Abstract
Background The purpose of this study is to describe the prevalence of Papanicolaou (Pap) smear use for cervical cancer screening and to estimate its association with type of health care insurance.
Methods A cross-sectional study using data from the Health, Well-Being and Aging in Latin America and the Caribbean Study (SABE). The sample includes 6357 women aged 60 and older from seven cities. The outcome was reporting a Pap smear for cervical cancer screening during the previous 2 years. Main independent variable was health care insurance. Covariates were demographic or socioeconomic variables, medical conditions and functional status.
Results Prevalence of Pap smear use across the seven cities ranged from 21% in Bridgetown to 45% in Mexico City. In a multivariate analysis of the combined sample, without Havana that has universal health care insurance, women with public insurance (OR 0.55, 95% CI 0.43–0.71) or with no insurance (OR 0.23, 95% CI 0.15–0.34) were less likely to have a Pap smear compared with women with private insurance. Also, women with no insurance were less likely to have a Pap smear (OR 0.40, 95% CI 0.30–0.54) compared with women with any health insurance.
Conclusions In general, the prevalence of Pap smear use was lower than that reported for Hispanic populations in the United States. Overall, lack of health insurance or having public health insurance determined lower odds for having a Pap smear for cervical cancer screening.
Keywords: Older women, cancer screening, Latin America and Caribbean, health insurance, Pap smear
Introduction
Socioeconomic development is usually related to cervical cancer mortality rates in Latin American and Caribbean countries.1,2 Between 1960 and 1994, Haiti, Bolivia and Nicaragua, countries of low social and economic development, had increased mortality rates from cervical cancer.1 In the same period of time, Argentina and Uruguay, two countries with developmental patterns similar to those of more developed countries, had the lowest mortality rates from cervical cancer in the region.1
There is a great variation of the potential impact of cancer screening on mortality related to cervical cancer in Latin American and Caribbean countries. In Puerto Rico, Colombia, Argentina, Brazil and Chile, cervical cancer screening had a greater impact by decreasing mortality rates. However, in Cuba, Costa Rica and Mexico, there were very limited changes in cervical cancer mortality following the introduction of Papanicolaou (Pap) smear as a screening method.1,3,4 In despite of lack of consistent data, cancer screening practices may determine the stage at diagnosis for cervical cancer among women in these countries.5,6
Some authors have recommended cancer screening focused in young women (30s and 40s) for low- and middle-income countries.7,8 However, those recommendations may not apply for less developed countries. Indeed, data from the International Agency for Research in Cancer showed that Latin American and Caribbean countries tend to have higher cervical cancer incidence rates in older women as compared with younger women in more developed countries. For example, in 2002, age-adjusted incidence rate ratios older/younger (65+/15–64) women were 4.2 for Barbados, 3.4 for Chile, 3.2 for Mexico, 2.9 for Costa Rica, 2.2 for Brazil, 1.8 for Cuba, 1.8 for Uruguay and 1.7 for Buenos Aires, while it was only 1.2 for the United States.9 In addition, women aged 65 years or older tend to have a higher incidence of invasive cervical cancer compared with women aged <65 years.3 In 2002, in the United States, age-adjusted incidence rate ratios older/younger (65+/<65) for women were 1.6 for whites, 2.9 for blacks, 1.5 for American Indians/Alaska natives, 2.3 for Asian or Pacific Islander and 2.3 for Hispanics.10 Higher cervical cancer incidence rate ratios (older/younger) makes knowing screening patterns for older women in Latin America and the Caribbean of critical relevance.
Factors related to increased cancer screening utilization in Latin American and Caribbean countries include high income, high education, health insurance, being married, having a regular doctor, having high functional status and sexual partners approval of gynaecological examination.4,11–16 However, there are limited data related to the effect of the type of health care insurance on cervical cancer screening practices among older women in Latin American and Caribbean countries.11,12 The objective of this study was to determine the association between health insurance and cervical cancer screening use (Pap smear) among older women from seven cities using data from the Health, Well-Being and Aging in Latin America and the Caribbean Study (SABE).
Methods
Study population
The study population was a total number of 6357 women aged 60 years or older living in urban areas of Buenos Aires (Argentina), Bridgetown (Barbados), Sao Paulo (Brazil), Santiago (Chile), Mexico City (Mexico), Havana (Cuba) and Montevideo (Uruguay).
