Abstract
There is this wrong notion that the only standard abdominal incision is the midline incision. Cases have been seen in which an abdominal incision extends from the xyphoid process to the symphysis pubis just to remove a perforated appendix! It is also not unusual to see a groin incision together with a lower abdominal incision for an obstructed inguinal hernia repair that “slipped” back into the abdominal cavity during preparation for surgery. Even though the trend nowadays in surgery is to opt for laparoscopic and mini-incision surgery, the basic rule in surgery is to have an incision that will be comfortable for the surgeon and provide adequate access to the area of pathology.
Keywords: Incisions, Abdomen, General Surgery
Introduction
What prompted this review article is because of the wrong notion that the only standard abdominal incision is the midline incision. Cases have been seen in which an abdominal incision extends from the xyphoid process to the symphysis pubis just to remove a perforated appendix! The reason proffer for this was “……we thought the patient had a perforated duodenal ulcer, so we made an upper midline incision. On exploring the abdomen we found out that it was a perforated pelvic appendix, so we extended our upper midline incision downwards to have adequate access to remove the appendix”!
It is also not unusual to see a groin incision together with a lower abdominal incision for an obstructed inguinal hernia that “slipped back” into the abdominal cavity during preparation for repair.
One of the most underrated aspects of surgical procedure is the placement of skin incisions. The purpose of this paper is to identify various types of abdominal incisions that make certain surgical procedure a bit easier, and to avoid unnecessary long abdominal incisions.
Materials and methods
A literature search was performed using PubMed, MEDLINE/Index Medicus, and the internet. Also, Atlas of Surgical Procedures, and some described procedures in some surgical textbook of surgery were consulted. Personal notes on operative surgery were also used. Only studies in English language were considered and used for this review article.
1. Equivocal Incision
When confronted with an undiagnosed non-traumatic “acute abdomen”, sometimes it is usually very difficult to know where to place the incision since the cause of the “acute abdomen” may not be known preoperatively. Sometimes the surgeon enters the abdomen by making an upper midline incision, only to find out on entering the abdomen that the cause of the acute abdomen is in the pelvis! He will therefore have no choice but to extend the upper midline incision down to the pelvic area! This will then produce a situation in which an appendix or a twisted ovarian cyst or ileal typhoid perforation are surgically treated with an incision from the xyphoid process to the symphysis pubis!
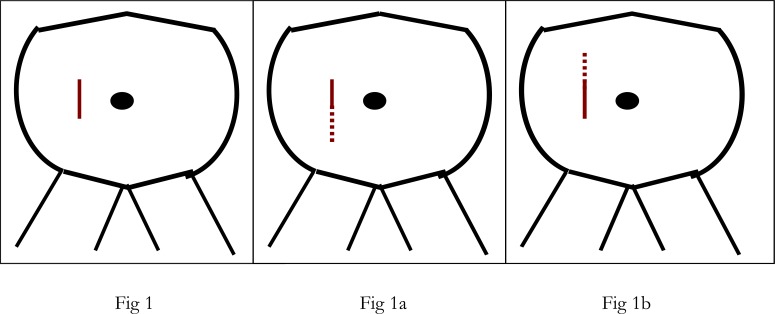
The equivocal incision (fig 1) is designed to avoid this embarrassment. This incision is made initially about 2ins above and 2ins below the level of the umbilicus in the right paramedian area (fig 1). The right paramedian area is selected and not the left because conditions that can cause acute abdomen, and that may be difficult to diagnose preoperatively are on the right side of the abdomen. Examples are liver abscess, inflammatory biliary tract disease, perforated duodenal ulcer, Meckel’s diverticulitis, ileal typhoid perforation, mesenteric lymphadenitis, and appendicitis. Inflamed organs on the left side of the abdomen tend not to cause much diagnostic problems preoperatively, and therefore initial adequate surgical incision can therefore be planned accordingly.
Fig 1.
