Abstract
To improve cancer pain management, the Medical Oncology Department of Sun Yat-sen University Cancer Center (SYSUCC) launched the Good Pain Management (GPM) Ward Program, which has been recognized by the Chinese Ministry of Health and promoted throughout the nation. This retrospective case-control study was designed to evaluate the effectiveness of the program. Patients diagnosed with malignant solid tumors with bone metastasis were eligible. Patients who were admitted 6 months before the initiation of the GPM program were used as the control group, and patients admitted 6 months after the initiation of the program were used as the GPM group. The pain-reporting rate and pain management index (PMI) were calculated. The pain levels before and after pain management were compared. A total of 475 patients (244 in the control group and 231 in the GPM group) were analyzed. The pain-reporting rate of the GPM group was significantly higher than that of the control group (62.8% vs. 37.7%, P < 0.001). The PMI of the GPM group was significantly higher than that of the control group (0.083 vs. -0.261, P < 0.001). Therefore, the GPM Ward Program improved the pain management of cancer patients and provided experience for improving cancer pain management in the future.
Keywords: Good pain management, cancer pain management, pain-reporting rate, pain management index
As a fearful and burdensome symptom, pain widely exists in cancer patients[1]. Cancer pain has many negative effects, which lead to a decrease in the quality of life[2]. Therefore, cancer pain management has been considered to be increasingly important throughout the world. However, there is still not enough attention being drawn to it. Two studies published in the Journal of Clinical Oncology (JCO) indicated that an appropriate understanding of pain importance, cancer pain evaluation, and correct pain treatment was still lacking[3],[4].
Cancer pain treatment was gradually standardized in China after the Ministry of Health launched the Chinese version of the World Health Organization (WHO) cancer three-step analgesic ladder guidelines and the corresponding clinical guidelines in 1993[5]–[7]. Before the guidelines were introduced, pain control in China was poor. A survey conducted from 1991 to 1992 indicated that 67% of cancer patients had not received adequate pain treatment [8]. However, after the standardization of cancer pain treatment, there were still 41.3% to 52.9% of patients who were prescribed inadequate analgesics or not satisfied with pain treatment[9]–[11]. On the other hand, morphine consumption per capita in China in 1993 was only 0.01 mg, but this figure was 66.53 mg in Denmark and 20.80 mg in the United States[12]. After the WHO's three-step ladder for cancer pain treatment was promoted nationwide, the consumption of morphine increased significantly. However, the average consumption still lags far behind that in other developed countries [13].
There were several reasons for ineffective pain control in China. First, patients' misconceptions about pain and analgesics led to over-concern about the adverse effects and addictive properties of analgesics, reluctance to report pain, and resistance to opioid analgesics. Second, due to a lack of personalized pain control knowledge, some medical staff could not appropriately manage pain. Third, some local hospital policies for regulating narcotics might restrict the use of opioid analgesics[10], [14]–[18].
To improve pain management, we developed the Good Pain Management (GPM) Ward Program in the Medical Oncology Department of the Sun Yat-sen University Cancer Center (SYSUCC)on April 13th, 2009. The program has been recognized by the Chinese Ministry of Health and promoted throughout the nation since March 2011[19].
