ABSTRACT
The 6-min walk test (6MWT) has been used to examine subjective dyspnea, predict mortality and measure clinical outcomes in studies of patients with chronic pulmonary or heart disease. Although the 6MWT is useful to assess the general ability to perform daily physical activity, it is difficult to evaluate time-dependent responses. To improve the 6MWT, we devised a new index, which is the number of steps walked per second (NSPS). We performed the 6MWT in 11 healthy subjects and 7 patients with chronic obstructive pulmonary disease (COPD) and calculated the NSPS. The mean NSPS was significantly higher in the healthy subjects than in the COPD patients, while the coefficient of variation of the NSPS was significantly smaller in healthy subjects compared with COPD patients. Calculation of the NSPS was useful to evaluate the walking pattern. This modified 6MWT may be helpful for assessing the efficacy of rehabilitation and drug therapy for COPD.
Keywords: 6-min walk test, chronic obstructive pulmonary disease, dyspnea, walking pattern
The 6-min walk test (6MWT) has been used to assess functional status and measure clinical outcomes in studies of patients with chronic respiratory disease. This test assesses the farthest distance that a patient can walk in 6 min.1 It was recently reported that the 6-min walking distance (6MWD) is useful for predicting mortality in patients with chronic obstructive pulmonary disease (COPD) but the efficacy of exercise-related oxygen desaturation is less clear.2 However, patients with severe COPD frequently cannot walk for 6 min without stopping and may have to rest several times during the 6MWT due to dyspnea. Moreover, some patients cannot walk at a constant pace, and the conventional 6MWT is difficult to evaluate in terms of time-dependent parameters such as the instantaneous walking speed. Since oxygen desaturation can improve after resting, the resting time and walking pattern may influence the results of this test in COPD patients. We developed a modified 6MWT in which the walking pattern was examined by determining the number of steps per second (NSPS).
SUBJECTS AND METHODS
Subjects and patients
Eleven healthy subjects (6 males and 5 females) and 7 clinically stable male patients with COPD participated in this study (Table 1). Exclusion criteria were unstable cardiovascular, orthopedic or neurologic conditions. This study was approved by Tottori University and the Hitachi Memorial Hospital ethical board (approval number 1845) and all participants gave written informed consent.
Table 1. Profile of the subjects and results of the 6MWT: average NSPS.
| Healthy subjects | Patients with COPD | P value* | |
| Number of subjects | 11 | 7 | |
| Age (yr) | 68.6 (5.4) | 70.7 (4.8) | 0.316 |
| Height (m) | 1.58 (0.07) | 1.60 (0.06) | 0.934 |
| Weight (kg) | 61.0 (8.3) | 48.7 (7.9) | 0.012 |
| FVC (L) | 2.98 (0.72) | 2.78 (0.92) | 0.696 |
| FEV1 (L) | 2.48 (0.62) | 1.34 (0.75) | 0.008 |
| FEV1, % predicted (%) | 103.2 (14.2) | 55.2 (27.1) | 0.0018 |
| 6MWD (m) | 486.9 (35.0) | 289.5 (123.7) | 0.005 |
| Total number of steps | 711.9 (47.1) | 511.0 (153.5) | 0.009 |
| Mean NSPS (step/s) | 1.98 (0.13) | 1.42 (0.43) | 0.0009 |
| CV of NSPS (%) | 7.4 (1.3) | 44.7 (45.3) | 0.0097 |
| Total resting time (s) | 0 | 65.6 (83.8) | 0.0062 |
| Delta Borg scale | 0.1 (0.2) | 1.6 (1.1) | 0.002 |
| Lowest SpO2 (%) | 94.4 (1.2) | 88.0 (5.7) | 0.0052 |
| Mean SpO2 (%) | 95.5 (0.9) | 90.9 (4.1) | 0.0043 |
Values, mean (SD).
* Mann-Whitney’s U test.
6MWT, 6-min walk test; COPD, chronic obstructive pulmonary disease; CV, coefficient of variation; FVC, Forced vital capacity, FEV1, Forced expiratory volume in 1 s; NSPS, number of steps walked per second.
The NSPS was calculated as [steps walked in 5 s] × 0.2, and was calculated 72 times (360 s ÷ 5 s) in each subject.
The CV of NSPS was calculated as [SD/mean NSPS] × 100 (%).
Delta Borg scale: modified Borg scale after walking − modified Borg scale before walking.
