Abstract
Objective To compile and evaluate the evidence on the effects on health and social outcomes of computer based peer to peer communities and electronic self support groups, used by people to discuss health related issues remotely.
Design and data sources Analysis of studies identified from Medline, Embase, CINAHL, PsycINFO, Evidence Based Medicine Reviews, Electronics and Communications Abstracts, Computer and Information Systems Abstracts, ERIC, LISA, ProQuest Digital Dissertations, Web of Science.
Selection of studies We searched for before and after studies, interrupted time series, cohort studies, or studies with control groups; evaluating health or social outcomes of virtual peer to peer communities, either as stand alone interventions or in the context of more complex systems with peer to peer components.
Main outcome measures Peer to peer interventions and co-interventions studied, general characteristics of studies, outcome measures used, and study results.
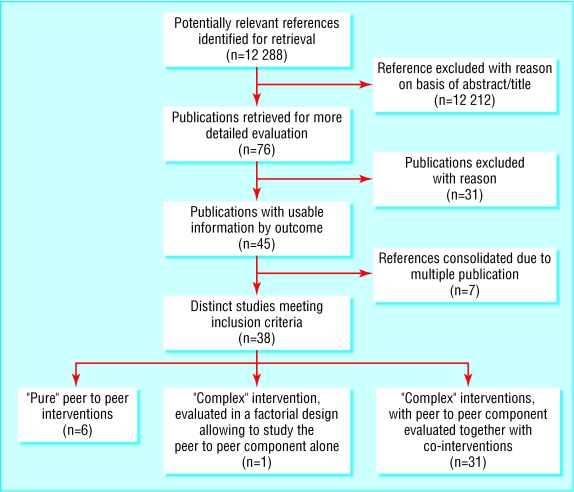
Results 45 publications describing 38 distinct studies met our inclusion criteria: 20 randomised trials, three meta-analyses of n of 1 trials, three non-randomised controlled trials, one cohort study, and 11 before and after studies. Only six of these evaluated “pure” peer to peer communities, and one had a factorial design with a “peer to peer only” arm, whereas 31 studies evaluated complex interventions, which often included psychoeducational programmes or one to one communication with healthcare professionals, making it impossible to attribute intervention effects to the peer to peer community component. The outcomes measured most often were depression and social support measures; most studies did not show an effect. We found no evidence to support concerns over virtual communities harming people.
Conclusions No robust evidence exists of consumer led peer to peer communities, partly because most peer to peer communities have been evaluated only in conjunction with more complex interventions or involvement with health professionals. Given the abundance of unmoderated peer to peer groups on the internet, research is required to evaluate under which conditions and for whom electronic support groups are effective and how effectiveness in delivering social support electronically can be maximised.
Introduction
One of the most promising aspects of the rise of ehealth is the widespread availability of electronic peer to peer community venues, where people with common interests gather “virtually” to share experiences, ask questions, or provide emotional support and self help. Virtual communities are social networks formed or facilitated through electronic media.1 Although such communities already existed in the era before the world wide web (for example, in bulletin board systems and private networks that enable peer to peer communities), the primary medium for virtual communities today is the internet, in mailing lists, newsgroups or usenet discussion forums, web based discussion forums, and live chatrooms. Virtual communities can be seen as mental health and social support interventions. They often have the function and character of self support groups and are then also called electronic support groups. As of April 2004 Yahoo!Groups (www.yahoo.com) listed almost 25 000 electronic support groups in the health and wellness section. Although plenty of descriptive and anecdotal information exists on the potential benefits2 and harms of online peer support,3 we sought evidence—beyond case studies and qualitative work—for the efficacy of virtual communities as stand alone or adjunct interventions in health care and their impact on health related outcome measures.
