Abstract
Purpose: A primary goal for aging policy is to optimize independence in later life. We estimate the cross-sectional association between physical and social challenge in the home environment and use of assistive devices (AD) for mobility in the home, controlling for lower extremity physical performance (short physical performance battery [SPPB]) and other factors. Design and Methods: Data are from the Women’s Health and Aging Study I, a prospective study of the factors related to physical disability in a sample of moderately to severely disabled older women. We describe these associations in the baseline sample overall and also within subsets who do and do not have both a baseline and a 3-year follow-up observation. Results: On average, physical challenge in the home environment is inversely associated with level of AD use (p < .05) in the overall sample, independent of SPPB, living alone, and other factors. We do not find a significant (p < .05) association between social challenge and the level of AD use in the overall sample. Findings by follow-up responder status were similar (with minor variability). Implications: Future cohorts who are better educated and more receptive to technology may confront challenges in the home environment that limit their ability to age in place. Our findings suggest that the physical challenges of the home are significantly related to AD use. Future analyses that explore the mechanisms of the home environment as a source of challenges to independent functioning could help in the design of future interventions for these cohorts as they age.
Key Words: Technology, Aging in place, Function (physical mental)
A primary goal for aging policy is to optimize independence in later life. Many older adults have lived in their homes for many years, having chosen housing and neighborhoods that were good places to live, work, and raise families. As they age and the prevalence of chronic diseases and functional impairments increases, older Americans may experience a mismatch between their own physical capacity, the challenges of their home environments, and the availability of help.
Gaps in “person-environment fit” can be addressed in different ways, including use of “compensatory strategies” (Weiss, Hoenig, & Fried, 2007). Elements of compensatory strategies include use of environmental modifications that reduce the demands of the physical environment; assistive devices (ADs) that increase the individual’s capabilities; personal assistance; and behavioral change. Although each of these approaches represents ways of coping with disablement, environmental modifications and AD use constitute forms of self-care and thus enhance independence. In contrast, for example, personal assistance involves the cooperation and availability of helpers and thus creates a state of dependence even as it reduces disability (Agree, 1999).
The majority of older adults with disabilities use an AD, most often for mobility (Agree & Freedman, 2000; Agree, Freedman, & Sengupta, 2004), and the number has been growing (Freedman, Agree, Martin, & Cornman, 2006; Schoeni, Freedman, & Martin, 2008). Devices can be important aids to mobility in the home, but the physical challenges of the home environment may interfere with their use. For example, walkers may be less useful on uneven surfaces and wheelchairs can be problematic in the presence of steps. However, if such features signal environments of greater challenge, they may also indicate a greater need for an AD to navigate in the home. Similarly, other members of the household (e.g., a spouse) who can provide personal assistance define a social resource in the home environment. Hoenig and colleagues also used data from the Women’s Health and Aging Study I (WHAS I) to show that coresidence is associated with use of personal assistance for mobility activities in the home (Hoenig et al., 2006), which is consistent with Spillman (2005), who used National Long-term Care Survey data to show a link between living with a spouse and use of help (and, conversely, that living alone is associated with equipment use).
Although existing work has studied the association between the home environment and compensatory strategies generally (Ganesh, Fried, Taylor, Pieper, & Hoenig, 2011; Hoenig et al., 2006), researchers have not focused specifically on AD use, which may differ from other approaches to address gaps in the person-environment fit. A comprehensive theoretical approach to such issues is through the lens of the seminal work of Lawton and Nahemow (1973), which was subsequently updated (Lawton, 1998) and continues to influence the field of environmental gerontology (Scheidt & Norris-Baker, 2004; Wahl & Weisman, 2003) and the study of disability more generally (IOM, 1991, 2007; Verbrugge & Jette, 1994). This framework (originally formulated in psychological and behavioral domains) argues that successful functioning is the result of a balance between the level of challenge present in the environment and an individual’s abilities to meet those challenges.
However, a central limitation to our application of the Lawton and Nahemow framework in this study are its strong causal implications, which are inconsistent with our preliminary, descriptive stage of investigation. Furthermore, physical and social environments have complex and multilayered functions (Rowles, Oswald, & Hunter, 2004; Wahl, Iwarsson, & Oswald, 2012) that are beyond the scope of the present analysis. Therefore, we instead take a descriptive approach that is consistent with the strengths and limitations of our data. We ask are different dimensions of the home environment associated with AD use, viewing the latter as an outcome for mobility? Furthermore, does the association either differ at a single point in time between those who will and will not survive and fully participate in a future study wave or differ across time within the same subset of women?
Understanding how the physical and social dimensions of the home environment are associated with the use of ADs is critical (Hoenig, Giacobbi, & Levy, 2007), particularly at a time when the availability of human help is likely to decline. Today’s elders are the parents of the baby boom and thus generally have larger families with children to help them, but the boomers will enter old age with fewer children to rely on for support (Agree & Hughes, 2012; Hughes & Waite, 2007). In addition, future elderly cohorts also will be better educated on average than previous cohorts (Crystal, 2007; Freedman, Schoeni, Martin, & Cornman, 2007), and thus perhaps increasingly receptive to the use of ADs to meet their needs as they age (Pressler & Ferraro, 2010).