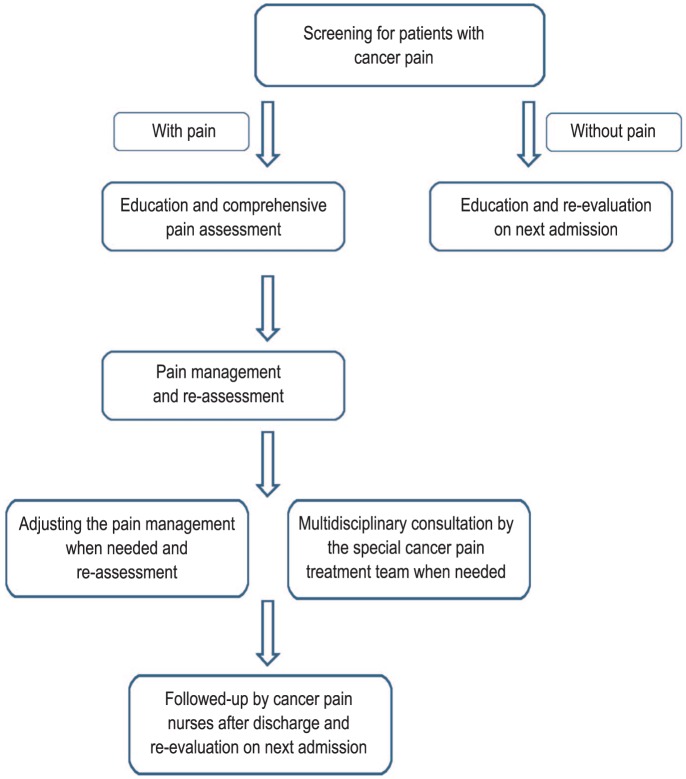
The GPM Ward Program mainly involved four aspects. First, training and education for cancer pain treatment. For the medical staff (mainly physicians and nurses) of the GPM Ward, training in standardized cancer pain management according to the WHO and National Comprehensive Cancer Network (NCCN) guidelines was conducted every month. Moreover, a patient education system was set up. Posters about cancer pain and pain management were placed on the walls of every GPM Ward. Courses on pain knowledge were delivered once a month, and educational booklets were also issued to encourage the patients to pay more attention to cancer pain as well as dispel their misunderstanding of pain treatment. Second, good pain management in daily practice. In the GPM Ward, a pain assessment scale was posted at the patient's bed-side to assist the patient and medical staff in dynamically assessing pain. Every participating hospital established a special cancer pain treatment team, which included professional cancer pain managing physicians, surgeons, anesthetists, radiologists, nurses, and pharmacists. The team was responsible for supervising cancer pain treatment as well as providing advice on comprehensive pain management for difficult cases. Figure 1 illustrates the flowchart of pain management. Third, analgesic drug administration and supplement. The Department of Pharmacy was required to prepare at least 3 different types of opioid analgesics at two different doses, including both short-acting and extended release formulations. For patients with cancer pain, 15 daily doses of extended release opioid analgesics were available for every single prescription. These policies were created to increase the accessibility of opioid analgesics and promote their appropriate use by medical staff. Forth, follow-up and external evaluation system. After discharge from the hospital, patients with pain would be asked to keep a diary about pain intensity, analgesic drug taking, and adverse events. The patients were followed up through telephone by cancer pain management nurses. Moreover, according to the regulations of Ministry of Health, a group of experts on cancer pain management was formed to supervise the performance of the participating hospitals and to provide feedback to improve the program. Additionally, the program planned to build 150 GPM Wards throughout the country within 3 years.
Figure 1. Flowchart of pain management in the Good Pain Management (GPM) Ward Program.
The purpose of this study was to evaluate the improvement of cancer pain management in the Medical Oncology Department of SYSUCC. The following hypothesis was tested: the GPM Ward Program could encourage the patients and medical staff to pay more attention to cancer pain, improve the pain control skills of medical staff, and lead to better pain management.
Patients and Methods
Patient enrollment
This investigation was a retrospective case-control study. The independent ethics committee of SYSUCC approved this study. Patient eligibility included a pathologic diagnosis of malignant solid tumor, being newly diagnosed with bone metastasis by radiologic examinations [computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography/computed tomography (PET/CT)], and being admitted to the Medical Oncology Department of SYSUCC.
The eligible patients who were admitted 6 months before the initiation of the program (between October 13th, 2008 and April 12th, 2009) were used as the control group, and the eligible patients who were admitted 6 months after the initiation of the program (between April 13th, 2009 and October 12th, 2009) were used as the GPM group. Only patients diagnosed with a malignant solid tumor with bone metastases were enrolled to reduce the bias introduced by disease heterogeneity. All sample data were obtained from the medical records or the hospital information system.
