Abstract
Background
Tobacco dependence disorder is a chronic relapsing condition, yet treatment is delivered in discrete episodes of care that yield disappointing long-term quit rates.
Methods
We conducted a randomized controlled trial from June 1, 2004, through May 31, 2009, to compare telephone-based chronic disease management (1 year; longitudinal care [LC]) with evidence-based treatment (8 weeks; usual care [UC]) for tobacco dependence. A total of 443 smokers each received 5 telephone counseling calls and nicotine replacement therapy by mail for 4 weeks. They were then randomized to UC(2 additional calls) or LC(continued counseling and nicotine replacement therapy for an additional 48 weeks). Longitudinal care targeted repeat quit attempts and interim smoking reduction for relapsers. The primary outcome was 6 months of prolonged abstinence measured at 18 months of follow-up.
Results
At 18 months, 30.2% of LC participants reported 6 months of abstinence from smoking, compared with 23.5% in UC (unadjusted, P=.13). Multivariate analysis showed that LC (adjusted odds ratio, 1.74; 95% CI, 1.08–2.80), quit attempts in past year (1.75; 1.06–2.89), baseline cigarettes per day (0.95; 0.92–0.99), and smoking in the 14- to 21-day interval post-quit (0.23; 0.14–0.38) predicted prolonged abstinence at 18 months. The LC participants who did not quit reduced smoking more than UC participants (significant only at 12 months). The LC participants received more counseling calls than UC participants (mean, 16.5 vs 5.8 calls; P<.001), longer total duration of counseling (283 vs 117 minutes; P<.001), and more nicotine replacement therapy (4.7 vs 2.4 boxes of patches; P<.001).
Conclusion
A chronic disease management approach increases both short- and long-term abstinence from smoking.
Trial Registration
clinicaltrials.gov Identifier: NCT00309296
More than 75% of smokers report that they would like to quit, and approximately one-third of smokers attempt to quit each year, but less than 10% successfully achieve long-term abstinence.1 Current models for tobacco treatment involve discrete episodes of care, usually a combination of behavioral and pharmacologic strategies delivered during 6 to 12 weeks.2 Unfortunately, most smokers relapse within 3 months of treatment. Long-term abstinence measured 6 to 12 months after a quit attempt and when the individual is no longer receiving medication is consistently lower than at the end of treatment. Consequently, there is interest in whether treatment is discontinued prematurely and whether prolonged treatment might increase long-term abstinence.
The chronic nature of drug dependence, including nicotine, has been compared with other medical disorders, such as diabetes, hypertension, and asthma.3 In 2000, the US Public Health Service4 first designated tobacco dependence a chronic disease. Current models of tobacco treatment, 5 however, do not incorporate principles of chronic disease management, such as continuity of care, stepped care improvement (vs extinction) of symptoms, and self-management. Commentaries6,7 emphasize the chronic and relapsing nature of tobacco dependence, but there are few empirical tests of specific longitudinal treatment models for this disorder. Studies8,9 have tested methods to recycle smokers through treatment, but most protocols simply repeat prior interventions without addressing smoking behavior between quit attempts.
Smokers who relapse after a quit attempt are generally considered “failures.” This assessment neglects the fact that some people who resume smoking do so at a reduced level and maintain some smoking reduction long-term.10–13 There is controversy regarding the long-term sustainability and health benefits of smoking reduction,14 but we were interested in whether integration of smoking reduction, as an intermediate goal in a chronic disease management approach, has potential to keep smokers engaged in the quitting process. Smoking reduction might decrease nicotine dependence,15 increase motivation to quit smoking,16,17 and elicit additional cessation attempts.18
The objective of this randomized controlled trial was to test whether a longitudinal care approach—modeled on principles of chronic disease management—is more effective than a discrete episode of state-of-the-science treatment to promote prolonged smoking abstinence. The trial incorporated interim smoking reduction as an option for smokers who relapsed but emphasized it as a step toward the ultimate goal of quitting smoking completely.
METHODS
The protocol for the Tobacco Longitudinal Care Study was approved by the institutional review board at the University of Minnesota and Department of Veterans Affairs Medical Center, Minneapolis, Minnesota.
DESIGN OVERVIEW
This was a randomized controlled trial to compare long-term smoking cessation outcomes between longitudinal care (LC) and usual care (UC) treatment groups. The LC group received smoking cessation treatment (combined behavioral and pharmacologic therapies) for 1 year. This treatment recommended repeat quit attempts or smoking reduction for those who failed to quit after the initial attempt. The UC group received standard, evidence-based treatment that lasted 8 weeks. The primary outcome was 6 months of prolonged smoking abstinence, measured at 18 months.
SETTING AND PARTICIPANTS
We recruited participants from November 1, 2005, through July 31, 2007, in the Minneapolis–St Paul, Minnesota, region, working in cooperation with officers at regional labor unions. Inclusion criteria were men and women aged 18 to 80 with a history of smoking at least 5 cigarettes per day and interested in making a quit attempt in the next 14 days. Participants were required to have a personal telephone, speak English, and not be pregnant or plan pregnancy in the upcoming year.