Methods
Data
Data are from the WHAS I, a prospective study of the factors related to physical disability in disabled older women. The study was conducted between 1992 and 1998 with 1,002 women at baseline representing the one third of most physically disabled women aged 65 or older living in the Baltimore area. Participants were interviewed, given a physical exam and the short physical performance battery (SPPB; Guralnik et al., 1994) every 6 months for approximately three years. The methodology and descriptive findings of the study are detailed elsewhere (Guralnik, Fried, Simonsick, Kasper, & Lafferty, 1995; Kasper, Shapiro, Guralnik, Bandeen-Roche, & Fried, 1999; Simonsick et al., 1997).
We use data from the baseline and final rounds of the study. After excluding observations with missing data at baseline, our analysis sample comprises 875 women. Of this baseline sample, 441 women survived and also provided complete data for the final round of observation. Of the 434 women who participated in the baseline but did not provide complete data for the follow-up, 123 (28%) died, 139 (32%) had missing data on at least one necessary variable in the final round, and 172 (40%) were excluded for other reasons. We will refer to the two subsets as “follow-up responders” (i.e., those who have both a baseline and a follow-up observation) and “follow-up nonresponders” (i.e., those who have a baseline observation only).
Variables
Our outcome of interest is the self-reported use of ADs for mobility (i.e., cane, walker, or wheelchair) in the home. We code the variable as ordinal from “no AD use in the home” to “cane use only” and, finally, “walker and/or wheelchair use in the home (which may or may not also include cane use).”
Our independent variable of interest is challenge in the home environment, which we define both as social and physical. Social challenge is represented by a binary indicator for whether the respondent lives alone (vs. with a spouse or others). Physical challenge is measured by a mean-zero score reflecting the sum of first dimension coordinates of a multiple correspondence analysis (MCA; Greenacre, 2007) on the indicator matrix composed of three binary indicators for physical challenges in the home: (a) having to step up/down to get into the house, (b) not having bathroom/bedroom/kitchen on the same floor, and (c) having more than four rooms in house. We performed the MCA separately on the analysis samples at baseline and follow-up.
We include in our models a measure of physical competence: the SPPB (Guralnik et al., 1994) for physical performance, focusing on lower extremity ability. This measure closely reflects the true individual capacity for functioning that underlies physical competence (Freedman, 2009). The SPPB is described in detail elsewhere (Guralnik et al., 1994); briefly, it includes scores for a walk, chair stand, and balance task and ranges from 0 to 12 (best ability). Only women with scores for at least two of the three tasks are assigned nonmissing totals (for a small number of women with one missing score, the sum of the two nonmissing scores was multiplied by 1.5). We also include controls for age at baseline (continuous) and other variables related to disability or adoption of AD (Pressler & Ferraro, 2010; Spillman, 2005; Thorpe et al., 2008): binary indicators for race/ethnicity (black vs. white) and 12 or more years of education and body mass index (BMI). We divide BMI into tertiles to capture potential nonlinearity in the relationship (cutpoints defined by the baseline analysis sample: lower = 25.3, upper = 30.2).
Analysis
After generating our physical challenge score using MCA, we estimate a generalized ordered logistic regression model (Williams, 2006) for our dependent variable in the overall sample at baseline, as well as separately within the three sample subsets (follow-up responders at baseline, follow-up nonresponders at baseline, and follow-up responders at the follow-up observation); that is, we estimate a series of cross-sectional models and not a repeated measures specification. In each case (i.e., separately for the overall sample and each of the sample subsets), we conduct a two-step process to build the most parsimonious specification, following Williams (2006). In the first step, we estimate the full model (i.e., including all independent variables and with the middle BMI tertile category as the reference group for BMI) without imposing the proportionality assumption across levels of the outcome for any of the coefficients. We use the estimates from this model to identify any variables with a significant (p < .05) deviation from proportionality across levels of the outcomes (as given by the “gamma” specification of the model; see Williams (2006, p. 10 and cites therein). We then estimate a final version of the model that leaves those variables with significant deviations from proportionality in the prior specification as unrestricted across levels of the outcome while imposing a proportionality constraint on the remaining coefficient estimates. Finally, we use a likelihood ratio (LR) χ2 test to evaluate the relative fit of the two specifications (and then against a fully constrained specification). We use Stata Statistical Software version 11.0 for all analyses (StataCorp, 2009), including the gologit2 procedure (Williams, 2006).