Cancer pain management and assessment
Patients who had not received any anticancer therapy were defined as previously untreated cases, other patients were defined as treated cases. Patients who had more than 3 metastatic bone lesions were defined as multiple bone metastatic cases, and other patients were defined as non-multiple bone metastatic cases. The levels of alkaline phosphatase or lactic dehydrogenase that were higher than the upper limit of the normal range were considered abnormal. The pain levels were classified as none (0), mild (1-3), moderate (4-6), and severe (7-10), based on a numerical rating scale (NRS)[20], [21].
The pain-reporting rate was the proportion of patients who reported pain on admission after being diagnosed with bone metastasis. The pain management index (PMI) was used to evaluate the adequacy of pain treatment[22]. The pain level was subtracted from the analgesic level to produce the PMI score, which ranged from -3 (severe pain receiving no analgesic drugs) to +3 (receiving enough analgesic drugs and reporting no pain). A negative PMI was an indicator of inadequate analgesic drugs, and positive scores represented acceptable treatment. The pain level after pain management was also recorded if the patient reported pain on admission. The pain levels were compared before and after pain management to evaluate the effectiveness of the pain treatment.
Statistical analysis
SPSS for Windows software (version 19.0, IBM) was used for all data analyses. The normality of the quantitative variables was analyzed by the Shapiro-Wilk test. Quantitative variables with a normal distribution were analyzed by the independent-sample t test. Quantitative variables departing from a normal distribution were analyzed by the Mann-Whitney U test. Pearson's χ2 test and McNemar's exact test were used to test the differences in the distribution of categorical variables where appropriate. All significance levels refer to two-sided tests. A P value of < 0.05 was considered significant.
Results
Patient demographics
A total of 475 patients (244 in the control group and 231 in the GPM group) were analyzed in this study. The demographic and disease characteristics of the patients are summarized in Table 1. No significant difference was found in any demographic or disease characteristics between the two groups.
Table 1. Demographics and disease characteristics of the 475 cancer patients.
| Characteristic | Control group [cases (%)] | GPM group [cases (%)] | P |
| Total | 244 | 231 | |
| Sex | 0.546 | ||
| Male | 144 (59.0) | 130 (56.3) | |
| Female | 100 (41.0) | 101 (43.7) | |
| Median age (years) | 51 | 52 | 0.407 |
| Diagnosis | 0.741 | ||
| Lung cancer | 128 (52.4) | 115 (49.8) | |
| Nasopharyngeal carcinoma | 41 (16.8) | 38 (16.4) | |
| Breast cancer | 42 (17.2) | 49 (21.2) | |
| Others | 33 (13.5) | 29 (12.6) | |
| ECOG PS score | 0.433 | ||
| 0 | 14 (5.7) | 19 (8.2) | |
| 1 | 179 (73.4) | 171 (74.0) | |
| 2 | 51 (20.9) | 41 (17.7) | |
| Previous anticancer therapy | 0.466 | ||
| Untreated | 137 (56.1) | 122 (52.8) | |
| Treated | 107 (43.8) | 109 (47.2) | |
| Bone metastatic lesions | 0.135 | ||
| Multiple | 168 (68.8) | 144 (62.3) | |
| Non-multiple | 76 (31.1) | 87 (37.7) | |
| ALP level | 0.212 | ||
| Normal | 95 (38.9) | 103 (44.6) | |
| Abnormal | 149 (61.1) | 128 (55.4) | |
| LDH level | 0.175 | ||
| Normal | 99 (40.6) | 108 (46.8) | |
| Abnormal | 145 (59.4) | 123 (53.2) |
GPM, the Good Pain Management Ward Program; ECOG PS, Eastern Cooperative Oncology Group performance status; ALP, alkaline phosphatase; LDH, lactate dehydrogenase.
Characteristics of pain on first admission
The pain levels of the patients in the control and GPM groups on admission are summarized in Table 2. At admission, the pain-reporting rate was significantly higher in the GPM group than in the control group (62.8% vs. 37.7%, P< 0.001), and the proportion of mild pain was also significantly higher in the GPM group than in the control group (32.4% vs. 16.3%, P = 0.006).