This equivocal incision can be either muscle-splitting or muscle retracting. Once the abdomen has been entered through this 4-inch equivocal incision, an assessment can be made as to the area where the pathology is. The incision is then extended downwards (fig 1a), or upwards (fig 1b) for adequate exposure to deal with the pathology depending on where it is. This equivocal incision if placed lower can also be regarded as a right paramedian incision (1)
2. Inguinal Incision
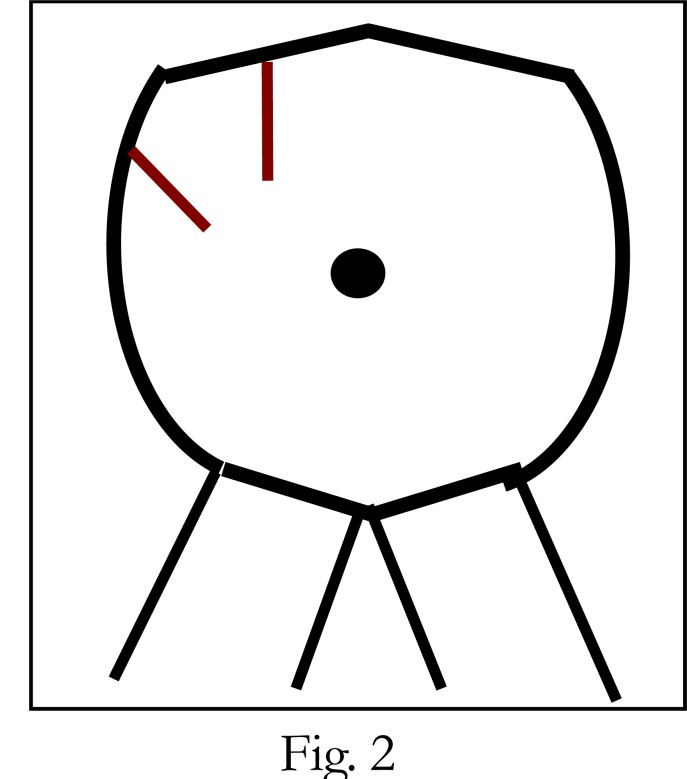
This is the standard incision for inguinal herniorrhaphy. However, in obstructed inguinal hernia, during an attempt to operate on the patient, after anaesthesia and during skin preparation for surgery, the obstructed loop may slip back inside the abdomen because of the relaxation of the muscle. It is not necessary to make another lower abdominal incision (fig 2) in an effort to retrieve the loop of bowel for inspection to see if it is gangrenous or not. What needs to be done is to widen the ring at the groin, where the loop was initially trapped and then grab with a Babcock forceps the loop of bowel from the inside of the abdominal cavity and with a gentle traction pull out the loop from the widened internal ring for inspection.
Fig 2.
Not Recommended
If there is a gangrenous segment, resection and anastomosis can be performed through this area, and then the loop returned back into the abdominal cavity. Herniorrhaphy can then be performed to close the defect. Any structure that cannot be pulled out from this widened internal ring while applying gentle traction on the loop with a Babcock forceps did not come out initially, and therefore was not trapped in the inguinal ring, and therefore inspection is not necessary. For cosmetic reasons, skin incision nowadays for herniorrhaphy is usually a curvilineal incision along the skin crease. The skin can then be reflected as necessary to expose the internal and the external rings. (The fig 2 above is not recommended)
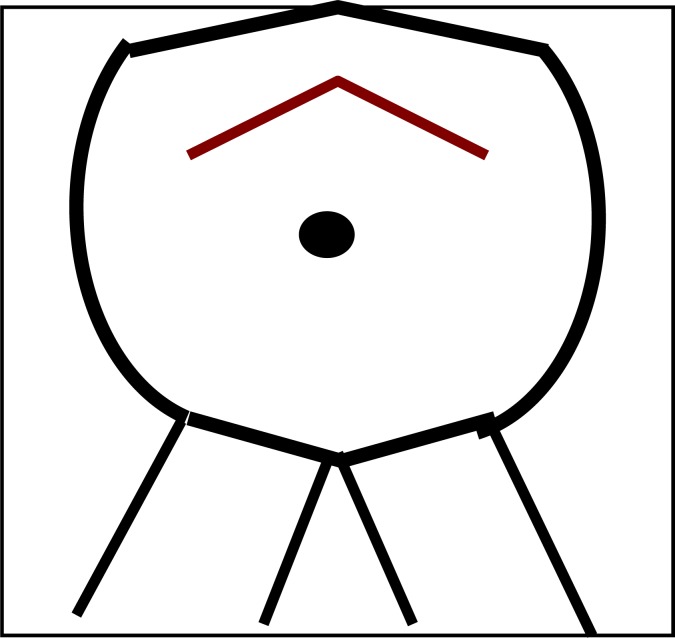
3. Bucket Handle Incision (fig 3)
Fig 3.
