Abstract
Introduction
The epidemic of nutrition related non-communicable diseases such as type 2 diabetes mellitus and obesity has reached to epidemic portion in the Sri Lanka. However, to date, detailed data on food consumption in the Sri Lankan population is limited. The aim of this study is to identify energy and major nutrient intake among Sri Lankan adults.
Methods
A nationally-representative sample of adults was selected using a multi-stage random cluster sampling technique.
Results
Data from 463 participants (166 Males, 297 Females) were analyzed. Total energy intake was significantly higher in males (1913 ± 567 kcal/d) than females (1514 ± 458 kcal/d). However, there was no significant gender differences in the percentage of energy from carbohydrate (Male: 72.8 ± 6.4%, Female: 73.9 ± 6.7%), fat (Male: 19.9 ± 6.1%, Female: 18.5 ± 5.7%) and proteins (Male: 10.6 ± 2.1%, Female: 10.9 ± 5.6%).
Conclusion
The present study provides the first national estimates of energy and nutrient intake of the Sri Lankan adult population.
Keywords: Dietary survey, Nutrition survey, Energy intake, Sri Lanka, Adults
Introduction
The epidemic of nutrition related non-communicable diseases (NCDs) such as type 2 diabetes mellitus, obesity, Cardio Vascular Diseases (CVDs) and certain cancers are continuing to challenge the health sectors in Asia [1]. Sri Lanka is a low-middle income South Asian country with a population of 20 million. Despite Sri Lanka’s relatively good health status, during the last two decades NCDs have become a more prominent health issue in the country [2]. A quarter of Sri Lankan adults suffer from metabolic syndrome [3]. According to Sri Lanka Diabetes and Cardiovascular Study (SLDCS), the prevalence of diabetes among Sri Lankan adults was nearly 11% and one fifth of adults in Sri Lanka have diabetes or pre-diabetes while one third of those with diabetes are undiagnosed [4]. Premarathna et al., have also reported that there was an increase in the incidences of hospitalization of Sri Lankan adults by 36%, 40% and 29% due to diabetes mellitus, hypertensive disease and ischemic heart disease, respectively, in 2010 compared to 2005 [5]. In Sri Lanka, diet-related chronic diseases currently account for 18.3% of all deaths and 16.7% of hospital expenditure [1]. There is a significant health burden due to NCDs and this will be a challenge to the health sector in a developing country like Sri Lanka.
Some methods to assess the quantity and quality of dietary intake include prospective food records (with weighed or estimated food portions), retrospective 24-hour recalls (24 HDR), and food frequency questionnaires (FFQs) [6]. The 24HDR which is less time consuming and has a low respondent burden, is the method used to gather the quantitative estimate of all foods and beverages that an individual has consumed in the previous 24 hours at a population level. Several national dietary surveys have used 24 HDR and it is known to be acceptable for gathering dietary information on a given day at the population level [7,8].
National diet and nutrition surveys provide valuable information on a possible partial explanation for the eople’s health status and disease risk [9]. Assessment of the dietary and nutritional status of the population is essential to monitor the ongoing nutrition transition in a country [6]. As a developing country, no studies have been carried out to investigate the information on the diet of Sri Lankans and their nutritional status at a national level. Since Sri Lanka is a multi cultural country, peoples’ foods and dietary habits at a national level should be assessed with a representative sample of Sri Lankan adults, which will be more useful to implement health policies and to initiate many interventions. By keeping this view in mind, the current dietary survey was carried out to assess the intakes of energy, macro-nutrients and selected other nutrients with respect to socio demographic characteristics and the nutritional status of Sri Lankan adults.
Methodology
Study sampling and the subjects
The eligible respondents of this study were healthy Sri Lankan adults aged ≥ 18 years recruited from a sub sample of a Sri Lanka Diabetes and Cardiovascular Study [4]. In this study, a total of 600 subjects were randomly selected representing all nine provinces. This sample population was then stratified for area of residence and ethnicity. Description of sample selection is published elsewhere [10]. Written informed consent for participation in the study was obtained and ethical approval for this study was taken from the Ethical Review Committee, Faculty of Medicine, University of Colombo, Sri Lanka.
Measurements
Socio-demographic variables
The selected subjects were initially contacted via telephone or a postal notice by the study team and the information regarding the study was provided in order to obtain their willingness to participate in the study. On the study day, the purpose of the study was briefly explained to the subjects and the information sheets of the study were also given out. Written consent was obtained from each volunteer prior to data collection. Socio-demographic details and diabetes status were obtained by using an interviewer-administered questionnaire and body weight and height were measured using a standard method. Areas of residence, ethnicities, and education levels were categorized according to Sri Lankan governmental standards [11]. Body mass index (BMI) was calculated by weight (in kilograms) divided by height squared (in meters) and several cut-offs were presented as recommended by WHO experts for Asian populations [12].
Dietary assessment
Dietary data were obtained from a 24 HDR method. The subjects were asked to recall all foods and beverages, consumed over the previous 24-hour period. Respondents were probed for the types of foods and food preparation methods. For uncommon mixed meals, the details of recipes and preparation methods were collected at the time of taking the 24 HDR. Dietary recalls were collected by two trained nutritionists who had received uniform training and adhered to the standard operating procedure (SOP). As dietary assessment aids, the standard household measurements such as plate, bowl, cup, glass, and different spoons etc. and food photograph atlases were used to facilitate the quantification of portion sizes. One medium sized coconut spoon of rice was taken as 100 g, a full plate as 400 g, one cup of liquid as 150 ml, one glass of liquid as 200 ml, a table spoon as 15 g and a tea spoon was taken as 5 g. For different curries, weights of average respective amounts were taken. Household measurements were clarified by demonstration of the real utensils and the food portion size photographs. When subjects recalled some food amount in grams, that information was directly entered. Further details of dietary assessment were published previously [10].
Data analysis
All foods recorded in 24 HDR were converted into grams and then, the intake of total energy, macro nutrients (Carbohydrate, Protein and Fat), sodium and dietary fiber were analyzed using NutriSurvey 2007 (EBISpro, Germany) which was modified for Sri Lankan food recipes. As no updated nutritional database has been gathered for some Sri Lankan food, we used the US Department of Agriculture (USDA) nutrient database [13] as our standard to estimate nutrient content in addition to local and regional food composition databases [14,15]. Due to the absence of energy and nutrient information on local mixed cooked dishes, we used a cookery book [16]. All the recipes were accepted after checking for face validity by consulting local housewives and nutritionists. According to recipes, ingredients were weighed to the nearest 1 g for edible portions of the foods. Then food items were cooked accordingly and the end product was weighed. Nutritional composition of the final meal was calculated by entering nutritional values and the weights of individual ingredients to the spreadsheet. The sum of each nutrient was computed and standardized to 100 g of final product. We also excluded participants whose reported daily energy intake was not between 800 and 4200 kcal to identify under- and over-reporters of food intake [17].
Statistical analysis
All data were doubly entered and rechecked in Microsoft Excel 2007. Data sorting and cleaning were carried out before data analysis. Data on energy, macro-nutrients and some selected nutrient intakes were transferred from the NutriSurvey 2007 to the Minitab version 15.0 for statistical analysis. Nutrient intake distributions are presented as mean ± SE, median, 25th and 75th percentiles to characterize population intake levels for socio-demographic characteristics (gender, ethnicity, age groups, and educational levels) and BMI categories. One-way ANOVA and t-test were used to examine the differences in mean intakes energy and nutrients intakes. P value < 0.05 was considered statistically significant.
Results
Socio-demographic profile
From 600 subjects, 491 (81.8%) participated and 28 of subjects under-reported their energy intake. So, a total of 463 (77.2%) was included for the analysis. Socio demographic profiles and BMI categories of the subjects are presented in Table 1. The majority of the subjects were from rural areas (59.7%) and 33% of the population were from urban areas followed by the estate sector (tea plantation area) 7.3%. The majority were women (n = 297). By ethnic groups, Sinhalese (78%), Sri Lankan Tamil (9%), Indian Tamil (7%), and Muslim (6%) in this survey. Adults between the age of 41 and 50 years formed the biggest group (25.27%) while the smallest group was the youngest adults aged between 18-30 yrs (13.17%). It was significant that a majority of the study population (39%) had received formal education up to Ordinary Level. The next largest group was adults (25%) who had studied up to Advanced Level.