Data source
Data were from the SABE Study that consisted of a round of cross-sectional surveys from cities in seven Latin American and Caribbean countries during 1999–2000.17,18 The Pan American Health Organization (PAHO) coordinated the overall SABE study and directed its logistics and the Center for Demography and Ecology, University of Wisconsin-Madison, jointly with PAHO, designed the study. Local, country-based teams constituted by a principal investigator and his/her associates trained the interviewers in each city. The universe of the study was the population aged 60 and older residing in the metropolitan areas of Buenos Aires, Bridgetown, Santiago and Mexico City, and in the cities of Sao Paulo, la Havana and Montevideo. Response rates were 60% in Buenos Aires, 85% in Bridgetown, 85% in Sao Paulo, 84% in Santiago, 85% in Mexico City, 95% in Havana and 66% in Montevideo. Two cities with lowest response rates, Buenos Aires19 and Montevideo,20 were compared with their corresponding Census information, finding their socio-demographic distributions comparable. The percentages of interviews by proxy were 3.7% in Buenos Aires, 3.9% in Bridgetown, 13.1% in Sao Paulo, 7.9% in Santiago, 9.7% in Havana, 8.2% in Mexico City and 1.4% in Montevideo. A classical multistage clustered sampling with stratification of the units at the highest levels of aggregation was used: the primary sampling unit was a cluster of independent households within predetermined geographic areas, grouped into socioeconomic strata and divided into secondary sampling units, each containing a smaller number of households. Finally, the household and target individuals, person 60 years and older, were randomly selected. Then, the potential participants were contacted to set an interview at home. The interviews were conducted in English for Bridgetown (Barbados), Portuguese for Sao Paulo (Brazil) and Spanish for all other cities, using the same validated questionnaires. Oral and written consent forms—approved by the Human Subjects Committee at each city with the corresponding affiliated Medical Research Institution or University—were obtained from all subjects, and personal identifiers were deleted. If a person having accepted to be interviewed failed the cognitive test, a proxy was selected to respond to some parts of the questionnaire.17,18
Variables
The dependent variable was Pap smear use. Pap smear use was assessed by the question: ‘In the last 2 years have you had a Pap smear that is a test to determine whether you have cervical or uterine cancer?’ Pap smear use was dichotomized as user (coded 1) and non-user (coded 0).
Main independent variable was health care insurance and was categorized as private insurance, public or military insurance and no insurance. In some models, we used any insurance (code = 0: private, public or military) vs no insurance (code = 1). Sociodemographic correlates examined were age (years), marital status (currently married, yes or no) and education (years). Financial strain was assessed by the question: ‘Do you believe that you (and your spouse/companion) have enough money to cover your daily living necessities’ (yes or no). This measure replaced income information that was often incomplete and not reliable in this survey, and correlated very well across wealth categories (e.g. economic resources) and access to health care (e.g. insurance).21
Medical conditions were assessed asking the respondent if she had been ever told by a doctor or other health care provider that she had diabetes mellitus, arthritis, hypertension, heart disease or stroke (yes or no). A summary score for medical conditions was constructed, from 0 to 5, and used as a continuous variable. Women were asked if ever had cancer (yes or no) or hysterectomy (a surgery to remove the uterus, yes or no). Functional status was assessed by eight instrumental activities of daily living items (IADL).22 Women were asked if they had difficulty in performing any of these activities at the time of the interview: using the telephone, travelling alone, going shopping for groceries, preparing own meals, taking own medicine, handling own money, doing light house work or doing heavy house work. IADL was used as continuous variable (score from 0 to 8).
Statistical analysis
Descriptive statistics were used to report prevalence of Pap smear use and to describe characteristics of the study population. Multivariate logistic regression analyses (models 1 and 2) were used to estimate the odds of having a Pap smear in each survey and in the combined sample of surveys from Buenos Aires, Bridgetown, Mexico, Montevideo, Santiago and Sao Paulo, where dummy variables for city were included. Model 1 included a comparison between private insurance vs public/military insurance or no insurance. Model 2 included a comparison between any insurance (private insurance or public/military) vs no insurance. In models 1 and 2, Havana, that had universal health insurance coverage, was excluded. Because cities were not randomly selected in the survey, the combined sample of six sites was treated as fixed effect. In the multivariate analysis of the combined sample of six sites, we added a dummy variable for cities and choose Mexico City as the reference because it had the highest prevalence of Pap smear. There were no effect modifications between cities and health insurance on Pap smear use. To adjust for stratified sampling survey design, data were weighted by using complex survey analyses. All analyses were performed using the SAS System for Windows, version 9.1 (SAS Institute, Inc., Cary, NC).
Results
Table 1 shows sociodemographics and health characteristics of Latin American and Caribbean older women (aged ≥60) from the SABE study. Sao Paulo has a relatively younger population and Bridgetown has a relatively older population compared with other cities. Between one-quarter and two-quarters of women were currently married. Most women had health insurance, except in Bridgetown and Mexico City where 87 and 28% of women have no insurance, respectively. The mean number of years of education was highest in Havana and Santiago and lowest in Sao Paulo and Mexico City. Women in Havana reported the lowest percentage for having enough money to cover daily living necessities while women in Mexico City reported the highest. The lowest mean number of medical conditions was reported in Mexico City and the highest in Havana. The prevalence of self-reported cancer ranged from 2.5% in Mexico City to 7.3% in Montevideo. History of hysterectomy ranged from 13.1% in Buenos Aires to 30.2% in Bridgetown. The highest number of IADL difficulties were reported in Sao Paulo and Santiago.
Table 1.