Table 2. Pain characteristics of the 475 cancer patients on admission.
| Pain level | Control group [cases (%)] | GPM group [cases (%)] |
| No | 152 (62.3) | 86 (37.2) |
| Mild | 15 (6.1) | 47 (20.3) |
| Moderate | 56 (23.0) | 72 (31.2) |
| Severe | 21 (8.6) | 26 (11.2) |
| Total | 244 (100) | 231 (100) |
Analgesic administration
The analgesics prescribed for pain management are summarized in Table 3. For the patients with mild pain, the non-analgesic treatment rate was lower in the GPM group than in the control group (21.3% vs. 46.7%, P = 0.055). For the patients with moderate pain, the strong opioid treatment rate was significantly higher in the GPM group than in the control group (44.4% vs. 16.1%, P = 0.010).
Table 3. Analgesics prescribed for the 475 cancer patients.
| Analgesicsprescribed | Pain level on admission [cases (%)] |
|||||||
| Control group |
GPM |
|||||||
| Mild | Moderate | Severe | Total | Mild | Moderate | Severe | Total | |
| No analgesic | 7 (46.7) | 5 (8.9) | 0 (0.0) | 12 (13.0) | 10 (21.3) | 4 (5.6) | 0 (0.0) | 14 (9.7) |
| Non-opioid | 7 (46.7) | 11 (19.6) | 1 (4.8) | 19 (20.7) | 33 (70.2) | 3 (4.2) | 0 (0.0) | 36 (24.8) |
| Weak opioid | 1 (6.7) | 31 (55.4) | 4 (19.0) | 36 (39.1) | 4 (8.5) | 33 (45.8) | 3 (11.5) | 40 (27.6) |
| Strong opioid | 0 (0.0) | 9 (16.1) | 16 (76.2) | 25 (27.2) | 0 (0.0) | 32 (44.4) | 23 (88.5) | 55 (37.9) |
| Total | 15 (16.3) | 56 (60.9) | 21 (22.8) | 92 | 47 (32.4) | 72 (49.7) | 26 (17.9) | 145 |
The mean PMI score for the GPM group was significantly higher than that for the control group (0.083 vs. -0.261, P < 0.001). The negative PMI rate (inadequate pain treatment rate) in the GPM group was significantly lower than that in the control group [13.8% (20/145) vs. 30.4% (28/92), P = 0.002].
Characteristics of the co-interventions
The co-interventions for pain management in both groups are shown in Table 4. No significant differences were found between the two groups in the percentage of patients who received bisphosphonates, radiotherapy, or non-steroidal anti-inflammatory drugs (NSAIDs) with concomitant opioid treatment.
Table 4. Co-intervention rate for pain management.
| Intervention | Control group (%) | GPM group (%) | P |
| Bisphosphonates | 53.3 | 50.3 | 0.662 |
| Radiotherapy | 5.4 | 2.8 | 0.294 |
| NSAIDs | 59.0 | 63.2 | 0.604 |
NSAIDs, non-steroidal anti-inflammatory drugs.
Effectiveness of pain treatment
The pain levels after pain management were recorded for the patients who reported pain on admission and are listed in Table 5. The pain levels before and after pain management were compared to analyze the effectiveness of the pain treatment.
Table 5. Pain characteristics of the cancer patients after pain management.
| Pain level before treatment | Pain level after treatment [cases (%)] |
|||||||||
| Control group |
GPM group |
|||||||||
| None | Mild | Moderate | Severe | Total | None | Mild | Moderate | Severe | Total | |
| Mild | 10(66.7) | 4(26.7) | 1(6.7) | 0(0.0) | 15(16.3) | 39(83.0) | 6(12.8) | 2(4.2) | 0(0.0) | 47(32.4) |
| Moderate | 16(28.6) | 19(33.9) | 19(33.9) | 2(3.6) | 56(60.9) | 32(44.4) | 30(41.7) | 9(12.5) | 1(1.4) | 72(49.7) |
| Severe | 5(23.8) | 8(38.1) | 5(23.8) | 3(14.3) | 21(22.8) | 8(30.8) | 11(42.3) | 5(19.2) | 2(7.7) | 26(17.9) |
| Total | 31(33.7) | 31(33.7) | 25(27.2) | 5(5.4) | 92 | 79(54.5) | 47(32.4) | 16(11.0) | 3(2.1) | 145 |
The complete remission (pain level decreased to none) rate of pain in the GPM group was significantly higher than that in the control group [54.5% (79/145) vs. 33.7% (31/92), P = 0.002]. The remission rate of moderate to severe pain patients (decreased to mild or none) in the GPM group was significantly higher than that in the control group [82.6% (81/98) vs. 62.3% (48/77), P = 0.002]. The uncontrolled pain rate (the same or severer pain after pain treatment) in the GPM group was significantly lower than that in the control group [13.8% (20/145) vs. 31.5% (29/92), P = 0.001].