Table 1.
Socio-demographic characteristics of the survey population
| Characteristics |
Total (n = 463) |
Men (n = 166) |
Women (n = 297) |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
|
Area of residence |
|
|
|
|
|
|
| Urban |
153 |
33.0 |
45 |
26.5 |
108 |
36.4 |
| Rural |
276 |
59.6 |
102 |
61.4 |
174 |
58.6 |
| Estate |
34 |
7.4 |
19 |
11.5 |
15 |
5.0 |
|
Age group (yrs) |
|
|
|
|
|
|
| 18-29 |
61 |
13.2 |
27 |
16.3 |
34 |
12.7 |
| 30-39 |
84 |
18.1 |
23 |
13.8 |
61 |
22.8 |
| 40-49 |
117 |
25.3 |
38 |
22.9 |
79 |
29.6 |
| 50-59 |
106 |
22. 9 |
40 |
20.1 |
66 |
24.7 |
| >60 |
95 |
20.5 |
38 |
22.9 |
57 |
21.4 |
|
Ethnicity |
|
|
|
|
|
|
| Sinhala |
360 |
77.7 |
118 |
71.0 |
242 |
82.5 |
| Muslim |
27 |
5.8 |
8 |
4.8 |
19 |
6.4 |
| Sri Lankan Tamil |
42 |
9.1 |
20 |
12.1 |
22 |
7.4 |
| Indian Tamil |
34 |
7.3 |
20 |
12.1 |
14 |
4.7 |
|
Educational level |
|
|
|
|
|
|
| No schooling |
27 |
58.3 |
11 |
6.6 |
16 |
5.4 |
| Up to 5 years |
113 |
24.4 |
43 |
25.9 |
70 |
23.6 |
| Up to O/L |
182 |
39.3 |
59 |
35.5 |
123 |
41.4 |
| Up to A/L |
116 |
25.1 |
46 |
27.7 |
70 |
23.6 |
| Graduate |
25 |
5.4 |
07 |
4.2 |
18 |
6.1 |
|
BMI category |
|
|
|
|
|
|
| ≤ 18.5 kg.m-2 |
64 |
13.8 |
29 |
17.5 |
35 |
11.8 |
| > 18.5 - ≤ 22.9 kg.m-2 |
163 |
35.2 |
75 |
45.2 |
88 |
29.6 |
| > 23 - ≤ 24.99 kg.m-2 |
76 |
16.4 |
21 |
12.6 |
55 |
18.5 |
| > 25 - ≤ 27.5 kg.m-2 |
95 |
20.5 |
32 |
19.3 |
63 |
21.1 |
| ≥ 27.5 kg.m-2 | 65 | 14.1 | 09 | 5.4 | 56 | 18.9 |
Energy intake
Table 2 represents the distribution of energy intake of Sri Lankan adults. The mean energy intake of men was significantly higher (1912.7 kcal/d) than that of women (1513.6 kcal/d) (p < 0.05). People living in the estate sector have a significant lower energy intake compared to both the urban and rural subjects (p < 0.05). Muslims had the highest intake of daily energy (1748.8 kcal) while Indian Tamils had the lowest (1437.7 Kcal/d) which statistically significant for both men and women (p < 0.05). Energy consumption of both gender groups declined gradually with their age. Energy intake increased gradually with educational level. According to BMI categories, lower energy levels were reported in both extremes and no distinct pattern was seen.
Table 2.
Energy intake (kcal) of Sri Lankan adults by socio-demographic characteristics
| Characteristics |
All subjects (n =463) |
Men (n = 166) |
Women (n = 297) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
||||
| 25 | 75 | 25 | 75 | 25 | 75 | ||||||||||
|
Area of residence | |||||||||||||||
| Urban |
1669 |
45 |
1594 |
1217 |
2005 |
1910 |
89 |
1899 |
1522 |
2218 |
1569 |
50 |
1453 |
1158 |
1885 |
| Rural |
1677 |
32 |
1590 |
1304 |
1994 |
1975 |
57 |
1926 |
1518 |
2300 |
1502 |
32 |
1462 |
1193 |
1728 |
| Estate |
1439 |
61 |
1468 |
1114 |
1690 |
1581 |
72 |
1635 |
1294 |
1847 |
1258 |
87 |
1340 |
973 |
1470 |
|
Ethnicity | |||||||||||||||
| Sinhala |
1669 |
28 |
1256 |
1589 |
1977 |
1947 |
51 |
1901 |
1518 |
2247 |
1533 |
30 |
1447 |
1173 |
1790 |
| Muslim |
1749 |
84 |
1435 |
1647 |
2156 |
1949 |
173 |
1984 |
1458 |
2324 |
1664 |
91 |
1626 |
1401 |
2026 |
| Sri Lankan Tamil |
1671 |
100 |
1189 |
1526 |
2091 |
2061 |
161 |
2094 |
1660 |
2352 |
1317 |
62 |
1334 |
1071 |
1523 |
| Indian Tamil |
1438 |
61 |
1468 |
1114 |
1690 |
1546 |
77 |
1634 |
1225 |
1833 |
1283 |
90 |
1354 |
993 |
1472 |
|
Age group (years) | |||||||||||||||
| 18-30 |
1832 |
75 |
1942 |
1297 |
2301 |
2166 |
95 |
2064 |
1942 |
2392 |
1567 |
91 |
1385 |
1108 |
2052 |
| 31-40 |
1808 |
64 |
1661 |
1403 |
2059 |
2250 |
148 |
1777 |
1633 |
2726 |
1641 |
56 |
1596 |
1346 |
1892 |
| 41-50 |
1634 |
46 |
1545 |
1268 |
1906 |
1810 |
89 |
1848 |
1418 |
2099 |
1549 |
51 |
1507 |
1197 |
1821 |
| 51-60 |
1614 |
49 |
1544 |
1233 |
1905 |
1859 |
70 |
1639 |
1595 |
2037 |
1465 |
60 |
1361 |
1134 |
1701 |
| >61 |
1487 |
47 |
1394 |
1138 |
1747 |
1688 |
84 |
2155 |
1305 |
2094 |
1353 |
48 |
1257 |
1068 |
1626 |
|
Educational level | |||||||||||||||
| No schooling |
1287 |
73 |
1202 |
905 |
1589 |
1442 |
115 |
1484 |
1123 |
1792 |
1181 |
89 |
1117 |
882 |
1469 |
| Up to 5 years |
1556 |
39 |
1528 |
1233 |
1831 |
1748 |
69 |
1715 |
1380 |
1992 |
1438 |
42 |
1451 |
1138 |
1655 |
| Up to O/L |
1677 |
40 |
1788 |
1299 |
2468 |
1970 |
77 |
1873 |
1493 |
2356 |
1536 |
41 |
1473 |
1194 |
1787 |
| Up to A/L |
1823 |
55 |
1763 |
1378 |
2183 |
2058 |
89 |
2086 |
1590 |
2292 |
1668 |
65 |
1583 |
1224 |
2008 |
| Graduate |
1594 |
102 |
1470 |
1226 |
2000 |
2221 |
119 |
2234 |
1977 |
2543 |
1350 |
78 |
1265 |
1065 |
1635 |
|
BMI category | |||||||||||||||
| ≤ 18.5 kgm-2 |
1548 |
64 |
1409 |
1173 |
1799 |
1782 |
113 |
1637 |
1288 |
2151 |
1354 |
54 |
1325 |
1135 |
1466 |
| >18.5 - ≤ 22.9 kgm2 |
1731 |
45 |
1642 |
1296 |
2064 |
1946 |
66 |
1886 |
1522 |
2290 |
1548 |
56 |
1439 |
1113 |
1907 |
| >23 - ≤ 24.9 kgm-2 |
1666 |
60 |
1570 |
1294 |
1857 |
1910 |
118 |
1817 |
1493 |
2083 |
1532 |
62 |
1466 |
1233 |
1724 |
| > 25 - ≤ 27.5 kgm-2 |
1674 |
52 |
1677 |
1285 |
1977 |
1988 |
99 |
1987 |
1650 |
2324 |
1556 |
56 |
1579 |
1224 |
1790 |
| ≥ 27.5 kgm-2 | 1541 | 54 | 1520 | 1169 | 1871 | 1851 | 147 | 1892 | 1569 | 2103 | 1491 | 56 | 1430 | 1138 | 1728 |
Carbohydrate intake
The mean daily carbohydrate intake was shown in Table 3. The total mean carbohydrate intake of Sri Lankan adults was approximately 304.4 g (71.2% of total energy from Carbohydrates as shown in Figure 1). By strata, rural adults had a higher intake of carbohydrate (307.7 g) than their estate counterparts (270.3 g). Mean carbohydrate intake was highest in Sinhalese (308.7 g) and lowest in Indian Tamils (269.9 g). Male adults’ carbohydrate intake (352.4 g/day) was significantly higher than that of women (277.5 g/day). Carbohydrate intake declined with age.