RANDOMIZATION
Participants were randomly assigned to 1 of the 2 treatment groups by a computer-generated scheme, blocked in masked groups of 20. The randomization schedule was maintained by personnel independent from the study.
INTERVENTION
There was a counseling, medication, and run-in phase for both treatment groups. The intervention for both groups was conducted by 2 trained tobacco-cessation counselors and delivered by telephone. Each participant had a single counselor for the duration of treatment whenever possible. Calls were audiotaped and stored electronically. To ensure treatment fidelity, a clinical psychologist and a physician led weekly supervision meetings to review a random sample of calls and to discuss counseling and medication issues.
Nicotine patch, gum, and lozenge were available (free, delivered by mail) to the UC group for 8 weeks and to the LC group for 1 year. Nicotine replacement therapy (NRT) choices were modeled on common clinical practice and based on the principles that all participants (1) received medication unless they had a contraindication, (2) tried monotherapy before combination therapy, and (3) chose therapy type on the basis of prior experience, contraindications, intensity of withdrawal symptoms, and participant preference.
For the run-in period, all participants received identical evidence-based cessation treatment, with behavioral and pharmacologic components.2 Five scheduled calls took place during 4 weeks using a front-loaded, relapse-sensitive schedule shown to be effective in other trials19: before quitting, 1 to 3 days after quitting, then at 1 week, 2 weeks, and 4 weeks after quitting. The prequit call lasted 30 to 60 minutes and included designating a quit date, choosing medications, and making mailing arrangements. Call content included problem solving, skills training, social support, medication support, and relapse prevention.
If participants completed at least 3 of the 4 counseling calls planned during the first 2 weeks, they were randomized to the LC or UC protocol at 4 weeks. Treatment assignment was not revealed to the participant or counselor until the 4-week call.
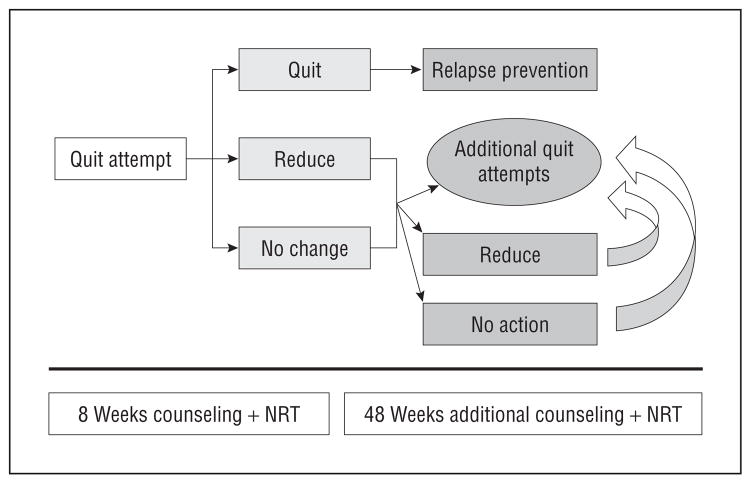
Longitudinal Care
The LC protocol started at the 4-week call and included contingencies for whether participants were abstinent, had relapsed (but to a reduced number of cigarettes), or had resumed the original amount of smoking (Figure 1). If participants were abstinent, counselors used relapse prevention strategies, including (1) identification of future high-risk situations and skills to handle them; (2) methods to maintain abstinence, such as lifestyle changes; (3) building self-efficacy and social support; and (4) issues of weight and exercise. Calls were made a minimum of monthly during the year.
Figure 1.
Longitudinal care smoking intervention. NRT indicates nicotine replacement therapy.
If participants relapsed, counselors urged them to make a new quit attempt as soon as they were willing. If participants were not interested in making another quit attempt, counselors explained that smoking reduction was an alternative and provided positive reinforcement for this choice as a step toward quitting. Counselors stressed a goal of at least 50% reduction from the baseline amount of cigarettes smoked (and <15 cigarettes per day), emphasizing that more reduction was better than less at any level of smoking. Strategies such as delaying smoking, eliminating cigarettes in specific situations, and scheduled reduction were discussed. Counselors aimed to call every 2 weeks, but the schedule was determined by participants’ progress and receptivity to the telephone sessions. If participants chose to neither make a quit attempt nor reduce smoking, calls were made monthly and they were asked again if they wanted to set a quit date or to reduce the amount of cigarettes smoked.
In the LC group, medications could be used for repeat quit attempts or to maintain smoking reduction. Participants who continued to smoke could use the same NRT as when they tried to quit, use an alternative form of NRT, increase the dose of NRT, or add another form of NRT to result in combination therapy. Choices between these options were based on past experience, intensity of nicotine withdrawal symptoms, and smoker preference. The NRT recommendations for reducers included 1 piece of 4-mg gum to substitute for 1 cigarette, or a 21-mg patch (for those who smoked >10 cigarettes per day).