Discussion
In this study, we found that after the GPM Program initiation, the pain-reporting rate was elevated significantly, as patients with mild pain were especially willing to report pain symptoms. The analgesic treatments were more frequently administered, especially strong opioids for moderate and severe pain. The PMI after the GPM Program initiation was positive, which indicated better cancer pain management. The patients' reported outcomes were significantly ameliorated, as the complete pain remission rate was higher after the GPM Program initiation.
Cancer pain management remains a serious problem throughout the world. Pain screening is the first step to manage cancer patient pain. In patients with advanced/metastatic/terminal disease, a systemic review reported that 64% of patients would experience pain[23]. In China, a nationwide survey conducted in 29 provinces, which included 1,555 patients, revealed that cancer-related pain had occurred in 61.6% of the patients, and for advanced cancer patients, the prevalence of pain was as high as 70% to 85%[24]. Moreover, cancer patients with bone metastases often suffered from significant pain. It has been reported that two-thirds of patients with bone metastases would experience pain[25]–[27].
However, in our study the pain-reporting rate on admission for the control group was only 37.7%, which was much lower than the data reported by previous studies[23]–[27]. Additionally, all the demographic and disease characteristics were comparable between the control and GPM groups, but the pain-reporting rate increased significantly to 62.8% in the GPM group. Furthermore, the proportion of patients who reported mild pain in the control group was also significantly lower than that in the GPM group (16.3% vs. 32.4%, P = 0.006). Therefore, it is reasonable to believe that some patients in the control group suffered from pain without reporting it, especially when the pain was not severe. The GPM Program encouraged patients to pay more attention to pain and report the pain, even when it was mild.
Despite established pain treatment guidelines, there are still many cancer patients who do not receive adequate pain treatment. A landmark study conducted by the Eastern Cooperative Oncology Group (ECOG) in 1994 has shown that 42% of 1,308 patients in outpatient oncology care had inadequate analgesic prescribed[22]. The results of the ECOG study and other studies led to an increased attention to the pain management of cancer patients. Nevertheless, a recent prospective observational study of pain and analgesic administration in medical oncology outpatients with solid tumors showed that of 2,026 patients having reported pain or requiring analgesics at the initial assessment, 33% were still receiving inadequate analgesics[3].
In our study, the mean PMI value was negative in the control group (mean, -0.261; median, 0; and range, -2 to 1). According to the PMI value, 30.4% of the patients in the control group received inadequate pain treatment. Considering that some patients in the control group suffered from pain without reporting it and did not receive any pain management, this problem could be worse. However, in the GPM group, the mean PMI value was significantly higher and above 0 (mean, 0.083; median, 0; and range, -2 to 1), and the proportion of under-treatment decreased to 13.8%. Moreover, it was worthwhile to note that the proportion of patients receiving strong opioids for moderate pain in the GPM group was significantly higher than that in the control group (44.4% vs. 16.1%, P = 0.001). The GPM Program encouraged the clinicians to pay more attention to patient pain, improved their skills of appropriate analgesic administration, and emboldened them to use strong opioids more actively.
Comprehensive treatment, including bisphosphonates, radiotherapy, NSAIDs, and corticosteroids, was also essential for good pain management[28]–[30]. However, in our study, only about half of the patients in both groups (53.3% in the control group and 50.3% in the GPM group) had bisphosphonates prescribed. Palliative radiotherapy for bone pain was also used less frequently in both groups (5 patients in the control group and 4 in the GPM group). Additionally, NSAIDs were prescribed for only 59.0% of the patients in the control group and 63.2% in the GPM group. The relatively low usage of these three co-interventions might also contribute to the current pain management status in China, and it needs to be improved in the future.