Characteristics of study population, women aged 60 years and older
| Characteristics | Buenos Aires n = 655 | Bridgetown n = 915 | Sao Paulo n = 1262 | Santiago n = 855 | Mexico City n = 738 | Montevideo n = 915 | Havana N = 1197 | Total sample n = 6357 |
|---|---|---|---|---|---|---|---|---|
| Age (years) | 71.0 (0.30) | 73.1 (0.29) | 69.7 (0.21) | 70.9 (0.34) | 70.2 (0.31) | 71.0 (0.27) | 71.7 (0.30) | 70.7 (0.14) |
| Married | 43.3 | 23.4 | 41.3 | 42.1 | 38.7 | 35.4 | 22.5 | 39.7 |
| Education (years) | 6.1 (1.16) | 5.1 (0.11) | 4.2 (0.10) | 6.6 (0.25) | 4.2 (0.15) | 5.8 (0.14) | 6.8 (0.12) | 5.6 (0.08) |
| Health insurance | ||||||||
| Private | 9.5 | 8.4 | 37.9 | 6.8 | 3.1 | 66.1 | – | 17.7 |
| Public/military | 76.0 | 4.6 | 59.7 | 82.9 | 69.1 | 32.7 | – | 68.3 |
| None | 14.5 | 86.9 | 2.4 | 10.3 | 27.8 | 1.2 | – | 14.0 |
| Enough moneya | 31.8 | 33.5 | 31.0 | 29.6 | 50.8 | 40.9 | 19.4 | 35.6 |
| Number of medical conditions (0–5) | 1.5 (0.04) | 1.5 (0.03) | 1.4 (0.03) | 1.5 (0.04) | 1.2 (0.04) | 1.5 (0.04) | 1.7 (0.03) | 1.4 (0.01) |
| Cancer | 6.0 | 3.5 | 3.5 | 5.7 | 2.5 | 7.3 | 3.6 | 4.6 |
| History of hysterectomy | 13.1 | 30.2 | 16.6 | 13.2 | 18.2 | 15.6 | 16.6 | 14.6 |
| IADL difficulties (0–8) | 0.7 (0.05) | 0.6 (0.04) | 1.0 (0.05) | 1.0 (0.08) | 0.9 (0.07) | 0.4 (0.04) | 0.8 (0.05) | 0.8 (0.02) |
Data are presented as weighted percentages or means (standard error). Number of medical conditions include hypertension, diabetes, heart attack, arthritis and stroke.
aEnough to cover daily living necessities; – no data for health insurance categories in Havana are presented, where insurance is universal.
Table 2 shows the prevalence of Pap smear use by city and the bivariate associations between Pap smear use and health insurance categories among women aged 60 years and older. The prevalence of Pap smear use was highest in Mexico City (46%) and Sao Paulo (44%) and lowest in Bridgetown (21%) and Montevideo (24%). Women with private insurance have the highest prevalence of Pap smear use while women with no health insurance have the lowest in Buenos Aires, Sao Paulo, Mexico City and the total sample.
Table 2.
Prevalence (%) of Pap smear screening use, in the prior 2 years, overall and by insurance categories, women aged 60 years and older, (1999–2000)
| Buenos Aires n = 655 | Bridgetown n = 915 | Sao Paulo n = 1262 | Santiago n = 855 | Mexico City n = 738 | Montevideo n = 915 | Havana N = 1197 | Total samplen = 6357 | |
|---|---|---|---|---|---|---|---|---|
| Overall percentage of Pap smear | 37.2 | 21.1 | 43.6 | 36.3 | 45.5 | 23.7 | 27.3 | 38.1 |
| Health insurance | ||||||||
| Private | 69.4 | 33.2 | 54.8 | 44.7 | 60.2 | 25.8 | – | 47.4 |
| Public/military | 35.8 | 24.0 | 37.8 | 35.3 | 52.6 | 20.0 | – | 39.4 |
| None | 24.6a | 19.8 | 14.3a | 39.6 | 25.9a | 11.4 | – | 26.1a |
Data are presented as weighted percentages.
aP < 0.0001; – no data for health insurance categories in Havana are presented, where insurance is universal.
Table 3 shows multivariate analyses for health insurance predicting Pap smear use for each city and the combined sample of six cities. In model 1, older women residing in Buenos Aires (OR 0.31, 95% CI 0.16–0.60; OR 0.14, 95% CI 0.06–0.32) and Sao Paulo (OR 0.56, 95% CI 0.41–0.75; OR 0.14, 95% CI 0.04–0.48), and in the combined sample (OR 0.55, 95% CI 0.43–0.71; OR 0.23, 95% CI 0.15–0.34) with public/military insurance or no insurance were less likely to have a Pap smear during the previous 2 years compared to women with private health insurance. In model 2, older women residing in Buenos Aires (OR 0.39, 95% CI 0.21–0.73), Sao Paulo (OR 0.20, 95% CI 0.06–0.67) and Mexico City (OR 0.34, 95% CI 0.23–0.51) and the total sample (OR 0.40, 95% CI 0.30–0.54) with no insurance were less likely to report a Pap smear during the previous 2 years compared to women with any health insurance. In addition to health insurance, in the combined sample of six cities (both models 1 and 2), other independent predictors for having a Pap smear were younger age, being married, higher education and a high number of medical conditions, history of cancer or a low number of functional difficulties. Also, other cities had decreased odds for having a Pap smear compared with Mexico City.
Table 3.
