Abstract
Introduction:
Product standards reducing the level of nicotine in cigarettes could significantly improve public health by reducing smoking behavior and toxicant exposure. However, relatively little is known about how the regulatory strategy could impact alcohol use, a closely related health behavior that is also a major contributor to morbidity and mortality. The primary objective of this paper is to predict the effect of nicotine reduction on alcohol use, identify priorities for future research, and highlight areas for mitigating any adverse outcomes.
Methods:
We critically reviewed and integrated literatures examining the effects of very low nicotine content (VLNC) cigarettes on smoking-related outcomes (nicotine exposure, nicotine withdrawal, and smoking as a cue to drink) and, in turn, the effects of those outcomes on alcohol use.
Results:
Current evidence suggests reducing the nicotine content of cigarettes may benefit public health by reducing alcohol use and problematic drinking over time as a consequence of reduced exposure to nicotine and the smoking cues associated with drinking. Nicotine withdrawal could increase risk of drinking, although these effects should be short-lived and could be mitigated by other sources of nicotine. Gender, hazardous drinking, and psychiatric comorbidities are likely to be important moderators of the effects of VLNC cigarettes.
Conclusions:
It is imperative to broadly assess the public health impact of potential tobacco product regulations by including measures of closely related health behaviors that could be impacted by these interventions. Nicotine reduction in cigarettes may contribute to improved public health through reductions in alcohol use.
INTRODUCTION
Cigarette smoking is the leading cause of preventable death in the United States, contributing to at least 400,000 deaths each year (Adhikari, Kahende, Malarcher, Pechacek, & Tong, 2009; Mokdad, Marks, Stroup, & Gerberding, 2004). The 2001 Institute of Medicine (IOM) report highlights that tobacco product regulations are critical methods to enhance national cessation rates (Stratton, Shetty, Wallace, & Bondurant, 2001). As originally proposed by Benowitz and Henningfield (1994), regulations mandating reduced nicotine levels in cigarettes below a “threshold” for dependence could lessen the negative health impact of cigarettes (Zeller & Hatsukami, 2009). Nicotine is the main addictive substance in tobacco that sustains smoking (Corrigall, 1999; Harvey et al., 2004; USDHSS, 1988). Product standards that drastically reduce nicotine content of cigarettes are now possible due to the Family Smoking Prevention and Tobacco Control Act (FSPTCA), which allows the Food and Drug Administration (FDA) to reduce nicotine levels in cigarettes to nonzero levels (Congress, 2009). Furthermore, the World Health Organization (WHO) Framework Convention on Tobacco Control, Article 9, describes anticipated guidelines for the regulation of the content and emissions of tobacco products (WHO, 2003).
The opportunity for regulations has prompted research to evaluate the public health impact of the regulatory strategy (Zeller & Hatsukami, 2009). A growing literature demonstrates that smoking very low nicotine content (VLNC) cigarettes decreases nicotine exposure, nicotine dependence and smoking (Benowitz et al., 2012; Donny, Houtsmuller, & Stitzer, 2007; Hatsukami, Heishman, et al., 2013; Hatsukami, Kotlyar, et al., 2010) and promotes abstinence (Hatsukami, Kotlyar, et al., 2010). VLNC cigarettes have substantially reduced levels of nicotine in the tobacco (e.g., 2mg/g; Benowitz & Henningfield, 1994; Benowitz et al., 2012) compared to conventional cigarettes (e.g., mean of 16mg/g; Kozlowski et al., 1998; Malson, Sims, Murty, & Pickworth, 2001), resulting in substantially lower nicotine yields (<0.2mg) than cigarettes typically sold in the United States (0.8mg). Furthermore, they are distinguishable from “light” or “mild” cigarettes that use filter ventilation to reduce nicotine yields and promote compensatory smoking (Benowitz, 2001; Bernert et al., 2005; Hecht et al., 2005). As a result, with VLNC cigarettes, smoking behavior decreases with little evidence of lasting compensation (Donny et al., 2007; Hatsukami, Heishman, et al., 2013; Hatsukami, Hertsgaard, et al., 2013; Hatsukami, Kotlyar, et al., 2010).
Enacting a low nicotine product standard for cigarettes (and possibly other tobacco products) requires evidence that the proposed standard would likely improve public health. While evidence will emphasize the effects on smoking and related exposure to harmful smoke constituents, estimates of the public health impact should include unintended consequences on nonsmoking behaviors (Henningfield et al., 1998). Of particular concern is alcohol use. Alcohol is widely used among smokers and a leading contributor of preventable morbidity and death (Mokdad et al., 2004). In the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), 21.7% of the total population reported using both alcohol and tobacco products during the past year (Falk, Yi, & Hiller-Sturmhöfel, 2006). Although the overall prevalence of co-use has likely declined due to reductions in tobacco use (Centers for Disease Control and Prevention, 2011), co-use remains widespread among smokers (McKee & Weinberger, 2013). Furthermore, co-use is higher among important risk groups, such as young adults and nicotine- or alcohol-dependent individuals (Falk et al., 2006). Thus, regulating tobacco products could have a widespread health impact among smokers by changing alcohol use.
While smoking and drinking are closely related, the effects of VLNC cigarettes on drinking remain unknown. To date, only one study has examined the effects of VLNC cigarettes on drinking (Barrett, Tichauer, Leyton, & Pihl, 2006). VLNC cigarettes reduced subsequent drinking relative to normal nicotine content cigarettes; however, the study relied on a single laboratory-based assessment in young adult men who were nondaily smokers.
The primary objective of this paper is to evaluate the current literature to predict the effect of nicotine reduction on alcohol use, identify priorities for future research, and highlight areas for mitigating any adverse outcomes. As described below, we focus on 3 primary pathways by which a reduction in the nicotine content of cigarettes might affect alcohol use. VLNC cigarettes would be expected to affect nicotine exposure, smoking as a cue to drink, and withdrawal (Figure 1) and each of these mechanisms could impact drinking.
Figure 1.
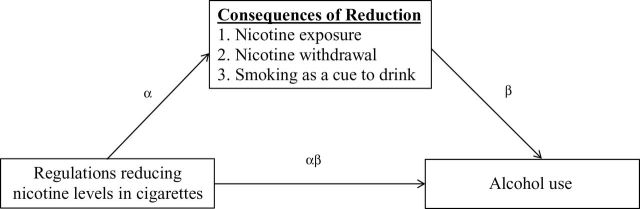
The processes linking nicotine reduction strategies to alcohol use in a mediation framework.
A Mechanistic Framework for Estimating the Effect of VLNC Cigarettes on Alcohol Use
Individuals co-use alcohol and tobacco products for several reasons (McKee & Weinberger, 2013; Neale & Kendler, 1995; Shiffman, Balabanis et al. 1995). Shared genetic or environmental risk factors may increase the risk of co-use (Neale & Kendler, 1995; Shiffman, Balabanis, Fertig, & Allen, 1995) without the behaviors being causally related (i.e., so-called third variable explanations). To the degree to which co-use results from shared risk factors, disrupting smoking will not likely affect drinking. Conversely, smoking and drinking may be causally linked such that the consequences of smoking cigarettes (e.g., nicotine exposure, behavioral aspects of smoking) increase the probability or effect of drinking (McKee, O’Malley, Shi, Mase, & Krishnan-Sarin, 2008; Shiffman, Balabanis et al., 1995). This paper focuses on the potential causal mechanisms in order to estimate the impact of nicotine reduction on alcohol use outcomes. Risk factors are considered in the context of potential moderating effects of these mechanisms.
The causal influence of VLNC cigarettes on drinking can be predicted by reviewing the empirical support for mechanisms that could mediate the impact of nicotine reduction. Specifically, one would anticipate an effect of VLNC cigarettes on drinking if: (a) VLNC cigarettes impact proposed mediators (e.g., nicotine exposure, smoking as a cue to drink, and withdrawal) (i.e., α) and (b) mediators impact alcohol outcomes (i.e., β; Figure 1) (Baron & Kenny, 1986). Thus, the present review aims to predict the public health impact of VLNC cigarettes on alcohol use over time by evaluating these pathways.
CAUSAL PATHWAYS LINKING VLNC CIGARETTE AND ALCOHOL USE
Nicotine Exposure
VLNC cigarettes immediately reduce nicotine delivery by substantially lowering the amount of nicotine in the tobacco (Hatsukami, Perkins, et al., 2010). Ad libitum smoking of a VLNC cigarette results in lower plasma nicotine and cotinine levels, a nicotine metabolite, than smoking a standard cigarette (Benowitz, Jacob, & Herrera, 2006; Pickworth, Fant, Nelson, Rohrer, & Henningfield, 1999). Immediately switching to VLNC cigarettes exclusively for 1 week (Hatsukami, Heishman, et al., 2013) or 6 weeks (Hatsukami, Hertsgaard, et al., 2013; Hatsukami, Kotlyar, et al., 2010) markedly reduces levels of cotinine and nicotine equivalents with cotinine approaching abstinent smoker levels within a week (Buchhalter, Acosta, Evans, Breland, & Eissenberg, 2005; Hatsukami, Heishman, et al., 2013). Thereafter, cotinine levels continue to decrease slowly (Hatsukami, Kotlyar, et al., 2010). Similar, but more gradual, reductions in nicotine exposure markers are observed when smoking progressively reduced nicotine content cigarettes for up to 6 months (Benowitz et al., 2007, 2012).