Results
Scoring of the Physical Environment Challenge Measure and Descriptive Statistics for All Variables
The MCA results for both baseline and follow-up are displayed in Figure 1, which show coordinates for the first two dimensions. We use only the first dimension to generate our physical environment challenge score (we do not use the second dimension). The first dimension captures the primary dimension of variability, reflecting 65.1% of the variance among women at baseline and 66% at follow-up, and separates the high from low physical challenge values for each of the three indicators: “low challenge” values lie to the left of the origin, whereas the “high challenge” values are plotted to the right. We note that the axis in both cases has been negated (i.e., we multiplied the estimated coordinates through by minus 1) to yield a score that increases in challenging features. Thus, larger values of the first dimension score signify greater challenge.
Figure 1.
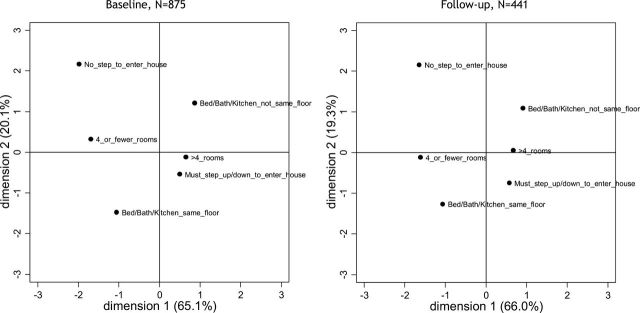
Plot of coordinates from the multiple correspondence analysis (MCA) of home physical environment challenge summary score component variables, baseline and follow-up. Coordinates are in standard normalization and the axes and scores were negated to define the score as “increasing” in challenge.
Table 1 shows that overall average age at baseline is about 78 years, average SPPB score is about 6.4 and average BMI 28.4, 28% of the sample is black and a little over a third have 12 or more years of education. At baseline, a quarter of the women report using at least one of the three types of ADs for mobility in the home. The sample is roughly split at baseline between women who do and do not live alone (and the physical challenge score is set to a mean of 0 by design). Several of the variables differ by follow-up responder status at baseline. Responders at baseline are, on average, younger and have better physical performance and higher BMI at baseline than nonresponders (p < .05 for each), with no significant differences in race/ethnicity or education. Fewer responders than nonresponders use AD for mobility in the home at baseline. There is no statistically significant difference at baseline between survivors and nonsurvivors in the proportion living alone, but responders on average tend to have home environments that are more physically challenging than those of nonresponders (average first dimension MCA score of 0.25 vs. −0.25, respectively; p < .05). Table 1 also provides summary information for the 441 women with complete data at follow-up, though we do not statistically test for differences from the preceding sample subsets. Average lower extremity physical performance fell somewhat over time within this subset, as did average BMI, but both are still higher than the respective nonresponder averages (at baseline). The frequency in AD use categories increased a bit as did the proportion of women living alone, whereas the average home physical environment became less challenging (but still somewhat more challenging than among the nonresponders at baseline).
Table 1.
Summary Information for Variables at Baseline and Follow-Up, Overall and by Follow-Up Responder Status
| At baseline | At follow-up | |||
|---|---|---|---|---|
| Overall sample (N = 875) | Follow-up responders, at baseline (n = 441) | Follow-up nonresponders, at baseline (n = 434) | Follow-up responders, at follow-up (n = 441) | |
| Dependent variables | ||||
| Summary indicator of indoor AD use (three categories); frequency, % of N b | ||||
| No AD (%) | 649 (74.17) | 369 (83.67) | 280 (64.52) | 344 (78.0) |
| Cane only (%) | 148 (16.91) | 55 (12.47) | 93 (21.43) | 67 (15.19) |
| Walker and/or wheelchair (with or without cane) (%)a | 78 (8.91) | 17 (3.85) | 61 (14.06) | 30 (6.8) |
| Independent variables | ||||
| Social challenge (lives alone vs w/spouse, relative, or nonrelative); frequency, % of n | ||||
| Low challenge (does not live alone) | 441 (50.4) | 233 (52.83) | 208 (47.93) | 227 (51.47) |
| High challenge (lives alone) | 434 (49.6) | 208 (47.17) | 226 (52.07) | 214 (48.53) |
| Physical challenge in the home environment—first dimension MCA scoreb | ||||
| Mean (SD) | 0 (2.42) | 0.25 (2.28) | −0.25 (2.54) | 0 (2.44) |
| Minimum/maximum | −4.73/2.01 | −4.73/2.01 | −4.73/2.01 | −4.32/2.16 |
| Physical performance score, SPPBb | ||||
| Mean (SD) | 6.38 (3.06) | 7.49 (2.73) | 5.25 (2.97) | 6.77 (3.21) |
| Minimum/maximum | 0/12 | 1/12 | 0/12 | 0/12 |
| Age at baselineb | ||||
| Mean (SD) | 78.16 (7.98) | 75.93 (7.17) | 80.42 (8.13) | — |
| Minimum/maximum | 65/101 | 65/95 | 66/101 | — |
| Race/ethnicity | ||||
| White (%) | 627 (71.66) | 323 (73.24) | 304 (70.05) | — |
| Black (%) | 248 (28.34) | 118 (26.76) | 130 (29.95) | — |
| Education | ||||
| Less than 12 years of education (%) | 565 (64.57) | 276 (62.59) | 289 (66.59) | — |
| 12 or more years of education (%) | 310 (35.43) | 165 (37.41) | 145 (33.41) | — |
| BMIb | ||||
| Mean (SD) | 28.44 (6.78) | 29.3 (6.53) | 27.57 (6.91) | 28.73 (6.66) |
| Minimum/maximum | 12.09/63.21 | 12.94/52.05 | 12.09/63.21 | 14.17/55.44 |
Notes: SPPB = short physical performance battery; BMI = body mass index; MCA = multiple correspondence analysis.