Usual Care
At the end of the 4-week call, counselors explained to UC participants that they had 1 more call at 8 weeks and then treatment would be complete (a total of 6 calls). During the 8-week call, they were advised that if they wanted further treatment, they should contact resources available through their health insurance or in the community.
OUTCOMES AND FOLLOW-UP
Data were collected via telephone by trained research assistants masked to treatment assignment. Participants provided demographic information and completed a smoking history, Perceived Stress Scale,20 Center for Epidemiologic Studies–Depression Scale,21 and Alcohol Use Disorders Identification Test–Consumption22 at baseline. Follow-up data collection points were at 21 days and at 3, 6, 12, and 18 months; participants were paid $25 for each completed visit. Smoking outcomes were assessed using standard questionnaire items23,24 and the Timeline Followback procedure.25 The primary outcome was 6 months of prolonged abstinence, measured 18 months after the initial quit date. Secondary outcomes included 7-day point prevalent abstinence, total duration of abstinence, and smoking reduction. Intensity of treatment was measured by recording the number and duration of telephone sessions and the amount of medication sent to each participant.
STATISTICAL ANALYSIS
The proposed sample size for this trial (220 per group) was based on a hypothesized prolonged abstinence rate of 10% for UC and 20% for LC (power, 80%; α =.05). Summary statistics included means, SDs, medians, and ranges for continuous variables and frequency counts plus percentages for categorical or ordered characteristics. Comparisons between the LC and UC groups were made using the 2-sample t test or Wilcoxon rank sum test for quantitative factors. The Fisher exact test compared the 2 study arms for binary factors, including the unadjusted adherence rates. Prolonged abstinence and 7-day point prevalent abstinence at 18 months were compared between LC and UC groups using a multiple logistic regression that adjusted for patient characteristics and potential risk factors. Goodness of fit and diagnostic tests were applied to each final model. Possible interaction terms between significant covariates were evaluated. All outcome analysis was performed as intention-to-treat where participants who were not reached at follow-up time points were considered to be continuing smokers. To evaluate the change in abstinence over time, a generalized linear mixed-effects model for binary outcome (PROC GLIMMIX; SAS Institute, Cary, North Carolina) was used for prolonged (6, 12, and 18 months) and 7-day point prevalent abstinence (21 days through 18 months). All statistical analyses were performed using SAS, version 9.2 (SAS Institute). P <05 was considered statistically significant.
RESULTS
PARTICIPANTS
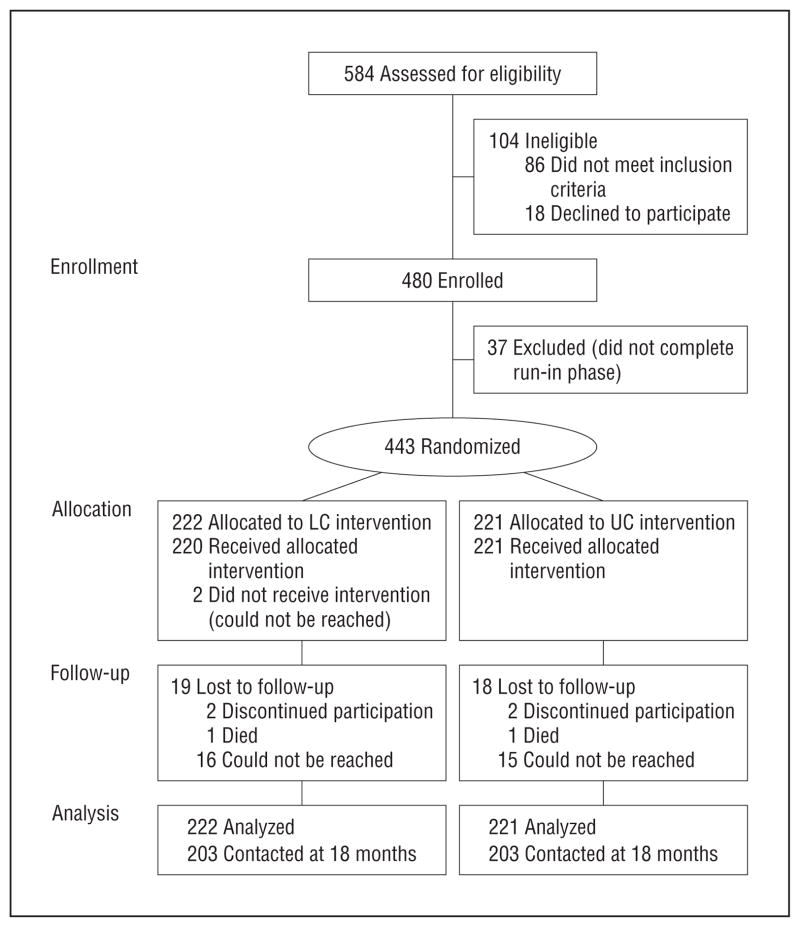
Of 584 individuals assessed for eligibility, 443 were randomized (Figure 2). Eighty-six were excluded for not meeting eligibility criteria, 18 declined to participate, and 37 did not complete the run-in phase (1 died, 7 refused, and 29 did not complete 3 of 4 scheduled calls). Of 222 participants assigned to LC, 220 received the intervention and 203 of 222 (91.4%) were reached for 18-month follow-up. Of 221 assigned to UC, 221 received the intervention and 203 of 221 (91.9%) were reached for 18-month follow-up.