Relatedly, the risk of compensatory smoking behavior is low for cigarettes with VLNC, perhaps because it is difficult to meaningfully increase nicotine exposure through increased smoking (Hatsukami, Perkins, et al., 2010). As the nicotine content of tobacco in VLNC cigarettes is reduced, modified smoking (e.g., blocking ventilation holes of “light” cigarettes”) will not markedly increase nicotine yield. Nicotine intake would need to be increased by using products with unaltered nicotine levels. For instance, using the nicotine patch alongside VLNC cigarettes results in higher levels of salivary cotinine than using VLNC cigarettes alone (Donny et al., 2007; Hatsukami, Hertsgaard, et al., 2013), despite smoking fewer VLNC cigarettes per day (Hatsukami, Hertsgaard, et al., 2013). Similarly, using nonmedicinal products that contain nicotine (e.g., smokeless tobacco, e-cigarettes) could increase nicotine exposure. Little is known about multiproduct use because studies of VLNC cigarettes have limited other tobacco use by participants.
Reduced nicotine exposure impacts alcohol use. As previously described, smoking VLNC cigarettes reduced drinking relative to normal nicotine content cigarettes in a single laboratory session among nondaily smoking men (Barrett et al., 2006). Similar findings have been reported among young adult men who were nondaily smokers administered placebo or nicotine containing patches (Acheson, Mahler, Chi, & de Wit, 2006; Barrett et al., 2006). Unlike male nondaily smokers, young adult daily smokers who drink heavily and female nondaily smokers have exhibited increased alcohol use with a placebo relative to nicotine patch (Acheson et al., 2006; McKee et al., 2008), which suggests that gender, level of nicotine dependence, and hazardous drinking could moderate the relation between nicotine and drinking.
Together, the findings suggest that short-term reductions nicotine exposure impacts alcohol use; however, the effect of nicotine reduction on drinking over time has not been described. Moreover, in several of the studies, participants arrive to the lab deprived of smoking and nicotine, which introduces the confounding effects of smoking behavior and withdrawal symptoms on drinking (see discussions below). As a result, carefully reviewing the empirical support for the effects of nicotine per se on the determinants of alcohol use is warranted to predict the effects of VLNC cigarettes.
Direct Effects of Nicotine on the Effects of Alcohol
Nicotine may influence the effects of alcohol by (a) altering blood alcohol levels that correspond with an administered dose (i.e., alcohol metabolism) and (b) modulating the effects of alcohol at a given blood alcohol level (i.e.., reinforcement enhancement).
Nicotine could accelerate alcohol metabolism by increasing liver metabolic enzymes like cytochrome P4502E1 (CYP2E1) (Lieber, 1994; Matsumoto et al., 1996) and facilitating the initial metabolism of alcohol by gastric alcohol dehydrogenase (gADH) (Crabb, 1995) by slowing gastric emptying (Holt, Stewart, Adam, & Heading, 1980; Lim et al., 1993). Higher alcohol metabolic rate associated with increased gADH activity is believed to decrease risk for heavy drinking and has been linked to gender and ethnic variations in drinking (Agarwal & Goedde, 1992; Frezza et al., 1990). Nicotine exposure, however, has not consistently increased the availability of CYP2E1. CYP2E1 levels are similar in human smokers compared to nonsmokers, regardless of alcoholism history (Lucas et al., 1999; Lucas, Ménez, Girre, Berthou et al., 1995; Lucas, Ménez, Girre, Bodénez et al., 1995). In contrast, nicotine appears to acutely slow gastric emptying in a dose-dependent fashion among adolescent and adult rats and adult human daily smokers (Chen, Parnell, & West, 2001; Gritz et al., 1988; Johnson, Horowitz, Maddox, Wishart, & Shearman, 1991; Parnell, West, & Chen 2006). This is consistent with research that has detected delayed alcohol absorption as indicated by slower initial increases of blood alcohol levels among daily smokers exposed to nicotine administered by nasal spray and cigarettes compared to placebo (Johnson et al., 1991; Perkins et al., 1995). Similar effects have been detected in preclinical research (Chen et al., 2001); however, the effects of nicotine on blood alcohol levels have not been replicated in some preclinical (Collins, Burch, de Fiebre, & Marks, 1988) and clinical studies (McKee et al., 2008; Perkins, Fonte, & Grobe, 2000). Thus, nicotine reduction due to VLNC cigarettes may increase alcohol blood levels by quickening gastric emptying and promoting alcohol absorption.
Nicotine may also affect alcohol use by impacting the reinforcing properties of alcohol. Nicotine enhances the reinforcing properties of other reinforcers through a nonassociative process (Caggiula et al., 2009; Donny et al., 2003). Specifically, contingent and noncontingent nicotine administration enhances responding to other reinforcers (Barr, Pizzagalli, Culhane, Goff, & Evins, 2008; Chaudhri et al., 2006; Donny et al., 2003; Perkins & Karelitz, 2013). A recent review by McKee and Weinberger (2013) implicated nicotine as indirectly potentiating alcohol reward through the mesolimbic dopamine system. Consistent with this mechanism, young adults who smoke normal nicotine content cigarettes work harder on computer tasks to earn alcoholic beverages than those who smoke a VLNC cigarette (Barrett et al., 2006) and abstain from smoking overnight (Perkins et al., 2000). Furthermore, nicotine patches increased the price male nonsmokers would pay for alcohol relative to placebo; however, the opposite effect was observed among women (Acheson et al., 2006). Nicotine also increases operant responding for alcohol by male rats (Clark, Lindgren, Brooks, Watson, & Little, 2001; Lê, Corrigall, Harding, Juzytsch, & Li, 2000). Overall, it appears that nicotine may increase responding for alcohol among dependent (Perkins et al., 2000) and nondaily smokers (Acheson et al., 2006; Barrett et al., 2006), which is consistent with the reinforcement-enhancing properties of nicotine.
The reinforcement-enhancing effects of nicotine on alcohol use may also be explained by nicotine enhancing the subjective and behavioral effects of alcohol use (Zacny, 1990). The effects of alcohol are biphasic. At low doses and as blood alcohol levels increase, stimulant-like effects occur (Martin, Earleywine, Musty, Perrine, & Swift, 1993). In contrast, at high doses and as blood levels decrease, depressant-like effects are experienced. Together, the relative stimulant and sedating effects of alcohol influence its reinforcing properties such that greater stimulating effects and diminished sedating effects tend to promote drinking (King, de Wit, McNamara, & Cao, 2011; Quinn & Fromme, 2011).
Research suggests that nicotine could enhance the reinforcing properties of drinking by adding to its stimulant-like effects (Kouri, McCarthy, Faust, & Lukas, 2004; Perkins et al., 1995) while mitigating its depressant and sedating effects (Acheson et al., 2006; Perkins et al., 1995, 2000; Ralevski et al., 2012; Zancy, 1990). These effects may be partly explained by the shared role of the nicotinic acetylcholine receptor (nAChR) system in nicotine and alcohol reinforcement (see McKee & Weinberger, 2013, for review). Specifically, nicotine exerts its effects through the nAChR system (Benwell, Balfour, & Anderson, 1988; for review Buisson & Bertrand, 2002), which has also been implicated in the effects of alcohol (for review, see Chi & de Wit, 2003; Davis & de Fiebre, 2006; Dohrman & Reiter, 2003). Indeed, among nonsmokers, a nAChR antagonist, mecamylamine, reduces subjective stimulant responses to alcohol (Blomqvist, Hernandez-Avila, Van Kirk, Rose, & Kranzler, 2002; Chi & de Wit, 2003) even after controlling for blood alcohol levels (Blomqvist et al., 2002; Young, Mahler, Chi, & de Wit, 2005). Likewise, the AChR partial agonist varenicline reduces alcohol self-administration among heavy drinking smokers (McKee et al., 2009). Hence, nicotine-induced changes in the function and/or number of nAChRs would mediate changes in the pharmacological effects of alcohol at a given blood concentration.
It is important to note that the effects of nicotine on the subjective effects of alcohol, particularly the stimulant effects, have not been consistently replicated (Perkins et al., 2000; Ralevski et al., 2012). While the inconsistencies may be partly explained by variability in the administration and doses of nicotine and alcohol examined (for review, Perkins, 1997), the desensitization of nAChRs due to nicotine may also play a role (Picciotto, Addy, Mineur, & Brunzell, 2008). Specifically, repeated exposure to nicotine may reduce the responsivity of particular nAChR subtypes to nicotine and other drugs. Furthermore, individual difference factors may explain the variability. Nicotine may enhance the stimulant-like effects strongly among women and attenuate the depressant effects primarily among men (Perkins et al., 1995) contributing to gender differences in response (Acheson et al., 2006). Similarly, a subset of smokers who drink to cope with stress may prefer the sedating effects (Cooper, Frone, Russell, & Mudar, 1995), which would make the effects of nicotine on the sedating effects undesirable. Thus, outside of instances where the sedating effects of alcohol are preferred, nicotine reduction may reduce alcohol use after smoking because the stimulant-like effects would no longer be enhanced.
Nicotine Withdrawal
An anticipated consequence of nicotine reduction is the emergence of withdrawal symptoms including negative affect, cognitive impairment, and physical discomfort (Hughes, Higgins, & Hatsukami, 1990). Previous research has detected increased withdrawal symptoms after immediately switching to VLNC cigarettes (Hatsukami, Hertsgaard, et al., 2013; Hatsukami, Kotlyar, et al., 2010), but not while gradually switching to VLNC cigarettes over the course of 6 months (Benowitz et al., 2012). On average, withdrawal increases within 1 day of switching to VLNC cigarettes (Buchhalter, Acosta, et al., 2005) and returns to baseline levels within 2 weeks (Hatsukami, Hertsgaard, et al., 2013; Hatsukami, Kotlyar, et al., 2010). The withdrawal symptoms associated with immediately switching to VLNC cigarettes tend to be less severe than withdrawal following total smoking abstinence and select symptoms, such as craving, may not significantly increase at all (Benowitz et al., 2007; Buchhalter, Acosta, et al., 2005; Buchhalter, Schrinel, & Eissenberg, 2001; Donny et al., 2007; Hatsukami, Kotlyar, et al., 2010). Immediately switching to VLNC cigarettes appears to specifically increase restlessness, impatience, difficulty concentrating (Buchhalter, Acosta, et al., 2005), irritability, and eating (Buchhalter, Acosta, et al., 2005; Donny & Jones, 2009).