aWomen who are coded as using a walker and/or wheelchair in the home may or may not also use a cane.
bDenotes significant difference between follow-up responder and nonresponder sample subsets at baseline (p < .05), using a two-sample t test (for continuous variables) or χ2 test (for categorical variables).
Regression Model Results
Table 2 gives the regression model results for the overall sample, as well as for the follow-up responder and nonresponder subsets. We only present parameter estimates for the final specification of each model. As well, coefficient estimates that are held proportional (and thus are constant across outcome levels) are displayed only once (noted at the lower outcome level threshold, “no AD”). Coefficient estimates that are not held proportional are displayed for both outcome level thresholds.
Table 2.
Results From Generalized Ordered Logistic Regression Models Predicting Level of Assistive Device (AD) Use in the Home (no AD, cane only, or walker, and/or wheelchair with or without cane), Overall Analysis Sample, Follow-Up Responders and Nonresponder Subsamples at Baseline, and Follow-Up Responders at Follow-Up
| Overall sample, at baseline | Follow-up responders, at baseline | Follow-up nonresponders, at baseline | Follow-up responders, at follow-up | |
|---|---|---|---|---|
| Outcome level: no ADsa,b | ||||
| Social challenge (lives alone, vs. w/spouse, relative, or nonrelative) | 1.03 [0.69,1.54] | 1.86+ [0.93,3.70] | 0.75 [0.45,1.25] | 0.94 [0.51,1.75] |
| Physical challenge in the home environment—first dimension MCA score | 0.92* [0.85,0.99] | 0.84** [0.73,0.96] | 0.98 [0.89,1.08] | 0.88* [0.78,0.99] |
| Physical performance score, SPPB | 0.64*** [0.59,0.69] | 0.60*** [0.52,0.69] | 0.65*** [0.59,0.73] | 0.72*** [0.65,0.79] |
| Age at baseline | 1.03* [1.00,1.05] | 1.02 [0.98,1.07] | 1.03+ [1.00,1.06] | 1.09*** [1.05,1.14] |
| Black | 0.84 [0.57,1.25] | 0.83 [0.41,1.69] | 0.86 [0.53,1.39] | 1.49 [0.81,2.73] |
| 12 or more years of education | 1.14 [0.78,1.65] | 1.66 [0.88,3.11] | 0.91 [0.57,1.46] | 1.32 [0.76,2.30] |
| BMI bottom tertile | 1.05 [0.68,1.60] | 0.65 [0.29,1.46] | 1.27 [0.75,2.15] | 0.77 [0.40,1.48] |
| BMI top tertile | 1.54+ [1.00,2.38] | 1.38 [0.68,2.80] | 1.73+ [0.98,3.05] | 1.48 [0.76,2.88] |
| Outcome level: cane onlya,b | ||||
| Physical challenge in the home environment—first dimension MCA score | 1.03 [0.84,1.27] | 0.86* [0.77,0.97] | ||
| Physical performance score, SPPB | 0.54*** [0.47,0.61] | 0.47*** [0.36,0.61] | 0.56*** [0.47,0.66] | |
| Black | 0.085* [0.011,0.65] | |||
| Observations | 875 | 441 | 434 | 441 |
| Model Log likelihood | −495.9 | −170.2 | −311.6 | −217.9 |
| Model χ2 | 299.1 | 130.9 | 148.1 | 148.9 |
| Probability > χ 2 | p < .001 | p < .001 | p < .001 | p < .001 |
Notes: SPPB = short physical performance battery; BMI = body mass index; MCA = multiple correspondence analysis.
Coefficients are exponentiated to yield odds ratios and 95% confidence intervals are in brackets, OR [CI].
aThe highest category for the dependent variable is “walker and/or wheelchair use in the home, which may or may not also include cane use.”
bOnly parameter estimates that are unique across levels of the outcome are shown; parameters that are constrained to be equal across levels are shown once (for the lowest outcome level threshold, “No AD”).
+ p < .10. *p < .05. **p < .01. ***p < .001.
Overall Sample.