The pain levels before and after pain management were compared to analyze the effectiveness of the pain treatment. The results implied that the pain management of the GPM group was significantly improved compared with the control group. In the present study, the use of bisphosphonates, radiotherapy, and NSAIDs was comparable between the control and GPM groups. Therefore, more attention being paid to the pain by both the patients and clinicians and the improved skills of appropriate opioid analgesic administration by the clinicians may account for these results.
There were several limitations of this study. First, this investigation was a retrospective case-control study. Second, the study was conducted in a single center with a limited number of patients. In addition, the patients in the control and GPM groups did not receive treatment during the same period of time. Therefore, a large multi-center prospective study is needed to evaluate the findings of our study. However, the GPM Ward Program resonated on a national scale and was elected as one of the top-ten breakthroughs of Chinese Clinical Oncology in 2012 by the Chinese Society of Clinical Oncology (CSCO) and China Medical Tribune[31]. This article could also provide some basis for other developing countries to improve cancer pain management in the future.
In conclusion, our study indicated that the GPM Ward Program improved the pain management of cancer patients in our center and should be continually promoted throughout the nation.
References
- 1.Goudas LC, Bloch R, Gialeli-Goudas M, et al. The epidemiology of cancer pain. Cancer Invest. 2005;23:182–190. [PubMed] [Google Scholar]
- 2.Serlin RC, Mendoza TR, Nakamura Y, et al. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995;61:277–284. doi: 10.1016/0304-3959(94)00178-H. [DOI] [PubMed] [Google Scholar]
- 3.Fisch MJ, Lee JW, Weiss M, et al. Prospective, observational study of pain and analgesic prescribing in medical oncology outpatients with breast, colorectal, lung, or prostate cancer. J Clin Oncol. 2012;30:1980–1988. doi: 10.1200/JCO.2011.39.2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Breuer B, Fleishman SB, Cruciani RA, et al. Medical oncologists' attitudes and practice in cancer pain management: a national survey. J Clin Oncol. 2011;29:4769–4775. doi: 10.1200/JCO.2011.35.0561. [DOI] [PubMed] [Google Scholar]
- 5.Sun WZ, Hou WY, Li JH. People's Republic of China: status of cancer pain and palliative care. J Pain Symptom Manage. 1996;12:127–129. doi: 10.1016/0885-3924(96)00095-4. [DOI] [PubMed] [Google Scholar]
- 6.Zhang H, Gu WP, Joranson DE, et al. People's Republic of China: status of cancer pain and palliative care. J Pain Symptom Manage. 1996;12:124–126. doi: 10.1016/0885-3924(96)00094-2. [DOI] [PubMed] [Google Scholar]
- 7.Sun Y. China: status of cancer pain and palliative care. J Pain Symptom Manage. 1993;8:399–403. doi: 10.1016/0885-3924(93)90062-z. [DOI] [PubMed] [Google Scholar]
- 8.Wang XS, Mendoza TR, Gao SZ, et al. The Chinese version of the Brief Pain Inventory (BPI-C): its development and use in a study of cancer pain. Pain. 1996;67:407–416. doi: 10.1016/0304-3959(96)03147-8. [DOI] [PubMed] [Google Scholar]
- 9.Zhou LJ, Qiu C, Li XY. Cancer pain management: a survey in Shanghai. Nurs J Chin PLA. 2007;24:25–27. [Google Scholar]
- 10.Yu S, Wang XS, Cheng Y, et al. Special aspects of cancer pain management in a Chinese general hospital. Eur J Pain. 2001;5(Suppl A):15–20. doi: 10.1053/eujp.2001.0274. [DOI] [PubMed] [Google Scholar]
- 11.Dong WX, Li JH, Liu CL. The reasons and nursing strategies of uncontrolled cancer pain in cancer patients. J Nur Training. 2006;21:1019–1020. [Google Scholar]