Withdrawal symptoms after switching to VLNC cigarettes are likely transient; however, it may be important to minimize discomfort when switching to the product for the first time among key risk groups. Several psychiatric comorbidities predict abstinence-related withdrawal severity and could also play a role in withdrawal associated with VLNC cigarettes, such as depression, anxiety, disordered eating, attention deficit hyperactivity disorder (ADHD), and other substance or alcohol dependencies (McClernon et al., 2011; Pomerleau, Marks, & Pomerleau, 2000; Pomerleau et al., 2005; Weinberger, Desai, & McKee, 2010). Furthermore, women report more withdrawal after smoking abstinence than men, particularly negative affect (Evans, Blank, Sams, Weaver, & Eissenberg, 2006; Leventhal et al., 2007). Notably, although these individual differences are reliably observed in the context of smoking cessation, it remains unknown if the same disparities would occur with VLNC cigarettes because the sensory and behavioral aspects of smoking would be largely intact. For example, individuals diagnosed with schizophrenia are at an increased risk of withdrawal following smoking cessation; however, they exhibit similar withdrawal suppressing effects of VLNC cigarettes to individuals without schizophrenia (Tidey, Rohsenow, Kaplan, Swift, & AhnAllen, 2013). Likewise, nonpharmacological aspects of smoking, such as visual or olfactory cues, appear to be particularly important predictors of smoking behavior among women (Perkins et al., 2000; Perkins, Jacobs, Sanders, & Caggiula, 2002), which could diminish the gender difference in withdrawal in the context of VLNC cigarette use.
Withdrawal-induced negative affective and tension states could put smokers at risk for alcohol use. Several motivational theories of alcohol use suggest that individuals may learn to drink alcohol in order to cope with negative affective states (Cooper et al., 1995; Wills & Shiffman, 1985). Drinking to cope is most common among individuals who lack alternative coping strategies to reduce negative affect (Cooper et al., 1995; Dermody, Cheong, & Manuck, 2013). As smokers typically alleviate withdrawal symptoms by smoking (Baker, Brandon, & Chassin, 2004), smokers who do not experience complete withdrawal relief from smoking VLNC cigarettes may resort to alternative substances to regulate their negative affect symptoms. Alleviating negative affect is a motive for drinking among smokers (Novak, Burgess, Clark, Zvolensky, & Brown, 2003). As a result, a smoker’s alcohol use may increase when withdrawal increases, which may be more likely to occur during the first 2 weeks of switching to VLNC cigarettes.
Consistent with the role of self-medicating nicotine withdrawal, smokers who demonstrated significantly elevated withdrawal symptoms after smoking abstinence increase their alcohol use relative to individuals who wore a nicotine containing patch (McKee et al., 2008) or smoked a normal nicotine content cigarette (Palfai, Monti, Ostafin, & Hutchison, 2000). In contrast, in one study of abstinent nicotine-dependent smokers, participants did not increase their alcohol use (Perkins et al., 2000). It is unclear if the findings contradict the other studies because withdrawal levels were not reported. It is expected that self-medication motives would be less prevalent among individuals who generally experience fewer withdrawal symptoms, such as among nondaily smokers (Shiffman, Paty, Gnys, Kassel, & Elash, 1995). Among nondaily smokers, smoking and alcohol use are related; however, the associations are more consistent with reinforcement enhancement than self-medication motives. Specifically, with the exception of women in one study (Acheson et al., 2006), abstinent nondaily smokers have exhibited less drinking than individuals who were exposed to nicotine or smoked (Acheson et al., 2006; Barrett et al., 2006). Together, the findings suggest that alcohol use could increase among nicotine-dependent smokers who experience withdrawal when switching to VLNC cigarettes.
Factors associated with motives to drink to cope, such as a history of heavy drinking, female gender, or age, could increase one’s risk for drinking to cope with nicotine withdrawal. A history of alcohol dependence is associated with drinking as coping strategy for negative affect (Carpenter & Hasin, 1999; Cooper et al., 1995), which could occur with withdrawal. Consistent with alcohol dependence as a risk factor, smoking abstinence appears to predict increased drinking among hazardous drinkers (McKee et al., 2008; Palfai et al., 2000), but not moderate drinkers (Perkins et al., 2000). Smoking abstinence, however, does not appear to predict drinking urges among alcohol-dependent individuals early in recovery (J. L. Cooney, N. L. Cooney, Pilkey, Kranzler, & Oncken, 2003). Similarly, women are at risk for self-medicating negative affect with alcohol (for review, Nolen-Hoeksema, 2004; Hesselbrock & Hesselbrock, 2006), particularly once they reach adulthood (for review, Kuntsche, Knibbe, Gmel, & Engels, 2006). Gender differences in alcohol use after brief smoking abstinence have not been consistently supported (e.g., a few hours or overnight) (Palfai et al., 2000; Perkins et al., 2000). Thus, smoking VLNC cigarettes could negatively impact individuals at risk for drinking to cope, such as women and those with a history of alcohol dependence symptoms.
Despite the risk of self-medicating withdrawal symptoms, the transient nature of withdrawal suggests that compensatory drinking via this mechanism would be short-lived. On average, withdrawal after switching to VLNC cigarettes should dissipate within 2 weeks (Hatsukami, Perkins, et al., 2010), which highlights a key time period for future research to explore risk of compensatory drinking. Thereafter, negative affect and stress tend to decrease below prequit levels (for review, Kassel, Stroud, & Paronis, 2003). As a result, over time, VLNC cigarettes could reduce negative affect and stress by limiting nicotine exposure and promoting smoking cessation, which would reduce the need to self-medicate these symptoms by drinking.
Smoking as a Cue to Drink
As previously described, the primary mechanism by which nicotine reduction in cigarettes would improve public health is through a reduction in smoking behavior. Research suggests that individuals smoke a VLNC cigarette similarly to a usual brand cigarette when trying them for the first time. In particular, there are no significant differences in puffing behavior, expired carbon monoxide levels (Nadal, Chappell, & Samson, 1998; Rose & Behm, 2004), or tar exposure (Benowitz et al., 2006) per cigarette beyond the first 2 VLNC cigarettes smoked among adults (MacQueen et al., 2012). Among adolescents, puffing behavior has been shown to increase while smoking a VLNC cigarette relative to a high-yield nicotine cigarette (Kassel et al., 2007); however, it is important to determine if the compensatory changes in smoking may dissipate after multiple smoking bouts as has been seen among adult smokers.
Prolonged use of VLNC cigarettes tends to gradually decrease the number of VLNC cigarettes smoked per day. On average, within the first week of switching to VLNC cigarettes, treatment-seeking individuals smoke VLNC cigarettes at a similar rate to normal nicotine content cigarettes (Hatsukami, Heishman, et al., 2013; Hatsukami, Kotlyar, et al., 2010). Thereafter, VLNC cigarette use appears to decrease gradually (Hatsukami, Heishman, et al., 2013; Hatsukami, Hertsgaard, et al., 2013; Hatsukami, Kotlyar, et al., 2010), and in one study, reached significant reductions within 2 weeks and reductions of nearly 8 cigarettes per day after 6 weeks of use (Hatsukami, Kotlyar, et al., 2010). Furthermore, nontreatment seekers smoked approximately 4 fewer VLNC cigarettes per day after using the product exclusively in an in-patient setting for 8 days (Donny et al., 2007). In cases where the nicotine content of cigarettes is progressively reduced over time in nontreatment seekers, reductions in cigarettes per day are relatively small and delayed (Benowitz et al., 2012). Thus, the reinforcing properties of VLNC cigarettes may lessen over time such that smoking behavior gradually decreases, with the most rapid effects on smoking behavior after immediately switching to VLNC cigarettes.
In addition to reducing cigarettes smoked, VLNC cigarettes may facilitate successful quit attempts. Smoking VLNC cigarettes appears to increase self-efficacy ratings and contemplating making a quit attempt among individuals who were not previously interested in quitting smoking (Benowitz et al., 2007, 2012). Furthermore, smoking VLNC cigarettes for up to 6 weeks improves quit rates among treatment-seeking smokers (Hatsukami, Kotlyar, et al., 2010; Walker et al., 2012), although this effect has not been consistently replicated (Hatsukami, Hertsgaard, et al., 2013). In particular, 23% of individuals using VLNC cigarettes alongside Quitline care achieved continuous abstinence for 6 months compared to 15% using Quitline care alone (Walker et al., 2012). Similarly, 30% of individuals who make a quit attempt after smoking VLNC cigarettes achieved CO and cotinine verified abstinence for 4 weeks compared to 14% of individuals who smoked cigarettes with an intermediate nicotine yield (0.3mg; Hatsukami, Kotlyar, et al., 2010).
Among nonsmokers, it is also anticipated that VLNC cigarettes will prevent smoking initiation. For legal and ethical reasons, examining the effects of VLNC cigarettes on smoking uptake is not possible using human subjects. However, animal research has demonstrated that rats do not acquire self-administration at very low nicotine doses (Donny et al., 2012). Furthermore, nicotine appears to be an important determinant of smoking behavior among youth (Collins et al., 2010; Kassel et al., 2007; Veilleux et al., 2011), which suggests that VLNC cigarettes could prevent smoking uptake among adolescent nonsmokers.