6MWT
The test was conducted in flat corridors with lengths of 54 or 74 m at Tottori University or Hitachi Memorial Hospital, respectively, according to the published guideline.1 Oxygen saturation of arterial blood was measured by pulse oximetry (SpO2) with a finger sensor (Pulsox 300i, Konica-Minolta, Tokyo, Japan) and was continuously recorded during the test. Then pulse oximetry variables were analyzed by DS-5 Pulsox analysis software (Konica-Minolta). The severity of dyspnea was subjectively assessed before and after the 6MWT using a modified Borg scale. 3 It has been reported that at least 2 practice walks should be performed before the 6MWT because training influences the results.4, 5 Healthy subjects did 2 practice walks before the 6MWT, which was performed at the 3rd trial. COPD patients performed at least 2 practice walks on another day before the actual test because dyspnea and fatigue could influence the results of the 6MWT if patients practiced on the same day. The patients were allowed to sit on a chair to rest if needed, and resumed walking when they had recovered sufficiently. The duration of every rest was measured with a stopwatch. All of the walking tests were recorded by digital video and the 6MWD was measured.
Calculating the NSPS
The number of steps walked by each subject every 5 s was counted manually with a hand counter while viewing a video monitor. The walking speed (m/s) can be considered as the average step length (m/step) × NSPS (step/s). We defined that NSPS was calculated as the number of steps walked in a 5-s period divided by 5, and this was consecutively done 72 times (360 s ÷ 5 s) in each subject. Because NSPS is proportional to the walking speed, it usually decreases when a patient walks more slowly and falls to zero if the patient stops walking. The mean value of NSPS was defined as [ NSPS(5k)] ÷ 72, where NSPS(5k) is the value of NSPS at 5k s (k = 1, 2, 3, . . ., 72). The coefficient of variation (CV) of NSPS was calculated as follows: [SD/mean of NSPS] × 100 (%). The mean and CV of NSPS were determined in each subject.
Statistical analyses
The values are presented as the mean (SD). We used Mann-Whitney's U test for the assessment of any difference between healthy subjects and COPD patients (StatFlex, ViewFlex, Tokyo, Japan). Differences were considered to be statistically significant at P < 0.05.
RESULTS
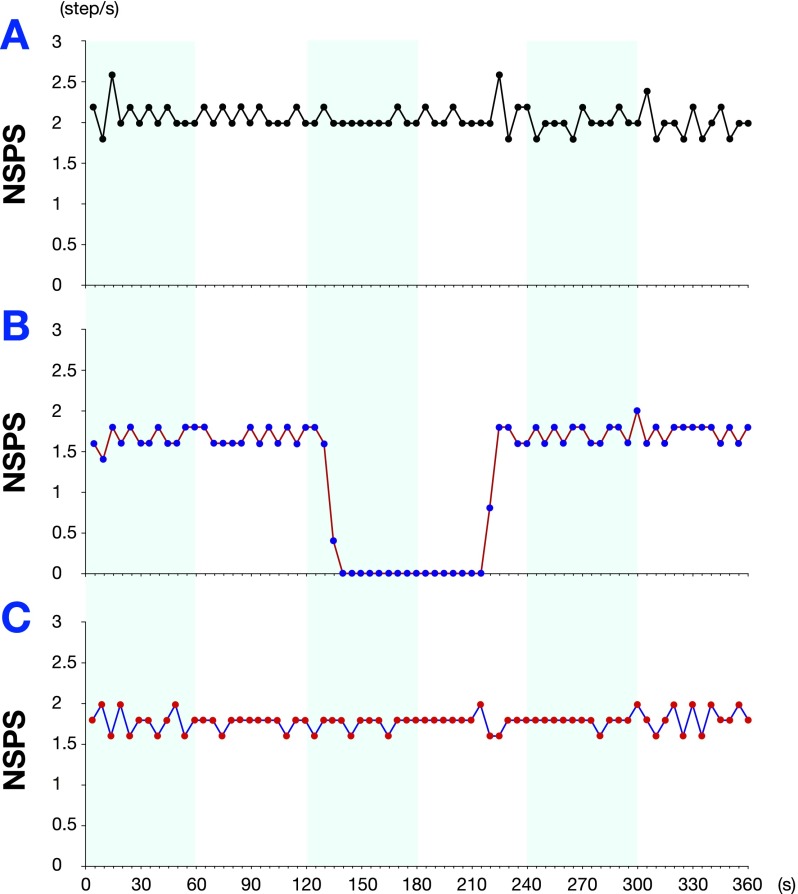
Figure 1 shows examples of the walking pattern determined from the NSPS in a healthy subject and 2 COPD patients with and without rest. NSPS increased as the walking pace became faster. While the healthy subject walked without resting, the patients rested for a total of 83 s (Fig. 1B). Table 1 shows the characteristics of all subjects and the results of the 6MWT with NSPS. The 6MWD of the healthy subject [486.9 (35.0) m] was significantly longer than that of the patients [289.5 (123.7) m]. Four of the 7 patients had to rest on a chair [1.0 (1.2) times] during the 6MWT, and the total resting time was 65.6 (83.8) s. In contrast, the healthy subject did not stop during the test. The mean NSPS of the healthy subject [1.98 (0.13) step/s] was significantly larger than that of the patients [1.42 (0.43) step/s]. The CV of NSPS, which assesses both the walking pace and the resting time, also showed a significant difference between the healthy subjects [7.4 (1.3) %] and the COPD patients [44.7 (45.3) %] (Table 1). The 6MWD of the patients without rest [405.0 (42.9) m] was significantly longer than that with rest [202.9 (77.7) m] (P < 0.05). The mean NSPS of patients without rest [1.80 (0.10) step/s] was significantly larger than that with rest [1.20 (0.37) step/s] (P < 0.05). The CV of NSPS of patients without rest [8.0 (1.4) %] was significantly smaller than that with rest [72.2 (41.9) %] (P < 0.05). The lowest SpO2 of patients without rest [92.7 (2.1) %] was significantly higher than that with rest [84.5 (4.9) %] (P < 0.05).