Table 3.
Carbohydrate intake (g) of Sri Lankan adults by socio-demographic characteristics
| Characteristics |
All subjects (n =463) |
Men (n = 166) |
Women (n = 297) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
||||
| 25 | 75 | 25 | 75 | 25 | 75 | ||||||||||
|
Area of residence | |||||||||||||||
| Urban |
305.9 |
8.7 |
290.7 |
217.5 |
373.5 |
343.5 |
16.3 |
346.7 |
262.8 |
414.1 |
290.4 |
10.0 |
259.1 |
259.1 |
349.1 |
| Rural |
307.7 |
6.2 |
292.3 |
233.0 |
365.7 |
367.1 |
11.4 |
353.9 |
285.3 |
425.6 |
272.8 |
5.88 |
262.1 |
262.1 |
324.7 |
| Estate |
270.3 |
11.8 |
266.6 |
213.0 |
320.6 |
295.0 |
13.7 |
309.5 |
237.2 |
345.4 |
239.0 |
17.7 |
237.2 |
237.2 |
262.7 |
|
Ethnicity | |||||||||||||||
| Sinhala |
308.7 |
5.6 |
292.3 |
229.7 |
368.0 |
363.1 |
10.3 |
346.8 |
289.3 |
427.7 |
282.2 |
5.9 |
262.0 |
214.3 |
330.8 |
| Muslim |
298.0 |
13.9 |
299.9 |
245.2 |
348.4 |
316.8 |
30.7 |
282.8 |
247.3 |
404.6 |
290.0 |
15.1 |
299.9 |
245.2 |
348.4 |
| Sri Lankan Tamil |
298.9 |
17.7 |
269.9 |
203.4 |
375.1 |
367.9 |
27.3 |
369.6 |
315.9 |
402.0 |
236.1 |
12.6 |
226.8 |
199.6 |
267.2 |
| Indian Tamil |
269.9 |
11.9 |
266.6 |
213.0 |
320.6 |
288.0 |
14.7 |
300.6 |
233.8 |
341.5 |
244.2 |
18.1 |
237.7 |
196.2 |
270.8 |
|
Age group (years) | |||||||||||||||
| 18-30 |
338.9 |
15.1 |
340.2 |
233.7 |
425.8 |
401.9 |
19.0 |
400.7 |
345.5 |
440.1 |
289.0 |
18.6 |
247.7 |
206.0 |
392.2 |
| 31-40 |
305.0 |
10.8 |
299.5 |
252.8 |
344.1 |
423.6 |
28.6 |
395.8 |
309.5 |
477.8 |
305.0 |
10.8 |
299.5 |
252.8 |
344.1 |
| 41-50 |
298.7 |
8.6 |
294.6 |
232.8 |
352.1 |
330.4 |
17.1 |
316.3 |
252.4 |
381.3 |
283.4 |
9.4 |
272.6 |
226.9 |
333.3 |
| 51-60 |
291.9 |
9.4 |
273.5 |
225.5 |
348.5 |
339.1 |
13.2 |
329.0 |
275.1 |
398.1 |
263.2 |
11.4 |
235.4 |
198.2 |
321.7 |
| >61 |
273.8 |
9.1 |
261.0 |
203.9 |
324.8 |
310.2 |
16.4 |
306.6 |
233.7 |
371.9 |
249.5 |
9.35 |
239.0 |
201.4 |
390.4 |
|
Educational level | |||||||||||||||
| No schooling |
242.9 |
13.5 |
235.7 |
174.2 |
305.5 |
270.9 |
21.1 |
259.2 |
211.4 |
318.2 |
223.6 |
16.4 |
216.2 |
160.6 |
258.0 |
| Up to 5 years |
286.4 |
7.8 |
276.4 |
228.9 |
331.6 |
323.8 |
14.3 |
317.6 |
244.5 |
386.8 |
263.5 |
7.9 |
261.3 |
216.1 |
307.1 |
| Up to O/L |
309.3 |
7.7 |
290.8 |
233.2 |
364.8 |
366.8 |
15.5 |
345.5 |
290.9 |
415.5 |
281.8 |
7.4 |
262.6 |
221.1 |
329.5 |
| Up to A/L |
332.5 |
11.1 |
323.1 |
243.7 |
399.0 |
373.1 |
16.9 |
374.7 |
300.3 |
427.9 |
305.9 |
13.8 |
279.6 |
216.0 |
360.8 |
| Graduate |
284.8 |
18.5 |
239.0 |
203.6 |
343.1 |
399.2 |
22.5 |
401.6 |
323.0 |
440.4 |
240.3 |
13.5 |
232.2 |
200.0 |
293.1 |
|
BMI category | |||||||||||||||
| ≤ 18.5 kgm-2 |
292.0 |
13.3 |
254.2 |
220.1 |
329.8 |
342.6 |
23.5 |
323.7 |
237.5 |
401.9 |
250.1 |
10.3 |
238.2 |
205.7 |
268.8 |
| >18.5 - ≤ 22.9 kgm2 |
318.1 |
8.7 |
301.6 |
230.5 |
376.3 |
356.3 |
12.5 |
335.8 |
291.5 |
418.3 |
285.5 |
11.0 |
258.5 |
213.2 |
349.5 |
| >23 - ≤ 24.9 kgm-2 |
305.2 |
12.1 |
275.1 |
236.2 |
349.9 |
350.5 |
22.6 |
346.7 |
266.6 |
401.7 |
280.2 |
12.8 |
258.5 |
213.2 |
349.5 |
| > 25 - ≤ 27.5 kgm-2 |
303.4 |
9.8 |
301.9 |
236.3 |
356.3 |
363.2 |
20.3 |
368.0 |
291.3 |
426.0 |
280.9 |
9.8 |
283.1 |
214.9 |
331.7 |
| ≥ 27.5 kgm-2 | 282.4 | 10.4 | 264.6 | 221.4 | 334.1 | 325.8 | 28.2 | 317.6 | 263.4 | 378.0 | 275.5 | 11.0 | 262.8 | 211.1 | 329.4 |
Figure 1.
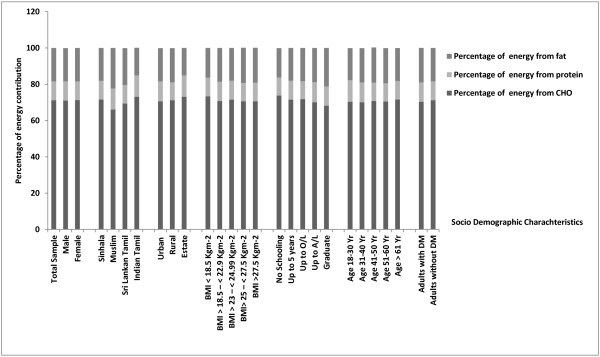
Percentage energy contribution from macronutrients according to gender, ethnicity and area of residance, BMI, educational level and age group.
Protein intake
Sri Lankan adults recorded a mean daily protein intake of 44.6 g whilst men’s intake (52.8 g) was significantly higher than women’s intake (40.0 g). As shown in Table 4, rural (42.9 g/day) and estate (43.7 g/day) adults had similar daily intakes of protein. However, by ethnicity, mean protein intake was significantly higher in Muslims (52.2 g) compared others. Youngest group by age also consumed significantly more protein than others but only for men.