Multivariate analyses for health insurance predicting Pap smear use in women aged 60 years and older (1999–2000)
| Buenos Aires n = 655 OR (95% CI) | Bridgetown n = 915 OR (95% CI) | Sao Paulo n = 1262 OR (95% CI) | Santiago n = 855 OR (95% CI) | Mexico City n = 738 OR (95% CI) | Montevideo n = 915 OR (95% CI) | Total samplea n = 5340 OR (95% CI) | |
|---|---|---|---|---|---|---|---|
| Model 1 | |||||||
| Health insurance | |||||||
| Private | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Public/military | 0.31 (0.16–0.60) | 0.55 (0.20–1.53) | 0.56 (0.41–0.75) | 1.23 (0.46–3.27) | 1.08 (0.39–2.99) | 0.86 (0.55–1.33) | 0.55 (0.43–0.71) |
| None | 0.14 (0.06–0.32) | 0.64 (0.36–1.14) | 0.14 (0.04–0.48) | 1.14 (0.37–3.53) | 0.37 (0.13–1.06) | 0.47 (0.09–2.34) | 0.23 (0.15–0.34) |
| Model 2 | |||||||
| Health insurance | |||||||
| Private, public or military | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| None | 0.39 (0.21–0.73) | 0.77 (0.46–1.27) | 0.20 (0.06–0.67) | 0.94 (0.49–1.78) | 0.34 (0.23–0.51) | 0.50 (0.10–2.47) | 0.40 (0.30–0.54) |
OR, Odds ratio; CI, confidence intervals.
Odds ratios were weighted and adjusted for age, marital status, education, insurance status, having enough money to cover daily necessities, number of medical conditions (hypertension, diabetes, heart attack, arthritis and stroke; score 0–5), cancer, history of hysterectomy and IADL (score 0–8). In the total sample, odds ratios were also adjusted for cities as dummy variables.
aWithout Havana.
Discussion
This is a comparative analysis of the relationship between health insurance and cervical cancer screening methods among older women living in urban areas of seven Latin American and Caribbean cities. Overall, we found that women with public/military health insurance or with no insurance were less likely to have a Pap smear in the previous 2 years compared with women with private health insurance; that relationship remained after adjusting for other relevant socio-demographic and health factors. Also, women with no insurance were less likely to have a Pap smear compared to women with any health insurance.
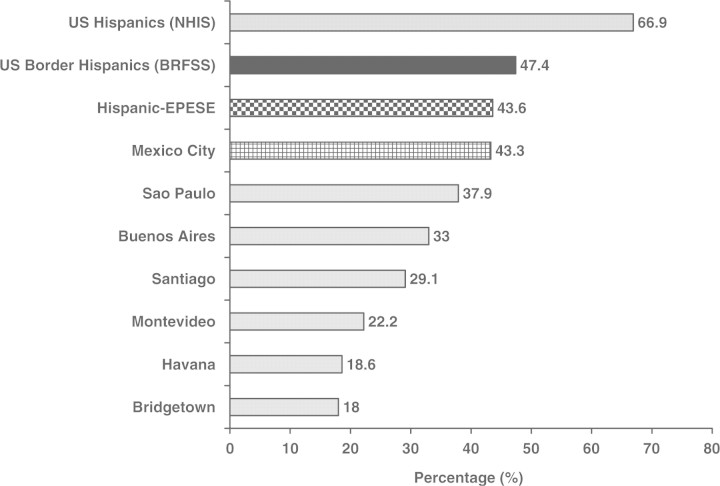
To compare our results with other data for Hispanic older women in the United States, we also calculated prevalence of Pap smear use in our sample, but using age 65 and older (Figure 1). Prevalence of Pap smear use across the six cities among women aged 65 and over ranged from 18% in Bridgetown to 43% in Mexico City, and was lower than that reported in studies for Hispanics in the US. Using data from the Behavioral Risk Factors Surveillance System (1999–2000), Coughlin and Uhler23 reported a prevalence of Pap smear use in the previous 2 years of 47.4% for Hispanics women aged 65 and over in US–Mexico border counties. Using data from the National Health Interview Survey (2000), Swan et al.24 reported a prevalence of Pap smear use in the previous 2 years of 66.9% for Hispanic women aged 65 and over in the US. Finally, using data from the Hispanic Established Population for the Epidemiologic Study of the Elderly (Hispanic EPESE, 1995–96), Wu et al.25 reported a prevalence of 43.6% among Mexican American women aged 67 and older residing in the Southwestern United States.
Figure 1.
Prevalence of a Pap smear during the previous 2 years among women 65 years and older in Latin America, the Caribbean (1999–2000) and the US Hispanic populations: the US National Health Interview Survey (2000),18 the US Behavioral Risk Factors Surveillance System (Border Counties, 1999–2000)17 and the Hispanic established population for the Epidemiologic Study of the elderly (1995–96).19
Our finding related to the association between health insurance and increased screening use is consistent with other reports in Hispanic populations in the United States.23–29 Health insurance has been treated as a proxy for access to social and economic resources that influence health status and use of preventive services.23–29 Lack of health insurance is correlated to lower education, which is an indicator of less economic resources, therefore, economic barriers could be an important explanatory factor for disparities on screening methods. Parts of the effects of health insurance on access to care can be explained by other socioeconomic indicators such as income, education or occupation.30 However, in three cities, Buenos Aires, Sao Paulo and Mexico City, and in the combined sample of six cities, health insurance had an independent effect to determine Pap smear utilization.