VLNC cigarettes could impact alcohol outcomes by altering the ability of smoking to cue alcohol use. Among smokers, smoking may act as a drug cue for alcohol use. Research suggests that presenting drug cues, such as drug images, may promote drug urges and use (Carter & Tiffany, 1999). Specifically, images of alcoholic beverages been shown to increase urges to drink among drinkers compared to nonalcohol cues (Drobes, 2002; George et al., 2001), particularly among alcoholics (Thomas, Drobes, & Deas, 2005). In addition to alcohol-specific cues, cigarettes may act as a cue for drinking (Shiffman, Balabanis, et al., 1995). The repeated co-use of these substances among individuals may establish conditioned associations between them such that smoking behavior may cue subsequent drinking.
Smoking appears to act as a behavioral cue for drinking. Among alcohol-dependent smokers, smoking-related images have been shown to increase drinking urges compared to neutral and unpleasant images, producing similar effects as alcohol-related images (Drobes, 2002). While exposure to smoking-related images also increased drinking urges among social drinkers, the effect was not as robust. Similarly, among young adults who are heavy social drinkers, holding a lit cigarette did not influence drinking urges, expectancies, or volume consumed, compared to holding a pencil regardless if the individual was nicotine deprived or not (Palfai et al., 2000). It is possible that smoking is a weaker behavioral cue for drinking among social drinkers because smoking frequently occurs without drinking. Specifically, smoking typically follows a daily cycle (Chandra, Shiffman, Scharf, Dang, & Shadel, 2007); whereas, normative drinking among smokers does not occur daily and is concentrated on weeknights or weekends (Jackson, Colby, & Sher, 2010; Shiffman, 2009). In contrast, among alcohol-dependent smokers, an extensive history of alcohol and smoking co-use may set up cigarettes as a cue for drinking. Likewise, alcohol use may also be closely tied to smoking among nondaily smokers, who tend to smoke and drink concurrently (Harrison & McKee, 2008; Jackson et al., 2010). Thus, reduced smoking frequency after switching to VLNC cigarettes could reduce alcohol use and weaken the association between cigarette cues and alcohol use.
It is also anticipated that the effectiveness of smoking as a behavioral cue to drink will be undermined by very low levels of nicotine in the cigarettes. As previously described, nicotine appears to the primary factor through which smoking increases the reinforcing process of alcohol. Thus, if the nicotine in regular cigarettes acts as a discriminative stimulus that predicts enhanced alcohol reward, smoking VLNC cigarettes would not be expected to produce the same effect on drinking. Instead, over time, smoking cues would come to predict low (not high) doses of nicotine and may not trigger the same urge to drink. As a result, VLNC cigarettes could reduce the urge to drink while smoking even in the context of continued smoking behavior.
SUMMARY
While only one study has directly examined, among nondaily smokers, the effects of VLNC cigarettes on drinking (Barrett et al., 2006), the reviewed literature highlights several interrelated mechanisms that reveal how a nicotine reduction policy could impact alcohol use. Each of these processes unfolds differently over time, which suggests that their relative influence on drinking could change in a time-dependent manner. In particular, among current smokers, switching to VLNC cigarettes will immediately and drastically reduce nicotine exposure, modestly increase withdrawal for approximately 2 weeks, and gradually decrease smoking behavior. Each of these processes appear to be positively related to drinking, suggesting that the effects of VLNC cigarettes on the intermediate processes would correspond with similar changes in alcohol use. First, there is convincing evidence that nicotine enhances the reinforcing properties of alcohol through several mechanisms. Thus, reducing nicotine exposure through VLNC cigarettes is expected to reduce alcohol reinforcement and use. Second, among a subset of smokers, nicotine withdrawal may increase motivation to drink alcohol in order to cope with the associated negative affect states. As a result, some smoker’s may increase alcohol use when withdrawal peaks during the first 2 weeks of switching to VLNC cigarettes. Third, smoking may act as a cue to drink, particularly among heavy drinkers and nondaily smokers. While the support for the pathway is relatively modest, decreased smoking rate and new associations between smoking cues and low doses of nicotine due to VLNC cigarette use could reduce the extent to which smoking behavior would be associated with drinking. Thus, as a whole, these processes may ultimately contribute to decreased alcohol use over time, outside of a short-term risk period following switching to VLNC cigarettes.
Preventing the initiation of smoking could also affect alcohol use through each of the previously described mechanisms, such as smoking cues and reinforcing effects of alcohol. Animal research has demonstrated that nicotine may facilitate alcohol self-administration among adolescent and adult alcohol-naive rats (Doyon et al., 2013; Kemppainen, Hyytiä, & Kiianmaa, 2009; Smith, Horan, Gaskin, & Amit, 1999), and the effect may be strongest among rats with an extensive nicotine self-administration history (Kemppainen et al., 2009). While the average age of onset for alcohol use tends to be younger than tobacco use (Parra, O’Neill, & Sher, 2003), smoking onset predicts drinking levels. Observational research suggests that smokers drink more and are at risk of heavy drinking relative to never-smokers (Grucza & Bierut, 2006; Harrison, Desai, & McKee, 2008; Weitzman & Chen, 2005), which suggests that preventing the initiation of smoking with VLNC cigarettes could positively impact alcohol use.
CONCLUSIONS AND FUTURE DIRECTIONS
Cigarette and alcohol use are closely related health behaviors and FDA regulations reducing the nicotine content of cigarettes could impact alcohol use among smokers. Reductions in nicotine exposure and the cues associated with smoking would be expected to decrease alcohol use over time, with nicotine exposure playing the most important role early in the public policy change and smoking behavior emerging as an important factor, particularly if smokers ultimately achieve abstinence. This conclusion is consistent with the existing literature suggesting that smoke-free legislation and tobacco taxes reduce drinking (McKee & Weinberger, 2013).
The present review adds to the existing literature by demonstrating that the mechanisms producing these effects can motivate drinking differently over time. There could be an important temporal pattern of effects that emerges as the potential influence of each pathway on alcohol use unfolds. As a result, research will need to be designed in such a way that facilitates examining the associations over time to estimate the effects of the regulations. Strategies including repeated measurements of alcohol use and intermediate processes and utilizing analytic techniques that examine these effects over time are critical to estimate the public health impact (e.g., time-varying effects model; Lanza, Vasilenko, Liu, Li, & Piper, 2013).
While switching to VLNC cigarettes could lower drinking rates, the review highlights the initial weeks after switching to VLNC cigarettes as a risk period for increased drinking. Withdrawal symptoms could promote drinking in order to regulate negative affective states through self-medication. This mechanism may be particularly important for individuals who smoke primarily to ward off withdrawal symptoms, like nicotine-dependent daily smokers. Fortunately, it is anticipated that the risk of this iatrogenic effect would be small and short-lived because VLNC cigarettes largely suppress withdrawal relative to complete smoking abstinence and withdrawal symptoms appears to dissipate within approximately 2 weeks, on average. Furthermore, depressed affect is most commonly associated with self-medication (Dermody et al., 2013; Hussong & Chassin, 1994; Hussong, Hicks, Levy, & Curran, 2001), but, on average, appears to be completely suppressed during the first 5 days of switching (Buchhalter, Acosta, et al., 2005; Donny & Jones, 2009). As the time course of nicotine withdrawal is complex and varies between symptoms (for review see Hughes, 2007), daily assessments of withdrawal symptoms that motivate self-medication beyond the first 5 days of switching could provide valuable insight into the progression of withdrawal.
The conclusions of the present review should be considered in light of the relatively homogenous samples examined in the research literature, particularly with regards to factors impacting the relative importance of positive and negative reinforcement processes in drug use. As a whole, the laboratory studies examining the effects of nicotine and smoking on alcohol use have primarily relied on young adults with little comorbidity or other tobacco product use. However, diversity in drug use motives and histories may correspond with varied effects of nicotine reduction on smoking behavior and withdrawal as well as differential effects of these intermediate processes on drinking. Future research of groups who could be at risk of withdrawal and subsequent self-medication is warranted and could help clarify to what extent VLNC cigarettes might have a negative impact on drinking. The review highlighted several subgroups, such as adult women, daily smokers, and individuals who have co-occurring psychiatric conditions or alcoholism. These subgroups appear to be at risk for both increased withdrawal and drinking to cope motives. It remains unclear how these individual difference factors play out in the context of long-term VLNC cigarette use. While one way to circumvent risk among these groups is to gradually reduce nicotine content because that appears, on average, to prevent withdrawal symptoms (Benowitz et al., 2012), this benefit needs to be weighed against potential delays in reductions in cigarettes smoked and nicotine dependence. Additional methods could include providing other sources of nicotine, such as nicotine replacement therapy (NRT), to assist with the transition to VLNC cigarettes.
Future research is also needed to evaluate the risk of co-use or product switching to compensate for the reduced nicotine levels of VLNC cigarettes, particularly among subgroups who tend to co-use tobacco products like young, white men (McClave-Regan & Berkowitz, 2011; Rath, Villanti, Abrams, & Vallone, 2012). To date, examinations of the effects of VLNC cigarettes have been conducted among smokers who do not regularly use other tobacco or nicotine products; however, about 6% of adolescents use smokeless tobacco products and a majority of them also smoke combustible tobacco products (Agaku, Ayo-Yusuf, Vardavas, Alpert, & Connolly, 2013). Reductions of nicotine in cigarettes could prompt increased use of other nicotine containing products, such as e-cigarettes, which could mitigate the anticipated effects of VLNC cigarette policies on alcohol use. Research that imitates a free market place by allowing participants to use other nicotine and tobacco products in tandem with VLNC cigarettes would be valuable when evaluating this outcome. Studies that have examined VLNC cigarette use alongside the nicotine patch suggest that cigarette use and nicotine exposure still decrease over time and at a faster rate than VLNC cigarettes alone (Donny & Jones, 2009; Hatsukami, Hertsgaard, et al., 2013). The faster reduction in cigarette use may result from the patch suppressing withdrawal symptoms that participants would otherwise try to suppress through continued smoking of VLNC cigarettes or their usual brand. Thus, it is possible that even with the increase use of alternative products, the decrease in cigarettes smoked and total nicotine exposure could reduce drinking.