Column 2 of Table 2 shows that our final model for the overall sample assumes proportionality across levels of the outcome for all parameters except the SPPB (LR χ2 p = .42; relative to a model with all coefficient parameter estimates free to vary across outcome levels). Results for this model indicates that, controlling for the other variables included in the model, women living in more physically challenging home environments have 8% smaller odds (p < .05) of using a higher level of AD in the home. The coefficient estimate for our social environment challenge measure, living alone, is not significant. Our results also show that better physical performance is strongly, negatively associated with levels of AD use, and that this association is stronger at the higher threshold level of AD (36% and 46% lower odds of higher levels of AD use, respectively; p < .001 for both estimates).
Contrast of Findings Across Follow-Up Responder and Nonresponder Subsets.
The last three columns of Table 2 show results for the follow-up responder and nonresponder subsets at baseline (columns 3 and 4, respectively) and the responders at follow-up (column 5). We highlight two points. First, the modest inverse association between physical challenge and use of AD in the home is reasonably consistent across each subset and time point, though among baseline subsets our analyses identified nonproportionality in the associations across levels of AD use. Specifically, a significant inverse association (p < .05) was identified only at the lower outcome level threshold among follow-up responders at baseline (column 3), whereas a significant inverse association (p < .05) was identified only at the higher outcome threshold among nonresponders at baseline (column 4). Second, the sample subset analyses weakly suggest that the lack of an association between living alone and use of AD displayed in the overall sample may differ by follow-up responder status. At baseline, responders who live alone have a higher odds (OR = 1.86, p < .10) of using a greater level of AD in the home relative to women who do not live alone, whereas nonresponders who live alone have no significant difference in the use of AD. The estimate in the rightmost column in Table 2 shows no significant association among responders at follow-up. We do not provide detailed interpretations for the other control variables in the model, except to note that the nonproportional and extreme coefficient estimate for the variable Black at the higher AD use threshold (in column 5) is based on sparse data in the relevant cells.
Discussion
We provide estimates of the cross-sectional association between challenge in the home environment and use of AD for mobility in the home, controlling for lower extremity physical performance and other factors. We describe these associations in a baseline sample of moderately to severely disabled women and also explore these associations within subsets of women who ultimately will and will not survive to and participate in the 3-year follow-up observation.
Our results suggest that, on average, the presence of greater physical challenges in the home environment is associated with lower levels of AD use, independent of physical competence (SPPB), social challenge (living alone), and other factors. We obtain similar results across the subsets defined by follow-up responder status (with minor variability). We find no significant association neither between social challenge in the home and AD use in the overall sample nor between two of the three subsets; the association was positive and weakly significant only among follow-up responders at baseline, though the direction of this association is consistent with prior findings (Spillman, 2005). However, our results also may weakly suggest that the positive association may fade within person over time (i.e., among responders at follow-up). Thus, perhaps the myriad factors underlying survival and participation (net of physical performance and the other variables included in our models) may affect the mechanisms through which older women use AD—particularly those associated with coresidence.
Lower extremity physical performance was also consistently, inversely associated with AD use and, furthermore, the association was stronger across the greater AD use threshold. It is important to note that at better levels of physical performance fewer women use AD (see the cross-tabulation between these two variables at baseline in Supplementary Table 1). In order to ensure that our findings do not reflect model extrapolation where AD is not used, we reestimated our final models on a subset of the data restricted to women with a physical performance score less than or equal to seven (n = 525 for the overall sample). As indicated by the results shown in Supplementary Table 2, our central findings are essentially unaffected.
Although our results may differ from those by Ganesh and colleagues (2011) and Hoenig and colleagues (2006) who also examine the WHAS I baseline, these analyses are not directly comparable to ours because these articles focus on composites of multiple compensatory strategies (although each analysis uses some of the same underlying variables, e.g., living alone and environment barriers). Hoenig and colleagues (2006) found that those with barriers in the home have a greater odds of using “any” compensatory strategy, as did the analysis by Ganesh and colleagues (2011), depending on what other variables were included. With regard to social challenge, both studies find that living with someone is associated with greater odds of using personal assistance relative to AD only (i.e., it affects the type of compensatory strategy among those who use them). More generally, however, within the context of prior findings in the literature, we suggest that our results serve to highlight the complexity of the interaction between people and their environments.
Our study, like others, has a number of limitations. First and foremost, as we have discussed earlier, our results are descriptive and do not identify causal relationships. We do not address the myriad choices related to use of AD in general, or of a particular type of device, as well as the environments in which women live at the time they are observed. This leaves open many issues, including the role of selection into living environments. For example, a question that might be suggested by our observation (Table 1) that average home environment physical challenge among responders at baseline was higher than among nonresponders is perhaps healthier women chose to live in more challenging environments? As well, how might environments, in turn, affect function (which may also be affected by AD use)? Thus, it would be inappropriate to infer from this study any causal relationships between home environment challenge and health or function. These complex, potentially bidirectional relationships are beyond our descriptive aims but comprise very important directions for future work (e.g., see Seplaki, 2002, for an exploration of some of these issues). Investigations into such questions may hypothesize, for example, that some degree of challenge in the home may reduce the need for AD use in the future (e.g., see the review by Wahl, Fänge, Oswald, Gitlin, & Iwarsson, 2009, on associations between home environment and disability outcomes). To illustrate, perhaps having to step up to enter the house is a kind of limited activity that increases lower leg strength over time; this would be consistent with research in other contexts suggesting that relatively low levels of physical activity may be beneficial (Wen et al., 2011).