The PAHO, provided guidelines for organizing national cancer control programmes in Latin American and Caribbean countries, emphasizing cervical cancer screening for all countries.31,32 However, most countries in the region do not have an organized cervical cancer screening programme. Indeed, with the exception of Chile, countries host of the cities in this study have opportunistic or unorganized cervical cancer screening programmes.4,5,16,33–36 Therefore, the health system may explain in part why Pap smear use is affected by health insurance.
In some cities where health insurance was not associated with Pap smear use, particular characteristics of the host country may help to explain those findings. For example, in spite of low frequencies of health insurance coverage, there is a free health care for all Barbadians, and older persons have unrestricted access to primary health care, which is available at the polyclinics that are operated by the Government.37,38 This may be an explanation why health insurance had not effect on Pap smear screening utilization in Bridgetown.
In addition, in Chile, 1987, the Ministry of Health implemented the National Cervical Cancer Program for cervical cancer screening. Coverage by at least one Pap smear in the previous 3 years rose from 43% in 1989 to 66% in 1991 in women 25- to 64-years-old of the Metropolitan Region of Santiago.39 Between 1980 and 2001, age adjusted cervical cancer mortality rate decreased from 12.8% to 6.8% per 100 000 women.4 Then, an organized cervical cancer screening programme may explain why there was no relationship between health insurance and Pap smear use in Santiago.
One potential explanation why insurance has not effect on Pap smear use in Montevideo (Table 3, models 1 and 2) was its lowest percentage of uninsured women with only 1.2%. In addition, other factors such as older age, lower education, history or hysterectomy were associated with decreased odds of having a Pap smear. In contrast, being married or having history of cancer were associated with increased odds of having a Pap smear. In Mexico City, the odds for Pap smear use did not differ when comparing private insurance vs public or Military insurance (Table 3, model 1), but other socioeconomic factors were associated with higher odds of Pap smear use (e.g. higher education). However, when considering any insurance vs no insurance (Table 3, model 2), the effect of insurance on the odds of Pap smear was independent from socioeconomic factors.
In some cities, the high prevalence of cancer may affect the prevalence of Pap smear. History of cancer or being a cancer survivor have been associated with increased screening use in some studies.40–42 Indeed, in our study, cancer was independent predictor of Pap smear in Montevideo and Buenos Aires. However, in these cities or in the combined sample the effect of insurance on Pap smear use remained when adjusting for history of cancer.
On the other hand, women with history of hysterectomy tend to have lower rates of Pap smear screening. According to cancer screening guidelines, an estimated 90% of hysterectomized women should not be screened for cervical cancer.43 In our study, 15% of the total sample had history of hysterectomy, but information was not available on whether the surgery occurred in relation to the Pap smear, the reason for the hysterectomy (e.g. cervical neoplasia), or if the hysterectomy was supracervical (leaving intact cervix) where continued Pap smear for cervical cancer screening would be appropriate. In despite of this limitation, this factor may explain in part why insurance status did not have any effect on screening in Bridgetown that had the highest rates of hysterectomy (30%). Indeed, having a hysterectomy was independently associated with lower odds of having a Pap smear in Havana, Montevideo and especially Bridgetown, where women who reported a hysterectomy were 65% less likely to have a Pap smear as compared with those not having a hysterectomy.
Cuba has particular characteristics, with modest infrastructure investment combined with a well-developed public health system have generated health measures comparable with those of industrialized countries.44 In Cuba, a cervical cytology screening programme offering Pap smears every 2 years to women aged ≥20 years, was implemented through the primary health care services in 1968, and Pap smear screening has been focused in younger populations.45 Indeed, in our data for Havana, holding all variables constant (without insurance in the model) each additional year of age resulted in a 12% decrease in the odds of having a Pap smear. This is a potential explanation for why Havana had a very low prevalence rate for Pap smear use.
This study has some limitations. Our reliance in cross-sectional data precludes establishing causal order between certain variables and screening methods use. Data on Pap smear screening use were self-reported, which may affect the accuracy of our measures and consequently our results. Some studies have shown low concordance between self-report of Pap smear and medical chart reports, especially in low-income women.46,47 However, in other studies, concordance between self-reported data and medical record documentation has been reported as greater for a Pap smear, although women tend to underestimate the time since their last screening.48–50 Finally, we did not control for cultural barriers that may affect cervical cancer screening utilization among Latinas. For example, in Mexican women, reasons for not obtaining a Pap smear are anxiety regarding physical privacy, considering pelvic examination as uncomfortable and fears that any gynaecological treatment would leave them sexually disabled.12,34,35
The SABE survey does not represent the diversity of the elderly population that exists in the selected countries because the information was collected only in large urban areas. Patterns of availability and screening usage may differ dramatically in rural settings. Indeed, women living in rural areas in the United States have higher cervical cancer incidence (especially invasive) and mortality rates;51–53 and they are less likely to be screened for cervical carcinoma compared with those residing in urban areas.53 Women residing in rural areas in less developed countries tend to have lower access to health care and preventive services, and they usually have greater cultural barriers for cancer screening compared with women residing in urban areas.13,54
This study has also some strengths. The lowest percentages of Pap smear screening methods for older women with no insurance were consistent across most of the cities and in the combined sample. The effect of health insurance on Pap smear screening remained after we controlled for demographic and socioeconomic factors known to be related to inequality on cancer screening such as education level and financial. On the other hand, our results may aid the development of specific health policies such as providing free access to cervical cancer screening among those older women with less socioeconomic resources or without insurance.