In the early years of kidney transplantation (2) surgery, this incision was very popular in preparing a kidney recipient for transplantation. Preparation of a potential recipient in those days included (i) vagotomy and pyloroplasty. This is to prevent ulcer diathesis that may occur as a result of steroid therapy following transplantation; (ii) splenectomy, to reduce immune cells that may enhance rejection; (iii) appendectomy, because the donor kidney is usually placed in the right lower quadrant of the recipient, it is therefore essential not to confuse an attack of appendicitis with the pain of early kidney rejection, since the appendix has been removed; (iv) bilateral nephrectomy (although this is no more considered necessary); and (v) oophorepexy in females. This is to hide the ovaries under the pubic bone to avoid the effect of radiation on the ovaries when the transplanted donor kidney is irradiated immediately after transplantation to destroy initial immune cells that might attack the donor kidney. This bucket-handle incision which is essentially a joined bilateral subcostal incision allows easy access to all these areas, and allows all these surgical procedures to be performed at the same time through this single incision. The healing of this incision is very good even though many of the patients are anaemic and have some degree of uremia.
4. Left Subcostal Incision
This is ideal for an elective splenectomy especially if the spleen is very enlarged as in cases of tropical splenomegaly syndrome (3),(4) and in Hassab’s operation (5),(6),(7) for oesophageal varices. It also provides easy access to the upper part of the stomach and intraabdominal oesophagus. This incision is also ideal for devascularisation of the upper part of oesophagus as in Hassab’s and Sugiura operations for oesophagel varices (5),(6)
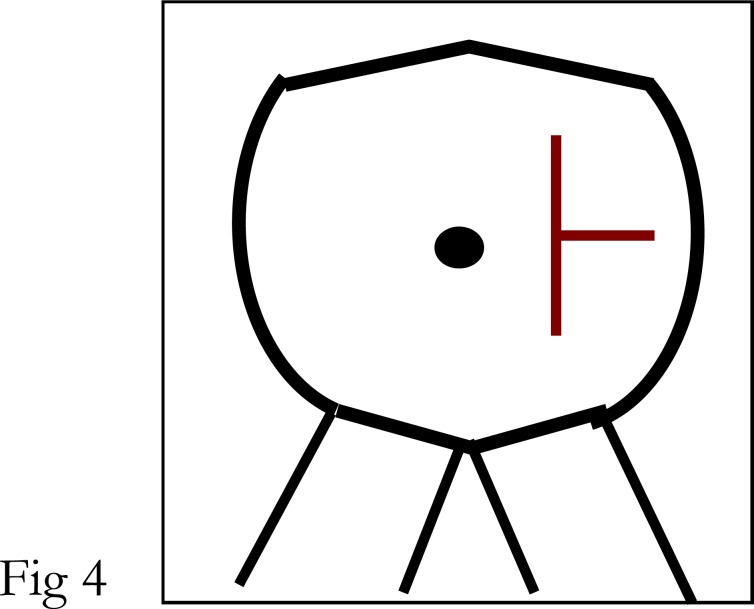
5. Marwedel Incision (fig4) (1)
Fig 4.
This incision gives good access to the liver especially the left lobe, stomach, spleen, hepatic flexure, splenic flexure and transverse colon. The only problem is that the “T” junction may not heal properly initially.