Methods
Inclusion and exclusion criteria
We sought randomised controlled trials, non-randomised controlled trials, and cohort studies to draw conclusions about effectiveness, as well as before and after studies and interrupted time series to draw conclusions about promising interventions. We retrieved observational and qualitative studies, cross sectional surveys, and content analyses of community interactions and used these to inform the background and discussion, but we did not systematically search for or abstract these studies. We included studies, in any language, published in peer reviewed journals or “grey” literature (dissertations, government reports, etc) that met the following criteria. Firstly, the intervention studied was a virtual community (or had a virtual community component), defined for the purpose of this study as a group of individuals with similar or common health related interests and predominantly non-professional backgrounds (patients, healthy consumers, or informal caregivers) who interact and communicate publicly through a computer communication network such as the internet, or through any other computer based tool (including non-text based systems such as voice bulletin board systems), allowing social networks to build over a distance. Secondly, the content focus of the virtual community was on health or healthcare issues in the broadest sense, including emotional and social support, health education, or health related behaviour change. Thirdly, the outcomes measured were knowledge, health, psychological or social outcomes, or use of health services. Fourthly, a control group (or a baseline measure) was present and outcome measures were reported.
We excluded studies where the only community building components were videoconferencing or telephone interactions or where the intervention was giving people computers, communication tools, or internet or web access (for example, studies such as the HomeNet4 study), unless participants were at the same time enrolled in a specific health related online support group.
Search strategy
Detailed search strategies are presented in appendix 1 on bmj.com. Briefly, we combined three search concepts “[self support and computer communication network] or e-communityvenue”, with various synonyms for each of these three concepts. To maximise recall we applied no methodological filters.
To cover not only the medical but also the social sciences and electronics literature, we conducted extensive searches across disciplines in the following bibliographical databases: Medline (Ovid, 1966-October 2003), Embase (Ovid, 1980-week 40, 2003), CINAHL (Ovid, 1982-October 2003), PsycINFO (Ovid, 1972-September 2003), Evidence Based Medicine Reviews (Ovid, second quarter 2003), Electronics and Communications Abstracts (CSA, 1981-October 2003), Computer and Information Systems Abstracts (CSA, 1981-October 2003), Educational Resources Information Center (ERIC; CSA, 1966-October 2003), Library and Information Science Abstracts (LISA, 1969-September 2003), ProQuest Digital Dissertations (ProQuest, 1997-October 2003), Web of Science (ISI, 1980-December 2003).
Study identification and abstraction
Two pairs of reviewers (GE-CR and JP-AS), with each reviewer working independently, each screened half of the abstracts to decide whether the full paper should be obtained. Disagreements were resolved by discussion. At least two reviewers then again screened full text articles, and a decision on including or excluding a study was made through discussion and consensus. At least one reviewer abstracted included studies into an electronic abstraction form (Microsoft Access), consisting of 72 questions pertaining to study characteristics and results. Team review and discussion of all abstracted studies ensured consistency in the abstraction of studies.
Results
Included studies
From all databases combined we identified and screened a total of 12 288 abstracts (figure). We selected 76 publications for retrieval of full text versions. Forty five publications met our inclusion criteria, describing 38 distinct studies: 20 randomised controlled trials, three meta-analyses of n of 1 trials, three non-randomised controlled trials, one cohort study, and 11 before and after studies (for included studies see tables A-D, for excluded studies see appendix 2, for multiple publications of the same study see appendix 3, all on bmj.com).
Figure 1.
CONSORT flow diagram of studies reviewed
Only six of these studies dealt with “pure” peer to peer interventions.5-10 One study had a 2×2 factorial design (full or control website combined with or without peer to peer group), enabling the comparison of a peer to peer group with a minimal co-intervention with other arms.11 The remaining 31 studies evaluated complex interventions where the virtual community was only an adjunct to a broader intervention that often included structured psychoeducational components or treatment programmes, entailed giving printed brochures or videos, computers or web television access to participants, incorporated decision support or one to one therapeutic relationships with health professionals, offered personal online diaries, or contained games (table A on bmj.com). Examples of such complex interventions with peer to peer “adjunct” components are CHESS, Computerlink, Starbright World, Bosom Buddies, and Student Bodies. Because of the multiple components within these interventions it is not possible to draw more generalisable conclusions about the value of online peer to peer communication from them, as the results will be confounded by the co-interventions.