The present review focused on the effects of VLNC cigarettes on alcohol use, given the widespread co-use. However, a similar framework can be applied to estimate potential consequences on the use of other substances and, more broadly, health behaviors. For individuals who frequently smoke cigarettes and use other substances, reductions in cigarettes smoked could produce similar reductions in other substances used through cued-reactivity and reward enhancement mechanisms. As nicotine administration enhances responding to other reinforcers, the effect likely applies to substances outside of alcohol (Chaudhri et al., 2006; Donny et al., 2003). Furthermore, like with alcohol use, individuals who tend to self-medicate negative affect by engaging in negative health behaviors and other substance use could engage in these behaviors while experiencing withdrawal.
While an important outcome of making cigarettes less addictive is reducing smoking rates, it is necessary to broadly define public health impact to include unintended health consequences on nonsmoking behaviors. The present review demonstrates that VLNC cigarettes could impact a closely related health behavior, alcohol use, but that the effects of the policy on drinking could differ over time and among subpopulations. While the relation between VLNC cigarettes and alcohol use has only been observed in one study during a short timeframe (i.e., single laboratory session), the indirect pathways between the 2 behaviors have been more extensively studied and provide valuable insight into their direct relation. Specifically, it appears that reducing the nicotine content of cigarettes could have a broader positive impact on public health by also decreasing alcohol use.
FUNDING
Research reported in this publication was supported by the National Institute on Drug Abuse and FDA Center for Tobacco Products (CTP) (U54 DA031659). SSD was also supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (F31AA022291).
DECLARATION OF INTERESTS
None declared.
ACKNOWLEDGMENT
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the U.S. Food and Drug Administration.
REFERENCES
- Acheson A., Mahler S. V., Chi H., de Wit H. (2006). Differential effects of nicotine on alcohol consumption in men and women. Psychopharmacology, 186, 54–63. 10.1007/s00213-006-0338-y [DOI] [PubMed] [Google Scholar]
- Adhikari B., Kahende J., Malarcher A., Pechacek T., Tong V. (2009). Smoking-attributable mortality, years of potential life lost, and productivity losses–United States, 2000–2004. Journal of the American Medical Association, 301, 593–594. 10.1001/jama.301.6.593 [Google Scholar]
- Agaku I. T., Ayo-Yusuf O. A., Vardavas C. I., Alpert H. R., Connolly G. N. (2013). Use of conventional and novel smokeless tobacco products among US adolescents. Pediatrics, 132, e578–e586. 10.1542/peds.2013-0843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal D. P., Goedde H. W. (1992). Medicobiological and genetic studies on alcoholism. Role of metabolic variation and ethnicity on drinking habits, alcohol abuse and alcohol-related mortality. The Clinical Investigator, 70, 465–477. 10.1007/BF00210227 [DOI] [PubMed] [Google Scholar]
- Baker T. B., Brandon T. H., Chassin L. (2004). Motivational influences on cigarette smoking. Annual Review of Psychology, 55, 463–491. 10.1146/annurev.psych.55.090902.142054 [DOI] [PubMed] [Google Scholar]
- Baron R. M., Kenny D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182 [DOI] [PubMed] [Google Scholar]
- Barr R. S., Pizzagalli D. A., Culhane M. A., Goff D. C., Evins A. E. (2008). A single dose of nicotine enhances reward responsiveness in nonsmokers: Implications for development of dependence. Biological Psychiatry, 63, 1061–1065. 10.1016/j.biopsych.2007.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett S. P., Tichauer M., Leyton M., Pihl R. O. (2006). Nicotine increases alcohol self-administration in non-dependent male smokers. Drug and Alcohol Dependence, 81, 197–204. 10.1016/j.drugalcdep.2005.06.009 [DOI] [PubMed] [Google Scholar]
- Benowitz N. L. (2001). Compensatory smoking of low-yield cigarettes. National Cancer Institute. Risks associated with smoking cigarettes with low machine yields of tar and nicotine. Smoking and Tobacco Control Monograph No. 13, 39–63 [Google Scholar]
- Benowitz N. L., Dains K. M., Hall S. M., Stewart S., Wilson M., Dempsey D., Jacob P. (2012). Smoking behavior and exposure to tobacco toxicants during 6 months of smoking progressively reduced nicotine content cigarettes. Cancer Epidemiology, Biomarkers and Prevention, 21, 761–769. 10.1158/1055-9965.epi-11-0644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz N. L., Hall S. M., Stewart S., Wilson M., Dempsey D., Jacob P., 3rd (2007). Nicotine and carcinogen exposure with smoking of progressively reduced nicotine content cigarette. Cancer Epidemiology, Biomarkers and Prevention, 16, 2479–2485. 10.1158/1055-9965.epi-07-0393 [DOI] [PubMed] [Google Scholar]
- Benowitz N. L., Henningfield J. E. (1994). Establishing a nicotine threshold for addiction. The implications for tobacco regulation. New England Journal of Medicine, 331, 123–125 [DOI] [PubMed] [Google Scholar]
- Benowitz N. L., Jacob P., 3rd, Herrera B. (2006). Nicotine intake and dose response when smoking reduced-nicotine content cigarettes. Clinical Pharmacology and Therapeutics, 80, 703–714. 10.1016/j.clpt.2006.09.007 [DOI] [PubMed] [Google Scholar]
- Benwell M. E., Balfour D. J., Anderson J. M. (1988). Evidence that tobacco smoking increases the density of (-)-[3H]nicotine binding sites in human brain. Journal of Neurochemistry, 50, 1243–1247 [DOI] [PubMed] [Google Scholar]
- Bernert J. T., Jain R. B., Pirkle J. L., Wang L., Miller B. B., Sampson E. J. (2005). Urinary tobacco-specific nitrosamines and 4-aminobiphenyl hemoglobin adducts measured in smokers of either regular or light cigarettes. Nicotine and Tobacco Research, 7, 729–738. 10.1080/1462220050025976 [DOI] [PubMed] [Google Scholar]
- Blomqvist O., Hernandez-Avila C. A., Van Kirk J., Rose J. E., Kranzler H. R. (2002). Mecamylamine modifies the pharmacokinetics and reinforcing effects of alcohol. Alcoholism, Clinical and Experimental Research, 26, 326–331. 10.1111/j.1530-0277.2002.tb02541.x [PubMed] [Google Scholar]
- Buchhalter A. R., Acosta M. C., Evans S. E., Breland A. B., Eissenberg T. (2005). Tobacco abstinence symptom suppression: The role played by the smoking-related stimuli that are delivered by denicotinized cigarettes. Addiction (Abingdon, England), 100, 550–559. 10.1111/j.1360-0443.2005.01030.x [DOI] [PubMed] [Google Scholar]
- Buchhalter A. R., Schrinel L., Eissenberg T. (2001). Withdrawal-suppressing effects of a novel smoking system: Comparison with own brand, not own brand, and de-nicotinized cigarettes. Nicotine and Tobacco Research, 3, 111–118. 10.1080/14622200110042636 [DOI] [PubMed] [Google Scholar]
- Buisson B., Bertrand D. (2002). Nicotine addiction: The possible role of functional upregulation. Trends in Pharmacological Sciences, 23, 130–136. 10.1016/S0165-6147(00)01979-9 [DOI] [PubMed] [Google Scholar]
- Caggiula A. R., Donny E. C., Palmatier M. I., Liu X., Chaudhri N., Sved A. F. (2009). The role of nicotine in smoking: A dual-reinforcement model. In Rick A. Bevins & Anthony R. Caggiula (Eds.), The motivational impact of nicotine and its role in tobacco use (Vol. 5, pp. 91–109). University of Nebraska: Lincoln, NE; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter K. M., Hasin D. S. (1999). Drinking to cope with negative affect and DSM-IV alcohol use disorders: A test of three alternative explanations. Journal of Studies on Alcohol, 60, 694–704 [DOI] [PubMed] [Google Scholar]
- Carter B. L., Tiffany S. T. (1999). Meta-analysis of cue-reactivity in addiction research. Addiction (Abingdon, England), 94, 327–340. 10.1046/j.1360-0443.1999.9433273.x [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2011). Vital signs: Current cigarette smoking among adults aged ≥18 – United States 2005–2010. MMWR: Morbidity and Mortality Weekly Report, 60, 1207–1212 [PubMed] [Google Scholar]
- Chandra S., Shiffman S., Scharf D. M., Dang Q., Shadel W. G. (2007). Daily smoking patterns, their determinants, and implications for quitting. Experimental and Clinical Psychopharmacology, 15, 67–80. 10.1037/1064-1297.15.1.67 [DOI] [PubMed] [Google Scholar]
- Chaudhri N., Caggiula A. R., Donny E. C., Booth S., Gharib M., Craven L., … Sved A. F. (2006). Operant responding for conditioned and unconditioned reinforcers in rats is differentially enhanced by the primary reinforcing and reinforcement-enhancing effects of nicotine. Psychopharmacology, 189, 27–36. 10.1007/s00213-006-0522-0 [DOI] [PubMed] [Google Scholar]
- Chen W. J., Parnell S. E., West J. R. (2001). Nicotine decreases blood alcohol concentration in neonatal rats. Alcoholism, Clinical and Experimental Research, 25, 1072–1077. 10.1111/j.1530-0277.2001.tb02319.x [PubMed] [Google Scholar]