Table 4.
Protien intake (g) of Sri Lankan adults by socio-demographic characteristics
| Characteristics |
All subjects (n =463) |
Men (n = 166) |
Women (n = 297) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
||||
| 25 | 75 | 25 | 75 | 25 | 75 | ||||||||||
|
Area of residence | |||||||||||||||
| Urban |
47.8 |
3.6 |
41.0 |
31.8 |
53.3 |
62.7 |
11.6 |
47.7 |
37.8 |
67.1 |
41.6 |
1.4 |
38.8 |
29.7 |
50.5 |
| Rural |
42.9 |
0.9 |
39.8 |
32.5 |
50.7 |
48.7 |
1.6 |
45.6 |
35.6 |
57.9 |
39.5 |
1.0 |
37.6 |
29.9 |
46.2 |
| Estate |
43.7 |
2.4 |
42.1 |
32.6 |
54.9 |
50.4 |
3.1 |
53.0 |
38.8 |
61.9 |
35.1 |
2.2 |
33.8 |
27.3 |
44.4 |
|
Ethnicity | |||||||||||||||
| Sinhala |
44.2 |
1.6 |
39.8 |
32.1 |
50.5 |
52.6 |
4.5 |
35.6 |
35.6 |
57.1 |
40.1 |
0.9 |
37.5 |
29.7 |
47.6 |
| Muslim |
52.2 |
2.6 |
49.9 |
40.9 |
61.3 |
58.6 |
5.1 |
47.3 |
47.3 |
70.1 |
49.4 |
2.9 |
47.7 |
40.2 |
60.8 |
| Sri Lankan Tamil |
44.1 |
3.2 |
38.8 |
29.8 |
52.8 |
54.8 |
5.5 |
38.6 |
38.6 |
65.1 |
34.4 |
1.8 |
34.0 |
27.9 |
39.6 |
| Indian Tamil |
43.4 |
2.5 |
42.1 |
32.6 |
54.9 |
48.9 |
3.3 |
38.2 |
38.2 |
61.0 |
35.3 |
2.5 |
33.9 |
27.3 |
44.4 |
|
Age group (yrs) | |||||||||||||||
| 18-30 |
57.4 |
8.6 |
46.8 |
34.3 |
60.6 |
74.9 |
18.8 |
52.3 |
43.8 |
74.9 |
43.4 |
2.6 |
41.0 |
31.8 |
53.9 |
| 31-40 |
47.6 |
2.0 |
42.9 |
34.5 |
52.6 |
59.5 |
4.8 |
53.3 |
41.5 |
72.5 |
43.1 |
2.0 |
40.4 |
32.6 |
47.0 |
| 41-50 |
42.6 |
1.2 |
41.0 |
32.7 |
50.5 |
46.5 |
2.3 |
44.9 |
35.5 |
54.3 |
40.8 |
1.4 |
49.9 |
37.9 |
69.8 |
| 51-60 |
41.9 |
1.5 |
38.1 |
29.6 |
50.8 |
48.4 |
2.5 |
48.2 |
37.0 |
56.2 |
38.0 |
1.7 |
34.6 |
27.3 |
46.2 |
| >61 |
39.1 |
1.4 |
34.4 |
29.9 |
45.4 |
43.7 |
2.5 |
40.2 |
32.2 |
54.9 |
36.0 |
1.6 |
33.5 |
28.6 |
41.0 |
|
Educational level | |||||||||||||||
| No schooling |
33.1 |
2.0 |
33.8 |
25.3 |
38.3 |
67.7 |
22.1 |
52.3 |
43.8 |
74.9 |
31.9 |
2.7 |
32.4 |
24.2 |
41.1 |
| Up to 5 years |
41.9 |
1.4 |
38.8 |
30.5 |
49.3 |
59.5 |
4.8 |
53.3 |
41.5 |
72.5 |
38.8 |
1.5 |
37.7 |
28.6 |
44.7 |
| Up to O/L |
42.7 |
1.1 |
39.6 |
32.4 |
50.5 |
46.5 |
2.3 |
44.9 |
35.5 |
54.3 |
39.4 |
1.1 |
36.4 |
30.0 |
46.3 |
| Up to A/L |
52.9 |
4.7 |
45.5 |
35.7 |
56.5 |
48.4 |
2.5 |
48.2 |
37.0 |
56.3 |
44.4 |
1.8 |
40.8 |
32.7 |
53.8 |
| Graduate |
44.24 |
3.5 |
40.2 |
32.2 |
57.5 |
43.7 |
2.5 |
40.2 |
32.2 |
54.9 |
39.4 |
4.1 |
34.3 |
29.5 |
41.9 |
|
BMI Category | |||||||||||||||
| ≤ 18.5 kgm-2 |
41.6 |
1.2 |
39.9 |
31.8 |
46.6 |
45.8 |
2.9 |
43.0 |
35.6 |
52.4 |
38.1 |
2.3 |
34.1 |
29.6 |
43.2 |
| >18.5 - ≤ 22.9 kgm2 |
47.6 |
3.4 |
41.0 |
32.5 |
53.3 |
55.6 |
7.0 |
46.0 |
36.2 |
59.1 |
40.6 |
1.6 |
37.8 |
29.4 |
50.3 |
| >23 - ≤ 24.9 kgm-2 |
44.6 |
2.0 |
41.1 |
32.7 |
49.3 |
52.8 |
3.9 |
47.7 |
35.6 |
59.0 |
40.0 |
1.8 |
34.1 |
29.6 |
43.2 |
| > 25 - ≤ 27.5 kgm-2 |
43.8 |
1.5 |
39.9 |
32.6 |
54.4 |
52.6 |
2.8 |
53.2 |
41.9 |
64.4 |
40.5 |
1.7 |
37.9 |
30.5 |
48.7 |
| ≥ 27.5 kgm-2 | 41.1 | 1.7 | 37.7 | 29.5 | 48.3 | 52.1 | 6.2 | 56.3 | 33.3 | 70.8 | 39.3 | 1.7 | 36.5 | 29.0 | 46.3 |
Fat intake
Estimated daily mean fat intake of Sri Lankan adults was 35 g. A more or less similar fat consumption was noted for rural and urban residents (Table 5) whereas estate people had significantly lower intake of fat (24.76 g; p < 0.05). The youngest age group recorded the highest fat intake (37.7 g) while the lowest intake was observed in the oldest age group (30.8 g). By ethnic groups, Muslims had the highest fat intake (44.7 g) whilst the Indian Tamils had the lowest (24 g) which is significantly lower than Muslims (p < 0.05). With education level, fat consumption was increased particularly among men. Adults with normal BMI and BMI > 25 - ≤ 27.5 kgm-2 had a higher fat intake than other BMI categories.
Table 5.