Virtual communities evaluated as stand alone interventions
The six studies evaluating “pure” virtual communities were before and after studies evaluating web based discussion forums,6,10 a chat room,8 or a combination of a chat room and newsgroup,9 with one cohort study evaluating mailing lists7 and one non-randomised controlled trial evaluating a voice bulletin board system.5 We identified no randomised trials evaluating the effects of peer to peer communities alone. We found one factorial design randomised controlled trial that compared the effects of the different components (including the peer to peer component) of a complex intervention with each other.11 The reporting of this trial is incomplete, however, as no P values for all comparisons are provided. Of the six studies, only one7 dealt with unmoderated venues; the remaining studies all reported some degree of facilitation by a health professional. With one exception, even studies coded as “stand alone” peer to peer interventions therefore had involvement from health professionals, with trained individuals leading the groups as moderators or facilitators by stimulating discussions, formulating questions, or posting topics of interest or educational material on the bulletin boards.
Impact of virtual communities on health and social outcomes
Table B on bmj.com summarises the characteristics of the studies; tables C and D on bmj.com report quantitative and qualitative findings from them, respectively. Tables 1 and 2 summarise the outcome measures reported most often across all studies. Depression and social support (each used in 12 studies) were the most commonly used measures. Only three studies, among them a before and after study and a cohort study, found significant improvements in depression scores, and nine studies (among them eight randomised controlled trials) did not find or report an intervention effect on depression. Similarly conflicting are the data for social support measures; five studies found significant effects and seven studies did not.
Table 1.
Summary of most often used outcome measures except smoking and their results
| Outcome | Instrument | Study identifier (author, year, first page No; see table A on bmj.com for references) | Design | Significance level* |
|---|---|---|---|---|
| Depression | Centre for Epidemiological Studies depression scale (CES-D) | Barrera 2002-McKay 2002 | RCT | NS |
| Bass 1998-Casper 1995-Brennan 1995-McClendon 1998 | RCT | NS | ||
| Brennan 1998-489 | RCT | Not reported | ||
| Glasgow 2003-410 | RCT | NS | ||
| Houston 2002-2062 (“pure” peer to peer intervention) | Cohort study | P<0.05† | ||
| Lieberman 2003-920 (“pure” peer to peer intervention) | Before and after study | P<0.001‡ | ||
| McKay 2001-1328 | RCT | NS | ||
| Tate 2001-1172 | RCT | Not reported | ||
| Tate 2003-1833 | RCT | Not reported | ||
| Winzelberg 2003-1164 | RCT | P<0.01† | ||
| Beck depression inventory | Quick 1999-Thesis (“pure” peer to peer intervention) | Before and after study | NS | |
| Medical outcome survey | Gustafson 1999-1 | RCT | NS | |
| Social support | Modified 6 items from interpersonal support evaluation list (ISEL) | Barrera 2002-McKay 2002 | RCT | P<0.05† |
| Instrumental and expressive social support (IESS) scale | Bass 1998-Casper 1995-Brennan 1995-McClenndon 1998 | RCT | NS | |
| 4 item social support scale adapted from multidimensional scale of perceived social support (MPSS) | Celio 2000-650 | RCT | NS | |
| 5 point scale developed by the authors | Gustafson 1999-1 | RCT | P<0.05† | |
| 6 item social support scale | Gustafson 2001-435 | RCT | P<0.01† | |
| “Perceived support from friends and relatives” | Hamman 2002-Thesis (“pure” peer to peer intervention) | Before and after study | NS | |
| “Number of peer contacts initiated by group members” | Harvey-Berino 2002-103 | RCT | NS | |
| Perceived social support-friends scale | Hazzard 2002-69 | Controlled clinical trial | P<0.05† | |
| Medical outcomes study social support survey | Houston 2002-2062 (“pure” peer to peer intervention) | Cohort study | NS | |