Fig. 1.
Walking patterns of a healthy subject and COPD patients based on the NSPS. The healthy subject (A: a 66-year-old woman) and the COPD patient with rest (B: a 64-year-old man) and the COPD patient without rest (C: a 68-year-old man) walked 504.5 m, 224.5 m and 356.5 m, respectively. Although the healthy could walk without stopping, the patient (B) rested for 83 s. When the walking pace is slower, the NSPS is smaller, and becomes zero if the patient stops walking. COPD, chronic obstructive pulmonary disease; NSPS, number of steps per second.
DISCUSSION
To improve the 6MWT, we determined NSPS as a new index. When we performed this modified 6MWT in healthy subjects and COPD patients, we found that the NSPS was useful for examining the walking property in the 6MWT.
The 6MWT has been reported to predict mortality in COPD patients2, 6 and this test has been used in many studies. Golpe et al.2 recently reported that exercise-related oxygen desaturation during the 6MWT was not an independent predictor according to multivariate analysis. However, some severe COPD patients cannot walk for 6 min without resting, and their walking pace is slower than that of healthy subjects. Some of our COPD patients rested during the 6MWT, and exercise-related oxygen desaturation could improve after resting. Therefore, if exercise-related oxygen desaturation is used as an index for predicting mortality, the resting time needs to be considered and previous reports are not clear about this point. In the present preliminary study, we examined the NSPS as a new index for the 6MWT that could be calculated easily. The mean and CV of NSPS in COPD patients were significantly different with and without rest. In particular, the CV of NSPS is an index of both the walking pace and the resting time. A graph of NSPS versus time displays the walking pattern of a patient during the 6MWT, and the results can be easily interpreted.
Consideration of walking steps during 6MWT may contribute new analyses of physiological condition in patients with COPD. Moreover, it has been reported that a 3-dimensional accelerometer can accurately detect steps while a subject is walking.7 Use of an accelerometer would allow the NSPS to be computed automatically. The present study has several limitations with the most obvious being its relatively small sample size. Also, we did not investigate a random sample of COPD patients with a spectrum of disease severity. We could not compare the clinical efficacy between 6MWD and NSPS. Further studies are needed to clarify the clinical usefulness and estimate whether the prognosis and mortality in COPD patients can be predicted by our new indices for the 6MWT.
The authors declare no conflict of interest.
REFERENCES
- 1.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117 [DOI] [PubMed] [Google Scholar]
- 2.Golpe R, Pérez-de-Llano LA, Méndez-Marote L, Veres-Racamonde A. Prognostic value of walk distance, work, oxygen saturation, and dyspnea during 6-minute walk test in COPD patients. Respir Care. 2013;58:1329–1334 [DOI] [PubMed] [Google Scholar]
- 3.Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990;16(Suppl 1):55–58 [DOI] [PubMed] [Google Scholar]
- 4.Solway S, Brooks D, Lacasse Y, Thomas S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 2001;119:256–270 [DOI] [PubMed] [Google Scholar]
- 5.Sciurba F, Criner GJ, Lee SM, Mohsenifar Z, Shade D, Slivka W; National Emphysema Treatment Trial Research Group. Six-minute walk distance in chronic obstructive pulmonary disease: reproducibility and effect of walking course layout and length. Am J Respir Crit Care Med. 2003;167:1522–1527 [DOI] [PubMed] [Google Scholar]
- 6.Casanova C, Cote C, Marin JM, Pinto-Plata V, de Torres JP, Aguirre-Jaíme A.Distance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPD. Chest. 2008;134:746–752 [DOI] [PubMed] [Google Scholar]
- 7.Jehn M, Schmidt-Trucksäess A, Schuster T, Hanssen H, Weis M, Halle M.Accelerometer-based quantification of 6-minute walk test performance in patients with chronic heart failure: applicability in telemedicine. J Card Fail. 2009;15:334–340 [DOI] [PubMed] [Google Scholar]