Fat intake (g) of Sri Lankan adults by socio-demographic characteristics
| Characteristics |
All subjects (n =463) |
Men (n = 166) |
Women (n = 297) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
||||
| 25 | 75 | 25 | 75 | 25 | 75 | ||||||||||
|
Area of residence | |||||||||||||||
| Urban |
35.3 |
1.3 |
31.3 |
23.8 |
43.2 |
42.8 |
2.98 |
37.1 |
27.6 |
58.2 |
32.2 |
1.3 |
29.8 |
22.8 |
38.5 |
| Rural |
36.1 |
0.9 |
34.2 |
23.8 |
43.8 |
41.9 |
1.70 |
39.1 |
29.6 |
50.2 |
32.7 |
1.1 |
30.2 |
21.6 |
40.6 |
| Estate |
24.8 |
1.8 |
22.3 |
17.0 |
34.8 |
27.3 |
2.39 |
22.8 |
17.9 |
35.4 |
21.6 |
2.6 |
18.7 |
14.6 |
26.4 |
|
Ethnicity | |||||||||||||||
| Sinhala |
34.8 |
0.8 |
32.4 |
23.0 |
42.6 |
40.4 |
1.53 |
37.6 |
28.7 |
49.8 |
32.1 |
0.9 |
29.8 |
21.5 |
39.6 |
| Muslim |
44.7 |
4.0 |
37.9 |
29.4 |
61.3 |
57.0 |
8.68 |
55.4 |
37.5 |
78.6 |
39.6 |
3.8 |
36.4 |
25.0 |
54.6 |
| Sri Lankan Tamil |
39.0 |
2.9 |
32.8 |
25.6 |
52.0 |
48.2 |
4.67 |
46.0 |
30.2 |
62.9 |
30.6 |
2.4 |
28.6 |
22.1 |
35.4 |
| Indian Tamil |
24.9 |
1.8 |
22.3 |
17.2 |
34.8 |
26.8 |
2.32 |
22.3 |
17.4 |
35.3 |
22.2 |
2.7 |
21.2 |
15.7 |
26.9 |
|
Age group (years) | |||||||||||||||
| 18-30 |
37.7 |
2.2 |
36.3 |
24.8 |
44.9 |
45.0 |
3.58 |
39.1 |
33.8 |
60.4 |
32.0 |
2.2 |
30.8 |
22.6 |
41.7 |
| 31-40 |
36.6 |
1.8 |
33.9 |
24.6 |
44.3 |
45.4 |
4.48 |
40.1 |
29.5 |
60.9 |
33.2 |
1.7 |
29.6 |
24.2 |
42.2 |
| 41-50 |
35.4 |
1.6 |
31.8 |
24.1 |
41.9 |
40.5 |
2.96 |
37.7 |
28.0 |
53.2 |
33.0 |
1.8 |
30.8 |
21.6 |
39.0 |
| 51-60 |
35.6 |
1.6 |
32.8 |
22.7 |
45.0 |
38.8 |
2.82 |
34.3 |
24.0 |
49.7 |
33.6 |
1.8 |
32.4 |
22.1 |
39.2 |
| >61 |
30.8 |
1.4 |
27.4 |
20.7 |
39.6 |
36.1 |
2.39 |
34.2 |
23.7 |
46.8 |
27.3 |
1.7 |
24.4 |
19.0 |
33.0 |
|
Educational level | |||||||||||||||
| No schooling |
23.6 |
2.1 |
20.5 |
16.4 |
30.8 |
26.6 |
3.34 |
22.8 |
17.9 |
32.8 |
21.4 |
2.6 |
19.5 |
13.6 |
29.0 |
| Up to 5 years |
32.1 |
1.2 |
39.2 |
23.2 |
29.9 |
34.9 |
1.84 |
35.4 |
24.9 |
42.0 |
30.4 |
1.5 |
29.0 |
22.3 |
36.6 |
| Up to O/L |
35.0 |
1.2 |
31.7 |
22.1 |
44.8 |
40.3 |
2.30 |
38.0 |
25.3 |
52.2 |
32.5 |
1.3 |
29.0 |
20.7 |
41.0 |
| Up to A/L |
39.6 |
1.6 |
36.4 |
26.7 |
46.0 |
46.0 |
3.05 |
39.4 |
31.9 |
60.8 |
35.4 |
1.7 |
34.6 |
24.3 |
42.8 |
| Graduate |
39.3 |
3.9 |
34.2 |
23.8 |
58.5 |
61.6 |
5.25 |
60.9 |
56.6 |
76.1 |
30.6 |
3.2 |
35.4 |
21.8 |
28.4 |
|
BMI category | |||||||||||||||
| ≤ 18.5 kgm-2 |
28.8 |
1.8 |
24.2 |
17.3 |
35.6 |
33.3 |
3.04 |
28.0 |
19.6 |
43.8 |
25.1 |
2.0 |
22.6 |
16.4 |
30.6 |
| >18.5 - ≤ 22.9 kgm2 |
37.2 |
1.4 |
34.8 |
23.7 |
46.7 |
42.6 |
2.16 |
38.8 |
29.2 |
51.8 |
32.3 |
1.5 |
30.0 |
22.1 |
40.9 |
| >23 - ≤ 24.9 kgm-2 |
34.2 |
1.6 |
32.5 |
25.4 |
39.5 |
39.0 |
3.52 |
33.7 |
26.9 |
57.5 |
32.0 |
1.5 |
32.6 |
25.6 |
38.0 |
| > 25 - ≤ 27.5 kgm-2 |
36.8 |
1.6 |
35.8 |
24.1 |
45.5 |
42.2 |
3.06 |
38.3 |
29.6 |
53.3 |
34.8 |
1.9 |
32.8 |
22.2 |
44.8 |
| ≥ 27.5 kgm-2 | 34.0 | 2.0 | 28.7 | 24.0 | 40.0 | 44.9 | 7.02 | 37.8 | 26.4 | 66.2 | 32.3 | 2.0 | 28.6 | 22.4 | 39.3 |
Energy contribution from macro nutrients
As a whole, 71.2% energy come from carbohydrates among Sri Lankan adults, 10.8% from protein and 18.9% from fat. Comparisons of the percentage of energy derived from macronutrients according to socio demographic profile and BMI categories were shown in Figure 1. By ethnic distribution, Muslims had more energy from fat (22.3%) while Indian Tamils had the lowest amount of fat (15.5%) and highest intake of carbohydrates (75%). The percentage of calories from protein were relatively higher among the graduates. In contrast, adults who did not receive a formal education had a higher percentage of energy from carbohydrates compared to other groups. There was no difference in energy distribution between diabetic and non-diabetic subjects.
Dietary fiber
The daily mean dietary fiber intake of Sri Lankan adults was 18.1 g (men: 21.3 g; women: 16.3 g; p < 0.05). By area of residence, estate adults had a higher dietary fiber intake (20.6 g) than their urban and rural counterparts (Table 6). Mean dietary fiber intake was highest in Indian Tamils (20.6 g) and lowest in Sinhalese (17.6 g) (p < 0.05). Dietary fiber intake increased with educational level and a similar trend was observed for women as men. Daily dietary fiber intake was always higher among men than women with different socio demographic characteristics. Adults aged > 60 years had the lowest intake of fiber.
Table 6.