Figure 2.
Diagram of participant flow. LC indicates longitudinal care; UC, usual care.
Baseline characteristics of participants are shown in Table 1. The mean age was 42 years, and 60.2% of the cohort was female. The mean (SD) number of cigarettes per day at baseline was 17.7 (8.2). There were no statistically significant differences in baseline characteristics between treatment groups.
Table 1.
Baseline Characteristics
| Characteristic | Longitudinal Care (n=222) | Usual Care (n=221) | P Value | |
|---|---|---|---|---|
| Demographic | ||||
| Age, mean (SD), y | 42.0 (12.3) | 42.4 (11.4) | .72 | |
| Sex, No. (%) | ||||
| Female | 132/222 (59.5) | 135/220 (61.4) |
|
.70 |
| Male | 90/222 (40.5) | 85/220 (38.6) | ||
| Employment status, No. (%) | ||||
| Full time | 190/222 (85.6) | 194/221 (87.8) |
|
.58a |
| Part time | 19/222 (8.6) | 15/221 (6.8) | ||
| Retired | 1/222 (0.5) | 2/221 (0.9) | ||
| Unemployed/unable to work | 12/222 (5.4) | 10/221 (4.5) | ||
| Marital status, No. (%) | ||||
| Never married | 65/222 (29.3) | 62/220 (28.2) |
|
.25b |
| Separated/divorced | 53/222 (23.9) | 45/220 (20.5) | ||
| Married | 98/222 (44.1) | 110/220 (50.0) | ||
| Widowed | 6/222 (2.7) | 3/220 (1.4) | ||
| Educational level, No. (%) | ||||
| ≤High school | 51/222 (23.0) | 46/219 (21.0) |
|
.65c |
| Some college | 104/222 (46.9) | 109/219 (49.8) | ||
| College graduate | 54/222 (24.3) | 54/219 (24.7) | ||
| Graduate school | 13/222 (5.9) | 10/219 (4.6) | ||
| Annual income, $, No. (%) | ||||
| <19 999 | 24/222 (10.9) | 25/221 (11.3) |
|
.98 |
| 20 000–39 999 | 85/222 (38.3) | 78/221 (35.3) | ||
| 40 000–59 999 | 72/222 (32.5) | 87/221 (39.4) | ||
| 60 000–74 999 | 26/222 (11.7) | 19/221 (8.6) | ||
| 75 000–99 999 | 6/222 (2.7) | 6/221 (2.7) | ||
| ≥100 000 | 2/222 (0.9) | 2/221 (0.9) | ||
| Don’t know/refused/missing | 7/222 (3.2) | 4/221 (1.8) | ||
| Hispanic or Latino ethnicity, No. (%) | 7/220 (3.2) | 6/219 (2.7) | >.99 | |
| Race, No. (%) | ||||
| White | 207/219 (94.5) | 205/217 (94.5) |
|
>.99d |
| Black | 8/219 (3.7) | 8/217 (3.7) | ||
| Other | 4/217 (1.8) | 4/217 (1.8) | ||
| Smoking history | ||||
| Age of regular smoking, y | ||||
| Mean (SD) | 17.3 (4.9) | 17.7 (4.4) |
|
.44 |
| Median (range) | 17.0 (9–52) | 17.0 (7–44) | ||
| Quit attempt in past 12 mo, No. (%) | 126/222 (56.8) | 136/221 (61.5) | .33 | |
| Cigarettes per day at baseline | ||||
| Mean (SD) | 17.9 (8.4) | 17.4 (7.9) |
|
.66 |
| Median (range) | 17.5 (5–50) | 20.0 (5–40) | ||
| Lives with a smoker, No. (%) | 87/221 (39.4) | 89/221 (40.3) | .92 | |
| Cigarette Dependence Scale-12 score, possible range 12–60 | ||||
| Mean (SD) | 46.2 (7.8) | 45.6 (7.0) |
|
.34 |
| Median (range) | 47.0 (20–59) | 46.0 (22–59) | ||
| Stress, depression, and alcohol use scores | ||||
| Perceived Stress Scale, possible range 0–16 | ||||
| Mean (SD) | 6.0 (3.0) | 6.1 (3.0) |
|
.57 |
| Median (range) | 6.0 (0–14) | 6.0 (0–15) | ||
| CES-D scale, possible range 0–60 | ||||
| Mean (SD) | 13.1 (8.7) | 13.1 (8.5) |
|
.98 |
| Median (range) | 11.0 (2–51) | 11.0 (2–54) | ||
| AUDIT-C, possible range 0–12 | ||||
| Mean (SD) | 4.5 (3.0) | 4.5 (2.7) |
|
.82 |
| Median (range) | 5.0 (0–11) | 4.0 (0–12) | ||
Abbreviations: AUDIT-C, Alcohol Use Disorders Identification Test–Consumption; CES-D, Center for Epidemiologic Studies–Depression.