- Chi H., de Wit H. (2003). Mecamylamine attenuates the subjective stimulant-like effects of alcohol in social drinkers. Alcoholism, Clinical and Experimental Research, 27, 780–786. 10.1097/01.ALC.0000065435.12068.24 [DOI] [PubMed] [Google Scholar]
- Clark A., Lindgren S., Brooks S. P., Watson W. P., Little H. J. (2001). Chronic infusion of nicotine can increase operant self-administration of alcohol. Neuropharmacology, 41, 108–117. 10.1016/s0028-3908(01)00037-5 [DOI] [PubMed] [Google Scholar]
- Collins A. C., Burch J. B., de Fiebre C. M., Marks M. J. (1988). Tolerance to and cross tolerance between ethanol and nicotine. Pharmacology, Biochemistry, and Behavior, 29, 365–373. 10.1016/0091-3057(88)90170-0 [DOI] [PubMed] [Google Scholar]
- Collins C. C., Epstein D. H., Parzynski C. S., Zimmerman D., Moolchan E. T., Heishman S. J. (2010). Puffing behavior during the smoking of a single cigarette in tobacco-dependent adolescents. Nicotine and Tobacco Research, 12, 164–167. 10.1093/ntr/ntp176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Congress. (2009). Family Smoking Prevention and Tobacco Control Act. H.R. 1256. U.S. Congress. Washington, DC: U.S. Government Printing Office [Google Scholar]
- Cooney J. L., Cooney N. L., Pilkey D. T., Kranzler H. R., Oncken C. A. (2003). Effects of nicotine deprivation on urges to drink and smoke in alcoholic smokers. Addiction (Abingdon, England), 98, 913–921. 10.1046/j.1360-0443.2003.00337.x [DOI] [PubMed] [Google Scholar]
- Cooper M. L., Frone M. R., Russell M., Mudar P. (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology, 69, 990–1005. 10.1037/0022-3514.69.5.990 [DOI] [PubMed] [Google Scholar]
- Corrigall W. A. (1999). Nicotine self-administration in animals as a dependence model. Nicotine and Tobacco Research, 1, 11–20. 10.1080/14622299050011121 [DOI] [PubMed] [Google Scholar]
- Crabb D. W. (1995). Ethanol oxidizing enzymes: Roles in alcohol metabolism and alcoholic liver disease. Progress in Liver Diseases, 13, 151–172 [PubMed] [Google Scholar]
- Davis T. J., de Fiebre C. M. (2006). Alcohol’s actions on neuronal nicotinic acetylcholine receptors. Alcohol Research and Health, 29, 179–185 [PMC free article] [PubMed] [Google Scholar]
- Dermody S. S., Cheong J., Manuck S. (2013). An evaluation of the stress-negative affect model in explaining alcohol use: The role of components of negative affect and coping style. Substance Use and Misuse, 48, 297–308. 10.3109/10826084.2012.761713 [DOI] [PubMed] [Google Scholar]
- Dohrman D. P., Reiter C. K. (2003). Ethanol modulates nicotine-induced upregulation of nAChRs. Brain Research, 975, 90–98. 10.1016/s0006-8993(03)02593-9 [DOI] [PubMed] [Google Scholar]
- Donny E. C., Chaudhri N., Caggiula A. R., Evans-Martin F. F., Booth S., Gharib M. A., … Sved A. F. (2003). Operant responding for a visual reinforcer in rats is enhanced by noncontingent nicotine: Implications for nicotine self-administration and reinforcement. Psychopharmacology, 169, 68–76. 10.1007/s00213-003-1473-3 [DOI] [PubMed] [Google Scholar]
- Donny E. C., Houtsmuller E., Stitzer M. L. (2007). Smoking in the absence of nicotine: Behavioral, subjective and physiological effects over 11 days. Addiction (Abingdon, England), 102, 324–334. 10.1111/j.1360-0443.2006.01670.x [DOI] [PubMed] [Google Scholar]
- Donny E. C., Jones M. (2009). Prolonged exposure to denicotinzied cigarettes with or without transdermal nicotine. Drug and Alcohol Dependence, 104, 23–33. 10.1016/j.drugalcdep.2009.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donny E. C., Taylor T. G., LeSage M. G., Levin M., Buffalari D. M., Joel D., Sved A. F. (2012). Impact of tobacco regulation on animal research: New perspectives and opportunities. Nicotine and Tobacco Research, 14, 1319–1338. 10.1093/ntr/nts162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyon W. M., Dong Y., Ostroumov A., Thomas A. M., Zhang T. A., Dani J. A. (2013). Nicotine decreases ethanol-induced dopamine signaling and increases self-administration via stress hormones. Neuron, 79, 530–540. http://dx.doi.org/10.1016/j.neuron.2013.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drobes D. J. (2002). Cue reactivity in alcohol and tobacco dependence. Alcoholism, Clinical and Experimental Research, 26, 1928–1929. 10.1097/01.ALC.0000040983.23182.3A [DOI] [PubMed] [Google Scholar]
- Evans S. E., Blank M., Sams C., Weaver M. F., Eissenberg T. (2006). Transdermal nicotine-induced tobacco abstinence symptom suppression: Nicotine dose and smokers’ gender. Experimental and Clinical Psychopharmacology, 14, 121–135. 10.1037/1064-1297.14.2.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk D. E., Yi H. Y., Hiller-Sturmhöfel S. (2006). An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Research and Health, 29, 162–171 [PMC free article] [PubMed] [Google Scholar]
- Frezza M., di Padova C., Pozzato G., Terpin M., Baraona E., Lieber C. S. (1990). High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. The New England Journal of Medicine, 322, 95–99. 10.1056/NEJM199001113220205 [DOI] [PubMed] [Google Scholar]
- George M. S., Anton R. F., Bloomer C., Teneback C., Drobes D. J., Lorberbaum J. P., … Vincent D. J. (2001). Activation of prefrontal cortex and anterior thalamus in alcoholic subjects on exposure to alcohol-specific cues. Archives of General Psychiatry, 58, 345–352. 10.1001/archpsyc.58.4.345 [DOI] [PubMed] [Google Scholar]
- Gritz E. R., Ippoliti A., Jarvik M. E., Rose J. E., Shiffman S., Harrison A., Vunakis H. V. (1988). The effect of nicotine on the delay of gastric emptying. Alimentary Pharmacology and Therapeutics, 2, 173–178. 10.1111/j.1365-2036.1988.tb00685.x [DOI] [PubMed] [Google Scholar]
- Grucza R. A., Bierut L. J. (2006). Cigarette smoking and the risk for alcohol use disorders among adolescent drinkers. Alcoholism, Clinical and Experimental Research, 30, 2046–2054. 10.1111/j.1530-0277.2006.00255.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison E. L., Desai R. A., McKee S. A. (2008). Nondaily smoking and alcohol use, hazardous drinking, and alcohol diagnoses among young adults: Findings from the NESARC. Alcoholism, Clinical and Experimental Research, 32, 2081–2087. 10.1111/j.1530-0277.2008.00796.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison E. L., McKee S. A. (2008). Young adult non-daily smokers: Patterns of alcohol and cigarette use. Addictive Behaviors, 33, 668–674. 10.1016/j.addbeh.2007.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey D. M., Yasar S., Heishman S. J., Panlilio L. V., Henningfield J. E., Goldberg S. R. (2004). Nicotine serves as an effective reinforcer of intravenous drug-taking behavior in human cigarette smokers. Psychopharmacology, 175, 134–142. 10.1007/s00213-004-1818-6 [DOI] [PubMed] [Google Scholar]
- Hatsukami D. K., Heishman S. J., Vogel R. I., Denlinger R. L., Roper-Batker A. N., Mackowick K. M., … Donny E. (2013). Dose-response effects of spectrum research cigarettes. Nicotine and Tobacco Research, 15, 1113–1121. 10.1093/ntr/nts247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami D. K., Hertsgaard L. A., Vogel R. I., Jensen J. A., Murphy S. E., Hecht S. S., … Allen S. S. (2013). Reduced nicotine content cigarettes and nicotine patch. Cancer Epidemiology, Biomarkers and Prevention, 22, 1015–1024. 10.1158/1055-9965.epi-12-1439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami D. K., Kotlyar M., Hertsgaard L. A., Zhang Y., Carmella S. G., Jensen J. A., … Stepanov I. (2010). Reduced nicotine content cigarettes: Effects on toxicant exposure, dependence and cessation. Addiction (Abingdon, England), 105, 343–355. 10.1111/j.1360-0443.2009.02780.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami D. K., Perkins K. A., LeSage M. G., Ashley D. L., Henningfield J. E., Benowitz N. L., … Zeller M. (2010). Nicotine reduction revisited: Science and future directions. Tobacco Control, 19, e1. 10.1136/tc.2009.035584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecht S. S., Murphy S. E., Carmella S. G., Li S., Jensen J., Le C., … Hatsukami D. K. (2005). Similar uptake of lung carcinogens by smokers of regular, light, and ultralight cigarettes. Cancer Epidemiology, Biomarkers and Prevention, 14, 693–698. 10.1158/1055-9965.EPI-04-0542 [DOI] [PubMed] [Google Scholar]
- Henningfield J. E., Benowitz N. L., Slade J., Houston T. P., Davis R. M., Deitchman S. D. (1998). Reducing the addictiveness of cigarettes. Council on Scientific Affairs, American Medical Association. Tobacco Control, 7, 281–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock V. M., Hesselbrock M. N. (2006). Are there empirically supported and clinically useful subtypes of alcohol dependence? Addiction (Abingdon, England), 101(suppl. 1), 97–103. 10.1111/j.1360-0443.2006.01596.x [DOI] [PubMed] [Google Scholar]