Dietary fiber intake (g) of Sri Lankan adults by socio demographic characteristics
| Characteristics |
All subjects (n =463) |
Men (n = 166) |
Women (n = 297) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
||||
| 25 | 75 | 25 | 75 | 25 | 75 | ||||||||||
|
Area of residence | |||||||||||||||
| Urban |
18.1 |
0.7 |
16.2 |
12.2 |
22.6 |
19.7 |
1.4 |
17.0 |
13.8 |
25.5 |
17.5 |
0.8 |
15.4 |
11.9 |
21.0 |
| Rural |
17.7 |
0.5 |
16.6 |
12.2 |
21.3 |
21.3 |
0.8 |
18.6 |
15.6 |
26.8 |
15.6 |
0.5 |
15.1 |
11.1 |
19.0 |
| Estate |
20.6 |
1.9 |
17.7 |
12.8 |
28.7 |
24.9 |
2.8 |
22.3 |
14.6 |
33.1 |
15.2 |
1.5 |
16.7 |
8.8 |
19.5 |
|
Ethnicity | |||||||||||||||
| Sinhala |
17.7 |
0.4 |
16.4 |
12.1 |
21.4 |
20.2 |
0.8 |
17.8 |
14.1 |
24.9 |
16.4 |
0.5 |
15.6 |
11.3 |
19.7 |
| Muslim |
18.8 |
1.4 |
18.0 |
12.8 |
24.4 |
22.4 |
2.3 |
22.7 |
16.7 |
24.8 |
17.2 |
1.7 |
15.3 |
12.1 |
19.5 |
| Sri Lankan Tamil |
18.8 |
1.3 |
17.4 |
12.4 |
26.4 |
23.8 |
2.0 |
26.4 |
15.6 |
31.8 |
14.3 |
1.0 |
13.6 |
11.1 |
18.6 |
| Indian Tamil |
20.6 |
1.9 |
17.6 |
12.8 |
28.7 |
24.5 |
2.6 |
20.8 |
15.2 |
32.7 |
15.0 |
1.6 |
15.5 |
8.7 |
19.9 |
|
Age group (years) | |||||||||||||||
| 18-30 |
18.1 |
1.0 |
16.9 |
11.7 |
22.3 |
21.6 |
1.7 |
21.0 |
14.2 |
26.5 |
15.3 |
1.1 |
14.4 |
10.7 |
19.2 |
| 31-40 |
18.6 |
0.9 |
17.1 |
13.0 |
22.1 |
22.8 |
1.8 |
20.9 |
17.0 |
27.1 |
17.0 |
0.9 |
16.4 |
12.2 |
20.0 |
| 41-50 |
18.2 |
0.7 |
17.0 |
13.4 |
22.0 |
19.9 |
1.5 |
17.4 |
14.0 |
25.5 |
17.4 |
0.8 |
16.4 |
12.9 |
20.5 |
| 51-60 |
18.8 |
0.9 |
16.5 |
12.0 |
25.4 |
23.4 |
1.6 |
20.4 |
15.6 |
31.3 |
16.0 |
1.0 |
14.4 |
10.1 |
19.6 |
| >61 |
16.6 |
0.8 |
15.6 |
10.5 |
20.4 |
19.3 |
1.4 |
18.3 |
14.8 |
23.7 |
14.8 |
1.0 |
13.0 |
9.2 |
18.8 |
|
Educational level | |||||||||||||||
| No Schooling |
15.6 |
1.2 |
19.1 |
10.5 |
17.0 |
17.0 |
2.2 |
17.2 |
10.5 |
22.1 |
14.6 |
1.4 |
15.9 |
10.1 |
18.9 |
| Up to 5 years |
17.6 |
0.8 |
15.4 |
11.8 |
20.4 |
21.9 |
1.7 |
18.3 |
14.1 |
29.1 |
15.0 |
0.8 |
13.6 |
10.8 |
18.8 |
| Up to O/L |
17.6 |
0.6 |
16.3 |
12.2 |
21.0 |
20.5 |
1.1 |
17.4 |
14.1 |
26.8 |
16.2 |
0.6 |
15.6 |
11.4 |
19.6 |
| Up to A/L |
19.9 |
0.8 |
18.4 |
13.9 |
25.3 |
22.3 |
1.3 |
21.0 |
15.8 |
26.9 |
18.2 |
1.1 |
17.7 |
12.8 |
22.1 |
| Graduate |
17.8 |
1.6 |
18.0 |
10.6 |
23.0 |
24.2 |
2.7 |
23.3 |
22.4 |
27.1 |
15.3 |
1.7 |
13.6 |
9.8 |
20.1 |
|
BMI category | |||||||||||||||
| ≤ 18.5 kgm-2 |
16.9 |
0.9 |
15.8 |
11.9 |
21.2 |
18.8 |
1.4 |
17.2 |
13.8 |
23.4 |
15.4 |
1.0 |
14.3 |
10.6 |
19.4 |
| >18.5 - ≤ 22.9 kgm-2 |
19.1 |
0.7 |
17.1 |
13.0 |
22.6 |
23.0 |
1.1 |
20.9 |
15.6 |
27.4 |
15.8 |
0.8 |
14.6 |
11.5 |
18.8 |
| >23 - ≤ 24.9 kgm-2 |
17.3 |
1.0 |
16.2 |
11.2 |
22.0 |
19.1 |
1.8 |
16.7 |
13.2 |
26.8 |
16.4 |
1.1 |
13.8 |
10.8 |
20.8 |
| > 25 - ≤ 27.5 kgm-2 |
18.2 |
0.7 |
17.0 |
13.6 |
22.4 |
20.6 |
1.4 |
17.2 |
15.8 |
26.6 |
17.4 |
0.8 |
16.4 |
13.1 |
20.9 |
| ≥ 27.5 kgm-2 | 17.2 | 1.2 | 15.5 | 9.3 | 20.4 | 23.6 | 4.4 | 21.2 | 11.9 | 33.2 | 17.3 | 0.8 | 16.4 | 13.0 | 20.6 |
Sodium
Daily mean sodium intake was 3.26 g and 2.51 g for men and women, respectively (p < 0.05). Dietary sodium intake of Sri Lankan adults according to demographic and BMI categories is shown in Table 7. Mean sodium intake of rural adults was 2.89 g, followed by urban adults (2.73 g). The Estate sector had the lowest intake (2.48 g). Muslims and Sri Lankan Tamils had a higher intake of sodium than Sinhalese and Indian Tamils. With aging, sodium intake declined and the youngest age group recorded the highest intake (3.04 g).
Table 7.
Sodium intake (mg) of Sri Lankan adults by socio-demographic characteristics
| Characteristics |
All subjects (n =463) |
Men (n = 166) |
Women (n = 297) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
Mean |
±SE |
Median |
Percentiles |
||||
| 25 | 75 | 25 | 75 | 25 | 75 | ||||||||||
|
Area of residence | |||||||||||||||
| Urban |
2729 |
102 |
2509 |
1835 |
3411 |
3100 |
196 |
3003 |
1952 |
3893 |
2574 |
116 |
2362 |
1711 |
3242 |
| Rural |
2890 |
81 |
2582 |
2025 |
3507 |
3396 |
155 |
3190 |
2448 |
4211 |
2605 |
84 |
2374 |
1870 |
3143 |
| Estate |
2477 |
156 |
2378 |
1800 |
3072 |
2889 |
184 |
2665 |
2377 |
3502 |
1954 |
200 |
2036 |
1359 |
2350 |
|
Ethnicity | |||||||||||||||
| Sinhala |
2769 |
61 |
2523 |
1934 |
3391 |
3155 |
107 |
2969 |
2228 |
3877 |
2580 |
70 |
2372 |
1825 |
3225 |
| Muslim |
3012 |
301 |
2610 |
1941 |
3910 |
2983 |
345 |
3256 |
2085 |
3760 |
3023 |
407 |
2469 |
1612 |
4023 |
| Sri Lankan Tamil |
3306 |
333 |
2797 |
1954 |
4487 |
4400 |
588 |
4492 |
2624 |
5463 |
2311 |
176 |
2189 |
1803 |
2859 |
| Indian Tamil |
2488 |
154 |
2378 |
1800 |
3072 |
2831 |
184 |
2598 |
2144 |
3467 |
1997 |
209 |
2096 |
1440 |
2363 |
|
Age group (years) | |||||||||||||||
| 18-30 |
3045 |
145 |
3071 |
2186 |
3519 |
3436 |
238 |
3179 |
2536 |
4258 |
2736 |
162 |
2873 |
1915 |
3441 |
| 31-40 |
2940 |
144 |
2532 |
2048 |
3667 |
3883 |
311 |
3856 |
2379 |
4669 |
2584 |
135 |
2390 |
1903 |
2985 |
| 41-50 |
2778 |
99 |
2536 |
2048 |
3667 |
2976 |
173 |
2655 |
2163 |
3833 |
2683 |
120 |
2480 |
2023 |
3245 |
| 51-60 |
2832 |
162 |
2448 |
1817 |
3441 |
3188 |
307 |
2560 |
2013 |
3924 |
2616 |
180 |
2211 |
1678. |
3299 |
| >61 |
2564 |
114 |
2363 |
1652 |
3265 |
3108 |
187 |
3106 |
2290 |
3822 |
2201 |
123 |
2003 |
1577 |
2511 |
|
Educational level | |||||||||||||||
| No schooling |
2290 |
193 |
2157 |
1359 |
2954 |
2923 |
279 |
2530 |
2200 |
3562 |
1855 |
206 |
1740 |
1203 |
2302 |
| Up to 5 years |
2697 |
114 |
2403 |
1847 |
3351 |
2984 |
169 |
2772 |
2198 |
3813 |
2521 |
148 |
2188 |
1684 |
3032 |
| Up to O/L |
2825 |
104 |
2500 |
1944 |
3461 |
3353 |
233 |
3200 |
2057 |
3910 |
2571 |
99 |
2371 |
1903 |
3031 |
| Up to A/L |
2971 |
113 |
2715 |
2122 |
3437 |
3300 |
187 |
2999 |
2479 |
4385 |
2755 |
136 |
2645 |
1937 |
3249 |
| Graduate |
3046 |
269 |
3126 |
1739 |
3910 |
4384 |
447 |
4432 |
3562 |
5215 |
2526 |
241 |
2663 |
1506 |
3408 |
|
BMI category | |||||||||||||||
| ≤ 18.5 kgm-2 |
2580 |
147 |
2296 |
1649 |
3383 |
3124 |
252 |
2927 |
2052 |
4219 |
2129 |
129 |
2054 |
1541 |
2793 |
| >18.5 - ≤ 22.9 kgm2 |
3029 |
114 |
2665 |
2069 |
3622 |
3464 |
192 |
3231 |
2509 |
4111 |
2659 |
121 |
2449 |
1879 |
3261 |
| >23 - ≤ 24.9 kgm-2 |
2775 |
150 |
2486 |
1914 |
3241 |
2896 |
232 |
2536 |
1958 |
3716 |
2708 |
196 |
2443 |
1858 |
3211 |
| > 25 - ≤ 27.5 kgm-2 |
2756 |
120 |
2509 |
1974 |
3405 |
3179 |
119 |
3213 |
2278 |
4126 |
2596 |
143 |
2257 |
1800 |
3240 |
| ≥ 27.5 kgm-2 | 2615 | 133 | 2351 | 1769 | 3502 | 3286 | 435 | 3810 | 2099 | 4306 | 2507 | 135 | 2255 | 1660 | 3287 |
Discussion
Although national dietary and nutrition surveys have a number of important functions and can provide much valuable information, Sri Lanka had never conducted a national food consumption survey before, probably due to lack of human and financial resources. This is the first attempt to report energy and macronutrients intakes in a fairly representative sample over the island using updated food composition data. Subject distribution of ethnic groups, area of residence and educational levels closely mirror the national statistics [11].