In conclusion, the organization of the countries’ health system and the screening programmes in each country (e.g. most opportunistic) may explain in part the low prevalence of cervical cancer screening across cities, and in the effect of health care insurance on Pap smear use among Latin American and Caribbean older women. In the overall combined sample and in most of the cities, health insurance, any insurance or especially private insurance, was associated with higher odds of having a Pap smear in older women. Low percentages of older women having regular screening for cervical cancer is of great concern, especially given the higher age-adjusted cervical cancer incidence rate ratios (older/younger) in countries such as Barbados, Mexico and other Latin American and Caribbean nations. Therefore, an organized screening programme, and health insurance along with other socioeconomic support are needed to increase coverage and follow-up of screening programmes among older women in these populations.
Acknowledgements
C.A.R.O. acknowledges financial support from the Department of Defense (W81XWH-06-1-0290) and from the Multicultural Health and Healthcare Research Network, Health Quality Scholar Program at the University of California Los Angeles and the Robert Wood Johnson Foundation.
Conflicts of interest: None declared.
KEY MESSAGES.
Prevalence of Pap smear use across the seven cities ranged from 21% in Bridgetown to 45% in Mexico City.
Latin American and Caribbean older women have lower cervical cancer screening prevalence rates compared with Hispanic older women residing in the United States.
Lack of health insurance was associated with lower odds for having a Pap smear for cervical cancer screening.
References
- 1.Arrossi S, Sankaranarayanan R, Parkin DM. Incidence and mortality of cervical cancer in Latin America. Salud Publica Mex. 2003;45(Suppl 3):S306–14. doi: 10.1590/s0036-36342003000900004. [DOI] [PubMed] [Google Scholar]
- 2.Bosetti C, Malvezzi M, Chatenoud L, et al. Trends in cancer mortality in the Americas, 1970-2000. Ann Oncol. 2005;16:489–511. doi: 10.1093/humrep/mdi086. [DOI] [PubMed] [Google Scholar]
- 3.Bleggi Torres LF, Werner B, Totsugui J, et al. Cervical cancer screening program of Parana: cost-effective model in a developing country. Diagn Cytopathol. 2003;29:49–54. doi: 10.1002/dc.10269. [DOI] [PubMed] [Google Scholar]
- 4.Sepulveda C, Prado R. Effective cervical cytology screening programmes in middle-income countries: the Chilean experience. Cancer Detect Prev. 2005;29:405–11. doi: 10.1016/j.cdp.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Sankaranarayanan R, Budukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bull World Health Organ. 2001;79:954–62. [PMC free article] [PubMed] [Google Scholar]
- 6.Hanchard B, Blake G, Wolff G, et al. Age-specific incidence of cancer in Kingston and St Andrew, Jamaica, 1993-1997. West Indian Med J. 2001;50:123–29. [PubMed] [Google Scholar]
- 7.Mandelblatt JS, Lawrence WF, Gaffikin L, et al. Costs and benefits of different strategies to screen for cervical cancer in less-developed countries. J Natl Cancer Inst. 2002;94:1469–83. doi: 10.1093/jnci/94.19.1469. [DOI] [PubMed] [Google Scholar]
- 8.Goldie SJ, Gaffikin L, Goldhaber-Fiebert JD, et al. Cost-effectiveness of cervical cancer screening in five developing countries. N Engl J Med. 2005;353:2158–68. doi: 10.1056/NEJMsa044278. [DOI] [PubMed] [Google Scholar]
- 9.Ferlay J, Bray F, Pisani P, Parkin DM. IARC Cancer Base No. 5, version 2.0. Lyon: IARC Press; 2004. GLOBOCAN 2002. Cancer Incidence, Mortality and Prevalence Worldwide. [Google Scholar]
- 10.National Cancer Institute. SEER Statistics. Cervix uterine cancer. [(Accessed on April 4, 2008)]. Available at: http://seer.cancer.gov/faststats/sites.php?stat=Incidence&site=Cervix+Uteri+Cancer&x=5&y=15.