Full time vs all other categories.
Married vs all other categories.
High school or less vs more than high school.
Whites vs nonwhites.
SMOKING CESSATION
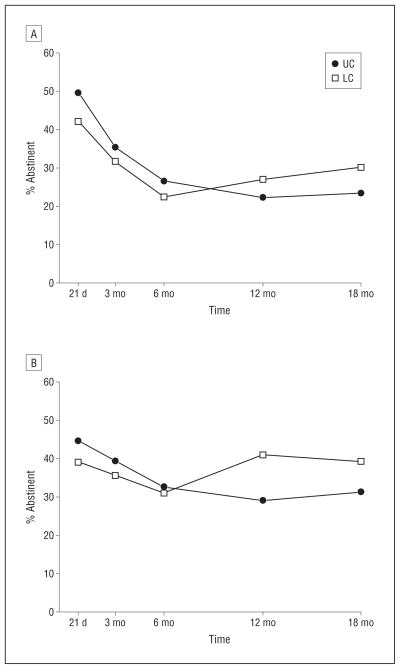
At 21 days after the first quit date (before randomization), 7-day point prevalent abstinence was reported by 39.2% in the LC group and 44.8% in the UC group (P=.25). Unadjusted rates of prolonged and 7-day point prevalent smoking abstinence from 21 days through 18 months are graphed in Figure 3. Abstinence rates were slightly higher in the UC group than in the LC group until 6 months. Subsequently, UC rates stabilized and LC rates continued to increase. At 18 months, 6-month prolonged abstinence was 30.2% in the LC group and 23.5% in the UC group (unadjusted, P=.13). Seven-day point prevalent abstinence followed a similar pattern.
Figure 3.
Graphs of unadjusted rates of prolonged abstinence (A) and 7-day point prevalent smoking abstinence (B) for intent-to-treat for 443 participants from 21 days through 18 months. LC indicates longitudinal care; UC, usual care.
Results of logistic regression to adjust for differences between groups at the time of randomization are shown in Table 2. The significant predictors of prolonged abstinence at 18 months were LC treatment arm (odds ratio, 1.74; 95% CI, 1.08–2.80; P=.02), quit attempt(s) in the past year (1.75; 1.06–2.89; P=.03), cigarettes per day at baseline (0.95; 0.92–0.99; P=.01), and cigarettes smoked in the past week reported at day 21 (0.23; 0.14–0.38; P<.001). We observed similar results for 7-day point prevalent abstinence. Repeated-measures analysis confirmed the significant effect of LC for both prolonged and 7-day point prevalent abstinence outcomes after accounting for the interaction between study group and time.
Table 2.
Logistic Regression for Prolonged Abstinence at 18 Months, Including Study Arm and Other Potential Baseline Characteristics, for 421 Participantsa
| Covariate | Odds Ratio (95% CI) | P Value |
|---|---|---|
| LC arm | 1.74 (1.08–2.80) | .02 |
| Age, y (increase of 1 y) | 1.02 (1.00–1.04) | .07 |
| Female sex | 0.83 (0.51–1.35) | .45 |
| Married | 1.32 (0.79–2.20) | .29 |
| Income (increase of 1 category)b | 0.99 (0.84–1.15) | .86 |
| Quit attempts in past y (yes) | 1.75 (1.06–2.89) | .03 |
| Cigarettes per day at baseline | 0.95 (0.92–0.99) | .01 |
| Live with smoker | 1.13 (0.68–1.87) | .64 |
| Time to first cig of the d | 1.22 (1.00–1.50) | .052 |
| CES-D scale (increase of 1) | 0.98 (0.95–1.01) | .18 |
| Smoked in past wk at d 21 | 0.23 (0.14–0.38) | <.001 |
Abbreviations: CES-D, Center for Epidemiologic Studies–Depression; LC, longitudinal care.
No 2-way interaction terms between the significant covariates had a P<.10.
Each category of annual income increased by $10 000 up to $60 000, then by $15 000 up to $75 000, then by $25 000 up to $100 000; the last category is $100 000 or more.