Differences in calorie consumption were seen according to demographic and BMI categories. Men consume larger portions of foods and are expected to obtain a higher amount of energy than their female counterparts [18]. The intake of energy by Sri Lankan men was found to be higher than that of women by about 350 kcals. Similar differences were reported among Malaysian adults [19] and in Britain the difference was nearly 700 kcal [20]. When compared to people living in urban and rural areas, estate workers are getting the least energy. Lower mean energy intake was reported among Malaysian estate workers [21]. The decline in calorie consumption with age was probably due to reduction in physical activity levels and poor appetite, particularly in older adults. Different energy intakes in ethnic groups may represent their cultural eating habits. For instance, Muslim people tend to have a higher energy intake and eat more fat rich food items compared to Indian Tamils. Up to A/L by education level, energy consumption was gradually increased, this is probably associated with increased purchasing power with higher education status; however, graduate groups may be also aware of health issues associated with excess energy. In developed countries, calorie consumption is inversely associated with education levels [22]. Except for the very obese category, consumption of total energy intake was steadily rising with BMI categories. Under-reporting of food intake by obese subjects is well documented [23].
The total daily intake of protein in Sri Lankan adults is almost half that of the US adults and, among Americans 2/3 of all protein, is derived from animal sources [24]. In contrast, plant sources (rice and pulses) are the main contributors of protein among Sri Lankan adults [10,25]. American men consume over 100 gms of fat daily and for women it is 65 g [26]. Corresponding values for Sri Lankans are 40.5 grams and 31.9 grams. In addition to the amount of fat, the type of fat is crucial for development of diet-related chronic diseases such as cardiovascular disease. Although, sub types of fat are not reported in this analysis, the main lipid source in Sri Lankan diet is coconut milk/oil which is high in saturated fatty acids [27]. Therefore, it is important to conduct further studies to explore the coconut consumption and associated cardiovascular disease risk in this population.
Energy-providing macronutrient proportions could vary in different populations. According to the ranges of population nutrient intake goals recommended by WHO, the percentage of energy from total carbohydrates, fats and proteins should be 55-75%, 15-30% and 10-15%, respectively [28]. British adults consume less than fifty percent of energy (men: 47.7%; women: 48.5%) from carbohydrates, whilst fat intake contributes 35.8% and 34.9% of total energy for men and women respectively. The contribution of protein as an energy source is 16.5% for both sexes [20]. In contrast to western countries, Malaysians get nearly 60% of their energy from carbohydrates, 14% of energy from protein and the rest from fats [19]. In contrast to western countries and some Asian countries, Sri Lankan adults consume proportionally more carbohydrates (>71% of energy) and less fat (<19% of energy) and proteins (<11%). The prevalence of diabetes in Sri Lanka is 11% and one fifth of adults are suffering from diabetes despite low levels of obesity (BMI > 30 = 3.7%). Since the study is cross-sectional in nature, we cannot conclude the association between the relatively larger contribution of energy from carbohydrate and higher prevalence of diabetes/dysglycemia among Sri Lankan adults, in spite of carbohydrates contributing over 70% of energy for both diabetics and non-diabetics. Longitudinal studies assessing the prospective risk of developing diabetes and the proportion of energy derived from macronutrients are needed to fully elucidate an association. A high intake of carbohydrate may lead to hyperinsulinaemia, high serum TAG and low HDL-cholesterol levels and chronic consumption of large carbohydrate meals may cause postprandial hyperglycaemia and hypertriacylglycerolaemia and eventually develop insulin resistance and diabetes [29].
A generous intake of dietary fiber reduces risk of developing many diseases including coronary heart disease, stroke, hypertension, diabetes, obesity, and certain gastrointestinal disorders as well as improving metabolic parameters and immune functions [30]. The definition, method of measuring fiber and recommendations varies in different countries. The backbone of our food composition data is based on USDA. According to US guidelines, the current recommendation is to consume 14 g per every 1000 kcals, therefore using the energy guideline of 2000 kcal/day for women and 2600 kcal/day for men, the recommended daily dietary fiber intake is 28 g/day for adult women and 36 g/day for adult men [31]. Although Sri Lankan adults consume fewer energy compared to US adults, their dietary fiber intake is insufficient according to their calorie intake.
Epidemiological, clinical and animal-experimental evidence showed a direct relationship between dietary electrolyte consumption and blood pressure [32]. Furthermore, clinical trials show that a reduction in salt (NaCl) intake reduces BP levels in normotensive and hypertensive populations and prevents the development of hypertension [32]. Recommended Na intake is maximum of 2.3 g/day [32]. Our findings showed most Sri Lankan adults exceed current recommendations. The high consumption of Sodium may be associated with the epidemic of hypertension (Men: 18.8%; Women: 19.3%) among Sri Lankan adults [33].
This study has several limitations. Sri Lanka has over 20 million inhabitants. Therefore, diet records of a sample of 463 subjects may not represent the eating patterns of the whole population. However, a well-conducted UK NDNS [20] measured the dietary records of 1724 respondents and achieved a lower response rate of 47%. Considering available resources, the high response rate and satisfactory representation of demographic parameters, we believe this is a reasonable sample size. Secondly, 24HDR may not be the best tool to determine habitual diet, because of the non-representative diet and recall bias. However, we selected random 24HDR, which were evenly distributed within weekdays and weekends. Random 24HDR in a large sample has been used in other national surveys in other countries [7]. Thirdly, our findings were limited to energy and selected major macronutrients due to sub quality nutritional information on sub categories of macronutrients and micronutrients of Sri Lankan mixed dishes (Additional file 1). Another limitation is that despite of reports of high alcohol consumption among Sri Lankan men [34], alcohol intake was under-reported in our study (<0.5%). In this survey, low energy reporters (<800 kcal/day) were excluded, therefore exclusion will have biased the data towards higher intakes. Lastly, we did not attempt to correlate energy intake and its adequacy to this population as calorie recommendations may vary with several factors such as gender, age, body weight, body composition and physical activity level.
Acknowledging the limitations of the survey, the present study provides the first national estimates of energy and nutrient intake of the Sri Lanka adult population. It is evident that consumption of high levels of carbohydrate, fat mainly from saturated sources, low protein, low dietary fiber and high levels of sodium may have detrimental effects on health and be related to the current epidemic of NCDs. Unfortunately, current food-based dietary guidelines are based on limited research [25]. Therefore, well-designed and nationally representative studies are needed to explore the association between diet and chronic disease among Sri Lankan adults. Moreover, regular diet and nutrition surveys should be carried out to obtain information on dietary patterns and nutrient intakes and, ideally, periodical monitoring is needed to identify the changing trends in food intake and to assess public responses to dietary recommendations.
Competing interests
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The authors declare that they have no financial or non-financial competing interests.
