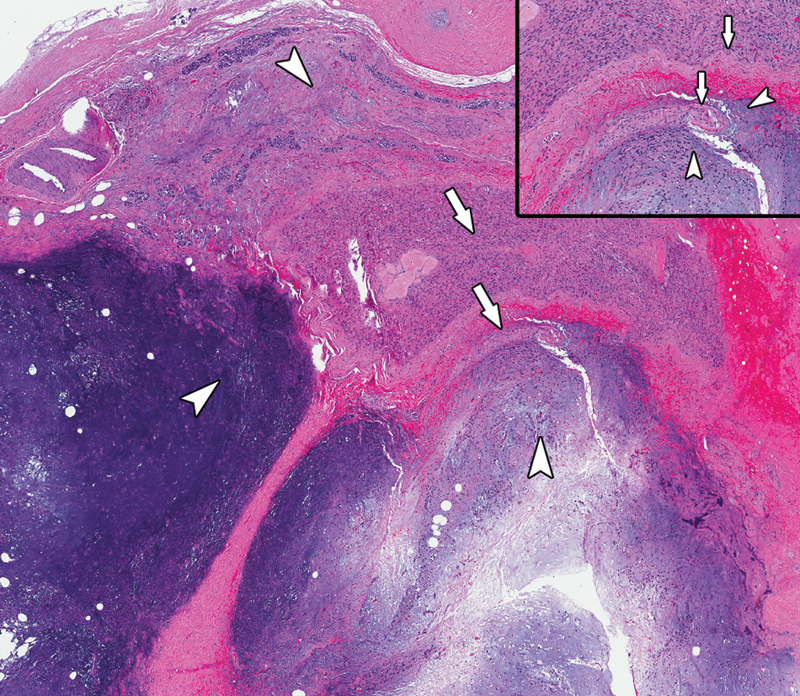
Encasement of large-caliber nerve and arborizing branches (arrows) by salivary mixed tumor with chondroid and epithelial components (arrowheads), consistent with pleomorphic adenoma (hematoxylin-eosin; low-power view). Inset: Small nerve branch embedded in pleomorphic adenoma (hematoxylin-eosin; high-power view).
Discussion
The differential diagnosis of facial paralysis in a patient with a tumor commonly includes primary facial nerve tumor, malignant tumor of the parotid gland or metastatic skin cancer, and glomus jugulare or other temporal bone neoplasm; pleomorphic adenomas are rarely included. In patients with salivary gland tumors, facial nerve paralysis, local invasion, and the presence of metastatic lesions form a triad that classically indicates a malignant process. The presence of facial nerve palsy also seems to be associated with a poorer prognosis. A large multi-institutional study performed by Eneroth et al in 1977 revealed that 14% of patients (145 of 1029) with salivary gland malignancies presented with facial nerve weakness. Patients with facial nerve weakness had a poorer prognosis, with a 5-year survival rate of only 9%.3 In 2011, Wierzbicka et al reported an incidence of facial nerve weakness of 31% of patients (32 of 103) with parotid gland malignancies. In this series, patients with facial nerve weakness had a 3-year disease-free survival rate of 45%, compared with 88% in those without any facial nerve paresis.2
Although strong evidence in the literature supports the association of facial nerve dysfunction with parotid gland malignancy, this clinical finding should not be considered pathognomonic for malignant disease. Although several studies analyzing large series of patients with parotid tumors reported the occurrence of facial palsy only in patients with malignancy,4 5 6 facial palsy due to benign parotid gland tumors has also been reported. A comprehensive review of the literature revealed 17 such cases7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 (Table 1). The present case differs from the ones already discussed in the literature in two aspects. First, it was the smallest benign parotid tumor causing facial nerve palsy with the exception of a 0.5-cm tumor in a 9-year old boy reported by Mamakos et al.10 Second, the present case is the first in which a benign parotid tumor causing facial palsy was initially thought to originate from the facial nerve on the basis of preoperative imaging and frozen-section analysis.