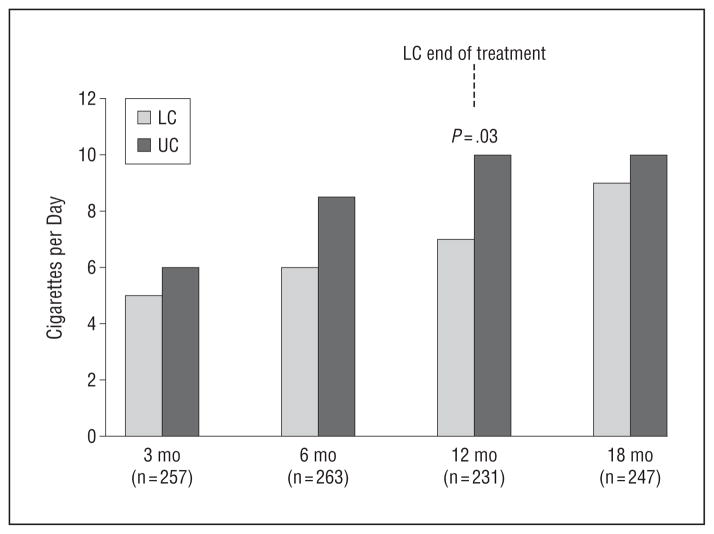
Daily cigarette use was recorded in the Timeline Followback starting from the initial quit date until the last contact. The median percentage of days reporting no cigarette use was 57.1% in the LC group and 30.1% in the UC group (P=.03). Among prolonged abstainers (n=119), the cumulative frequency of quitters in the LC group increased steadily through the 12-month treatment period following the initial quit, but there were only 7 additional quitters in the UC group after 8 weeks (end of treatment). Among participants who did not quit, there was more smoking reduction in the LC than UC group at all time points, but the differences were statistically significant only at 12 months (P=.03) (Figure 4).
Figure 4.
Smoking reduction in the longitudinal care (LC) and usual care (UC) groups: median number of cigarettes per day in nonquitters. At 3, 6, 12, and 18 months, the number missing was 15, 22, 32, and 19 for the LC and 10, 18, 25, and 19 for the UC group, respectively.
RECEIPT OF TREATMENT
Participants in the LC group made significantly more quit attempts than those in the UC group (mean, 8.7 vs 6.6; P=.009). The mean (SD) number of calls in the LC group was 16.5 (7.3) (range, 4–48), compared with 5.8 (0.6) (range, 3–8) in the UC group (P<.001). The mean (SD) total duration of counseling time in the LC group was 283 (172) minutes (range, 61–1115 minutes), compared with 117 (31) minutes (range, 35–200 minutes) in the UC group (P<.001). In the LC group, both behavioral and pharmacologic treatment continued during the year. The mean number of calls in the first, second, third, and fourth quarters of the year was 6.2, 3.1, 2.8, and 2.7, respectively.
Among UC participants, 59.3% used monotherapy (34.4% patch, 14.0% gum, or 10.9% lozenge), compared with 41.4% of LC participants (24.3% patch, 10.4% gum, or 6.8% lozenge) (P<.001). The most common combination therapies were patch plus gum and patch plus lozenge. More LC participants (13.1%) used patch, gum, and lozenge during the treatment than did UC participants (1.8%). Participants in the LC group received a mean of 4.7 boxes of nicotine patch (range, 0–21 boxes), compared with 2.4 boxes (range, 0–6 boxes) in the UC group (P<.001), and received 1.6 boxes of nicotine lozenge (range, 0–46 boxes), compared with 0.6 boxes (range, 0–6 boxes) in the UC group (P=.001). The difference between groups in receipt of nicotine gum followed the same trend, but was not significant. In the LC group, NRT continued to be prescribed during the year: the mean number of boxes of NRT for each quarter was 2.7, 1.0, 0.9, and 0.8, respectively. No serious adverse events related to treatment were reported.
On average, the cost of counseling per participant was $718 in the LC group compared with $379 in the UC group. Using competitive market prices, the mean cost of NRT per participant in the LC group was $226 compared with $107 in the UC group.
COMMENT
This randomized controlled trial shows that a smoking intervention based on chronic disease management principles of care—targeting the goal of quitting smoking but incorporating failures, setting interim goals, and continuing care until the desired outcome is achieved—is approximately 75% more effective at accomplishing long-term abstinence than delivery of a discrete episode of care for smoking cessation. The intervention lasted 1 year, but quit rates in the LC group continued to rise during the year without reaching a plateau, suggesting that treatment might be even more effective if extended longer.
The chronic disease management model may be more effective by providing more-intensive care and a long-term relationship with a counselor who comes to know and understand an individual, and therefore it may provide better social support than standard care. Incorporating a reduction strategy permitted counselors to provide positive reinforcement for outcomes other than cessation and to avoid framing relapse as a failure. A LC model not only reinforces the notion that cessation may necessitate an ongoing series of quit attempts but also allows counselors to adjust treatment in response to smokers’ ongoing experience with quitting. Smokers also receive more NRT, which may improve effectiveness. This intervention strategy differs from studies of extended treatment because it incorporates the probability of interim relapse. It differs from recycling studies because the intervention includes a plan for the period following relapse after a quit attempt, and subsequent quit attempts build on past experience.