| “Increased perception of support from peers” | Johnson 2001-E24 | Before and after study | P<0.05‡ | |
| Perceived social support scale | Lacoursiere 2003-Thesis | Controlled clinical trial | NS | |
| Online social support scale | Zabinski 2001-129 | Before and after study | Not reported | |
| Healthcare use | Fewer phone calls to doctors | Alemi 1996-32 | Controlled clinical trial | P<0.05† |
| More phone calls to providers | Gustafson 1999-1 | RCT | P<0.05† | |
| Visits to emergency departments | Gustafson 1999-1 | RCT | NS | |
| Non-emergency visits | Gustafson 1999-1 | RCT | NS | |
| Shorter duration of hospital visits | Gustafson 1999-1 | RCT | P<0.05† | |
| Fewer hospital admissions during intervention | Gustafson 1999-1 | RCT | P<0.05† | |
| Doctor's Visits | Lorig 2002-792 | RCT | NS | |
| Eating disorder | Eating disorder examination questionnaire (EDE-Q) | Celio 2000-650 | RCT | P<0.01† |
| EDE-Q-weight/shape subscale | Winzelberg 1998-339 | RCT | NS | |
| Winzelberg 2000-346 | RCT | NS | ||
| Zabinski 2001-401 | RCT | NS | ||
| Zabinski 2001-129 | Before and after | P<0.05‡ | ||
| Eating disorder inventory (EDI) drive for thinness subscale | Celio 2000-650 | RCT | P<0.05† | |
| Winzelberg 1998-339 | RCT | NS | ||
| Winzelberg 2000-346 | RCT | P<0.05† | ||
| Zabinski 2001-401 | RCT | NS | ||
| Zabinski 2001-129 | Before and after study | P<0.05‡ | ||
| EDI bulimia subscale | Winzelberg 1998-339 | RCT | NS | |
| Winzelberg 2000-246 | RCT | NS | ||
| Zabinski 2001-401 | RCT | NS | ||
| Zabinski 2001-129 | Before and after study | NS | ||
| Body mass index (BMI) | Winzelberg 1998-339 | RCT | NS | |
| Zabinski 2001-401 | RCT | NS | ||
| Zabinski 2001-129 | Before and after study | NS | ||
| Weight loss | Body weight | Harvey-Berino 2002-103 | RCT | NS |
| Harvey-Berino 2002-1254 | RCT | P<0.05†§ | ||
| Tate 2001-1172 | RCT | P<0.05† | ||
| Tate 2003-1833 | RCT | P<0.05ঠ| ||
| Diabetes control | Glycosylated haemoglobin | Barrera 2002-McKay 2002 | RCT | NS |
| Glasgow 2003-410 | RCT | NS | ||
| Hamman 2002-Thesis (“pure” peer to peer intervention) | Before and after study | NS | ||
| lafusco 2000-1853 (“pure” peer to peer intervention) | Before and after study | P<0.001‡ |
For a complete list of all outcome measures and their results see table C on bmj.com.
All P values refer to a within group comparison (before and after a peer to peer intervention or complex intervention with peer to peer component) or a between group comparison between an arm with peer to peer intervention or complex intervention and an arm without peer to peer intervention or complex intervention. A significant finding usually means significant differences in favour of a peer to peer intervention (or intervention with peer to peer component), unless otherwise indicated.
NS=non-significant at P<0.05 level.
Differences between groups for randomised controlled trials, controlled clinical trials, cohort studies.
Differences within groups (before and after, person to person intervention).
Favouring face to face support over internet group.
When considering control group (peer to peer support) as before and after design.
Table 2.
Summary of outcome measures for smoking and their results
| Smoking | Duration of abstinence, measured | Study identifier (author, year, first page No; see table A on bmj.com for references) | Design | % abstinent (of all participants who started the intervention) |
|---|---|---|---|---|
| For 7 days at 3 months | Feil 2003-189 | Before and after study | 18% | |
| For 7 days at 4 and 12 weeks after enrolment | Johs-Artisensi 2002-Thesis | RCT | 4%, 30% (NS)* | |
| For at least 3 months | Schneider 1986-274 | Before and after study | 31% | |
| For at least 3 months | Schneider 1986-277 | Before and after study | 25% | |
| After 1, 3, and 6 months | Schneider 1990-141 (“pure” peer to peer intervention) | RCT | 6.8%, 5.5%, 9.3% (NR)† | |
| In the past week at baseline, after the intervention, and 1 month after intervention | Woodruff 2001-239 | Before and after study | 7.7%, 15.4%, 23.1% |
NS=not significant at P<0.05 level. Compared with brochure only (18%, 32%). Authors also report 24 hour abstinence rates.