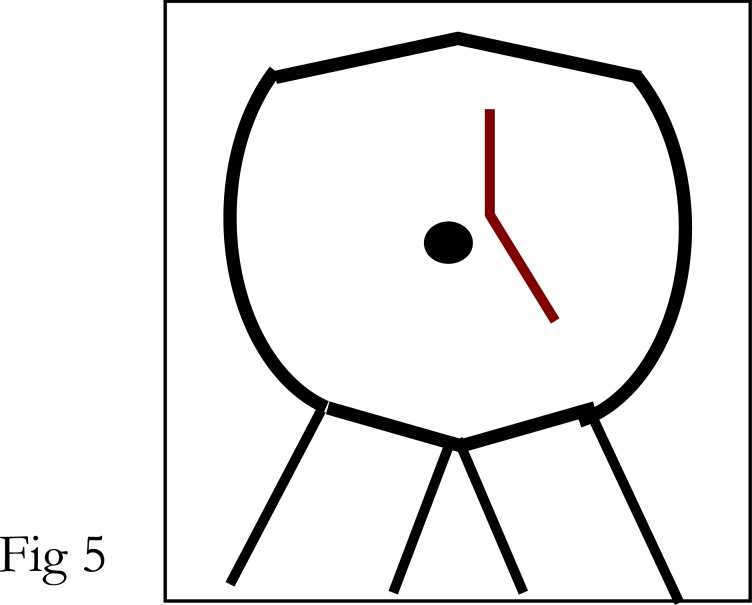
6. Bevan Incision (fig 5) (1)
Fig 5.
This incision serves a similar purpose as Marwedel incision. The advantage here is that there is no “T” junction to worry about in the healing process.
7. Right Subcostal Incision (Kocher’s) incision (1),(8)
This is a very popular incision for biliary tract surgery especially for cholecystectomy. However when biliary exploration or biliary anastomosis with a segment of bowel is needed, it may not be very suitable.
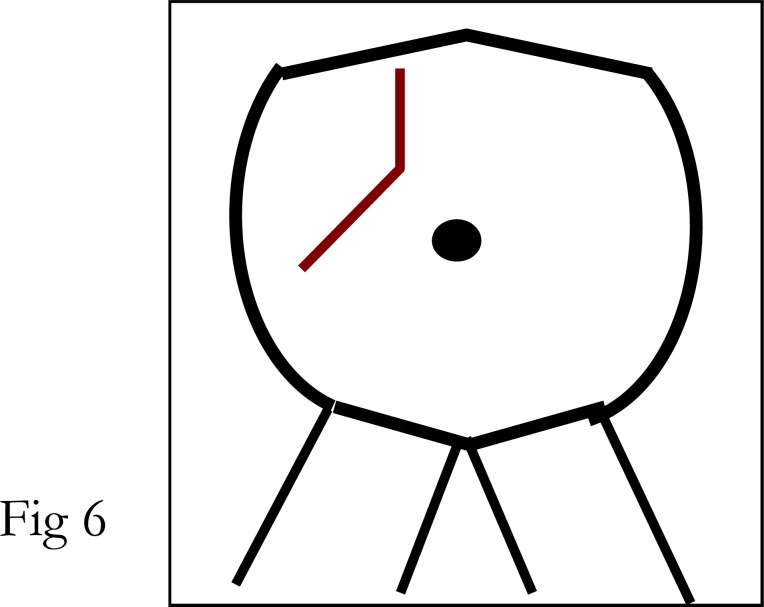
8. Kehr Incision (fig 6) (1),(8)
Fig 6.
This incision is more suitable than Kocher’s incision when biliary tract anastomosis is desired. It is therefore ideal for choledocho-duodenostomy, choledochojejunostomy, and cholecysto-jejunostomy.
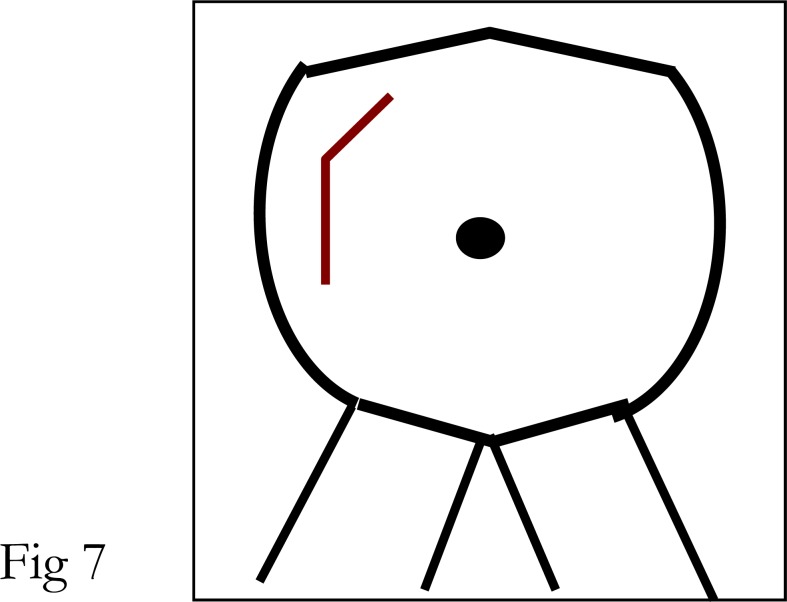
9. Mayo-Robson Incision (fig 7) (1)
Fig 7.