Table 1. Reported cases of facial palsy due to benign parotid tumors.
| Study | Age, y/Sex | Histology | Size, cm | Presumed mechanism |
|---|---|---|---|---|
| Ward and Hendrick7 | 41/F | Pleomorphic adenoma | >10 | Hemorrhage/stretch |
| La Ventura et al8 | 70/F | Pleomorphic adenoma | 2.5 | Stretch |
| Cimorra et al9 | 55/M | Pleomorphic adenoma | 3 | Stretch |
| Mamakos et al10 | 9/M | Pleomorphic adenoma | 0.5 | Temporal bone invasion/compression |
| Papangelou et al11 | 76/M | Oncocytoma | 2.5 | Stretch |
| Lesser and Spector12 | 75/M | Warthin tumor | 5 | Inflammation/stretch |
| Whillis et al13 | 60/F | Warthin tumor | 6 | Inflammation/stretch |
| DeLozier et al14 | 72/F | Warthin tumor | 4 | Inflammation/stretch |
| Blevins et al15 | 59/F 62/M |
Pleomorphic adenoma Pleomorphic adenoma |
3 2 |
Temporal bone invasion/compression Temporal bone invasion/compression |
| Newman et al16 | 70/F | Warthin tumor | 5 | Inflammation |
| Koide et al17 | 79/M | Warthin tumor | 6 | Compression/ischemia |
| Srinivasan et al18 | 62/M | Lipoma | 4 | Unknown |
| Berry et al19 | 82/F | Warthin tumor | Not reported | Unknown |
| Maini and Osborne20 | 72/M | Warthin tumor | 3.5 | Inflammation or ischemia |
| Marioni et al21 | 86/M | Warthin tumor | 6 | Unknown |
| Woodhouse et al22 | 69/M | Warthin tumor | 6 | Compression/ischemia or Bell palsy |
| Present case | 71/F | Pleomorphic adenoma | 1 | Temporal bone invasion/compression |
To our knowledge, the case that we describe here is the first reported case of facial palsy caused by a pleomorphic adenoma that had the imaging characteristics of an intraparotid schwannoma. The diagnosis of schwannoma was suggested by preoperative imaging findings and was initially thought to be confirmed on intraoperative frozen-section analysis. Also, the progression of the facial weakness over a period of 4 years without other signs of malignancy did not suggest a cancerous etiology. However, as demonstrated by this case and discussed by other authors,23 imaging characteristics of intraparotid schwannomas are not specific, and an accurate preoperative diagnosis may be difficult.
In the present case, the preoperative imaging showed a smooth mass centered on the facial nerve with erosion of the stylomastoid foramen with enhancement in the vertical segment of the intratemporal facial nerve, which led us initially to suspect a facial nerve schwannoma rather than a pleomorphic adenoma. On computed tomography, an intraparotid schwannoma can appear as a smooth, circumscribed intraparotid lesion, with possible dilatation of the stylomastoid foramen and fallopian canal in case of intratemporal extension. On gadolinium-enhanced magnetic resonance imaging, intraparotid schwannomas are isointense to hypointense on T1 and isointense to hyperintense on T2, with strong contrast agent uptake.23 However, the imaging patterns of intraparotid schwannomas can be similar to those of other, more common benign parotid tumors, such as pleomorphic adenoma. Indeed, pleomorphic adenomas also present on computed tomography as smooth, well-delineated masses. Nodularity is sometimes found on the outer surface, and larger tumors may be more heterogeneous.24 On magnetic resonance imaging, pleomorphic adenomas present as well-circumscribed masses hypointense on T1, hyperintense on T2, and with heterogeneous enhancement with gadolinium.25
Accurate preoperative diagnosis helps the surgeon determine the optimal therapeutic approach. However, as illustrated by this case, accurate preoperative diagnosis is not always possible. There are differences between the surgical treatment of pleomorphic adenomas and the surgical treatment of intraparotid facial nerve schwannomas. The recurrence rate after gross resection of intraparotid facial nerve schwannomas seems to be negligible if at all existent.23 However, when a pleomorphic adenoma is resected, a cuff of normal tissue must be included to avoid recurrence due to failure to remove the pseudopod-like extensions of tumor.26 27 In the present case, a portion of the facial nerve was resected along with the mass. This decision to resect the facial nerve was facilitated by the long-standing facial nerve paralysis. Negative margins were confirmed, and nerve grafting was performed. Thus the surgical treatment would not have been different even if we had initially suspected a pleomorphic adenoma rather than a facial nerve schwannoma.