Abstinence rates at each of the three points in time in the arm with peer to peer group and minimal psychoeducational intervention, compared with abstinence rates in the control arm (no peer to peer group and minimal psychoeducational intervention), which were 3.6%, 2.9%; and 7.6%. NR=significance level for this comparison not reported.
Measures of healthcare use were obtained in only three studies, with contradicting results: Alemi et al, evaluating a voice bulletin board, reported a significant decrease, Gustafson et al a significant increase in phone calls to providers.5,12
Nine studies focused on structured weight loss or healthy body weight interventions with peer to peer components, again with mixed, but mostly non-significant, results. In one study the internet support group even sustained a significantly smaller weight loss than face to face support groups.13
Five studies evaluated communities for diabetic patients; four of them measured glycosylated haemoglobin as an outcome measure, which has repeatedly been shown to be responsive to educational and behavioural interventions in diabetes.14 Only one study (a before and after study without control) showed a significant improvement.12
Six studies investigated the effect of smoking cessation programmes that included peer to peer groups. In a factorial design randomised controlled trial11 the effect of the two main components (psychoeducation programme on the website and peer to peer group) were evaluated separately. Abstinence rates after 1, 3, and 6 months in the arm with peer to peer group and minimal information intervention were slightly higher than in the arm with no peer to peer group and minimal information (6.8%, 5.5%, 9.3% ν 3.6%, 2.9%, 7.6%, no P values reported). Abstinence rates were similar in the arm with peer to peer group and full psychoeducational intervention and the arm with no peer to peer group and full psychoeducational intervention (7.5%, 7.5%, 10% ν 6.6%, 6.6%, 10.8%). Similar to many other studies in this field, this randomised controlled trial had methodological problems, with more than half of the participants not responding to follow up surveys and low usage of the intervention (less than 10% used the intervention).
Quality of studies
Although we did not formally score quality, we coded certain aspects of study quality. Among the 20 randomised controlled trials, only three trials described their randomisation methods in sufficient detail to permit the ascertainment of allocation concealment. One randomised controlled trial had used a clearly inappropriate randomisation method, using the last digit of the Compuserve ID to determine the intervention.11 All studies were necessarily unblinded and most outcomes self reported. Intention to treat analysis had been conducted for only eight randomised controlled trials.
Discussion
Despite extensive searches in the health, social sciences, communication, and informatics literature we failed to find robust evidence on the health benefits of virtual communities and peer to peer online support. In 31 studies investigators evaluated complex interventions, combining, for example, educational or cognitive behaviour therapy components with peer to peer communities, making it impossible to draw conclusions on the effectiveness of “pure” electronic peer to peer interactions as used daily by millions of people participating in internet discussion groups or mailing lists. The six studies that investigated peer to peer communication as stand alone interventions tended to have less than optimum research designs with few participants. Half of the studies that evaluated “pure” peer to peer interventions were before and after studies. As many participants improve “naturally” over time (regression to the mean), these studies are insufficient to attribute improvements of psychological or health outcomes to the intervention. In those cases where authors found statistically significant effects, no information was given as to whether the (often minimal) group differences were clinically significant. Most studies were exploratory in nature and many investigators administered multiple instruments and made multiple comparisons, diminishing the worth of a “positive” finding (for example, in a study with 20 comparisons one would expect one comparison being “significant” on a 5% level by chance alone).