A second limitation is that our sample included only moderately to severely disabled women, and in a single geographic area. This, therefore, implies a focus on a particular phase of disablement (Verbrugge & Jette, 1994).
Third, the measure of our dependent variable (AD use in the home) is fairly crude; however, although we are limited to the measures available to us, we did explore other categorizations and concluded that the chosen delineation represented a good combination of substance and reliability.
Similarly, we had only three variables with which to characterize physical challenges in the home environments (e.g., see Gitlin et al., 2002, Iwarsson et al., 2007, or Seplaki, 2002, for more comprehensive approaches) and even these aspects are multifaceted. For example, Oswald, Jopp, Rott, and Wahl (2011) present evidence that the number of rooms can serve a positive role or a negative role among young-old versus old-old, respectively.
Finally, we cannot assess the role of cognitive impairment in these associations because the sample was screened to be cognitively intact at baseline (Kasper et al., 1999).
There are also many additional interesting and important issues to explore but those are beyond the scope of the present analysis. We neither address the role of formal care nor the intensity of AD use (i.e., how often a particular device is used). In addition, there are issues surrounding the use of AD in the context of compensatory strategies more generally. For example, the findings by Hoenig and colleagues (2006) highlight that the use of AD is commonly accompanied by behavioral changes, too, as well as in conjunction with human help. It is also possible that living alone may actually be less challenging than a situation in which a participant lives with a spouse for whom they care. Thus, we again emphasize that home environments are a context of complex and multilayered interactions (Rowles et al., 2004; Wahl et al., 2012).
Our analysis also has a number of strengths. Our approach of examining the association cross-sectionally, first overall and then within subsets of responders and nonresponders and across time among follow-up responders allows us to parsimoniously control for selection bias over time due to factors associated with survival and participation. At the same time, with this approach (e.g., as opposed to a repeated measures analysis), we also hope to emphasize caution against inappropriate causal interpretation of our findings. Our goal here has been to provide an initial set of descriptive estimates for the cross-sectional association between environment and AD use, controlling for physical performance and other factors.
We also use a flexible parametric model for ordered categorical-dependent variables, and we develop a score for home environment challenge from a small list of discrete measures using a multivariate method. Finally, our analysis provides a focus on an important and complex element of compensatory strategies, the use of AD. Hoenig and colleagues point out that their analysis does not allow for differentiation among the type of compensatory strategy, and they urge future studies to, “examine which compensatory strategies are most effective in which circumstances” (Hoenig et al., 2006, p. 267).
In this article, we made the decision to constrain our application of the Lawton and Nahemow (1973) framework which, although it provides a useful lens for thinking about the issues at hand, is very complex, posits causal relationships, and includes dimensions that are challenging to measure. We choose to explore “first principles” in this domain with a descriptive, cross-sectional analysis. Future work will need to continue to elucidate these complex relationships.
Our findings provide some preliminary evidence that the physical challenges of the home may be an important area to target in the development of future interventions geared toward enhancing the ability of aging cohorts to remain in their homes as they age. New cohorts that are better educated and more receptive to the independent use of technology as a solution to functional needs provide an opportunity for medical professionals to incorporate home environment evaluations as a tool to improve safety and functioning among elders and perhaps help to provide additional evidence of their value to payers (Gitlin, Jacobs, & Earland, 2010). Thus, future analyses should explore these relationships in order to identify the mechanisms that drive them and, in turn, how we can develop opportunities for coming generations of elders to live successfully in the community.
Supplementary Material
Supplementary material can be found at: http://gerontologist.oxfordjournals.org.
Funding
This work was supported by the National Institutes of Health (K01AG031332 to C. L. Seplaki and R37AG19905 to L. P. Fried).
Supplementary Material
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health. An early version of this work was presented on November 17, 2006 at the Annual Meeting of the Gerontological Society of America in Dallas, TX. We are grateful to two anonymous referees for their helpful comments on the manuscript.