Only a small number of published reports describe prolonged behavioral treatment for smoking cessation. A study by Hall et al26 compared 12-week treatment (control) with a 52-week treatment that included either extended NRT, extended cognitive behavioral treatment, or extended NRT and cognitive behavioral treatment. Extended cognitive behavioral treatment, but not NRT or combination therapy, resulted in a significant increase in 7-day point prevalent abstinence at 2 years (55% vs 36%; P=.01). Ellerbeck and colleagues27 compared moderate-intensity and high-intensity disease management interventions offered every 6 months for 2 years. They found smokers were willing to make repeated pharmacotherapy-assisted quit attempts, leading to progressively more smoking abstinence. Studies have also tested the effect of extending nicotine patch28,29 or bupropion30 treatment as a relapse prevention strategy but without impressive results.
A limitation of the trial we report is difficulty distinguishing the effects of extended behavioral treatment, extended medication treatment, and smoking reduction components of the intervention. Also, results were not biochemically confirmed, but the study population was not at high risk for incorrectly reporting smoking status. 31 Finally, smokers recruited from labor unions may not be representative of the smoking population at large.
In summary, these results demonstrate that a chronic disease model of care for treatment of tobacco dependence is more effective than a discrete episode of care. Unfortunately, when a smoker expresses the desire to stop smoking and tries to quit, the odds are against success. Clinical interventions should acknowledge the likelihood of relapse and incorporate this interim outcome into ongoing work toward the goal of complete abstinence. The efficacy of LC treatment should be tested in the varied settings in which tobacco treatment is delivered, including quit lines. Evidence from this study and others suggest this approach is feasible and that smokers will participate with success.
Acknowledgments
Funding/Support: This work was funded by grant P50 DA013333 (National Cancer Institute/National Institute on Drug Abuse) from the Transdisciplinary Tobacco Use Research Center on Tobacco Exposure Reduction.
Footnotes
Additional Contributions: We thank Greta Friedemann-Sanchez, PhD, for her contributions to the design of the data collection; Stephen Weiss, for cost analysis data; Bonnie Houg, PhD, and Kristen Murphy, for their counseling roles; and Anne Marie Weber-Main, PhD, for her critical review and edit of the manuscript.
Author Contributions: Drs Joseph, Fu, Rothman, Kodl, Lando, and Hatsukami had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Joseph, Fu, Rothman, Kodl, Lando, and Hatsukami. Acquisition of data: Joseph, Fu, Lindgren, Rothman, Kodl, and Doyle. Analysis and interpretation of data: Joseph, Fu, Lindgren, Rothman, and Kodl. Drafting of the manuscript: Joseph, Fu, Kodl, and Lando. Critical revision of the manuscript for important intellectual content: Joseph, Fu, Lindgren, Rothman, Kodl, Lando, Doyle, and Hatsukami. Statistical analysis: Lindgren and Kodl. Obtained funding: Joseph, Fu, Rothman, Lando, and Hatsukami. Administrative, technical, and material support: Joseph, Doyle, and Hatsukami. Study supervision: Joseph, Fu, Kodl, and Doyle.
Financial Disclosure: Dr Hatsukami has received funding from Nabi Biopharmaceuticals for conduct of a phase III clinical trial for a nicotine vaccine.
References
- 1.US Department of Health and Human Services (USDHHS), Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. . The Health Consequences of Smoking: A Report of the Surgeon General. Washington, DC: USDHHS; 2004. [Google Scholar]
- 2.PHS Guideline Update Panel, Liaisons, and Staff. [Accessed August 23, 2011];Treating tobacco use and dependence: 2008 update. 2008 http://www.rcjournal.com/contents/09.08/09.08.1217.pdf.
- 3.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 4.Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence: Clinical Practice Guideline. Rockville, MD: US Dept of Health and Human Services, Public Health Service; 2000. [Google Scholar]
- 5.Polisena J, Coyle D, Coyle K, McGill S. Home telehealth for chronic disease management: a systematic review and an analysis of economic evaluations. Int J Technol Assess Health Care. 2009;25(3):339–349. doi: 10.1017/S0266462309990201. [DOI] [PubMed] [Google Scholar]
- 6.Fiore MC, Baker TB. Smoking cessation treatment and the good doctor club. Am J Public Health. 1995;85(2):161–163. doi: 10.2105/ajph.85.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McLellan DL, Wright J. The National Women’s Tobacco Control Plan. J Public Health Policy. 1996;17(1):47–58. [PubMed] [Google Scholar]