Possible explanations
The absence of evidence does not mean that virtual communities have no effect. Several explanations are possible for the lack of studies and evidence. Firstly, there is little commercial or professional interest in evaluating “pure” virtual communities and “unsophisticated” peer to peer interventions such as mailing lists, as opposed to more complex interventions or interventions led by health professionals. Secondly, studies investigating “natural” self helping processes are difficult to recreate in controlled research environments. Many studies seemed underpowered, and only five provided sample size calculations or justifications. Another possible explanation for the failure of many authors to show an effect of virtual communities is that participants may need to have the intrinsic desire to communicate with other people in order for virtual communities to be beneficial. Participants in self help groups may be a self selected subgroup in whom self help processes are effective, and researchers “recruiting from the street” may be looking at the wrong populations. A third possible (but related) reason could be lack of participants' “compliance.” Some investigators reported that the virtual community component was not heavily used,6,15-17 making it difficult to show an effect.
It was, however, encouraging that some interventions did show an effect, and that in only two instances the control was favourable over the virtual community in terms of a health outcome13 or resource use.12 In some studies7,18-20 an association between greater use of peer to peer groups and better outcomes was observed, indicating a dose-response association, but the direction of causation (whether increased use leads to better outcomes, or whether an improvement in outcomes such as depression due to other factors leads to increased use) is unclear.
No negative effects reported
It has been argued that online relationships are less valuable than offline ones and detract from social involvement with friends.21 Concerns have also been raised over quality,22-24 extreme verbal inhibition and aggression,25,26 hoaxes and spam,27 encouragement of suicide,28 and privacy issues29 on internet groups. In studies included for this review, no negative effect or harm has been reported. The absence of evidence does, however, not mean that such harm does not exist, in particular as most studies had high dropout rates and did not conduct an intention to treat analysis. We do not know what happened to the people who discontinued the studies and whether their inclusion would have shown a negative “net effect.”
In view of the wide variation in interventions, measurement tools, and populations studied, and the lack of methodological rigour in the majority of studies reviewed, the effect of online support groups on health related outcomes and healthcare resource use remains unclear.
Limitations
Only one database (LISA) has a subject heading for virtual communities; we may therefore have missed more complex ehealth systems or interventions that have peer to peer components if these were not evident from the abstract or title. However, we are unlikely to have overlooked studies evaluating “pure” electronic peer to peer interventions, and the paucity of such studies is striking.
Another concern is publication bias, which we attempted to minimise by including five dissertations. Their inclusion in this systematic review proved to be crucial. Interestingly, the four dissertations with “negative” (non-significant) findings remained unpublished whereas the one dissertation with positive results was published as a journal article; this implies that more (mostly negative) work may have been conducted but remained unpublished.
Implications for future research
Virtual communities are promising interventions, used everyday by millions on the internet. Many questions remain and should be the focus of future research. Little is known about the conditions and factors (of the group or individual) influencing outcomes. Whether virtual communities benefit from professional (or laypersons') moderation or facilitation is not clear either. With the exception of two studies, all investigators used professionally moderated or facilitated groups, or the level of moderation remained unclear. It is not clear whether virtual communities can substitute or complement face to face support groups. One study compared a computer mediated (voicemail) support group with a face to face group, noting that participation rates were significantly higher in the virtual group,5 but another study showed that virtual groups may be less effective than face to face groups to sustain weight loss.14 In terms of the outcome measures used, future studies should also include measures of resource use, as it is currently not clear whether participation in a peer to peer group reduces or increases the use of health care.
The lack of measurable evidence from controlled studies is in sharp contrast to the increasing body of anecdotal and descriptive information on the self helping processes in virtual communities, indicating that virtual communities are in fact the single most important aspect of the web with the biggest impact on health outcomes.30,31
Although qualitative studies—if conducted ethically—are needed and give fascinating insights into people's self helping processes in virtual communities,29 quantitative research is required to evaluate under which conditions and for whom electronic support groups are effective and how effectiveness in delivering social support can be maximised. Factorial design randomised controlled trials can help to evaluate which components of a complex intervention are contributing to an effect, but many problems remain, as by their nature they are not well defined, reproducible interventions, participants tend to be self selected, and participants for which the groups do not work are often lost to follow up. Given the abundance of unmoderated peer to peer groups on the internet, researchers must focus their efforts not only on sophisticated professionally led systems, but shift their attention to consumer led, self help venues. Perhaps in this way the research community can best help consumers to help themselves, a guiding principle of support groups regardless of the venue in which they occur.