References
- Agree E. M. (1999). The influence of personal care and assistive devices on the measurement of disability. Social Science & Medicine (1982), 48, 427–443 [DOI] [PubMed] [Google Scholar]
- Agree E. M., Freedman V. A. (2000). Incorporating assistive devices into community-based long-term care: An analysis of the potential for substitution and supplementation. Journal of Aging and Health, 12, 426–450 [DOI] [PubMed] [Google Scholar]
- Agree E. M., Freedman V. A., Sengupta M. (2004). Factors influencing the use of mobility technology in community-based long-term care. Journal of Aging and Health, 16, 267–307 [DOI] [PubMed] [Google Scholar]
- Agree E., Hughes M. E. (2012). Demography of families in later life. In Blieszner R., Bedford V. H. (Eds.), Handbook of families and aging, (2nd ed., pp. 9–34). Santa Barbara, CA: Praeger; [Google Scholar]
- Crystal S. (2007). Population aging and benefit sustainability: The impact of baby boomer aging on the health care system. In Schaie K. W., Uhlenberg P. (Eds.), Social structures, demographic changes and the well-being of older persons, societal impact on aging series, (pp. 52–70). New York: Springer Publishing Company; [Google Scholar]
- Freedman V. A. (2009). Adopting the ICF language for studying late-life disability: A field of dreams? Journal of Gerontology: Medical Sciences, 64, M1172–M1174; discussion 1175. 10.1093/gerona/glp095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman V. A., Agree E. M., Martin L. G., Cornman J. C. (2006). Trends in the use of assistive technology and personal care for late-life disability, 1992-2001. Gerontologist, 46, 124–127 [DOI] [PubMed] [Google Scholar]
- Freedman V. A., Schoeni R. F., Martin L. G., Cornman J. C. (2007). Chronic conditions and the decline in late-life disability. Demography, 44, 459–477 [DOI] [PubMed] [Google Scholar]
- Ganesh S. P., Fried L. P., Taylor D. H., Jr, Pieper C. F., Hoenig H. M. (2011). Lower extremity physical performance, self-reported mobility difficulty, and use of compensatory strategies for mobility by elderly women. Archives of Physical Medicine and Rehabilitation, 92, 228–235. 10.1016/j.apmr.2010.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin L. N., Jacobs M., Earland T. V. (2010). Translation of a dementia caregiver intervention for delivery in homecare as a reimbursable Medicare service: Outcomes and lessons learned. Gerontologist, 50, 847–854. 10.1093/geront/gnq057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin L. N., Schinfeld S., Winter L., Corcoran M., Boyce A. A., Hauck W. (2002). Evaluating home environments of persons with dementia: Interrater reliability and validity of the Home Environmental Assessment Protocol (HEAP). Disability and Rehabilitation, 24, 59–71 [DOI] [PubMed] [Google Scholar]
- Greenacre M. J. (2007). Correspondence analysis in practice, (2nd ed.). Boca Raton, FL: Chapman & Hall/CRC; [Google Scholar]
- Guralnik J. M., Fried L. P., Simonsick E. M., Kasper J. D., Lafferty M. E. (Eds.). (1995). The women’s health and aging study: Health and social characteristics of older women with disability, Bethesda, MD: National Institute on Aging; NIH Pub. No. 95–4009. Retrieved from www.grc.nia.nih.gov/branches/ledb/whasbook/title.htm [Google Scholar]
- Guralnik J. M., Simonsick E. M., Ferrucci L., Glynn R. J., Berkman L. F., Blazer D. G., et al. (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology: Medical Sciences, 49, M85–M94 [DOI] [PubMed] [Google Scholar]
- Hoenig H., Ganesh S. P., Taylor D. H., Jr, Pieper C., Guralnik J., Fried L. P. (2006). Lower extremity physical performance and use of compensatory strategies for mobility. Journal of the American Geriatrics Society, 54, 262–269 [DOI] [PubMed] [Google Scholar]
- Hoenig H., Giacobbi P., Levy C. E. (2007). Methodological challenges confronting researchers of wheeled mobility aids and other assistive technologies. Disability and Rehabilitation. Assistive Technology, 2, 159–168 [DOI] [PubMed] [Google Scholar]
- Hughes M. E., Waite L. J. (2007). The aging of the second demographic transition. In Schaie K.W., Uhlenberg P. (Eds.), Social structures: The impact of demographic changes on the well-being of older persons, (pp. 179–211). New York: Springer [Google Scholar]
- IOM. (1991). Disability in America: Toward a national agenda for prevention. Washington, DC: National Academy Press; [Google Scholar]
- IOM (2007). The future of disability in America. Washington, DC: National Academy Press; [Google Scholar]
- Iwarsson S., Wahl H. W., Nygren C., Oswald F., Sixsmith A., Sixsmith J., et al. (2007). Importance of the home environment for healthy aging: Conceptual and methodological background of the European ENABLE-AGE Project. Gerontologist, 47, 78–84 [DOI] [PubMed] [Google Scholar]