- 12.United Nations International narcotics control board . Narcotic drugs: estimated world requirements-statistics for 1993. United Nations Publication; 1993. [Google Scholar]
- 13.United Nations International narcotics control board . Narcotic drugs: estimated world requirements-statistics for 2012. United Nations Publication; 2012. [Google Scholar]
- 14.Li TD. Present implementation situation and prospects of cancer pain control strategy in China. China J Cancer Prev Treat. 2003;10:1–5. [in Chinese] [Google Scholar]
- 15.Wang XQ, Duan PP. The research progress of influencing factors of cancer pain control. J Nursing Ad. 2012;12:406–407. [Google Scholar]
- 16.Su YJ, Wang CL, Weng L, et al. A survey on physician knowledge and attitudes towards clinical use of morphine for cancer pain treatment in China. Support Care Cancer. 2010;18:1455–1460. doi: 10.1007/s00520-009-0768-2. [DOI] [PubMed] [Google Scholar]
- 17.Wang XS, Li TD, Yu SY, et al. China: status of pain and palliative care. J Pain Symptom Manage. 2002;24:177–179. doi: 10.1016/s0885-3924(02)00435-9. [DOI] [PubMed] [Google Scholar]
- 18.Huang Y. Current status of pain management in China: an overview. Eur J Pain. 2001;5(Suppl A):67–71. doi: 10.1053/eujp.2001.0283. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Health Announcement of launching the Good Pain Management ward program. Available at: http://www.moh.gov.cn/mohyzs/s3586/201104/51234.shtml (accessed on Dec 30, 2013). [in Chinese] [Google Scholar]
- 20.Deng D, Fu L, Zhao YX, et al. The relationship between cancer pain and quality of life in patients newly admitted to Wuhan Hospice Center of China. Am J Hosp Palliat Care. 2012;29:53–59. doi: 10.1177/1049909111418636. [DOI] [PubMed] [Google Scholar]
- 21.van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. High prevalence of pain in patients with cancer in a large population-based study in The Netherlands. Pain. 2007;132:312–320. doi: 10.1016/j.pain.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 22.Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- 23.van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18:1437–1449. doi: 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- 24.Gu WP, Liu ZM. Present situation of cancer pain and its related problems in China. Chin J Drug Depend. 1999;8:4–5. [Google Scholar]
- 25.Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain. 1997;69:1–18. doi: 10.1016/s0304-3959(96)03267-8. [DOI] [PubMed] [Google Scholar]
- 26.Costa L, Major PP. Effect of bisphosphonates on pain and quality of life in patients with bone metastases. Nat Clin Pract Oncol. 2009;6:163–174. doi: 10.1038/ncponc1323. [DOI] [PubMed] [Google Scholar]
- 27.Bonica JJ. Management of cancer pain. Acta Anaesth Scand. 1982;74:75–82. doi: 10.1111/j.1399-6576.1982.tb01852.x. [DOI] [PubMed] [Google Scholar]
- 28.Wong R, Wiffen PJ. Bisphosphonates for the relief of pain secondary to bone metastases. Cochrane Database Syst Rev. 2002;2:CD002068. doi: 10.1002/14651858.CD002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Porter AT, Fontanesi J. Palliative irradiation for bone metastasis—a new paradigm. Int J Radiat Oncol Biol Phys. 1994;29:1199–1200. doi: 10.1016/0360-3016(94)90421-9. [DOI] [PubMed] [Google Scholar]
- 30.Yalçin S, Güllü IH, Tekuzman G, et al. A comparison of two nonsteroidal anti-inflammatory drugs (diflunisal versus dipyrone) in the treatment of moderate to severe cancer pain: a randomized cross over study. Am J Clin Oncol. 1998;21:185–189. doi: 10.1097/00000421-199804000-00019. [DOI] [PubMed] [Google Scholar]
- 31.China Medical Tribune The top-ten progression of Chinese clinical oncology in 2012. Available at: http://zt.cmt.com.cn/zt/csco2012list/index.html (accessed on Dec 24, 2013). [in Chinese]