What is already known on this topic
Thousands of electronic health related peer to peer support groups in the form of mailing lists, chat rooms and discussion forums are available on the internet
Anecdotal evidence shows that electronic peer to peer self help groups might be beneficial interventions, although some also warn of the dangers of such groups
To our knowledge, no systematic synthesis of the effects of peer to peer support groups has been conducted to date
What this study adds
Numerous controlled studies with peer to peer components have been conducted, but only a few evaluated the effect of peer to peer groups alone
Most studies failed to show an effect, or effects were confounded by potential effects of co-interventions
Quantitative studies with factorial design or evaluating pure peer to peer interventions are needed to provide robust evidence on the effects of peer to peer support groups
Supplementary Material
 Tables A-D and appendixes 1-3 are on bmj.com
Tables A-D and appendixes 1-3 are on bmj.com
Contributors: GE and JP have contributed equally to the study and are joint guarantors. GE wrote the first drafts of the protocol and the manuscript including all online tables, coordinated the research, and obtained funding; JP and AS compiled tables 1 and 2; GE and CR developed the extraction database; CR and AS coordinated obtaining the papers. GE, JP, AS and CR participated in the protocol development, screened abstracts, abstracted papers (GE and JP 15 each, AS 11, CR 7), and revised manuscript drafts. ME developed the search strategies and conducted the searches. ME, AS and CR are listed alphabetical, with the order of authors not necessarily reflecting their contribution
Competing interests: None declared.
Note about process: While GE has the same departmental affiliation and works (with AS and CR) in the same centre as Alejandro Jadad, guest editor of this theme issue, it was submitted to the BMJ in the normal way, and Jadad neither played any part in the decision making over this paper, nor was he involved in conception or conduct of this study.
References
- 1.Wellman B. An electronic group is virtually a social network. In Kiesler S, ed. Cultures of the internet. Mahwah, NJ: Lawrence Erlbaum, 1997: 170-205.
- 2.Landro L. Alone together. Cancer patients and survivors find treatment—and support—online. It can make all the difference. Oncologist 1999;4: 59-63. [PubMed] [Google Scholar]
- 3.Fearon B. Enter at own risk. Noticeboard 2003; 11.
- 4.Kraut R, Lundmark V, Patterson M, Kiesler S, Mukopadhyay T, Scherlis W. Internet paradox: a social technology that reduces social involvement and psychological well-being? Am Psychologist 1998;53: 1017-31. [DOI] [PubMed] [Google Scholar]
- 5.Alemi F, Mosavel M, Stephens RC, Ghadiri A, Krishnaswamy J, Thakkar H. Electronic self-help and support groups. Med Care 1996;34: OS32-OS44. [DOI] [PubMed] [Google Scholar]
- 6.Hamman CJ. Effect of a nurse-managed support group via an internet bulletin board on the perception of social support among adolescents with insulin-dependent diabetes mellitus [dissertation]. Texas Tech University, 2000: 1-102.
- 7.Houston TK, Cooper LA, Ford DE. Internet support groups for depression: a 1-year prospective cohort study. Am J Psychiatry 2002;159: 2062-8. [DOI] [PubMed] [Google Scholar]
- 8.Iafusco D, Ingenito N, Prisco F. The chatline as a communication and educational tool in adolescents with insulin-dependent diabetes: preliminary observations. Diabetes Care 2000;23: 1853. [DOI] [PubMed] [Google Scholar]
- 9.Lieberman MA, Golant M, Giese-Davis J, Winzlenberg A, Benjamin H, Humphreys K, et al. Electronic support groups for breast carcinoma. Cancer 2003;97: 920-5. [DOI] [PubMed] [Google Scholar]
- 10.Quick, Ben Gordon. The role of support groups on the Internet for those suffering from chronic kidney disease [dissertation]. University of the Pacific, 1999: 1-128.