- Kasper J. D., Shapiro S., Guralnik J. M., Bandeen-Roche K. J., Fried L. P. (1999). Designing a community study of moderately to severely disabled older women: The Women’s Health and Aging Study. Annals of Epidemiology, 9, 498–507 [DOI] [PubMed] [Google Scholar]
- Lawton M. P. (1998). Chapter 1: Environment and aging: Theory revisited. In Scheidt R. J., Windley P. G. (Eds.), Environment and aging theory: A focus on housing, (pp. 1–31). Westport, CT: Greenwood Press; [Google Scholar]
- Lawton M. P., Nahemow L. (1973). Ecology and the aging process. In Eisdorfer C., Lawton M. P. (Eds.), The psychology of adult development and aging, (pp. 619–674). Washington DC: American Psychological Association; [Google Scholar]
- Oswald F., Jopp D., Rott C., Wahl H. W. (2011). Is aging in place a resource for or risk to life satisfaction? Gerontologist, 51, 238–250. 10.1093/geront/gnq096 [DOI] [PubMed] [Google Scholar]
- Pressler K. A., Ferraro K. F. (2010). Assistive device use as a dynamic acquisition process in later life. Gerontologist, 50, 371–381. 10.1093/ geront/gnp170 [DOI] [PubMed] [Google Scholar]
- Rowles G. D., Oswald F., Hunter E. G. (2004). Interior living environments in old age. In Wahl H.-W., Scheidt R., Windley P. G. (Eds.), Annual review of gerontology and geriatrics (aging in context: socio-physical environments), (pp. 167–193). New York: Springer Publishing Company; [Google Scholar]
- Scheidt R. J., Norris-Baker C. (2004). The general ecological model revisited: Evolution, current status, and continuing challenges. In Wahl H.-W., Scheidt R. J., Windley P. G. (Eds.), Annual review of gerontology and geriatrics (aging in context: socio-physical environments), (pp. 59–84). New York: Springer Publishing Company; [Google Scholar]
- Schoeni R. F., Freedman V. A., Martin L. G. (2008). Why is late-life disability declining? Milbank Quarterly, 86, 47–89. 10.1111/ j.1468-0009.2007.00513.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seplaki C. L. (2002). The measurement and dynamic analysis of elderly living environment transitions and outcomes.Unpublished doctoral dissertation, University of Wisconsin-Madison. Retrieved from http://forward.library.wisconsin.edu/catalog/ocm51464057
- Simonsick E. M., Maffeo C. E., Rogers S. K., Skinner E. A., Davis D., Guralnik J. M., Fried L. P. (1997). Methodology and feasibility of a home-based examination in disabled older women: The Women’s Health and Aging Study. Journal of Gerontology: Medical Sciences, 52, M264–M274 [DOI] [PubMed] [Google Scholar]
- Spillman B. C. (2005). Assistive device use among the elderly: Trends, characteristics of users, and implications for modeling. Washington, DC: The Urban Institute under contract from the Office of Disability Aging and Long-Term Care Policy, Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; [Google Scholar]
- StataCorp. (2009). Stata statistical software: Release 11. College Station, TX: StataCorp LP; [Google Scholar]
- Thorpe R. J., Jr, Kasper J. D., Szanton S. L., Frick K. D., Fried L. P., Simonsick E. M. (2008). Relationship of race and poverty to lower extremity function and decline: Findings from the Women’s Health and Aging Study. Social Science & Medicine, 66, 811–821. 10.1016/j.socscimed.2007.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge L. M., Jette A. M. (1994). The disablement process. Social Science & Medicine, 38, 1–14 [DOI] [PubMed] [Google Scholar]
- Wahl H. W., Fänge A., Oswald F., Gitlin L. N., Iwarsson S. (2009). The home environment and disability-related outcomes in aging individuals: What is the empirical evidence? Gerontologist, 49, 355–367. 10.1093/geront/gnp056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl H. W., Iwarsson S., Oswald F. (2012). Aging well and the environment: Toward an integrative model and research agenda for the future. Gerontologist, 52, 306–316. 10.1093/geront/gnr154 [DOI] [PubMed] [Google Scholar]
- Wahl H. W., Weisman G. D. (2003). Environmental gerontology at the beginning of the new millennium: Reflections on its historical, empirical, and theoretical development. Gerontologist, 43, 616–627 [DOI] [PubMed] [Google Scholar]
- Weiss C. O., Hoenig H. M., Fried L. P. (2007). Compensatory strategies used by older adults facing mobility disability. Archives of Physical Medicine and Rehabilitation, 88, 1217–1220 [DOI] [PubMed] [Google Scholar]
- Wen C. P., Wai J. P., Tsai M. K., Yang Y. C., Cheng T. Y., Lee M. C., et al. (2011). Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. Lancet, 378, 1244–1253. 10.1016/S0140-6736(11)60749-6 [DOI] [PubMed] [Google Scholar]
- Williams R. (2006). Generalized ordered logit/partial proportional odds models for ordinal dependent variables. The Stata Journal, 6, 58–82 A pre-publication version is available at http://www.nd.edu/~rwilliam/gologit2/gologit2.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