This is also regarded as a “hockey stick” incision. It is essentially a reverse of the Kehr incision. But also serves the same purpose in terms of exposure for a surgical procedure.
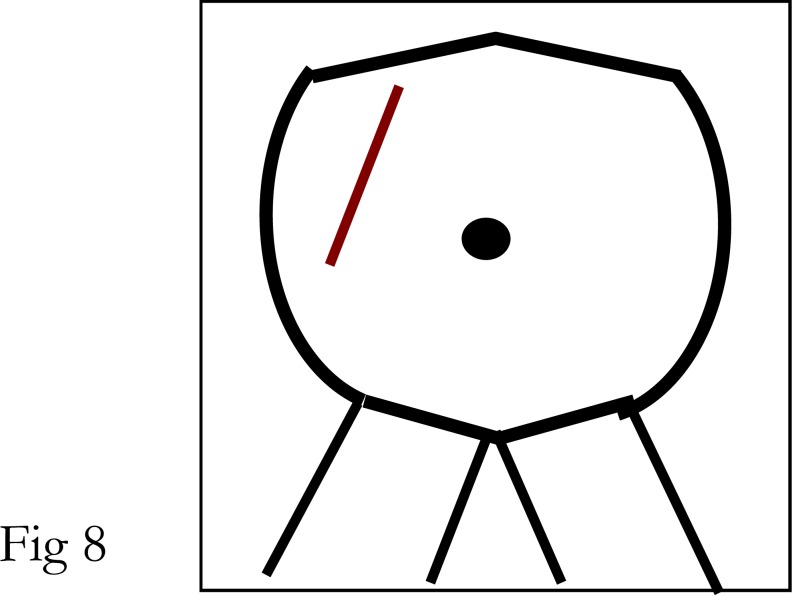
10. Masson Incision (fig 8) (1)
Fig 8.
This incision serves the same purpose as Mayo- Robson and Kehr incisions. In this case the rectus abdominal muscle may have to be cut in a diagonal manner.
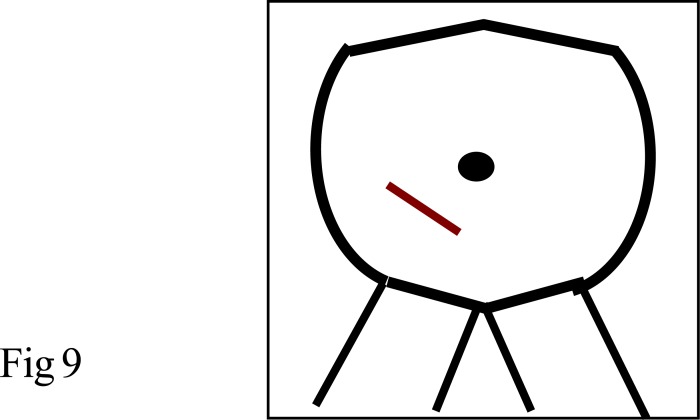
11. McBurney Incision (fig 9) (1),(8),(9),(10)
Fig 9.
This is one of the earliest incisions for appendicitis. It is also referred to as “Grid iron” incision. It is a popular incision for appendicitis.