- 11.Schneider SJ, Walter J, O'Donnell R. Computerized Communication as a medium for behavioral smoking cessation treatment: controlled evaluation. Comp Hum Behav 1990;6: 141-51. [Google Scholar]
- 12.Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F, et al. Impact of a patient-centered, computer-based health information/support system. Am J Prev Med 1999;16: 1-9. [DOI] [PubMed] [Google Scholar]
- 13.Harvey-Berino J, Pintauro S, Buzzell P, DiGiulio M, Casey GB, Moldovan C, et al. Does using the internet facilitate the maintenance of weight loss? Int J Obes Relat Metab Disord 2002;26: 1254-60. [DOI] [PubMed] [Google Scholar]
- 14.Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. 2003;29: 488-501. [DOI] [PubMed] [Google Scholar]
- 15.Johs-Artisensi JL. The effect of web-based support as an adjunct to a self-help smoking cessation program [dissertation]. University of North Texas, 2002: 1-121.
- 16.McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The diabetes network internet-based physical activity intervention: a randomized pilot study. Diabetes Care 2001;24: 1328-34. [DOI] [PubMed] [Google Scholar]
- 17.Winzelberg AJ, Taylor CB, Sharpe T, Eldredge KL, Dev P, Constantinou PS. Evaluation of a computer-mediated eating disorder intervention program. Int J Eat Disord 1998;24: 339-49. [DOI] [PubMed] [Google Scholar]
- 18.Dunham PJ, Hurshman A, Litwin E, Gusella J, Ellsworth C, Dodd PW. Computer-mediated social support: single young mothers as a model system. Am J Community Psychol 1998;26: 281-306. [DOI] [PubMed] [Google Scholar]
- 19.Bass DM, McClendon MJ, Brennan PF, McCarthy C. The buffering effect of a computer support network on caregiver strain. J Aging Health 1998;10: 20-43. [DOI] [PubMed] [Google Scholar]
- 20.Flatley-Brennan P. Computer network home care demonstration: a randomized trial in persons living with AIDS. Comput Biol Med 1998;28: 489-508. [DOI] [PubMed] [Google Scholar]
- 21.Cummings J, Butler D, Kraut R. The quality of online social relationships. Communications of the ACM 2002;45: 103-8. [Google Scholar]
- 22.Culver JD, Gerr F, Frumkin H. Medical information on the Internet: a study of an electronic bulletin board. J Gen Intern Med 1997;12: 466-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelly W, Connolly V, Bilous R, Stewart A, Nag S, Bowes D, et al. Reader beware: diabetes advice on the web. Pract Diabetes Int 2002;19: 108-10. [Google Scholar]
- 24.Houghton AR, Wolstenholme CR, Hudson I. What questions do patients ask in a cardiology newsgroup and how reliable are the answers? Br J Cardiol 2001;8: 165-8. [Google Scholar]
- 25.Kim MS, Raja NS. Verbal aggression and self-disclosure on computer bulletin boards [report]. Hawaii, 1991: 1-19.
- 26.Kayany JM. Contexts of uninhibited online behavior: flaming in social newsgroups on Usenet. J Am Soc Informat Sci 1998;49: 1135-41. [Google Scholar]
- 27.Ebbinghouse C. Frauds, hoaxes, myths, and chain letters: or, what's this doing in my e-mail box? Searcher 1998;6: 50-5. [Google Scholar]
- 28.Golant M, Winzelberg A, Lieberman M, States M, Berman H, Levy S, et al. Discussions about suicide in internet delivered cancer support groups. Psychooncology. 2003;12: S96. [Google Scholar]
- 29.Eysenbach G, Till JE. Ethical issues in qualitative research on internet communities. BMJ 2001;323: 1103-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferguson T. From patients to end users. BMJ 2002;324: 555-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eysenbach G. The impact of the internet on cancer outcomes. CA Cancer J Clin 2003;53: 356-71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.