- Holt S., Stewart M. J., Adam R. D., Heading R. C. (1980). Alcohol absorption, gastric emptying and a breathalyser. British Journal of Clinical Pharmacology, 9, 205–208. 10.1111/j.1365-2125.1980.tb05834.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. R. (2007). Effects of abstinence from tobacco: Etiology, animal models, epidemiology, and significance: A subjective review. Nicotine & Tobacco Research, 9, 329–339. 10.1080/14622200701188927 [DOI] [PubMed] [Google Scholar]
- Hughes J. R., Higgins S. T., Hatsukami D. (1990). Effects of abstinence from tobacco: A critical review. In Kozlowski L. T., Annis H. M., Cappell H. D., Glaser F. B., Goodstadt M. S., Israel Y., Kalant H., Sellers E. M., Vingilis E. R. (Eds.), Research advances in alcohol and drug problems (Vol. 10, pp. 317–398). [Google Scholar]
- Hussong A. M., Chassin L. (1994). The stress-negative affect model of adolescent alcohol use: Disaggregating negative affect. Journal of Studies on Alcohol, 55, 707–718 [DOI] [PubMed] [Google Scholar]
- Hussong A. M., Hicks R. E., Levy S. A., Curran P. J. (2001). Specifying the relations between affect and heavy alcohol use among young adults. Journal of Abnormal Psychology, 110, 449–461. 10.1037//0021-843x.110.3.449 [DOI] [PubMed] [Google Scholar]
- Jackson K. M., Colby S. M., Sher K. J. (2010). Daily patterns of conjoint smoking and drinking in college student smokers. Psychology of Addictive Behaviors, 24, 424–435. 10.1037/a0019793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R. D., Horowitz M., Maddox A. F., Wishart J. M., Shearman D. J. (1991). Cigarette smoking and rate of gastric emptying: Effect on alcohol absorption. BMJ: British Medical Journal, 302, 20–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassel J. D., Greenstein J. E., Evatt D. P., Wardle M. C., Yates M. C., Veilleux J. C., Eissenberg T. (2007). Smoking topography in response to denicotinized and high-yield nicotine cigarettes in adolescent smokers. Journal of Adolescent Health, 40, 54–60. http://dx.doi.org/10.1016/j.jadohealth.2006.08.006 [DOI] [PubMed] [Google Scholar]
- Kassel J. D., Stroud L. R., Paronis C. A. (2003). Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychological Bulletin, 129, 270–304. 10.1037/0033-2909.129.2.270 [DOI] [PubMed] [Google Scholar]
- Kemppainen H., Hyytiä P., Kiianmaa K. (2009). Behavioral consequences of repeated nicotine during adolescence in alcohol-preferring AA and alcohol-avoiding ANA rats. Alcoholism, Clinical and Experimental Research, 33, 340–349. 10.1111/j.1530-0277.2008.00838.x [DOI] [PubMed] [Google Scholar]
- King A. C., de Wit H., McNamara P. J., Cao D. (2011). Rewarding, stimulant, and sedative alcohol responses and relationship to future binge drinking. Archives of General Psychiatry, 68, 389–399. 10.1001/archgenpsychiatry.2011.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouri E. M., McCarthy E. M., Faust A. H., Lukas S. E. (2004). Pretreatment with transdermal nicotine enhances some of ethanol’s acute effects in men. Drug and Alcohol Dependence, 75, 55–65. 10.1016/j.drugalcdep.2004.01.011 [DOI] [PubMed] [Google Scholar]
- Kozlowski L. T., Mehta N. Y., Sweeney C. T., Schwartz S. S., Vogler G. P., Jarvis M. J., West R. J. (1998). Filter ventilation and nicotine content of tobacco in cigarettes from Canada, the United Kingdom, and the United States. Tobacco Control, 7, 369–375. 10.1136/tc.7.4.369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E., Knibbe R., Gmel G., Engels R. (2006). Who drinks and why? A review of socio-demographic, personality, and contextual issues behind the drinking motives in young people. Addictive Behaviors, 31, 1844–1857. 10.1016/j.addbeh.2005.12.028 [DOI] [PubMed] [Google Scholar]
- Lanza S. T., Vasilenko S. A., Liu X., Li R., Piper M. E. (2013). Advancing the understanding of craving during smoking cessation attempts: A demonstration of the time-varying effect model. Nicotine & Tobacco Research. Advance online publication. 10.1093/ntr/ntt128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lê A. D., Corrigall W. A., Harding J. W., Juzytsch W., Li T. K. (2000). Involvement of nicotinic receptors in alcohol self-administration. Alcoholism, Clinical and Experimental Research, 24, 155–163. 10.1111/j.1530-0277.2000.tb04585.x [DOI] [PubMed] [Google Scholar]
- Leventhal A. M., Waters A. J., Boyd S., Moolchan E. T., Lerman C., Pickworth W. B. (2007). Gender differences in acute tobacco withdrawal: Effects on subjective, cognitive, and physiological measures. Experimental and Clinical Psychopharmacology, 15, 21–36. 10.1037/1064-1297.15.1.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieber C. S. (1994). Mechanisms of ethanol-drug-nutrition interactions. Clinical Toxicology, 32, 631–681. 10.3109/15563659409017974 [DOI] [PubMed] [Google Scholar]
- Lim R. T., Jr, Gentry R. T., Ito D., Yokoyama H., Baraona E., Lieber C. S. (1993). First-pass metabolism of ethanol is predominantly gastric. Alcoholism, Clinical and Experimental Research, 17, 1337–1344. 10.1111/j.1530-0277.1993.tb05250.x [DOI] [PubMed] [Google Scholar]
- Lucas D., Ferrara R., Gonzalez E., Bodenez P., Albores A., Manno M., Berthou F. (1999). Chlorzoxazone, a selective probe for phenotyping CYP2E1 in humans. Pharmacogenetics, 9, 377–388 [DOI] [PubMed] [Google Scholar]
- Lucas D., Ménez C., Girre C., Berthou F., Bodénez P., Joannet I., … Menez J. F. (1995). Cytochrome P450 2E1 genotype and chlorzoxazone metabolism in healthy and alcoholic Caucasian subjects. Pharmacogenetics, 5, 298. [DOI] [PubMed] [Google Scholar]
- Lucas D., Ménez C., Girre C., Bodénez P., Hispard E., Ménez J.-F. (1995). Decrease in cytochrome P4502E1 as assessed by the rate of chlorzoxazone hydroxylation in alcoholics during the withdrawal phase. Alcoholism: Clinical and Experimental Research, 19, 362–366. 10.1111/j.1530-0277.1995.tb01516.x [DOI] [PubMed] [Google Scholar]
- Macqueen D. A., Heckman B. W., Blank M. D., Janse Van Rensburg K., Evans D. E., Drobes D. J. (2012). Transient compensatory smoking in response to placebo cigarettes. Psychopharmacology, 223, 47–54. 10.1007/s00213-012-2685-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malson J. L., Sims K., Murty R., Pickworth W. B. (2001). Comparison of the nicotine content of tobacco used in bidis and conventional cigarettes. Tobacco Control, 10, 181–183. 10.1136/tc.10.2.181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C. S., Earleywine M., Musty R. E., Perrine M. W., Swift R. M. (1993). Development and validation of the Biphasic Alcohol Effects Scale. Alcoholism, Clinical and Experimental Research, 17, 140–146. 10.1111/j.1530-0277.1993.tb00739.x [DOI] [PubMed] [Google Scholar]
- Matsumoto M., Takahashi H., Maruyama K., Higuchi S., Matsushita S., Muramatsu T., … Ishii H. (1996). Genotypes of alcohol-metabolizing enzymes and the risk for alcoholic chronic pancreatitis in Japanese alcoholics. Alcoholism, Clinical and Experimental Research, 20(suppl. 9), 289A–292A [PubMed] [Google Scholar]
- McClave-Regan A. K., Berkowitz J. (2011). Smokers who are also using smokeless tobacco products in the US: A national assessment of characteristics, behaviours and beliefs of ‘dual users’. Tobacco Control, 20, 239–242. 10.1136/tc.2010.039115 [DOI] [PubMed] [Google Scholar]
- McClernon F. J., Van Voorhees E. E., English J., Hallyburton M., Holdaway A., Kollins S. H. (2011). Smoking withdrawal symptoms are more severe among smokers with ADHD and independent of ADHD symptom change: Results from a 12-day contingency-managed abstinence trial. Nicotine and Tobacco Research, 13, 784–792. 10.1093/ntr/ntr073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee S. A., Harrison E. L. R., O’Malley S. S., Krishnan-Sarin S., Shi J., Tetrault J. M., … Balchunas E. (2009). Varenicline reduces alcohol self-administration in heavy-drinking smokers. Biological Psychiatry, 66, 185–190. http://dx.doi.org/10.1016/j.biopsych.2009.01.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee S. A., O’Malley S. S., Shi J., Mase T., Krishnan-Sarin S. (2008). Effect of transdermal nicotine replacement on alcohol responses and alcohol self-administration. Psychopharmacology, 196, 189–200. 10.1007/s00213-007-0952-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee S. A., Weinberger A. H. (2013). How can we use our knowledge of alcohol-tobacco interactions to reduce alcohol use? Annual Review of Clinical Psychology, 9, 649–674. 10.1146/annurev-clinpsy-050212-185549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad A. H., Marks J. S., Stroup D. F., Gerberding J. L. (2004). Actual causes of death in the United States, 2000. JAMA: The Journal of the American Medical Association, 291, 1238–1245. 10.1001/jama.291.10.1238 [DOI] [PubMed] [Google Scholar]
- Nadal R., Chappell A. M., Samson H. H. (1998). Effects of nicotine and mecamylamine microinjections into the nucleus accumbens on ethanol and sucrose self-administration. Alcoholism, Clinical and Experimental Research, 22, 1190–1198. 10.1111/j.1530-0277.1998.tb03898.x [PubMed] [Google Scholar]