This case raises some additional points. The duration of facial paralysis was central to our diagnosis and treatment planning. If this patient had presented with an acute onset of facial weakness and imaging suggesting schwannoma, we would have considered facial nerve decompression. The decision to perform an intraoperative biopsy would then have depended on surgical findings at time of decompression with the decision to sacrifice the nerve and perform nerve grafting predicated on the pathologic findings and the degree of facial weakness. Further, even though an incisional biopsy on a pleomorphic adenoma might have produced tumor spillage, the patient did not receive any postoperative radiation because we reserve this treatment modality for proven multifocal recurrence.
The presented case illustrates that facial palsy is not always an indicator of malignancy. This case also highlights the difficulty of accurate preoperative and even intraoperative diagnosis of salivary gland tumors.
Acknowledgment
We wish to thank Stephanie Deming for her help in the final editorial review of this case report.
References
- 1.Eneroth C M. Facial nerve paralysis. A criterion of malignancy in parotid tumors. Arch Otolaryngol. 1972;95(4):300–304. doi: 10.1001/archotol.1972.00770080494002. [DOI] [PubMed] [Google Scholar]
- 2.Wierzbicka M, Kopeć T, Szyfter W, Kereiakes T, Bem G. The presence of facial nerve weakness on diagnosis of a parotid gland malignant process. Eur Arch Otorhinolaryngol. 2012;269(4):1177–1182. doi: 10.1007/s00405-011-1882-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eneroth C M, Andreasson L, Beran M. et al. Preoperative facial paralysis in malignant parotid tumours. ORL J Otorhinolaryngol Relat Spec. 1977;39(5):272–277. doi: 10.1159/000275367. [DOI] [PubMed] [Google Scholar]
- 4.Frazell E L. Clinical aspects of tumors of the major salivary glands. Cancer. 1954;7(4):637–659. doi: 10.1002/1097-0142(195407)7:4<637::aid-cncr2820070403>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 5.Beahrs O H, Woolner L B, Carveth S W, Devine K D. Surgical management of parotid lesions. Review of seven hundred sixty cases. Arch Surg. 1960;80:890–904. doi: 10.1001/archsurg.1960.01290230008002. [DOI] [PubMed] [Google Scholar]
- 6.Bardwill J M. Tumors of the parotid gland. Am J Surg. 1967;114(4):498–502. doi: 10.1016/0002-9610(67)90005-0. [DOI] [PubMed] [Google Scholar]
- 7.Ward G E, Hendrick J W. Baltimore, MD: Williams & Wilkins; 1950. Tumors of the Head and Neck; pp. 388–389. [Google Scholar]
- 8.LaVenuta F, Flynn W F, Moore J A. Facial nerve paralysis secondary to benign parotid tumor. Arch Otolaryngol. 1969;90(5):603–604. doi: 10.1001/archotol.1969.00770030605014. [DOI] [PubMed] [Google Scholar]
- 9.Cimorra G A, Ferreira V, Martinez-Tello F J. Spontaneous facial nerve paralysis associated with an ipsilateral benign parotid tumor. Case report. Plast Reconstr Surg. 1972;50(5):523–525. doi: 10.1097/00006534-197211000-00025. [DOI] [PubMed] [Google Scholar]
- 10.Mamakos M S, Wright R, Earle A S. Facial palsy in a child with a parotid tumor. Int Surg. 1977;62(9):468–469. [PubMed] [Google Scholar]
- 11.Papangelou L P, Alkalai K, Kyrillopoulou M. Facial nerve paralysis in the presence of a benign parotid tumor. Arch Otolaryngol. 1982;108(7):458–459. [PubMed] [Google Scholar]
- 12.Lesser R W, Spector J G. Facial nerve palsy associated with Warthin's tumor. Arch Otolaryngol. 1985;111(8):548–549. doi: 10.1001/archotol.1985.00800100096016. [DOI] [PubMed] [Google Scholar]