- 11.Mendoza-Sassi R, Beria JU. Prevalence of having a regular doctor, associated factors, and the effect on health services utilization: A Population-based Study in Southern Brazil. Cad Saude Publica. 2003;19:1257–66. doi: 10.1590/s0102-311x2003000500004. [DOI] [PubMed] [Google Scholar]
- 12.Bingham A, Bishop A, Coffey P, et al. Factors affecting utilization of cervical cancer prevention services in low-resource settings. Salud Publica Mex. 2003;45(Suppl 3):S408–16. doi: 10.1590/s0036-36342003000900015. [DOI] [PubMed] [Google Scholar]
- 13.Watkins MM, Gabali C, Winkleby M, Gaona E, Lebaron S. Barriers to cervical screening in rural Mexico. Int J Gynecol Cancer. 2002;12:475–79. doi: 10.1046/j.1525-1438.2002.01170.x. [DOI] [PubMed] [Google Scholar]
- 14.Aguilar-Perez JA, Leyva-Lopez AG, Angulo-Najera D, Salinas A, Lazcano-Ponce EC. Tamizaje en cáncer cervical: conocimiento de la utilidad y uso de citología cervical en México. Rev Saude Publica. 2003;37:100–6. doi: 10.1590/s0034-89102003000100015. [DOI] [PubMed] [Google Scholar]
- 15.Reyes-Ortiz CA, Freeman J, Peláez M, Markides KS, Goodwin JS. Mammography use among older women of seven Latin American and the Caribbean cities. Prev Med. 2006;42:375–80. doi: 10.1016/j.ypmed.2006.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reyes-Ortiz CA, Camacho ME, Amador LF, Velez LF, Ottenbacher K, Markides KS. Education, literacy and cancer screening among Latin American and Caribbean older adults. Cancer Control. 2007;14:388–95. doi: 10.1177/107327480701400409. [DOI] [PubMed] [Google Scholar]
- 17.Albala C, Lebrao ML, Leon Diaz EM, et al. Encuesta Salud, Bienestar y Envejecimiento (SABE): metodología de la encuesta y perfil de la población estudiada. Rev Panam Salud Publica. 2005;17:307–22. doi: 10.1590/s1020-49892005000500003. [DOI] [PubMed] [Google Scholar]
- 18.Wong R, Pelaez M, Palloni A, Markides KS. Survey data for the study of aging in Latin American and the Caribbean. J Aging Health. 2006;18:157–79. doi: 10.1177/0898264305285655. [DOI] [PubMed] [Google Scholar]
- 19.Instituto Nacional de Estadisticas y Censos. Censo Nacional de Población, Hogares y Viviendas año2001; Buenos Aires, Argentina. [(Accessed on April 3, 2008)]. Available at: www.indec.mecon.ar/webcenso/index.asp.
- 20.Instituto Nacional de Estadística. VII Censo General de Población, III Hogares y V Viviendas, año1996; Montevideo, Uruguay. [(Accessed on April 3, 2008)]. Available at www.ine.gub.uy/biblioteca/CENSO96/montevideo.htm.
- 21.Wallace SP, Gutierrez VF. Equity of access to health care for older adults in four major Latin American cities. Rev Panam Salud Publica. 2005;17:394–409. doi: 10.1590/s1020-49892005000500012. [DOI] [PubMed] [Google Scholar]
- 22.Fillenbaum GG. Screening the elderly: a brief instrumental activity of daily living measure. J Am Geriatr Soc. 1985;33:698–706. doi: 10.1111/j.1532-5415.1985.tb01779.x. [DOI] [PubMed] [Google Scholar]
- 23.Coughlin SS, Uhler RJ. Breast and cervical cancer screening practices among Hispanic women in the United States and Puerto Rico, 1998-1999. Prev Med. 2002;34:242–51. doi: 10.1006/pmed.2001.0984. [DOI] [PubMed] [Google Scholar]
- 24.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–40. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 25.Wu HZ, Black SA, Freeman JL, Markides KS. Older Mexican American women and cancer screening: progress toward targets for Healthy People 2000. Ethn Dis. 2001;11:645–51. [PubMed] [Google Scholar]
- 26.Zambrana RE, Breen N, Fox SA, Gutierrez-Mohamed ML. Use of cancer screening practices by Hispanic women: analyses by subgroup. Prev Med. 1999;29(6 Pt 1):466–77. doi: 10.1006/pmed.1999.0566. [DOI] [PubMed] [Google Scholar]
- 27.Selvin E, Brett KM. Breast and cervical cancer screening: sociodemographic predictors among White, Black, and Hispanic women. Am J Public Health. 2003;93:618–23. doi: 10.2105/ajph.93.4.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernandez-Esquer ME, Espinoza P, Ramirez AG, McAlister AL. Repeated Pap smear screening among Mexican-American women. Health Educ Res. 2003;18:477–87. doi: 10.1093/her/cyf037. [DOI] [PubMed] [Google Scholar]
- 29.Rodríguez MA, Ward LM, Perez-Stable EJ. Breast and cervical cancer screening: impact of health insurance status, ethnicity, and nativity of Latinas. Ann Fam Med. 2005;3:235–41. doi: 10.1370/afm.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lahelma E, Martikainen P, Laaksonen M, Aittomaki A. Pathways between socioeconomic determinants of health. J Epidemiol Community Health. 2004;58:327–32. doi: 10.1136/jech.2003.011148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. Policies and managerial guidelines for national cancer control programs. Rev Panam Salud Publica. 2002;12:366–70. [PubMed] [Google Scholar]
- 32.La Salud de las Américas. Vol. 2. Washington, DC: OPS; 1998. Organización Panamericana de la Salud. Publicación Científica de la OPS No. 569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mackay J, Jemal A, Lee NC, Parkin DM. The Cancer Atlas. Atlanta, Georgia: American Cancer Society; 2006. [Google Scholar]
- 34.Flores Y, Bishai D, Lazcano E, et al. Improving cervical cancer screening in Mexico: results from the Morelos HPV Study. Salud Pública Méx. 2003;45(Suppl 3):388–98. doi: 10.1590/s0036-36342003000900013. [DOI] [PubMed] [Google Scholar]
- 35.Hernández-Avila M, Lazcano-Ponce EC, de Ruiz PA, Romieu I. Evaluation of the cervical cancer screening programme in Mexico: A Population-based Case-control Study. Int J Epidemiol. 1998;27:370–76. doi: 10.1093/ije/27.3.370. [DOI] [PubMed] [Google Scholar]
- 36.Pinho AA, Junior IF, Schraiber LB, D’Oliveira AFPL. Cervical cancer screening in the Municipality of Sao Paulo: coverage and factors involved in submitting the Pap test. Cad Saude Publica. 2003;19(Suppl 2):S303–13. doi: 10.1590/s0102-311x2003000800012. [DOI] [PubMed] [Google Scholar]
- 37.Pan American Health Organization. Country Health Profiles. 1998. [(Accessed on April 12, 2007)]. Available at: www.paho.org/english/hia_1998ed.htm.