- 8.Gourlay SG, Forbes A, Marriner T, Pethica D, McNeil JJ. Double blind trial of repeated treatment with transdermal nicotine for relapsed smokers. BMJ. 1995;311(7001):363–366. doi: 10.1136/bmj.311.7001.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lando HA, Pirie PL, Roski J, McGovern PG, Schmid LA. Promoting abstinence among relapsed chronic smokers: the effect of telephone support. Am J Public Health. 1996;86(12):1786–1790. doi: 10.2105/ajph.86.12.1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hughes JR, Cummings KM, Hyland A. Ability of smokers to reduce their smoking and its association with future smoking cessation. Addiction. 1999;94(1):109–114. doi: 10.1046/j.1360-0443.1999.9411097.x. [DOI] [PubMed] [Google Scholar]
- 11.Nørregaard J, Tønnesen P, Simonsen K, Petersen L, Säwe U. Smoking habits in relapsed subjects from a smoking cessation trial after one year. Br J Addict. 1992;87(8):1189–1194. doi: 10.1111/j.1360-0443.1992.tb02006.x. [DOI] [PubMed] [Google Scholar]
- 12.Hughes JR. Reduced smoking: an introduction and review of the evidence. Addiction. 2000;95(suppl 1):S3–S7. doi: 10.1080/09652140032008. [DOI] [PubMed] [Google Scholar]
- 13.Hughes J, Lindgren P, Connett J, Nides M. Lung Health Study. Smoking reduction in the Lung Health Study. Nicotine Tob Res. 2004;6(2):275–280. doi: 10.1080/14622200410001676297. [DOI] [PubMed] [Google Scholar]
- 14.Hughes JR, Carpenter MJ. The feasibility of smoking reduction: an update. Addiction. 2005;100(8):1074–1089. doi: 10.1111/j.1360-0443.2005.01174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farkas AJ. When does cigarette fading increase the likelihood of future cessation? Ann Behav Med. 1999;21(1):71–76. doi: 10.1007/BF02895036. [DOI] [PubMed] [Google Scholar]
- 16.Fagerström KO, Tejding R, Westin A, Lunell E. Aiding reduction of smoking with nicotine replacement medications: hope for the recalcitrant smoker? Tob Control. 1997;6(4):311–316. doi: 10.1136/tc.6.4.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riggs RL, Hughes JR, Pillitteri JL. Two behavioral treatments for smoking reduction: a pilot study. Nicotine Tob Res. 2001;3(1):71–76. doi: 10.1080/14622200020032114. [DOI] [PubMed] [Google Scholar]
- 18.Carpenter MJ, Hughes JR, Solomon LJ, Callas PW. Both smoking reduction with nicotine replacement therapy and motivational advice increase future cessation among smokers unmotivated to quit. J Consult Clin Psychol. 2004;72(3):371–381. doi: 10.1037/0022-006X.72.3.371. [DOI] [PubMed] [Google Scholar]
- 19.Zhu SH, Stretch V, Balabanis M, Rosbrook B, Sadler G, Pierce JP. Telephone counseling for smoking cessation: effects of single-session and multiple-session interventions. J Consult Clin Psychol. 1996;64(1):202–211. doi: 10.1037//0022-006x.64.1.202. [DOI] [PubMed] [Google Scholar]
- 20.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 21.Radloff L. CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 22.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. Ambulatory Care Quality Improvement Project (ACQUIP). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 23.Hughes JR, Benowitz N, Hatsukami D, Mermelstein RJ, Shiffman S. Clarification of SRNT workgroup guidelines for measures in clinical trials of smoking cessation therapies. Nicotine Tob Res. 2004;6(5):863–864. doi: 10.1080/1462220042000282564. [DOI] [PubMed] [Google Scholar]
- 24.Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob Res. 2003;5(1):13–25. [PubMed] [Google Scholar]
- 25.Sobell L, Sobell M. Timeline Followback Instructions and Materials for Alcohol, Cigarettes, Marijuana and Other Drugs and SCQ and DTCQ Feedback Programs. Toronto, CA: Addiction Research Foundation; 1996. [Google Scholar]
- 26.Hall SM, Humfleet GL, Muñoz RF, Reus VI, Robbins JA, Prochaska JJ. Extended treatment of older cigarette smokers. Addiction. 2009;104(6):1043–1052. doi: 10.1111/j.1360-0443.2009.02548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ellerbeck EF, Mahnken JD, Cupertino AP, et al. Effect of varying levels of disease management on smoking cessation: a randomized trial. Ann Intern Med. 2009;150(7):437–446. doi: 10.7326/0003-4819-150-7-200904070-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schnoll RA, Patterson F, Wileyto EP, et al. Effectiveness of extended-duration transdermal nicotine therapy: a randomized trial. Ann Intern Med. 2010;152 (3):144–151. doi: 10.7326/0003-4819-152-3-201002020-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tønnesen P, Nørregaard J, Säwe U, Simonsen K. Recycling with nicotine patches in smoking cessation. Addiction. 1993;88(4):533–539. doi: 10.1111/j.1360-0443.1993.tb02060.x. [DOI] [PubMed] [Google Scholar]
- 30.Killen JD, Fortmann SP, Murphy GM, Jr, et al. Extended treatment with bupropion SR for cigarette smoking cessation. J Consult Clin Psychol. 2006;74(2):286–294. doi: 10.1037/0022-006X.74.2.286. [DOI] [PubMed] [Google Scholar]
- 31.Velicer WF, Prochaska JO, Rossi JS, Snow MG. Assessing outcome in smoking cessation studies. Psychol Bull. 1992;111(1):23–41. doi: 10.1037/0033-2909.111.1.23. [DOI] [PubMed] [Google Scholar]