- 13.Whillis D, Goepel J R, Shorthouse A J. Facial paralysis due to a benign parotid tumour. Br J Surg. 1989;76(1):95. doi: 10.1002/bjs.1800760130. [DOI] [PubMed] [Google Scholar]
- 14.DeLozier H L, Spinella M J, Johnson G D. Facial nerve paralysis with benign parotid masses. Ann Otol Rhinol Laryngol. 1989;98(8 Pt 1):644–647. doi: 10.1177/000348948909800815. [DOI] [PubMed] [Google Scholar]
- 15.Blevins N H, Jackler R K, Kaplan M J, Boles R. Facial paralysis due to benign parotid tumors. Arch Otolaryngol Head Neck Surg. 1992;118(4):427–430. doi: 10.1001/archotol.1992.01880040093015. [DOI] [PubMed] [Google Scholar]
- 16.Newman L, Loukota R A, Bradley P F. An infarcted Warthin's tumour presenting with facial weakness. Br J Oral Maxillofac Surg. 1993;31(5):311–312. doi: 10.1016/0266-4356(93)90067-7. [DOI] [PubMed] [Google Scholar]
- 17.Koide C, Imai A, Nagaba A, Takahashi T. Pathological findings of the facial nerve in a case of facial nerve palsy associated with benign parotid tumor. Arch Otolaryngol Head Neck Surg. 1994;120(4):410–412. doi: 10.1001/archotol.1994.01880280038006. [DOI] [PubMed] [Google Scholar]
- 18.Srinivasan V, Ganesan S, Premachandra D J. Lipoma of the parotid gland presenting with facial palsy. J Laryngol Otol. 1996;110(1):93–95. doi: 10.1017/s0022215100132827. [DOI] [PubMed] [Google Scholar]
- 19.Berry M G, Brown A A, Lee P H, Kangesu L. Acute facial-nerve paralysis with parotid adenolymphoma. Br J Plast Surg. 2001;54(5):454–456. doi: 10.1054/bjps.2001.3604. [DOI] [PubMed] [Google Scholar]
- 20.Maini S, Osborne J E. Ischaemic necrosis and facial palsy in Warthin's tumour of the parotid gland. Auris Nasus Larynx. 2002;29(1):99–101. doi: 10.1016/s0385-8146(01)00120-1. [DOI] [PubMed] [Google Scholar]
- 21.Marioni G, de Filippis C, Gaio E, Iaderosa G A, Staffieri A. Facial nerve paralysis secondary to Warthin's tumour of the parotid gland. J Laryngol Otol. 2003;117(6):511–513. doi: 10.1258/002221503321892433. [DOI] [PubMed] [Google Scholar]
- 22.Woodhouse N R, Gok G, Howlett D C, Ramesar K. Warthin's tumour and facial nerve palsy: an unusual association. Br J Oral Maxillofac Surg. 2011;49(3):237–238. doi: 10.1016/j.bjoms.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 23.Gross B C, Carlson M L, Moore E J, Driscoll C L, Olsen K D. The intraparotid facial nerve schwannoma: a diagnostic and management conundrum. Am J Otolaryngol. 2012;33(5):497–504. doi: 10.1016/j.amjoto.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Brunese L, Ciccarelli R, Fucili S. et al. Pleomorphic adenoma of parotid gland: delayed enhancement on computed tomography. Dentomaxillofac Radiol. 2008;37(8):464–469. doi: 10.1259/dmfr/79964183. [DOI] [PubMed] [Google Scholar]
- 25.Habermann C R, Arndt C, Graessner J. et al. Diffusion-weighted echo-planar MR imaging of primary parotid gland tumors: is a prediction of different histologic subtypes possible? AJNR Am J Neuroradiol. 2009;30(3):591–596. doi: 10.3174/ajnr.A1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stennert E, Guntinas-Lichius O, Klussmann J P, Arnold G. Histopathology of pleomorphic adenoma in the parotid gland: a prospective unselected series of 100 cases. Laryngoscope. 2001;111(12):2195–2200. doi: 10.1097/00005537-200112000-00024. [DOI] [PubMed] [Google Scholar]
- 27.Witt R L. The significance of the margin in parotid surgery for pleomorphic adenoma. Laryngoscope. 2002;112(12):2141–2154. doi: 10.1097/00005537-200212000-00004. [DOI] [PubMed] [Google Scholar]