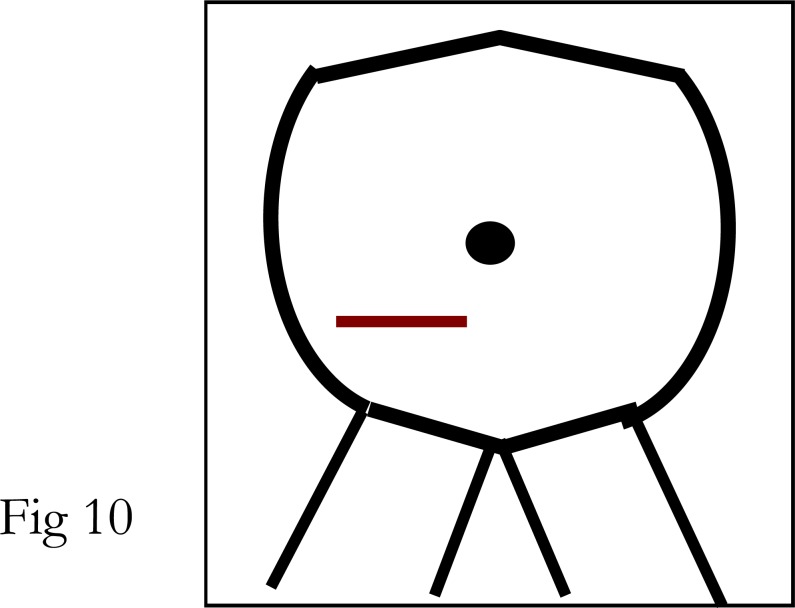
12. Transverse or Davis-Rockey Incision (fig 10) (10)
Fig 10.
This transverse incision is preferred by many for the removal of appendix because it gives a better cosmeticscar on healing and the incision can easily be extended medially during surgery if needed.
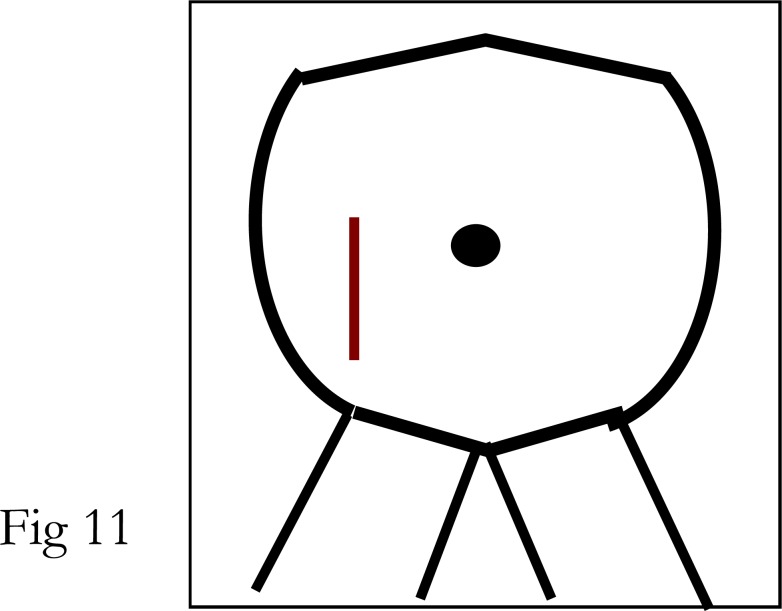
13. Battle-Jalaquier-Kammerer-Lennander Incision (fig 11) (1)
Fig 11.
This is usually referred to as Battle incision for short. It is a lower right paramedian incision but placed more laterally than the standard paramedian incision. It is suitable for dealing with acute appendicitis and pathologies in the right lower quadrant of the abdomen.
14. Pfannenstiel Incision (fig 12) (1),(8)
Fig 12.
This is a popular incision in gynaecological pelvic surgery. It has good cosmetic effect. It is also suitable for prostatic surgery in men.
15. Thoraco-abdominal Incision
Any of the appropriate upper abdominal incision can be combined with a thoracotomy incision to form a thoraco-abdominal incision. This is ideal for surgery of the lower oesophagus, surgery of the cardiac portion of the stomach and resection of lower oesophagus.
Discussion
The basic rule in surgery is to make an incision big enough and adequately placed to allow a comfortable access to the area of operation. Now with minimal invasive surgical procedures and laparoscopic surgery, pendulum seems to be shifting from “big to small”. However the important thing is that the incision should be such that the operating surgeon is comfortable with the exposure and access.