- 38.Hambleton IR, Clarke K, Broome HL, Fraser HS, Brathwaite F, Hennis AJ. Historical and current predictors of self-reported health status among elderly persons in Barbados. Rev Panam Salud Publica. 2005;17:342–52. doi: 10.1590/s1020-49892005000500006. [DOI] [PubMed] [Google Scholar]
- 39.Salas I. Methodology for reorganization of the cervical cancer program in Chile. Cancer Detect Prev. 2006;30:38–43. doi: 10.1016/j.cdp.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 40.Trask PC, Rabin C, Rogers ML, et al. Cancer screening practices among cancer survivors. Am J Prev Med. 2005;28:351–56. doi: 10.1016/j.amepre.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 41.Legg JS, Fauber TL, Ozcan YA. The influence of previous breast cancer upon mammography utilization. Womens Health Issues. 2003;13:62–67. doi: 10.1016/s1049-3867(02)00194-9. [DOI] [PubMed] [Google Scholar]
- 42.Duffy CM, Clark MA, Allsworth JE. Health maintenance and screening in breast cancer survivors in the United States. Cancer Detec Prev. 2006;30:52–57. doi: 10.1016/j.cdp.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 43.Solomon D, Breen N, McNeel T. Cervical cancer screening rates in the United States and the potential impact of implementation of screening guidelines. CA Cancer J Clin. 2007;57:105–11. doi: 10.3322/canjclin.57.2.105. [DOI] [PubMed] [Google Scholar]
- 44.Cooper RS, Kennelly JF, Orduñez-Garcia P. Health in Cuba. Int J Epidemiol. 2006;35:817–24. doi: 10.1093/ije/dyl175. [DOI] [PubMed] [Google Scholar]
- 45.Fernandez-Garrote L. Pan American Health Organization. Evaluation of the cervical cancer control program in Cuba. Bull Pan Am Health Organ. 1996;30:387–91. [PubMed] [Google Scholar]
- 46.Pizarro J, Schneider TR, Salovey P. A source of error in self-reports of Pap test utilization. J Community Health. 2002;27:351–56. doi: 10.1023/a:1019888627113. [DOI] [PubMed] [Google Scholar]
- 47.Hiatt RA, Perez-Stable EJ, Quesenberry C, Jr, Sabogal F, Otero-Sabogal R, McPhee SJ. Agreement between self-reported early cancer detection practices and medical audits among Hispanic and non-Hispanic white health plan members in northern California. Prev Med. 1995;24:278–85. doi: 10.1006/pmed.1995.1045. [DOI] [PubMed] [Google Scholar]
- 48.Gordon NP, Hiatt RA, Lampert DI. Concordance of self-reported data and medical record audit for six cancer screening procedures. J Natl Cancer Inst. 1993;85:566–70. doi: 10.1093/jnci/85.7.566. [DOI] [PubMed] [Google Scholar]
- 49.Caplan LS, McQueen DV, Qualters JR, Leff M, Garrett C, Calonge N. Validity of women's self-reports of cancer screening test utilization in a managed care population. Cancer Epidemiol Biomarkers Prev. 2003;12:1182–87. [PubMed] [Google Scholar]
- 50.Paskett ED, Tatum CM, Mack DW, Hoen H, Case LD, Velez R. Validation of self-reported breast and cervical cancer screening tests among low-income minority women. Cancer Epidemiol Biomarkers Prev. 1996;5:721–26. [PubMed] [Google Scholar]
- 51.Benard VB, Coughlin SS, Thompson T, Richardson LC. Cervical cancer incidence in the United States by area of residence, 1998 2001. Obstet Gynecol. 2007;110:681–86. doi: 10.1097/01.AOG.0000279449.74780.81. [DOI] [PubMed] [Google Scholar]
- 52.Coughlin SS, Thompson TD, Hall HI, Logan P, Uhler RJ. Breast and cervical carcinoma screening practices among women in rural and nonrural areas of the United States, 1998-1999. Cancer. 2002;94:2801–12. doi: 10.1002/cncr.10577. [DOI] [PubMed] [Google Scholar]
- 53.Schootman M, Fuortes LJ. Breast and cervical carcinoma: the correlation of activity limitations and rurality with screening, disease incidence, and mortality. Cancer. 1999;86:1087–94. [PubMed] [Google Scholar]
- 54.Castro-Jimenez MA, Londoño-Cuellar PA, Vera-Cala LM. Use and determinants of Pap smear in a rural Colombian municipality 1998-1999. Rev Salud Publica (Bogota) 2006;8:248–57. doi: 10.1590/s0124-00642006000300010. [DOI] [PubMed] [Google Scholar]