Authors’ contributions
RJ contributed to the data collection, data analysis and drafted the manuscript. ST analyzed nutrient values. NB, MS, PK and AH were supervisory team members on the project and contributed to study design, interpretation of data and revision of the manuscript. All authors read and approved the final manuscript.
Supplementary Material
Selected micronutrient intake among Sri Lankan adults.
Contributor Information
Ranil Jayawardena, Email: ranil7@gmail.com.
Shalika Thennakoon, Email: shalika_san@yahoo.com.
Nuala Byrne, Email: n.byrne@qut.edu.au.
Mario Soares, Email: M.Soares@curtin.edu.au.
Prasad Katulanda, Email: pkatulanda@yahoo.com.
Andrew Hills, Email: ahills@mmri.mater.org.au.
Acknowledgements
The authors would like to acknowledge Miss Fathima Shakira and other members in the Diabetes Research Unit, Colombo, for their contribution in arranging logistics for the study.
References
- Popkin BM, Horton S, Kim S. The Nutritional Transition and Diet-Related Chronic Diseases in Asia: Implications for Prevention. Washington, DC: International Food Policy Research Institute FCND Discussion Paper; 2001. p. 105. [Google Scholar]
- Jayasekara R, Schultz T. Health status, trends, and issues in Sri Lanka. Nurs Health Sci. 2007;9:228–233. doi: 10.1111/j.1442-2018.2007.00328.x. [DOI] [PubMed] [Google Scholar]
- Katulanda P, Ranasinghe P, Jayawardena R, Sheriff R, Matthews D. Metabolic syndrome among Sri Lankan adults: prevalence, patterns and correlates. Diabetol Metab Syndr. 2012;4:24. doi: 10.1186/1758-5996-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katulanda P, Constantine GR, Mahesh JG, Sheriff R, Seneviratne RD, Wijeratne S, Wijesuriya M, McCarthy MI, Adler AI, Matthews DR. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka–Sri Lanka Diabetes, Cardiovascular Study (SLDCS) Diabet Med. 2008;25:1062–1069. doi: 10.1111/j.1464-5491.2008.02523.x. [DOI] [PubMed] [Google Scholar]
- Premaratne R, Amarasinghe A, Wickremasinghe AR. Hospitalisation trends due to selected non-communicable diseases in Sri Lanka, 2005–2010. Ceylon Med J. 2005;50:51–54. doi: 10.4038/cmj.v50i2.1568. [DOI] [PubMed] [Google Scholar]
- Walter Willett EL. In: Monographs in Epidemiology and Biostatistics. Willett W, editor. Oxford: Oxford University Press; 1998. Nutritional epidemiology; pp. 101–147. [Google Scholar]
- University of Otago and Ministry of Health. A Focus on Nutrition: Key findings of the 2008/09 New Zealand Adult Nutrition Survey. Ministry of Health; 2011. [Google Scholar]
- Giskes K, Turrell G, Patterson C, Newman B. Socio-economic differences in fruit and vegetable consumption among Australian adolescents and adults. Public Health Nutr. 2002;5:663–669. doi: 10.1079/PHN2002339. [DOI] [PubMed] [Google Scholar]
- Sasaki S. The value of the National Health and Nutrition Survey in Japan. Lancet. 2011;378:1205–1206. doi: 10.1016/S0140-6736(11)61220-8. [DOI] [PubMed] [Google Scholar]
- Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Hills AP. Consumption of Sri Lankan adults: an appraisal of serving characteristics. Public Health Nutr. 2013;16(4):653–658. doi: 10.1017/S1368980012003011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistical Abstract. [ http://www.statistics.gov.lk/page.asp?page=Population%20and%20Housing]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- USDA. Foods List. 24 2012. [Google Scholar]
- Perera WDAJPM, Thaha SZ. Tables of Food Composition For Use in Sri Lanka. 1979.
- Gopalan CRBV, Balasubramanian SC. Nutritive Value of Indian Foods. 1989. Hyderabad.
- Dissanayake C. Ceylon Cookery. 9. Sri Lanka: Stamford Lake (pvt) Ltd; 2010. [Google Scholar]
- Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi F. Dietary diversity score and cardiovascular risk factors in Tehranian adults. Public Health Nutr. 2006;9:728–736. doi: 10.1079/phn2005887. [DOI] [PubMed] [Google Scholar]
- Caster WO. Systematic estimation of food intakes from food frequency data. Nutr Res. 1986;6:469–472. doi: 10.1016/S0271-5317(86)80189-0. [DOI] [Google Scholar]
- Mirnalini KZM, Safiah MY, Tahir A, Siti Haslinda MD, Siti Rohana D, Khairul Zarina MY, Mohd Hasyami S, Normah H. Energy and nutrient intakes: findings from the Malaysian Adult Nutrition Survey (MANS) Mal J Nutr. 2008;14:1–24. [PubMed] [Google Scholar]
- Swan G. Findings from the latest national diet and nutrition survey. Proc Nutr Soc. 2004;63:505–512. doi: 10.1079/PNS2004381. [DOI] [PubMed] [Google Scholar]
- Chee SSZH, Ismail MN, Ng KK. Anthropometry, dietary patterns and nutrient intakes of Malaysian estate workers. Mal J Nutr. 1996;2:112–126. [PubMed] [Google Scholar]
- Rennie KL, Jebb SA. Prevalence of obesity in Great Britain. Obes Rev. 2005;6:11–12. doi: 10.1111/j.1467-789X.2005.00164.x. [DOI] [PubMed] [Google Scholar]
- Heitmann BL, Lissner L. Dietary underreporting by obese individuals–is it specific or non-specific? BMJ. 1995;311:986–989. doi: 10.1136/bmj.311.7011.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit E, Nieto FJ, Crespo CJ, Mitchell P. Estimates of animal and plant protein intake in US adults: results from the Third National Health and Nutrition Examination Survey, 1988–1991. J Am Diet Assoc. 1999;99:813–820. doi: 10.1016/S0002-8223(99)00193-5. [DOI] [PubMed] [Google Scholar]
- Samaranayake UMM. Food Base Dietary Guidelines for Sri Lanka. Colombo: Nutrition Division, Ministry of Healthcare and Nutrition, Sri Lanka; 2011. [Google Scholar]
- Kennedy ET, Bowman SA, Powell R. Dietary-fat intake in the US population. J Am Coll Nutr. 1999;18:207–212. doi: 10.1080/07315724.1999.10718853. [DOI] [PubMed] [Google Scholar]
- Amarasiri WA, Dissanayake AS. Coconut fats. Ceylon Med J. 2006;51(2):47–51. doi: 10.4038/cmj.v51i2.1351. [DOI] [PubMed] [Google Scholar]
- Report of a Joint WHO/FAO Expert Consultation. Diet, Nutrition and the Prevention of Chronic Diseases. 2003.
- Misra A, Khurana L, Isharwal S, Bhardwaj S. South Asian diets and insulin resistance. Br J Nutr. 2009;101:465–473. doi: 10.1017/S0007114508073649. [DOI] [PubMed] [Google Scholar]
- Anderson JW, Baird P, Davis RH Jr, Ferreri S, Knudtson M, Koraym A, Waters V, Williams CL. Health benefits of dietary fiber. Nutr Rev. 2009;67:188–205. doi: 10.1111/j.1753-4887.2009.00189.x. [DOI] [PubMed] [Google Scholar]
- USDA. The Food Supply and Dietary Fiber: Its Availability and Effect on Health. Department of Agriculture; 2007. [Google Scholar]
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG. for DASH–Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- Wijewardene K, Mohideen MR, Mendis S, Fernando DS, Kulathilaka T, Weerasekara D, Uluwitta P. Prevalence of hypertension, diabetes and obesity: baseline findings of a population based survey in four provinces in Sri Lanka. Ceylon Med J. 2005;50:62–70. doi: 10.4038/cmj.v50i2.1571. [DOI] [PubMed] [Google Scholar]
- Rahav G, Wilsnack R, Bloomfield K, Gmel G, Kuntsche S. The influence of societal level factors on men’s and women’s alcohol consumption and alcohol problems. Alcohol Alcohol. 2006;41:i47–i55. doi: 10.1093/alcalc/agl075. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Selected micronutrient intake among Sri Lankan adults.