- Neale M. C., Kendler K. S. (1995). Models of comorbidity for multifactorial disorders. American Journal of Human Genetics, 57, 935–953 [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. (2004). Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review, 24, 981–1010. 10.1016/j.cpr.2004.08.003 [DOI] [PubMed] [Google Scholar]
- Novak A., Burgess E. S., Clark M., Zvolensky M. J., Brown R. A. (2003). Anxiety sensitivity, self-reported motives for alcohol and nicotine use, and level of consumption. Journal of Anxiety Disorders, 17, 165–180. 10.1016/S0887-6185(02)00175-5 [DOI] [PubMed] [Google Scholar]
- Palfai T. P., Monti P. M., Ostafin B., Hutchison K. (2000). Effects of nicotine deprivation on alcohol-related information processing and drinking behavior. Journal of Abnormal Psychology, 109, 96–105. 10.1037/0021-843X.109.1.96 [DOI] [PubMed] [Google Scholar]
- Parnell S. E., West J. R., Chen W. J. (2006). Nicotine decreases blood alcohol concentrations in adult rats: A phenomenon potentially related to gastric function. Alcoholism, Clinical and Experimental Research, 30, 1408–1413. 10.1111/j.1530-0277.2006.00168.x [DOI] [PubMed] [Google Scholar]
- Parra G. R., O’Neill S. E., Sher K. J. (2003). Reliability of self-reported age of substance involvement onset. Psychology of Addictive Behaviors, 17, 211–218. http://dx.doi.org/10.1037/0893-164X.17.3.211 [DOI] [PubMed] [Google Scholar]
- Perkins K. A. (1997). Combined effects of nicotine and alcohol on subjective, behavioral and physiological responses in humans. Addiction Biology, 2, 255–267 [DOI] [PubMed] [Google Scholar]
- Perkins K. A., Fonte C., Grobe J. E. (2000). Sex differences in the acute effects of cigarette smoking on the reinforcing value of alcohol. Behavioural Pharmacology, 11, 63–70 [DOI] [PubMed] [Google Scholar]
- Perkins K. A., Jacobs L., Sanders M., Caggiula A. R. (2002). Sex differences in the subjective and reinforcing effects of cigarette nicotine dose. Psychopharmacology, 163, 194–201. 10.1007/s00213-002-1168-1 [DOI] [PubMed] [Google Scholar]
- Perkins K. A., Karelitz J. L. (2013). Reinforcement enhancing effects of nicotine via smoking. Psychopharmacology, 228, 479–486. 10.1007/s00213-013-3054-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins K. A., Sexton J. E., DiMarco A., Grobe J. E., Scierka A., Stiller R. L. (1995). Subjective and cardiovascular responses to nicotine combined with alcohol in male and female smokers. Psychopharmacology, 119, 205–212 [DOI] [PubMed] [Google Scholar]
- Picciotto M. R., Addy N. A., Mineur Y. S., Brunzell D. H. (2008). It is not “either/or”: Activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Progress in Neurobiology, 84, 329–342. 10.1016/j.pneurobio.2007.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickworth W. B., Fant R. V., Nelson R. A., Rohrer M. S., Henningfield J. E. (1999). Pharmacodynamic effects of new de-nicotinized cigarettes. Nicotine and Tobacco Research, 1, 357–364. 10.1080/14622299050011491 [DOI] [PubMed] [Google Scholar]
- Pomerleau C. S., Marks J. L., Pomerleau O. F. (2000). Who gets what symptom? Effects of psychiatric cofactors and nicotine dependence on patterns of smoking withdrawal symptomatology. Nicotine and Tobacco Research, 2, 275–280. 10.1080/14622200050147547 [DOI] [PubMed] [Google Scholar]
- Pomerleau O. F., Pomerleau C. S., Mehringer A. M., Snedecor S. M., Ninowski R., Sen A. (2005). Nicotine dependence, depression, and gender: Characterizing phenotypes based on withdrawal discomfort, response to smoking, and ability to abstain. Nicotine and Tobacco Research, 7, 91–102. 10.1080/14622200412331328466 [DOI] [PubMed] [Google Scholar]
- Quinn P. D., Fromme K. (2011). Subjective response to alcohol challenge: A quantitative review. Alcoholism, Clinical and Experimental Research, 35, 1759–1770. 10.1111/j.1530-0277.2011.01521.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralevski E., Perry E. B., Jr, D’Souza D. C., Bufis V., Elander J., Limoncelli D., … McKee S. (2012). Preliminary findings on the interactive effects of IV ethanol and IV nicotine on human behavior and cognition: A laboratory study. Nicotine and Tobacco Research, 14, 596–606. 10.1093/ntr/ntr258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rath J. M., Villanti A. C., Abrams D. B., Vallone D. M. (2012). Patterns of tobacco use and dual use in US young adults: The missing link between youth prevention and adult cessation. Journal of Environmental and Public Health, 2012. http://dx.doi.org/10.1155/2012/679134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose J. E., Behm F. M. (2004). Effects of low nicotine content cigarettes on smoke intake. Nicotine and Tobacco Research, 6, 309–319. 10.1080/14622200410001676378 [DOI] [PubMed] [Google Scholar]
- Shiffman S. (2009). Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment, 21, 486–497. 10.1037/A0017074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Balabanis M., Fertig J., Allen J. (1995). Associations between alcohol and tobacco. Alcohol and tobacco: From basic science to clinical practice. NIAAA Research Monograph, 30, 17–36 [Google Scholar]
- Shiffman S., Paty J. A., Gnys M., Kassel J. D., Elash C. (1995). Nicotine withdrawal in chippers and regular smokers: Subjective and cognitive effects. Health Psychology, 14, 301–309. 10.1037/0278-6133.14.4.301 [DOI] [PubMed] [Google Scholar]
- Smith B. R., Horan J. T., Gaskin S., Amit Z. (1999). Exposure to nicotine enhances acquisition of ethanol drinking by laboratory rats in a limited access paradigm. Psychopharmacology, 142, 408–412 [DOI] [PubMed] [Google Scholar]
- Stratton K., Shetty P., Wallace R., Bondurant S. (2001). Clearing the smoke: The science base for tobacco harm reduction–executive summary. Tobacco Control, 10, 189–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas S. E., Drobes D. J., Deas D. (2005). Alcohol cue reactivity in alcohol-dependent adolescents. Journal of Studies on Alcohol, 66, 354–360 [DOI] [PubMed] [Google Scholar]
- Tidey J. W., Rohsenow D. J., Kaplan G. B., Swift R. M., Ahnallen C. G. (2013). Separate and combined effects of very low nicotine cigarettes and nicotine replacement in smokers with schizophrenia and controls. Nicotine and Tobacco Research, 15, 121–129. 10.1093/ntr/nts098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDHSS. (1988). Nicotine addiction: A report of the surgeon general. Rockville, MD: US Department of Health and Human Services Office of the Assistant Secretary for Health Office on Smoking and Health [Google Scholar]
- Veilleux J. C., Kassel J. D., Heinz A. J., Braun A., Wardle M. C., Greenstein J., … Conrad M. (2011). Predictors and sequelae of smoking topography over the course of a single cigarette in adolescent light smokers. The Journal of Adolescent Health, 48, 176–181. 10.1016/j.jadohealth.2010.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker N., Howe C., Bullen C., Grigg M., Glover M., McRobbie H., … Whittaker R. (2012). The combined effect of very low nicotine content cigarettes, used as an adjunct to usual Quitline care (nicotine replacement therapy and behavioural support), on smoking cessation: A randomized controlled trial. Addiction (Abingdon, England), 107, 1857–1867. 10.1111/j.1360-0443.2012.03906.x [DOI] [PubMed] [Google Scholar]
- Weinberger A. H., Desai R. A., McKee S. A. (2010). Nicotine withdrawal in U.S. smokers with current mood, anxiety, alcohol use, and substance use disorders. Drug and Alcohol Dependence, 108, 7–12. 10.1016/j.drugalcdep.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman E. R., Chen Y. Y. (2005). The co-occurrence of smoking and drinking among young adults in college: National survey results from the United States. Drug and Alcohol Dependence, 80, 377–386. 10.1016/j.drugalcdep.2005.05.008 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2003). WHO framework convention on tobacco control. A56/8. Geneva: WHO; Retrieved March 3, 2014 from http://whqlibdoc.who.int/publications/2003/9241591013.pdf?ua=1 [Google Scholar]
- Wills T. A., Shiffman S. (1985). Coping and substance use: A conceptual framework. In S. Shiffman & T. A. Wills (Eds.), Coping and substance use (pp. 3–24). Orlando, FL: Academic Press [Google Scholar]
- Young E. M., Mahler S., Chi H., de Wit H. (2005). Mecamylamine and ethanol preference in healthy volunteers. Alcoholism, Clinical and Experimental Research, 29, 58–65. 10.1097/01.ALC.0000150007.34702.16 [DOI] [PubMed] [Google Scholar]
- Zacny J. P. (1990). Behavioral aspects of alcohol-tobacco interactions. In Galanter M. (Ed.), Recent developments in alcoholism: An official publication of the American Medical Society on Alcoholism, the Research Society on Alcoholism, and the National Council on Alcoholism (Vol. 8, pp. 205–219). New York: Plenum; [PubMed] [Google Scholar]
- Zeller M., Hatsukami D; Strategic Dialogue on Tobacco Harm Reduction Group. (2009). The Strategic Dialogue on Tobacco Harm Reduction: A vision and blueprint for action in the US. Tobacco Control, 18, 324–332. 10.1136/tc.2008.027318 [DOI] [PMC free article] [PubMed] [Google Scholar]