Generally, upper abdominal incision can be midline through the lineal alba or paramedian. The paramedian incision can be mucle- retracting or muscle-splitting (1), (8). If necessary, the midline incision may be extended through the umbilicus or by the side of umbilicus. Incision through the umbilicus has no negative effect on wound healing. The upper abdominal incision gives good access to the viscera in the upper abdomen and this incision can be combined with a thoracotomy for oesophageal surgery.
Lower abdominal incisions can also be midline, paramedian or pfannenstiel incisions. The pfannestiel incision produces a good cosmetic effect, and when possible should be routinely used in women with pelvic gynaecological pathologies.
There is a general belief that subcuticular closure of skin incision is not suitable for a potentially infected wound. This is not always the case. An unpublished data has shown that using subcuticular closure for skin incision does not have much adverse effect on the wound, even if the wound is potentially infected. Using an absorbable suture material like chromic catgut for subcuticular closure allows early discharge since there is no need to remove the suture. Non-absorbable suture materials like prolene or nylon sutures are also ideal for subcuticular skin closure. But these have to be removed later after the healing process has been completed. An alternative to subcuticular closure is to close the skin incision using vertical-mattress-alternatingwith- simple suture method. The vertical mattress suture evert the cut edges and the simple suture invert the skin edges, thus giving rise to good skin approximation.
Nowadays, the groin incisions for herniorrhaphy is placed along the skin crease in the groin to form a curvilineal incision. With this, adequate hernia repair can be performed, and it also gives a good cosmetic result.
Conclusion
Even though the trend in surgery nowadays is to opt for laparoscopic and mini-incisions, it is essential to be familiar with the location of various skin incisions that will provide easy and adequate access to the area of pathology.
Acknowledgement
I thank my daughter, Miss Olubunmi Olukemi Ajao for producing the illustrations in this paper
REFERENCES
- 1.Madden JL, editor. General and Abdominal Surgery. Second. Vol. 1. New York: Appleton-Century-Crofts; 1958. Atlas of technics in surgery; pp. 26–99. [Google Scholar]
- 2.Ajao OG, Callender CO, Stevens J, Sampson C. Spontaneous renal allograft rupture 4 years after transplantation. Urol Int. 1984;39:49–51. doi: 10.1159/000280944. [DOI] [PubMed] [Google Scholar]
- 3.Ajao OG. Tropical splenomegaly: surgical aspects. Trans Roy Soc Trop Med & Hyg. 1981;75:877–881. doi: 10.1016/0035-9203(81)90437-5. [DOI] [PubMed] [Google Scholar]
- 4.Ajao OG. Enlarged spleen syndrome. J Natl Med Assoc. 1980;72:323–325. [PMC free article] [PubMed] [Google Scholar]
- 5.Hassab MA. Gastroesophageal decongestion and splenectomy in the treatment of oesophageal varices in bilharzial cirrhosis. Surg. 1967;61:169–176.3. [PubMed] [Google Scholar]
- 6.Sugiura M, Futagawa S. Further evaluation of the Sugiura procedure in the treatment of oesophageal varices. Arch Surg. 1977. pp. 1317–1320. [DOI] [PubMed]
- 7.Ajao OG, Ajayi OO, Soyanwo OA, et al. Cup-and-spill gastric deformity following Hassab’s procedure for oesophageal varices: Case report. East Afr J Med. 1995;72:468–470. [PubMed] [Google Scholar]
- 8.Rob C, Smith R, Morgan CN, editors. Operative Surgery. Abdomen and Rectum and Anus. Second. London: Butterworths; 1969. pp. 6–16. [Google Scholar]
- 9.Condon RE. Appendicitis in Davis-Christopher textbook of Surgery. Sabiston. Tenth. Philadelphia, London, Toronto: W.B. Saunders; 1972. pp. 933–934. [Google Scholar]
- 10.Storer EH. In: Appendix in Principles of Surgery. Schwartz SI, editor. New York, Toronto, Sydney, London: McGraw-Hill Book Company; 1969. p. 1027. [Google Scholar]